
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
PERSPECTIVE article
Front. Psychiatry, 24 November 2021
Sec. Sleep Disorders
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.767760
This article is part of the Research TopicSleep and Psychological Trauma or StressView all 10 articles
Sleep disturbances frequently co-occur with posttraumatic stress disorder (PTSD). Insomnia and nightmares are viewed as core symptoms of PTSD. Yet, relations between disturbed sleep and PTSD are far more complex: PTSD is linked to a broad range of sleep disorders and disturbed sleep markedly affects PTSD-outcome. This article provides a concise overview of the literature on prevalent comorbid sleep disorders, their reciprocal relation with PTSD and possible underlying neurophysiological mechanisms. Furthermore, diagnostic procedures, standard interventions—particularly first choice non-pharmacological therapies—and practical problems that often arise in the assessment and treatment of sleep disturbances in PTSD are described. Finally, we will present some perspectives on future multidisciplinary clinical and experimental research to develop new, more effective sleep therapies to improve both sleep and PTSD.
Sleep disturbances frequently occur in posttraumatic stress disorder (PTSD) and are reported by 70–90% of patients (1). Nightmares (intrusions) and difficulties sleeping (hyperarousal) are specifically included in the diagnostic (DSM-5) criteria of the disorder (2). In addition, various other sleep disorders are common in PTSD [e.g., (3, 4)]. It has long been thought that interventions focusing on trauma itself would eventually reduce disturbed sleep, but accumulating evidence shows that sleep disorders play a central role in both the development and maintenance of PTSD [e.g., (5, 6)] and therefore require particular clinical attention.
In this paper we provide an overview of prevalent sleep disorders in PTSD, the reciprocal association of sleep disturbances and PTSD and its underlying mechanisms, as well as information on accurate assessment and treatment of disturbed sleep tailored to the PTSD patient population. Finally, our perspectives for future research directed at more effective sleep-targeted interventions and integrated treatment strategies are described. Our aim is to enhance awareness of clinical practitioners of the importance of targeting sleep in PTSD treatment.
The majority of patients with PTSD, about 50–70%, suffer from recurrent distressing nightmares (see Table 1 for an overview of the most frequently occurring sleep disorders in PTSD, their characteristics, ways of assessment and treatment). These can be exact replications or more symbolic representations of traumatic experiences, and primarily occur during rapid eye movement sleep (REMS) (7). Insomnia symptoms, reported by ~70% of patients (8), are often related to increased autonomic arousal and fear of sleep: fear of loss of control and/or of having nightmares (9, 10). PTSD is also associated with obstructive sleep apnea (OSA), concerning 40–90% of PTSD patients (11). The repeated OSA events lead to frequent oxygen desaturations and arousals. Insomnia, nightmares and OSA may trigger and exacerbate each other, forming a vicious cycle (1, 4). In addition, multiple studies found a high proportion (around 33%) of periodic limb movement disorder (PLMD) in PTSD patients (12). The limb movements during sleep are associated with arousals/awakenings. Also relatively prevalent in PTSD are periods of sleep paralysis, typically occurring during (REM) sleep-wake transitions, which are often accompanied by distressing experiences, referred to as hypnagogic or hypnopompic hallucinations (13). Although the exact frequency is unclear, PTSD is also linked to remarkable disruptive nocturnal behaviors, including abnormal vocalizations and complex body movements. These parasomnias are generally thought to occur during non-REMS (confusional arousals, night terrors, sleepwalking), but may also take place during REMS, implying REMS behavior disorder (RBD)-like periods of REMS without the usual muscle atonia (RWA) with dream enactment. Mysliwiec et al. (14) proposed a distinct trauma-associated sleep disorder (TASD), conceptualized as a parasomnia encompassing nightmares, disruptive nocturnal behaviors as well as RWA [see (15) for an illustrative case study]. In support of this idea, a recent study in a large sample of veterans found self-reported dream enactment in nearly 40%. However polysomnography (PSG) showed no RWA in 80% of this group, indicating a non-REMS parasomnia, rather than a REMS phenomenon (16). Furthermore, in those veterans with RWA, RBD appeared related to PTSD (prevalence rate 15%) and even more so to the combination of PTSD and traumatic brain injury (prevalence rate 21%). Therefore, it is still controversial whether TASD really represents a separate sleep disorder (17, 18).
