- 1School of Nursing, Hawassa University College of Medicine and Health Sciences, Hawassa, Ethiopia
- 2Department of Midwifery, Hawassa University College of Medicine and Health Sciences, Hawassa, Ethiopia
Background: COVID-19 causes immense psychological pressure on communities in addition to physical misery. There is currently a scarcity of data on the psychological impact of the COVID-19 epidemic on Ethiopian healthcare workers (HCWs). Therefore, this study was aimed to assess the post-traumatic stress disorder (PTSD) symptoms and its predictors following COVID-19 pandemic among healthcare workers (HCWs) in southern Ethiopia.
Methods: A hospital based cross-sectional study design was used among 387 randomly selected HCWs between September 25 and October 25, 2020 at four selected public hospitals in Sidama National Regional State, southern Ethiopia. Impact of Event Scale-Revised (IES-R) was used to collect data post-traumatic stress disorder (PTSD) symptoms. Logistic regression analyses with 95% CI were used to examine the relationship between independent and outcome variables.
Result: The prevalence of PTSD symptoms was found in 56.8% of participants. Significant factors that increase risk of PTSD symptoms were being female (AOR = 1.91, 95% CI = 1.19, 3.05), married (AOR = 1.87, 95% CI = 1.12, 3.14) and nurses (AOR = 3.31, 95% CI = 1.66, 6.63). On the other hand, HCWs working other than emergency unit such as inpatients/wards (AOR = 0.43, 95% CI = 0.24, 0.75), OPD (AOR = 0.48, 95% CI = 0.24, 0.97) and other units (AOR = 0.49, 95% CI = 0.25, 0.96) less likely to be affected by PTSD symptoms.
Conclusion: The current study showed high levels of PTSD symptoms as psychological challenges for HCWs. Sex, age, marital status, type of profession and working environment were significant factors for PTSD symptoms in HCWs during the pandemic. HCWs require mental health support during and after the pandemic.
Introduction
The coronavirus disease (COVID-19) pandemic, which began in China, continues to pose a global health hazard (1). The COVID-19 outbreak was declared as a public health emergency of worldwide concern by the World Health Organization (WHO) on January 30, 2020 (2). Globally, there have been about 260 million confirmed cases and almost 5.2 million COVID-19 related deaths reported by the end of November, 2021 (3). In Ethiopia, there were about 371,000 confirmed COVID-19 cases and more than 6,700 deaths in the country by the end of November, 2021, with a 1.82% case fatality rate (4).
COVID-19's rapid spread around the world has placed significant strain on healthcare workers (HCWs) who are directly and indirectly combating the pandemic, potentially increasing the risk of negative mental health outcomes (5). COVID-19 causes significant psychological stress and other health-related issues in HCWs, as they are responsible for infected patients, have frequent interactions with patients' families/relatives, and are occasionally scrutinized by the public (6). HCWs also fear that they can develop COVID-19 themselves, because of the increased risk of exposure to the virus. They are concerned that the infection is brought home and passed on to families and friends (7). In addition, wearing protective equipment for extended periods of time causes breathing difficulties and limited access to toilets and water, resulting in physical and mental exhaustion (7). There are frequent reports of excessive job load, isolation and prejudice and so they are extremely prone to physical weariness, fear, emotional disturbance and sleep problems (8).
Previous studies indicated that health-related pandemic disasters have been linked to posttraumatic stress disorder (PTSD) symptoms (9–11). The COVID-19 pandemic has the potential to be a traumatic situation. According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), the presence of symptoms from the following four symptom clusters is required for the diagnosis of PTSD: Intrusion symptoms associated with traumatic event(s); persistent avoidance of stimuli associated with traumatic event(s); negative changes in cognition and mood associated with traumatic event(s); and significant changes in arousal and reactivity associated with traumatic event(s) beginning or becoming more severe following the occurrence of traumatic event(s) (12).
The psychological pressure on HCWs dealing with COVID-19 is great (13) such as post-traumatic stress symptoms. According to a study done in China during the initial outbreak of COVID-19, 53.8% of respondents rated moderate to severe level of psychological distress (14). A study conducted in health care workers in Singapore reported that 7.7% for clinical concern of PTSD (15). The prevalence of symptoms of PTSD in Oslo, Norway were 28.9% among HCWs (16). About one-fourth (27.7%) had clinically important symptoms of post-traumatic stress among workers in Mexico in another study (17). A similar study in Chinese nurses showed that 16.8% had symptoms of PTSD (18). According to recent studies in Ethiopian HCWs, the prevalence of psychological distress or PTSD symptoms ranges from 51.6 to 78.3% (19–23).
HCWs who work in emergency rooms, intensive care units (ICU), and isolation wards are more likely to acquire psychological problems (24). According to a study conducted in Singapore, doctors and those who are single have a higher risk of developing psychiatric symptoms than nurses and those who are married, respectively (25). Moreover, lack of social support and communication, as well as maladaptive coping and a lack of training, are all major risk factors for developing psychological morbidities (24).
