
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 06 October 2021
Sec. Mood Disorders
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.731537
 Tobias Weigl1
Tobias Weigl1 Franziska Marie Lea Beck-Hiestermann2
Franziska Marie Lea Beck-Hiestermann2 Nikola Maria Stenzel2
Nikola Maria Stenzel2 Sven Benson3
Sven Benson3 Manfred Schedlowski3,4
Manfred Schedlowski3,4 Susan Garthus-Niegel5,6,7*
Susan Garthus-Niegel5,6,7*Background: About 3–4% of women in community samples suffer from childbirth-related posttraumatic stress disorder (PTSD). Surprisingly, the recently developed City Birth Trauma Scale (City BiTS) was the first diagnostic tool for childbirth-related PTSD covering DSM-5 criteria for PTSD. Since no questionnaire on childbirth-related PTSD is available in German, we aimed to validate a German translation of the City BiTS and to provide information on its psychometric properties.
Methods: A community sample of 1,072 mothers completed an online survey, which included questions on sociodemographic and obstetric characteristics, the German version of the City BiTS, the Impact of Event Scale-Revised (IES-R), the PTSD Checklist for DSM-5 (PCL-5), Edinburgh Postnatal Depression Scale (EPDS), and the anxiety subscale of the Depression, Anxiety, and Stress Scale (DASS-Anxiety).
Results: Exploratory factor analysis (EFA) on a random split-half sample confirmed the previously reported two-factorial structure of the City BiTS. The factors “Childbirth-related symptoms” and “General symptoms” explained about 53%, 52% of variance. Internal consistency was good to excellent for the subscales and the total scale (Cronbach's Alpha = 0.89−0.92). In a confirmatory factor analysis (CFA) in the holdout sample the two-factorial solution reached the best model fit out of three models. Correlation analyses showed convergent validity of the City BiTS (total scale and subscales) with the IES-R and PCL-5 and divergent validity with the EPDS and the DASS-Anxiety.
Limitations: Data were acquired in a community sample and prevalence rates might not be representative for mothers of high-risk groups, e.g., after preterm birth.
Conclusions: The German version of the City BiTS is the first German questionnaire which allows to assess symptoms of childbirth-related PTSD according to DSM-5 criteria. Besides an improvement in clinical routine it will help to make data on prevalence of childbirth-related PTSD internationally comparable. In addition, this work provides a basis to assess childbirth-related PTSD in studies conducted with a longitudinal study design or in high-risk samples.
Recent data suggest, that giving birth even without any further medical complications for mother or child may lead to PTSD in 3–4% of women and the prevalence might increase during the first year postpartum (1–4). In populations with risk factors such as operative birth or giving birth to a child with very low birth weight, even up to 15.7 or 18.5% of women might be affected (3, 4). The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) refers to posttraumatic stress disorder (PTSD) as a reaction to events in which a person is exposed to “actual or threatened death or serious injury, or a threat to the physical integrity of self or others” (5). Symptoms include intrusions, avoidance of trauma-related stimuli, alterations in mood and cognitions, as well as alterations in arousal and reactivity (5). While accidents, wars, or natural disasters represent well-known traumatic stressors, childbirth may also meet DSM criteria for a traumatic event (6). Yet, childbirth-related PTSD is not regularly assessed in postpartum routine care.
Adverse effects of childbirth-related PTSD are not limited to impaired maternal mental health. In fact, consequences may include a negative impact on the couple relationship, the parent-child relationship, or even the child's development (7–12). Therefore, early identification of childbirth-related PTSD may be beneficial for the whole family. Self-report questionnaires offer an economic and efficient way for the assessment of mental health problems in the peripartum period (13). So far, three questionnaires have been developed to assess symptoms of childbirth-related PTSD. Two of them however, the Traumatic Event Scale as well as the Perinatal PTSD Questionnaire, are based on outdated diagnostic criteria from DSM-IV (14–16). Only the recently developed City Birth Trauma Scale (City BiTS) was established in consideration of diagnostic criteria from DSM-5 (17). Next to the original English version, the City BiTS has been validated and translated into Turkish, Spanish, Hebrew, Croatian, and French (18–22). In addition to identifying the need for individual prevention and treatment of childbirth-related PTSD, cross-cultural validations will help to establish the City BiTS as a standardized measure internationally, allowing for comparisons of childbirth-related PTSD symptoms between different languages and cultures.
To date there exists no validated German measure to assess childbirth-related PTSD (23). This is a hindrance in research and clinical care. To close this gap, the aim of the present study was therefore to provide a translated German version of the City BiTS and to determine its psychometric properties in a community sample.
