- 1Department of Psychiatry, Hunan Brain Hospital (Second People's Hospital of Hunan Province), Changsha, China
- 2Department of Psychiatry, National Clinical Research Center for Mental Disorders, The Second Xiangya Hospital of Central South University, Changsha, China
- 3Department of Psychological Sciences, College of Arts and Sciences, Texas Tech University, Lubbock, TX, United States
- 4Department of Cardiovascular Surgery, The Second Xiangya Hospital, Central South University, Changsha, China
Background: Doctor-patient relationship (DPR) is very important for patient outcomes, especially during a public health emergency like the COVID-19 pandemic. However, few studies have evaluated DPR and related sentiments from medical professionals' perspectives. Thus, the aim of the study is to provide a better understanding of DPR from medical professionals' perspectives during the COVID-19 pandemic in China.
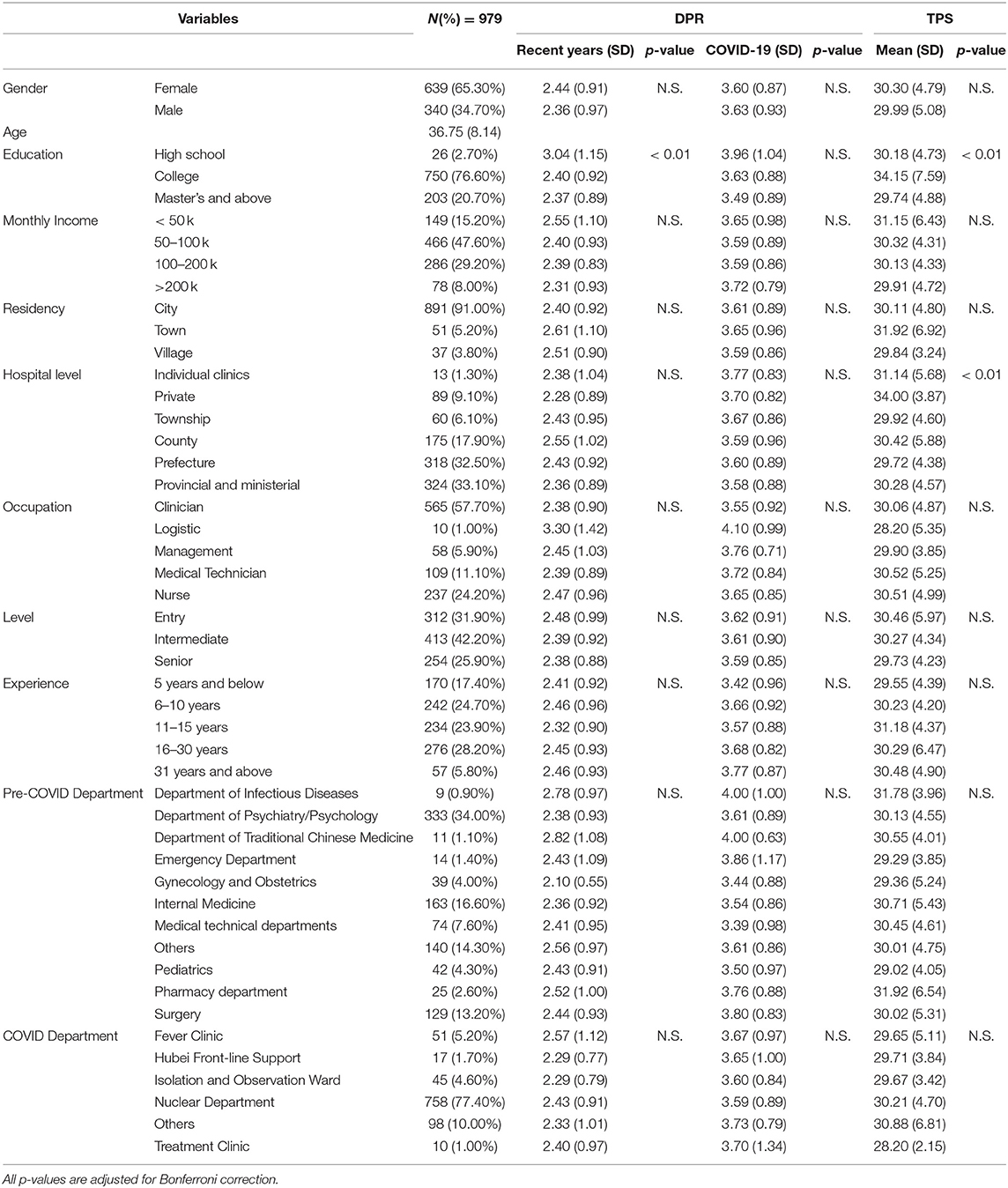
Methods: A total of 979 medical professionals, including doctors, nurses, technicians, and other workers have completed a series of questionnaires to evaluate their attitudes toward DPR, trust, violence against doctors, factors that affected and improved DPR, and the importance of these factors on DPR. Analyses of variances (ANOVA) and linear regressions were used to analyze the effects of the pandemic, demographic variables, and various elements on DPR.
Results: One-way ANOVA revealed a significant effect of education on recent DPR [F(2, 976) = 6.17, p < 0.001 and trust at F(2, 976) = 9.54, p < 0.001], indicating that individuals with higher level of education (bachelor's degree, Master's degree and above) showed poorer recent DPR and lower level of trust. The level of hospital also showed a significant effect on trust [F(5, 973) = 3.79, p = 0.0021]. Cochran's Q test revealed a significant difference in factors that affected [Q(11) = 3,997.83, p < 0.001] and improved [Q(8) = 3,304.53, p < 0.001] DPR. Backward stepwise linear regressions revealed predictors for changes during [F(9, 969) = 21.17, p < 0.001, R2 = 0.16], shortly after [F(7, 971) = 54.98, p < 0.001, R2 = 0.28], and long after [F(10, 968) = 37.83, p < 0.001, R2 = 0.29] the pandemic.
Conclusions: Medical professionals' perceptions of DPR is important as they provide basis for the improvement in working environment of medical professionals and hospital visiting experience of patients, as well as healthcare policy making and preparation for future public health emergencies.
