- 1Institut für Sinnes- und Sprachneurologie, Konventhospital Barmherzige Brüder Linz, Linz, Austria
- 2Research Institute for Developmental Medicine, Johannes Kepler University Linz, Linz, Austria
- 3AJ Drexel Autism Institute, Drexel University, Philadelphia, PA, United States
- 4Olga Tennison Autism Research Centre, La Trobe University, Melbourne, VIC, Australia
- 5Child and Adolescent Psychiatry and Psychotherapy, University Medical Center Göttingen and Leibniz Science Campus Primate Cognition, Göttingen, Germany
- 6Centre of Neurodevelopmental Disorders (KIND), Centre for Psychiatry Research, Department of Women's and Children's Health, Karolinska Institutet, Stockholm, Sweden
- 7Interdisciplinary Developmental Neuroscience, Division of Phoniatrics, Medical University of Graz, Graz, Austria
- 8Institut für Linguistik, Universität Graz, Graz, Austria
Children with autism spectrum disorder (ASD) show difficulties in social communication behaviors, emotion regulation and daily living skills, and they frequently present with challenging behaviors. In parents of children with ASD, higher rates of stress and mental health problems have been reported than in parents of either typically developing children or children with other conditions. In this study, we tested whether maternal well-being changes with improved social communicative behaviors of children with ASD receiving early intervention. We examined developmental changes in 72 pre-schoolers and stress levels in their mothers (measured by the Parental Stress Inventory) before and after a 12-month community-based intervention program based on the Early Start Denver Model, a naturalistic developmental behavioral intervention targeting social communication. Multiple regression analyses showed that maternal child-related stress was predicted by changes in children's social communication behaviors (measured with the Pervasive Developmental Disorder Behavior Inventory). Gains in the early social communication behavior domain were the strongest predictor of post-intervention child-related maternal stress, surpassing adaptive behavior, language and non-verbal cognitive gains, and reduction in challenging behavior. These findings support the hypothesis that, in children with ASD, the acquisition of social communication behaviors contribute to improvements in maternal well-being.
Introduction
Autism spectrum disorder (ASD) is characterized by difficulties in social communication, patterns of restricted/repetitive behaviors and interests, and onset in early childhood (1). Higher rates of chronic parental stress, reduced overall well-being, increased occurrence of anxiety and depression and lower parental self-efficacy have been reported for parents of children with ASD compared to parents of either typically developing children or children with other disabilities such as Down syndrome or cerebral palsy (2–6). Mothers of children with ASD often score higher on stress levels than fathers (7). These increased rates of parental stress suggest that ASD-specific core symptoms, such as social communication difficulties and restricted and repetitive behaviors, might contribute to diminished parental well-being (8). Additionally, comorbid conditions—such as attention deficit hyperactivity disorder (ADHD), oppositional defiant disorder (9), behavioral/emotional problems (10–12) and anxiety or depression (13, 14)—that are often comorbid with ASD might intensify maternal stress.
Child Factors Impacting Parental Health
A number of characteristics and behaviors of children with ASD have been associated with parental distress, including autism severity (15, 16), social communication deficits (17, 18), and challenging behaviors (10, 17). Peculiar speech-language functions or atypical communication is often the parents' first and major concern that leads them to seek professional help (19). Especially difficulties in social communication continue—across the lifespan—to cause parental distress, including anxiety and confusion about their child's behavior and parental feelings of inefficacy (20). Furthermore, higher rates of aggressive and self-injurious behaviors have been reported in children with severe social communication deficits (21). The link between challenging behaviors and increased parental stress is well-established (22). In addition to communication problems and challenging behaviors, impairments in cognitive and adaptive functioning that frequently occur in ASD are major causal factors of parental stress (23, 24) and frustration (25).
Effects of Intervention on Parental Well-Being
In his developmental systems model for early intervention Guralnick (26) described the bidirectional relationship between family factors (e.g., socioeconomic status, mental health, coping styles, and social support) and child development mediated by family-child interactions that include parent-child communication and socio-emotional connectedness. Stressed parents are less likely to engage in positive interactions with their children and to be actively involved in intervention programs. However, social and cognitive difficulties in affected children must be regarded as stressors that may impact parent-child interaction and may consequently increase parental stress. Intervention approaches that focus on child social communication behaviors are therefore expected to positively affect parental stress. Research into the effect of specific components of intervention programs targeting child behavior (e.g., communication, cognitive functioning, and adaptive skills) on parental stress remains limited. Ozturk et al. (27) reported that improvements in social communication skills following early intervention had a positive impact on maternal satisfaction and psychological distress as measured by the Depression Anxiety and Stress Scale (28). Additional research has shown that family-centered approaches that directly target family outcomes by providing socio-emotional support to families and/or parent training in positive interaction strategies with their child are associated with greater family involvement, self-efficacy and well-being (26, 29). Examples include the parent-implemented Early Start Denver Model (P-ESDM) intervention (10) and the PACT program (30), both of which have been associated with reductions in parental stress.
The aim of this study was to evaluate whether stress in mothers of children with ASD is impacted by changes in child behavior after a 1-year early-intervention program. To this end, we deployed a community-based intervention (31) utilizing the ESDM approach. The ESDM is an evidence-supported early-intervention program for children with ASD aged 1–4, with a focus on promoting social communication behaviors. The principles and strategies of ESDM are informed by behavioral and developmental research that highlights the importance of early social engagement and social communication in the development of children with ASD (32–37). Empirical support for the ESDM includes evidence of improvements in cognitive and communication functioning (38, 39).
Based on the body of knowledge gained through these studies, we hypothesized (1) that maternal child-related stress would decrease between baseline (T1) and post-intervention (T2) in mothers of children receiving ESDM intervention for 1 year; (2) that the enhancement of social communication behaviors between T1 and T2, assessed by parent report, predicts the outcome of maternal child-related stress at T2; and that (3) improvements in (a) verbal skills and (b) non-verbal cognition (both directly assessed with standardized instruments) and (c) adaptive behavior skills and (d) behavioral problems (both parent-reported) predict the outcome of maternal child-related stress at T2.
Methods
The study was conducted at the Institute of Neurology of Senses and Language, hospital of St. John of God Linz, which provides multidisciplinary diagnostic and intervention services for children with developmental disorders, with a focus on communication disorders.
