
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Psychiatry , 18 November 2021
Sec. Autism
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.722874
This article is part of the Research Topic Early Intervention in Autism Spectrum Disorder (ASD) View all 11 articles
Autism Spectrum Disorder (ASD) is a neurodevelopmental disorder affecting multiple developmental domains including social communication, behavioral-affective, sensorimotor, and cognitive systems. There is growing evidence for the use of holistic, whole-body, Creative Movement Therapies (CMT) such as music, dance, yoga, theater, and martial arts in addressing the multisystem impairments in ASD. We conducted a comprehensive quantitative and qualitative review of the evidence to date on the effects of CMT on multiple systems in individuals with ASD. The strongest evidence, both in terms of quantity and quality, exists for music and martial arts-based interventions followed by yoga and theater, with very limited research on dance-based approaches. Our review of 72 studies (N = 1,939 participants) across participants with ASD ranging from 3 to 65 years of age suggests that at present there is consistent evidence from high quality studies for small-to-large sized improvements in social communication skills following music and martial arts therapies and medium-to-large improvements in motor and cognitive skills following yoga and martial arts training, with insufficient evidence to date for gains in affective, sensory, and functional participation domains following CMT. Although promising, our review serves as a call for more rigorous high-quality research to assess the multisystem effects of CMT in ASD. Based on the existing literature, we discuss implications of our findings for autism researchers and also provide evidence-based guidelines for clinicians to incorporate CMT approaches in their plan of care for individuals with ASD.
Autism Spectrum Disorder (ASD) is a neurodevelopmental disorder that affects multiple domains including the social communication, behavioral-affective, sensorimotor, and cognitive systems. Currently, around 1 in every 54 children in the United States qualify for a diagnosis of ASD (1) and boys are almost four times more likely to be diagnosed with ASD than girls of the same age (2). The hallmark impairments in ASD include poor reciprocal social interactions, difficulties with verbal and non-verbal communication, and restricted and repetitive behaviors and interests (3). For instance, children with ASD have difficulties in responding to social stimuli, sharing their play with peers and caregivers, developing and maintaining relationships, as well as understanding body language, gestures, and facial expressions of others (4–8). In terms of behavioral-affective impairments, children demonstrate repetitive and stereotyped behaviors such as finger flicking and hand flapping, highly circumscribed and restricted interests, insist on sameness relative to daily routines/schedules, demonstrate extreme distress to small changes in daily routines, and difficulties with transitions between activities (2, 9). Moreover, children may also have sensory symptoms including hypo- and hyper-sensitivity to sensory input and unusual responses to sensory stimuli in multiple domains including auditory, tactile-proprioceptive, vestibular, olfactory, and visual senses (9–12). In addition, children may also demonstrate disruptive behaviors such as aggression, tantrums, defiance, and self-injurious behaviors, as well as increased levels of negative affect (10, 11, 13, 14). Moreover, children with ASD also demonstrate cognitive difficulties such as attentional deficits, impaired decision-making, and impaired executive functioning (i.e., working memory, cognitive flexibility, self-control, generativity, and planning), with deficits being more pronounced during open-ended compared to structured settings (15–17).
Besides the diagnostic symptoms, children with ASD also exhibit a variety of other impairments within the sensorimotor domain that may lead to significant challenges in their activities of daily living (18–26). Although the exact prevalence estimates of motor impairments in ASD vary widely across studies from around 35% to over 85%, there is a growing consensus that children diagnosed with ASD exhibit motor impairments in gross and fine motor skills (e.g., bilateral coordination, gait and postural stability, handwriting, manual dexterity skills, and visuomotor control), as well as socially-embedded motor skills, including imitation, praxis (performance of skilled functional movement sequences/gestures), and interpersonal synchrony (ability to synchronize movements with those of another person) (19, 22, 27–38). Several studies have documented the association between motor impairments and severity of core autism symptoms in social communication, repetitive behaviors, and cognitive domains (22, 39–47). Moreover, sensorimotor difficulties could limit children's social participation and affect their activities of daily living including self-care, mobility, and leisure (41, 48–51). In short, children with ASD have multisystem impairments that need to be addressed through holistic evidence-based interventions (22, 24, 52–54).