Introduction
The year 2020 has experienced an international public health crisis, the pandemic of novel coronavirus disease 2019 (COVID-19). To date, the disease caused by SARS-Cov-2 has affected more than 70 countries worldwide (1). Due to its highly contagious nature (2), diverse clinical manifestations (3), and long incubation period (4), this pandemic poses a serious threat to human health. As a result, many other fields, such as public psychological health (5) and well-being (6), as well as medical systems (7–9), have been affected by this crisis. The doctor-patient relationship (DPR) is one of the affected aspect (10, 11).
DPR is important for good medical practice, as it influences compliance with treatment and shapes subjective perception about the doctor, patient, and medical services (12). During a health crisis like the COVID-19 pandemic, positive DPR is even more important as it directly influences the overall psychological and physical health of people. A recent study reported that people's confidence in medical services and satisfaction with healthcare information provided to the public directly affected the mental and psychological health of the public during the COVID-19 pandemic (13).
In China, the rapidly evolving pandemic has led to concerns in the entire health-care system and brought unprecedented challenges to DPR in China (14, 15). Many medical professionals were sent to the frontline in their counties or cities or were sent to Hubei province to meet the high and urgent demand for medical resources (16, 17). Overburdened hospitals and medical professionals were faced with a large influx of patients with COVID-19, affecting the routine care activities in the hospitals (18). Strict preventive strategies, such as physical distancing, face mask, and personal protective equipment to prevent virus transmission, created barriers to effective doctor-patient communication, eventually leading to a reduced trust in doctors and other healthcare workers (19). Moreover, given the lack of curative interventions, this time of uncertainty brought stress on both medical workers and patients (20), which might lead to the worsening of DPR.
Despite the negative impacts of COVID-19 on DPR, medical workers in China bravely rose to the challenge; many of them worked voluntarily at the frontline against the pandemic (21). Their professionalism affected society's perception of medical professionals and strengthened mutual trust and understanding between patients and medical workers (22–24), with many reports referring to medical professionals as heroes and praising their hard work through media, which in turn led to improvement of DPR. With the above factors affecting the DPR in China, the impact of the COVID-19 epidemic on China's DPR has led to heated debate (25).
As the COVID-19 pandemic is a health crisis, medical professionals shouldered the burden of great responsibility and heavy workload more painfully than most other groups (26). According to media reports, many Chinese medical professionals expressed that DPR has been significantly improved during the COVID-19 pandemic due to better patient compliance, as well as increased trust and respect from patients. A recent study reported improved DPR during the pandemic from the patients' perspective (27). However, quantitative empirical research on the perception of DPR among Chinese medical workers during the pandemic has not yet been carried out.
Therefore, in the present study, we used empirical investigation methods to examine the perception of DPR in Chinese medical workers. We also investigated factors predicting changes in DPR during the pandemic and approaches that could improve DPR. Based on previous literature, we hypothesized that medical workers might have a positive view of DPR during the pandemic; we also predicted that several factors such as communication, media, and understanding of medical work will be main predictors for DPR. Hopefully, this study will provide a forward-looking perspective for the influence of the crisis on DPR as well as key points for clinicians and even policy makers to help develop a more constructive and positive DPR.
Methods
Respondents
This is a cross-sectional, retrospective, anonymous study carried out between March 12 and March 30, 2020. In this online study, we used convenience and snowball sampling approaches to recruit respondents in China via advertisement posted on various websites and social media. The inclusion criteria were as follows: (1) aged 18 years and above, (2) engaged in medical works, (3) living in China, and (4) still working during the pandemic. Interested respondents were given a hyperlink to Questionnaire Star (https://www.wjx.cn), a professional website for surveys, with an ethics approved consent form in the first page. Respondents who provided consent via the electronic informed consent form were able to proceed to the demographic survey and the DPR questionnaire. This study was approved by the Ethics Committee of the Second Xiangya Hospital of Central South University (No. LYE2020041).
Measures
Socio-Demographics
Socio-demographic information, including age, gender, level of education, monthly income, residency, position, title, years of working, level of hospitals they work at, and the department they work at during the pandemic, was collected and recorded for all respondents.
General Perception of DPR
Respondents' general perception of DPR before and during the COVID-19 pandemic was assessed through a series of questions like “What do you think of the doctor-patient relationship in China in recent years/during the COVID-19 pandemic?” The answers were provided with the use of a 5-point Likert scale ranging from 1 (extremely adversarial) to 5 (very harmonious). Respondents were also asked about their views of the short-term and long-term trends of DPR changing after the pandemic. The answer of these two questions were also rated on a 5-point Likert scale ranging from 1 (significantly worsened) to 5 (significantly improved). Change in DPR was computed by taking the centering scores around the 0-point, followed by taking the difference between the DPR during the pandemic and before the pandemic. In other words, the score of 0 indicated no change in the perception of DPR, while scores above 0 indicated improvement in DPR, and scores below 0 indicated the worsening of DPR.
DPR Measured by DDPRQ-10
DPR from the doctor's perspective was assessed using Difficult Doctor-Patient Relationship Questionnaire (DDPRQ-10), which has been used for the assessment of DPR in emergency care (28), primary care (29), and many other previous studies in China (30, 31). It is a doctor-rated scale to assess the degree of difficulty in their communications with patients. The scale consists of 10 questions rated on a 6-point Likert scale ranging from 1 (not at all) to 6 (a great deal), with a total score ranging from 10 to 60 and higher scores indicating poorer DPR.
Doctor's Trust in Patients
We used the Physician Trust Scale (TPS) compiled and revised by Liu in 2016 (32) (with a Cronbach's alpha of 0.93 in the validation sample), which was derived from the Physician Trust in the Patient Scale (PTPS) developed by Thom et al. (33) to measure the degree of doctors' trust in patients. It consists of 10 questions that are rated on a 5-point Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). The total score is the sum of the scores of the 10 questions, which ranges from 10 to 50. Higher scores indicate greater trust of doctors in patients.
Perceived Respect and Trust Before and During COVID-19
Respondents' perceived respect and trust from patients (perceived patients' respect/trust) before and during the COVID-19 pandemic was assessed through questions such as “How much respect/trust does the patient have for your profession before/ during the pandemic?” Respondents' perceived respect and trust from most people other than their patients (perceived most people's respect/trust) were measured through questions such as “How much respect/trust does most other people have for your profession before/ during the pandemic?” Each respondent was supposed to answer a total of eight questions, which were rated on a 5-point Likert scale ranging from 1 (very disrespectful/distrustful) to 5 (very respectful/trustful).