Outcome Measures
Parenting Stress Index Short Form
The widely used Parenting Stress Index Short Form (40) is a self-report for measuring difficulties related to the parenting role. The questionnaire is available in German (41) and normed to German mothers of a non-clinical group of children and has good to excellent validity and reliability scores. The PSI-SF resulted from a factor analysis of the original long form with a correlation for the total stress scores of r = 0.94, p < 0.001 (42) and the subscales show high internal consistency, with alphas of 0.91–0.95 and test–retest reliability from 0.85 to 0.87 (41). The PSI has frequently been used with a wide range of pediatric populations (43–45). The German short form comprises 48 items (12 subscales with 4 items) which are rated on a 5-point Likert scale, with higher scores reflecting higher stress. The PSI parental domain consists of seven subscales (e.g., “Isolation” and “Health Problems”) and was labeled as “PSI parental stress” in this study. The PSI child domain—which is a measure of the stressor or demand—consists of five subscales (e.g., “Acceptability” and “Demandingness”), which was labeled as “PSI child-related stress.” In addition to these two main domains, norms exist for a PSI composite score.
Predictors of Maternal Stress Outcome
Pervasive Developmental Disorder Behavior Inventory—Social Approach Behaviors
The Social Approach Behaviors dimension (SOCAPP) of the PDDBI (46) assesses a variety of primarily non-verbal social communication behaviors that are challenging for children with ASD. The scale comprises the following nine subdomains: visual social approach behaviors (e.g., “Pays attention to other's face when given instructions or when asked questions”), positive affect behaviors (e.g., “Smiles when praised”), responsiveness to social inhibition cues (e.g., “Completely stops inappropriate behavior for at least a day when warned or punished”), social play behaviors (e.g., “Selects his/her own toys to play with and allows other(s) to play along”), imaginative play behaviors [e.g., “Shows more complex imaginative toy play (e.g., ‘feeds doll, makes Superman™ toy fly')”], empathy behaviors (e.g., “Tries to physically or verbally comfort others when they are sad”), social interaction behaviors [e.g., “Seeks affection (e.g., hugs and kisses) from caregivers or siblings”], social imitative behaviors (e.g., “Can imitate tongue clicking”) and gestural approach behaviors [e.g., “Moves arm(s)/hand(s) in beckoning motion to signal others to come to him/her”]. The SOCAPP scale has an excellent reliability score (α = 0.91) and highly correlates with the Childhood Autism Rating Scale [(47); r = 0.60], the Vineland Adaptive Behavior Scales [(48); Socialization r = 0.58] and the Griffiths scales [(49); General IQ r = 0.63]. The SOCAPP composite score can be interpreted as strengths/weaknesses in the use of a large variety of social communication behaviors compared to an age-referenced norm sample of children with ASD, further labeled as “PDDBI SOCAPP.”
Aberrant Behavior Checklist
The Aberrant Behavior Checklist (50) is a 58-item behavior rating scale which is used to measure behavioral problems across five subdomains. All items are rated on a 4-point Likert scale (0–3), with higher scores indicating more severe problems. Following the recommendation of Kaat et al. (51), we report only scores of given subscales of the ABC with a proven robust factor structure, acceptable to excellent internal consistencies and also recently reported norm values for children with ASD <6 years and ID. Others have shown that the ABC is a sensitive instrument applicable in treatment and intervention studies (52, 53). We concentrated on external behavioral problems and the link to maternal stress outcome. Therefore, the scales Stereotypy (e.g., “repetitive hand movements”), Hyperactivity/Non-compliance (e.g., “excessively active”) and Irritability, including items encompassing intense emotional states, such as self-aggression, and aggressive behaviors (e.g., “cries and screams” and “willingly hurts him/herself”), were chosen to measure this construct. The internal consistencies for the chosen factors were: Stereotypic Behavior α = 0.87, Hyperactivity/Non-compliance α = 0.94 and Irritability α = 0.92 (51). We labeled these three scales as “ABC Stereotypy,” “ABC Hyperactivity,” and “ABC Irritability.”
Mullen Scales of Early Learning
Child non-verbal and verbal cognitive abilities were assessed using the Mullen Scales of Early Learning (54), which is a standardized developmental assessment for children 0–68 months of age. The enclosed and so named developmental domains are Visual Reception, Fine Motor Skills, Receptive Language and Expressive Language. Reliabilities were obtained for younger (0–2 years) and older (2–5 years) children with good stability coefficients for the younger group (0.82–0.85) and less reliable coefficients for the older group (0.71–0.79) with very high interrater reliability for both age groups (0.91–0.99). Since we encountered floor effects when calculating T-scores for our sample, we derived developmental quotients (DQ: age-equivalent/chronological age × 100) for each subscale in accordance with others [e.g., (55)]. As measures of non-verbal development, a composite score of the age-corrected MSEL subdomains Fine Motor Skills and Visual Recognition and, by analogy, as a measure of verbal DQ a composite of the Expressive and Receptive Language scales were derived and labeled as “MSEL Non-verbal” and “MSEL Verbal.”
Vineland Adaptive Behavior Scales 2nd Edition
The Vineland Behavior Scales Second Edition (56) is a questionnaire which measures daily living skills as reported by parents and includes personal skills (e.g., “eating, dressing, or personal hygiene”), domestic skills (e.g., “being careful using sharp objects”; “household tasks such as putting toys away”) and community skills (e.g., “remaining within safe distance of caregiver”). Reasons for selecting this specific subscale were time restrictions and the high relevance to children and families in everyday life (57). As for the MSEL subdomains, developmental quotients (age-equivalent/chronological age * 100) were derived for this subscale for better comparability with the reported MSEL subdomains and labeled as “VABS Daily Living.”
Controlling Predictor Variables
To control for potentially confounding variables, we included child's age (“Age Child”), multilingualism of family (“Multilingualism”) and maternal educational level (“Mother's Level of Education”) in our analyses.
Intervention
Participants
Seventy-two children with ASD (63 male, 9 female) aged 29–60 months (M = 41.56; SD = 7.10) and their parents enrolled in this study. Most of the participating families were multilingual (72.2%) with 44.5% of the mothers holding at least a high school diploma and with an average of 1.10 (SD = 1.14) siblings living in the family. Participants were recruited consecutively from the community-based early-intervention program provided by our department, where they had been referred after diagnostic assessment between March 2014 and February 2020. Participants met DSM-5 criteria for ASD according to diagnostic assessments based on a multidisciplinary evaluation process using the ADOS-2 (58), which included a clinical assessment and a questionnaire battery (as described above). Intervention was offered to all families who met the following criteria: (a) child diagnosed with ASD, (b) non-verbal developmental age of at least 1 year, (c) parents requested early intervention, and (d) sufficient language skills (German or English). Assessments were administered in the family's primary language, with translation support when needed.