In a high-pressure, high-risk anti-pandemic situation, HCWs frequently experience a variety of psychological issues (26). As a result, psychological assessment and intervention in victims and rescuers, such as medical personnel and volunteers, are critical for pandemic control. This concept is beneficial not only for early actions and psychological intervention, but also for significantly improving pandemic control and accelerating social recovery (27). Therefore, the mental health of HCWs should be safeguarded, since this can impact the success of the healthcare delivery and the control of COVID-19 pandemic.
It is critical to have a reliable estimate of the prevalence of mental health problems among HCWs during the COVID-19 pandemic in order to prevent, identify, and treat it. Despite the fact that numerous studies on the psychological impact of HCWs during the pandemic have been conducted in various countries, there is still paucity of evidences in Ethiopia (19–23), particularly in the southern area. Thus, the aim of this study is to assess the PTSD symptoms and its predictors among healthcare workers (HCWs) during COVID-19 pandemic in southern Ethiopia.
Our findings could be useful in developing interventions to help HCWs cope with the COVID-19 pandemic and future outbreaks. Also, this could help government organizations and healthcare professionals protect the community's mental health as the COVID-19 pandemic spreads across Ethiopia.
Materials and Methods
Study Area
This study was conducted at selected public hospitals (Hawassa University Comprehensive Specialized Hospital (HUCSH), Adare General Hospital, Leku Primary Hospital and Yirgalem General Hospital) in Sidama National Regional State.
Study Design and Period
Institution based cross sectional study design was conducted among HCWs between September 25 and October 25, 2020.
Study Subject
This study was conducted among front line HCWs working in medical and surgical inpatient units, intensive care units, emergency departments, and outpatient units. In addition, non-frontline health professionals who are working at regular chronic care clinic, laboratory, pharmacy, delivery etc. units were included.
Sample Size and Sampling Procedure
The required sample size was determined using single population proportion formula n = (Zα/2)2* p(1-p)/d2, where n is the sample size, z is the standard normal score set at 1.96, d is the desired degree of accuracy and p is the estimated proportion of the target population. Due to the lack of previous research to inform our expected sample proportion (p), we use a value that gives our sample size maximum i.e., p = 0.5. Then by taking P = 50%. Zα/2 = 1.96 and w = 5%, the computed sample size was 384 and by taking 10% non-response rate, the total sample size computed was 422.
The overall sample size was proportionally allocated to each health institution. Then simple random sampling method was used to select the study participants by taking the lists from the human resource office of each respective health institution.
Data Collection Methods
The English version of the Impact of Event Scale-Revised (IES-R) was used to collect data. The IES-R is a self-administered questionnaire that has been used to assess the psychological impact (PTSD symptoms) of a public health crisis within 1 week of exposure (28). This is a 22-item Likert scale questionnaire ranging from 0 (not at all) to 4 (extremely), with a total score between 0 and 88. It is composed of three subscales and aims to measure avoidance, intrusion, and hyperarousal symptoms (29). It had high levels of internal consistency (Intrusion: Cronbach's alpha = 0.87–0.94, Avoidance: Cronbach's alpha = 0.84–0.87, Hyperarousal: Cronbach's alpha = 0.79–0.91) and test-retest reliability was ranged from 0.89 to 0.94 (9, 30, 31). The total IES-R score was divided into normal (0–23), mild (9, 24–31), moderate (14, 31–33), and severe (>37) psychological impact (PTSD symptoms). A score of 24 or more considered as a cut-off score for the presence of PTSD symptoms or psychological trauma (31). The internal consistency or Cronbach's alpha of IES-R in this study was 0.94.
Four nurses were involved in data collection after receiving a 2-day intensive training on data collection techniques. A pre-test was performed in 5% of the sample to identify potential problems with data collection instruments and to ensure the consistency of the questionnaires. During the data collection process, supervisors checked each questionnaire for completeness on a daily basis.
Data Processing and Analysis
Collected data were entered to Epi-data version 3.1 and exported to SPSS version 24 for windows for analysis. Descriptive statistics were used to identify distributions of socio-demographic characteristics of the study participants. The magnitude of psychological impact, were described as a percentage. Logistic regression analyses with 95% CI were used to see the association between each independent and outcome variable. Finally, those variables which showed statistical significance at P < 0.05 and 95% CI in the final model was reported as independently associated with psychological impact. The model fitness test was checked using the Hosmer and Lemeshow goodness of fit test.
Results
Socio-Demographic Characteristics
The study included 387 health professionals, with a 91.7% response rate. The remaining 35 questionnaires were incomplete and were not analyzed. The majority of study participants 227 (58.7%) were male, 233 (60.2%) were aged 26–35 years, nearly half 191 (49.4%) were married, about three-fourth 298 (77.0) had BSc degree, 230 (59.4%) had ≤ 5 years of experience, 224 (57.9%) were living with their family, half 197 (50.9%) were nurses by profession and about one-third 138 (35.7%) were working at emergency department. Socio-demographic characteristics were described in Table 1.
