- 1Department of Psychiatry, Faculty of Medicine, Universiti Teknologi MARA, Sungai Buloh, Malaysia
- 2Department of Public Health Medicine, Faculty of Medicine, Universiti Teknologi MARA, Shah Alam, Malaysia
Background: Medical students are not spared from the challenges related to the Covid-19 lockdown. The fear and uncertainties may lead to traumatic symptoms and test their resilience and sense of coping. Thus, this study aims to determine the prevalence of peri-traumatic distress symptoms and its association with the level of resilience and the coping strategies used during the lockdown among medical students.
Materials and Methods: This was a cross-sectional online questionnaire survey involving medical students from a public university in Malaysia. It was conducted during the COVID-19 lockdown or Movement Control Order (MCO) where the students were asked to fill in the COVID-19 Peri-traumatic Distress Index (CPDI), Brief COPE Inventory, and Connor Davidson Resilience Scale (CDRS-25).
Results: A total of 282 clinical and 172 pre-clinical medical students were involved. Peri-traumatic distress symptoms were reported by 27% out of the total students. This study found that those who were having peritraumatic distress symptoms were from the pre-clinical years, had poor internet access, as well as lower resilience levels, and used more dysfunctional coping strategies. Pre-clinical medical students with difficult internet access were eight times more likely to have peritraumatic distress symptoms.
Conclusions: Given the high level of peri-traumatic distress symptoms reported by medical students during the lockdown, it is vital to identify the vulnerable students, assess their needs and risks to mental health problems during this challenging time as the pandemic is still ongoing with countries going in and out of lockdown depending on the cases at the time. The university administration for each University in Malaysia will need to have a clear academic guideline and policy as well as providing improved infrastructure to minimize the distress faced by medical students.
Introduction
The COVID-19 pandemic posed unique challenges to everyone in the world. It affects the country and the community in various aspects such as its economy, putting increasing strains on resources, particularly the healthcare system, and renders other areas such as the educational system to a halt. COVID-19 is a global pandemic that challenges an individual's mental health, coping abilities, and resilience. During a pandemic, the individual's resilience might be tested, and it may cause various psychological distress reactions, risky behaviors, and even psychiatric disorders (1). The COVID-19 lockdown has been shown to have an adverse effect on people in the community. A study comparing the mental wellbeing of people in lockdown in Asia, Africa, and European countries showed that it had a negative effect on both mental wellbeing and mood, particularly depressive symptoms during the lockdown as compared to before the lockdown (2). Banerjee et al. (3) in a systematic review on the psychological impact of lockdown in the South-Asian population, reported an increase in depression, anxiety, somatic concerns, alcohol-related disorders, and insomnia.
In Malaysia, the COVID-19 lockdown or Movement Control Order (MCO) started from the middle of March 2020 until the middle of May 2020. All education centers were closed immediately and for students, regardless of whether they are in primary, secondary, or tertiary education level, being at home due to the movement control order created many challenges to the students and families as well. The university students were instructed to return home immediately upon announcement of the MCO by the Malaysian Government and online classes were commenced. The abrupt change learning method coupled with the COVID-19 related fear and lockdown created many challenges for undergraduate students. COVID-19 specific worries, isolation in social networks, lack of interaction and emotional support, and physical isolation were associated with poorer mental health in students (4). Students reported academic and everyday difficulties with high levels of mental health distress where levels of depression and anxiety were higher during the lockdown and these were associated with the inability to focus on studies and loss of employment (4–6).
Medical students were not spared from such challenges. Peri-traumatic distress is emotional and physiological distress experienced during and/or immediately after a traumatic event and is associated with the development and severity of posttraumatic stress disorder (PTSD) and related psychological difficulties. Medical students' perception and definition of risk and danger to themselves and/or to their families may have changed during this pandemic. These coupled with the fear and uncertainties may lead to traumatic symptoms and cause challenges to their usual coping abilities and resilience. Their concerns of continuing medical studies, the lack of routine and schedules, loss of social connections, and being in isolation put them at risk of developing further psychological distress such as depression and anxiety (7–9). The pandemic may give rise to peri-traumatic distress to medical students and lockdown as a traumatic experience has not been explored in medical students. As these peri-traumatic distress symptoms may be a precursor to depression and anxiety, the University's mental health services need to be aware of these issues and plan for prevention, active screening, and intervention to the medical students who are currently struggling.