Implementation of the Intervention
The intervention team consisted of 12 therapists from various disciplines (speech-language therapy, occupational therapy, clinical psychology, special education) certified in the ESDM. The training and certification process lasted between 7 and 13 months (35). Prior to intervention, most of the parents took part in a parent-training workshop comprising six 2-h meetings per week which was developed and offered by the department's intervention team. Parents attended at least 1 weekly appointment with the interventionist over the 1-year intervention at which parent coaching was provided. During this period, therapy was delivered two to three times a week with a duration of 90 min. For further details on the intervention see (59).
Design and Statistical Analysis
In this study we used a within-subject longitudinal design (T1-T2) to measure developmental change in child variables and parental stress that occurred during the 12-month intervention period. All variables of interest were measured using the standardized instruments listed above at T1. All measures—except the ADOS-2 assessment—were re-administered after the intervention period (T2), with an average of 11.49 (range: 9–13; SD = 0.87) months between T1 and T2. All data analyses were conducted with SPSS 26 statistical software. Paired sample tests were performed to separately analyze differences in child and maternal dimensions before and after treatment. To control for Type 1 errors due to multiple comparisons, the Bonferroni-Holm correction was applied to all child and maternal p-values. First, bivariate Pearson correlations between putative predictors were derived, and then between putative predictors and outcome variables. For all comparisons, Cohen's d was calculated and reported. All predictor variables were checked for multicollinearity, with very good variance inflation factors and tolerance values. Several multiple and hierarchical regressions were performed to examine the extent of variance explained by defined predictor variables.
Results
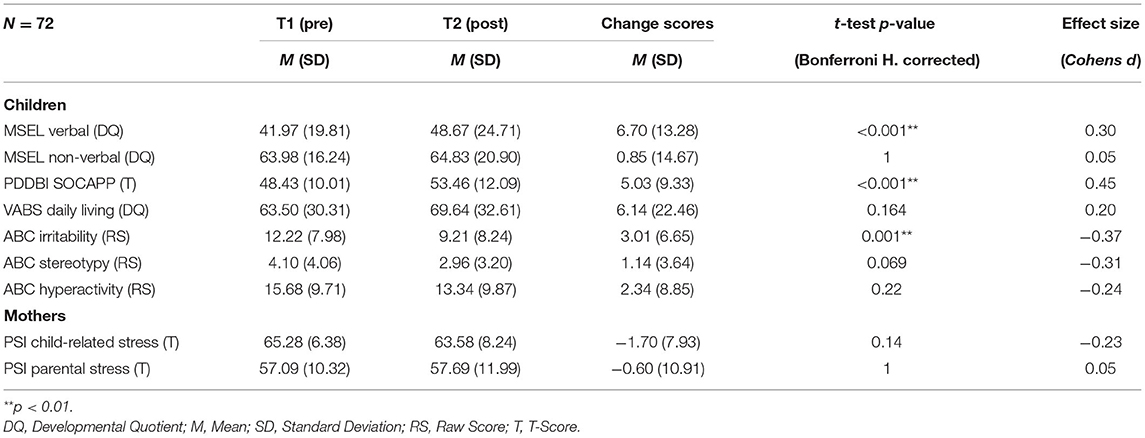
At baseline the children showed severe delays in language development (MSEL Verbal DQ = 41.97; SD = 19.81) and less severe delays in non-verbal development (MSEL Non-verbal DQ = 63.98; SD = 16.24). Social Approach Behaviors (PDDBI SOCAPP) as rated by parents indicated average levels (T = 48.43, SD = 10.01) compared to a normed sample of children with ASD. The parent-rated PSI child-related stress score was above the chosen clinically relevant individual level of T ≥ 65 in accordance with others (60), with a group mean of T = 65.28 (SD = 6.38). The PSI parental stress score (non-child-related) was statistically increased (T = 57.09; SD = 10.32) using a one sample t-test [t(63) = 5.50; p < 0.001] with a comparison value of T = 50. Table 1 reports the results for child development and maternal stress at intervention start (T1) and post-intervention (T2). There were no significant maternal stress changes for PSI child-related stress [T2-T1: t(63) = 1.79; p = 0.14] or PSI parental stress [T2-T1: t(63) = −0.44; p = 1.00] for the whole group. In an exploratory analysis, we split the mothers into two groups: clinically significant PSI child-related stress score at T1 (T ≥ 65) and subclinical (T < 65) score. Conducting a two-factor variance analysis (Group × Time) for the PSI child-related stress group (clinical, subclinical) and time (T1, T2) revealed an significant interaction effect [F(1,62) = 12.86; p = 0.001]. The clinical PSI child-related stress group showed a significant reduction [t(39) = 3.66; p = 0.001], the subclinical PSI child-related group showed a trend in the opposite direction [t(23) = −1.71; p = 0.101].
Although PSI parental stress scores were significantly higher than in the norm group at both time points, these scores were not clinically relevant at the group level and were significantly lower than the PSI child-related stress scores pre- and post-intervention, which were clinically significant (T ~ 65) at the group level. Importantly, for the PSI child-related stress score, our sample exhibited ceiling effects (T-value of 70: at T1 N = 31 and at T2 N = 27). As also shown in Table 1, children made statistically significant improvements between T1 and T2 in the dimensions of language development (MSEL Verbal DQ; p < 0.001; d = 0.30), Social Approach Behaviors (PDDBI SOCAPP; p < 0.001, d = 0.45) and Irritability (ABC-Irritability; p = 0.001; d = 0.37). No significant changes in child MSEL Non-verbal DQ (p = 1.00; d = 0.05) or Daily Living Skills (VABS Daily Living; p = 0.164; d = 0.20) were found.
Intercorrelations between the putative predictors of maternal stress are presented in Supplementary Material. Correlations between putative predictors and maternal stress at T2 are reported in Table 2. PSI child-related stress at T2 correlated moderately with PSI child-related stress at T1 (r = 0.44, p < 0.001) and with PSI parental stress at T1 (r = 0.38, p = 0.002) and weakly with PDDBI SOCAPP gains (r = −0.28, p = 0.018). PSI child-related stress at T2 did not correlate with Mother's Level of Education (r = 0.04) or MSEL Non-verbal/Verbal gains (both r's = −0.16). We did not find a significant correlation with VABS Daily Living gains or reduction in behavioral problems. PSI parental stress at T2 correlated significantly only with PSI parental and child-related stress at T1.