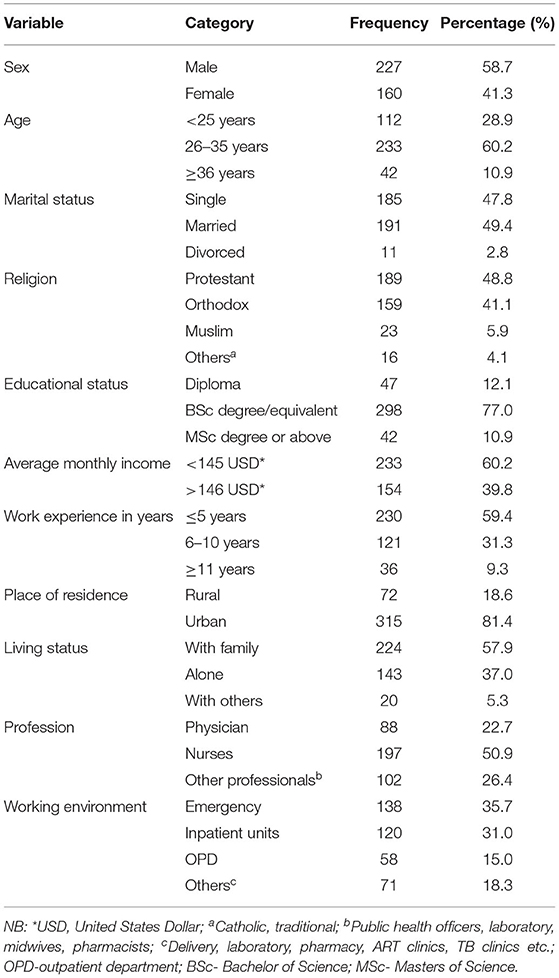
Table 1. Socio-demographic characteristics of the study participants during COVID-19 pandemic in selected hospitals of Sidama National Regional State, southern Ethiopia 2020 (n = 387).
Prevalence of PTSD Symptoms
The prevalence of PTSD symptoms was found to be 56.8% (Figure 1).
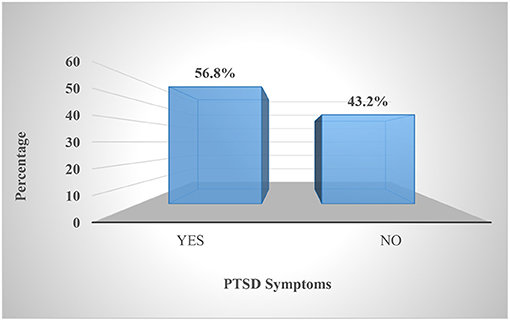
Figure 1. Prevalence of psychological impact (PTSD symptoms) of the study participants during COVID-19 pandemic in selected hospitals of Sidama National Regional State, southern Ethiopia, 2020 (n = 387).
Moreover, about one-third 142 (36.7%) of participants have severe, 28 (7.8%) have moderate and 50 (12.9%) mild level of PTSD symptoms as illustrated by Figure 2.
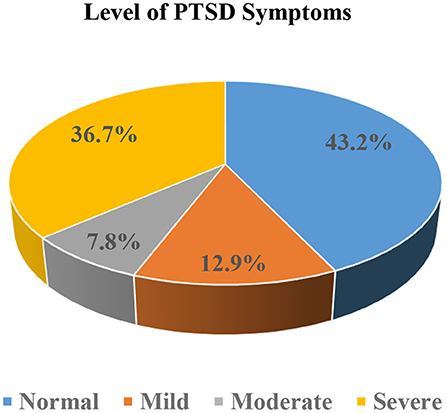
Figure 2. Severity level of PTSD symptoms of the study participants during COVID-19 pandemic in selected hospitals of Sidama National Regional State, southern Ethiopia, 2020 (n = 387).
Independent Predictors of PTSD Symptoms
Significant factors that increase risk of PTSD symptoms were being female (AOR = 1.91, 95% CI = 1.19, 3.05), married (AOR = 1.87, 95% CI = 1.12, 3.14) and nurses (AOR = 3.31, 95% CI = 1.66, 6.63). On the other hand, HCWs working other than emergency unit such as inpatients/wards (AOR = 0.43, 95% CI = 0.24, 0.75), OPD (AOR = 0.48, 95% CI = 0.24, 0.97) and other units (AOR = 0.49, 95% CI = 0.25, 0.96) less likely to be affected by PTSD symptoms (Table 2).