The cross-sectional data presented in this article are part of the longitudinal “LABOR”-study (Longitudinal Analysis of Birth mode and Outcomes Related) in which three different groups of women were recruited: pregnant women, women who had their baby within the last 12 months, and women who had their baby more than 12 months ago. After their first assessment, all participants were asked if they were willing to take part in further follow-up assessments, scheduled at 3, 6, and 9 months after study entry. For the present study, only women of the second group, i.e., women who gave birth within the last 12 months were included. Exclusion criteria were death of the child during or after birth, younger age than 18 years, and insufficient German language skills. Invitations to take part in the study were posted on social media, such as Instagram and Facebook, as well as parents' blogs and forums between February and April 2020. The study was conducted online with the use of the platform EFS survey by QuestBack (unipark.de). Several arrangements ensured high quality of data. The platform offers the possibility to block participants from completing the questionnaire more than once. To ensure that participation was not only motivated by incentives like money or gift cards, women did not receive any kind of compensation. Since answers were obligatory for the participants, no imputation for missing values had to be conducted. Participants could complete the questionnaire on a smartphone or computer with an active internet connection in an environment of their choice. Participants were informed that some of the questions might relate to unpleasant or even traumatic experiences, which might trigger unwanted memories and emotions. Further, participants were informed about their right to withdraw from the study at any given time and were advised to seek professional help if needed (informed consent included a list of mental health services like the German National Suicide and Crisis Line). A total of 1,072 women who met inclusion criteria gave informed consent to follow the study protocol. Ethical approval was granted by the ethics committee of the Psychologische Hochschule Berlin (approval no. AZ: EK201921-II) and the study was performed in accordance with the Declaration of Helsinki. All data were stored anonymously and in accordance with the German General Data Protection Regulation (GDPR). On average, it took participants around 45 min to complete the whole assessment, including further questionnaires, which were not relevant for this study. Participants could pause and continue the questionnaire afterwards.
Sociodemographic information was assessed including maternal age, relationship status, as well as educational status. Questions regarding obstetric characteristics included length of gestation, infant age, parity, type of delivery [spontaneous vaginal delivery, instrumental vaginal delivery, emergency, or planned cesarean section (CS)], pregnancy at risk (yes/no), and preterm birth (see Table 1 for further details).
The City BiTS is a self-report questionnaire with 29 items, which was developed based on DSM-5 criteria in order to assess childbirth-related PTSD in women (17). Two dichotomous items (yes/no) assess the stressor criterion (i.e., threatened death or serious injury of the mother or the baby during labor, birth, or immediately afterwards). The frequency of intrusion, avoidance, negative cognitions/mood, and hyperarousal symptoms in the week prior to assessment is measured with 20 items. Items are rated on a four-point Likert scale from 0 (never) to 3 (5 or more times) to produce a sum score ranging from 0 to 60, with higher scores indicating elevated levels of PTSD-symptoms. Two additional items allow to screen for a dissociative subtype of PTSD. Another five items assess the onset of symptoms (from before the birth to more than 6 months after birth), duration of symptoms (from <1 month to >3 months), distress (yes/sometimes/no) as well as impairment (yes/sometimes/no), and exclusion criteria (i.e., symptoms due to medication, alcohol, drugs, or physical illness; yes/maybe/no).
In the original validation study, the subscales “Birth-related symptoms” (predominantly consisting of items which measure intrusion, avoidance, and negative cognitions/mood related to birth) and “General symptoms” (mainly consisting of items assessing negative cognitions/mood and hyperarousal) have been identified. The original version of the City BiTS showed excellent reliability with Cronbach's Alpha = 0.92 for the total scale (17). Upon consent from the original author (Susan Ayers), the City BiTS was translated into German, using the back-translation method (24). The back-translation was then discussed with the original author. This resulted in minor adjustments in the wording. Additionally, 10 participants of a pilot sample were asked to complete the German version of the City BiTS and to express any difficulties they had regarding comprehensibility. This did not result in any changes of the questionnaire.
The Impact of Event Scale-Revised (IES-R) is a self-report questionnaire assessing symptoms of PTSD in accordance with criteria of the DSM-IV (25). After specifying a certain stressful life event, items can be answered on a four-point scale with the response options 0 (not at all), 1 (rarely), 3 (sometimes), and 5 (often) referring to the last 7 days. In our study, women were instructed to refer to their birth experience only. Scores can be calculated for the Intrusion (7 items), Avoidance (8 items), and Hyperarousal (7 items) subscales. For the German version, authors advise against a total sum score and suggest an algorithm, which has been used in this study. Values above zero indicate probable PTSD (26).
Symptoms of PTSD were also assessed with the PTSD Checklist for DSM-5 (PCL-5). The PCL-5 is a self-report measure comprising 20 items based on the DSM-5, and can be subdivided in the clusters intrusion (items 1–5), avoidance (items 6–7), negative mood and cognition (items 8–14), and hyperarousal (items 15–20). Each item reflects the severity of a PTSD symptom during the month prior to assessment. Ratings are carried out on a five-point Likert scale from 0 (not at all) to 4 (extremely). The German version was used and women were instructed to answer in relation to the birth of their last child (27).
Symptoms of depression were measured with the German version of the Edinburgh Postnatal Depression Scale (EPDS), the most common self-report scale to assess depression in the postpartum period (28, 29). The EPDS consists of 10 items. With a four-point scale from 0 to 3, the sum score ranges from 0 to 30. Higher scores reflect higher levels of depression. A cut-off ≥10 indicates a substantial level of depressive symptoms suggesting that further diagnostic procedures should be performed (29, 30).