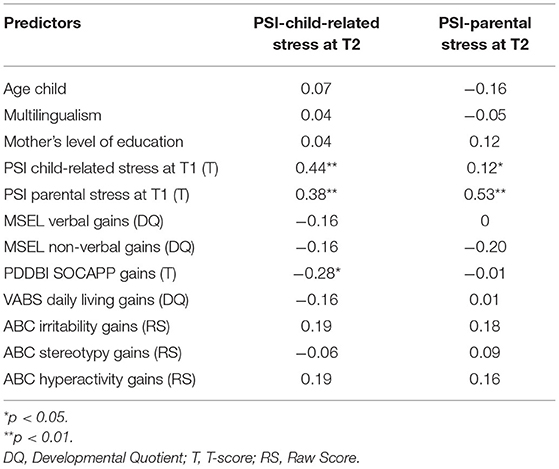
Table 2. Correlations (pooled) between putative predictors and PSI child-related gains (difference) and PSI child-/parental outcome (after 12 months).
Four independent multiple regression analyses were performed to examine the predictive value of sociodemographic variables and verbal- and non-verbal gains on PSI stress outcome at T2 (see Table 3). Age Child, Mother's Level of Education, Multilingualism and MSEL Verbal/Non-verbal gains did not explain any substantial variance of PSI child-related or PSI parental outcome at T2. Due to their lack of significance, and in accordance with previous studies (17), none of the controlling predictor variables listed in Table 3 was included in further regression analyses.
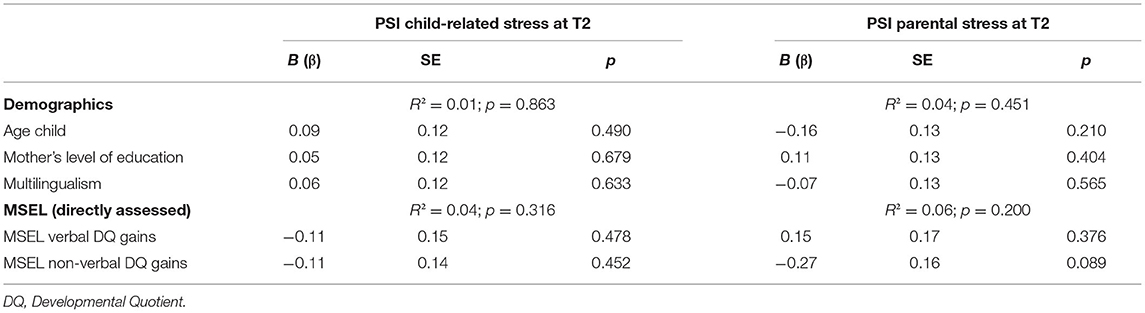
Table 3. Multiple regression analyses using z-standardized (pooled) values of demographic variables and MSEL verbal/non-verbal DQ gains predicting PSI child-related and parental stress at T2.
Two independent multiple hierarchical regression analyses were carried out to examine relations between the independent predictor variables and the dependent PSI child-related and PSI parental stress at T2 variables. In both models, the following variables were sequentially entered: PSI child-related and PSI parental stress at T1 in step 1, PDDBI SOCAPP gains in step 2, VABS Daily Living gains in step 3 and ABC Irritability-, ABC Stereotypy-, and ABC Hyperactivity- gains in step 4 (see Tables 4, 5).
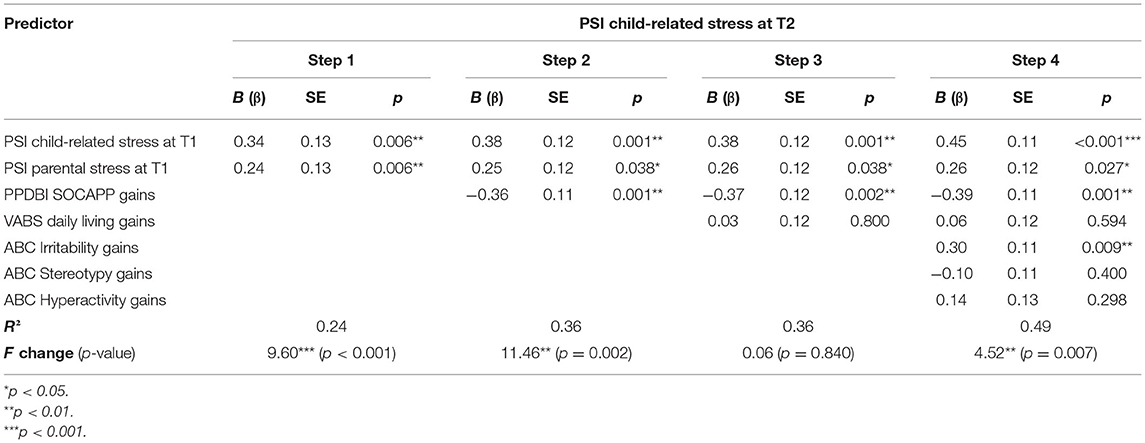
Table 4. Hierarchical multiple regression analysis (pooled) predicting PSI child-related stress at T2.
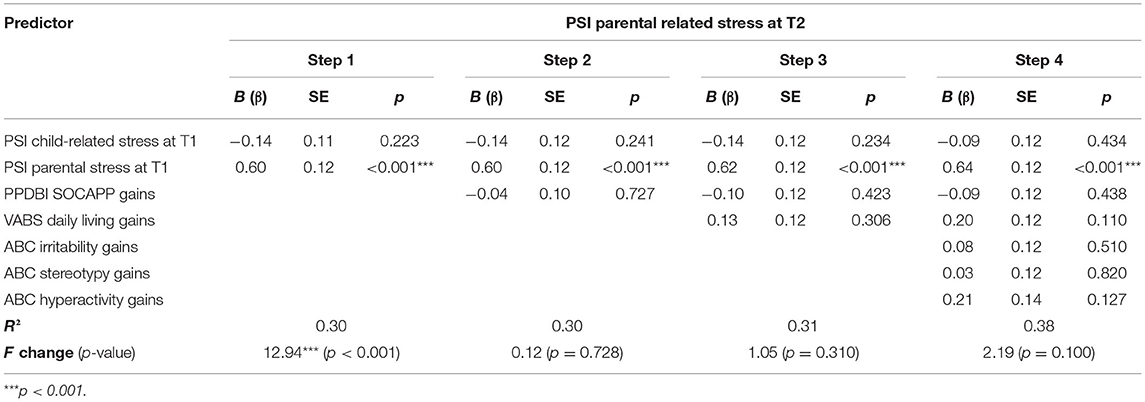
Table 5. Hierarchical multiple regression analysis (pooled) predicting PSI parental related stress at T2.