Resilience and having good coping strategies are important in mitigating the stressful impact and peri-traumatic distress of lockdown. Globally, studies have shown that university students have employed several coping strategies during the lockdown which included seeking social support, avoidance through technology and playing video games, cognitive strategies, and religion (10–14). Resilience is seen as the ability to have psychological flexibility and the emotional capability to deal and adapt to difficult or traumatic life challenges whilst maintaining a meaningful quality of life. The ability to recover from an adverse event is also determined by a person's resilience (15). A study done on young adults between 18–25 years old found that the relationship between stress, coping and resilience during the pandemic lockdown was complicated (16). A good level of resilience seemed to protect against developing some mental disorders but not with others. Having a high resilience level among university students was associated with lower rates of depression and anxiety during the pandemic but not protective against post-traumatic distress disorder (17). However, another study done on the role of psychological flexibility and inflexibility during the pandemic lockdown fond that having psychological flexibility protects against peri-traumatic distress, depression and anxiety (18). To the authors knowledge, there has been no studies that investigated the association between peri-traumatic distress with coping and resilience among medical students or other faculties done to date.
Therefore, this study aimed to ascertain the prevalence of peri-traumatic distress symptoms among medical students and its association with the level of resilience of medical students and the coping strategies used during the lockdown in Malaysia.
Materials and Methods
This study was a cross-sectional online questionnaire survey involving medical students from a public university in Malaysia. It was conducted during the COVID-19 lockdown or Movement Control Order (MCO) in Malaysia which started from the middle of March 2020 until the middle of May 2020.
Participants and Study Procedure
The questionnaires were sent to all 1125 medical students from Year 1 and Year 2 (pre-clinical) and Year 3 to 5 (clinical) via Whatsapp software. The design of the survey allows us to take consent before the respondent can fill in the questionnaires. The questionnaires were comprised of sociodemographic and MCO-related details, COVID-19 Peri-traumatic Distress Index (CPDI), Brief COPE Inventory, and Connor Davidson Resilience Scale (CDRS-25).
Those who scored positive as having distress will be contacted for further assessment once consented. A minimum of 350 respondents was needed and at the end of the study, 454 medical students responded. The students received a cover letter prior to the answering the questionnaires reassuring them about anonymity, confidentiality, and that published results were solely for scientific purpose. Ethical approval was obtained from the University's Research Ethics Committee REC/07/2020 (MR/167).
Measures
COVID-19 Peri-Traumatic Distress Index (CPDI)
It was adapted from The Peri-traumatic Distress Scale (PDI) that was used to assess emotional, cognitive, and physical reactions occurring during a critical incident and immediately after. The COVID-19 Peri-traumatic Distress Index (CPDI) (19) assesses the frequency of anxiety, depression, specific phobias, cognitive change, avoidance, and compulsive behavior, physical symptoms, and loss of social functioning in the past week, ranging from 0 to 100. A score between 28 and 51 indicates mild to moderate distress. A score of 52 and above indicates severe distress. The Cronbach's alpha of CPDI was 0.95 (p < 0.001). The total raw score should be increased by 4 to make it 100 (Display score). The displayed score will be further categorized into Normal: 0–28, Mild: 29–52, Severe: 53–100 psychological distress.
Brief COPE Inventory
It was created by Carver (20) and was an abbreviated version of the full COPE Inventory. This questionnaire aims to assess the type of coping behavior using 14 coping strategies. Two items in the list represent these coping strategies: self-distraction, active coping, denial, substance abuse, emotional support, instrumental support, behavioral disengagement, venting, positive reframing, planning, humor, acceptance of religion, and self-blame. Each item was accompanied by a 4 point Likert scale with a score of 0 as 'I haven't been doing this at all', a score of 1 as 'I've been doing this a little bit', a score of 2 as 'I've been doing this a medium amount' and a score of 3 as 'I've been doing this a lot'. Items that scored a value of ≤ 1 were converted to a value of 0 to signify that the particular coping strategy was not performed at all, whereas items that scored a value of ≥2 were converted to a value of 1 to signify otherwise. The total score for a particular coping method was accumulated together and interpreted as follows: a score of 0 signified that the students did not perform the coping method at all, a score of 1 signified that the student had performed at least one out of two of the particular coping method and a score of 2 signified that the students had performed both of the coping methods. This questionnaire has been commonly used to determine the common coping behaviors in several studies involving medical students (21, 22).