Workplace Violence Before and During COVID-19
Violence experienced by the respondents were assessed through four questions rated on a binary (yes-no) scale. The questions were “Have you experienced verbal/physical violence before/during the pandemic?” and “Have your colleagues experienced verbal/physical violence before/during the pandemic?” From the questions, eight variants could be obtained. The changes in workplace violence were calculated by taking the difference before and during the COVID-19 pandemic, and then classified into four categories: higher level of violence, same level of violence, no violence, and lower level of violence.
Important Elements That Will Impact DPR During the Pandemic
For this part, respondents should rate 10 items regarding the importance of factors that might impact the DPR during the pandemic, for example, “positive media reports on medical workers, such as the praise for their volunteering in Wuhan or the frontline of other areas” and “the national policy to provide free treatment for patients diagnosed with and suspected of COVID-19 infection.” All the items were rated on a 4-point Likert Scale ranging from 1 (negative influence) to 4 (positive influence).
Factors That Could Affect and Improve DPR in General
For this part, respondents were supposed to select five from twelve or nine items that might affect or improve DPR. The pool of items included “medical knowledge,” “communication,” “medical insurance,” “medical technology,” and “hospital management.” These items did not specifically target the period around the COVID-19 pandemic; the respondents should give their answers on the basis of their experience in recent years. See Table 3 for details.
Data Quality Control
To ensure the quality of the data, we performed quality control to further exclude unreliable responses. In this process, we needed to make sure questionnaires with logic verification error were eliminated, respondents only completed their questionnaires once regardless of what device they used (e.g., mobile phone, computer), and the minimum response time must be more than 3 min. Finally, respondents must enter a verification code upon the submission of their final responses.
Statistical Analysis
One-way analysis of variance (ANOVA) was used to analyze the impact of ten respondent demographic variables with regard to DPR in recent years, DPR during the pandemic, and trust (see Table 1 for details), with each demographic variable as an independent variable and DPR and trust as dependent variables. The Bonferroni method was used for the correction of multiple comparisons in the ANOVAs, with the significance threshold set at p < 0.005. Post-hoc analyses for demographics were conducted using Tukey's test to find the variables that showed significant differences in the scores of DPR and trust. One-way ANOVA was also used to examine whether changes in workplace violence had an impact on DPR. The changes in workplace violence were used as an inter-subject variable, and the change in DPR was used as a dependent variable. Cochran's Q test was used to find factors that affected and improved DPR separately.
Three stepwise backward linear regression was used to analyze the important elements that affected DPR during the pandemic and might affect short-term and long-term DPR after the pandemic. Changes in respect, trust, verbal and physical violence, and other elements of DPR were used to predict DPR changes. In addition, change in DPR during the pandemic and the expected short-term change in DPR after the pandemic were also used as predictors for short-term and long-term DPR. All statistical significance levels were set at p < 0.05 (two-tailed) unless stated otherwise. All the data were analyzed with the use of R 4.0.3.
Results
Demographic Information
A total of 1,064 respondents completed the survey; 42 were excluded because of uncompleted questionnaire, another 32 were excluded because of responses that could not be logically verified by the platform, and 11 were excluded as their time of completion was shorter than the minimum time required, i.e., 3 min. The final sample consisted of 979 respondents, with a response rate of 92%. For the respondents included, the mean age was 36.75 years (SD = 8.14, range = 18–68 years), 65.30% were female (N = 639), 953 had a bachelor's degree or above (97.30%), and 891 lived in the urban area (91.00%). With regard to the level of hospital, respondents working in provincial hospitals accounted for the highest proportion (N = 324, 33.10%). Most of the respondents are clinicians (N = 565, 57.70%), and a large proportion of them held intermediate titles (N = 413, 42.20%). Other demographic characteristics are presented in Table 1.
DPR Before and During the COVID-19 Pandemic
In this study, we found that the Cronbach's alpha of DDPRQ-10 was 0.43 for data before the COVID-19 pandemic and 0.18 for data during the COVID-19 pandemic, indicating poor reliability of the DDPRQ-10 in this sample. Therefore, we used general DPR questions (recent-year DPR, DPR around the COVID-19 period) for the analyses instead.
One-way ANOVA revealed a significant effect of education on recent-year DPR [F(2, 976) = 6.17, p < 0.001, η2 = 0.012] after Bonferroni correction. No significant difference was found in other demographic variables for recent-year DPR. Tukey's post-hoc test revealed that compared to high school education (M = 0.039, SD = 1.15), respondents with bachelor's degree (M = −0.60, SD = 0.93, p = 0.0018), master's degree and above (M = −0.63, SD = 0.89, p = 0.0017) had a lower score in recent-year DPR (Figure 1).