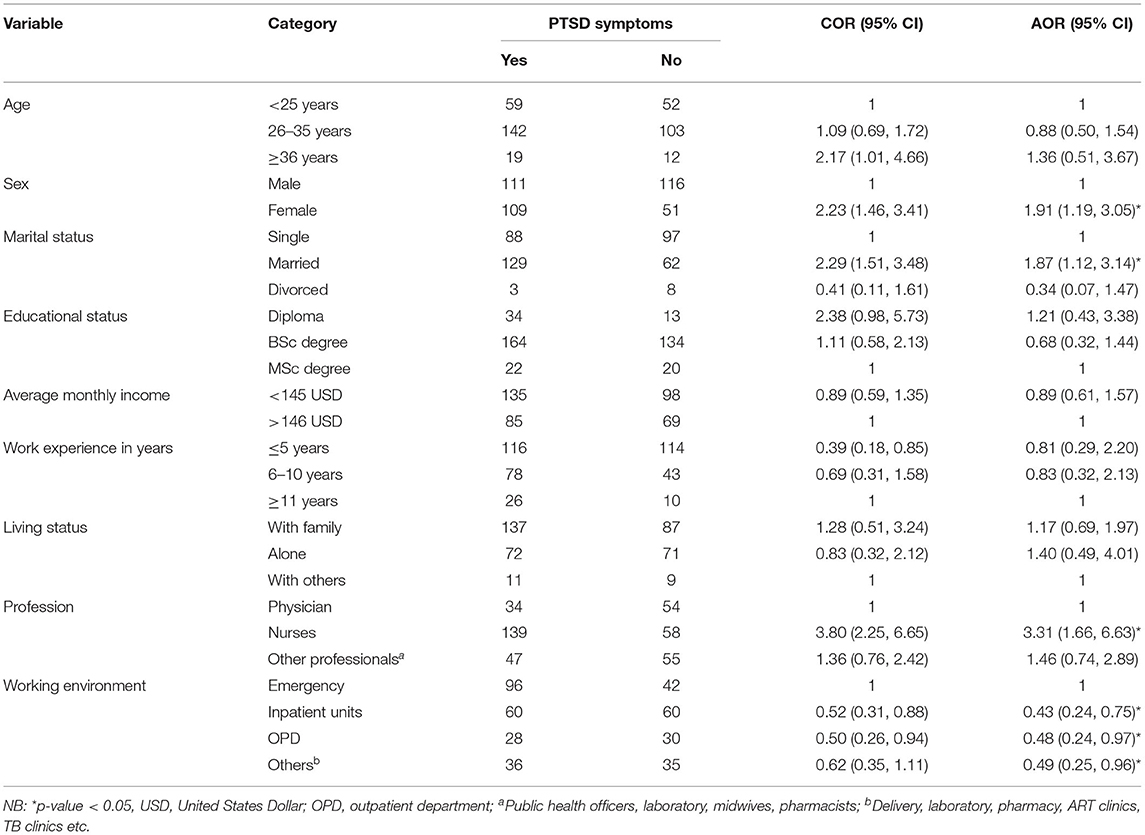
Table 2. Factors associated with PTSD symptoms of the study participants during COVID-19 pandemic in selected hospitals of Sidama National Regional State, southern Ethiopia, 2020 (n = 387).
Discussion
Millions of people have died as a result of the COVID-19 pandemic, which has had a dramatic impact on the global population, and health-care providers have had to work a much busier schedule and for longer hours than predicted during this pandemic time. This study evaluates the severity of psychological trauma, known as post-traumatic stress disorder (PTSD), among health care workers during the COVID-19 pandemic in southern Ethiopia. It is added to a few other studies that have investigated this issue in Ethiopia (19–23).
The prevalence of PTSD symptoms was found to be 56.8% and more than one-third (36.7%) of participants had severe levels of PTSD symptoms. This finding is similar with recent studies in different parts of Ethiopia such as North Shoa (58%) (21), Northwest Ethiopia (55.1%) (19), and Gedeo Zone (51.6%) (22). In addition, studies from China (53.8%) (14), Italy (55%) (32), Spain (56.6%) (33), UK (60.6%) (34), and New York, US (57%) (35) reported similar findings to our study. But, a higher prevalence of PTSD (78%) were reported in southwest Ethiopia (20). Similarly a recent research by Zhang et al. found out that nearly three-fourth (73.4%) (IES-R ≥ 9) of study participants reported psychological trauma (36), which is higher than our finding. However, the prevalence of PTSD symptoms in this study was higher than in a study conducted in Oslo, Norway (28.9%) (16), Mexico (27.7%) (17), Italy (36.7%) (37), and Chinese nurses (16.8%) (18). Moreover, a recent literature review has shown that 11–74.4% of HCPs develop symptoms of PTSD (38). And also, several other investigations have shown very different results. Even if the same scale is employed, the use of diverse testing procedures and methodology in research, as well as the use of different classifications, contribute to widely disparate estimations of the prevalence of PTSD symptoms (39). In general, HCWs appear to be suffering from extensive mental health concerns during the COVID-19 epidemic (40, 41). Both before and after the epidemic, HCWs have a high demand for psychological care. The significant prevalence of psychological trauma confirmed with this study and other previous studies (19–23) suggests that HCWs in Ethiopia will require psychiatric care in the future.