Connor Davidson Resilience Scale (CDRS-25)
It was originally developed as a self-report measure of resilience and (23). CDRS−25 has been validated for the Malaysian population and widely used resilience scale where the 25-item scale has the total possible scores range from 0–100. It measures several components of resilience: the ability to adapt to change, the ability to deal with what comes along, the ability to cope with stress, the ability to stay focused and think clearly, the ability to not get discouraged in the face of failure, the ability to handle unpleasant feelings such as anger, pain or sadness. The higher the score, the higher the resilience level.
Statistical Analysis
All the responses will be collected in a spreadsheet and transferred to IBM SPSS version 25.
CPDI: Mean (SD) scores for total and each category will be calculated.
Brief COPE: The association between the category of sociodemographic factors and severity of psychological stress will be analyzed by chi-square test. Multinomial logistic regression analysis will be performed to determine the sociodemographic factors associated with psychological distress.
CDRS-25: The total possible scores range from 0–100. The higher the score, the higher the resilience level. The cut-off point is determined from the mean.
Results
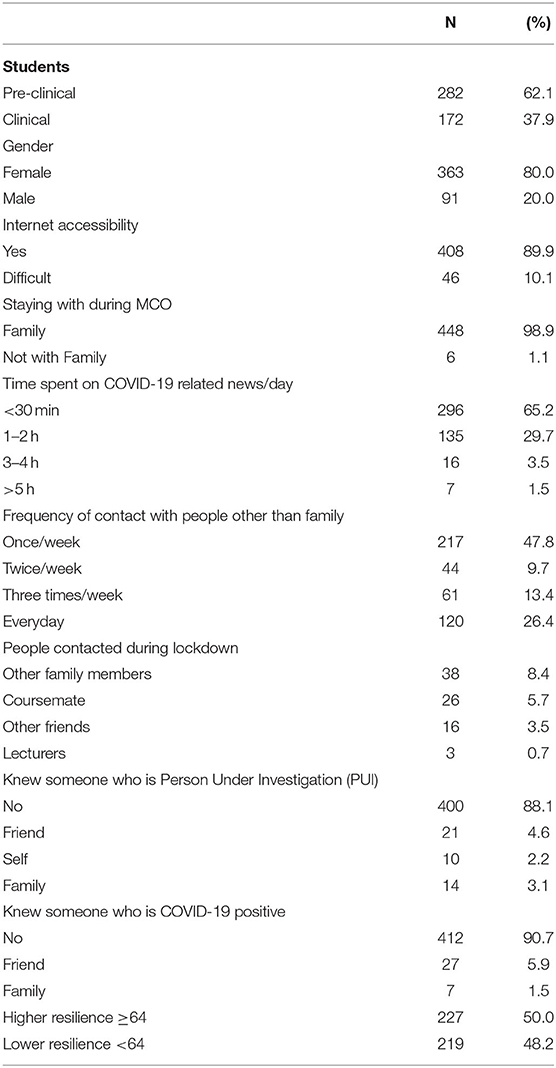
A total of 454 medical students responded to the questionnaires of which 62.1 and 37.9% were pre-clinical and clinical, respectively. Table 1 shows the medical students' profiles and COVID-19 related data.
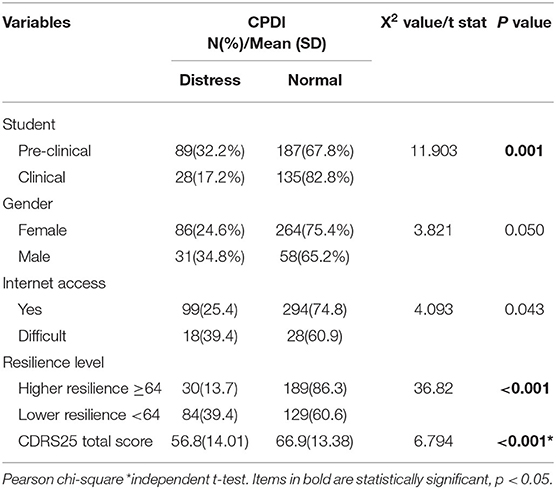
Among the 454 who responded, 439 students completed the CPDI scale. The prevalence of peri-traumatic distress among the medical undergraduates was 27% (N = 439). Table 2 showed that a significantly higher proportion of distress was found among the pre-clinical students, and in terms of sociodemographic and COVID-19 related variables, female students were more distressed as compared to their male counterparts. All other variables were not statistically significant.