Current standard interventions for ASD focus primarily on addressing the core social communication and behavioral impairments. Some popular evidence-based approaches include Applied Behavioral Analysis (ABA) (55), Treatment and Education of Autism and related Communication Handicapped Children (TEACHH) (56), Picture Exchange Communication System (PECS) (57), as well as developmental approaches such as Floor time (58), Social Communication, Emotional Regulation and Transactional Support Model (SCERTS) (59), Early Start Denver Model (ESDM) (60), and Pivotal Response Training (PRT) (61, 62). ABA-based approaches are considered the gold standard treatment for ASD and use principles of operant conditioning and intensive structured task practice to promote social communication and behavioral skills (55, 63–68). Similarly, the TEACHH approach uses visual cues to promote learning through picture schedules and also provides guidelines to increase structure and consistency in the environment, supplies-used, and therapists working with children with ASD (56, 69). Conventional therapies are usually very structured, adult-driven, and use a more sedentary approach (67, 70, 71). On the other hand, developmental approaches facilitate age-appropriate developmental skills such as joint attention, play, and imitation using child-preferred, play-based therapeutic activities within naturalistic settings (67, 70, 72). However, interestingly, both conventional and developmental approaches do not focus on addressing the sensorimotor impairments that are clearly highly prevalent in ASD (22, 46). This highlights a dire need to expand therapeutic interventions to address not just the core impairments but also the multiple co-morbidities in ASD.
Over the past several years, there has been a growing interest in exploring the effects of novel, alternative and integrated behavioral treatment approaches in addressing the multisystem impairments in ASD (27, 73–84). These holistic, whole-body movement-based, multisystem treatment approaches include but are not limited to structured physical activity, music therapies, yoga, martial arts, dance, and theater-based interventions (53, 73, 85–89). For the purpose of this review, we use the term “Creative Movement Therapy (CMT)” as an umbrella term that encompasses alternative behavioral interventions including music, dance, yoga, martial arts, and theater. The rationale for grouping these interventions together is that all these approaches use movement to integrate the social, emotional, cognitive, and physical aspects of the individual. Approaches involving CMT differ from conventional ASD interventions in that they are based in whole-body movement and promote self-expression (e.g., theater), creativity (e.g., innovative ways of moving body and using props in dance and theater), and improvisation (e.g., music making using instruments, moving to the rhythm of music). These interventions typically encourage child-led activities, playful exploration, and are therefore inherently more enjoyable and motivating for children with ASD (53, 90). From a theoretical perspective, CMT approaches are grounded in the ecological Dynamical Systems Theory (DST) (91, 92) and the Shared Affective Motion Experience (SAME) theory (93). The DST emphasizes that basic perception-action cycles of bodily movement form the basis for higher-order social communication and cognitive skills (82). Similarly, the SAME theory suggests that music- and movement-based experiences are multimodal in nature and activate similar “mirror” networks in the brain of participants, thereby forming the basis for social, emotional, and motoric connectedness between them (83). This is especially crucial for individuals with ASD given their deficits in multimodal integration stemming from long-distance brain under-connectivity (94–96).
In addition, given their very nature, CMT interventions are known to have multisystem effects on the sensorimotor domains as well as on the social communication, cognitive/attentional, and behavioral/affective domains in individuals with ASD. For instance, practicing simple and complex movement sequences during choreographed dance routines provides opportunities to promote rhythmic synchronization, multi-limb coordination, balance, gait, and postural control in participants (85). On the other hand, music-based group activities provide a medium for children with ASD to connect with social partners, improve communication abilities, and lead to greater positive affect/engagement (4, 6, 53, 93, 97–103). Similarly, short bouts of exercise that incorporate self-discipline, goal-oriented behavior, multistep action sequences, and sustained focus, as seen with any martial arts-based techniques, could enhance cognitive abilities such as executive functioning in children with ASD (104).