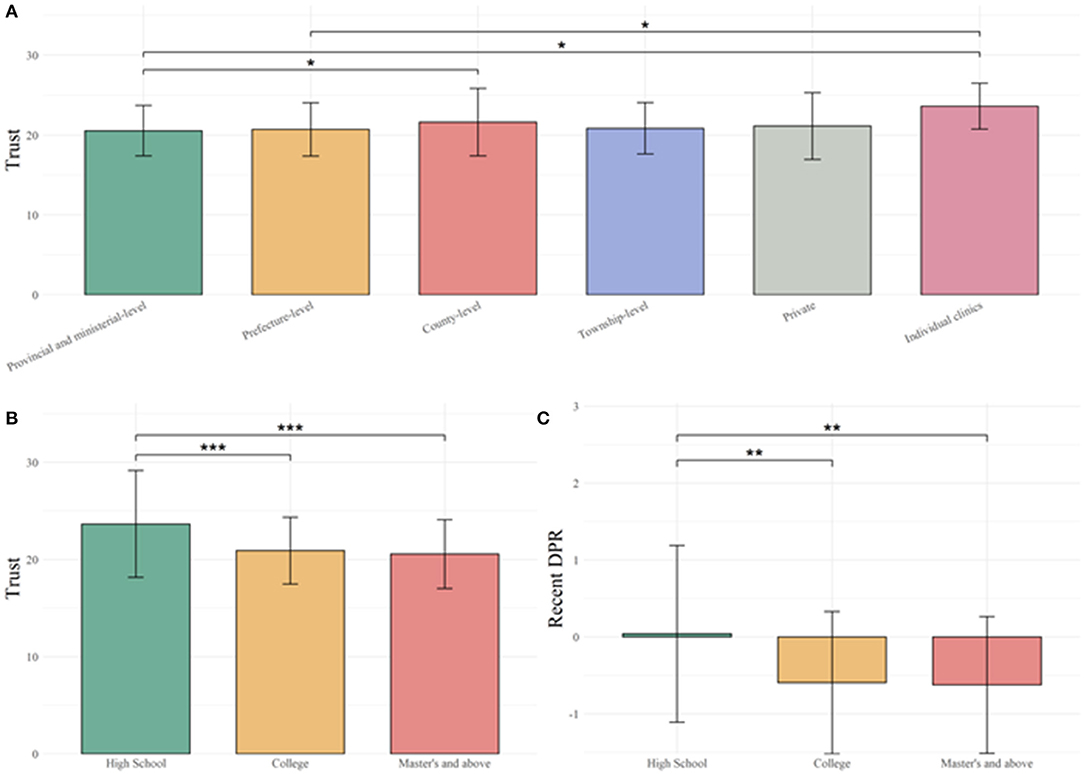
Figure 1. Change in perception of trust in medical services and doctor-patient relationship (DPR) before and during COVID-19. (A) Medical professionals working at prefecture-level and provincial and ministerial-level hospitals have lower trust in patients than those working in individual clinics. Furthermore, medical professionals working at provincial and ministerial-level hospitals have lower trust in patients than those working at county-level hospitals. (B) Medical professionals who have completed high school had higher trust in patients compared to those who have college or master's degree and above. (C) Medical professionals who have completed high school had positive change in DPR compared to medical professionals who have completed college or master's degree and above. * <0.05, ** <0.01, *** <0.001.
Medical Professionals' Trust in Patients During the COVID-19 Pandemic
The Cronbach's alpha of TPS was 0.74 for the total score, indicating that it was adequate for analysis. One-way ANOVA revealed a significant effect of education [F(2, 976) = 9.54, p < 0.001 η2 = 0.019] and the level of hospital [F(5, 973) = 3.79, p = 0.0021, η2 = 0.019] on trust in patients after Bonferroni correction. No significant difference was found in other demographic variables for trust. Tukey's post-hoc test for the level of hospital revealed that compared to provincial hospitals (M = 29.70, SD = 4.38), respondents who worked at county-level hospitals (M = 31.10, SD = 5.68, p = 0.022) and individual clinics (M = 34.00, SD = 3.87, p = 0.023) had higher levels of trust in their patients. And compared to respondents working at prefecture-level hospitals (M = 29.90, SD = 4.60), those working at individual clinics (p = 0.037) had higher levels of trust in their patients. Tukey's post-hoc test for education levels also showed that compared to high school education (M = 34.20, SD = 7.59), respondents with bachelor's degree (M = 30.20, SD = 4.73, p < 0.001), and master's degree and above (M = 29.7, SD = 4.88, p < 0.001) had lower trust in their patients (Figure 1).
Perceived Respect and Trust Before and During COVID-19
Mixed-factorial ANOVA revealed a main effect of perceived self-/other-trust [F(1, 3911) = 54.27, p < 0.001, η2 = 0.014] and timepoint [F(1, 3911) = 41.45, p < 0.001, η2 = 0.011]. However, no significant trust × timepoint interaction was found [F(1, 3911) = 0.55, p > 0.05]. It was also found that perceived other-trust (M = 3.66, SD = 0.64) was higher than perceived self-trust (M = 3.59, SD = 0.63). Perceived trust was greater during the COVID-19 pandemic (M = 3.75, SD = 0.64), as compared to that before the pandemic (M = 3.50, SD = 0.60).
Mixed-factorial ANOVA revealed a main effect of perceived self-/other-respect [F(1, 3911) = 225.56, p < 0.001, η2 = 0.058] and timepoint [F(1, 3911) = 88.71, p < 0.001, η2 = 0.023]. However, no significant perceived respect × timepoint interaction was found [F(1, 3911) = 2.87, p > 0.05]. Perceived other-respect (M = 3.50, SD = 0.64) was higher than perceived self-respect (M = 3.44, SD = 0.71); and perceived respect was greater during the COVID-19 pandemic (M = 3.69, SD = 0.67), as compared to that before the pandemic (M = 3.25, SD = 0.62).
Violence Against Doctors Before and During COVID-19
Respondents reported that verbal violence against them and their colleagues decreased by 56.68 and 82.80%, respectively, during the pandemic, and physical violence against them and their colleagues also decreased by 85.96 and 76.11%, respectively. One-way ANOVA revealed no significant effect of physical or verbal offenses toward the respondents or their colleagues on the DPR (Ps > 0.05).
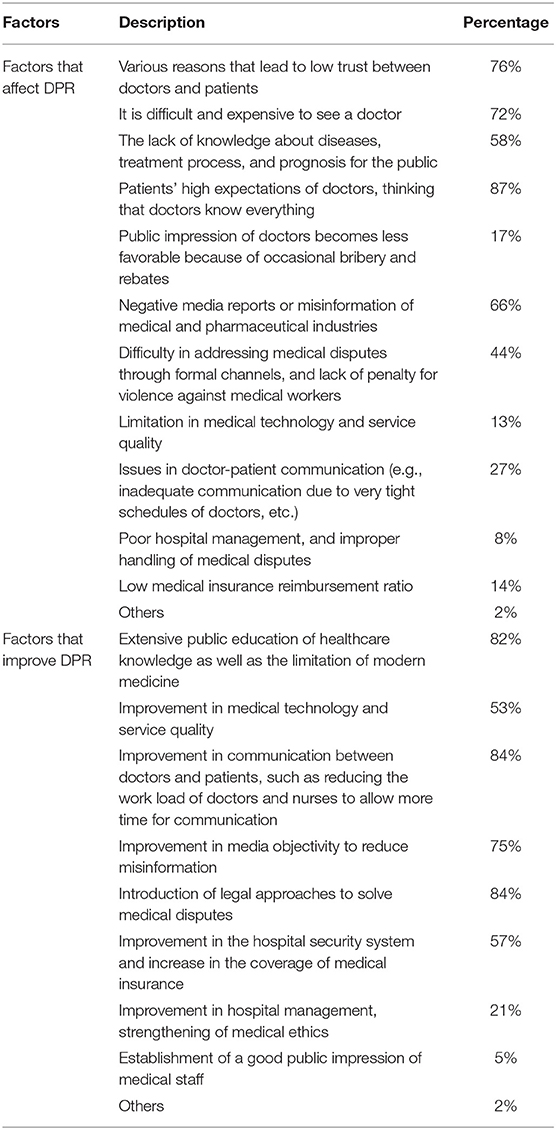
Factors That Affect and Improve DPR
Cochran's Q test revealed the significant factors that affected DPR [Q(11) = 3,997.83, p < 0.001]. The top five factors were high expectations for doctors and the opinion that doctors should know everything (87%), various causes of low mutual trust between doctors and patients (76%), patient's lack of knowledge (69%), negative reports or misinformation of medical and pharmaceutical industries by the media (66%), and difficulty in visiting a doctor and high cost for the consultation (58%).