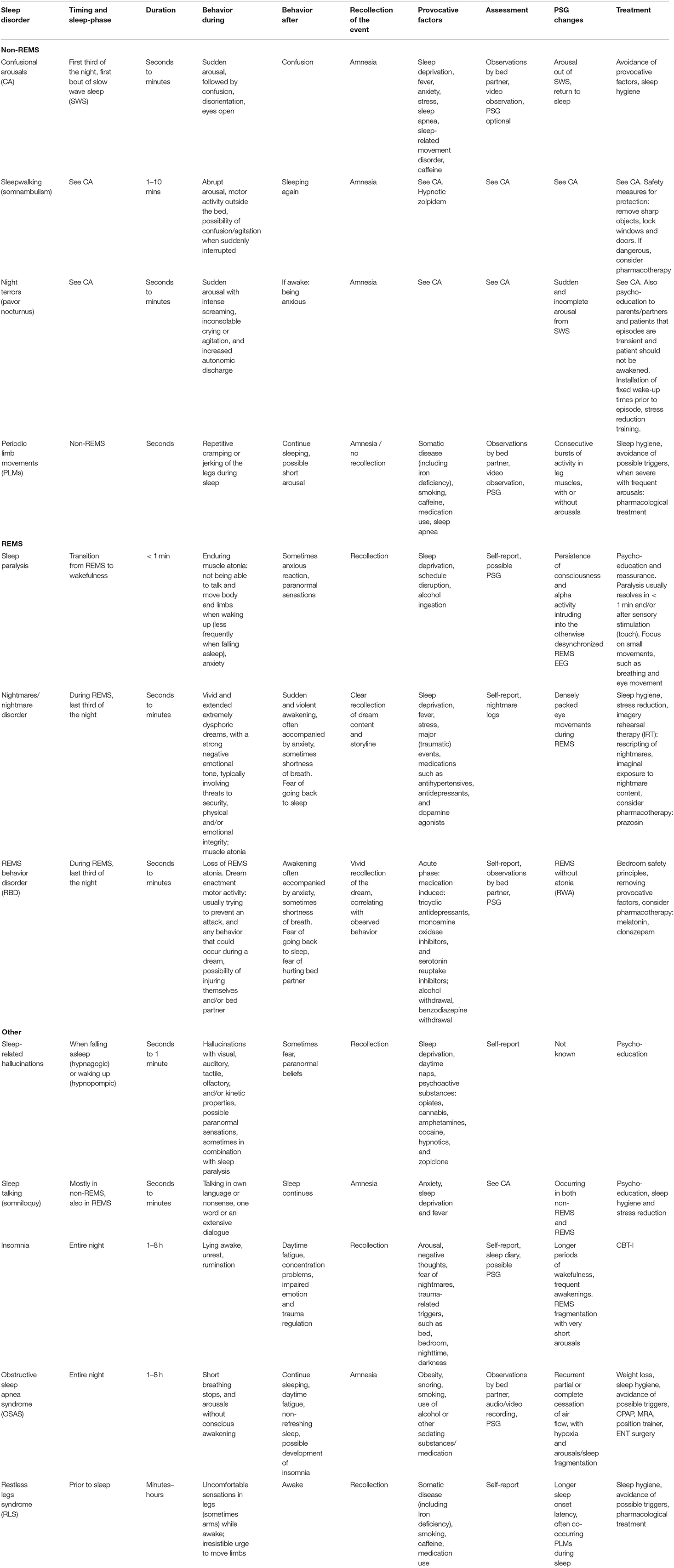
Table 1. Overview of frequently occurring sleep disorders in PTSD: characteristics, assessment and treatments.
Research strongly indicates that disturbed sleep is not merely a symptom or consequence of PTSD, but constitutes a predisposing, precipitating and perpetuating factor for PTSD. Sleep disturbances prior to and/or shortly after trauma increase the risk for PTSD (5, 12). For instance, in patients admitted to an emergency department after a motor vehicle collision both pre-trauma insomnia and nightmares predicted subsequent PTSD development (19). Furthermore, sleep disturbances affect the clinical course of PTSD: poor sleep quality is associated with reduced responsiveness to trauma-focused therapy [e.g., (20, 21)], while interventions targeting insomnia, nightmares or OSA improve sleep quality and ameliorate daytime PTSD symptoms (22). For example, Kanady et al. (9) observed that cognitive behavioral treatment of insomnia (CBT-I) in patients with PTSD and insomnia significantly decreased hypervigilance as well as PTSD symptom severity, and both were related to persistent reductions in fear of sleep. Moreover, sleep disturbances often persist after trauma-focused therapy (10). For example, Walters et al. (23) recently showed that prolonged exposure therapy improved daytime PTSD symptoms, but did not ameliorate insomnia and nightmares in veterans with PTSD. Residual insomnia has been shown to be an important risk factor for the development of and relapse in diverse mental disorders [e.g., (24)].
