- 1College of Medicine, King Saud bin Abdulaziz University for Health Sciences, Jeddah, Saudi Arabia
- 2King Abdullah International Medical Research Center (KAIMRC), Jeddah, Saudi Arabia
- 3Department of Clinical Pharmacy, College of Pharmacy, Taif University, Taif, Saudi Arabia
- 4Department of Pharmaceutical Sciences, Fakeeh College for Medical Sciences, Jeddah, Saudi Arabia
Medical students experience significant stress, which may interfere with their sleeping routines; consequently, they are at a higher risk of misusing sleeping pills. Therefore, this cross-sectional convenience sampling study aims to evaluate medical students’ attitudes toward the usage of sleeping pills, as well as the prevalence of their misuse and the associated factors. A self-administered online questionnaire survey was completed by 338 medical students at the College of Medicine of the King Saud bin Abdulaziz University for Health Sciences. Of 338 participants, 84 (24.85%) reported using sleeping pills. The prevalence of sleeping pill misuse was 26.63% (n = 90). The most common misuse behavior of sleeping pills was self-prescription (n = 72, 21.30%). The factors associated with sleeping pill misuse were stimulants usage (n = 69, 92%, p = 0.0072), high grade point average (n = 63, 84%, p = 0.046), preclinical years (n = 52, 69.3%, p = 0.042), and longer average time required to fall asleep (n = 53, 70.7%, p = 0.008). The prevalence of sleeping pill misuse is high among medical students, particularly among those in preclinical years. Therefore, enhancing awareness regarding sleeping pill misuse is crucial. This can be achieved through campaigns, workshops, and providing information regarding the dangers of sleeping pill misuse in the curriculum.
1 Introduction
Medical students are often vulnerable to anxiety and stress due to medicine being a highly demanding career choice, both academically and professionally. Excessive stress can result in health problems, which can lower students’ self-esteem and affect their academic performance. Medical students may experience harmful effects as a consequence of excessive stress, which could impact their cognitive functioning and learning. If left unmanaged, any form of stress can lead to sleeping problems, burnout, and dropout (1–4).
Research from Canada and the United States indicates a higher prevalence of depression, anxiety, and psychological issues among medical students, compared with the general population (5). Possible sources of recurrent stress and anxiety include high curriculum difficulty, which requires students to cover large amounts of information within a short time span, and frequent examinations. Other sources of stress involve personal competency, endurance, and external life events. Furthermore, an increase in concern was linked to a rise in stress and anxiety. Meanwhile, social and personal issues in students’ daily lives comprise another source of stress and anxiety that must be dealt with through adequate stress management strategies (6, 7).
Among Saudi students of the King Faisal University’s College of Medicine (COM), the prevalence of stress was reported to be 53% in 2013 (8). Moreover, research conducted at a medical university in the United Arab Emirates revealed a significant association between stress and psychological morbidity (9). Another study conducted at the King Saud bin Abdulaziz University for Health Sciences revealed a significant link between poor sleep quality and stress (1). Students who experienced stress were more likely to have poor sleep quality, while students with a cumulative grade point average (GPA) lower than 4.25 were approximately four times more likely to have poor sleep quality (1). Psychological stress can result in depression and have other negative effects on students, such as reduced performance in classes or clinical practice and poor sleep quality (8, 10, 11). Stress is a major problem for medical students both in Saudi Arabia and worldwide. Therefore, investigating stress management techniques for this population is crucial. Some effective coping strategies for stress include time management and academic counseling (12). However, some students may indulge in unhealthy coping behaviors, such as the misuse of drugs.
According to a study conducted at a Pakistani medical school, drug misuse was reported by 4.9% of students (13). Moreover, studies have shown that the most common motives for prescription drug misuse among university students include personal enhancement related to sports and educational attainment, mental health (e.g., sleep disturbances and anxiety), or physical health (e.g., managing pre-existing illnesses). Fewer than half of the users said they were involved in prescription drug misuse for recreational purposes (e.g., to party, get high, experiment) (14).
The World Health Organization defines the misuse of medication as “the use of a substance for a purpose not consistent with legal or medical guidelines.” Additionally, self-prescription is defined as “the selection and use of medicines/medicinal products, including herbal and traditional products by individuals, to treat self-recognized illness or symptoms, or the intermittent or continued use of a medication prescribed by a physician for chronic or recurring diseases or symptoms” (15). A study conducted at King Khalid University revealed that 98.7% of students reported self-medication. The primary sources of information for self-medication were self-knowledge, relatives, pharmacists, and friends (16).
Medication misuse can negatively affect students’ performance as well as their psychological and physical health, and can cause adverse long-term consequences (17). One of the most commonly abused categories of prescription medications is Central Nervous System (CNS) depressant drugs; these medications slow brain activity, making them useful for treating anxiety, panic, acute stress reactions, and sleep disorders (18, 19). CNS depressants include sedatives, drugs used for treating sleep disorders, hypnotics, and sleeping pills (18). The term “sleeping pill” is a generic term referring to prescription or over-the-counter drugs that promote, induce, or maintain sleep (20). Sleeping pill use can have serious side effects and may even result in addiction if used over a long period, leading to long-term health consequences, including disturbed thinking, headaches, constipation or diarrhea, and muscle weakness (20).
In recent years, the use of CNS-depressant drugs by medical students and doctors has attracted attention and concern from researchers, educational institutions, and medical societies. A study conducted at the King Saud University in 2011 found that 17% of medical students reported sedative drug use at some time since enrollment (12). Other studies have shown similar findings, thus confirming that the use of CNS-depressant drugs is prevalent among medical students, which makes this a sensitive and important issue (21, 22).
Although previous studies indicate that medical students’ use of CNS-depressant drugs is prevalent, no study has assessed Saudi Arabian medical students’ attitudes toward sleeping pill usage or identified the factors associated with the misuse. Therefore, this study primarily aimed to investigate the attitudes of medical students at the King Saud bin Abdulaziz University for Health Sciences toward sleeping pill usage. We also aimed to estimate the prevalence of sleeping pill misuse and determine the factors that contribute to such behavior.