Cochran's Q test revealed the significant factors that improved DPR [Q(8) = 3,304.53, p < 0.001]. The top five factors were the improvement of medical legislations (84%), good doctor-patient communication (84%), basic medical knowledge for patients (82%), media responsibility (75%), and medical insurance (57%). See Table 2 for details.
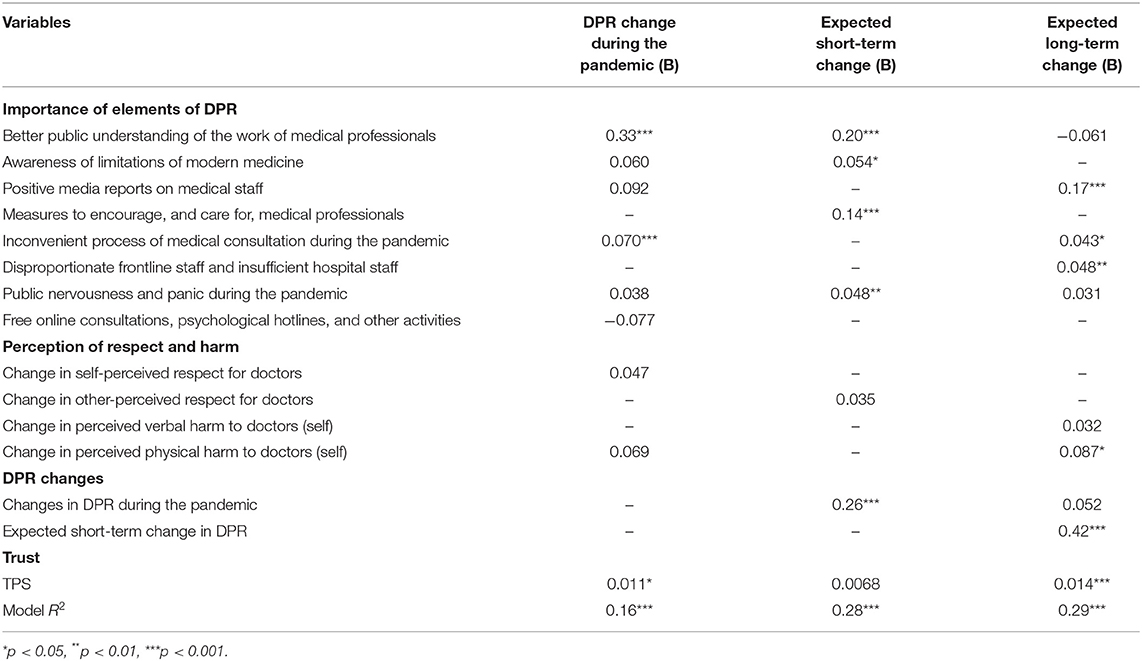
Factors Predicting Changes in DPR After the Pandemic
Backward stepwise linear regression for changes in DPR during the pandemic revealed a significant model at F(9, 969) = 21.17, p < 0.001, and R2 = 0.16. Better understanding of the work of medical professionals (B = 0.33, p < 0.001), inconvenience in medical consultation during the pandemic (B = 0.070, p < 0.001), and medical professionals' trust in patients (B = 0.011, p = 0.023) were found positively associated with the DPR during the pandemic.
Backward stepwise linear regression revealed a significant model for short-term DPR after the pandemic [F(7, 971) = 54.98, p < 0.001, R2 = 0.28]. Better understanding of the work of medical professionals (B = 0.20, p < 0.001), inconvenience in medical consultation during the pandemic (B = 0.054, p = 0.038), measures to encourage and care for medical professionals (B = 0.14, p < 0.001), public nervousness and panic during the pandemic (B = 0.048, p =0.0012), and change in DPR during the pandemic (B = 0.26, p < 0.001) were associated with higher expectation of short-term DPR in the future.
Backward stepwise linear regression revealed a significant model for expected long-term DPR after the pandemic [F(10, 968) = 37.83, p < 0.001, R2 = 0.29]. Positive media reports on medical staff (B = 0.17, p < 0.001), inconvenience in medical consultation during the pandemic (B = 0.043, p = 0.018), disproportionate frontline and insufficient hospital staff (B = 0.048, p = 0.011), medical professionals' trust in patients (B = 0.014, p < 0.001), change in perception of physical harm to doctors (self; B = 0.087, p = 0.012), and expected short-term DPR after the pandemic (B = 0.42, p < 0.001) were associated with higher expectation of long-term DPR in the future. Details are shown in Table 3.
Discussion
To our knowledge, this is the first quantitative empirical study on the perception of DPR among Chinese medical workers during the pandemic. This study revealed that Chinese medical workers were optimistic about the DPR during the COVID-19 outbreak. We also examined how their perceptions of DPR were impacted by multiple factors, such as demographic characteristics and changes in healthcare systems in response to the pandemic. In addition, several significant predictors for DPR after the pandemic were also found.
Consistent with the mainstream media report of doctor-patient interaction, the participants in the present study experienced a better DPR during the outbreak, reporting more respect and trust and less violence from the public, which supported our hypothesis that Chinese medical professionals might report improved DPR during the COVID-19 pandemic. In their fight against the virus, both medical workers and patients were supportive and understanding to each other (34). Meanwhile, medical workers have received national recognition and gained public support and respect during the outbreak, which further improved their image and social status (23, 35). Furthermore, policies were developed to provide incentives to medical workers and protect them in all aspects, including psychological health services, daily needs, work-related injury compensation, subsidies and allowances, etc. (36, 37). All of the above factors contributed to a better DPR perceived by Chinese medical workers.