The reciprocal relations between sleep disturbances and PTSD suggest that disturbed sleep constitutes a causal factor in PTSD (25, 26). This causality is partly based on sleep's role in memory consolidation and emotion regulation (27, 28). While memory consolidation takes place during both slow wave sleep (SWS; deep non-REMS) and REMS, the processing of emotional memories is thought to happen primarily during REMS (29). In PTSD, traumatic memories arise in part from a failure in extinction learning, i.e., learning that the previously conditioned stimulus no longer represents a threat (30, 31). It is postulated that REMS disturbances, resulting from the noradrenergic hyperactivation typical of PTSD, hamper the consolidation of extinction memory, leading to a failure of the extinction memory to persist and generalize (32). So far the experimental support for this idea is limited, but nonetheless growing. Sleep disturbances following a traumatic event, including fragmented REMS, predict the development of PTSD (33–35). In polysomnographic studies, PTSD is characterized by reduced SWS and increased REM density (36, 37) as well as REMS fragmentation (38). These characteristics may well result from increased noradrenergic tone during (REM) sleep in PTSD patients (39, 40). Focusing on the role of sleep in the treatment of PTSD, a recent study found that the level of SWS and REM density positively predict treatment outcome (41). This and other clinical studies point toward an additional role of non-REMS disturbances, particularly a shortage of SWS, in the development and perpetuation of PTSD. Furthermore, shared neuromodulatory pathways may also underlie the relationship between PTSD and disturbed sleep. Especially (hyperactive) noradrenergic projections from the locus coeruleus (LC), as part of both the sleep-wake and PTSD-related circuitry, could form a final common pathway in generating the state of hyperarousal typical for both PTSD and disturbed sleep (32). Insomnia (42), nightmares (26) and most other sleep disorders discussed in this perspective are characterized by hyperarousal, frequent disruptions in REMS and aberrant LC-firing. In case of OSA, trauma-related hyperarousal may promote sleep disordered breathing (43). Vice versa, untreated OSA may contribute to development of PTSD, being a continuous stressor leading to sympathetic overactivity and disruption of sleep (44). As OSA events often occur during REMS, it is the brain's capacity to process negative emotions during REMS that is most likely affected.
Sleep disturbances can be screened and assessed with a clinical interview and objectified with other measures such as actigraphy and PSG. An actigraph and/or smartwatch can be helpful in detecting nightly arousals and limb movements, as well as daily rhythms in sleep and activity, and estimating sleep onset latency, total sleep time and sleep efficiency (45). PSG (with/without overnight video recording) provides an accurate picture of multiple physiological parameters related to sleep and wakefulness. PSG is less suitable as a screening tool, because it is an elaborate measurement which might not be readily accessible and financially feasible.
For an accurate diagnosis of PTSD according to DSM-5 criteria (2), the Clinician Administered PTSD Scale (CAPS-5) (46) can be used. It is a structured interview to diagnose current and life-time PTSD. However, the CAPS-5 is not sufficient for assessing the presence of sleep disorders, as it contains only two questions regarding sleep problems, considering nightmares and sleep disturbance in general. Diagnoses of sleep disorders are easily missed if specific diagnostic criteria are not inquired about. Therefore an accurate clinical assessment according to the International Classification of Sleep Disorders 3 (ICSD-3) (47) of sleep history, present sleep quality, sleep-wake behavior (preferably including information from the bedpartner to get a more accurate report of nightly behaviors) and screening for sleep disorders is essential.
We recommend an extensive clinical interview as there is no comprehensive questionnaire for screening diverse sleep disturbances in PTSD available. The diagnostic procedure should include an assessment of daily routines, diet, substance (ab)use, medication, mental state, presence of diseases and/or pain (or other physical limitations that compromise sleep), activity levels during night and day, and sleep behaviors including fear of sleep (10) [see (48) for a comprehensive review of the assessment and treatment guidelines of insomnia].
In PTSD the following events should be evaluated. (1) Presence of trauma-related triggers associated with sleep, the bedroom, nighttime and/or darkness, as these triggers might maintain a high arousal level, thereby hampering sleep onset and sleep maintenance. (2) Evaluation of circadian rhythm sleep-wake disorders in (uniformed) personnel working irregular hours (military personnel, police officers, fire-fighters, first responders). (3) Presence of parasomnias and distinguishing the different parasomnias, which is important for psychoeducation as well as treatment indication. For the detection of nightmares, which occur primarily during REMS, screening questionnaires such as the Nightmare Disorder Index (NDI) might be useful (49). However, both patients with PTSD and clinicians tend to misinterpret all nightly behaviors/experiences as nightmares. As the NDI does not cover other parasomnias, the clinician should always ask further about the experiences. Non-REMS parasomnias, such as confusional arousals, night terrors and sleepwalking, are often misdiagnosed as nightmares. Experiences during non-REMS parasomnias are generally not remembered well. The associated emotional distress can therefore be different from nightmares that are typically remembered vividly. It is important to ask patients to describe their nightmares in detail: What is the story in the dream? Is this trauma-related or more symbolic? What is the emotional intensity? Other parasomnias, such as sleep paralysis with or without hypnagogic and/or hypnopompic hallucinations, can be distressing, but they are not the same as nightmares. (4) Patient and bedpartner need to be asked about snoring, breathing stops, arousals and other symptoms to screen for OSA. One should take into account that the usually reported excessive daytime sleepiness is often not experienced by PTSD patients with OSA, possibly due to hyperarousal, yielding low scores on a screening questionnaire such as the Epworth Sleepiness Scale (50). An overnight audio-recording can be a useful tool to screen for sleep-related breathing problems. However, a PSG is the most objective measurement to assess OSA and its severity (51). (5) Patients and bedpartner can be asked about movements during sleep, and if present these movements can be objectified and interpreted with video-assisted PSG.