2 Materials and methods
2.1 Study design, setting, and participants
A self-administered online questionnaire survey was conducted in this cross-sectional convenience sampling study. The study included students attending the college of medicine (COM) at the King Saud bin Abdulaziz University for Health Sciences. The COM is located within the King Abdulaziz Medical City and has two branches—in Riyadh and in Jeddah. In the 2019–2020 academic year, there were 1,177 and 781 COM attendees at the Riyadh and Jeddah branches, respectively, totaling 1,958 students. The only inclusion criterion was regularly attending the COM; thus, no exclusion criteria were stipulated. The sample size was calculated using Raosoft software (23). The required sample size was estimated at a 95% confidence level with a 50% assumed prevalence of sleeping pill usage and a 5% margin of error. The recommended sample size was determined to be 322. The survey was distributed from 2 September 2021 to 14 December 2021. The survey questionnaire was developed by the authors, based on a previously published validated questionnaire, with minor modifications, to evaluate both quantitative and qualitative variables (12). To retest the questionnaire, a pilot study was performed on a sample of 10 students to assess data-gathering procedures and ensure the reliability of the questionnaire. Any required modifications were then made. The participants were informed of the purpose of the research and their right to refuse participation, and that their personal information would be kept completely confidential.
2.2 Data collection
The self-administered questionnaire comprised 20 questions, divided into three sections. The first section was aimed at collecting socio-demographic information: age, gender, residence, stream, college branch (Riyadh or Jeddah), academic year, GPA, and smoking status. The university accepts students who have graduated from other specialties; this path is called stream II, while stream I refers to students whose first specialty after high school was medicine. Academic years were also subdivided, based on the university’s curriculum, where the first year is a foundation year in which students are not enrolled in the COM; years 2–4 comprise the preclinical phase, and years 5 and 6 comprise the clinical phase. The first section of the survey also included questions regarding physical exercise, use of any type of stimulants during the exam period, and additional information regarding sleeping status to assess sleep pattern and quality and any sleeping disorders. The third section was preceded by a one-question section where participants were asked whether they had ever used sleeping pills after entering COM; based on their answers, respondents were either directed to the third section or to the end of the survey. The third section comprised four questions that investigated participants’ use of sleeping pills, wherein they specified the name of the drug used, either by writing the name or choosing from a list containing the names of some of the most commonly used sleeping pills. The students were also asked about the reasons for their sleeping pill usage, whether they consumed the pills in greater amounts than recommended, and their frequency of consumption. In summary, the third section was intended to gather information regarding the misuse of sleeping pills and to determine its prevalence.
2.3 Data analysis
Data analysis was conducted using Microsoft Excel 2016 and IBM® SPSS Statistics version 28.0 software (IBM Corp., Armonk, NY, USA). Descriptive statistics were used, and the dataset (demographic characteristics, sleeping status, prevalence of sleeping disorders, sleeping pill usage, and attitudes) are presented as frequencies (N) and percentages (%). A chi-squared test and a Fisher’s exact test were performed to determine the association of demographic characteristics with medical students’ attitudes. A p-value of <0.05 was considered statistically significant.
2.4 Ethical consideration
The King Abdullah International Medical Research Center provided ethical approval for this study (IRB number: SP21J/025/02). All participants provided their informed consent, after we assured them of their anonymity and data confidentiality. The data were gathered anonymously and recorded in an Excel document on Google Forms. No information that may be used to identify a participant was sought.
3 Results
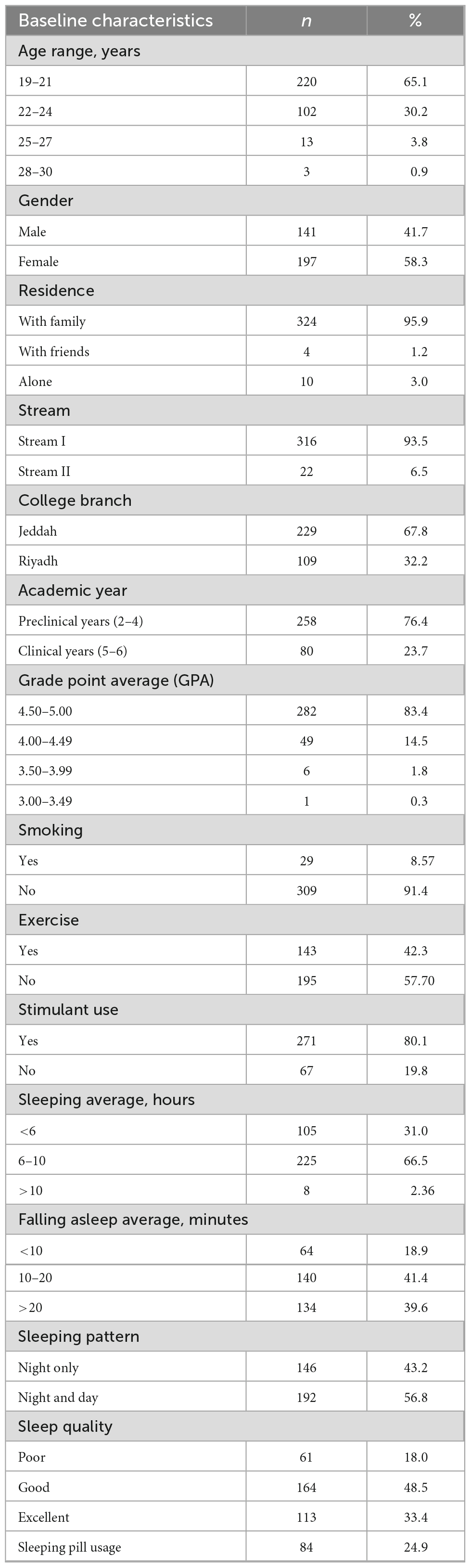
A total of 338 medical students responded to the online questionnaire. As illustrated in the summary of demographic characteristics (Table 1). Most respondents (n = 220, 65.1%) were aged 19–21 years, less than a third (n = 102, 30.2%) were 22–24 years, and only a few (n = 16, 4.7%) were older than 24 years. The sample included 141 (41.7%) male students and 197 (58.3%) female students. Almost all participants reported residing with their families (n = 324, 95.9%), while only a few reported living alone (n = 10, 3.0%) or with friends (n = 4, 1.2%). A higher proportion of respondents were stream I students (n = 316, 93.5%), and the remainder (n = 22, 6.5%) were stream II. Most of the students were from the Jeddah branch (n = 229, 67.8%), and the rest (n = 109, 32.2%) were from Riyadh. Further, 258 students (76.3%) were in pre-clinical years, and 80 (23.7%) in clinical years. Most of the respondents reported having a GPA of 4.5–5 (n = 282, 83.4%) and using stimulants (n = 271, 80.2%). Moreover, most respondents were non-smokers (n = 309, 91.4%). More than half of the respondents exercised regularly and had a night and day sleeping pattern. Less than one-third (n = 61, 18%) of the respondents reported poor sleep quality. Similarly, 18.9% of respondents (n = 64) reported requiring less than 10 min to fall asleep.