As shown in Table 4, PSI child-related and PSI parental stress at T1 scores predicted 24% of the variance of PSI child-related stress at T2 (Fchange = 9.60, p < 0.001). Adding PDDBI SOCAPP gains in step 2 led to a highly significant improvement (plus 12%), which resulted in a total explanation of variance of 36% (Fchange = 11.32 p < 0.001). PDDBI SOCAPP gains (β = −0.36, p = 0.001) were revealed to be a stronger predictor than PSI parental stress at T1 (β = 0.25, p = 0.038) and as predictive as the PSI child-related stress at T1 score (β = 0.38, p = 0.001). Adding VABS Daily Living gains in a third step showed no change in variance explanation. In a fourth step, we added three ABC subscale change scores (ABC Irritability, ABC Stereotypy, ABC Hyperactivity), which led to a significant improvement in variance explanation in this final model (plus 13%; R2 = 0.49; Fchange = 4.52, p = 0.007). The three strongest predictors in this final model were PSI child-related stress at T1 (β = 0.45, p < 0.001), PDDBI SOCAPP gains (β = −0.39, p = 0.001) and ABC Irritability gains (β = 0.30, p = 0.009).
In contrast, as demonstrated in Table 5, only PSI parental stress at T1 contributed markedly to variance explanation (30%) of PSI parental stress at T2 in a first analytical step (Fchange = 2.94, p < 0.001). Incorporating PDDBI SOCAPP gains in a second (R2 = 0.30) and VABS Daily Living gains in a third step (R2 = 0.31) resulted in no change in variance explanation of PSI parental stress at T2. The fourth step, entering the three ABC subscale change scores (ABC Irritability, ABC Stereotypy, ABC Hyperactivity), led to a non-significant increase in variance explanation (plus 7%; R2 = 0.38; Fchange = 2.19, p = 0.100). In this final model, the only significant predictor of PSI parental stress at T2 was—as in the other steps—PSI parental stress at T1 (β = 0.64, p < 0.001).
Discussion
In this study we examined changes in maternal stress before and after ESDM intervention, and the relationship between stress outcomes and various dimensions of child development during the 1-year intervention period. As the ESDM focuses on the enhancement of child social communication behaviors, our particular interest was in the specific role of social communication development in predicting maternal stress, also considering gains in language, non-verbal cognition, adaptive skills and a reduction in aberrant behaviors. Our results did not support our first hypothesis of maternal stress decreasing during the intervention period. No significant differences in maternal stress between baseline and post-intervention were found, neither for child-related nor for parental stress in mothers. That maternal stress does not change significantly in the course of primarily child-related interventions is supported by previous findings (10, 11). Our data showed very high values comparable with those in other studies of young children with ASD (61). Child-related maternal stress scores were clinically relevant and persisted throughout the intervention period. Interestingly, in further exploratory analyses we found differences in child-related maternal stress development between mothers who reported clinically relevant child-related stress scores at baseline (T score ≥ 65) and mothers who scored below (subclinical group). Mothers with very high child-related stress scores showed a significant reduction in child-related stress in contrast to the group of mothers with subclinical child-related stress, who reported a slight increase in child-related stress. This within-group interaction effect might in part explain our findings of no groupwise change in child-related stress score during intervention. Closer investigation of this preliminary finding is needed in further studies.
Our analyses support our second hypothesis that improvements of social communication behaviors predict a significant proportion of variance in maternal child-related stress when stress scores pre-intervention, gains in (everyday life) adaptive skills and a reduction in behavioral problems are considered. Improvements in social communication behaviors even turned out to be the strongest single predictor of maternal child-related stress. Our results corroborate previous findings of associations between social communication skills of children with ASD and parental stress (20, 27).
Contrary to our expectation (hypothesis 3a), significant gains in verbal skills failed to show a significant relationship with maternal stress. Changes in non-verbal cognition and adaptive skills (VABS Daily Living scores with very high standard deviations) during the intervention period were neither statistically significant nor did they correlate with maternal stress outcomes, and hypotheses (3b) and (3c) were thus not confirmed. However, reduced irritability (unlike stereotypy and hyperactivity) showed a significant relationship with maternal stress and contributed significantly to explaining variance in our model which included maternal stress pre-intervention and development of social communication behaviors.
Even though language delays have been reported to be a major concern of parents of children with ASD and a primary reason for seeking support (19), our data suggest that social communication behaviors (including appropriate everyday use of language or non-verbal means of communication) rather than verbal knowledge per se contributes to maternal stress. While other studies showed child adaptive behavior levels to be significantly related to maternal stress (24, 62), we did not find that improvements in everyday living skills as measured by the VABS contributed to the prediction of maternal stress. Since an individual's reduced ability to take care of themself is expected to cause distress in a caregiver, deviations in our results might be due to the lack of significant changes within the intervention period, which might in turn be related to the measure's sensitivity to change.
In line with hypothesis (3d), a reduction in irritative challenging behavior was negatively related to maternal stress and was a highly significant predictor in our final model, increasing the extent of explained variance in addition to the effects of development of social communication behaviors. Specific correlations between child aberrant behaviors and parental stress have also been reported by other studies (10, 17).
We did not find any predictive values of child-related maternal stress outcome among the socio-demographic variables, which seems surprising. Possibly because our group of children was very young and age-homogeneous, we did not find a correlation between age and maternal stress; similar findings have also been reported by others (63). As mentioned above, our group of families showed great heterogeneity in their cultural, educational and language backgrounds, which is probably the reason for not finding any correlations between multilingualism or maternal education and maternal stress outcome.
Unlike for child-related maternal stress outcome, we did not find significant predictors of parent-related maternal stress outcome, except the intervention start value of this dimension. No family or child developmental scores were predictive of parental stress outcome at T2.
Limitations
The findings of this study must be interpreted with caution, considering several limitations. First, the lack of a control group makes it impossible to determine if the reported changes reflect treatment effects. Other explanations (e.g., maturation) cannot be ruled out. Secondly, because of our clinic's standard procedure, families were seen by the same clinicians at follow up, which made blinding of the assessments impossible. Third, our parental rating scales were completed only by mothers. Although mothers are usually the primary caregivers, this makes it impossible to generalize our findings to fathers, who have also been reported as crucial to child development (64). Moreover, our maternal stress and social communication variables were based on maternal self-reported questionnaires. Fourth, there are concerns in relation to the PSI norms: As reported above, at both time points the PSI led to considerable ceiling effects, as reported by others (61, 65, 66), especially for the child domain. Concerns using the PSI-SF in studies with young children with ASD were also raised by Zaidman-Zait et al. (67). Fifth, one strength of this study—the use of a community sample—led to large heterogeneity in terms of family language and culture, with almost three quarters of the families being multilingual; this may have influenced the accuracy in answering the questionnaires, although assistance was offered whenever needed.