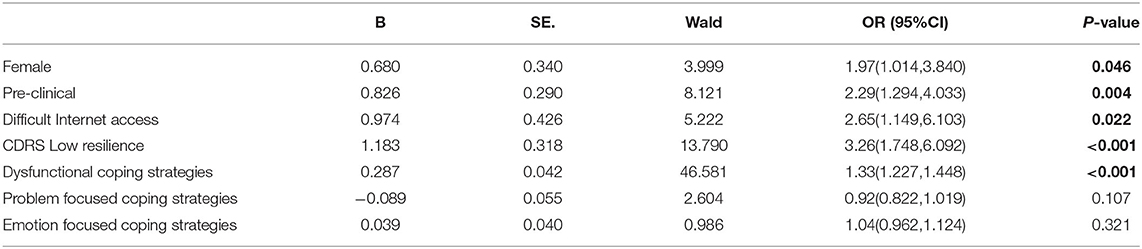
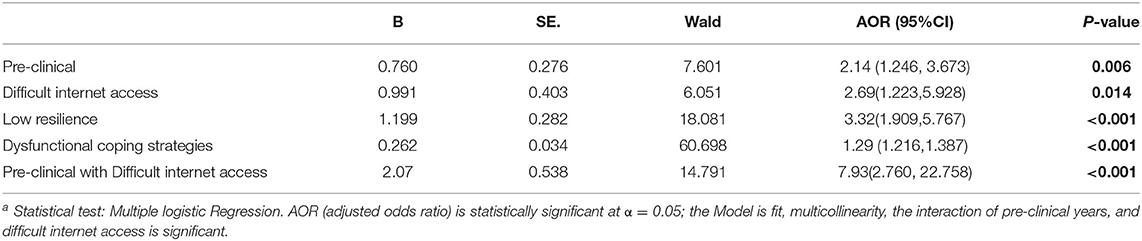
Out of seven variables included in simple logistic regression, there were four variables significantly associated with peri-traumatic distress (Table 3). All the five significant variables (pre-clinical, female, difficult internet access, low resilience, dysfunctional coping strategies) from simple logistic regression were then included in multiple logistic regression. However, in multiple logistic regression, female gender was not significantly associated (Table 4). Those in pre-clinical years were 2.14 times more likely to have peri-traumatic distress as compared to those in clinical years. Those who have difficulty with internet access were 2.69 times more likely to be distressed as compared to those who do not have difficulty with internet access. Medical students with lower resilience levels were 3.32 times more likely to have peri-traumatic distress symptoms as compared to those with higher resilience. This study also found that students who used dysfunctional coping strategies were 1.29 times more likely to have peritraumatic distress symptoms. Pre-clinical medical students with difficult internet access were 7.93 times more likely to have peritraumatic distress during the lockdown.
Discussion
The purpose of this study was to assess the prevalence of peri-traumatic distress symptoms among medical students and its association to the level of resilience and coping strategies used during the COVID-19 lockdown period. The COVID-19 Peri-traumatic Distress Index (CPDI) measures the frequency of anxiety, depression, specific phobias, cognitive change, avoidance, and compulsive behavior, physical symptoms, and loss of social functioning in the past week.
From this study, the prevalence of peri-traumatic distress symptoms among medical students during Covid-19 lockdown as measured using CPDI was found to be 26.7%. This is higher than the finding reported by (24) where the study found 13.2% of their participants had PTSD-positive symptoms as measured by Posttraumatic Stress Disorder Checklist-5, adapted to measure pre/peri/posttraumatic reactions in relation to COVID-19. In studies looking for psychological distress among university students, the finding is lower compared to the prevalence of anxiety in a study conducted among 16 university students which found that 56 % of students suffered from anxiety (25). However, the prevalence is higher than the prevalence in a study conducted by Sundarasen et al. (26) which found only 8% of students suffered from anxiety in the current COVID-19 situation. A cross-sectional web-based study conducted among university students across Bangladesh reported that 15% had moderately severe depression, whereas 18.1% were suffering from severe anxiety during the COVID-19 pandemic (6). However, this study used different tools to assess psychological distress, the Patient Health Questionnaire (PHQ-9) and Generalized Anxiety Disorder (GAD-7) questionnaires for the assessment of depression and anxiety, respectively. In a different study, Swiss undergraduate students under lockdown experienced worsening of stress, anxiety, loneliness, and depressive symptoms compared to before the period (4). The unprecedented nature of the COVID-19 Movement Control Order (MCO) in Malaysia has disrupted the daily routines and affected the psychological wellbeing of medical students in various aspects. Standard Operating Procedures (SOPs) or restrictions imposed during the MCO have negatively affected the freedom and autonomy in making simple daily decisions like leaving the house or getting together with friends. Young adults were struggling to cope with feelings of loneliness and isolation as a result of physical distancing from family and friends due to the lockdown. Sense of being unproductive, helplessness, and a loss of a sense of purpose were also experienced in this group. They also reported feelings of anxiety, sadness, and agitation (27).