With or without PTSD, non-pharmacological interventions are first choice in the treatment of insomnia, nightmares and other (non-REMS) parasomnias (48, 52–54). In line with this, a recent meta-analysis on studies in PTSD patients found that PTSD symptoms and sleep both improve across all PTSD and sleep treatments. Yet, sleep improved the most after sleep-focused interventions, especially psychotherapy approaches (55).
For insomnia CBT-I has shown the most evidence of efficacy (56). CBT-I consists of several therapeutic components targeting different aspects of the sleep disorder: psychoeducation about sleep and sleep hygiene, relaxation training, behavioral interventions such as stimulus control (focus on re-connection of bed/bedroom with sleep) and sleep restriction (focus on reduction of time in bed to total sleep time), and cognitive therapy (48). Drawn from clinical experience and the cognitive behavioral model of PTSD, the following interventions within CBT-I require specific attention in PTSD: relaxation training because of hyperarousal (57); treatment of trauma-related triggers associated with sleep, the bed and/or bedroom, with exposure in vivo, EMDR and/or cognitive therapy. Furthermore, other interventions promoting the feeling of safety, such as a photograph of a loved one next to the bed, sleeping with a dim light, soothing music or white noise can be helpful. An increasing number of studies in patients with both PTSD and insomnia show positive effects of CBT-I on sleep efficiency, time awake after sleep onset, self-reported insomnia severity and fear of sleep (58). Another practice based intervention is the use of weighted blankets, some patients benefit from it. It is a simple non-invasive intervention and a first trial shows promising results (59). However, the presence of OSA is a contra-indication.
If nightmares are particularly prominent and perpetuate fear of sleep and insomnia, one can decide to treat nightmares before starting trauma-focused therapy. Most evidence is found for imagery rehearsal therapy, a technique for rescripting the nightmare story toward a better ending (60). The new dream is subsequently rehearsed through imagination. Imaginal exposure to the nightmare story is another effective, however, less studied intervention (53). There are no studies on EMDR for nightmares, even though it can be argued that desensitization of the nightmare image might be helpful.
If the patient has night terror-induced arousals, the bedpartner can sooth the patient with a soft and low voice, directing him/her back to bed and to sleep. Do not force awakening, ensure safety and trust that the patient will have no recollection of the event. If the arousals occur often and generally at the same time of the night it can be helpful to awaken the patient 15–30 mins before the expected arousal to prevent its occurrence (61).
Continuous positive airway pressure (CPAP) and mandibular repositioning appliance (MRA) can be used, and show most evidence in the treatment of OSA syndrome. CPAP has been shown to successfully reduce PTSD symptoms, including nightmare frequency, possibly by stabilizing the arousal system (43). In veterans with subclinical PTSD, non-compliance to CPAP therapy leads to increased PTSD symptoms, implying that optimal OSA-treatment prevents progression to clinical PTSD (44). If OSA-treatment adherence, e.g., wearing a CPAP-mask or MRA, is complicated by trauma-related anxiety, this needs to be specifically addressed, for example with cognitive therapy or EMDR. Other treatment options may be considered, such as weight reduction.
There is no guideline available for the timing of sleep-targeted interventions in PTSD in relation to trauma-focused therapy. Because of the reciprocal relation between PTSD and sleep disturbances one can argue that the sequence of interventions should be determined by the most prominent symptoms. Moreover, regarding the heterogeneity of PTSD symptoms, it is unlikely that a “one size fits all” treatment will be found. Therefore, we recommend focusing the treatment on the most distressing symptoms and/or administer two different treatments, e.g., EMDR for PTSD and CBT-I for sleep disturbances, side by side. Through monitoring the treatment process, the treatment plan can be adjusted when necessary.
Several types of drugs have been specifically evaluated in PTSD-related sleep disorders (51). Alpha1-receptor antagonists such as prazosin are best supported by evidence, showing improvement in nightmares as well as insomnia (62, 63). Both sedating antipsychotics and antidepressants have been found beneficial in the treatment of PTSD, including specific positive effects on sleep quality and nightmares, but need close monitoring of negative effects such as hang-over, metabolic dysregulation, and induction/elevation of restless legs syndrome (RLS), PLMD and nightmares (64). The use of benzodiazepine-receptor agonists is controversial in patients with PTSD, not just because of generally known adverse effects, but specific negative outcomes such as worse therapy outcomes and increased risk of developing PTSD when used directly following trauma (65). Considering current evidence, pharmacological treatment of insomnia and nightmares in PTSD should be regarded as temporary and additional, rather than alternative, to psychological interventions.
Research convincingly demonstrates that PTSD is frequently associated with multiple and diverse sleep disorders that impact both PTSD development, maintenance and recovery. Thus, an early and comprehensive assessment of comorbid sleep disorders as well as their timely treatment is of high clinical relevance for patients with trauma and PTSD. In our opinion, centers providing (mental) health care to patients with PTSD should, therefore, include at least one clinician trained in sleep medicine and establish close collaboration with a sleep center for accurate assessment and (interdisciplinary) treatment of co-occurring sleep disorders.