The Depression, Anxiety, and Stress Scale-21 (DASS-21) consists of 21 items with three subscales assessing symptoms of depression, anxiety, and stress and has been validated in postpartum mothers (31, 32). Items can be rated on a scale from 0 (did not apply to me at all) to 3 (applies to me very much or most of the time), and sum scores can be calculated for each scale. In the present study, the German version of the subscale “DASS-Anxiety” was used (33).
Exploratory factor analysis (EFA) on a random split-half sample (n = 536), calculations of correlation coefficients for convergent and divergent validity, and tests for group differences were performed using IBM SPSS statistics version 27 for windows. Univariate ANOVA with Bonferroni post-hoc comparisons were used to analyze potential differences regarding type of delivery. Confirmatory factor analysis (CFA) in the holdout sample (n = 536) was performed using IBM SPSS Amos version 27. Fit indices included Root Mean Square Error of Approximation (RMSEA), Standardized Root Mean Square Residual (SRMR), Comparative Fit Index (CFI), and Tucker-Lewis Index (TLI). Good (and adequate, respectively) model fit is indicated by RMSEA ≤ 0.06 (0.06–0.08), SRMR ≤ 0.08, and CFI as well as TLI ≥0.95 (0.90–0.95) (34).
A total of N = 1,072 mothers were included in the final sample (age: M = 30.6, SD = 4.7). Almost all women were in a permanent relationship. Most children were born by spontaneous vaginal birth (n = 739) and for approximately 60% of mothers it was their first birth. Only 5% of births took place before gestational week 37 (see Table 1 for further details).
Responses to the City BiTS in accordance with DSM-5 criteria for PTSD are shown in Table 2. About 22% women fulfilled the stressor criterion by indicating that they believed they or their baby would be seriously injured or even die during childbirth (or immediately afterwards). A total of 28 (2.6%) women fulfilled all criteria to qualify for a PTSD diagnosis according to DSM-5 criteria.
With a Kaiser-Meyer-Olkin coefficient of 0.92 and a chi-squared value of (χ2 = 5336.06; df = 190; p < 0.001) in the Bartlett's test of sphericity, results indicated that the sample can be used for factor analysis (35, 36).
In accordance with previous validations of the City BiTS, an EFA using principal component analysis with varimax rotation was conducted (18, 21). Applying Kaiser's rule (retain Eigenvalues >1) and the screen test, a structure with two factors could be found. Factor 1 included items 3–12 and factor 2 included items 13–22. Items 23 and 24 were excluded from EFA, since they can be used to measure dissociative symptoms but do not represent main symptoms of PTSD. In our study, the total scale accounted for almost 52% of variance, with the subscales “Birth-related symptoms” and “General symptoms” explaining roughly 38 and 14% of the variance, respectively (see Table 3 for further details).
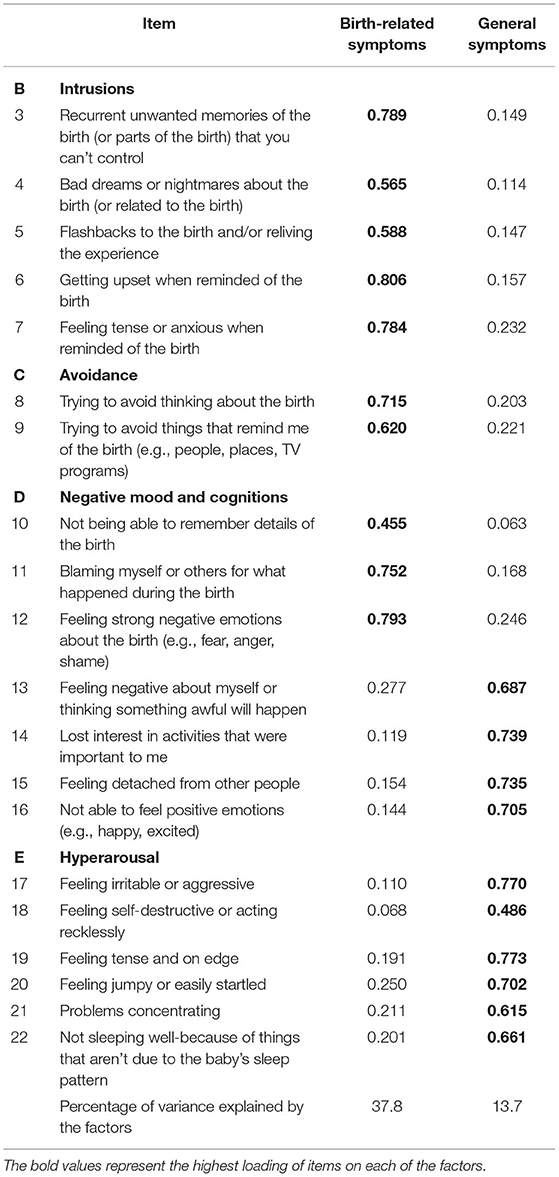
Table 3. Factor loadings of the EFA with two factors in principal component analysis with varimax rotation.