A significantly higher proportion of pre-clinical students (32.2%) experienced peri-traumatic distress symptoms compared to their clinical year counterparts (17.2%) during the MCO period. This is comparable to the findings from a previous study conducted in Lebanon (62%) which found a high level of stress among pre-clinical students (28). Academic factors that have been identified to be related to stress among medical students are academic demands, medical syllabus, exams, excessive workload, and the learning environment. Whereas individual factors that contributed to stress among these groups of students are the inability to cope, feelings of helplessness, increased emotional pressure and mental tension, and personal life events (29). During the COVID-19 pandemic, these students had to adapt to new changes in curricular delivery which mainly focused on online distance learning (ODL). Furthermore, the Year 1 students did not have any face-to-face contact with their educators and friends upon enrolment to the medical program to familiarize themselves with the new learning and teaching environment. This posed some challenges to establish an adequate support system within the program itself.
In this study, there is an association between difficult internet access and peritraumatic distress among medical students, and this association was almost eight times more likely in those in the pre-clinical years. This is consistent with a study done in Bangladesh in which students were very much affected psychologically due to poor and limited internet access (30). Since COVID-19 started last year, like any other part of the world, the University took an active initiative to adapt its teaching and learning online. Various factors posed challenges to online learning, such as the quality of virtual content, updates on technology, technical assistance, and interaction with other course mates (31). The students depend on the availability and efficiency of the internet at home, and unfortunately, not all areas in Malaysia have good internet coverage. In addition that, the students possibly could not afford a better internet connection due to the monthly charges. This had caused the students to face difficulties in participating in online classes and discussions. Assessments and exams were also conducted online. Due to this, they might be in distress thinking if they had optimum training or if anything would go faulty during their exams if the internet connection is difficult. Due to restricted movement during the lockdown, most students resort to virtual social interaction through social media or online activities such as gaming. A study by Alkan and Meinck (32) showed the importance of information technology in social communication in daily life, which is more relevant in the current pandemic situation. Therefore, the limitation of the internet connection could hinder this process which can cause psychological distress in these students.
Dysfunctional coping skills were significantly associated with peri-traumatic distress in this study whereby the students who employed this type of coping skills were more likely to become distressed. This concurs with the findings from previous studies that having dysfunctional coping skills not only will cause distress but also causes inefficiency to tackle the source of the stress, unlike those who use emotion-focused or problem-focused coping skills (33, 34). In the current COVID-19 pandemic, avoidant coping behavior which is part of dysfunctional coping skills was positively associated with distress and detrimental to psychological wellbeing (35). It is likely that the medical students who were distressed did not have better coping skills in dealing with their daily circumstances and stress. Likely the medical students adopt the dysfunctional coping styles because of their lack of experience as most of them are still early in their training to be doctors and have not developed the maturity to process their emotions and behavior to cope better. The lack of proper training of healthy coping skills in the formal curriculum in Medicine too can serve as the contributing factor of them lacking the appropriate skills. To the authors' knowledge, there is also no specific course incorporated in the curriculum of local medical schools, or in fact, medical schools in other Asian countries, that promotes self-health and wellness, although these skills are vital to cultivate the behavior that ensures the resilience throughout their lifetime career. Such curriculum had been introduced in most medical schools in the United States (36). During this pandemic, psychological flexibility has been associated with better coping and resilience level. It has been found to lower the risk of peri-traumatic distress, depression and anxiety (18).
Medical students who are more resilient have lower odds of experiencing peri-traumatic distress symptoms. This finding is similar to previous studies conducted among university students which concluded that resilience is vital in experiencing less psychological distress as it is a stable trait and negatively correlates with distress (37, 38). Hence it is important for educators to help in building and strengthening resilience among medical students to face the challenges and uncertainties posed by the COVID-19 pandemic. Resilience can be built or enhanced by the four main principles of being in control (being in control and calm when faced with difficulties), being involved (dedicated to deal with difficulties), being resourceful (capacity to find alternatives to deal with difficulties), and being “growth”-centric (ability to keep growing and bounce back better when faced with difficulties) (39).
