- Centre for Mental Health and Community Research, Maynooth University, Maynooth, Ireland
Background: Parental mental illness is common, costly, can lead to children developing mental disorders and impaired lifetime outcomes, and places a substantial burden on caregiving partners. Family Talk (FT) is a widely implemented, 7-session, whole-family programme, with promising evidence of effectiveness in targeting the intergenerational transmission of mental illness. However, to date, very little qualitative research of family experiences of FT has been undertaken. The objectives of this study were to: (1) investigate the experiences of families attending FT; and (2) explore the key facilitators and barriers to engagement in mainstream mental health settings.
Methods: This study was nested within a randomised controlled trial (RCT) of Family Talk [N = 86 families (139 parents, 221 children)] implemented in 15 adult, child and primary care mental health sites in Ireland. Semi-structured interviews were conducted with a purposive sample of 45 participants, including 23 parents with mental illness (PMI), 7 partners and 15 children/young people aged 9 to 18 years. Interview data were transcribed verbatim and analysed using constructivist grounded theory.
Results: Over two thirds of families across sites reported substantial benefits from participation in FT, including reduced stigma, giving children and partners a voice, increased service-user confidence, and improved family communication/relationships. Key facilitators identified by families included: programme delivery by a competent, non-judgmental clinician; the whole-family approach; and family readiness to engage. Barriers to engagement included stigma, family crises/relapse, service constraints, impact of COVID-19, and a need for further child, family and follow-up sessions/supports.
Conclusion: This study is the first qualitative analysis of family experiences of FT to be conducted within the context of an RCT and national programme to introduce family-focused practise for families with PMI. The findings illustrate that FT is beneficial across cultural/policy contexts, different mental disorders and can be implemented across adult and child mental health settings, including children with existing mental health challenges. Key barriers and facilitators to implementation were identified by families, all of which should help to inform the future implementation of FT, and other similar interventions, both in Ireland and elsewhere.
Introduction
It is estimated that 23% of all families have at least one parent who has, or had, a mental illness; this has been shown to increase the risk of children developing a mental disorder during their lifetime (range 41 to 77%), whilst multiplying five-fold their utilisation of health and social services, and placing a substantial emotional, financial and parenting burden on caregiving partners (1–3). In the Republic of Ireland (RoI), 20% of adults experience a mental health illness—the third highest incidence across 36 countries in Europe—costing the Irish state €11 billion per year (4). Furthermore, it is estimated that 280,000 children in the RoI are dependent on parents who have a mental illness (5).
The transmission of risk from parents to children involves a complex interplay of genetic, prenatal, family and environmental/social influences and is significantly mediated by the impact of parental symptoms on parent-child interactions (e.g., insensitive and erratic attunement)(2). Worryingly, these vulnerable families are often not identified or supported by mental health professionals in the RoI, or in other jurisdictions, due to: a lack of policy/practise guidance; little or no collaboration between Adult Mental Health Services (AMHS) and Child and Adolescent Mental Health Services (CAMHS); an individualised, crisis-oriented approach to assessment/treatment; competency and confidentiality concerns amongst mental health professionals who may feel ill-equipped to undertake family work; and parental stigma/fear of social services and losing custody of their children (6, 7).
Although the prevalence and burden of parental mental illness (PMI) is a cause for public concern, there is increasing evidence that integrated prevention and early intervention family-focused programmes/practise (FFPs) can help decrease the risk of developing mental disorders for children by up to 40% (8) and reduce referrals to child protection services (9). The Family Talk programme, in particular, has been identified in several systematic reviews (8, 10, 11) as a key intervention with promising evidence of effectiveness in improving parent and child understanding of mental illness and child internalising symptoms (12–16), with one study indicating enhanced family functioning and parental mental health recovery 4.5 years later (14).
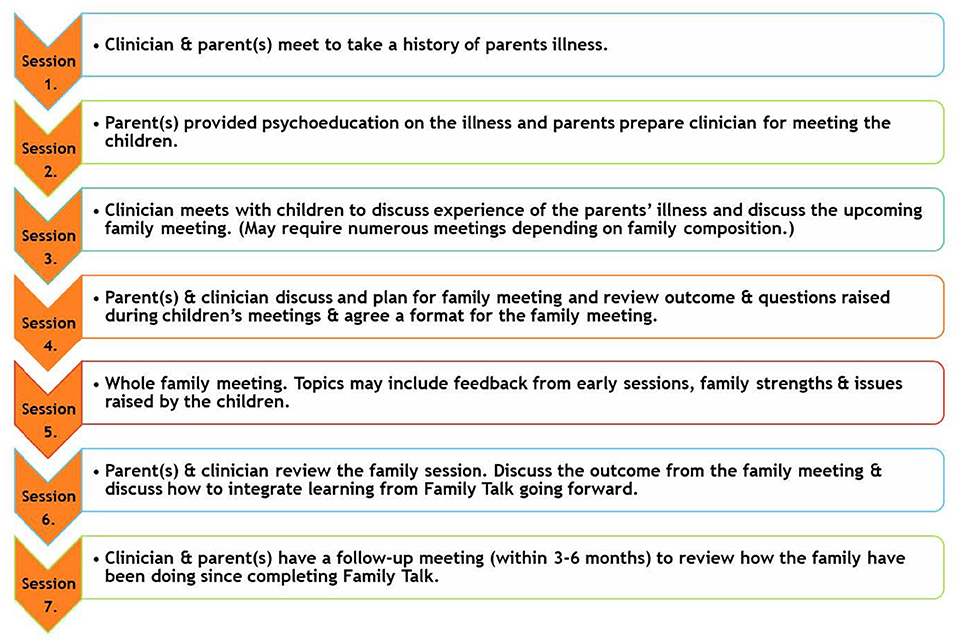
Family Talk (FT) was developed by William Beardslee and colleagues in the USA in the 1980's and is a manualised, 7-session, strengths-based, psycho-educational, whole-family approach designed to enhance family understanding and communication about parental mental illness, improve family interpersonal relationships, and promote family resilience and utilisation of social supports (12). The intervention involves a clinician meeting with each individual family, i.e. with parents (sessions 1, 2, 4, 6, 7), with each child individually (session 3), and with the whole family (session 4) (see Figure 1). Sessions typically last 60–90 min. The current evidence base for FT is limited by the small number of RCTs conducted to date and within only three countries (USA, Finland, Germany), generally small sample sizes, and mixed support for effectiveness in improving child externalising symptoms, parental mental health and family functioning (14, 15, 17, 18).
Due to its small but growing evidence base, FT has been implemented in recent years in several countries to support families where a parent has mental illness [e.g., the USA (Chicago), Costa Rica, Colombia, the Netherlands, Greece, Scandinavia (Norway, Sweden, Finland), Iceland, and Australia (Victoria)] (19). Internationally, there has been a growing trend, informed by the United Nations Convention on the Rights of the Child, to introduce legislation mandating support for children when a parent suffers from serious mental illness [e.g., the Swedish Health and Medical Service Act (20, 21)]. This legislation means that psychiatric services are obliged to take patient's children into consideration, including meeting their needs for information and support, and discussing issues of parenthood and the children's well-being (21). However, the continuing stigma around mental illness, especially as a parent, coupled with service provider constraints, often means that these policies are not implemented in practise (22).
Within the Irish context, whilst national practise guidelines have recently re-oriented toward a recovery,1 strengths-based model of care that recognises the needs of family carers and the value of family-focused mental health practise (23–25), there is no specific policy/practise guidance to support families with PMI in the RoI. Consequently, the national Health Service Executive (HSE) provided funding for the current research programme—called “PRIMERA” (Promoting Research and Innovation in Mental hEalth seRvices for fAmilies and children), the primary aims of which were to: (1) identify/develop, implement, and evaluate family-focused interventions for families with PMI; and (2) inform a “think family” care delivery agenda within mental health services in Ireland. Following an initial scoping study that demonstrated a lack of structured support for this population in the RoI, it was agreed with stakeholders that clinicians across 15 AMHS, CAMHS and child protection/welfare service sites would deliver Family Talk as part of a randomised controlled trial (RCT), with embedded qualitative and economic analyses (6, 26). FT was chosen for implementation as it: incorporates a structured “whole family” evidence-based approach; can be used with a range of mental disorders; provided freely available and high quality online training/resources2; and was replicable and capable of being implemented across sites in Ireland (6).
Despite the growing number of trial evaluations of FT, very few qualitative studies to date have investigated the experiences of families in attending FT. This means that little is known about the barriers and facilitators of change, intervention characteristics or contextual factors that may influence implementation and trial outcomes, particularly when delivered in real-world service settings (27). Indeed, the voices of service users, their families and particularly children, are rarely heard in controlled evaluations of FFPs (10, 28). Previously, it has been found that children may have a different perspective on “what helps” compared to parents and mental health practitioners (29). In addition, partners of service users have reported feeling uninvolved in research, which compounds their experience of feeling unsupported in their care burden by mental health services (30, 31). Thus, eliciting the views of children and other family members regarding FT delivery is important for informing the future development and refinement of this, and other similar, programmes.