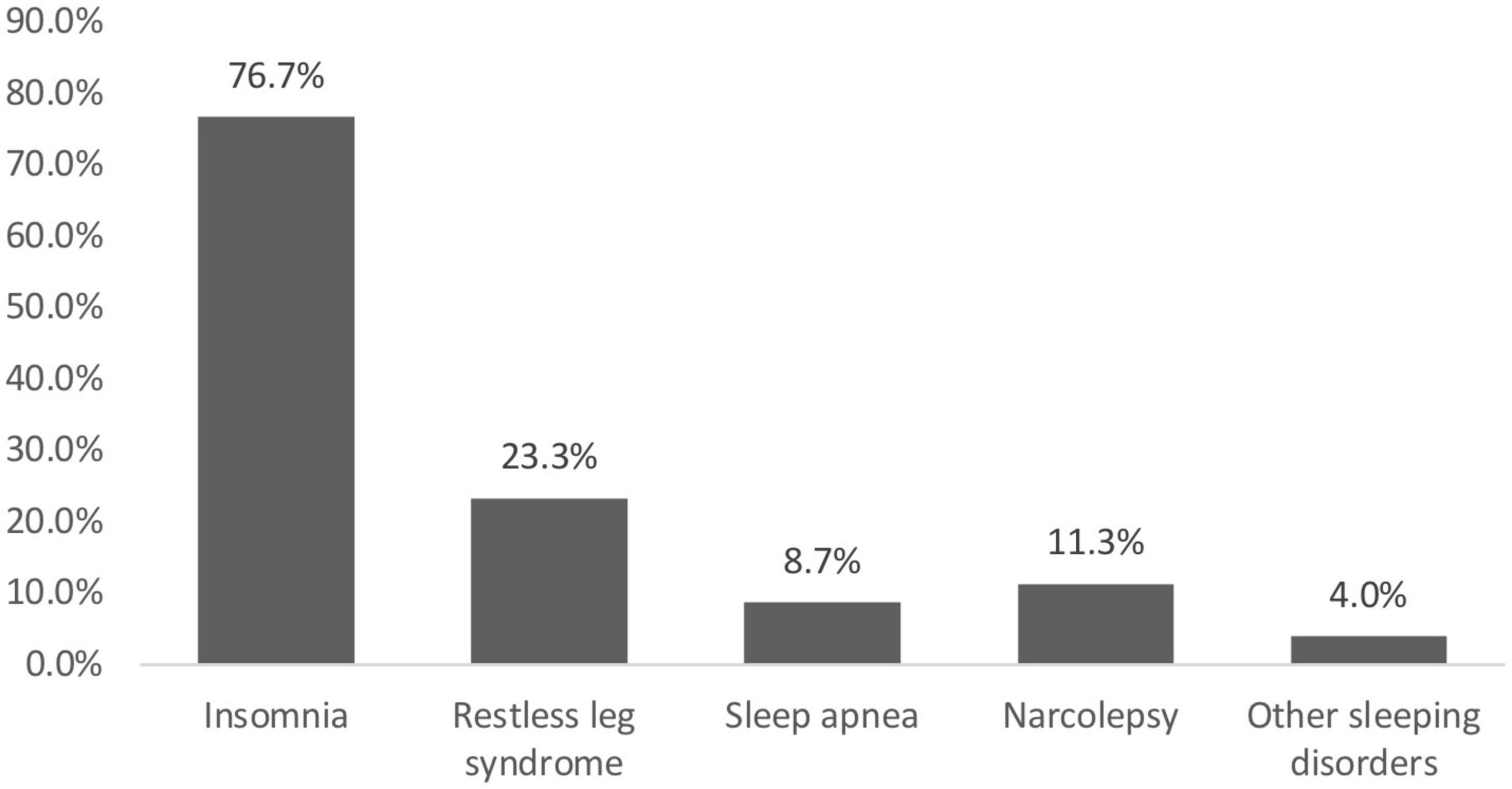
Survey findings reveal that 150 (44.4%) students had sleeping disorders. As illustrated in Figure 1, 115 (76.7%) of them suffered from insomnia, 35 (23.3%) had restless leg syndrome, 17 (11.3%) had narcolepsy, 13 (8.7%) experienced sleep apnea, and 6 (4%) had other sleeping disorders, which including waking up frequently, excessive daytime sleepiness, allergic rhinosinusitis and postnasal drip, nightmares, and one student reported waking up tired no matter how long he slept.