Yet, there are clear gaps in the knowledge on the links between PTSD and sleep and to optimize PTSD-outcome further research and innovations are warranted. For both research and clinical practice, it would be helpful to develop a screening instrument to more accurately assess all sleep disturbances and contributing factors relevant in PTSD populations, ultimately leading to a guideline for the assessment of sleep disorders in PTSD. Prospective studies of large, naturalistic cohorts suffering from trauma implementing both subjective and objective sleep measures, would be highly informative for instance with respect to delineating the sleep-related protective as well as risk factors in the development of PTSD. Furthermore, evidence on the efficacy of integrated PTSD and sleep treatment is limited to small samples, specific patient groups (veterans) and only a few sleep disorders (insomnia and nightmares) and interventions. Research needs to be expanded to include larger and more diverse groups of traumatized/PTSD patients (to entangle general and population-specific factors) and diverse, both pharmacological and non-pharmacological, treatment strategies for all relevant sleep disorders. Moreover, novel developments in the neuroscience of sleep may also guide PTSD treatment. Combining for instance trauma-focused treatment with new EEG-based techniques to deepen and lengthen SWS (66, 67) could have a synergistic effect through enhanced consolidation of the traumatic memories altered in therapy. Due to faster and more complex oscillatory dynamics, such sleep-based interventions are harder to perform during REMS. Alternatively, novel behavioral methods to strengthen memories during sleep (known as targeted memory reactivation, TMR) (68, 69) could in theory be used in PTSD during post-treatment sleep to augment treatment outcome (70).
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Lewis C, Lewis K, Kitchiner N, Isaac S, Jones I, Bisson JI. Sleep disturbance in post-traumatic stress disorder (PTSD): a systematic review and meta-analysis of actigraphy studies. Eur J Psychotraumatol. (2020) 11:1767349. doi: 10.1080/20008198.2020.1767349
2. American Psychiatric Association APA. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Press (2013).
3. Krakow B, Moore B, Ulibarri VA. Sleep-disordered breathing and posttraumatic stress disorder. In: Vermetten E, Germain A, Neylan TC, editors. Sleep and Combat-Related Post Traumatic Stress Disorder. New York, NY: Springer New York (2018), p. 243–52.
4. Pigeon WR, Gallegos AM. Posttraumatic stress disorder and sleep. Sleep Med Clin. (2015) 10:41–8. doi: 10.1016/j.jsmc.2014.11.010
5. Germain A, McKeon AB, Campbell RL. Sleep in PTSD: Conceptual model and novel directions in brain-based research and interventions. Curr Opinion Psychol. (2017) 14:84–9. doi: 10.1016/j.copsyc.2016.12.004
6. Hertenstein E, Feige B, Gmeiner T, Kienzler C, Spiegelhalder K, Johann A, et al. Insomnia as a predictor of mental disorders: a systematic review and meta-analysis. Sleep Med Rev. (2019) 43:96–105. doi: 10.1016/j.smrv.2018.10.006
7. Gieselmann A, Ait Aoudia M, Carr M, Germain A, Gorzka R, Holzinger B, et al. Aetiology and treatment of nightmare disorder: state of the art and future perspectives. J Sleep Res. (2019) 28:e12820. doi: 10.1111/jsr.12820
8. Ohayon MM, Shapiro CM. Sleep disturbances and psychiatric disorders associated with posttraumatic stress disorder in the general population. Compr Psychiat. (2000) 41:469–78. doi: 10.1053/comp.2000.16568
9. Kanady JC, Talbot LS, Maguen S, Straus LD, Richards A, Ruoff L, et al. Cognitive behavioral therapy for insomnia reduces fear of sleep in individuals with posttraumatic stress disorder. J Clin Sleep Med. (2018) 14:1193–203. doi: 10.5664/jcsm.7224
10. Werner GG, Riemann D, Ehring T. Fear of sleep and trauma-induced insomnia: a review and conceptual model. Sleep Med Rev. (2021) 55:101383. doi: 10.1016/j.smrv.2020.101383
11. Khazaie H, Ghadami MR, Masoudi M. Sleep disturbances in veterans with chronic war-induced PTSD. J Inj Violence Res. (2016) 8:99–107. doi: 10.5249/jivr.v8i2.808
12. Brownlow JA, Miller KE, Gehrman PR. Treatment of sleep comorbidities in posttraumatic stress disorder. Curr Psychiat Rep. (2020) 7:301–16. doi: 10.1007/s1190-015-0587-8
13. Solomonova E. Sleep paralysis: phenomenology, neurophysiology, and treatment. In: Christoff K, Fox KCR, editors. The Oxford Handjournal of Spontaneous Thought: Mind-Wandering, Creativity, and Dreaming. Oxford: Oxford University Press (2018), p 435–56.