Based on theoretical reasoning and results of previous studies, the fit of three different models was tested in CFA. Firstly, we tested a model with four factors as determined in the diagnostic criteria of PTSD in the DSM-5, including the dimensions Intrusions (items 3–7), Avoidance (items 8 and 9), Negative cognitions/mood (items 10–16), and Hyperarousal (items 17–20). This analysis showed a poor fit of the model with four factors [ = 1288.86, χ2/df = 7.86, RMSEA = 0.113, SRMR = 0.093, CFI = 0.81, TLI = 0.78].
Secondly, we tested a model with one overall factor. This model also had to be rejected [ = 2050.71, χ2/df = 12.06, RMSEA = 0.144, SRMR = 0.119, CFI = 0.68, TLI = 0.64].
Thirdly, we tested a model with two factors that has previously been shown to yield an acceptable to good model fit. However, in one prior study minor modifications of the model (i.e., deletion of item 8) were necessary to reach acceptable model fit (18). In the current study, the two-factor model with two correlated dimensions in accordance with the original validation (“Birth-related symptoms” and “General symptoms”) was the best fit to the data according to all fit indices [ = 771.27, χ2/df = 4.56, RMSEA = 0.082, SRMR = 0.056, CFI = 0.90, TLI = 0.89]. Yet, the 90% confidence interval for the RMSEA (0.076−0.088) was slightly above the suggested cut-off of 0.08 (37). However, since items of the City BiTS aim to measure symptoms of childbirth-related PTSD according to DSM-5 we decided against deletion of items.
Analysis of the internal consistency by Cronbach's Alpha resulted in good to excellent reliability of 0.90 for the “Birth-related symptoms” subscale, 0.89 for the “General symptoms” subscale, as well as 0.92 for the total scale. Deletion of any of the items did not increase Cronbach's Alpha substantially.
Convergent and divergent validity were tested by correlating both subscales and the total scale of the City BiTS against the IES-R, PCL-5, EPDS, and the DASS-Anxiety subscale (see Table 4).
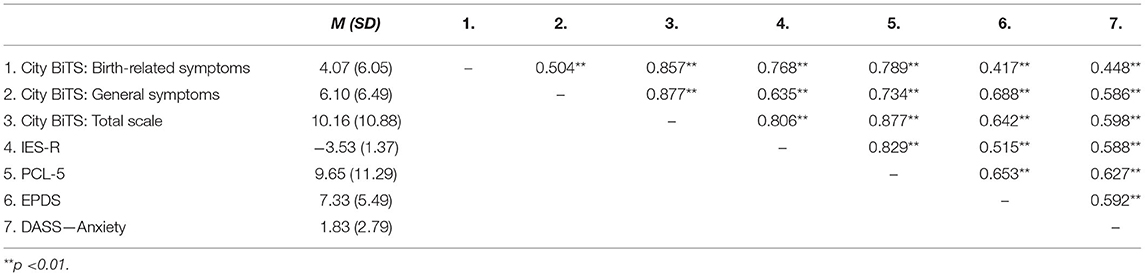
Table 4. Intercorrelations of the City BiTS (subscales and total scale) with measures of PTSD symptomatology, depression, and anxiety (N = 1,072).
Univariate ANOVA was employed to assess if more invasive and medically complicated types of delivery lead to more severe symptoms of PTSD. Main effects could be found for the subscales “Birth-related symptoms” and “General symptoms” as well as the total scale (all p < 0.001; see Table 5; Figure 1). Bonferroni post-hoc comparisons revealed that for the subscale “Birth-related symptoms” scores differed statistically significantly between spontaneous vaginal birth and all other types of delivery (all p < 0.001). Furthermore, there was a statistically significant difference between elective and emergency CS (p = 0.02). The only statistically significant difference found for scores of the scale “General symptoms” was between the groups spontaneous vaginal delivery and emergency CS (p < 0.001). For the score of the total scale the post-hoc comparisons revealed that the group spontaneous vaginal delivery differed from all other groups (p < 0.01). Other group differences could not be found (all n.s.).
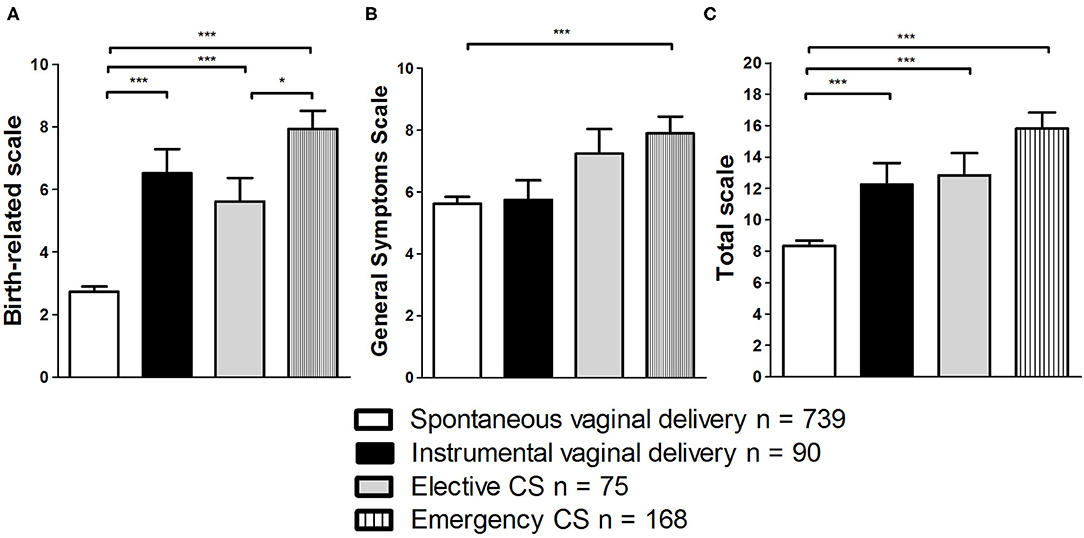
Figure 1. Comparison of effects of type of delivery on scores in City BiTS subscales “Birth-related symptoms” (A), “General symptoms” (B), and the total scale (C). *p < 0.05; ***p < 0.001. Data are shown as mean values ± SEM.