Strengths and Limitations
To the knowledge of the authors, this is the first study being conducted assessing peri-traumatic distress among medical students in Malaysia during the COVID-19 lockdown. It was conducted in a timely manner. However, this study poses a few limitations. Firstly, this is a cross-sectional study. Therefore, only factors associated with peri-traumatic distress can be assessed instead of the causal linkage. Secondly, the universal (non-probability) sampling method that had been used can lead to bias that will affect the accuracy of the result. Thirdly, participants in this study were limited to the involvement of medical students in one public University in Malaysia. It did not represent the whole population of tertiary education in Malaysia. In this study, the evaluation was done using self-reported questionnaires. Some forms of biases that could happen were recall bias, respond-bias, honesty, and the medical students' understanding of the questionnaires.
Lastly, the questionnaire served as a screening tool for peri-traumatic distress among medical students. It was not diagnostic in nature. In the future study, diagnostic tools can be used so that mental illness among the medical students can be detected, and referral or intervention can be offered.
Conclusions
In order to face the many challenges and the dynamic changes posed by this pandemic, medical students need to develop healthy coping skills and improve their resilience in order to bounce back stronger to continue on with their medical training. It is essential for the university administration to identify the vulnerable students, assess their needs and risks to mental health problems during this challenging time. One of the ways is for the University or faculty to provide good psychological support for their students, for example, by providing a hotline which the students can contact anytime they need to. Coping skills and resilience training, and psychological support groups for those in need can also be provided virtually so that students can utilize them wherever they are. Improving the infrastructure, such as better internet services on the campus, would be beneficial. The importance of constant and effective communication between the University and the students with clear guidelines and policies should not be undermined as it is empirical in alleviating the distressing effect of COVID-19.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by UiTM Research Ethics Committee REC/07/2020 (MR/167). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work, and approved it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ursano RJ, Fullerton CS, Weisaeth L, Raphael B. Textbook of Disaster Psychiatry. London, UK: Cambridge University Press. (2017). doi: 10.1017/9781316481424
2. Ammar A, Mueller P, Trabelsi K, Chtourou H, Boukhris O, Masmoudi L, et al. Psychological consequences of COVID-19 home confinement: The ECLB-COVID19 multicenter study. PLoS ONE. (2020) 15:1–13. doi: 10.1371/journal.pone.0240204
3. Banerjee D, Vaishnav M, Rao TS, Raju M, Dalal PK, Javed A, et al. Impact of the COVID-19 pandemic on psychosocial health and well-being in South-Asian (World Psychiatric Association zone 16) countries: a systematic and advocacy review from the Indian Psychiatric Society. Indian J Psychiatry. (2020) 62:S343–53. doi: 10.4103/psychiatry.IndianJPsychiatry_1002_20
4. Elmer T, Mepham K, Stadtfeld C. Students under lockdown: Comparisons of students' social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS ONE. (2020) 15:e0236337. doi: 10.1371/journal.pone.0236337
5. Kecojevic A, Basch CH, Sullivan M, Davi NK. The impact of the COVID-19 epidemic on mental health of undergraduate students in New Jersey, cross-sectional study. PLoS ONE. (2020) 15:e0239696. doi: 10.1371/journal.pone.0239696
6. Akhtarul Islam M, Barna SD, Raihan H, Nafiul Alam Khan M, Tanvir Hossain M. Depression and anxiety among university students during the COVID-19 pandemic in Bangladesh: a web-based cross-sectional survey. PLoS ONE. (2020) 15:e0238162. doi: 10.1371/journal.pone.0238162
7. Kaleem M, Talha M, Nazir R, Hafeez R. Perception and the associated apprehension stemming from novel COVID-19 among pakistani students. Pakistan Armed Forces Med J. (2020) 70:S237–43. Available online at: https://www.pafmj.org/index.php/PAFMJ/article/view/4882
8. Naser AY, Dahmash EZ, Al-Rousan R, Alwafi H, Alrawashdeh HM, Ghoul I, et al. Mental health status of the general population, healthcare professionals, and university students during 2019 coronavirus disease outbreak in Jordan: a cross-sectional study. Brain Behav. (2020) 10:1–13. doi: 10.1002/brb3.1730