Females were shown to have more likely experience PTSD symptoms in this study. This is backed up by a slew of studies showing that women are more likely than men to suffer from “internalizing” mental illnesses (42, 43). Male sex was independently related with a decreased prevalence of peritraumatic dissociative symptoms, according to a study by Azoulay et al. (44). Women were more likely than men to suffer from post-traumatic symptoms as a result of the stressful work environment (32). Furthermore, recent studies on COVID-19's health outcomes among HCWs reveal a high prevalence of mental health issues, particularly among women (45–47). On the one hand, women may have felt the pressure of working in the COVID-19 emergency more than their male counterparts because of the culturally bound double roles of women in the family, child-caring, and professional jobs. Women, on the other hand, place a higher value on their own internal experiences and the emotional states of others than men. Furthermore, a growing body of gender-specific research reveals that men use health-care services and report symptoms at a lower rate than women (48, 49).
In our study, we found out that the married HCWs were highly likely to experience PTSD symptoms than their counterparts. Similarly, PTSD symptoms were observed to be considerably greater among married employees in prior research conducted with healthcare professionals following COVID-19 outbreaks (50). Furthermore, in different studies conducted following the various outbreaks, married HCWs were found to be more concerned about their own health condition as well as the health of their families, leading to the conclusion that married HCWs experience more symptoms of psychological trauma (51, 52).
In comparison to physicians, nurses are more likely to experience PTSD symptoms, according to this study. Prior studies indicate that nurses are said to be at a higher risk of psychological disturbance or post-traumatic symptoms than doctors (19, 53–55). This may be due to nurses' workloads and night shifts, as well as being in contact with more risky patients than doctors (54). Of course, nursing personnel have longer and deeper interaction with COVID-19 patients, which provides the 24-h care, which raises the risk of psychological trauma, compared to other professionals (32). Physicians can be assumed to have certain unique somatization resistance which can be ascribed to their personal performance (56), professional experience, and self-awareness (57).
HCWs who worked in units other than emergency units were less likely to develop PTSD symptoms than those who worked in emergency units, according to our research. An Italian investigation came to a similar conclusion (32). Even though a patient's death is something that should be considered in any medical setting, especially in emergency rooms, it has been demonstrated to be one of the most common sources of stress for HCWs (58, 59). The emergency unit's so-called red zone, where most front-line HCWs perform their everyday operations, is a heavily contaminated and dangerous environment. Furthermore, doctors, nurses, and technicians may have lost a patient because to the pandemic or another medical issue. HCWs who saw the death of one of their COVID-19-infected patients, on the other hand, reported higher levels of psychological trauma (32). It is fact that, the death of a patient may remain an unspoken emotion, especially if overburdened by guilt and a sense of professional failure, which can influence the efficacy of physicians and other HCWs working with patients, resulting in significant adverse psychological consequences.
Even though, this study provided a baseline data, and we use a standardized tool IES-R designed to assess psychological trauma (PTSD symptoms), there are certain limitations to this research. To begin, PTSD symptoms were assessed solely by self-administered questionnaires rather than a psychiatric interview. Second, because we were unable to meet with HCWs face to face, we were unable to acquire extensive information about psycho-traumatic symptoms history. Third, this is a cross-sectional research paper. Fourth, no information on the type of mental health support provided to HCWs could be found. Therefore, longitudinal studies are needed to determine the prevalence of PTSD symptoms and its causative factors after the COVID-19 pandemic in the future researches.
Conclusion
High levels of symptoms of PTSD symptoms emerged in the present study as psychological difficulties experienced by HCWs. Being female, married and nurses were significant factors associated with high risk of PTSD symptoms. Whereas, HCWs working other than emergency unit such as (inpatients, OPD and other units) were less likely to experience PTSD symptoms. Given the anticipated waves of COVID-19 and other healthcare crises, identifying risk factors for PTSD among HCWs and providing treatment for those who require it is crucial. Also, HCWs require psychiatric support at which monitoring and control can be performed during and after the pandemic. Furthermore, it is better if Ministry of Health and other concerned bodies provide mental health and psycho-social support (MHPSS) and arranging for in-service training to raise awareness for HCWs.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by Hawassa University, College of Medicine and Health Sciences, Institutional Review Board (IRB) with reference number IRB/295/12. The participants provided their written informed consent to participate in this study. The same permission letter was written by the university to each health institution. The purpose of the study was explained for the respondents and the right to withdraw from the study at any time was assured. Coding was used to eliminate names and other personal identification of respondents throughout the study process to ensure participants confidentiality. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
MA, BD, YA, YR, and FT participated in the conception and designed the study and involved in the data collection and analysis of the study. SD involved in the analysis of the study. MA prepares the manuscript for publication. BD, YA, YR, FT, and SD critically reviewed the manuscript. All authors read and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to thank Hawassa University for providing funding for this study. Our heartfelt gratitude also goes to the data collectors and participants for their valuable contributions to the study process.
Abbreviations
AOR, Adjusted Odds Ratio; CI, Confidence Interval; COR, Crude Odds Ratio; COVID-19, the 2019 Coronavirus Disease; IES-R, Impact of Event Scale-Revised; HUCSH, Hawassa University Comprehensive Specialized Hospital; HCWs, Health Care Workers; OPD, Out Patient Department; PTSD, Post Traumatic Stress Disorder; WHO, World Health Organization.