This study set out to provide a translated German version of the City BiTS and to determine its psychometric properties resulting in the first questionnaire to assess childbirth-related PTSD based on DSM-5 criteria in German language. The results of our study provide further important knowledge on the psychometric properties of the City BiTS. Also for the German version a two-factorial solution could be found in EFA, which is in accordance with previous validation studies, both of the original English version as well as other translated versions (17–22). The subscale “Birth-related symptoms” explained about 38% and the subscale “General symptoms” about 14% of variance. Both subscales as well as the total scale showed good to excellent internal consistency in the tested sample. Furthermore, using CFA we tested the model fit for three different models. Neither a four-factorial model based on diagnostic criteria of PTSD in DSM-5, nor a one-factorial solution achieved adequate fit. The best model fit was achieved for the two-factorial structure, which is comparable to previous studies (18, 20, 21). Still, when assessing the model fit of this two-factor model, results of the CFA showed that some of the fit indices were only close to suggested cut-offs (34, 37). However, methodological literature in the field suggests that in applied research universal cut-off criteria recommended for CFA might be too strict and therefore arguable (38–42). In fact, these cut-offs were derived from simulation studies and are hard to be replicated. Thus, cut-offs in CFA should not be overgeneralized (34, 40). Given that there is a clear theoretical rationale underlying the two-factorial solution, the combination of fit metrics in our study can be interpreted as an acceptable fit of the model. Since the composition of samples can affect results of a CFA, we suggest further validations of the German version of the City BiTS also in different samples and subsequent comparisons in relation to model fit.
By using the IES-R, the PCL-5, the EPDS, and the DASS-Anxiety in our study, the instruments to examine convergent and divergent validity were similar to previous studies (19, 20). Since the PCL-5 is based on the DSM-5, it offered additional information on the convergent validity of the City BiTS. Regarding convergent and divergent validity, results need to be differentiated. The correlation between scores of depression and anxiety with the subscale “Birth-related symptoms” was weaker than with the subscale “General symptoms” and the total scale of the City BiTS, confirming divergent validity. As to be expected, all scales of the City BiTS showed moderate to strong correlations with other measures of PTSD. Thus, convergent validity could be confirmed.
Additionally, group comparisons could show that the subscale “Birth-related symptoms” differentiates well-between types of delivery. Spontaneous vaginal delivery seems to result in only few childbirth-related symptoms. In contrast, emergency CS led to highest maternal symptom load, in both subscales as well as in the total scale. These results once more confirm, that even though all mothers may potentially suffer from childbirth-related symptoms of PTSD, women with deliveries other than a spontaneous vaginal delivery are at higher risk to develop such symptoms. Interventions should take this fact into account (43). To date, a cut-off for the City BiTS has not yet been established. Clinical interviews can be considered the gold standard for the assessment of mental disorders and should be applied as an external criterion to establish a cut-off, which might help to use the City BiTS in perinatal healthcare services more easily. Nonetheless, even in the current form the City BiTS represents an efficient and economic instrument and may play an important role in the prevention and intervention of childbirth-related PTSD. Once women suffering from symptoms of childbirth-related PTSD are detected, they can be assigned to psychotherapy. Promising and viable techniques are cognitive behavioral therapy, eye movement desensitization and reprocessing, as well as debriefing (44). Besides, the multitude of translations of the City BiTS are vital for global research on childbirth-related PTSD. Initiatives like the International Survey of Childbirth-Related Trauma (INTERSECT) are therefore able to study prevalence's of childbirth-related PTSD globally and make results directly comparable (45).