9. Kim SM, Park SG, Jee YK, Song IH. Perception and attitudes of medical students on clinical clerkship in the era of the Coronavirus Disease 2019 pandemic. Med Educ Online. (2020) 25:1809929. doi: 10.1080/10872981.2020.1809929
10. Lechner W V, Laurene KR, Patel S, Anderson M, Grega C, Kenne DR. Changes in alcohol use as a function of psychological distress and social support following COVID-19 related University closings. Addict Behav. (2020) 110:106527. doi: 10.1016/j.addbeh.2020.106527
11. Salman M, Asif N, Mustafa ZU, Khan TM, Shehzadi N, Tahir H, et al. Psychological impairment and coping strategies during the COVID-19 pandemic among students in Pakistan: a cross-sectional analysis. Disaster Med Public Health Prep. (2020) 22:1–7. doi: 10.1017/dmp.2020.397
12. Balhara YPS, Kattula D, Singh S, Chukkali S, Bhargava R. Impact of lockdown following COVID-19 on the gaming behavior of college students. Indian J Public Health. (2020) 64:S172–6. doi: 10.4103/ijph.IJPH_465_20
13. Fernández Cruz M, Álvarez Rodríguez J, Ávalos Ruiz I, Cuevas López M, de Barros Camargo C, Díaz Rosas F, et al. Evaluation of the emotional and cognitive regulation of young people in a lockdown situation due to the Covid-19 pandemic. Front Psychol. (2020) 11:2933. doi: 10.3389/fpsyg.2020.565503
14. Morales-Rodríguez FM, Martínez-Ramón JP, Méndez I, Ruiz-Esteban C. Stress, coping, and resilience before and After COVID-19: a predictive model based on artificial intelligence in the university environment. Front Psychol. (2021) 12:647964. doi: 10.3389/fpsyg.2021.647964
15. Cénat JM, Noorishad PG, Blais-Rochette C, McIntee SE, Mukunzi JN, Darius WP, et al. Together for hope and resilience: a humanistic experience by the vulnerability, trauma, resilience and culture lab members during the COVID-19 pandemic. J Loss Trauma. (2020) 25:643–8. doi: 10.1080/15325024.2020.1774704
16. Marchini S, Zaurino E, Bouziotis J, Brondino N, Delvenne V, Delhaye M. Study of resilience and loneliness in youth (18–25 years old) during the COVID-19 pandemic lockdown measures. J Community Psychol. (2021) 49:468–80. doi: 10.1002/jcop.22473
17. Liu CH, Zhang E, Wong GTF, Hyun S, Hahm H. “Chris.” Factors associated with depression anxiety, and PTSD symptomatology during the COVID-19 pandemic: clinical implications for US young adult mental health. Psychiatry Res. (2020) 290:113172. doi: 10.1016/j.psychres.2020.113172
18. Pakenham KI, Landi G, Boccolini G, Furlani A, Grandi S, Tossani E. The moderating roles of psychological flexibility and inflexibility on the mental health impacts of COVID-19 pandemic and lockdown in Italy. J Context Behav Sci. (2020) 17:109–18. doi: 10.1016/j.jcbs.2020.07.003
19. Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y, et al. nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. General Psychiatry. (2020) 33:e100213. doi: 10.1136/gpsych-2020-100213
20. Carver CS. Brief COPE inventory. Int J Behav Med. (1997) 4:92–100. doi: 10.1207/s15327558ijbm0401_6
21. Al-Dubai SAR, Al-Naggar RA, Alshagga MA, Rampal KG. Stress and coping strategies of students in a medical faculty in Malaysia. Malaysian J Med Sci. (2011) 18:57–64.
22. Johari AB, Hassim IN. Stress and coping strategies among medical students in National University of Malaysia, Malaysia University of Sabah and Universiti Kuala Lumpur Royal College of Medicine Perak. Malaysian J Community Heal. (2009) 15:106–15.
23. Connor KM, Davidson JRT. Development of a new resilience scale: the connor-davidson resilience scale (CD-RISC). Depress Anxiety. (2003) 18:76–82. doi: 10.1002/da.10113
24. Bridgland VME, Moeck EK, Green DM, Swain TL, Nayda DM, Matson LA, et al. Why the COVID-19 pandemic is a traumatic stressor. PLoS ONE. (2021) 16:e0240146. doi: 10.1371/journal.pone.0240146
25. Muhammad I, Shahudin F, Vincent JH, Waqar A, Abdul Ghani R. The Psychological Impact of Coronavirus on University Students and Its Socio- economic Determinants in Malaysia. (2020) p. 0–14. doi: 10.2139/ssrn.3720759
26. Sundarasen S, Chinna K, Kamaludin K, Nurunnabi M, Baloch GM, Khoshaim HB, et al. Psychological Impact of COVID-19 and lockdown among university students in Malaysia : implications and policy recommendations. Int J Encironmental Res Public Heal. (2020) 17:2606. doi: 10.3390/ijerph17176206
27. Dhillon M, Mishra V. Life in lockdown: the psycho-social impacts of the COVID-19 pandemic on young. Indians. (2020) 11:324–30.