14. Mysliwiec V, Brock MS, Creamer JL, O'Reilly BM, Germain A, Roth BJ. Trauma associated sleep disorder: a parasomnia induced by trauma. Sleep Med Rev. (2018) 37:94–104. doi: 10.1016/j.smrv.2017.01.004
15. Feemster JC, Smith KL, McCarter SJ, St Louis EK. Trauma-associated sleep disorder: a posttraumatic stress/rem sleep behavior disorder mash-up? J Clin Sleep Med. (2019) 15:345–9. doi: 10.5664/jcsm.7642
16. Elliott JE, Opel RA, Pleshakov D, Rachakonda T, Chau AQ, Weymann KB, et al. Posttraumatic stress disorder increases the odds of REM sleep behavior disorder and other parasomnias in Veterans with and without comorbid traumatic brain injury. Sleep. (2020) 43:237. doi: 10.1093/sleep/zsz237
17. Rachakonda TD, Balba NM, Lim MM. Trauma-associated sleep disturbances: a distinct sleep disorder? Curr Sleep Med Rep. (2018) 4:143–8. doi: 10.1007/s40675-018-0119-2
18. Barone DA. Dream enactment behavior-a real nightmare: a review of post-traumatic stress disorder, REM sleep behavior disorder, and trauma-associated sleep disorder. J Clin Sleep Med. (2020) 16:1943–8. doi: 10.5664/jcsm.8758
19. Neylan TC, Kessler RC, Ressler KJ, Clifford G, Beaudoin FL, An X, et al. Prior sleep problems and adverse post-traumatic neuropsychiatric sequelae of motor vehicle collision in the AURORA study. Sleep. (2021) 44:zsaa200. doi: 10.1093/sleep/zsaa200
20. Kartal D, Arjmand H-A, Varker T, Cowlishaw S, O'Donnell M, Phelps A, et al. Cross-lagged relationships between insomnia and posttraumatic stress disorder in treatment-receiving veterans. Behav Ther. (2021) 52:982–94. doi: 10.1016/j.beth.2020.12.006
21. Sullan MJ, Crocker LD, Thomas KR, Orff HJ, Davey DK, Jurick SM, et al. Baseline sleep quality moderates symptom improvement in veterans with comorbid PTSD and TBI receiving trauma-focused treatment. Behav Res Therapy. (2021) 143:103892. doi: 10.1016/j.brat.2021.103892
22. Miller KE, Brownlow JA, Gehrman PR. Sleep in PTSD: treatment approaches and outcomes. Curr Opinion Psychol. (2020) 34:12–7. doi: 10.1016/j.copsyc.2019.08.017
23. Walters EM, Jenkins MM, Nappi CM, Clark J, Lies J, Norman SB, et al. The impact of prolonged exposure on sleep and enhancing treatment outcomes with evidence-based sleep interventions: a pilot study. Psychol Trauma. (2020) 12:175–85. doi: 10.1037/tra0000478
24. Lancel M, Boersma GJ, Kamphuis J. Insomnia disorder and its reciprocal relation with psychopathology. Curr Opinion Psychol. (2021) 41:34–9. doi: 10.1016/j.copsyc.2021.02.001
25. Pace-Schott EF, Germain A, Milad MR. Sleep and REM sleep disturbance in the pathophysiology of PTSD: the role of extinction memory. Biol Mood Anxiety Disord. (2015) 5:3. doi: 10.1186/s13587-015-0018-9
26. Spoormaker VI, Montgomery P. Disturbed sleep in post-traumatic stress disorder: secondary symptom or core feature? Sleep Med Rev. (2008) 12:169–84.
27. Rasch B, Born J. About sleep's role in memory. Physiol Rev. (2013) 93:681–766. doi: 10.1152/physrev.00032.2012
28. Goldstein AN, Walker MP. The role of sleep in emotional brain function. Annu Rev Clin Psychol. (2014) 10:679–708. doi: 10.1146/annurev-clinpsy-032813-153716
29. van der Helm E, Yao J, Dutt S, Rao V, Saletin JM, Walker MP, et al. sleep depotentiates amygdala activity to previous emotional experiences. Curr Biol. (2011) 21:2029–32. doi: 10.1016/j.cub.2011.10.052
30. Yehuda R, LeDoux J. Response variation following trauma: a translational neuroscience approach to understanding PTSD. Neuron. (2007) 56:19–32. doi: 10.1016/j.neuron.2007.09.006
31. Lebois LAM, Seligowski AV, Wolff JD, Hill SB, Ressler KJ. Augmentation of extinction and inhibitory learning in anxiety and trauma-related disorders. Annu Rev Clin Psychol. (2019) 15:257–84. doi: 10.1146/annurev-clinpsy-050718-095634
32. Richards A, Kanady JC, Neylan TC. Sleep disturbance in PTSD and other anxiety-related disorders: an updated review of clinical features, physiological characteristics, and psychological and neurobiological mechanisms. Neuropsychopharmacol. (2020) 45:55–73. doi: 10.1038/s41386-019-0486-5
33. Mellman TA, Bustamante V, Fins AI, Pigeon WR, Nolan B. REM sleep and the early development of posttraumatic stress disorder. Am J Psychiat. (2002) 159:1696–701. doi: 10.1176/appi.ajp.159.10.1696