The study has noteworthy strengths such as the large sample size and the use of several different measures to establish convergent and divergent validity. Most notably, our translation of the City BiTS is the first German questionnaire, which offers the possibility to assess childbirth-related PTSD on the basis of DSM-5 diagnostic criteria. Therefore, standardized use of the German version of the City BiTS in postpartum women could improve perinatal healthcare fundamentally. Yet, there are also limitations that need to be acknowledged. Our results were obtained from cross-sectional data and preexisting symptoms of mental disorders were not assessed. Thus, we cannot determine whether women who already suffered from symptoms of PTSD or other mental disorders exhibit different scores on the City BiTS than women with no such history. Therefore, future research should apply longitudinal designs measuring symptoms of childbirth-related PTSD at several points in time to allow for an estimation of trajectories. This could facilitate early identification of women at risk to suffer from chronic childbirth-related symptoms of PTSD (4, 46–48). Further, even though the sample size was large, a selection bias cannot be ruled out. Web-based surveys offer easy accessibility, but women who use social media on a regular basis are more likely to be represented in online samples (49). Thus, further studies should aim to recruit more representative samples of women. Additionally, in our sample only a low percentage of women fulfilled DSM-5 diagnostic criteria for PTSD. Even though the results are similar to previous studies, subsequent validation studies should include populations at a comparably higher risk for childbirth-related PTSD (3, 4, 50). Additional efforts should be made to examine women belonging to different ethnic groups.
The findings of the present study provide strong evidence that the German version of the City BiTS offers adequate psychometric properties. This version is fit for use and perinatal healthcare might improve by its application in postpartum women. Furthermore, a questionnaire especially developed to assess childbirth-related PTSD will hopefully heighten the acceptance of standardized measurement of mental health in the peripartum period. Due to its explicit wording, women might relate more to a questionnaire on childbirth-related PTSD than to more general questionnaires assessing PTSD which might make their participation in postpartum psychological assessment more likely. As a result, childbirth-related PTSD might get more widely recognized by healthcare providers and affected women. In addition, efficient identification of women suffering from symptoms of childbirth-related PTSD will expedite allocation to adequate treatment for PTSD and might prevent them from being treated for e.g., postpartum depression instead. Based on this knowledge, evidence-based prevention and intervention strategies for childbirth-related PTSD can be refined in the future. In summary, the German version of the City BiTS may represent a useful tool in clinical routine and could help to make prevalence estimates of childbirth-related PTSD comparable across different countries.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
This study involved human participants and was approved by the ethics committee of the Psychologische Hochschule Berlin, Berlin, Germany (approval no. AZ: EK201921-II). The participants provided their written informed consent to participate in this study.
TW, FB-H, NS, SB, MS, and SG-N designed the study and contributed to the interpretation of data and internal revision of the manuscript. TW managed the translation process of the scale, conducted the statistical analysis, interpretation of data, and wrote the first draft of the manuscript. TW, FB-H, NS, and SG-N executed and supervised the acquisition of data. All authors contributed to and have approved the final manuscript.
TW and SG-N are (management committee) members of COST action CA18211: DEVoTION: Perinatal Mental Health and Birth-Related Trauma: Maximizing best practice and optimal outcomes.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Dekel S, Stuebe C, Dishy G. Childbirth induced posttraumatic stress syndrome: a systematic review of prevalence and risk factors. Front Psychol. (2017) 8:560. doi: 10.3389/Fpsyg.2017.00560
2. Polachek IS, Fung K, Vigod SN. First lifetime psychiatric admission in the postpartum period: a population-based comparison to women with prior psychiatric admission. Gen Hosp Psychiatry. (2016) 40:25–32. doi: 10.1016/j.genhosppsych.2016.01.007
3. Grekin R, O'Hara MW. Prevalence and risk factors of postpartum posttraumatic stress disorder: a meta-analysis. Clin Psychol Rev. (2014) 34:389–401. doi: 10.1016/j.cpr.2014.05.003
4. Yildiz PD, Ayers S, Phillips L. The prevalence of posttraumatic stress disorder in pregnancy and after birth: a systematic review and meta-analysis. J Affect Disord. (2017) 208:634–45. doi: 10.1016/j.jad.2016.10.009
5. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Washington, DC: American Psychiatric Publishing (2013). p. 947.
6. Horsch A, Garthus-Niegel S. Posttraumatic stress disorder following childbirth. In: Pickles C, Herring J, editors. Childbirth, Vulnerability and Law: Exploring Issues of Violence and Control. Abingdon; Oxon; New York, NY: Routledge (2020). p. 49–66.