Another finding was the differences in the influence of levels of education and hospitals on trust and DPR. Medical workers with higher level of education (bachelor's and master's degree) had lower trust and DPR than those who received only high school education. Similar results were found in other studies, where education is significantly and negatively correlated with trust and DPR (31, 38). The present study also found that medical workers from a higher level of hospital had lower trust in patients than those from a lower level hospital, which was consistent with another study that reported a substantial influence of the level of hospital on DPR from the doctor's perspective (39). A possible reason for this counterintuitive finding is that most highly educated doctors work in higher-level hospitals, which are usually associated with higher workloads (40), greater pressure, as well as more medical disputes (41). The potential stressors may result in decreased enthusiasm of medical staff and negative views toward DPR and trust (42).
Our study also identified some predictors of DPR over time from medical workers' perspective, including patients' understanding of medical professionals, patients' awareness of the limitation of modern medicine, patients being supportive to medical professionals, positive media report about medical staff, medical professionals' trust in patients, the reduction of physical and verbal violence against doctors, etc. Notably, patients' understanding of medical professionals was significantly positively correlated with perceived DPR during and shortly after the pandemic, which was in line with previous reports, which demonstrated the needs of medical professionals for public understanding of the challenges they faced (43). In the fight against the pandemic, medical workers in China faced tremendous stress, burnout, physical health risks, psychological health issues, etc. (44, 45). Through the outbreak, people began to realize the limitation of modern medicine, and began to empathize and support medical workers, which in turn encouraged the medical professionals in their works and improved their perception of DPR. Patients' basic health knowledge is also important (46), as it helps them understand the limitation of medicine and improve their communication with doctors (47). Factors predicting long-term DPR after the pandemic are also critical, as they influences the public opinion toward medical workers in the long run. For example, positive media report about medical staff and positive press coverage about doctors could potentially improve public trust in doctors (24, 47). In addition, our study found that previous perception of DPR is positively correlated with expected short-term DPR, which was found to be positively associated with long-term DPR. From this result, we can be optimistic about the DPR in the future despite the challenges medical workers are faced with. As DPR is changing gradually over time, the findings in our study might be hints for the development of public health policies on the basis of status quo.
Implications for Public Health
The results of this study have great implications for long-term development of policies and medical systems for future medical emergencies. First, our findings suggested that the image of medical professionals has been improved through the pandemic. Previously, due to various factors such as information asymmetry, some people in China might have an unfavorable impression of medical professionals in recent years (48). However, during the pandemic, the heroic deeds of medical professionals are seen and recognized by the public. Second, we also found that the management of healthcare resources and contingency plans are important for medical emergencies (49, 50). Strategic leadership, adaptiveness, communication, information transparency, responsibility, and the professionalism will significantly benefit everyone in the country during a public health emergency (49, 51, 52). The interconnected system through digital means, as well as technology used to aid management and treatment will boost the capability of medical system to provide interventions. This can also improve the trust in the medical system, leading to better DPR. Finally, the government should seek to improve the healthcare education for the public to narrow the knowledge gap between medical workers and the public. With better understanding of doctors' work, patients might be more compliant with their treatment (46), show more respect to and trust in their doctors (24, 47), which might lead to better DPR in the long run. Overall, the current COVID-19 crisis has affected DPR in a variety of aspects, and we need to utilize the opportunities brought about by the current health issue to improve the DPR.
Limitations
Despite the insights of our study, there are a few limitations. First, this is a retrospective study on medical professionals' perception of DPR before and during the pandemic. Therefore, it is difficult to make sure whether these factors will still be predictors in the future. A longitudinal study might be needed to identify predictors for long-term changes in DPR. Second, the reliability of the DDPRQ-10 was found to be poor in this study; thus, we needed to use general questions regarding DPR. Future works are needed to develop valid and reliable questionnaires for the assessment of the relationship between two parties. Finally, regarding expected short-term and long-term changes in DPR, we did not provide a definition of the two terms; therefore, the respondents may answer relevant questions based on their own perception. Despite these limitations, our study had enough power and sample size to identify important factors and predictors of DPR, which is of great importance in the public health and policy making in China.
Conclusions
DPR is important for patient outcomes, especially during a public health emergency such as the COVID-19 pandemic. Understanding DPR from the doctor's perspective is crucial for medical administration, hospital management, and patient care. Our study showed that Chinese medical workers were optimistic about DPR during the COVID-19 outbreak. Demographic characteristics such as education and the level of hospital they are working at were associated with DPR and trust. We also identified predictors for changes in DPR during the pandemic and in short term and long term after the pandemic. These factors have broad implications for policy making and medical resource management, and may help improve the medical system and doctor-patient relationship in the future.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committee of The Second Xiangya Hospital of Central South University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
The study was conceptualized by YZ and TL. The data was collected and organized by YZ. Data were analyzed and interpreted by YZ and WY. The manuscript was drafted by YZ and revised by TL, XW, DY, YM, and QW. All authors have read and approved the final manuscript.