Conclusion and Future Directions
Our findings indicate that improvements in social communication behaviors, for instance, improved social approach behaviors, showing positive affect behaviors, interconnecting in social plays, or imitating social cues, directly affect maternal child-related stress. This influence was ahead of all other measured dimensions of child development (e.g., challenging behaviors, adaptive skills or verbal skills as directly assessed by standardized instruments and non-verbal cognition). Parents who perceive a lack of, or stagnation in, social functioning in their children with ASD often experience a weakening or loss of “relationship/connection” with their child, which can lead to anxiety, confusion and worries in everyday situations and a loss of parental self-efficacy, including perceived competence and self-confidence. Our results underline the importance of addressing social communication in early intervention programs, such as the ESDM (35) or PACT (30), as changes in child social communication appear to be beneficial to maternal well-being.
Finally, the inclusion of valid parental rating measures of social functioning in everyday life situations, such as the PDDBI, and measures of parental stress during intervention appear to be important for two reasons: First, more longitudinal data is needed to explore the reciprocal mechanisms that link the enhancement of social behaviors in young children with ASD and maternal (parental) stress or mental health levels. Secondly, early intervention programs target primarily children's skills, but often neglect professional support or intervention procedures for parents, as also highlighted by others (68, 69). A better understanding of the interconnection between children's social development and parental well-being is needed to improve early intervention programs with more sophisticated procedures to meet the needs of parents of children with ASD.
Data Availability Statement
The datasets generated and analyzed for this study are not publicly available due to the lack of confirmation by participating families to share their datasets with other institutions. Requests to access the datasets should be directed to ZG9taW5pay5sYWlzdGVyQGprdS5hdA==.
Ethics Statement
The ethical approval for this evaluation was granted by the Ethics Committee of the Hospital of St. John of God in Linz in April 2014. All participating parents gave their written informed consent for participation in the study and publication of results.
Author Contributions
DL and DH conceived and designed the study. DL performed the analysis and calculations and drafted the manuscript. DH and GV substantially revised the drafts and gave methodological feedback while planning the study. PM and JF supervised the project and gave input to the argumentation line of the study. All authors discussed the results and contributed to the final manuscript.
Funding
Article processing charge was funded by the Johannes Kepler University Open Access Publishing Fund.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors thank all participating parents for their patience in supporting their children and for their time spent filling out forms and questionnaires, and the clinicians and therapists of the Institute of Neurology of Senses at Konventhospital Barmherzige Brüder Linz who assisted with the assessments and data collection.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.797148/full#supplementary-material
References
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: Dsm-5. 5th ed. American Psychiatric Publishing. Washington, DC (2013).
2. Abbeduto L, Seltzer MM, Shattuck P, Krauss MW, Orsmond G, Murphy MM. Psychological well-being and coping in mothers of youths with autism, down syndrome, or fragile X syndrome. Am J Mental Retard. (2004) 109:237. doi: 10.1352/0895-8017(2004)109<237:PWACIM>2.0.CO;2
3. Cohrs AC, Leslie DL. Depression in parents of children diagnosed with autism spectrum disorder: a claims-based analysis. J Autism Dev Disord. (2017) 47:1416–22. doi: 10.1007/s10803-017-3063-y
4. Dabrowska A, Pisula E. Parenting stress and coping styles in mothers and fathers of pre-school children with autism and Down syndrome. J Intellect Disabil Res. (2010) 54:266–80. doi: 10.1111/j.1365-2788.2010.01258.x
5. Griffith GM, Hastings RP, Nash S, Hill C. Using matched groups to explore child behavior problems and maternal well-being in children with Down syndrome and autism. J Autism Dev Disord. (2010) 40:610–9. doi: 10.1007/s10803-009-0906-1
6. Hayes SA, Watson SL. The impact of parenting stress: a meta-analysis of studies comparing the experience of parenting stress in parents of children with and without autism spectrum disorder. J Autism Dev Disord. (2013) 43:629–42. doi: 10.1007/s10803-012-1604-y
7. Davis NO, Carter AS. Parenting stress in mothers and fathers of toddlers with autism spectrum disorders: associations with child characteristics. J Autism Dev Disord. (2008) 38:1278–91. doi: 10.1007/s10803-007-0512-z
8. Hartley SL, Seltzer MM, Head L, Abbeduto L. Psychological well-being in fathers of adolescents and young adults with down syndrome, Fragile X syndrome, and autism. Fam Relat. (2012) 61:327–42. doi: 10.1111/j.1741-3729.2011.00693.x
9. Brookman-Frazee L, Stadnick N, Chlebowski C, Baker-Ericzén M, Ganger W. Characterizing psychiatric comorbidity in children with autism spectrum disorder receiving publicly funded mental health services. Autism Int J Res Pract. (2018) 22:938–52. doi: 10.1177/1362361317712650
10. Estes A, Olson E, Sullivan K, Greenson J, Winter J, Dawson G, et al. Parenting-related stress and psychological distress in mothers of toddlers with autism spectrum disorders. Brain Dev. (2013) 35:133–8. doi: 10.1016/j.braindev.2012.10.004
11. Fiske KE. A Cross-Sectional Study of Patterns of Renewed Stress Among Parents of Children with Autism. New Brunswick, NJ: Rutgers The State University of New Jersey-New Brunswick (2009).
12. Lecavalier L, Leone S, Wiltz J. The impact of behaviour problems on caregiver stress in young people with autism spectrum disorders. J Intellect Disabil Res. (2006) 50:172–83. doi: 10.1111/j.1365-2788.2005.00732.x
13. Bitsika V, Sharpley CF. Stress, anxiety and depression among parents of children with autism spectrum disorder. Aust J Guid Counsell. (2004) 14:151–61. doi: 10.1017/S1037291100002466
14. Frantz R, Hansen SG, Machalicek W. Interventions to promote well-being in parents of children with autism: a systematic review. Rev J Autism Dev Disord. (2018) 5:58–77. doi: 10.1007/s40489-017-0123-3
15. Benson PR. The impact of child symptom severity on depressed mood among parents of children with ASD: the mediating role of stress proliferation. J Autism Dev Disord. (2006) 36:685–95. doi: 10.1007/s10803-006-0112-3
16. Schieve LA, Boulet SL, Kogan MD, Yeargin-Allsopp M, Boyle CA, Visser SN, et al. Parenting aggravation and autism spectrum disorders: 2007 National Survey of Children's Health. Disabil Health J. (2011) 4:143–52. doi: 10.1016/j.dhjo.2010.09.002
17. Brei NG, Schwarz GN, Klein-Tasman BP. Predictors of parenting stress in children referred for an autism spectrum disorder diagnostic evaluation. J Dev Phys Disabil. (2015) 27:617–35. doi: 10.1007/s10882-015-9439-z
18. Ekas NV, Lickenbrock DM, Whitman TL. Optimism, social support, and well-being in mothers of children with autism spectrum disorder. J Autism Dev Disord. (2010) 40:1274–84. doi: 10.1007/s10803-010-0986-y
19. Coonrod EE, Stone WL. Early concerns of parents of children with autistic and nonautistic disorders. Infants Young Child. (2004) 17:258–68. doi: 10.1097/00001163-200407000-00007
20. Marcus LM, Kunce LJ, Schopler E. Working with families. In: Volkmar FR, Paul R, Klin A, Cohen D, editors. Handbook of Autism and Pervasive Developmental Disorders. Hoboken, NJ: Wiley (2005). p. 1055–86.