References
1. Wang C. A novel coronavirus outbreak of global health concern. Lancet. (2020) (2020). 395:470–3. doi: 10.1016/S0140-6736(20)30185-9
2. Mahase E. China coronavirus: WHO declares international emergency as death toll exceeds 200. BMJ Clin Res Ed. (2020) 368:m408. doi: 10.1136/bmj.m408
3. WHO. COVID-19 Weekly Epidemiological Update: Edition 68. World Health Organization (2021). p. 1–24. Available online at: file:///C:/Users/Admin/Downloads/20211130_Weekly_Epi_Update_68.pdf
4. Ethiopian Public Health Institute (EPHI). COVID-19 Pandemic Preparedness and Response in Ethiopia Weekly Bulletin, Epi-Week- 47 (November 22 – 28, 2021): Bulletin Number 83. (2021). Available online at: https://ephi.gov.et/wp-content/uploads/2021/02/EPHI_PHEOC_COVID-19_Weekly_Bulletin_83_English_11302021.pdf
5. Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E KP. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. (2020) 88:901–7. doi: 10.1016/j.bbi.2020.05.026
6. Xiang Y-T, Yang Y, Li W, Zhang L, Zhang Q, Cheung T, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. (2020) 7:228–9. doi: 10.1016/S2215-0366(20)30046-8
7. Chen Q, Liang M, Li Y, Guo J, Fei D, Wang L, et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. (2020) 7:e15–6. doi: 10.1016/S2215-0366(20)30078-X
8. Kang L, Li Y, Hu S, Chen M, Yang C, Yang BX, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. (2020) 7:e14. doi: 10.1016/S2215-0366(20)30047-X
9. Asukai N, Kato H, Kawamura N, Kim Y, Kishimoto J, Miyake Y, et al. Reliability and validity of the Japanese-language version of the impact of event scale-revised (IES-R-J): Four studies of different traumatic events. J Nerv Ment Dis. (2002) 190:175–82. doi: 10.1097/00005053-200203000-00006
10. Hawryluck L, Gold WL, Robinson S, Pogorski S, Galea S, Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis. (2004) 10:1206–12. doi: 10.3201/eid1007.030703
11. Jeong H, Yim HW, Song YJ, Ki M, Min JA CJ CJ. Mental health status of people isolated due to Middle East Respiratory Syndrome. Epidemiol Heal. (2016) 38:e2016048. doi: 10.4178/epih.e2016048
12. American Psychiatric Association (APA). Diagnostic Statistical Manual of Mental Disorders. 5th ed. Washington, DC: APA (2013).
13. Huang JZ, Han MF, Luo TD, Ren AK, Zhou XP. Mental health survey of 230 medical staff in a tertiary infectious disease hospital for COVID-19. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. (2020) 38:192–5. doi: 10.3760/cma.j.cn121094-20200219-00063
14. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int J Environ Res Public Heal. (2020) 17:1–25. doi: 10.3390/ijerph17051729
15. Tan BY, Chew NW, Lee GK, Jing M, Goh Y, Yeo LL et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med. (2020) 173:317–20. doi: 10.7326/M20-1083
16. Urnes S, Id J, Ebrahimi OV, Hoffart A. PTSD symptoms among health workers and public service providers during the COVID-19 outbreak. PLoS ONE. (2020) 15:e0241032. doi: 10.1371/journal.pone.0241032
17. Patricia L, Hernández- MA. Psychological distress and signs of post-traumatic stress in response to the COVID-19 health emergency in a Mexican Sample. Psychol Res Behav Manag. (2020) 13:589–97. doi: 10.2147/PRBM.S259563
18. Wang Y, Guo H, Du X, Song W, Lu C, Hao W. Factors associated with post-traumatic stress disorder of nurses exposed to corona virus disease 2019 in China. Medicine. (2019) 99:1–6. doi: 10.1097/MD.0000000000020965
19. Asnakew S, Legas G, Muche T, Liyeh, Belete A, Haile K, et al. Prevalence of post-traumatic stress disorder on health professionals in the era of COVID-19 pandemic, Northwest Ethiopia, 2020 : a multi- centered cross-sectional study. PLoS ONE. (2021) 16:e0255340. doi: 10.1371/journal.pone.0255340
20. Yitayih Y, Mekonen S, Zeynudin A, Mengistie E, Ambelu A. Mental health of healthcare professionals during the early stage of the COVID-19 pandemic in Ethiopia. BJPsych Open. (2021) 7:1–6. doi: 10.1192/bjo.2020.130
21. Jemal K, Deriba BS, Geleta TA. Psychological distress, early behavioral response, and perception toward the COVID-19 pandemic among health care workers in North Shoa Zone, Oromiya Region. Front Psychiatry. (2021) 12:1–12. doi: 10.3389/fpsyt.2021.628898
22. Chekole YA, Minaye SY, Abate SM, Mekuriaw B. Perceived stress and its associated factors during COVID-19 among healthcare providers in Ethiopia : a cross-sectional study. Adv Public Heal. (2020) 2020:1–7. doi: 10.1155/2020/5036861
23. Asnakew S, Amha H, Kassew T. Mental health adverse effects of COVID-19 pandemic on health care workers in North West Ethiopia : a multicenter cross-sectional study. Neuropsychiatr Dis Treat. (2021) 17:1375–84. doi: 10.2147/NDT.S306300
24. Tiong WW KG. Ethical considerations in the review of Singapore's H1N1 pandemic response framework in 2009. Ann Acad Med Singapore. (2013) 42:246–50.