Funding
This study was supported by the National Key R&D Program of China (2017YFC1310400), the Technology innovation guidance plan of Hunan province (2017SK50315), the Project of Hunan Health and Family Planning Commission (B20180484), and the Science and Technology Plan of Changsha City, Hunan Province (kq2004106).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. He F, Deng Y, Li W. Coronavirus disease 2019: what we know? J Med Virol. (2020) 92:719–25. doi: 10.1002/jmv.25766
2. Mrityunjaya M, Pavithra V, Neelam R, Janhavi P, Halami PM, Ravindra PV. Immune-boosting, antioxidant and anti-inflammatory food supplements targeting pathogenesis of COVID-19. Front Immunol. (2020) 11:570122. doi: 10.3389/fimmu.2020.570122
3. Jin X, Lian JS, Hu JH, Gao J, Zheng L, Zhang YM, et al. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (COVID-19) with gastrointestinal symptoms. Gut. (2020) 69:1002–9. doi: 10.1136/gutjnl-2020-320926
4. Duruk G, Gümüşboga Z, Çolak C. Investigation of Turkish dentists' clinical attitudes and behaviors towards the COVID-19 pandemic: a survey study. Braz Oral Res. (2020) 34:e054. doi: 10.1590/1807-3107bor-2020.vol34.0054
5. Zhang J, Lu H, Zeng H, Zhang S, Du Q, Jiang T, et al. The differential psychological distress of populations affected by the COVID-19 pandemic. Brain Behav Immun. (2020) 87:49–50. doi: 10.1016/j.bbi.2020.04.031
6. Leigh JP, Fiest K, Brundin-Mather R, Plotnikoff K, Soo A, Sypes EE, et al. A national cross-sectional survey of public perceptions of the COVID-19 pandemic: self-reported beliefs, knowledge, and behaviors. PLoS ONE. (2020) 15:e0241259. doi: 10.1371/journal.pone.0241259
7. Lucero-Prisno DE 3rd, Essar MY, Ahmadi A, Lin X, Adebisi YA. Conflict and COVID-19: a double burden for Afghanistan's healthcare system. Confl Health. (2020) 14:65. doi: 10.1186/s13031-020-00312-x
8. Yaghi S, Ishida K, Torres J, Mac Grory B, Raz E, Humbert K, et al. SARS-CoV-2 and stroke in a New York healthcare system. Stroke. (2020) 51:2002–11. doi: 10.1161/STROKEAHA.120.030335
9. Baiyewu O, Elugbadebo O, Oshodi Y. Burden of COVID-19 on mental health of older adults in a fragile healthcare system: the case of Nigeria: dealing with inequalities and inadequacies. Int Psychogeriatr. (2020) 32:1181–5. doi: 10.1017/S1041610220001726
10. Vallelonga F, Elia F. Doctor-patient relationship at the time of COVID-19: travel notes. Intens Care Med. (2020) 46:1802. doi: 10.1007/s00134-020-06152-w
11. Simpson KJ, Porter BR. The new normal: patient-physician relationships during COVID-19. Metodist Debakey Cardiovasc J. (2020) 16:181–2. doi: 10.14797/mdcj-16-2-181
12. Banerjee A, Sanyal D. Dynamics of doctor-patient relationship: a cross-sectional study on concordance, trust, and patient enablement. J Family Community Med. (2012) 19:12–9. doi: 10.4103/2230-8229.94006
13. Wang C, Pan R, Wan X, Tan Y, Xu L, McIntyre RS, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. (2020) 87:40–8. doi: 10.1016/j.bbi.2020.04.028
14. Sun S, Xie Z, Yu K, Jiang B, Zheng S, Pan X. COVID-19 and healthcare system in China: challenges and progression for a sustainable future. Global Health. (2021) 17:14. doi: 10.1186/s12992-021-00665-9
15. Li H, Zhang Z, Li P, Nie H. Challenges and responses: a tertiary hospital in 2019-nCoV epidemic. Disaster Med Public Health Prep. (2020) 14:808–11. doi: 10.1017/dmp.2020.93
16. Xie L, Yang H, Zheng X, Wu Y, Lin X, Shen Z. Medical resources and coronavirus disease (COVID-19) mortality rate: evidence and implications from Hubei province in China. PLoS ONE. (2021) 16:e0244867. doi: 10.1371/journal.pone.0244867
17. Wang X, Zhang X, He J. Challenges to the system of reserve medical supplies for public health emergencies: reflections on the outbreak of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic in China. Biosci Trends. (2020) 14:3–8. doi: 10.5582/bst.2020.01043
18. Shanthanna H, Strand NH, Provenzano DA, Lobo CA, Eldabe S, Bhatia A, et al. Caring for patients with pain during the COVID-19 pandemic: consensus recommendations from an international expert panel. Anaesthesia. (2020) 75:935–44. doi: 10.1111/anae.15076
19. Ghosh A, Sharma K, Choudhury S. COVID-19 and physician-patient relationship: potential effects of 'masking', 'distancing' and 'others'. Fam Pract. (2021) 38:193–4. doi: 10.1093/fampra/cmaa092
20. Luo M, Guo L, Yu M, Jiang W, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public - a systematic review and meta-analysis. Psychiatry Res. (2020) 291:113190. doi: 10.1016/j.psychres.2020.113190
21. Health News. The White Coat Went Out to Battle. (2020). Available online at: http://szb.jkb.com.cn/jkbpaper/html/2020-03/12/node_3.htm (accessed March 12, 2020).
22. Shi W, Jiao Y. The COVID-19 pandemic: a live class on medical professionalism. QJM. (2020). doi: 10.1093/qjmed/hcaa157. [Epub ahead of print].
23. Jiang L, Broome ME, Ning C. The performance and professionalism of nurses in the fight against the new outbreak of COVID-19 epidemic is laudable. Int J Nurs Stud. (2020) 107:103578. doi: 10.1016/j.ijnurstu.2020.103578
24. Gan Y, Chen Y, Wang C, Latkin C, Hall BJ. The fight against COVID-19 and the restoration of trust in Chinese medical professionals. Asian J Psychiatr. (2020) 51:102072. doi: 10.1016/j.ajp.2020.102072
25. Gao B, Dong J. Does the impact of COVID-19 improve the doctor-patient relationship in China? Am J Med Sci. (2020) 360:305–6. doi: 10.1016/j.amjms.2020.05.039
26. Du J, Mayer G, Hummel S, Oetjen N, Gronewold N, Zafar A, et al. Mental health burden in different professions during the final stage of the COVID-19 lockdown in China: cross-sectional survey study. J Med Internet Res. (2020) 22:e24240. doi: 10.2196/24240
27. Zhou Y, Chen S, Liao Y, Wu Q, Ma Y, Wang D, et al. General perception of doctor–patient relationship from patients during the COVID-19 pandemic in China: a cross-sectional study. Front Public Health. (2021) 9:836. doi: 10.3389/fpubh.2021.646486
28. Maunder RG, Panzer A, Viljoen M, Owen J, Human S, Hunter JJ. Physicians' difficulty with emergency department patients is related to patients' attachment style. Soc Sci Med. (2006) 63:552–62. doi: 10.1016/j.socscimed.2006.01.001
29. Hahn SR. Physical symptoms and physician-experienced difficulty in the physician-patient relationship. Ann Intern Med. (2001) 134:897–904. doi: 10.7326/0003-4819-134-9_Part_2-200105011-00014
30. Wu H, Zhao X, Fritzsche K, Leonhart R, Schaefert R, Sun X, et al. Quality of doctor-patient relationship in patients with high somatic symptom severity in China. Complement Ther Med. (2015) 23:23–31. doi: 10.1016/j.ctim.2014.12.006
31. Qiao T, Fan Y, Geater AF, Chongsuvivatwong V, McNeil EB. Factors associated with the doctor-patient relationship: doctor and patient perspectives in hospital outpatient clinics of Inner Mongolia Autonomous Region, China. Patient Prefer Adherence. (2019) 13:1125–43. doi: 10.2147/PPA.S189345
32. Liu J. Study on the Influencing Factors of Doctor-Patient Trust in Kunhua Hospital of Yunnan Province (Master). Kunming University of Science and Technology (2016).