Although the preliminary evidence is promising, currently, it is unclear if CMT approaches can be considered as evidence-based interventions in ASD. Therefore, this review aims to synthesize the literature to date on the effects of CMT on social communication, behavioral-affective, cognitive, sensorimotor, and functional/participation skills of individuals with ASD across the lifespan (note that for the purpose of the review, we excluded studies that focused on structured physical activity, animal-assisted therapies, or technology-based interventions given the clear differences in the key intervention components of CMT approaches compared to the above-mentioned approaches). A few previous reviews have assessed the effects of CMT in children with ASD (75, 76, 78, 105). However, most of them have been restricted to examining the effects of a single type of CMT in individuals with ASD. It would be crucial to compile information on different CMT approaches to compare and contrast the differential effects of these approaches on multiple systems in ASD. Moreover, except a couple of reviews by Zou et al. and Geretsegger et al., none of the other reviews conducted a risk of bias analysis for the reviewed studies or calculated effect size (ES) estimates based on data reported in the reviewed literature (75, 105). Assessing methodological quality of studies through a risk of bias analysis enables researchers to estimate the level of confidence in study findings and guides interpretation of study results. Similarly, ES estimates from individual studies indicate the magnitude of the treatment effect and are thus crucial to evaluate the clinical utility of specific treatment approaches. We address these gaps in the literature by providing a comprehensive review of empirical reports studying the effects of CMT approaches through August 2021 in children with ASD. Specifically, we (i) summarize the narrative literature and compare the efficacy of different types of CMT in addressing multisystem impairments in individuals with ASD, and (ii) provide quantitative ES estimates for outcome measures addressed using CMT approaches to objectively evaluate the clinical importance of CMT for individuals with ASD.
We reviewed literature from four different electronic databases related to allied health, psychology, physical therapy/kinesiology, and education, namely, PubMed (1950–2021), PsycINFO (1969–2021), Scopus (1966–2021), and CINAHL (1937–2021). The combination of key terms used included, (a) “music,” “dance,” “yoga,” and “play,” (b) “intervention,” “therapy,” and (c) “autism” (please see Appendix 1 for details of search strategy). We also conducted additional hand searches of reference sections of included studies and previous review papers to identify missed literature through August 2021.
We included studies published in peer-reviewed journals that assessed the effects of creative movement and play-based therapies in individuals with ASD using experimental or quasi-experimental, longitudinal study designs. Studies were excluded based on the following criteria: (a) only included individuals with other developmental disabilities such as Cerebral Palsy, Down's Syndrome, Attention Deficit Hyperactivity Disorder, Intellectual disability, Spina Bifida, Dyslexia, Learning Disability, etc. [note that studies (N = 5) that recruited mixed samples i.e., individuals with ASD and individuals with other developmental diagnoses were included since we wanted the review to be comprehensive and inclusive of all studies that recruited samples of individuals with ASD], (b) review papers, case-studies, qualitative studies, purely narrative reports, observational studies or reports describing the protocol for a future study, (c) interventions directed solely toward parents/primary caregivers of individuals with ASD, (d) studies that used structured physical activity, animal-assisted therapies, or technology-based interventions in ASD, (e) reports in languages other than English, and (f) gray literature including theses and dissertations.
After screening 2,643 articles using our eligibility criteria [PubMed (1,354), PsycINFO (821), Scopus (267), and CINHAL (201)] and removing duplicates, 72 articles qualified for our review. Two trained research assistants and the last author screened titles and abstracts of the 2,643 articles based on our eligibility criteria. When necessary, full texts of articles were reviewed to assess eligibility of the study (see Figure 1 for details of search process). All three coders agreed in their ratings for 90% of studies. Disagreements between coders for study inclusion were resolved through discussions and consensus scoring.