28. Fares J, Saadeddin Z, Al H, Aridi H, El C, Karim M, et al. Extracurricular activities associated with stress and burnout in preclinical medical students. J Epidemiol Glob Health. (2016) 6:177–85. doi: 10.1016/j.jegh.2015.10.003
29. Fares J, Tabosh H Al, Saadeddin Z, Mouhayyar C El, Aridi H. Stress, Burnout and Coping Strategies in Preclinical Medical Students. 2016 75–81. doi: 10.4103/1947-2714.177299
30. Hasan N, Bao Y. Impact of “e-learning crack-up” perception on psychological distress among college students during COVID-!(pandemic: a mediating role of “fear of academic year loss” Child Youth. Serv Rev. (2020) 118:105355. doi: 10.1016/j.childyouth.2020.105355
31. Ssekakubo G, Suleman H, Marsden G. Issues of adoption: Have e-learning management systems fulfilled their potential in developing countries? In: Proceedings of the South African Institute of Computer Scientists and Information Technologists conference on knowledge, innovation and leadership in a diverse, multidisciplinary environment. (2011). p. 231–8. doi: 10.1145/2072221.2072248
32. Alkan M, Meinck S. The relationship between students' use of ICT for social communication and their computer and information literacy. Large-Scale Assessments Educ. (2016) 4:1–7. doi: 10.1186/s40536-016-0029-z
33. Cooper C, Katona C, Orrell M, Livingston G. Coping strategies and anxiety in caregivers of people with Alzheimer's disease : the LASER-AD study. J Affect Disord. (2006) 90:15–20. doi: 10.1016/j.jad.2005.08.017
34. Yusoff MSB, Yee LY, Wei LH, Siong TC, Hon L, Bin LX, et al. A study on stress, stressors and coping strategies among malaysian medical students. Int J Students' Res. (2011) 1:45–50. doi: 10.5549/IJSR.1.2.45-50
35. Dawson DL, Golijani-Moghaddam N. COVID-19: psychological flexibility, coping, mental health, and wellbeing in the UK during the pandemic. J Context Behav Sci. (2020) 17:126–34. doi: 10.1016/j.jcbs.2020.07.010
36. Shanafelt T, Dyrbye L. Oncologist burnout: causes, consequences, and responses. J Clin Oncol. (2012) 30:1235–41. doi: 10.1200/JCO.2011.39.7380
37. Antanas K, Rima V, Oddgeir F, Alvydas N. Distress and resilience associated with workload of medical students Antanas Kiziela, Rima Viliuniene, Oddgeir Friborg & Alvydas Navickas. J Ment Heal. (2018) 28:319–23. doi: 10.1080/09638237.2018.1521922
38. Bacchi S, Licinio J. Resilience and psychological distress in psychology and medical students. Acad Psychiatry. (2016) 41:185–8. doi: 10.1007/s40596-016-0488-0
Keywords: medical students, undergraduate, peritraumatic, distress, coping, resilience, COVID-19, lockdown
Citation: Mohamed S, Ismail Z, Shuib N and Ali NF (2021) Peri-Traumatic Distress and Its Relationship to Resilience and Coping Among Medical Students in Malaysia During COVID-19 Lockdown. Front. Psychiatry 12:789554. doi: 10.3389/fpsyt.2021.789554
Received: 05 October 2021; Accepted: 08 November 2021;
Published: 06 December 2021.
Edited by:
Nicholas L. Balderston, University of Pennsylvania, United StatesReviewed by:
Giulia Landi, University of Bologna, ItalyPrateek Varshney, National Institute of Mental Health and Neurosciences (NIMHANS), India
Copyright © 2021 Mohamed, Ismail, Shuib and Ali. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Salina Mohamed, c2FsaW5hMDc1QHVpdG0uZWR1Lm15
 Salina Mohamed
Salina Mohamed Zaliha Ismail
Zaliha Ismail Norley Shuib
Norley Shuib Nur Faizah Ali
Nur Faizah Ali