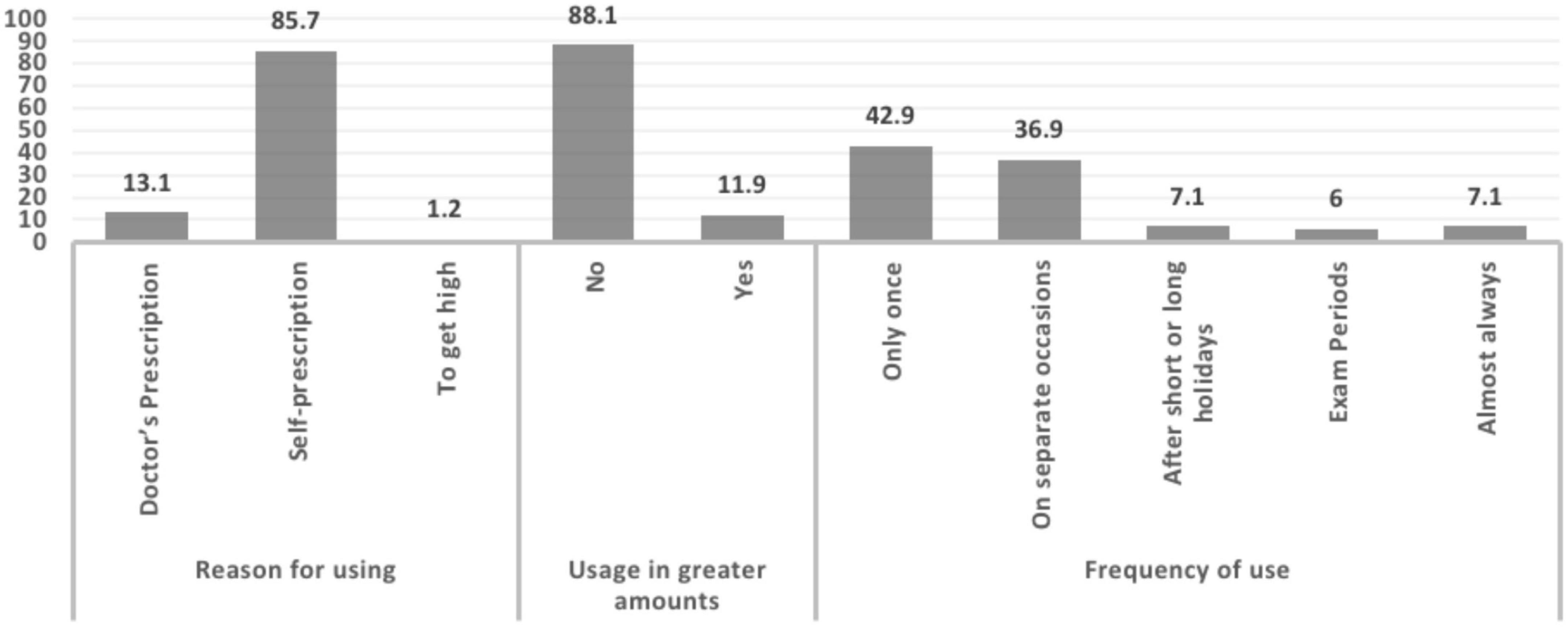
Attitudes toward the use of sleeping pills were assessed for students who reported using sleeping pills (n = 84, 24.9%). Of the 84 respondents, only 11 (13.1%) reported using sleeping pills with a doctor’s prescription. Conversely, more than two-thirds (n = 72, 85.7%) of students self-prescribed the medication, while only one (1.2%) respondent reported using sleeping pills for recreational purposes. In general, almost all respondents used sleeping pills in moderate amounts (n = 74, 88.1%), and only 10 (11.9%) reported usage in higher amounts. Frequency analysis of sleeping pill usage showed that only 6 (7.1%) respondents used sleeping pills almost always; similarly, 6 (7.1%) respondents used sleeping pills after short or long holidays. In addition, 36 (42.9%) respondents had used sleeping pills only once, and 31 (36.9%) used them on separate occasions (Figure 2).
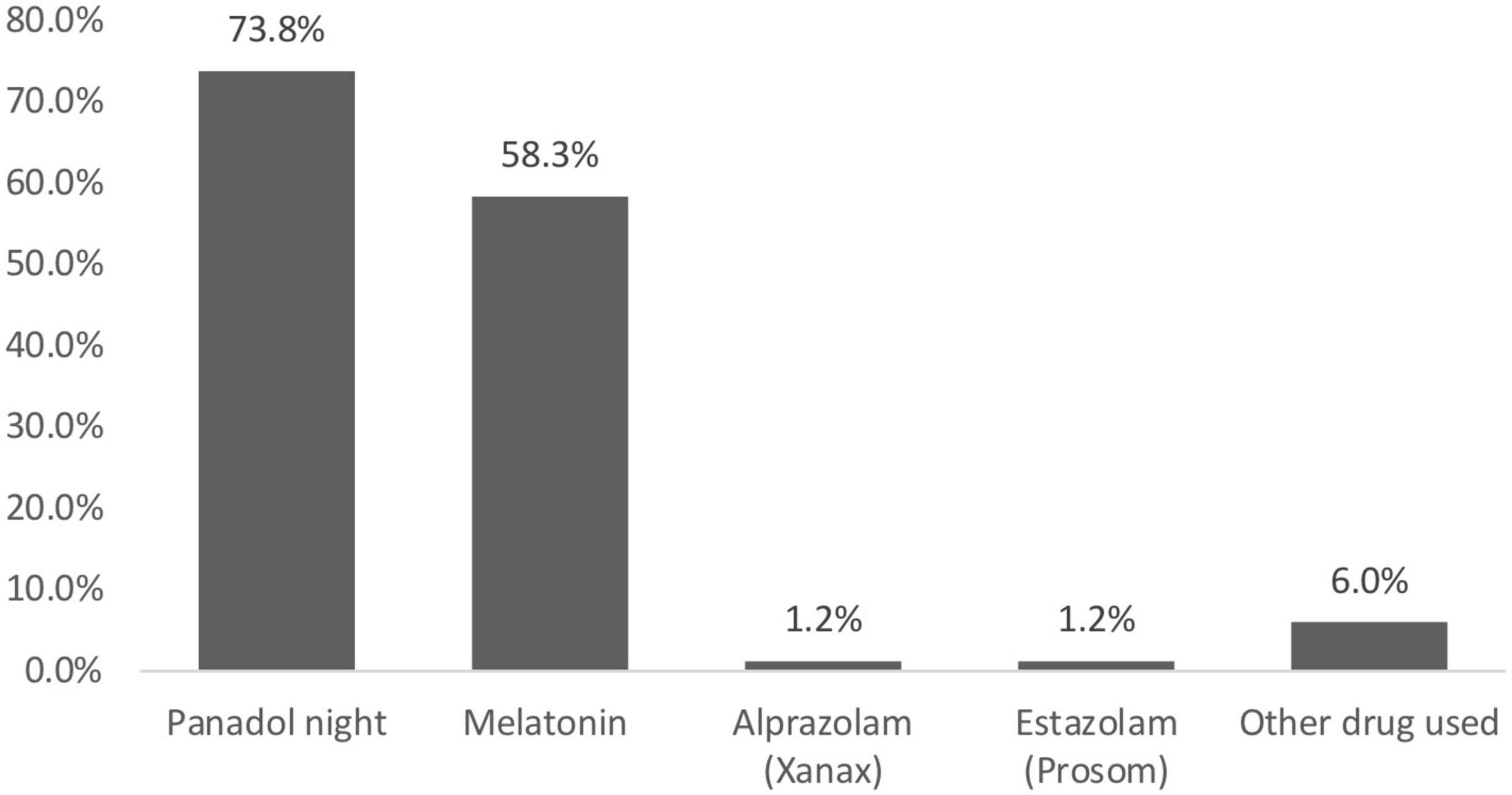
The most commonly used sleeping pill was Panadol Night (n = 62, 73.8%), followed by melatonin pills (n = 49, 58.3%). Alprazolam (Xanax) and estazolam (Prosom) had the same prevalence (1.2%). Some students reported using other sleeping pills (6%), namely, pseudoephedrine and lorazepam pills (Figure 3).