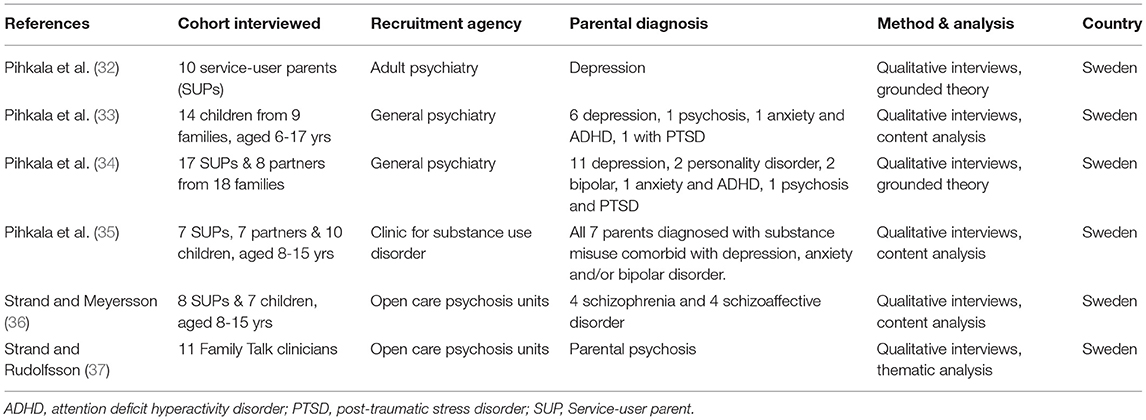
Five qualitative studies eliciting family experiences of FT have been conducted, to date, all undertaken in Sweden, three within outpatient psychiatric settings (32–34), one within a substance misuse clinic (35), and another in an open care psychosis unit (36). With regard to the last of these, a companion study of clinician reports of family experiences of FT was also conducted (37). Table 1 summarises the participant characteristics across these studies). Collectively, the findings from these studies from both parents and children show that: the silence around mental illness in their home had been broken, they had greater understanding of mental illness, and more open family communication and closer relationships, although the level of improvements varied across and within families (32–36). Service-user parents felt more equipped and empowered in their parenting role and children expressed relief from fears, less monitoring of their parents, less carework in the home, and being able to spend more time with friends and other interests (33, 35, 37).
Arguably, these findings are potentially biassed in that they did not interview families who refused to attend or disengaged from the programme. High rates of refusal and attrition have been noted elsewhere, often due to competing needs for daily survival and fear of judgement (15, 37). A limited range of informants (e.g., mostly PMIs with depression, limited data from partners or those who disengage from FT), small sample sizes, and an overall lack of cultural diversity, underscore the need for qualitative analyses to be undertaken across a wider variety of settings and contexts. For instance, FT is not always delivered in countries with specific policy/practise guidance for this population.
This qualitative study was nested within an RCT of the Family Talk intervention in Ireland for families with parental mental illness and children aged 5–18 years; the aim of the RCT was to assess the nature and extent of any pre-post intervention changes in child and family psychosocial functioning (26) and data analysis is currently underway. The objectives of the current study were to: (1) investigate the experiences of families attending FT; and (2) explore the processes of change, contextual factors or intervention characteristics that may influence trial outcomes in mainstream mental health settings (26).
Methods
Participants and Settings
The larger RCT included 86 families (139 parents, 221 children) in 15 sites across the RoI, involving adult, child, and primary care mental health services, and Tusla child protection services (26). Families (parents and children aged 5–18 years) were recruited by clinicians in each site from their existing waiting lists, and written informed consent/assent was obtained for their participation in the research (26). FT was delivered in a mental health outpatient clinic and/or in the home by a mental health professional, typically a social care worker, social worker, or psychologist. Families were eligible where a parent had a formally diagnosed mental disorder, with 80% of service-users attending AMHS for various mental disorders and 20% receiving antidepressant medication or primary care psychological support under the governance of a General Practitioner (26). Due to the high risk of intergenerational transmission of mental disorders (2), and a desire among stakeholders to increase family-focused collaboration between traditionally segregated adult (AMHS) and child mental health services (CAMHS) (6), we included families where children attended CAMHS or primary care services for mental health issues, as well as families where children were not involved with mental health services (26).
Participants were block randomised, on a 2:1 ratio, to the FT intervention (n = 56) or to a treatment as usual control group (n = 30). Assessments were carried out at baseline and at six month follow-up periods. At six-month follow-up, attrition was 37%, the rate of which doubled due to the impact of the COVID-19 lockdown restrictions (22.8 vs. 45%). More details on study parameters can be seen in the study protocol (26). The flow of participants from recruitment through the RCT to the qualitative studies is shown in Figure 2.
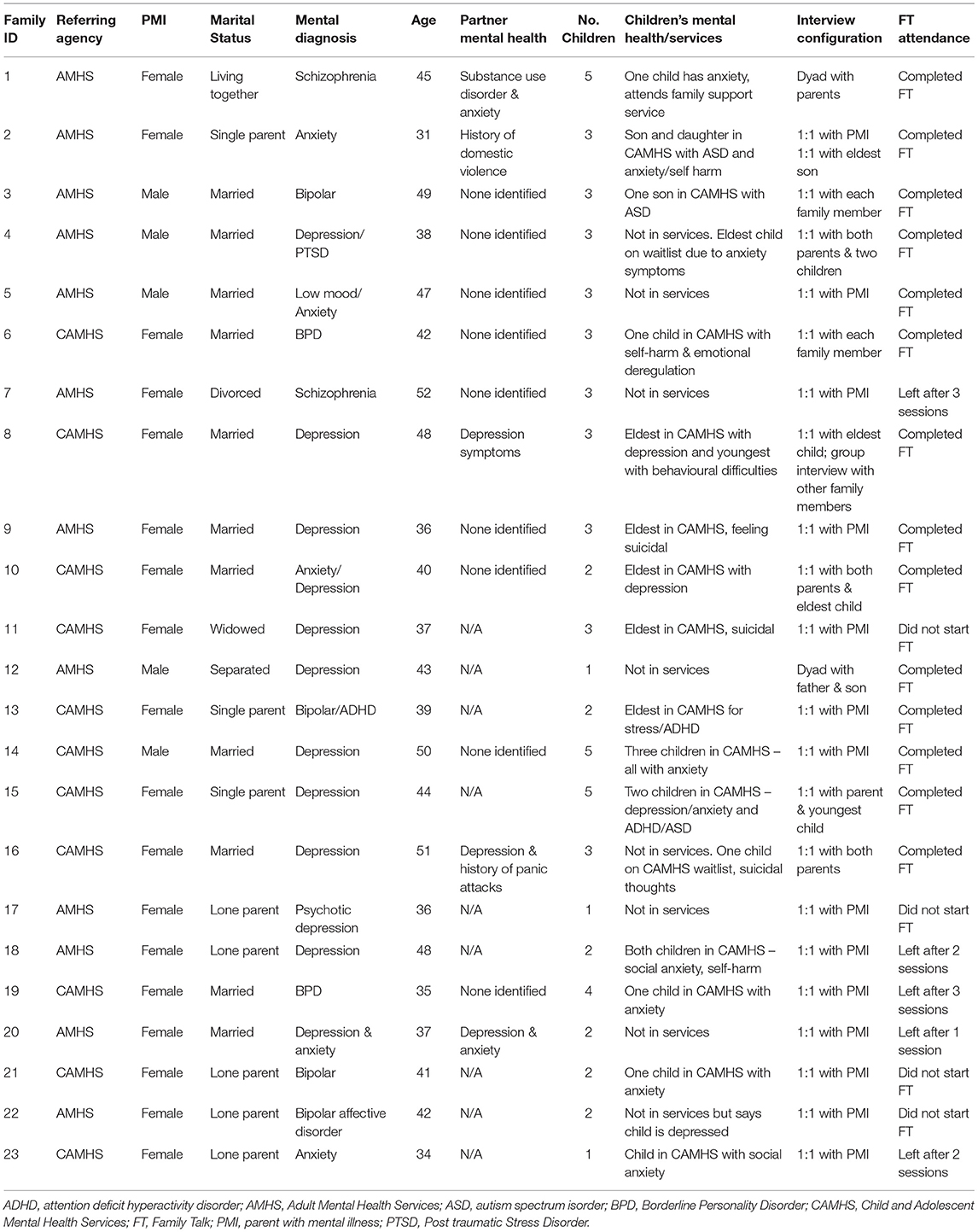
For the qualitative study, a purposive sampling method was used to approach prospective participants (n = 34 families) for interview on the basis of key demographic variables (e.g., age, gender, lone parent, mental disorder, number of children, site location and (mainly socially deprived) socioeconomic status). A series of 37 one-to-one semi-structured interviews and 3 group-based family interviews were undertaken at 6 month follow-up with a total of 45 participants from 23 families, including 23 parents with mental illness (PMI), 7 partners and 15 children/young people aged 9 to 18 years. (While children over five could participate in FT, only those aged over 8 years could participate in the research process as the assessment measures were not suitable for the younger age group). Fourteen families attended all FT sessions while nine dropped out after completing less than three sessions, and were interviewed to provide a “negative case” analysis. In the RCT sample, mean attendance in the intervention group was 4.4 sessions (SD = 1.2), with 53% attending all sessions.
The qualitative sample had a largely similar profile to the larger RCT cohort in terms of the demographics indicated above. Twelve of the interviewed families were recruited by AMHS and eleven by CAMHS. Service-user parents (i.e., parent was attending mental health services, usually AMHS, for their mental health challenges) had a mean age of 41.6 years (SD = 8.2) and were predominantly female (18/23), Caucasian (22/23), and socially disadvantaged (15/23); approximately half (11/23) were lone parents and the largest proportion reported anxiety/depression (n = 14/23), followed by bipolar disorder (n = 4), Borderline Personality Disorder (n = 2) and psychosis (n = 3). Six of the seven partners who agreed to be interviewed were married. Ten of the 15 child participants were male with a mean age of 13.2 years (SD = 2.8), and approximately half (8/15) reported attending, or were on a wait list for, CAMHS. The children in the larger RCT tended to be more evenly distributed by gender and were also a little younger (M = 10.3; SD = 5.3), whilst 42% were attending either CAMHS or psychology/family services (Table 2). More details on the characteristics of interviewed families can be seen in Table 2.
Data Collection and Analysis
Ethical approval (for both the RCT and qualitative study) was obtained from four research ethics committees including the HSE, the research institution where the research was carried out [name withheld for anonymous peer review], and two of the services with whom the research team worked (called Tusla and Saint John of God's Hospitaller Services).