25. Chan AOM HC. Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore. Occup Med Oxf Engl. (2004) 54:190–6. doi: 10.1093/occmed/kqh027
26. Kang P, Lv Y, Hao L, Tang B, Liu Z, Liu X, et al. Psychological consequences and quality of life among medical rescuers who responded to the 2010 Yushu earthquake: a neglected problem. Psychiatry Res. (2015) 230:517–23. doi: 10.1016/j.psychres.2015.09.047
27. Liu YH, Yang HN, Liu HL, Wang F, Hu LB, Zheng JC. Medical rescue of China National Earthquake Disaster Emergency Search and Rescue Team in Lushan earthquake. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. (2013) 25:265–7. doi: 10.3760/cma.j.issn.2095-4352.2013.05.004
28. Zhang MW. Usage of social media and smartphone application in assessment of physical and psychological well-being of individuals in times of a major air pollution crisis. JMIR mHealth uHealth. (2014) 2:e16. doi: 10.2196/mhealth.2827
29. Zhang MWB. Methodology of developing a smartphone application for crisis research and its clinical application. Technol Heal Care. (2014) 22:547–59. doi: 10.3233/THC-140819
30. Weiss DS, Marmar C. The impact of event scale – revised. In: Wilson JP, Keane TM, editors. Assessing Psychological Trauma PTSD. New York, NY: Guilford Press (1997). p. 399–411.
31. Creamer M, Bell RFS. Psychometric properties of the Impact of Event Scale - Revised. Behav Res Ther. (2003) 41:1489–96. doi: 10.1016/j.brat.2003.07.010
32. Conti C, Fontanesi L, Lanzara R, Rosa I, Porcelli P. Fragile heroes. The psychological impact of the COVID-19 pandemic on health-care workers in Italy. PLoS ONE. (2020) 11:e0242538. doi: 10.1371/journal.pone.0242538
33. Luceño-Moreno L, Talavera-Velasco B, Garci 'a-Albuerne Y M 'n-G 'a J. Symptoms of posttraumatic stress, anxiety, depression, levels of resilience and burnout in Spanish health personnel during the COVID-19 pandemic. Int J Environ Res Public Health. (2020) 17:5514. doi: 10.3390/ijerph17155514
34. Gilleen J, Santaolalla A, Valdearenas L, Salice C. Impact of the COVID-19 pandemic on the mental health and well-being of UK healthcare workers. BJPsych Open. (2021) 7:1–12. doi: 10.1192/bjo.2021.42
35. Shechter A, Diaz F, Moise N, Anstey DE, Ye S, Agarwal S et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen Hosp Psychiatry. (2020) 66:1–8. doi: 10.1016/j.genhosppsych.2020.06.007
36. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open J. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
37. Giusti EM, Pedroli E, Aniello GED, Badiale CS, Pietrabissa G, Manna C, et al. The psychological impact of the COVID-19 outbreak on health professionals : a cross-sectional study. Front Psychol. (2020) 11:1–9. doi: 10.3389/fpsyg.2020.01684
38. Preti E, Mattei V Di, Perego G, Ferrari F, Mazzetti M, Taranto P, et al. The psychological impact of epidemic and pandemic outbreaks on healthcare workers : rapid review of the evidence. Curr Psychiatry Rep. (2020) 22:1–22. doi: 10.1007/s11920-020-01166-z
39. Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, & Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. (2020) doi: 10.2139/ssrn.3594632
40. Mohamad-Hani Temsah SA. Understanding the psychological stress and optimizing the psychological support for the acute - care health - care workers during the COVID - 19 pandemic. Saudi Crit Care J. (2020) 4:25–7. doi: 10.4103/sccj.sccj_62_20
41. Alateeq DA, Aljhani S, Althiyabi I, Majzoub S. Journal of Infection and Public Health Mental health among healthcare providers during coronavirus disease (COVID-19) outbreak in Saudi Arabia. J Infect Public Health. (2020) 13:1432–7. doi: 10.1016/j.jiph.2020.08.013
42. Eaton NR, Keyes KM, Krueger RF et al. An invariant dimensional liability model of gender differences in mental disorder prevalence: evidence from a national sample. J Abnorm Psychol. (2012) 121:282–8. doi: 10.1037/a0024780
43. Seedat S, Scott KM, Angermeyer MC et al. Cross-national associations between gender and mental disorders in the World Health Organization world mental health surveys. Arch Gen Psychiatry. (2009) 66:785–95. doi: 10.1001/archgenpsychiatry.2009.36