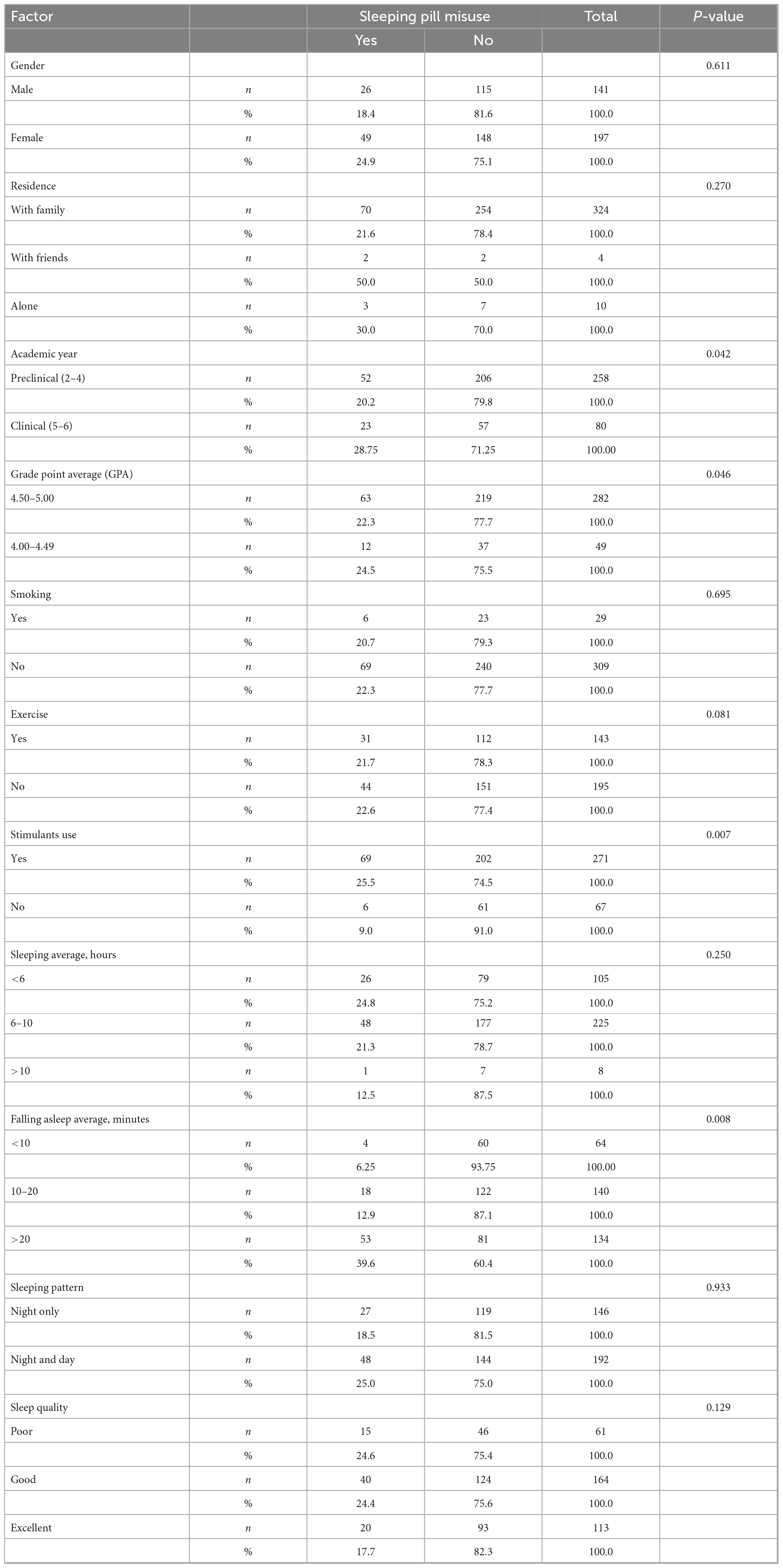
Of the 84 respondents who reported using sleeping pills, 75 (89.3%) students misused the pills. An analysis showed that academic year (p = 0.042), GPA (p = 0.046), stimulants use (p = 0.007), and longer average time required to fall asleep (p = 0.008) were significantly associated with sleeping pill misuse. Out of 197 female participated in this study (24.9%) n = 49 reported misusing of sleeping pills. Additionally, in 141 male only (18.4%) n = 21 misused sleeping pills. In 324 students who live with their family (21.6%) n = 70 misused sleeping pills, while (50%) n = 2 out of 4 students living with friends reported misusing sleeping pills. In addition, (30%) n = 3 out of 10 who live alone, reported misusing sleeping pills. Moreover, 52 (20.2%) students of preclinical years misused sleeping pills compared to 23 (28.75%) students of clinical years. Among students who had a high GPA, 63 (22.3%) students misused sleeping pills while respondents with a lower GPA who misused sleeping pills were 12 (24.5%) students. Among 29 students who are smokers (20.7%) n = 6 reported misusing sleeping pills; however, (22.3%) n = 69 of who aren’t smokers reported misusing sleeping pills. (21.7%) n = 31 of 143 who exercise, reported misusing sleeping pills, while (22,6%) n = 44 of who doesn’t exercise reported misusing sleeping pills. Out of 271 students who reported stimulants use, (25.5%) n = 69 reported misusing sleeping pills. However, (9.0%) n = 6 of students who doesn’t use stimulants, reported misusing sleeping pills. Among students who reported less than 6 h of sleep, 26 (24.8%) students were found to misuse sleeping pills; in contrast, 1 (12.5%) student who reported more than 10 h of sleep misused sleeping pills. While 53 (39.6%) respondents who needed more than 20 min, on average, to fall asleep reported misuse of sleeping pills, 4 (6.25%) respondents who needed less than 10 min to fall asleep misused sleeping pills. Moreover, 48 (25.0%) respondents who reported sleeping at night and day misused sleeping pills while 27 (18.5%) respondents who sleep at night only reported sleeping pills misuse. There were 61 students with a poor sleep quality, only (24.6%) n = 15 reported misusing sleeping pills; Moreover, out of 164 students with good sleeping quality, (24.4%) n = 40 reported misusing sleeping pills. In 113 students with excellent sleeping quality, (17.7%) n = 20 reported sleeping pill misuse (Table 2).