Consent/assent forms were administered to parents and children, outlining details of the PRIMERA study, its potential benefits/risks, and where to seek help if necessary. Parents provided written informed consent for their children to participate and then their children provided written informed assent. Interview schedules were devised for each of the three participant groups in order to guide, and provide a framework for, interviews. These included questions such as “Tell me about your experience of FT, “What did you like about it?,” “What would you change about FT?” and “Would you recommend FT to other families?” Families who completed <3 sessions were asked their reasons for not completing FT. Interviews lasted between 15 and 40 min, with 33 (73%) conducted in participant's homes, and 12 (27%) via online platforms during the COVID-19 lockdown restrictions. There was some evidence of possible gatekeeping in three families with the PMI limiting access to family members. In addition, two parents requested to sit in on the children's interview. The interviews were conducted by experienced researchers [CM (n = 38), SMcGa (n = 7)], with lived experience of PMI, and with qualifications in psychology, mediation and psychotherapy. Given the stigma and impact of PMI, every effort was made to create a warm and non-judgemental atmosphere to ensure that participants felt understood. In addition, rapport had been established prior to the interviews as both researchers had prior contact with families during the baseline and 6 month RCT assessments (blinding was broken after the 6 month assessment to complete the qualitative interviews). Parents received a €25 gift voucher as a token of thanks for participating in the qualitative interview and children received a €10 voucher. Interviews were audio recorded with consent and transcribed verbatim.
The data from the interviews were analysed using constructivist grounded theory and MAXQDA software in order to identify and organise themes (38, 39). Analysis was also informed by the Medical Research Council guidance for complex interventions (27). Data were analysed using line-by-line and focused coding, constant comparison of codes to find similarities and variations within categories and hierarchical linking of categories to generate super-ordinate (or overarching) themes. The epistemological stance of constructivist grounded theory is more explicit than grounded theory in acknowledging the interpretive or constructivist nature of generating themes (38). The research interviewers were sensitised to honouring the lived experience of all participants (and particularly children) given the lack of data from this often invisible cohort but also due, in part, to their history of PMI. All interview transcripts were read by CM and MF, CM coded and analysed all of the data, while three authors (MF, SMcGa, SOC) independently assessed the reliability of coding on 12 of the 45 (27%) interviews. Reporting conforms to COREQ (Consolidated Criteria for Reporting Qualitative Research) guidelines (40).
Results
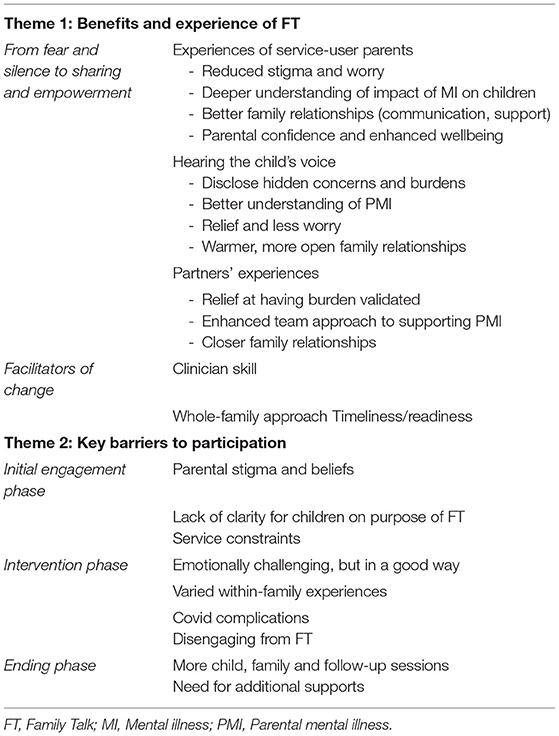
Two overarching themes were identified from the analysis: (1) Benefits and experiences of FT and (2) Key barriers to participation (Table 3). A number of subthemes were also identified within each.
Theme 1. Benefits and Experiences of FT: From Fear and Silence to Sharing and Empowerment
Despite initial reluctance and fear about discussing mental health in a family context, the majority of families who attended FT (14/16) reported substantial benefits from participation, including: reduced worry and stigma, a greater understanding of the impact of PMI on family members; giving children a voice; improved parental confidence and support; improved family communication, problem solving, and warmer relationships. A total of four sub-themes were identified here.
Benefits to PMI
Three quarters of service-user parents (12/16) reported a reduction in shame, stigma and worry about being a “bad parent” following the intervention, which helped to improve their sense of well-being and parental confidence. Labelling was a common source of stigma. One service-user parent, for instance, agreed to participate only on the condition that the term “bipolar” was not used with his children. Another parent recalled the pejorative names used by his wife, such as “crazy” or “mentaller”. Such labelling encouraged the PMI not to share their suffering and to try to appear “normal.”
“I became very good at hiding things, trying to adapt and fit in and mirroring other people that were deemed to be socially acceptable.” (PMI 5)
“After coming out and saying it to them, and talking to them about it, there is nothing to be ashamed of.” (PMI 13)
“It was hard. But it was very relieving because there was a lot of stuff that I would have been fearing to talk about or say out loud.” (PMI 12)
FT also helped parents to have a better understanding of the impact of their mental illness on their children. While most parents feared that discussion of their mental illness would burden their children, they were relieved to learn that more open communication enabled them to better understand their child's perspective, and empowered them to address child concerns and unspoken inaccurate beliefs. For example, one son panicked if his mother mentioned the doctor or heard an ambulance siren, fearing she would be re-hospitalised. Another secretly feared his mother was dying from cancer, while children in another family felt that they were somehow to blame for their mother's illness. The FT sessions also allowed parents to explain frightening past behaviour to their children, thereby allaying anxieties. Listening to their children's accounts was an emotional experience for all parents who completed FT.
“It helped us as a family to see from their [kids] vantage point how it affected them and try to give them what they wanted to try to move on.” (PMI 4)
“She [daughter aged 11 years] said she wasn't a very good daughter. When I was getting cross or why things weren't harmonious in the house, she felt that it was her fault.” (PMI 16)
“I was able to think of them more as people rather than my children that I'd be trying to protect, keep them safe from everything…Anything that they needed to talk about or worried about, and without fear of repercussion. Being able to say it in a safe place was good, for all of us really. There were tears and everyone at the end of it felt good and felt heard and respected in it.” (PMI 13)
“I just felt brilliant after it and I was able to tell them how proud I was of them and how much I love them. I can't just put words on it. But it has changed us for the better.” (PMI 15)
The direct involvement of children also helped parents to re-evaluate their understanding of children's prior behaviour; instead of assuming that silence indicated the child's lack of awareness of the illness or lack of care for the parent, the PMIs realised that a child's silence is more often an attempt to protect the family and/or to avoid burdening them.
“Beforehand I was saying, oh they don't want to talk to me… It's that they didn't want to be putting extra worry on me about anything because I had a mental health issue.” (PMI 6)
“I did not realise my eldest was being bullied for 2 years in school during my illness. He kept it to himself because at the time, he worried about me killing myself.” (PMI 1)
Service-user parents also indicated that the sessions improved their communication with, and support from, their partners, as well as from their children. Overall, improved family interactions and relationships appeared to assist mental health recovery and personal and parental confidence
“It gave me a sense of kind of, well not accomplishment…it was a huge sense of like, I'm doing this, I'm going to help [the children]…Having been through it, it gave me strength in a way.” (PMI 2)
Hearing the Child's Voice
All but three the children (12/15) reported that they found FT to be helpful despite their initial reservations about attending and the emotional challenge of participating in individual/family session (Three of the younger children found it difficult to recall FT as they were interviewed 4 months following FT). Children indicated that they felt empowered by the opportunity to: voice “hidden” concerns about PMI, family dynamics, and other issues; and to develop a deeper understanding of their parent's mental illness. Previously undisclosed concerns included: distress with the PMI's behaviour (e.g., anger, social withdrawal, self-harm) and/or with arguments and tension at home, feeling overburdened by caretaking activities, being bullied, educational disruption, child depression, suicidal ideation, feelings of blame, fear, sadness and injustice/anger. Eldest and only children were more likely to carry a largely unacknowledged burden in caring for family members, especially during heightened presentation of symptoms. Caretaking responsibilities included: caregiving, cleaning, shopping, cooking, financial responsibilities, and looking after the emotional well-being of siblings and the other parent. The dominant unspoken message of silence around PMI, combined with an often unavailable partner (due to work pressures, absence from the home, and/or emotional disconnection), left children feeling overwhelmed and unsupported.
“Dad was absolutely working his ass off to try and get money for us and taking care of Mam and running in and out of hospital. And doing school with us, trying to get us to do our homework and everything. He needed a lot of help. From a young age, myself and my sister had to take on a role, me more so because Dad was working and trying to provide. Mom was either in bed or in hospital, so I'd be like at school, have to come home, mind my siblings, my sister had to cook.” (Eldest child, 16 years old)
“I do get in a terrible mindset when it comes to my Mum's mental health because it's not nice… impacts on all of us as a family.” (Eldest child, 18 years old)
“I ask Mum for a lot of days off school because I get fed up with all the bullies...I used to have dark thoughts, not wanting to wake up.I do worry a lot. Because my Mum doesn't really have another person to help her, I'm normally that other person.” (Middle child, 10 years old)
“I pretty much have been in a really bad state since I was about nine, really low depression and suicidal. The only reason I didn't tell my parents was because my Mum's sick, my Dad doesn't care. It's not that they don't care, it's just that my Dad was working. I was kind of like, my Mum's in bed sick. I can't be talking to her, she needs to get better first.” (Middle child, 14 years old)
Many children indicated that their parents were unaware how much they had been affected by tense/volatile home situations, and had hidden their concerns to avoid burdening parents. As parents became more cognisant of children's needs, family members were motivated to reduce levels of anger/arguments, and to relate to each other in more warm, caring and fun ways, thereby leading to reduced stress and worry and increased child well-being. For instance, family members made more efforts to connect with each other by having regular meals, spending time with each other, and being generally more cooperative and supportive. Siblings also advocated for each other's well-being in sessions, which helped to improve sibling relationships following FT. While there was still some evidence of parentification among children following FT, several expressed relief that FT had broken the silence, secrecy and stigma around mental illness within their families, and that as well as feeling that parents were now listening to them, they also experienced increased empathy and compassion for their parents whom they perceived as “trying their best” in challenging circumstances.