34. Koren D, Arnon I, Lavie P, Klein E. Sleep complaints as early predictors of posttraumatic stress disorder: a 1-year prospective study of injured survivors of motor vehicle accidents. Am J Psychiat. (2002) 159:855–7. doi: 10.1176/appi.ajp.159.5.855
35. van Liempt S. Sleep disturbances and PTSD: a perpetual circle? Eur J Psychotraumatol. (2012) 3(Suppl3):19142. doi: 10.3402/ejpt.v3i0.19142
36. Kobayashi I, Boarts JM, Delahanty DL. Polysomnographically measured sleep abnormalities in PTSD: a meta-analytic review. Psychophysiology. (2007) 44:660–9. doi: 10.1111/j.1469-8986.2007.537.x
37. Zhang Y, Ren R, Sanford LD, Yang L, Zhou J, Zhang J, et al. Sleep in posttraumatic stress disorder: A systematic review and meta-analysis of polysomnographic findings. Sleep Med Rev. (2019) 48:101210. doi: 10.1016/j.smrv.2019.08.004
38. Habukawa M, Uchimura N, Maeda M, Kotorii N, Maeda H. Sleep findings in young adult patients with posttraumatic stress disorder. Biol Psychiat. (2007) 62:1179–82. doi: 10.1016/j.biopsych.2007.01.007
39. Insana SP, Hall M, Buysse DJ. Germain A. Validation of the Pittsburgh Sleep Quality Index Addendum for posttraumatic stress disorder (PSQI-A) in US male military veterans. J Trauma Stress. (2013) 26:192–200. doi: 10.1002/jts.21793
40. Mellman TA, Kumar A, Kulick-Bell R, Kumar M, Nolan B. Nocturnal/daytime urine noradrenergic measures and sleep in combat-related PTSD. Biol Psychiat. (1995) 38:174–9. doi: 10.1016/0006-3223(94)00238-x
41. Kobayashi I, Mellman TA, Altaee D, Howell MK, Lavela J. Sleep and processing of trauma memories. J Trauma Stress. (2016) 29:568–71. doi: 10.1002/jts.22137
42. Riemann D, Spiegelhalder K, Feige B, Voderholzer U, Berger M, Perlis M, et al. The hyperarousal model of insomnia: a review of the concept and its evidence. Sleep Med Rev. (2010) 14:19–31. doi: 10.1016/j.smrv.2009.04.002
43. Zhang Y, Ren R, Yang L, Zhou J, Sanford LD, Tang X. The effect of treating obstructive sleep apnea with continuous positive airway pressure on posttraumatic stress disorder: a systematic review and meta-analysis with hypothetical model. Neurosci Biobehav Rev. (2019) 102:172–83. doi: 10.1016/j.neubiorev.2019.03.019
44. Ullah MI, Campbell DG, Bhagat R, Lyons JA, Tamanna S. Improving PTSD symptoms and preventing progression of subclinical PTSD to an overt disorder by treating comorbid OSA with CPAP. J Clin Sleep Med. (2017) 13:1191–8. doi: 10.5664/jcsm.6770
45. Tsanas A, Woodward E, Ehlers A. Objective characterization of activity, sleep, and circadian rhythm patterns using a wrist-worn actigraphy sensor: insights into posttraumatic stress disorder. JMIR MHealth UHealth. (2020) 8:e14306. doi: 10.2196/14306
46. Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, Keane TM. The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5) [Clinical interview]. Available online at: https://www.ptsd.va.gov/professional/assessment/adult-int/caps.asp
47. American Academy of Sleep Medicine AASM. International Classification of Sleep Disorders (ICSD-3). 3 edn. Darien, IL: American Academy of Sleep Medicine (2014).
48. Riemann D, Baglioni C, Bassetti C, Bjorvatn B, Dolenc Groselj L, Ellis JG, et al. European guideline for the diagnosis and treatment of insomnia. J Sleep Res. (2017) 26:675–700. doi: 10.1111/jsr.12594
49. Dietch JR, Taylor DJ, Pruiksma K, Wardle-Pinkston S, Slavish DC, Messman B, et al. The Nightmare Disorder Index: development and initial validation in a sample of nurses. Sleep. (2021) 44:zsaa254. doi: 10.1093/sleep/zsaa254
50. Fabbri M, Beracci A, Martoni M, Meneo D, Tonetti L, Natale V. Measuring subjective sleep quality: a review. Int J Environ Res Public Health. (2021) 18:1082. doi: 10.3390/ijerph18031082
51. Colvonen PJ, Straus LD, Stepnowsky C, McCarthy MJ, Goldstein LA, Norman SB. Recent advancements in treating sleep disorders in co-occurring PTSD. Curr Psychiat Rep. (2018) 20:48. doi: 10.1007/s11920-018-0916-9
52. Qaseem A, Kansagara D, Forciea MA, Cooke M, Denberg TD, Clinical Guidelines Committee of the American College of Physicians. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. (2016)165:125–33. doi: 10.7326/M15-2175
53. Morgenthaler TI, Auerbach S, Casey KR, Kristo D, Maganti R, Ramar K, et al. Position paper for the treatment of nightmare disorder in adults: an American academy of sleep medicine position paper. J Clin Sleep Med. (2018) 14:1041–55. doi: 10.5664/jcsm.7178