4 Discussion
This study assessed medical students’ attitudes toward sleeping pill usage. The study also estimated the prevalence of sleeping pill misuse and the factors associated with it among Saudi medical students.
The misuse of sleeping pills can have negative consequences, affecting one’s mental and physical wellbeing. While limited international studies have reported similar findings, this discussion involves multiple national studies that have revealed findings consistent with those in our study. However, it should be noted that this cross-sectional study was conducted in 2021–2022; therefore, the COVID-19 pandemic may have potentially affected the findings.
Medical students’ attitudes toward the usage of sleeping pills were assessed after considering the following as indicators of misuse: use of sleeping pills almost daily, use in greater amounts than the recommended dose, self-prescription, and use for recreational purposes. Most students self-prescribed sleeping pills, which was considered a misuse attitude. Similar studies have shown self-prescription to be a common issue among medical students; self-prescription is exacerbated by easy accessibility and the availability of several types of over-the-counter drugs, such as Panadol Night and melatonin (24, 25). Although self-prescribed medications can have some benefits when used appropriately, it is a dangerous practice that can delay an accurate medical diagnosis and result in adverse effects, drug interactions, and developing dependence, thereby aggravating what was intended to be treated (26).
The analysis of respondents’ demographic variables revealed that several factors were significantly associated with sleeping pill misuse. Students who were in their preclinical years of college were found to misuse sleeping pills more frequently than those in their clinical years (p = 0.042). According to a study conducted in Brazil on sleep quality among medical students, students in the early years of medical school had poorer sleep quality, compared with those in later years (27). This can explain why the misuse of sleeping pills by students in their preclinical years was higher than that of those in their clinical years. Another variable that was significantly associated with sleeping pill misuse is GPA (p = 0.046). Students who had a higher GPA (4.50–5.00) were found to misuse sleeping pills more frequently than students with a lower GPA (4.00–4.49). However, a different study showed that students with lower GPA misused sedatives more frequently than those with a higher GPA. This inconsistency in findings may be due to the difference in medication class, tools, and population (12).
Almost all students who used sleeping pills were also found to be using stimulants (p = 0.007). Stimulant use can negatively impact the sleep-wake cycle, resulting in sleeping pill usage and misuse. It is well known that exercise enhances sleep quality (28). Interestingly, exercise was not associated with a decrease in sleeping pill misuse. This is consistent with the findings of a study conducted in India, which found no significant association between exercise and using sleeping pills (7).
An important variable to be mentioned is gender, although it was not statistically significant (p = 0.611). Women were found to be misusing sleeping pills more often than men, specifically by taking them in larger dosages. A similar study showed that women tend to misuse sleeping pills by self- prescription more than men (29). The exact reason for this finding is yet to be investigated; however, multiple studies point toward the effects of hormones on the circadian rhythm during the luteal phase of the menstrual cycle, when sleep disturbances are common, especially among those with premenstrual dysphoric disorder (30). Nonetheless, another study suggested that women have better sleep quality than men, which should make them misuse sleeping pills less frequently than men (31). More studies are needed to investigate the gender differences in sleep quality and sleeping pill misuse.
Sleeping pills that are available over the counter (e.g., Panadol Night and melatonin) were found to be more commonly used than sleeping pills that require a doctor’s prescription (e.g., Xanax). Similar findings were reported in a study conducted in Saudi Arabia among physicians during the pandemic, wherein melatonin usage was found to be 75.7% (24). It is important to mention that prescription of certain types of sleeping pills (e.g., zolpidem and zaleplon) is associated with an increased risk of suicidal thoughts and suicide attempts (25); therefore, doctors should be careful when prescribing such medications and prescribe them only in specific cases, when needed.
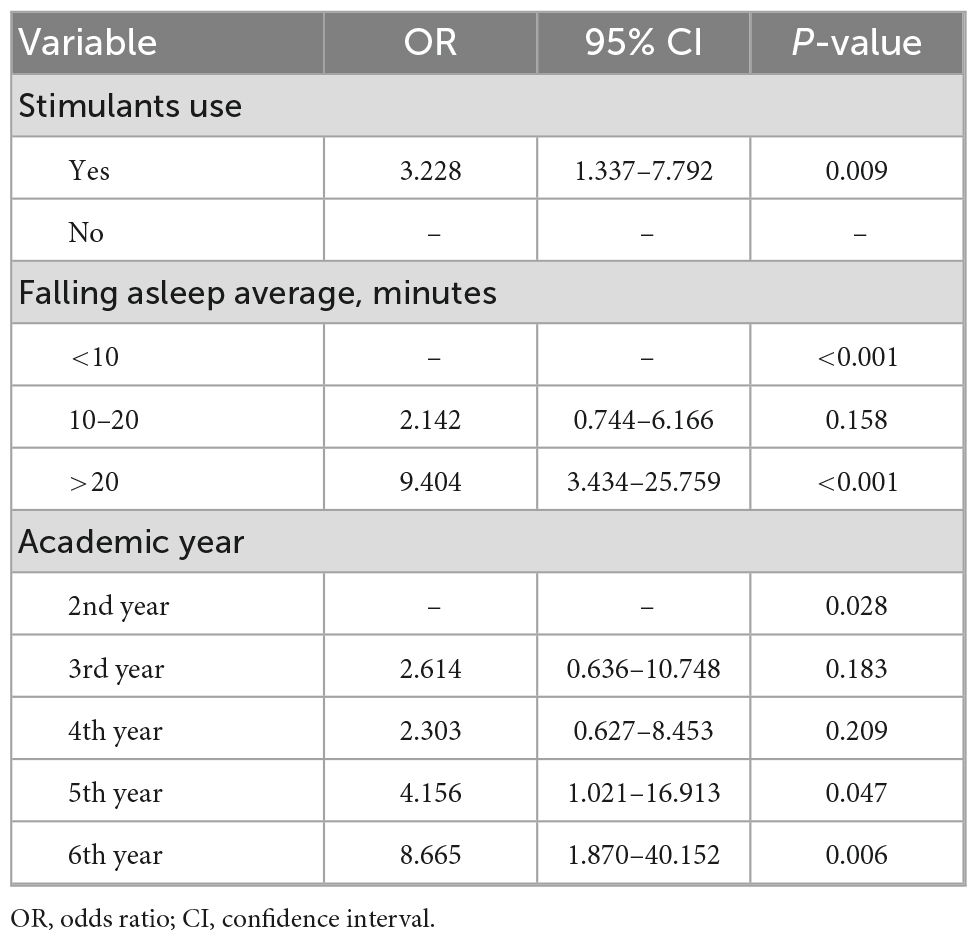