“I found it was helpful for the family, like to talk about this, because usually when we're home, we don't really talk about it properly.” (Youngest child, 12 years old)
“I felt like the course has helped quite a lot to be honest. Family life has just got a lot easier. We're not arguing as much, we're not shouting. It's just easier to talk to people now...You have the resources to actually talk about it and try and sort it out.” (Eldest child, 16 years old)
“It was definitely worth doing. Because without the course we mightn't have known anything about it. And for him [Dad] to understand that we understand what he has. It's kind of improving him and us.” (Middle child, 14 years old)
“He [FT clinician] was asking how I was getting along with my Dad and my Mam, and I said, “Ok, we fight a lot, then it improved” and then we were called back in, and we were just saying, “Me and my Dad improved,” and he [FT clinician] said, “That's good.” (Youngest child, 9 years old)
“I think everyone's being a lot less aggressive, everyone's just trying to be a bit nicer to each other. I think everything's kind of been a lot calmer, especially with my Dad, he's been a lot calmer recently and he's started to kind of take other people's opinions and ideas into account.” (Eldest child, 16 years old)
“It helped me a lot. It made me feel better.” (Eldest child, 10 years old)
Partners' Experiences
While partners corroborated the benefits noted above, the largest single gain from their perspective, was that FT provided them with a forum in which they could voice their experience of partnering and co-parenting with a PMI, often for the first time, despite their partner being in mental health services sometimes for up to 20 years. All partners spoke of the stresses of caregiving, financial and household responsibilities, feelings of loneliness, frustration and helplessness, and strains on their marital relationships. Partners indicated that their isolation was amplified by exclusion from the PMI's treatment/care plan, and that they lacked the knowledge or skills to help their partner. Maintaining the focus on the service user's ill health also negatively influenced some partners' self-care, with three partners (3/7) managing their own mental health difficulties including anxiety, depression and alcohol misuse.
“You feel like you're carrying a whole house on your shoulders. You feel like a right tool. I can't do anything right. I can't say anything right. I can't help…I don't know what to do.” (Partner 6)
“I needed to ring someone, just for advice or help. But there was nobody.” (Partner 4)
“Over the last 4 or 5 years, we even talked about splitting up.” (Partner 3)
All partners described relief at having their experiences validated by the FT clinician and acknowledged by the PMI. While heated discussions and angry outbursts were common in the initial sessions, they were seen as worthwhile as it increased understanding and empathy between parents on the burdens that each was carrying. Five partners indicated that their relationship with the PMI had improved following FT. Partners also expressed to the PMI that they wanted to know how best to support them and wanted to be involved in their careplans. The dialogical approach of FT sessions helped to encourage a team approach to supporting the PMI, helping both parents feel more connected.
“It's an opportunity for him [husband] to hear me voicing the impact that it has on me in a very calm manner, because I'm in front of somebody else. It also takes away some of the guilt or the blame for me on his side… when you are more involved in the treatment.” (Partner 3)
“These sessions were great because we were both able to see where the other person was coming from.” (Partner 1)
“I think it [Family Talk] is 100% needed. As I said, there was nobody out there for me or the kids that I knew about… I can't compliment it enough. It's just the best thing that happened.” (Partner 4)
Facilitators of Change
Clinician Skill
The majority of PMIs and partners indicated that it was the skill of FT clinicians that mediated the benefits for families. Parents welcomed the non-judgemental and strengths-based approach adopted by clinicians, and their skill in facilitating multiple perspectives across several developmental ages. In addition, the PMIs (12/16) appreciated the clinician-led, psycho-educational aspect of the programme, which led to a deeper understanding and normalisation of their mental health challenges.
“Family Talk was very positive because there was somebody, a trained professional who had seen this before-it was in a way normalised. The kids were worried they were the only family in Ireland who had this problem.” (PMI 5)
“Everything that I talked about and went through, I had full support from her [FT clinician]. I can't even tell you how good she was. I can't say it enough. She was unbelievable.” (PMI 12)
“Everyone can say how they felt without any fear...Everyone felt very good afterwards and it was like a weight lifted… It's like a friendship with someone [clinician] that knows what you're talking about.” (PMI 13)
Whole Family Approach
All family members believed that FT worked because it involved the whole family, and allowed multiple, often hidden, stigmas, concerns and burdens to be revealed and shared, thereby validating each person's lived experience, whilst also empowering them to be more supportive of each other. Participants indicated that the focus on the family unit had helped them to look beyond their individual burdens and to feel deeper understanding and empathy for each other.
“It [FT] opened up the family and they talked about what they wanted to say and everything and you knew exactly where you stood, and it was up to you then to change the wrong things to try change them to the right things...It was brilliant because it brought out everything, the good and the bad, which was good.” (Partner 7)
“I just remember it was good for our family to actually talk properly without any kind of aggression, without any blame… everyone could just say how they saw things and people would put in their input without anyone kind of being upset about it. It was good to have like outside influences making sure everything was just calm.” (Eldest child, 16 years old)
Timeliness/Readiness
Parents also indicated that timing, setting and their readiness for FT were important factors in engagement. If approached too early, they said that they might have denied the impact of their illness on their family/children. They also required a lead-in time to build up the courage and find words for the difficult initial conversations with their partners and children in order to convince them to participate. Furthermore, in order to engage properly with the programme, they indicated that they needed to have recovered from their worst symptoms. Parents also valued the flexibility of holding sessions within their homes or within clinics.
“We did it during the summer and it was ideal, we walked to it [clinic] through the park and went for coffee afterwards, just the whole experience of going was great for the family.” (PMI 4)
“This time last year I wasn't feeling well so I was able to focus on it this time.” (PMI 9)
Theme 2: Key Barriers to Participation
Key barriers to participation occurred during one of three phases, each of which was identified here as a subtheme including: (a) initial engagement; (b) attending the intervention; and (c) the concluding phase. An overview of challenges to participation can be seen in Figure 3.
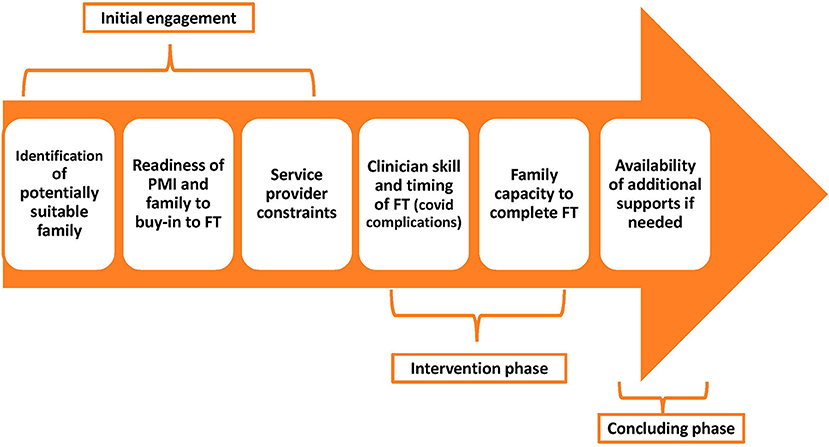
Figure 3. Challenges to participation in Family Talk during the engagement, intervention and ending phases.
Initial Engagement Phase
The most common barrier for families attending FT was parental attitudes/beliefs and stigma around mental illness. Parents were hesitant about participating for the following reasons: they felt stigma and shame in openly discussing their mental health challenges in the family context; they believed they were protecting children from the impact of their illness by not discussing it; they feared what their children would say; and a few were not ready to acknowledge that their illness might affect their children. Families required extensive preparatory input from clinicians to allay their fears to persuade them to engage with FT.
“The hardest part was actually admitting to him [the child] that I suffer with mental health problems. I hid away because for a long time, I have suffered with the stigma that goes with it.” (PMI 15)
“There's a very big stigma there. To make it easier to get through to him [partner], I think having someone else outside [clinician]. Through that, I felt a lot safer to try Family Talk.” (PMI 12)
Several children also highlighted their reservations about attending FT in terms of not understanding its purpose, fearing the focus would be on their wrongdoings (perceived or otherwise), and distrusting the viability of open discussion with typically uncommunicative parents. A couple of parents admitted that they had deliberately not clearly explained the purpose of FT to their children, for fear they would not attend.
“I would have preferred a bit more information. I didn't know what to expect and when we went in to speak with the girl who was doing it, I didn't know if the questions were going to be directed at us or about our parents. I was getting agitated because I was confused.” (Eldest child, 15 years old)
“I wasn't clear what it was about so I didn't know what to say.” (Middle child, 13 years old)
In addition, service constraints (e.g., staff turnover, uncovered maternity leave) disrupted/delayed FT delivery which meant that some families had an FT clinician with whom they were unfamiliar, meaning that additional time was needed to build rapport and trust before starting the intervention.
“I had never met her [FT clinician] so I think if maybe we had one or two sessions before just to get her to know a little bit better.” (Middle child, 17 years old)
Four of the interviewed families did not start FT due to family challenges and service constraint issues including: relapse in parental mental health; dealing with family crises (e.g., sexual assault, facing homelessness); deciding not to inform children about FT; being discharged from CAMHS before they could start FT; and suspension of FT delivery due to COVID-19 lockdown restrictions. It was interesting to note that discharge from CAMHS was cited as a reason for non-engagement because this reflects the lack of managerial priority given to family work and a perception by some CAMHS clinicians that working with parents is outside their service remit.