We employed the Physiotherapy Evidence Database (PEDro) scale and the NIH quality assessment tool (106, 107) to assess risk of bias in reviewed studies. The PEDro scale was used to evaluate the internal and external validity of randomized controlled trials (RCTs) and controlled clinical trials (CCT's) included within our review. The PEDro has a total of 11 items which are scored on a dichotomous scale (No = 0, Yes = 1) of which 10 items are scored for each RCT/CCT to obtain a study score out of a maximum possible score of 10 (first item on the PEDro is not included in the total score) (106). Studies with a PEDro score ≥ 6 are classified as having low risk of bias. For single group pre-post designs, we used the NIH quality assessment tool to assess risk of bias (107). The NIH tool comprises 12 items that are scored on a dichotomous scale (No = 0, 1 = Yes) to assess internal validity of reviewed studies. Questions 6, 7, 9, and 10 include multiple questions per item. For these questions, if studies satisfied all criteria listed in the item, we gave them full points (score of 1). However, if studies satisfied some but not all criteria, a partial score of 0.5 was awarded for the item. The original tool recommends raters to categorize studies based on their risk of bias into categories of “good,” “fair,” and “poor” with studies rated as “good” having low risk of bias and studies rated as “poor” having high risk of bias (106). We classified studies with total scores ≥ 9 as “good,” studies with total scores ≤ 6 as “poor,” and all other studies as having “fair” quality. In addition to the above-mentioned tools, we also used the Levels of evidence as outlined by Sackett et al. (108) to classify all the 72 studies. This grading, based on study design, ranges from Levels I-V. We only included studies from Levels I up to III in our review. Level I is the highest level of evidence and includes systematic reviews, meta-analyses, and RCT's with a PEDro score of ≥ 6, Level II includes RCT's with a PEDro score < 6 and all CCT's, whereas Level III includes single group before-after (pre-post) study designs.
We coded each study in the review for sample and study characteristics, methodological quality, intervention characteristics (FITT: Frequency, Intensity, Time, Type), assessments used, dependent variables, and treatment effects (see Appendix 2 for coding details). In addition to a narrative description of studies, we also report on quantitative ES from reviewed studies along with their confidence intervals to obtain estimates of the true magnitude of treatment effects following CMT in individuals with ASD. For parametric data, when adequate data were provided in the original report, we calculated ES i.e., standardized mean difference (d) values (109–111). For papers that reported non-parametric statistics, ES were calculated using U- and z- statistics (112). In studies where the original report did not provide estimates of central tendency and variability of measured outcomes, we calculated ES using parameter estimates (F- and t-values) and p-values. We acknowledge that these estimates are more inaccurate compared to ES estimates calculated using measures of central tendency and spread within the sample (see Tables 4A–C for details); however, we wanted to provide readers with ballpark estimates of ES. We classified ES according to Cohen's conventions as small (0.1–0.3), medium (0.3–0.49), or large (0.5 and above) (113). We also report 95% confidence intervals (CI) around ES estimates to identify robust, statistically significant effects of CMT in ASD (114, 115). Specifically, if a CI does not include 0, it implies a truly significant non-zero treatment effect at the 5% significance level. For the purpose of reliability, all authors as well as 2 undergraduate students coded a subset of the 72 studies using a detailed coding form. Intra-rater reliability of over 99% and inter-rater reliability of over 90% were achieved through consensus coding on scores that coders disagreed on. Following reliability, rest of the papers were divided and coded by the first and last authors.