The study provided evidence of factors associated with the misuse of sleeping pills, such as needing of more than 20 min to fall asleep, being in fourth grade, and using stimulants. In this study, students requiring more than 20 min to sleep showed a strong association with misusing sleeping pills (OR: 9.404; 95% CI, 3.434–25.759; p < 0.001). This could be related to poor mental health affecting students’ sleep quality, which means that they end up in need of taking sleeping aids. We also found that sleeping pill use is more common among those who reported poor sleep quality (OR: 2.361; 95% CI, 1.49–3.72), as well as participants who slept for 4–6 h per day (OR: 1.74; 95% CI, 1.12–2.70) (1). Sleeping disorders also increase the occurrence of sedative drug use by 14.9% (2). Fourth-year medical students were found to have a higher rate of misuse (OR: 2.303; 95% CI, 0.627–8.453, p = 0.209). Furthermore, a previous cross-sectional study (1) showed that third-year students were more likely to abuse sleeping pills than first- and second-year students (OR: 0.49; 95% CI, 0.30–0.79). This may be because, in preclinical years, students are committed to studying more, due to the stressful curriculum, which has a negative impact on their mental health and can cause sleep disorders (3). According to a study conducted in Ethiopia, stimulant users are more likely to use sedative drugs than non-stimulant users (2). Our research showed that there is a significant association between the misuse of sleeping pills and stimulant use (OR: 3.228; 95% CI, 1.337–7.792, p = 0.009). This may be due to the adverse effects of stimulant use on the sleep-wake cycle, which then leads to the misuse and abuse of sleeping pills. As stated by Al-Sayed et al. (1), there is no association between the use of sedatives and stimulants (Table 3).
This study has several limitations. First, it was limited by its cross-sectional survey design. Second, the convenience sampling technique may limit the generalizability of the results. Third, the lack of questionnaire validation also comprised a limitation. Finally, because this study was conducted in only one university and the questionnaire had a low response rate, the representativeness of the sample is negatively affected and the generalizability of the results is limited. Additionally, the accuracy of respondents’ answers could not be assessed owing to the social stigma attached to misuse, even though confidentiality was ensured. In addition, there is a possibility of cognitive denial or distortion in students’ reporting of their sleeping pill misuse. Future research could further investigate the specific patterns of sleeping pill misuse.
Data availability statement
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The King Abdullah International Medical Research Center provided ethical approval for this study (IRB number: SP21J/025/02). All participants provided their informed consent, after we assured them of their anonymity and data confidentiality. The data were gathered anonymously and recorded in an Excel document on Google Forms. No information that may be used to identify a participant was sought. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
MMA and RSA: conceptualization. AA, RSA, RIA, SA, and TB: data collection and analysis and writing—original draft preparation. MMA, MYA, and HA: visualization, supervision, and writing—review and editing. All authors read and approved the final version of the manuscript for publication.
Funding
This study was funded by King Abdullah International Medical Research Center, Jeddah, Saudi Arabia.
Acknowledgments
The authors are thankful to Alaa Althubaiti, Maryam Alotaibi, and Someiah Alyahya for their valuable contributions in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewers EM and MA declared a shared affiliation with the authors MMA, RSA, AA, SA, RIA, and TB to the handling editor at the time of review.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Almojali A, Almalki S, Alothman A, Masuadi E, Alaqeel M. The prevalence and association of stress with sleep quality among medical students. J Epidemiol Glob Health. (2017) 7:169–74. doi: 10.1016/j.jegh.2017.04.005
2. Sreedharan J, Ahmed S, Gomathi K. Psychological health of first-year health professional students in a medical university in the United Arab Emirates. Sultan Qaboos Univ Med J. (2012) 2:206–13. doi: 10.12816/0003114
3. Polychronopoulou A, Divaris K. Perceived sources of stress among Greek dental students. J Dent Educ. (2005) 69:687–92. doi: 10.1002/j.0022-0337.2005.69.6.tb03952.x
4. Frick L, Frick J, Coffman R, Dey S. Student stress in a three-year doctor of pharmacy program using a mastery learning educational model. Am J Pharm Educ. (2011) 75:64. doi: 10.5688/ajpe75464
5. Dyrbye L, Thomas M, Shanafelt T. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad Med. (2006) 81:354–73. doi: 10.1097/00001888-200604000-00009
6. Samreen S, Siddiqui N, Mothana R. Prevalence of anxiety and associated factors among pharmacy students in Saudi Arabia: a cross-sectional study. BioMed Res Int. (2020) 2020:2436538. doi: 10.1155/2020/2436538
7. Dalui S, Datta A, Ghosh A, Biswas S, Roy U, Biswas S. Self-medication of sleeping pills among MBBS students in a medical college of West Bengal, India. Int J Basic Clin Pharmacol. (2021) 6:1689. doi: 10.18203/2319-2003.ijbcp20172732
8. Abdel Rahman A, Al Hashim B, Al Hiji N, Al-Abbad Z. Stress among medical Saudi students at college of medicine, king faisal university. J Prev Med Hyg. (2013) 54:195–9.