“We really wanted to do Family Talk but our daughter told us she was sexually assaulted so it wasn't the right time.” (PMI 20)
“We were meant to go to it [FT] but then we were discharged [from CAMHS] and that was the end of it.” (PMI 18)
Intervention Phase
The findings suggest that FT was challenging for many families despite the non-judgemental support provided by FT clinicians. Several parents/partners reported difficulties in speaking openly in sessions and/or listening to the experiences of family members, although most ultimately felt that it was worthwhile because it improved family communication. Partners and parents were shocked by their children's previously undisclosed revelations, what children had observed, and the internal narratives being used by children to make sense of the family situation (e.g., “Mum has cancer,” “I made Dad ill”). There was also some unease that clinicians might “selectively” reveal what children had disclosed in the child session, leaving parents feeling uninformed. Furthermore, a couple of service-user parents believed that their partners had undiagnosed mental illness, and consequently were unhappy that the focus was primarily on their own mental health challenges.
“It was an eye opener. It was upsetting at the time, because to hear your child say certain things, it's really upsetting. But upsetting in a good way.” (Partner 4)
“We think we're protecting and sheltering them and, in the meantime, we're doing more damage.” (Partner 6)
Similarly, most children (10/15) reported emotional challenges in engaging with FT. For instance, most children had no prior relationship with the FT clinician and some perceived them as asking too many personal questions too quickly, without allowing time for trust and rapport to build. Four children said that they felt shy and/or embarrassed when answering clinician's questions. A couple of children also indicated that they did not want to answer questions as their parent had not discussed their mental illness with them before the FT child session. Another child left the individual session and informed his mother that he had not revealed anything because the school encourages pupils “not to talk to strangers.” A few children found the family session emotionally volatile but ultimately helpful, while one teenager was initially upset in learning details of their parent's illness. Despite these challenges, the skill of clinicians in engaging children (e.g., allowing time to adjust, facilitating their voice being heard in the family session) had helped build a safe space for all but two to open-up and to engage with the process.
“Sometimes she'd ask personal questions that I wouldn't feel comfortable answering...My mouth goes shut.” (Middle child, 10 years old)
“I was just sitting there quietly not really talking or saying anything. I felt completely thrown under the bus. I wasn't surprised. I would have liked more information.” (Eldest, 16 years old)
“It was kind of emotional but then it got helpful and pleasurable. We got to say what we wanted to say. Dad has become more open. He shows his emotions now. He used to bottle them up a lot before.” (Only child, 12 years old)
Interestingly, within four families, there were widely varying experiences of the perceived utility of FT. In three families, both children and partners reported considerable benefits but the PMI did not. One PMI said that she “did not want to hear what others [in her family] were saying and blanked out,” whilst another was wary of discussing mental health with his children in terms of diagnostic labels and believed the intervention, particularly with the children, was of insufficient duration and should have been delivered years earlier. Both of these parents had severe/enduring mental illness, were currently feeling very unwell, and had a history of being unhappy with mental health service provision. In the fourth family, FT was delivered in the morning when the PMI was heavily medicated, thereby limiting her level of engagement. Furthermore, while the child reported many benefits, both the PMI and her partner found it less helpful. The PMI was disappointed that FT had not focused on her daughter's mental health difficulties or her husband's “control issues,” while her partner said he found it difficult to share his concerns as he believed it would aggravate his wife's emotional instability. These varied experiences highlight that each family member presents with a unique history and motivations and can present a range of challenges for clinicians when considering a family's readiness for FT.
“Family Talk might not have helped Mum as much but it helped us.” (Eldest, 18 years old)
“I just don't think we got a whole lot from it. It is very one sided to be honest… when an issue did come up, if there was something with regards to myself or my husband, they just constantly kept bringing it back to “Well, how does that affect [child]?” (PMI 10)
“[The PMI] was getting so emotional because of her own opinions about things and stuff…I wasn't going to start dumping my own out there because it could have got messy and emotional. I didn't want to escalate any kind of like emotions. It was emotional enough. I was just kind of dealing with what was being brought up by [partner] and [child].” (Partner 1)
The COVID-19 pandemic restrictions have been shown to have had a considerable impact on population mental health and on those with pre-existing mental illness, both in Ireland and internationally (41–44). Seven families in this study were interviewed during the COVID-19 emergency, with three reporting sustained benefits from FT and that they were coping well with pandemic stresses, while four families reported increased mental distress and challenging child misbehaviour as a result of the restrictions; two of these families had disengaged from FT due to stigma/relapse issues and two indicated that FT delivery had been suspended due to the restrictions. Therefore, it appeared that the level of prior vulnerability and ability to engage with FT predicted how well families had coped with the stresses of the COVID-19 restrictions. In addition, one parent reported attending online sessions of FT for PMIs, partners, and older teenagers (16+) but these were not considered suitable for younger children or for family sessions and they had to wait until it could be delivered safely again in person and in line with COVID-guidelines.
“I don't think we could have dealt with months of isolation if we hadn't done FT. We make time for each other now at this stage. We watch family films or to sit down for dinner, meals.” (PMI 13)
“It wasn't the same but we were able to talk with him [clinician] on zoom. It was a while before the children could be seen so it wasn't ideal.” (PMI 5)
Disengaging From FT
Families who disengaged from FT after three or fewer sessions (n = 5) gave the following reasons. One said that FT was too emotionally upsetting, with another feeling a sense of blame for causing her children's mental health issues. A number of other factors also contributed to disengagement including family crisis, relapse in symptoms, and having too many competing priorities. Additional delays/disruption in FT delivery due to the COVID-19 restrictions also led to some degree of disillusionment and disengagement from mental health services. This was more common in areas where mental health clinicians were partially redeployed to frontline COVID-19 duties and could only provide minimal telephone support to service users (41). Interestingly, those who disengaged from FT were almost twice as likely as “completers” to be lone parents (6/9 vs. 5/14)–suggesting that the stresses of lone parenting may also have been a barrier to engagement.
“With covid, we are far less a priority for them. I don't know when or if we're ever going to get it.” (PMI 22)
“It felt like she was attacking me and it was my fault how the girls are...I don't need that.” (PMI 19)
Concluding Phase
Despite benefiting from FT, most attendee families (n = 12) found the programme to be too short and expressed a desire for more child, family and follow-up sessions to build family communication. Families had high expectations of FT, which appeared to be linked to their need for more (often unavailable) psychological and family support from mental health services. Three families reported that they were referred to further mental health supports (e.g., dialectical behaviour therapy), while two others were given a list of alternative supports including national mental health charities. Most, typically, parents reported that FT clinicians provided closure by affirming their availability if future issues arose but the lack of follow-up was problematic for some partners who were not offered additional support and who were unable to pay for private treatment outside of statutory service provision. However, it is important to note that three attendee families were interviewed during the first COVID-19 lockdown which severely limited their access to mental health and community services and to other social/family supports at that time. Nonetheless, there were numerous indications that this population would likely benefit from longer-term (family-focused) mental health support.
“It didn't feel like [it] was ready to be finished.” (Partner 3)
“I think more sessions with the family…and more time with the children would have really helped. The three of them went in one by one for 20 min. So it might have been a little bit rushed for them, they might not have had enough time.” (PMI 16)
“Family Talk is minimal… A taster...I think the hospital might have family therapy…But on a private basis so…” (PMI 2)
Discussion
This study is the first qualitative analysis of family experiences of FT conducted outside Sweden, the first situated within the context of an RCT of FT, and as part of the first nationwide endeavour to introduce FFP to adult and child mental health services in the RoI. The qualitative findings, in line with those reported in Swedish psychiatric settings (32–37), indicated many benefits for families who attended FT, including: reduced worry and stigma; a greater understanding of mental illness; giving children and partners a voice; improved parental confidence and family communication; and warmer relationships. Notably, the current study placed a greater emphasis on the caregiving, parental and financial stresses experienced by partners, all of whom for the first time had a forum in which to have their burdens validated, and a space in which to develop a more constructive team-based approach to supporting the PMI and the family unit. In addition, unlike previous qualitative studies, this study reported on the experiences of families who refused to attend or disengaged from the programme.
Importantly, the findings reported here, indicate that FT is acceptable and beneficial for families across different cultural/policy contexts, mental health settings, types of mental disorders, and among children with and without existing mental health challenges. Firstly, unlike Scandinavian countries where legislation has been introduced to safeguard children of PMI and where FT is implemented on a national level, the RoI lacks any “think family” policy/practise guidance for this population whilst service and public awareness of the need to support this population is erratic/unsystematic. There are also continuing high levels of mental health stigma in Ireland, which is an important barrier to help seeking (6, 45, 46). Given the challenges have been reported within Scandinavian (and other) countries in terms of translating family-focused legislation/policy into practise (22, 47), it was reassuring to find that FT was perceived as helpful by the vast majority of the families in this study, thereby highlighting the need for, and value of, such FFP supports for families where there is PMI.
Secondly, even though AMHS may appear the most natural fit for FT/FFP and provide a common context for the implementation of FFPs (45, 48, 49), families in this study reported benefits across both AMHS and CAMHS settings. FT is typically delivered as a preventive intervention to families whose children do not attend mental health services (14, 15) but in this study, most of the child participants, including those who attended CAMHS, reported that FT had improved their well-being and family relationships. Therefore, FFPs such as FT may also be helpful for children with existing mental health challenges, as well as promoting collaboration between adult and child mental health services, and increasing the identification of families through a “no wrong door” approach to family access, as promoted in the “Think Family” model in Northern Ireland (50).