21. Dominick KC, Davis NO, Lainhart J, Tager-Flusberg H, Folstein S. Atypical behaviors in children with autism and children with a history of language impairment. Res Dev Disabil. (2007) 28:145–62. doi: 10.1016/j.ridd.2006.02.003
22. McGrath PJ, Sourander A, Lingley-Pottie P, Ristkari T, Cunningham C, Huttunen J, et al. Remote population-based intervention for disruptive behavior at age four: Study protocol for a randomized trial of Internet-assisted parent training (Strongest Families Finland-Canada). BMC Public Health. (2013) 13:985. doi: 10.1186/1471-2458-13-985
23. Baker-Ericzén MJ, Brookman-Frazee L, Stahmer A. Stress levels and adaptability in parents of toddlers with and without autism spectrum disorders. Res Pract Pers Sev Disabil. (2005) 30:194–204. doi: 10.2511/rpsd.30.4.194
24. Hall HR, Graff JC. The relationships among adaptive behaviors of children with autism, family support, parenting stress, and coping. Issues Compr Pediatr Nurs. (2011) 34:4–25. doi: 10.3109/01460862.2011.555270
25. Bebko JM, Konstantareas MM, Springer J. Parent and professional evaluations of family stress associated with characteristics of autism. J Autism Dev Disord. (1987) 17:565–76. doi: 10.1007/BF01486971
26. Guralnick MJ. An overview of the developmental systems model for early intervention. Dev Syst Approach Early Interven. (2005) 1:3–28.
27. Ozturk Y, Vivanti G, Uljarevic M, Dissanayake C, Victorian ASELCC Team. Treatment-related changes in children's communication impact on maternal satisfaction and psychological distress. Res Dev Disabil. (2016) 56:128–38. doi: 10.1016/j.ridd.2016.05.021
28. Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the depression anxiety stress scales (DASS) with the beck depression and anxiety inventories. Behav Res Ther. (1995) 33:335–43. doi: 10.1016/0005-7967(94)00075-U
29. Bailey G. Emotional Well-Being for Children With Special Educational Needs and Disabilities: A Guide for Practitioners. Thousand Oaks, CA: Sage (2012).
30. Pickles A, Le Couteur A, Leadbitter K, Salomone E, Cole-Fletcher R, Tobin H, et al. Parent-mediated social communication therapy for young children with autism (PACT): long-term follow-up of a randomised controlled trial. Lancet. (2016) 388:2501–9. doi: 10.1016/S0140-6736(16)31229-6
31. Holzinger D, Laister D, Vivanti G, Barbaresi WJ, Fellinger J. Feasibility and outcomes of the early start denver model implemented with low intensity in a community setting in Austria. J Dev Behav Pediatr. (2019) 40:354–63. doi: 10.1097/DBP.0000000000000675
32. Dawson G, Toth K, Abbott R, Osterling J, Munson J, Estes A, et al. Early social attention impairments in autism: social orienting, joint attention, and attention to distress. Dev Psychol. (2004) 40:271–83. doi: 10.1037/0012-1649.40.2.271
33. Dawson G, Rogers S, Munson J, Smith M, Winter J, Greenson J, et al. Randomized, controlled trial of an intervention for toddlers with autism: the early start denver model. Pediatrics. (2010) 125:e17–23. doi: 10.1542/peds.2009-0958
34. Fein D, Barton M, Eigsti I-M, Kelley E, Naigles L, Schultz RT, et al. Optimal outcome in individuals with a history of autism. J Child Psychol Psychiatry Allied Discip. (2013) 54:195–205. doi: 10.1111/jcpp.12037
35. Rogers SJ, Dawson G. Early Start Denver Model for Young Children with Autism: Promoting Language, Learning, and Engagement. New York, NY: Guilford (2010).
36. Rogers SJ, Pennington BF. A theoretical approach to the deficits in infantile autism. Dev Psychopathol. (1991) 3:137–62. doi: 10.1017/S0954579400000043
37. Vivanti G, Stahmer AC. Can the early start denver model be considered ABA practice? Behav Anal Pract. (2021) 14:230–9. doi: 10.1007/s40617-020-00474-3
38. Fuller EA, Oliver K, Vejnoska SF, Rogers SJ. The effects of the early start denver model for children with autism spectrum disorder: a meta-analysis. Brain Sci. (2020) 10:368. doi: 10.3390/brainsci10060368
39. Rogers SJ, Vivanti G, Rocha M. Helping young children with autism spectrum disorder develop social ability: the early start denver model approach. In: Handbook of Social Skills and Autism Spectrum Disorder. Berlin: Springer (2017). p. 197–222.
40. Abidin RR. Parenting Stress Index-Short Form. Charlottesville, VA: Pediatric Psychology Press (1990).
41. Tröster H. EBI: Eltern-Belastungs-Inventar: deutsche Version des Parenting Stress Index (PSI) von RR Abidin. Gottingen: Hogrefe (2011).
42. Abidin RR. Parenting Stress Index. 3rd ed. Odessa, FL: Psychological Assessment Resources (1995).
43. Almutairi M. Mothers of Children with Autism: The Relationship Between Knowledge of Autism and Stress. Stockton, CA: University of the Pacific (2002).
44. Hudock RL. Examining Parenting Stress in Parents of Children With Autism Spectrum Disorders. EndNote Tagged Import Format. Bloomington, IN: Indiana University (2012).
45. McLennan JD, Doig J, Rasmussen C, Hutcheon E, Urichuk L. Stress and relief: parents attending a respite program. J Can Acad Child Adolesc Psychiatry. (2012) 21:261.