7. Cook N, Ayers S, Horsch A. Maternal posttraumatic stress disorder during the perinatal period and child outcomes: a systematic review. J Affect Disord. (2018) 225:18–31. doi: 10.1016/j.jad.2017.07.045
8. Garthus-Niegel S, Ayers S, Martini J, von Soest T, Eberhard-Gran M. The impact of postpartum post-traumatic stress disorder symptoms on child development: a population-based, 2-year follow-up study. Psychol Med. (2017) 47:161–70. doi: 10.1017/S003329171600235X
9. Winter L, Colditz PB, Sanders MR, Boyd RN, Pritchard M, Gray PH, et al. Depression, posttraumatic stress and relationship distress in parents of very preterm infants. Arch Womens Ment Health. (2018) 21:445–51. doi: 10.1007/s00737-018-0821-6
10. Taheri M, Takian A, Taghizadeh Z, Jafari N, Sarafraz N. Creating a positive perception of childbirth experience: systematic review and meta-analysis of prenatal and intrapartum interventions. Reprod Health. (2018) 15:73. doi: 10.1186/s12978-018-0511-x
11. Garthus-Niegel S, Horsch A, Handtke E, von Soest T, Ayers S, Weidner K, et al. The impact of postpartum posttraumatic stress and depression symptoms on couples' relationship satisfaction: a population-based prospective study. Front Psychol. (2018) 9:1728. doi: 10.3389/fpsyg.2018.01728
12. Weigl T, Garthus-Niegel S. [Questionnaires for the assessment of bonding during pregnancy and after birth (Part 3 of a series on psychological assessment during the peripartum period)]. Z Geburtshilfe Neonatol. (2021) Online ahead of print. doi: 10.1055/a-1471-8017
13. Weigl T, Garthus-Niegel S. [Questionnaires for the assessment of peripartum depression, anxiety and stress (Part 1 of a series on psychological assessment during the peripartum period)]. Z Geburtshilfe Neonatol. (2021) 225:300–5. doi: 10.1055/a-1471-7256
14. Callahan JL, Borja SE, Hynan MT. Modification of the perinatal PTSD questionnaire to enhance clinical utility. J Perinatol. (2006) 26:533–9. doi: 10.1038/sj.jp.7211562
15. Quinnell FA, Hynan MT. Convergent and discriminant validity of the perinatal PTSD questionnaire (PPQ): a preliminary study. J Trauma Stress. (1999) 12:193–9. doi: 10.1023/A:1024714903950
16. Wijma K, Söderquist J, Wijma B. Posttraumatic stress disorder after childbirth: a cross sectional study. J Anxiety Disord. (1997) 11:587–97. doi: 10.1016/s0887-6185(97)00041-8
17. Ayers S, Wright DB, Thornton A. Development of a measure of Postpartum PTSD: the city birth trauma scale. Front Psychiatry. (2018) 9:409. doi: 10.3389/fpsyt.2018.00409
18. Caparros-Gonzalez RA, Romero-Gonzalez B, Peralta-Ramirez MI, Ayers S, Galán-Paredes A, Caracuel-Romero A. Assessment of posttraumatic stress disorder among women after childbirth using the city birth trauma scale in Spain. Psychol Trauma. (2021) 13:545–54. doi: 10.1037/tra0001007
19. Handelzalts JE Hairston IS Matatyahu A. Construct validity and psychometric properties of the hebrew version of the city birth trauma scale. Front Psychol. (2018) 9:1726. doi: 10.3389/fpsyg.2018.01726
20. Nakić Radoš S, Matijaš M, Kuhar L, Andelinović M, Ayers S. Measuring and conceptualizing PTSD following childbirth: validation of the City Birth Trauma Scale. Psychol Trauma. (2020) 12:147–55. doi: 10.1037/tra0000501
21. Bayri Bingöl F, Bal MD, Dişsiz M, Sormageç MT, Yildiz PD. Validity and reliability of the Turkish version of the City Birth Trauma Scale (CityBiTS). J Obstet Gynaecol. (2020) 2020:1–9. doi: 10.1080/01443615.2020.1821354
22. Sandoz V, Hingray C, Stuijfzand S, Lacroix A, El Hage W, Horsch A. Measurement and conceptualization of maternal PTSD following childbirth: psychometric properties of the City Birth Trauma Scale-French Version (City BiTS-F). Psychol Trauma. (2021) Online ahead of print. doi: 10.1037/tra0001068
23. Weigl T, Garthus-Niegel S. [Questionnaires for the assessment of birth expectancy and birth experience (Part 2 of a series on psychological assessment during the peripartum period)]. Z Geburtshilfe Neonatol. (2021) Online ahead of print. doi: 10.1055/a-1471-7714
24. Brislin RW, Lonner WJ, Berry JW. Field Methods in Cross-Cultural Research. Beverly Hills, CA: SAGE. (1986).
25. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Arlington, VA: American Psychiatric Publishing, Inc. (1994).
26. Rosner R, Hagl M. Die revidierte Impact of Event-Skala (IES-R). Psychosom Konsiliarpsychiatr. (2008) 2:240–243. doi: 10.1007/s11800-008-0132-2
27. Kruger-Gottschalk A, Knaevelsrud C, Rau H, Dyer A, Schafer I, Schellong J, et al. The German version of the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): psychometric properties and diagnostic utility. BMC Psychiatry. (2017) 17:379. doi: 10.1186/s12888-017-1541-6
28. Hewitt CE, Gilbody SM, Mann R, Brealey S. Instruments to identify post-natal depression: which methods have been the most extensively validated, in what setting and in which language? Int J Psychiatry Clin Pract. (2010) 14:72–6. doi: 10.3109/13651500903198020
29. Bergant AM, Nguyen T, Heim K, Ulmer H, Dapunt O. [German language version and validation of the Edinburgh postnatal depression scale]. Dtsch Med Wochenschr. (1998) 123:35–40. doi: 10.1055/s-2007-1023895
30. Cox J. Thirty years with the Edinburgh postnatal depression scale: voices from the past and recommendations for the future. Br J Psychiatry. (2019) 214:127–9. doi: 10.1192/bjp.2018.245
31. Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck depression and anxiety inventories. Behav Res Ther. (1995) 33:335–43. doi: 10.1016/0005-7967(94)00075-U
32. Miller RL, Pallant JF, Negri LM. Anxiety and stress in the postpartum: is there more to postnatal distress than depression? BMC Psychiatry. (2006) 6:12. doi: 10.1186/1471-244X-6-12
33. Nilges P, Essau C. [Depression, anxiety and stress scales: DASS–a screening procedure not only for pain patients]. Schmerz. (2015) 29:649–57. doi: 10.1007/s00482-015-0019-z
34. Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equat Model Multidiscipl J. (1999) 6:1–55. doi: 10.1080/10705519909540118
35. Kaiser HF. An index of factorial simplicity. Psychometrika. (1974) 39:31–6. doi: 10.1007/BF02291575
36. Tobias S, Carlson JE. Brief report. BARTLETT'S test of sphericity and chance findings in factor analysis. Multivariate Behav Res. (1969) 4:375–7. doi: 10.1207/s15327906mbr0403_8