Thirdly, there did not appear to be any notable variations across family experiences here in terms of the PMI diagnosis, thereby highlighting the suitability of FT for disorders beyond parental depression, which was the original focus of the programme (13, 14). Whilst a small number of adult service users who attended all FT sessions felt that it had not been helpful, their children/partners, and other service users with similar disorders, reported a range of benefits. Similarly, two PMIs, suffering from depression and Borderline Personality Disorder respectively, indicated that they disengaged from FT after two to three sessions as they felt blamed/upset by the idea that their mental illness may affect their children. Previous qualitative studies have indicated that while FT may work across a range of disorders, those with Borderline Personality Disorder or low-functioning psychosis are more likely to struggle with establishing a therapeutic alliance and/or exhibit a lack of understanding/insight into the impact of their mental illness on their children (34, 37). Low functioning service users may possibly require additional psycho-educational sessions and/or complementary groups for patients and children, in order to share experiences and learn about their mental illness and its impact on their children (37).
The findings reported here also highlight a number of important facilitators and barriers to engagement, which should help inform the future implementation of FT/FFPs and could be tested as mediators/moderators of RCT outcomes. Key facilitators included timeliness, clinician attributes and expertise, and involvement of the whole family. The clinician's role was key in: providing a setting for parent, partner and child voices to be heard and validated; normalising the family's lived experience; reducing fear and stigma through psycho-education; and teaching a strengths-based, problem-solving approach to improve family communication and interactions. Previous qualitative studies of FT likewise, highlight the value of clinician attributes of confidence, competence, warmth and non-judgmentalism in contributing to better family experiences (33, 34), whereas conversely, a perception that clinicians lack competency has been linked to disengagement (Unpublished data, Preventive Intervention Project, 2013, https://fampod.org/file.php/1/collaborations/Columbia_Application_of_PIP.pdf). An interesting study by Marston et al. showed that when parents were given a family-focused DVD, but did not receive the support of a clinician, their understanding of the impact of their illness improved, but they did have the confidence to open up a dialogue about the illness with their children (51). Thus, the presence of a trained clinician with appropriate attributes is a critical element of FT (and other FFPs) in terms of engaging families and potentially producing more positive outcomes.
Families particularly valued the whole family approach. As noted in previous qualitative studies, they felt that this had enabled all perspectives to be surfaced and heard, and improved mutual understanding and family relationships (32–34). Nevertheless, whole-family programmes appear to be less commonly delivered than parent-only models (48, 49), most probably due to the additional buy-in and logistics required in involving children. Our findings suggest that without the involvement of the child(ren), parents may not become aware of their worries and burdens as demonstrated here by the surprise and alarm that parents reported when their children opened up during the FT sessions. In addition, within parent-only interventions, parents may not be sufficiently supported to find the right words to have a conversation with their children, and may also lack a forum to realise just how much their children/partners want to support them, but have been prevented from so doing by the silence and stigma associated with discussing mental illness within the home. Two RCTs which have compared FT with the parent-only Let's Talk about the Children found FT to be more effective in reducing child emotional symptoms and improving the parent–child relationship (13, 15).
Similarly, child programmes that exclude parents may reduce the likelihood of mutual understanding as parents lack the opportunity to discuss their stigma concerns, to gain insight into the impact of their mental illness on their children, and/or to build parental confidence. Enhancing parental confidence and competence has been identified as key to shaping the quality of parent-child relationships (52). Significantly, the involvement of partners is less common in the implementation of FFPs (3). The findings from the current study indicated that FT provided a forum, usually for the first time, for partners to express their burdens and stresses and to communicate with the PMI about how they can better support them. Given the level of burden and stress reported, and the protective boundary provided by a healthy second parent (2), it is imperative that services/FFPs help to strengthen the “safety net” that co-parents provide in families with PMI. Recent filicide tragedies in Ireland (e.g., McGinley case) highlight the ultimate cost of not involving family members in the service user's treatment (53).
Significant barriers to participation were also reported in the current study. Most family members, including both completers and drop-outs, indicated that they had experienced challenges in engaging with FT in the initial phase. Parental fears and stigma around mental illness were the most commonly reported barriers to participation. Children also expressed reservations about attending, indicating that they were uninformed about the purpose of FT and wanted prior contact with the clinician prior to commencing FT sessions. Other family barriers to engagement were also noted, including relapse in symptoms and family crises. Previous qualitative studies have similarly highlighted that fear of judgement and/or competing needs for daily survival may impede family engagement (32, 37). These findings suggest that clinicians may benefit from the development of FT/FFP training videos/protocols to promote effective engagement strategies and address potential barriers to participation and retention. For instance, addressing issues of stigma, readiness/timeliness, consent and confidentiality during the recruitment process and including quotes/videos from previous FT attendees may help to improve engagement (54). In addition, a child-friendly recruitment approach that used age-appropriate marketing literature and involved a meet-and-greet session with the facilitating clinician might help to address children's concerns about attending. Lastly, low functioning PMIs may benefit from additional psycho-educational sessions and complementary group supports to promote engagement (37).
Service constraints were also an inhibitive factor in family engagement with the programme. The capacity of FT clinicians to build rapport and familiarity with the family beforehand was undermined by high turnover of personnel and under-resourced mental health teams. In addition, a small number of families were discharged from AMHS/CAMHS before they could start FT, while several other families disengaged due to their unhappiness with long waiting lists, and delays/disruptions due to the COVID-19 lockdown restrictions. These difficulties reflect general underfunding of mental health services in the RoI, alongside a lack of policy/practise priority given to supporting this population in an Irish context (26, 45, 55).
Some challenges were also noted during the intervention phase. Firstly, while most families reported that FT was ultimately worthwhile, it was also seen as emotionally challenging at times. Many reported difficulties in speaking openly in sessions and/or listening to other's experiences and indeed, this was also shown in research by Pihkala et al. (33) in Sweden. The clinician's skill in facilitating multiple perspectives was instrumental in ensuring that family members could listen to each other without becoming overly defensive or upset. Secondly, there was some evidence that children within two families did not receive sufficient time in their individual child session (e.g., 20 min each). Moreover, while children largely reported benefits from FT, there was little mention of fun within sessions. Therefore, children may benefit from the inclusion of some light relief at the beginning or close of sessions (e.g., ice breakers, child-friendly videos, closing “fun” take-home exercise), as used in, for example, the Kidstime intervention (56). Thirdly, the COVID-19 lockdown restrictions had implications for the delivery of FT, including blended adaptation (both in-person and online sessions), as well as family disengagement following repeated delays to delivery. Notably, there was considerable variation in the capacity of sites to deliver FT during the lockdowns with some mental health staff partially redeployed to frontline COVID-19 duties and providing minimal phone support to patients while clinicians in other areas were able to continue home visits and outpatient clinics, following COVID-19 guidelines (41). Reassuringly however, it is likely that the future implementation of FT will be conducted in person in view of the >90% uptake of vaccination in the RoI (57).
Lastly, while most families benefitted from FT, they indicated a desire for additional child, family and follow-up sessions, thereby suggesting that some of their needs had not been met. This was also noted by FT clinicians working with lower functioning psychosis patients in Sweden (37), although it was not reported by families experiencing depression (32–35). Where possible, the concluding phase of FT should signpost families to additional family and mental health supports as required. Given the complexity of service user needs, a flexible spectrum of family-focused services may be necessary, as demonstrated internationally (58), although this level of family resources is not currently available in Ireland (6).
Strengths and Limitations of the Study
This study is the first qualitative analysis of family experiences of FT conducted outside Sweden and the first conducted within the context of an RCT and national programme to introduce FFP for families with PMI, in this case within the RoI. Service-user parents are typical of those who take part in RCTs and qualitative studies of FFPs (28), but the current study involved the recruitment of a large and diverse sample (in qualitative terms) of both child and adult participants, including PMIs, partners, children, and “drop-out” families. In addition, our sample was recruited from a number of mainstream adult and child mental health services and encompassed a variety of mental disorders as well as including both children who were and were not attending CAMHS. The analysis yields further important insights into the barriers and facilitators of implementation, as perceived by families, and will help to support and amplify the clinician experiences of FT which are reported here in a companion paper (as well as the RCT results when they become available).
The study was limited in a number of ways, including firstly, the transferability of the findings across different cultural contexts. However, the description of the study context should help in this regard. It is also possible that the findings may be biassed in that families who agreed to be interviewed had a more positive experience of FT, and in a small number of instances, we believe that gatekeeping from the PMI may have potentially excluded feedback from other family members who were invited to participate in the research. Importantly though, we interviewed nine families who had disengaged from FT after three or fewer sessions as well as families who had completed FT. In addition, the interval between FT and the child interviews (ranging from 3 to 5 months) created recall difficulties for three of the younger children in our sample, although the remainder (n = 12) had much to say about their involvement. This interval was necessary due to blinding in the RCT which had to be retained until after the 6 month assessment had been completed. Lastly, 7 of the 23 families were interviewed during the first COVID-19 lockdown, which severely restricted access to services and led to increased levels of psychological distress in the general population in Ireland (42), both of which may have impacted their experiences and views.
Implications for Policy, Practise and Research
Our findings highlight the value of a whole family approach when a parent has mental health challenges, particularly in revealing the hidden burdens that children carry, reducing fears and stigma, and improving empathy and communication among parents and children. The findings illustrate that FT can be successfully implemented across adult and child mental health settings and with families experiencing different mental disorders, thereby reflecting, at least to some extent, a “no wrong door” approach to identifying and supporting families. Key facilitators to implementation included delivery by a competent, non-judgmental clinician and family readiness to participate. The primary barrier to FT implementation was recruiting and engaging with families in the initial phase due, in large part, to family challenges and service constraints. Engagement may be improved if clinicians address issues of stigma, readiness, consent and confidentiality during the recruitment process and use quotes/videos from previous FT attendees. In addition, children's concerns about attending could be addressed using age-appropriate marketing literature and an initial meet-and-greet session with the facilitating clinician.