54. Hrozanova M, Morrison I, Riha RL. Adult NREM parasomnias: an update. Clocks Sleep. (2018) 1:87–104. doi: 10.3390/clockssleep1010009
55. Maher AR, Apaydin EA, Hilton L, Chen C, Troxel W, Hall O, et al. Sleep management in posttraumatic stress disorder: a systematic review and meta-analysis. Sleep Med. (2021). doi: 10.1016/j.sleep.2021.08.016
56. Benz F, Knoop T, Ballesio A, Bacaro V, Johann AF, Rücker G, et al. The efficacy of cognitive and behavior therapies for insomnia on daytime symptoms: a systematic review and network meta-analysis. Clin Psychol Rev. (2020) 80:101873. doi: 10.1016/j.cpr.2020.101873
57. Kelly MR, Robbins R, Martin JL. Delivering cognitive behavioral therapy for insomnia in military personnel and veterans. Sleep Med Clin. (2019) 14:199–208. doi: 10.1016/j.jsmc.2019.01.003
58. Ho FY, Chan CS, Tang KN. Cognitive-behavioral therapy for sleep disturbances in treating posttraumatic stress disorder symptoms: a meta-analysis of randomized controlled trials. Clin Psychol Rev. (2016) 43:90–102. doi: 10.1016/j.cpr.2015.09.005
59. Ekholm B, Spulber S, Adler M. A randomized controlled study of weighted chain blankets for insomnia in psychiatric disorders. J Clin Sleep Med. (2020) 16:1567–77. doi: 10.5664/jcsm.8636
60. Waltman SH, Shearer D, Moore BA. Management of post-traumatic nightmares: a review of pharmacologic and nonpharmacologic treatments since 2013. Curr Psychiatry Rep. (2018) 20:108. doi: 10.1007/s11920-018-0971-2
61. Ntafouli M, Galbiati A, Gazea M, Bassetti CLA, Bargiotas P. Update on nonpharmacological interventions in parasomnias. Postgrad Med. (2020) 132:72–9. doi: 10.1080/00325481.2019.1697119
62. Yücel DE, Emmerik AAP, Souama C, Lancee J. Comparative efficacy of imagery rehearsal therapy and prazosin in the treatment of trauma-related nightmares in adults: a meta-analysis of randomized controlled trials. Sleep Med Rev. (2019) 50:101248. doi: 10.1016/j.smrv.2019.101248
63. Zhang Y, Ren R, Sanford LD, Yang L, Ni Y, Zhou J, et al. The effects of prazosin on sleep disturbances in post-traumatic stress disorder: a systematic review and meta-analysis. Sleep Med. (2020) 67:225–31. doi: 10.1016/j.sleep.2019.06.010
64. de Jong J, Vermetten E. Medication for sleep problems in posttraumatic stress disorder. In: Vermetten E, Germain A, Neylan TC, editors. Sleep and Combat-Related Post Traumatic Stress Disorder. New York: Springer Science+Business Media LLC (2018), p. 325–48.
65. Guina J, Rossetter SR De RB, Nahhas RW, Welton RS. Benzodiazepines for PTSD: a systematic review and meta-analysis. J Psychiatr Pract. (2015) 21:281–303. doi: 10.1097/pra.0000000000000091
66. Marshall L, Helgadóttir H, Mölle M, Born J. Boosting slow oscillations during sleep potentiates memory. Nature. (2006) 444:610–3. doi: 10.1038/nature05278
67. Ngo HV, Martinetz T, Born J, Mölle M. Auditory closed-loop stimulation of the sleep slow oscillation enhances memory. Neuron. (2013) 78:545–53. doi: 10.1016/j.neuron.2013.03.006
68. Cellini N, Capuozzo A. Shaping memory consolidation via targeted memory reactivation during sleep. Ann N Y Acad Sci. (2018). doi: 10.1111/nyas.13855
69. Paller KA, Creery JD, Schechtman E. Memory and Sleep: How sleep cognition can change the waking mind for the better. Annu Rev Psychol. (2021) 72:123–50. doi: 10.1146/annurev-psych-010419-050815
70. van der Heijden A, van den Heuvel O, van der Werf Y, Talamini L, van Marle H. Targeted Memory Reactivation to augment TRAUMA therapy during sleep (TMR-TRAUMA study). Dutch Trial Register. (2017). Available online at: https://www.trialregister.nl/trial/6455
Keywords: PTSD, sleep, sleep disorders, nightmares, insomnia, sleep apnea, assessment, treatment
Citation: Lancel M, van Marle HJF, Van Veen MM and van Schagen AM (2021) Disturbed Sleep in PTSD: Thinking Beyond Nightmares. Front. Psychiatry 12:767760. doi: 10.3389/fpsyt.2021.767760
Received: 31 August 2021; Accepted: 02 November 2021;
Published: 24 November 2021.
Edited by:
Seog Ju Kim, Sungkyunkwan University, South KoreaReviewed by:
David Neubauer, Johns Hopkins University, United StatesCopyright © 2021 Lancel, van Marle, Van Veen and van Schagen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marike Lancel, bS5sYW5jZWxAcnVnLm5s
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.