All 72 studies reviewed were published between 1994 and 2021 although only 25% of the studies specifically mentioned the year of data collection in the published report. Out of the 72 studies that we reviewed, 25 used music therapy approaches, 11 studies employed yoga-based interventions, 16 studies assessed the efficacy of martial arts-based interventions, 12 studies employed theater-based interventions, 7 studies assessed the effects of dance, and lastly, 1 study employed a combination of music and dance therapies. Of these studies, 30 were conducted in the US, 8 studies were from Iran, 6 from India, 4 from Germany, 3 each from UK and South Korea, 2 each from Hong Kong, Italy, Australia, and Brazil, 1 study each conducted in the Netherlands, Portugal, Greece, Spain, Portugal and Spain, France and Canada, and finally three studies that were subsets of the same larger study (98, 116, 117) were conducted simultaneously across multiple countries of the world including Norway, Austria, Australia, Israel, Brazil, Italy, UK, Korea, and USA. Several research groups reported on the exact same sample or on subsets of overlapping samples across multiple papers. Specifically, 4 of the music therapy studies by Srinivasan et al., 2 music studies by Kim et al., 2 yoga-based studies by Radhakrishna et al., 3 martial arts studies by Bahrami et al., and 2 by Phung et al. reported data from the same sample across multiple papers (4, 6, 27, 86, 101, 104, 118–123). Furthermore, 3 music therapy papers (98, 116, 117) reported on samples collected as part of the same, large-scale international study, 3 theater-papers reported on data collected across multiple cohorts by Corbett et al. (124–126) and 2 more martial arts studies had an overlap in reported samples (127, 128).
The 72 studies had a total sample size of 1,939 participants with ASD. Among the studies that did provide gender-related data (total N = 1,573), there were 1,338 males and 235 females. Sixty-six studies were conducted in children between 3 and 21 years, 5 studies included both children and adults, and only 1 study was conducted purely in adults with ASD (see Table 1). Specifically, the ages of participants across CMT approaches were as follows: music (3–38 years), yoga (3–23 years), martial arts (5–17 years), theater (6–21 years), and dance (8–65 years), indicating that within the studies that met our inclusion criteria, music, yoga and dance approaches were the three types of CMT approaches that have been implemented in adults with ASD. All studies provided interventions to individuals with ASD only, except one study that provided training to both individuals with ASD and their caregivers (146). All studies reported that participants did not have prior exposure to CMT.
Sixty-seven studies recruited only individuals with ASD and the remaining 5 studies included children with ASD as well as children with other diagnoses including ADHD, anxiety disorder, learning disability, sensory processing disorder, and emotional and behavioral disorder. Across studies, the diagnosis of ASD was confirmed using multiple measures including standardized tests, physician report and parent-report questionnaires (see Table 1). Specifically, 41 studies employed gold standard measures such as the Autism Diagnostic Observation Schedule (ADOS), Autism Diagnostic Interview-Revised (ADI-R), Gilliam Autism Rating Scale (GARS), and Childhood Autism Rating Scale (CARS) to confirm ASD diagnosis, 19 studies relied on physician diagnosis made using criteria listed in the Diagnostic and Statistical Manual of Mental Disorders (DSM) or the International Classification of Disease (ICD), and 12 studies did not provide details of methods used to confirm participants' ASD diagnosis (see Table 1). In terms of intellectual functioning of participants, only 27 of the 72 studies reported on assessing Intellectual Quotient (IQ) scores using various scales such as Wechsler Abbreviated Scale of Intelligence-2nd edition (WASI-2) or the PsychoEducational Profile (PEP). Overall, only five studies included children with mild intellectual disability in their sample, with the remaining studies including participants without any accompanying intellectual disability (101, 117, 119, 150, 170). Although a vast majority of included studies did not report on socioeconomic status, the remaining studies primarily included participants from middle and upper-middle class families.