9. Davies S, Ang J, Revell V, Holmes B, Mann A, Robertson F, et al. Effect of sleep deprivation on the human metabolome. Proc Natl Acad Sci USA. (2014) 111:10761–6. doi: 10.1073/pnas.1402663111
10. Curcio G, Ferrara M, De Gennaro L. Sleep loss, learning capacity and academic performance. Sleep Med Rev. (2006) 10:323–37. doi: 10.1016/j.smrv.2005.11.001
11. Hamaideh S. Stressors and reactions to stressors among university students. Int J Soc Psychiatry. (2011) 57:69–80. doi: 10.1177/0020764009348442
12. Al-Sayed A, Al-Rashoudi A, Al-Eisa A, Addar A, Al-Hargan A, Al-Jerian A, et al. Sedative drug use among king saud university medical students: a cross-sectional sampling study. Depress Res Treat. (2014) 2014:378738. doi: 10.1155/2014/378738
13. Waqas A, Khan S, Sharif W, Khalid U, Ali A. Association of academic stress with sleeping difficulties in medical students of a Pakistani medical school: a cross sectional survey. PeerJ. (2015) 3:e840. doi: 10.7717/peerj.840
14. Bennett T, Holloway K. Motives for illicit prescription drug use among university students: a systematic review and meta-analysis. Int J Drug Policy. (2017) 44:12–22. doi: 10.1016/j.drugpo.2017.02.012
15. World Health Organization [WHO]. Guidelines for the regulatory assessment of medicinal products for use in self-medication. (2000). Available online at: https://apps.who.int/iris/handle/10665/66154. (accessed Jul 29, 2022).
16. Alshahrani S, Alavudeen S, Alakhali K, Al-Worafi Y, Bahamdan A, Vigneshwaran E. Self-medication among king khalid university students, Saudi Arabia. Risk Manag Healthc Policy. (2019) 12:2439. doi: 10.2147/RMHP.S230257
17. Dube K, Kumar A, Kumar N, Gupta S. Drug use among college students—an interim report. Bull Narc. (1977) 29:47–61.
18. National Institute on Drug Abuse. Prescription CNS depressants DrugFacts. (2020). Available online at: https://nida.nih.gov/publications/drugfacts/prescription-cns-depressants (accessed Nov 13, 2020).
19. Substance Abuse and Mental Health. Services administration. behavioral health trends in the United States: results from the 2014 national survey on drug use and health. (2015). Available online at: https://www.samhsa.gov/data/report/behavioral-health-trends-united-states-results-2014-national-survey-drug-use-and-health (accessed Jul 24, 2022).
20. Cleveland Clinic. Sleeping pills: types, side effects, & treatment. (2021). Available online at: https://my.clevelandclinic.org/health/drugs/15308-sleeping-pills (accessed Jan 30, 2021).
21. Akvardar Y, Demiral Y, Ergor G, Ergor A. Substance use among medical students and physicians in a medical school in Turkey. Soc Psychiatry Psychiatr Epidemiol. (2004) 39:502–6. doi: 10.1007/s00127-004-0765-1
22. Mancevska S, Bozinovska L, Tecce J, Pluncevik-Gligoroska J, Sivevska-Smilevska E. Depression, anxiety and substance use in medical students in the Republic of Macedonia. Bratisl Lek Listy. (2008) 109:568–72.
23. Rasosoft. Rasosoft Home. (2021). Available online at: http://www.raosoft.com/ (accessed Jan 30, 2021).
24. Aljaouni M, Hafiz A, Alalaw H, Alahmdi G, Alkhawaja I. Self-medication practice among medical and non-medical students at taibah university, Madinah, Saudi Arabia. Int J Acad Sci Res. (2015) 3:54–65.
25. Albasheer O, Mahfouz M, Masmali B, Ageeli R, Majrashi A, Hakami A, et al. Self-medication practice among undergraduate medical students of a Saudi tertiary institution. Trop J Pharm Res. (2016) 15:2253. doi: 10.4314/tjpr.v15i10.26
26. Tripković K, Šantrić Milićević M, Odalović M. Gender differences in predictors of self-medication with tranquillizers and sleeping pills: results of the population-based study in Serbia. Zdr Varst. (2020) 59:47–56. doi: 10.2478/sjph-2020-0007
27. Corrêa C, Oliveira F, Pizzamiglio D, Ortolan E, Weber S. Sleep quality in medical students: a comparison across the various phases of the medical course. J Bras Pneumol. (2017) 43:285–9. doi: 10.1590/S1806-37562016000000178
28. Yang P, Ho K, Chen H, Chien M. Exercise training improves sleep quality in middle-aged and older adults with sleep problems: a systematic review. J Physiother. (2012) 58:155–63. doi: 10.1016/S1836-9553(12)70106-6
29. AlAteeq D, Almokitib A, Mohideen M, AlBlowi N, Fayed A, Alshahrani S. Stress, sleep, and use of sleep aids among physicians during the COVID-19 pandemic. J Nat Sci Med. (2021) 4:197. doi: 10.24875/AIDSRev.M20000034
30. Shechter A, Boivin D. Sleep, hormones, and circadian rhythms throughout the menstrual cycle in healthy women and women with premenstrual dysphoric disorder. Int J Endocrinol. (2010) 2010:259345. doi: 10.1155/2010/259345
Keywords: sleeping pills, medical students, misuse, self-prescription, attitude, prevalence
Citation: Alasmari MM, Alkanani RS, Alshareef AS, Alsulmi SS, Althegfi RI, Bokhari TA, Alsheikh MY and Alshaeri HK (2022) Medical students’ attitudes toward sleeping pill usage: A cross-sectional study. Front. Psychiatry 13:1007141. doi: 10.3389/fpsyt.2022.1007141
Received: 30 July 2022; Accepted: 01 December 2022;
Published: 20 December 2022.
Edited by:
Aslam Khan, Riphah International University, Lahore, PakistanReviewed by:
Nasra Ayuob, Damietta University, EgyptEmad Masuadi, King Saud bin Abdulaziz University for Health Sciences, Saudi Arabia
Mohamed Eldigire Ahmed, King Saud bin Abdulaziz University for Health Sciences, Saudi Arabia
Copyright © 2022 Alasmari, Alkanani, Alshareef, Alsulmi, Althegfi, Bokhari, Alsheikh and Alshaeri. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Moudi M. Alasmari, ✉ YXNtYXJpbUBrc2F1LWhzLmVkdS5zYQ==
 Moudi M. Alasmari
Moudi M. Alasmari Raghad S. Alkanani
Raghad S. Alkanani Asmaa S. Alshareef
Asmaa S. Alshareef Shahd S. Alsulmi
Shahd S. Alsulmi Reuof I. Althegfi1
Reuof I. Althegfi1 Mona Y. Alsheikh
Mona Y. Alsheikh