46. Cohen IL, Sudhalter V. PDD Behavior Inventory (PDDBI). Lutz, FL: Psychological Assessment Resources (2005).
47. Schopler E, Reichler RJ, DeVellis RF, Daly K. Toward objective classification of childhood autism: childhood autism rating scale (CARS). J Autism Dev Disord. (1980) 10:91–103. doi: 10.1007/BF02408436
48. Sparrow SS, Balla DA, Cicchetti DV, Harrison PL. Vineland Adaptive Behavior Scales. Circle Pines, MN: American Guidance Service (1984).
49. Griffiths R. The abilities of young Children: A Comprehensive System of Mental Measurement for the First Eight Years of Life. Bucks: Association for Research in Infant and Child Development (1984).
50. Aman MG, Singh NN, Stewart AW, Field CJ. The aberrant behavior checklist: a behavior rating scale for the assessment of treatment effects. Am J Mental Defic. (1985) 89:485–91. doi: 10.1037/t10453-000
51. Kaat AJ, Lecavalier L, Aman MG. Validity of the aberrant behavior checklist in children with autism spectrum disorder. J Autism Dev Disord. (2014) 44:1103–16. doi: 10.1007/s10803-013-1970-0
52. Aman MG, McDougle CJ, Scahill L, Handen B, Arnold LE, Johnson C, et al. Medication and parent training in children with pervasive developmental disorders and serious behavior problems: results from a randomized clinical trial. J Am Acad Child Adolesc Psychiatry. (2009) 48:1143–54. doi: 10.1097/CHI.0b013e3181bfd669
53. Aman MG. Aberrant behavior checklist: current identity and future developments. Clin Exp Pharmacol. (2012) 2:e114. doi: 10.4172/2161-1459.1000e114
55. Rogers SJ, Estes A, Lord C, Vismara L, Winter J, Fitzpatrick A, et al. Effects of a brief Early Start Denver model (ESDM)-based parent intervention on toddlers at risk for autism spectrum disorders: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry. (2012) 51:1052–65. doi: 10.1016/j.jaac.2012.08.003
56. Sparrow SS, Balla DA, Cicchetti DV. Vineland Adaptive Behavior Scales–Second Edition (Vineland–II). Circle Pines, MN: American Guidance Service (2005).
57. Di Rezze B, Duku E, Szatmari P, Volden J, Georgiades S, Zwaigenbaum L, et al. Examining trajectories of daily living skills over the preschool years for children with autism spectrum disorder. J Autism Dev Disord. (2019) 49:4390–9. doi: 10.1007/s10803-019-04150-6
58. Lord C, Rutter M, DiLavore P, Risi S, Gotham K, Bishop S. Autism Diagnostic Observation Schedule−2nd Edition (ADOS-2). Los Angeles, CA: Western Psychological Corporation (2012). p. 284.
59. Laister D, Stammler M, Vivanti G, Holzinger D. Social-communicative gestures at baseline predict verbal and nonverbal gains for children with autism receiving the Early Start Denver Model. Autism Int J Res Pract. (2021) 25:1640–652. doi: 10.1177/1362361321999905
60. Anastopoulos AD, Guevremont DC, Shelton TL, DuPaul GJ. Parenting stress among families of children with attention deficit hyperactivity disorder. J Abnorm Child Psychol. (1992) 20:503–20. doi: 10.1007/BF00916812
61. Giovagnoli G, Postorino V, Fatta LM, Sanges V, Peppo L, de Vassena L, et al. Behavioral and emotional profile and parental stress in preschool children with autism spectrum disorder. Res Dev Disabil. (2015) 45–46:411–21. doi: 10.1016/j.ridd.2015.08.006
62. Tomanik S, Harris GE, Hawkins J. The relationship between behaviours exhibited by children with autism and maternal stress. J Intellect Dev Disabil. (2004) 29:16–26. doi: 10.1080/13668250410001662892
63. Rivard M, Terroux A, Parent-Boursier C, Mercier C. Determinants of stress in parents of children with autism spectrum disorders. J Autism Dev Disord. (2014) 44:1609–20. doi: 10.1007/s10803-013-2028-z
64. McStay RL, Dissanayake C, Scheeren A, Koot HM, Begeer S. Parenting stress and autism: the role of age, autism severity, quality of life and problem behaviour of children and adolescents with autism. Autism Int J Res Pract. (2014) 18:502–10. doi: 10.1177/1362361313485163
65. Richman DM, Belmont JM, Kim M, Slavin CB, Hayner AK. Parenting stress in families of children with cornelia de lange syndrome and down syndrome. J Dev Phys Disabil. (2009) 21:537–53. doi: 10.1007/s10882-009-9156-6
66. Rivas GR, Arruabarrena I, de Paúl J. Parenting stress index-short form: psychometric properties of the Spanish version in mothers of children aged 0 to 8 years. Psychosocial Interven. (2021) 30:27–34. doi: 10.5093/pi2020a14
67. Zaidman-Zait A, Mirenda P, Zumbo BD, Wellington S, Dua V, Kalynchuk K. An item response theory analysis of the parenting stress index-short form with parents of children with autism spectrum disorders. J Child Psychol Psychiatry. (2010) 51:1269–77. doi: 10.1111/j.1469-7610.2010.02266.x
68. Miranda A, Mira A, Berenguer C, Rosello B, Baixauli I. Parenting stress in mothers of children with autism without intellectual disability. Mediation of behavioral problems and coping strategies. Front Psychol. (2019) 10:464. doi: 10.3389/fpsyg.2019.00464
Keywords: autism spectrum disorder, social communication behaviors, maternal stress, early childhood, Early Start Denver Model, intervention outcomes
Citation: Laister D, Vivanti G, Marschik PB, Fellinger J and Holzinger D (2021) Enhancement of Social Communication Behaviors in Young Children With Autism Affects Maternal Stress. Front. Psychiatry 12:797148. doi: 10.3389/fpsyt.2021.797148
Received: 18 October 2021; Accepted: 11 November 2021;
Published: 07 December 2021.
Edited by:
Sara Calderoni, Fondazione Stella Maris (IRCCS), ItalyReviewed by:
Encarnacion Sarria, National University of Distance Education (UNED), SpainFernanda Dreux M. Fernandes, University of São Paulo, Brazil
Copyright © 2021 Laister, Vivanti, Marschik, Fellinger and Holzinger. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dominik Laister, ZG9taW5pay5sYWlzdGVyQGprdS5hdA==
 Dominik Laister
Dominik Laister Giacomo Vivanti
Giacomo Vivanti Peter B. Marschik
Peter B. Marschik Johannes Fellinger
Johannes Fellinger Daniel Holzinger
Daniel Holzinger