Study sample sizes across the different CMT interventions were as follows: 764 participants in music therapy interventions (455 received experimental intervention and 309 received control interventions), 317 in yoga therapy (184 in experimental group and 133 controls), 326 in martial arts (176 in experimental group and 150 control group participants), 246 participants in theater training (162 received experimental intervention and 84 were in control group; 1 theater study (N = 8) did not provide the distribution of the sample into the intervention groups), 262 participated in dance-based studies (139 received experimental group intervention and 123 received a control intervention), and 16 participated in combined music and dance intervention (8 in experimental and 8 in control group). There was great variability in sample sizes across individual studies. The largest sample size studies for different CMT approaches included 364 participants for music therapies (116), 61 participants for yoga therapy (147, 152), 57 participants for dance therapy (173), 48 participants for martial arts (155), 77 participants for theater–based interventions (125), and 56 participants for dance and other combined therapies (173).
Out of the 72 studies, 34 studies were RCTs, 17 were CCTs, 18 were pre-post designs, 2 studies were cross-over designs, and 1 study employed a reversal design. We scored the PEDro scale for the 52 clinical trials (16 music, 7 yoga, 13 martial arts, 8 theater, 7 dance, and 1 combined dance and music intervention) and the NIH quality assessment tool for the 20 single group pre-post design studies (9 music, 4 yoga, 3 martial arts, 4 theater) reviewed to assess risk of bias (see Tables 2A,B). The clinical trials included in the review employed the following control groups: waitlist control, ABA therapy, routine or enhanced standard-of-care, seated play, school-based educational programming, social skills training, physical education training, robotic therapy, equine-assisted therapy, or no intervention. In terms of fidelity of implementation of training procedures, of the total 72 studies, around 25% (N = 18) used and provided details of specific checklists employed to monitor the consistency of treatment implementation, another 22% (N = 16) provided brief details of some form of fidelity checks, and 51% (N = 38) of studies did not provide any information on intervention fidelity. In terms of intervention implementation, music therapy and yoga therapy-based studies were almost equally split between an individualized vs. group-based format (Music: 13 out of 25 studies and yoga: 5 out of 11 studies provided individualized intervention), whereas martial arts (12 out of 16 studies), theater (10 out of 12 studies), dance (6 out of 7 studies), and combination-based approaches frequently employed group-based implementation with group sizes varying between 3 and 12 participants (see Table 1).
Out of the 52 clinical trials, 50% studies (N = 26) had a high risk of bias (PEDro scores <6). No study satisfied all the 11 criteria (see Table 2A). Among factors contributing to risk of bias, few studies concealed allocation of subjects to intervention groups (N = 8), and blinding of subjects (N = 1), therapists (N = 9), and assessors (N = 20) were ensured to a varying extent by reviewed studies. Although not as frequent, other factors associated with risk of bias included random subject allocation (N = 36 satisfied the criterion) and baseline similarity of groups on key prognostic measures (N = 33 satisfied the criterion) (see Table 2A).
Based on the NIH quality assessment tool rating used for assessing the 20 pre-post designs, 1 study was rated as “poor” indicating high risk of bias, 12 studies were “fair” indicating moderate risk of bias, and 7 studies were rated as “good” indicating low risk of bias. Specifically, none of the studies measured outcomes multiple times at pretest and posttest to get stable estimates of child performance, and all but three studies did not discuss power analyses to justify the choice of sample sizes. Another area of concern included blinding of assessors which was ensured in only 3 studies. Finally, 50% studies (N = 10) did not report on validity and reliability of assessed outcome measures, with 30% of the remaining studies (N = 6) reporting on only one but not both these measures (see Table 2B).