Our findings also suggest that FT may not be suitable/sufficient for all families (e.g., low functioning service users) and should, ideally, be implemented as part of a suite of lower and higher intensity FFPs (58). There is an urgent need in the context of the RoI, to introduce “think family” practise guidelines and to provide dedicated funding to develop a multi-level, public-health response to identifying and supporting these families, as has been done in, for example, Scandinavia and Australia (33, 47). Under the United Nations Convention on the Rights of the Child (20), children have a right to a childhood and not be used as unpaid/unsupported carers filling gaps in service provision. Moreover, when child welfare is not considered in the treatment of service-user parents, it increases their risk of developing mental disorders and becoming the next generation of service users, and, in the most tragic (but thankfully rare) cases, can lead to their death by filicide (53). Internationally, systemic barriers to change need to be addressed, including mandatory auditing of the parenting status of adult mental health users, balancing the priority given to patient confidentiality with unmet family needs, increased collaboration between traditionally segregated AMHS and CAMHS services, and equipping clinicians with time and resources to undertake FFP.
Further qualitative and quantitative research on family and clinician experiences of FT implementation is required across different cultural/policy contexts, mental health and family settings, types of mental disorders and level of child mental health difficulties. Further research is also needed on the types of families that are more likely not to engage with FT, and to identify measures and/or supports that might increase engagement. For instance, there may be value in developing and evaluating training videos that teach recruitment strategies to see whether they improve engagement. In addition, qualitative analyses may inform RCT evaluations of FT/FFPs; for instance, RCTs could include as outcome measures, benefits identified in qualitative analyses, such as reduction in stigma, parental confidence/competence, service-user mental health, partner well-being, and family functioning. Moreover, facilitators and barriers to implementation identified in qualitative studies could be tested as moderator/mediator variables in quantitative research.
Data Availability Statement
The datasets presented in this article are not readily available because where participants provided consent/assent, an anonymised version of their data will be stored in the Irish Qualitative Data Archive. Ethical approval from an approved higher level institution will be required if the data is to be used in future research. Requests to access the datasets should be directed to TWFpcmVhZC5GdXJsb25nQG11Lmll.
Ethics Statement
The studies involving human participants were reviewed and approved by four ethics committees: the Social Research Ethics Committee in Maynooth University, Ireland (Reference number SRESC- 2018-100), the HSE Research Ethics Committee, Tusla Ethics Review Committee, and the Saint John of God's Research Ethics Committee. Parents/legal guardians provided written informed consent for their children to participate in the study, followed by their children providing written informed assent to participate.
Author Contributions
CM, MF, and SMcGi conceived and designed the study. CM conducted interviews and coded transcripts, with 25% of transcripts independently coded by MF, SMcGa, and SO'C. CM prepared the initial draft, with subsequent drafts undertaken by MF, with input from SMcGi, CM, and SMcGa. All authors contributed to the article and approved the submitted version
Funding
The PRIMERA research programme is funded by the Health Service Executive and the Maynooth University Higher Education Authority COVID-19 Costed Extension Fund.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We are very grateful to all the families who generously gave their time to participate in this study. We also owe special thanks to all of the dedicated clinicians and managers who agreed to participate in this research and to introduce and deliver Family Talk within their settings, including the Health Service Executive, Saint John of God Hospitaller services, and Tusla child protection agency.
Abbreviations
ADHD, attention deficit hyperactivity disorder; AMHS, adult mental health services; ASD, autism spectrum disorder; CAMHS, child and adolescent mental health services; FFP, family-focused practise/programmes; FT, Family Talk; HSE, Health Service Executive; MI, Mental illness; PMI, parents with mental illness; PRIMERA, Promoting Research and Innovation in Mental hEalth seRvices for fAmilies and children; PTSD, post-traumatic stress disorder; RCT, randomised controlled trial; RoI, Republic of Ireland; SUP, Service-user parent.
Footnotes
1. ^The approach argues against just treating or managing symptoms but focusing on building the resilience of people with mental illness and a change in outlook that is related to leading a meaningful, purposeful life, with or without ongoing episodes of illness (23).
References
1. Maybery D, Reupert A, Patrick K. Prevalence of children whose parents have a mental illness. Psychiatr Bull. (2009) 33:22–6. doi: 10.1192/pb.bp.107.018861
2. Hosman CMM, van Doesum KMT, van Santvoort F. Prevention of emotional problems and psychiatric risks in children of parents with a mental illness in the Netherlands: I. the scientific basis to a comprehensive approach. Aust e-J Adv Ment Health. (2009) 8:250–63. doi: 10.5172/jamh.8.3.250
3. Afzelius M, Östman M, Råstam M, Priebe G. Parents in adult psychiatric care and their children: a call for more interagency collaboration with social services and child and adolescent psychiatry. Nord J Psychiatry. (2018) 72:31–8. doi: 10.1080/08039488.2017.1377287
4. OECD/EU. Health at a glance: Europe 2018: State of Health in the EU cycle. (2018) (accessed September 5, 2021).
5. Central Statistics Office. Census of Population 2016-Profile 4 Households and Families. (2016). Available online at: https://www.cso.ie/en/releasesandpublications/ep/p-cp4hf/cp4hf/fmls/ (accessed September 5, 2021).
6. Mulligan C, Furlong M, McGilloway S. Promoting and implementing family-focused interventions for families with parental mental illness: scoping and installation. Adv Ment Health. (2020) 18:202–16. doi: 10.1080/18387357.2019.1614466
7. Jones M, Pietilä I, Joronen K, Simpson W, Gray S, Kaunonen M. Parents with mental illness–a qualitative study of identities and experiences with support services. J Psychiatr Ment Health Nurs. (2016) 23:471–8. doi: 10.1111/jpm.12321
8. Siegenthaler E, Munder T, Egger M. Effects of preventive interventions in mentally ill parents on the mental health of the mental health of offspring: systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. (2012) 51:817. doi: 10.1016/j.jaac.2011.10.018
9. Nicholson J, de Girolamo G, Schrank B editors. Parents with Mental and/or Substance Use Disorders and Their Children. Lausanne: Frontiers Media SA (2020).
10. Bee P, Bower P, Byford S, Churchill R, Calam R, Stallard P, et al. The clinical effectiveness, cost-effectiveness and acceptability of community-based interventions aimed at improving or maintaining quality of life in children of parents with serious mental illness: a systematic review. Health Technol Assess. (2014) 18:1–250. doi: 10.3310/hta18080
11. Reupert A, Cuff R, Drost L, Foster K, van Doesum KTM, van Santvoort F. Intervention programs for children whose parents have a mental illness: a review. MJA Open. (2012) 1:18–22. doi: 10.5694/mjao11.11145
12. Beardslee WR, Wright E, Rothberg PC, Salt P, Versage E. Response of families to two preventive intervention strategies: long-term differences in behavior and attitude change. J Am Acad Child Adolesc Psychiatry. (1996) 35:774–82. doi: 10.1097/00004583-199606000-00017
13. Beardslee WR, Salt P, Versage EM, Gladstone TRG, Wright EJ, Rothberg PC. Sustained change in parents receiving preventive interventions for families with depression. Am J Psychiatry. (1997) 154:510–5. doi: 10.1176/ajp.154.4.510
14. Beardslee WR, Wright EJ, Gladstone TR, Forbes P. Long term effects from a randomized trial of two public health preventive interventions for parental depression. J Fam Psychol. (2007) 21:703–13. doi: 10.1037/0893-3200.21.4.703
15. Solantaus T, Paavvonen EJ, Toikka S, Punamaki RL. Preventive interventions in families with parental depression. Eur Child Adolesc Psychiatry. (2010) 19:883–92. doi: 10.1007/s00787-010-0135-3
16. Christiansen H, Anding J, Schrott B, Röhrle B. Children of mentally ill parents—a pilot study of a group intervention program. Front Psychol. (2015) 6:1494. doi: 10.3389/fpsyg.2015.01494
17. Punamäki RL, Paavonen J, Toikka S, Solantaus T. Effectiveness of preventive family intervention in improving cognitive attributions among children of depressed parents: a randomized study. J Fam Psychol. (2013) 27:683. doi: 10.1037/a0033466
18. Compas BE, Forehand R, Keller G, Champion JE, Rakow A, Reeslund KL, et al. Randomized controlled trial of a family cognitive-behavioral preventive intervention for children of depressed parents. J Consult Clin Psychol. (2009) 77:1007. doi: 10.1037/a0016930
19. Beardslee WR, Solantaus TS, Morgan BS, Gladstone TR, Kowalenko NM. Preventive interventions for children of parents with depression: international perspectives. Med J Aust. (2013) 199:23–5. doi: 10.5694/mjao11.11289
20. United Nations Treaty Series. United Nations convention on the rights of the child. Treaty no. 27531. (1989) 1577. p. 3–178. Available online at: https://treaties.un.org/doc/Treaties/1990/09/19900902%2003-14%20AM/Ch_IV_11p.pdf (accessed September 5, 2021).
21. Swedish Health and Medical Service Act SFS. (2010:662). Requirements on Health Care. Stockholm: Ministry of Health. Available online at: https://www.riksdagen.se/sv/dokument-lagar/dokument/svensk-forfattningssamling/halso–ochsjukvardslag-1982763_sfs-1982-763 (accessed September 5, 2021).
22. Lauritzen C, Reedtz C, Van Doesum KT, Martinussen M. Implementing new routines in adult mental health care to identify and support children of mentally ill parents. BMC Heal Ser Res. (2014) 14:58. doi: 10.1186/1472-6963-14-58
23. Health Service Executive. BFT National clinical programme. (2019). Available online at: https://www.hse.ie/eng/about/who/cspd/ncps/mental-health/psychosis/resources/hse-early-intervention-in-psychosis-model-of-care-executive-summary-june-2019.pdf (accessed September 5, 2021).