37. Bollen KA, Long SJ. Testing Structural Equation. Newbury Park, CA: Sage Publications (1996). p. 320.
38. Perry JL, Nicholls AR, Clough PJ, Crust L. Assessing model fit: caveats and recommendations for confirmatory factor analysis and exploratory structural equation modeling. Meas Phys Educ Exerc Sci. (2015) 19:12–21. doi: 10.1080/1091367X.2014.952370
39. Barrett P. Structural equation modelling: adjudging model fit. Pers Individ Dif. (2007) 42:815–24. doi: 10.1016/j.paid.2006.09.018
40. Marsh HW, Hau K-T, Wen Z. In search of golden rules: comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing Hu and Bentler's (1999) findings. Struct Equat Model Multidiscipl J. (2004) 11:320–41. doi: 10.1207/s15328007sem1103_2
41. Chen F, Curran PJ, Bollen KA, Kirby J, Paxton P. An Empirical evaluation of the use of fixed cutoff points in RMSEA test statistic in structural equation models. Sociol Methods Res. (2008) 36:462–94. doi: 10.1177/0049124108314720
42. Brown TA. Confirmatory Factor Analysis for Applied Research. New York; London: The Guilford Press (2015). p. 482.
43. Horsch A, Vial Y, Favrod C, Harari MM, Blackwell SE, Watson P, et al. Reducing intrusive traumatic memories after emergency caesarean section: a proof-of-principle randomized controlled study. Behav Res Ther. (2017) 94:36–47. doi: 10.1016/j.brat.2017.03.018
44. Bruijn L de, Stramrood CA. Lambregtse-van den Berg MP, Rius Ottenheim N. Treatment of posttraumatic stress disorder following childbirth. J Psychosom Obstet Gynaecol. (2020) 41:5–14. doi: 10.1080/0167482X.2019.1593961
45. INTERSECT – International Survey of Childbirth-Related Trauma. (2021). Available online at: https://blogs.city.ac.uk/intersect/ (accessed May 19, 2021).
46. Muzik M, McGinnis EW, Bocknek E, Morelen D, Rosenblum KL, Liberzon I, et al. PTSD symptoms across pregnancy and early postpartum among women with lifetime PTSD diagnosis. Depress Anxiety. (2016) 33:584–91. doi: 10.1002/da.22465
47. Dikmen-Yildiz P, Ayers S, Phillips L. Longitudinal trajectories of post-traumatic stress disorder (PTSD) after birth and associated risk factors. J Affect Disord. (2018) 229:377–85. doi: 10.1016/j.jad.2017.12.074
48. Oh W, Muzik M, McGinnis EW, Hamilton L, Menke RA, Rosenblum KL. Comorbid trajectories of postpartum depression and PTSD among mothers with childhood trauma history: course, predictors, processes and child adjustment. J Affect Disord. (2016) 200:133–41. doi: 10.1016/j.jad.2016.04.037
49. McGee B, Leonte M, Wildenhaus K, Wilcox M, Reps J, LaCross L. Leveraging digital technology in conducting longitudinal research on mental health in pregnancy: longitudinal panel survey study. JMIR Pediatr Parent. (2021) 4:e16280. doi: 10.2196/16280
Keywords: posttraumatic stress disorder, childbirth, mothers, perinatal mental health, questionnaire, DSM-5
Citation: Weigl T, Beck-Hiestermann FML, Stenzel NM, Benson S, Schedlowski M and Garthus-Niegel S (2021) Assessment of Childbirth-Related PTSD: Psychometric Properties of the German Version of the City Birth Trauma Scale. Front. Psychiatry 12:731537. doi: 10.3389/fpsyt.2021.731537
Received: 27 June 2021; Accepted: 08 September 2021;
Published: 06 October 2021.
Edited by:
Rafael A. Caparros-Gonzalez, University of Granada, SpainReviewed by:
Nathalia Garrido-Torres, Virgen del Rocío University Hospital Seville, SpainCopyright © 2021 Weigl, Beck-Hiestermann, Stenzel, Benson, Schedlowski and Garthus-Niegel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Susan Garthus-Niegel, c3VzYW4uZ2FydGh1cy1uaWVnZWxAdW5pa2xpbmlrdW0tZHJlc2Rlbi5kZQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.