33. Thom DH, Wong ST, Guzman D, Wu A, Penko J, Miaskowski C, et al. Physician trust in the patient: development and validation of a new measure. Ann Fam Med. (2011) 9:148–54. doi: 10.1370/afm.1224
34. Xinhuanet. Noah's Ark. The Story of Fangcang Shelter Hospitals. (2020). Available online at: http://www.xinhuanet.com/2020-02/19/c_1125598560.htm (accessed February 19, 2020).
35. Xiang Y-T, Jin Y, Wang Y, Zhang Q, Zhang L, Cheung T. Tribute to health workers in China: A group of respectable population during the outbreak of the COVID-19. Int J Biol Sci. (2020) 16:1739. doi: 10.7150/ijbs.45135
36. Xinhua News. Measures Being Implemented to Care for Medics Across China: Official. (2020). Available online at: http://en.nhc.gov.cn/2020-03/09/c_77525.htm (accessed March 9, 2020).
37. China Daily. New Safety Rules for Medics Rolled Out. (2020). Available online at: https://www.chinadaily.com.cn/a/202002/15/WS5e46fde4a310128217277b53.html (accessed February 15, 2020).
38. Sun J, Zhang L, Sun R, Jiang Y, Chen X, He C, et al. Exploring the influence of resiliency on physician trust in patients: an empirical study of Chinese incidents. PLoS ONE. (2018) 13:e0207394. doi: 10.1371/journal.pone.0207394
39. Liu L, Xie Z, Qiu Z. Doctor-patient relationship in different level hospitals and influencing factors from doctor side. Med Phil. (2009) 30:30–1, 36.
40. Wen J, Cheng Y, Hu X, Yuan P, Hao T, Shi Y. Workload, burnout, and medical mistakes among physicians in China: a cross-sectional study. Biosci Trends. (2016) 10:27–33. doi: 10.5582/bst.2015.01175
41. He AJ, Qian J. Explaining medical disputes in Chinese public hospitals: the doctor–patient relationship and its implications for health policy reforms. Health Econ Policy Law. (2016) 11:359–78. doi: 10.1017/S1744133116000128
42. Liu S, Hu L, Wu S, Liu Y. What influences doctors' perceptions of the doctor-patient relationship? - A National Cross-Sectional Study in China. Res Square. (2020). doi: 10.21203/rs.3.rs-34404/v1. [Epub ahead of print].
43. Adams JG, Walls RM. Supporting the health care workforce during the COVID-19 global epidemic. JAMA. (2020) 323:1439–40. doi: 10.1001/jama.2020.3972
44. Dewey C, Hingle S, Goelz E, Linzer M. Supporting clinicians during the COVID-19 pandemic. Ann Intern Med. (2020) 172:752–3. doi: 10.7326/M20-1033
45. Shanafelt T, Ripp J, Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. (2020) 323:2133–4. doi: 10.1001/jama.2020.5893
46. Miller TA. Health literacy and adherence to medical treatment in chronic and acute illness: a meta-analysis. Patient Educ Couns. (2016) 99:1079–86. doi: 10.1016/j.pec.2016.01.020
47. Sun J, Liu S, Liu Q, Wang Z, Wang J, Hu CJ, et al. Impact of adverse media reporting on public perceptions of the doctor-patient relationship in China: an analysis with propensity score matching method. BMJ Open. (2018) 8:e022455. doi: 10.1136/bmjopen-2018-022455
48. Chen J, Zhou MY, Liu QY, Ye L, Cheng YR, Wang MW, et al. High time for ease the doctor-patient relationship in China. J Forensic Leg Med. (2020) 72:101961. doi: 10.1016/j.jflm.2020.101961
49. Shaker MS, Oppenheimer J, Grayson M, Stukus D, Hartog N, Hsieh EWY, et al. COVID-19: pandemic contingency planning for the allergy and immunology clinic. J Allergy Clin Immunol Pract. (2020) 8:1477–88.e1475. doi: 10.1016/j.jaip.2020.03.012
50. Xu W, Wu J, Cao L. COVID-19 pandemic in China: context, experience and lessons. Health Policy Technol. (2020) 9:639–48. doi: 10.1016/j.hlpt.2020.08.006
51. Malecki KMC, Keating JA, Safdar N. Crisis communication and public perception of COVID-19 risk in the era of social media. Clin Infect Dis. (2021) 72:697–702. doi: 10.1093/cid/ciaa758
Keywords: COVID-19, doctor-patient relationship, public education, media reports, medical resources, communication
Citation: Zhou Y, Yang WFZ, Ma Y, Wu Q, Yang D, Liu T and Wu X (2021) Doctor-Patient Relationship in the Eyes of Medical Professionals in China During the COVID-19 Pandemic: A Cross-Sectional Study. Front. Psychiatry 12:768089. doi: 10.3389/fpsyt.2021.768089
Received: 31 August 2021; Accepted: 04 October 2021;
Published: 28 October 2021.
Edited by:
Bin Zhang, Southern Medical University, ChinaReviewed by:
Ni Fan, Brain Hospital of Guangzhou Medical University, ChinaManli Huang, Zhejiang University, China
Copyright © 2021 Zhou, Yang, Ma, Wu, Yang, Liu and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tieqiao Liu, bGl1dGllcWlhbzEyM0Bjc3UuZWR1LmNu; Xiaoming Wu, MTc4MjAyMDkyQGNzdS5lZHUuY24=
 Yanan Zhou
Yanan Zhou Winson Fu Zun Yang
Winson Fu Zun Yang Yuejiao Ma
Yuejiao Ma Qiuxia Wu
Qiuxia Wu Dong Yang1
Dong Yang1 Tieqiao Liu
Tieqiao Liu