24. Health Service Executive. National Framework for Recovery in Mental Health. (2017). Available online at: https://www.hse.ie/eng/services/list/4/mental-health-services/advancingrecoveryireland/national-framework-for-recovery-in-mental-health/ (accessed September 5, 2021).
25. Health Service Executive. Family, carer, and supporter guide. (2020). Available online at: https://www.hse.ie/eng/services/list/4/mental-health-services/mentalhealthengagement/family-carer-and-supporter-guide/ (accessed September 23, 2021).
26. Furlong M, McGilloway S, Mulligan C., McGuinness C, Whelan N. Family talk versus usual services in improving child and family psychosocial functioning in families with parental mental illness (PRIMERA—Promoting Research and Innovation in Mental hEalth seRvices for fAmilies and children): study protocol for a randomised controlled trial. Trials. (2021) 22:243. doi: 10.1186/s13063-021-05199-4
27. Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al.: Process evaluation of complex interventions. UK Medical Research Council (MRC) guidance. BMJ. (2014) 350:h1258. doi: 10.1136/bmj.h1258
28. Maybery D, Reupert A. Parental mental illness: a review of barriers and issues for working with families and children. J Psychiatr Ment Health Nurs. (2009) 16:784–91. doi: 10.1111/j.1365-2850.2009.01456.x
29. Maybery D, Ling L, Szakacs E, Reupert AE. Children of a parent with a mental illness perspectives on need. Advanc Ment Health. (2005) 4:78–88. doi: 10.5172/jamh.4.2.78
30. Oltedal S, Garratt A, Johannessen JO. Psychiatric outpatients' experiences with specialized health care delivery. a Norwegian national survey. J Ment Health. (2007) 16:271–9. doi: 10.1080/09638230701279832
31. Bateson K, Darwin Z, Galdas P, Rosan C. Engaging fathers: acknowledging the barriers. J Health Visiting. (2017) 5:126–32. doi: 10.12968/johv.2017.5.3.126
32. Pihkala H, Johansson EE. Longing and fearing for dialogue with children—depressed parents' way into beardslee's preventive family intervention. Nord J Psychiatry. (2008) 62:399–404. doi: 10.1080/08039480801984800
33. Pihkala H, Sandlund M, Cederström A. Children in beardslee's family intervention: relieved by understanding of parental mental illness. Int J Soc Psychiatry. (2012) 58:623–8. doi: 10.1177/0020764011419055
34. Pihkala H, Sandlund M, Cederström A. Initiating communication about parental mental illness in families: an issue of confidence and security. Int J Soc Psychiatry. (2012) 58:258–65. doi: 10.1177/0020764010392088
35. Pihkala H, Dimova-Bränström N, Sandlund M. Talking about parental substance abuse with children: eight families' experiences of Beardslee's family intervention. Nord J psychiatry. (2017) 71:395–401. doi: 10.1080/08039488.2017.1308009
36. Strand J, Boström P, Grip K. Parents' descriptions of how their psychosis affects parenting. J Child Fam Stud. (2020) 29:620–31. doi: 10.1007/s10826-019-01605-3
37. Strand J, Rudolfsson L. A qualitative evaluation of professionals' experiences of conducting Beardslee's family intervention in families with parental psychosis. Int J Ment Health Promotion. (2017) 19:289–300. doi: 10.1080/14623730.2017.1345690
38. VERBI Software. MAXQDA 2020. Software. (2019). Available online at: www.maxqda.com (accessed March 30, 2020).
39. Charmaz K. Constructing Grounded Theory: A practical Guide Through Qualitative Analysis. London: Sage Publications (2006).
40. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. (2007) 19:349–57. doi: 10.1093/intqhc/mzm042
41. Furlong M, McGilloway S, Mulligan C, Killion MG, McGarr S, Grant A, et al. Covid-19 and Families With Parental Mental Illness: Crisis and Opportunity. Front Psychiatry. (2021) 12:567447. doi: 10.3389/fpsyt.2021.567447
42. Kelly BD. Impact of Covid-19 on mental health in Ireland: evidence to date. Ir Med J. (2020) 113:214. Available online at: http://imj.ie/wp-content/uploads/2020/12/Impact-of-Covid-19-on-Mental-Health-in-Ireland-Evidence-to-Date.pdf (accessed September 23, 2021).
43. Mental Health Foundation. The COVID-19 pandemic, Financial Inequality and Mental Health (2020). Available online at: https://www.mentalhealth.org.uk/our-work/research/coronavirus-mental-health-pandemic/covid-19-inequality-briefing (accessed September 5, 2021).
44. Quittkat HL, Dusing R, Holtmann FJ, Buhlmann U, Svaldi J, Vocks S. Perceived impact of Covid-19 across different mental disorders: a study on disorder-specific symptoms, psychosocial stress and behavior. Front Psychol. (2020) 11:586246. doi: 10.3389/fpsyg.2020.586246
45. Grant A, Goodyear M, Maybery D, Reupert A. Differences between Irish and Australian psychiatric nurses' family-focused practice in adult mental health services. Arch Psychiatr Nurs. (2016) 30:132–7. doi: 10.1016/j.apnu.2015.07.005
46. St Patrick's Mental Health Services. Attitudes to Mental Health Annual Survey. (2020). Available online at: https://www.stpatricks.ie/media/2941/attitudes-to-mental-health-survey-findings-2020-st-patricks-mental-health-services.pdf (accessed September 5, 2021).
47. Falkov A, Goodyear M, Hosman CM, Biebel K, Skogøy BE, Kowalenko N, et al. A systems approach to enhance global efforts to implement family-focused mental health interventions. Child Youth Serv. (2016) 37:175–93. doi: 10.1080/0145935X.2016.1104104
48. Maybery D, Goodyear M, Reupert A, Sheen J, Cann W, Dalziel K, et al. Developing an Australian-first recovery model for parents in Victorian mental health and family services: a study protocol for a randomised controlled trial. BMC Psychiatry. (2017) 17:1–7. doi: 10.1186/s12888-017-1357-4
49. Allchin B, O'Hanlon B, Weimand BM, Boyer F, Cripps G, Gill L, et al. An explanatory model of factors enabling sustainability of Let's Talk in an adult mental health service: a participatory case study. Int J Ment Health Syst. (2020) 14:1–6. doi: 10.1186/s13033-020-00380-9
50. Grant A, Lagson S, Devaney J, Davidson G, Duffy J, Perra O, et al. A Study of Health and Social Care Professionals' Family Focused Practice With Parents Who Have Mental Illness, Their Children and Families in Northern Ireland. (2018). Available online at: https://pureadmin.qub.ac.uk/ws/portalfiles/portal/154075911/Think_Family_Final_Long_Report_27.2.18_Final_Final.pdf (accessed September 5, 2021).
51. Marston N, Maybery D, Reupert A. Empowering families where a parent has a mental illness: a preliminary evaluation of the ‘family focus' DVD. Adv Ment Health. (2014) 12:136–46. doi: 10.1080/18374905.2014.11081891
52. Kamis C. The long-term impact of parental mental health on children's distress trajectories in adulthood. Soc Ment Health. (2021) 11:54–68. doi: 10.1177/2156869320912520
53. Wayman S. Mental Illness: Where Should Family Involvement Begin and End When a Parent Needs Treatment? (2021). Available online at: https://www.irishtimes.com/life-and-style/health-family/parenting/mental-illness-where-should-family-involvement-begin-and-end-when-a-parent-needs-treatment-1.4588412Irish~Times~15~June~2021 (accessed September 5, 2021).
54. Van Doesum KT, Riebschleger J, Carroll J, Grové C, Lauritzen C, Mordoch E, et al. Successful recruitment strategies for prevention programs targeting children of parents with mental health challenges: an international study. Child Youth Serv. (2016) 37:156–74. doi: 10.1080/0145935X.2016.1104075
55. Mental Health Reform. Pre-budget Submission. (2020). Available online at: https://www.mentalhealthreform.ie/wp-content/uploads/2019/07/Full-MHR-pre-budget-submission-2020_-FINAL.pdf (accessed September 5, 2021).
56. Cooklin A. “Mental health, mental illness, the family and others: How do we think about them together?” In: Cooklin A, Barnes GG, editors. Building Children's Resilience in the Face of Parental Mental Illness. London: Routledge (2020). p. 6–42.
57. Towey N. Covid-19 Vaccine Tracker: How Many People in Ireland Have Been Inoculated in Ireland? Available online at: https://www.irishtimes.com/news/health/covid-19-vaccine-tracker-how-many-people-have-been-inoculated-in-ireland-1.4481095#how%20many%20vaccinated~Irish~Times (accessed September 8, 2021).
Keywords: children, COPMI, Family Talk, mental health, mental disorder, mental illness, parents, qualitative research
Citation: Mulligan C, Furlong M, McGarr S, O'Connor S and McGilloway S (2021) The Family Talk Programme in Ireland: A Qualitative Analysis of the Experiences of Families With Parental Mental Illness. Front. Psychiatry 12:783189. doi: 10.3389/fpsyt.2021.783189
Received: 25 September 2021; Accepted: 22 October 2021;
Published: 15 November 2021.
Edited by:
Joanne Louise Riebschleger, Michigan State University, United StatesReviewed by:
Tariq Munshi, University of Toronto, CanadaJoanna Fox, Anglia Ruskin University, United Kingdom
Copyright © 2021 Mulligan, Furlong, McGarr, O'Connor and McGilloway. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mairead Furlong, TWFpcmVhZC5GdXJsb25nQG11Lmll
†These authors have contributed equally to this work and share first authorship
 Christine Mulligan
Christine Mulligan Mairead Furlong
Mairead Furlong Sharon McGarr
Sharon McGarr Siobhan O'Connor
Siobhan O'Connor