44. Azoulay E, Cariou A, Bruneel F, Demoule A, Kouatchet A, Reuter D, et al. Symptoms of anxiety, depression, and peritraumatic dissociation in critical care clinicians managing patients with COVID-19 a cross-sectional study 1388. Am J Respir Crit Care Med. (2020) 202:1388–98. doi: 10.1164/rccm.202006-2568OC
45. Luo M, Guo L, Yu M WH. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on Medical Staff and General Public–A Systematic Review and Meta-analysis. Psychiatry Res. (2020). 291:113190. doi: 10.1016/j.psychres.2020.113190
46. Rossi R, Socci V, Pacitti F, Di Lorenzo G, Di Marco A, Siracusano A, et al. Mental health outcomes among frontline and second-line health careworkers during the coronavirus disease 2019 (COVID- 19) Pandemic in Italy. JAMA Netw Open. (2020) 3:e2010185. doi: 10.1001/jamanetworkopen.2020.10185
47. Barello S, Palamenghi L GG. Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Psychiatry Res. (2020) 290:113129. doi: 10.1016/j.psychres.2020.113129
48. Seidler ZE, Dawes AJ, Rice SM, Oliffe JL DH. The role of masculinity in men's help-seeking for depression: a systematic review. Clin Psychol Rev. (2016) 49:106–18. doi: 10.1016/j.cpr.2016.09.002
49. Galdas PM, Cheater F MP. Men and health help-seeking behaviour: literature review. J Adv Nurs. (2005) 49:616–23. doi: 10.1111/j.1365-2648.2004.03331.x
50. Bulut D, Sefa M, Buket S, Ender K, Bulut C, Çelik S. Which of us were more affected by the pandemic? The psychiatric impacts of the COVID-19 pandemic on healthcare professionals in the province where the first quarantine units were established in Turkey. Int J Clin Pr. (2021) 75:e14235. doi: 10.1111/ijcp.14235
51. Nickell LA, Crighton EJ, Tracy CS, Al-Enazy H, Bolaji Y, Hanjrah S, et al. Psychosocial effects of SARS on hospital staff: survey of a large tertiary care institution. CMAJ. (2004) 170:793–8. doi: 10.1503/cmaj.1031077
52. Wu P, Fang Y, Guan Z, Fan B, Kong J, Yao Z, et al. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry. (2009) 54:302–11. doi: 10.1177/070674370905400504
53. Tham KY, Tan YH, Loh OH, Tan WL, Ong MK, Tang HK. Psychological morbidity among emergency department doctors and nurses after the SARS outbreak. Hong Kong J Emerg Med. (2005) 12:215–23. doi: 10.1177/102490790501200404
54. Zhang C, Yang L, Liu S, Ma S, Wang Y, Cai Z, et al. Survey of insomnia and related social psychological factors among medical staf involved in the 2019 novel coronavirus disease outbreak. Front Psychiatry. (2020) 11:306. doi: 10.3389/fpsyt.2020.00306
55. Temsah M, Barry M, Aljamaan F, Alhuzaimi AN. SARS-CoV-2 B.1.1.7 UK variant of concern lineage-related perceptions, COVID-19 vaccine acceptance and travel worry among healthcare workers. Front Public Heal. (2021) 9:686958. doi: 10.3389/fpubh.2021.686958
56. Zwack JSJ. If every fifth physician is affected by burnout, what about the other four? Resilience strategies of experienced physicians. Acad Med. (2013) 88:382–9. doi: 10.1097/ACM.0b013e318281696b
57. Zwack J, Abel CSJ. Physicians' resilience—salutogenetic practices and attitudes of experienced physicians. Psychother Psychosom Med Psychol. (2011) 61:495–502. doi: 10.1055/s-0031-1291276
58. Joliat G, Demartines NUE. Systematic review of the impact of patient death on surgeons. B J Surg. (2019) 1429–32. doi: 10.1002/bjs.11264
Keywords: psychological trauma, PTSD symptoms, health care workers, COVID-19, Ethiopia
Citation: Ayalew M, Deribe B, Abraham Y, Reta Y, Tadesse F and Defar S (2022) Post-traumatic Stress Disorder Symptoms and Its Predictors Among Healthcare Workers Following COVID-19 Pandemic in Southern Ethiopia: A Cross-Sectional Study. Front. Psychiatry 12:818910. doi: 10.3389/fpsyt.2021.818910
Received: 20 November 2021; Accepted: 10 December 2021;
Published: 04 January 2022.
Edited by:
Krystyna Kowalczuk, Medical University of Bialystok, PolandReviewed by:
Rahul Varma, Banaras Hindu University, IndiaMohamad-Hani Temsah, King Saud University, Saudi Arabia
Federica Ricci, University of Turin, Italy
Copyright © 2022 Ayalew, Deribe, Abraham, Reta, Tadesse and Defar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mohammed Ayalew, bWFtZWF5YWxlQGdtYWlsLmNvbQ==
 Mohammed Ayalew
Mohammed Ayalew Bedilu Deribe1
Bedilu Deribe1 Yared Reta
Yared Reta Fikru Tadesse
Fikru Tadesse