The mean duration of studies that provided music-based interventions was 12 weeks (SD = 9.73, Range = 4–52 weeks), with a mean frequency of around 2 sessions/week (SD = 1.3, Range = 2–5 times), and each session lasting around 40 min (SD = 14.9, Range = 30–90 min, see Table 1 for details). Studies that provided yoga therapy had the longest mean intervention duration of 20 weeks (SD = 23.99, Range = 4–82 weeks) with a mean frequency of around 3 times per week (SD = 1.81, Range = 1–5 times) for around 50 min per session (SD = 19.9, Range = 20–90 min). Martial arts and theater-based studies had similar intervention characteristics, i.e., average intervention duration ranged around 10 and 8 weeks respectively (Martial arts: SD = 3.44, Range = 4–14 weeks; Theater: SD = 3.38, Range = 4–12 weeks) and average frequency was around 2 sessions/week (Martial arts: SD = 1.01, Range = 1–4 times; Theater: SD = 1.86, Range = 1–5 times). However, the 2 CMT types differed greatly in terms of average session duration, with theater interventions (Mean ~175 min/session, SD = 90.56, Range = 60–300 min) lasting on an average for much longer time compared to martial arts interventions (Mean ~50 min/session, SD = 9.2, Range = 30–60 min). Lastly, interventions focusing on dance therapy had an overall mean duration of 9.5 weeks (SD = 1.76, Range = 7–12 weeks), with a mean frequency of around 1–2 sessions per week (SD = 0.78, Range = 7–12 weeks), and each session lasting for around 60 min (SD = 16.02, Range = 40–90 min).
In terms of intervention providers, most of the CMT approaches were provided by either licensed clinicians or specialized instructors trained in the CMT approach (N = 62). Fifteen studies (6 music, 3 yoga, 2 martial arts, 3 theater, 1 music and dance combined) asked teachers, caregivers, support staff, models, students or peers, etc. to assist in the intervention delivery process (see Table 1). Only 2 theater studies by Corbett et al. had teaching staff and peers deliver the intervention independently of clinicians after conducting a 2-day intensive training seminar (87, 165). Several papers mentioned using conventional ASD treatment strategies while providing CMT interventions to children with ASD. Common training strategies were based on principles of conventional ASD treatments such as ABA, TEACHH, and PECS and specifically included the use of picture schedules/visual cues, incremental prompting (verbal, gestural, modeling, hand-on-hand assistance), reinforcement schedules, structured and predictable training routines, motivational strategies, activities designed keeping in mind the participant's sensory needs, and the use of non-competitive, goal-directed, and child-led activities to ensure child compliance. Although a total of 15 studies (2 music, 2 yoga, 5 martial arts, 4 theater, 1 dance, 1 music and dance) mentioned progression in training across intervention weeks, only four of these studies (1 music, 1 yoga, 1 martial art, 1 theater) discussed specific principles of treatment progression over the course of the program. The remaining 57 studies provided no information on treatment principles and progression.
Common music therapy training approaches evaluated included Improvisational Music Therapy (IMT) and Relational Music Therapy (RMT). Similarly, yoga-based training approaches included Mandala Yoga and Mindfulness training, Relaxation Response-based training, and ABA based- integrated Yoga training. Common martial art approaches included Kata, Judo, Karate, Tai chi, and Taekwondo. Theater-based studies used programs such as the Social Emotional NeuroScience Endocrinology (SENSE) Theater, Social Competence Intervention Program (SCIP), and Socio-dramatic Affective Relational Intervention (SDARI). Lastly, Dance Movement Therapy (DMT) and traditional Greek dance were some of the approaches used in dance-based studies (see Table 1).
In terms of the location of intervention delivery, 5 studies (all music) delivered interventions at the child's home, 13 studies (4 music, 4 yoga, 2 martial arts, 1 theater, 1 dance, 1 music and dance) delivered interventions at the child's school, 30 studies (10 music, 1 yoga, 8 martial arts, 7 theater, 4 dance) provided intervention at other indoor settings such as a community center, YMCA, etc., 3 studies (1 music, 1 martial art, 1 theater) provided intervention either at the child's school or a community center, 2 studies (both yoga-based involving the same sample) conducted their intervention in a calm and open outdoor setting, and 19 of the remaining studies (5 music, 4 yoga, 5 martial arts, 3 theater, 2 dance) did not provide any specific information on where the intervention was provided.
Of the 72 studies reviewed, 31 reported within-group changes, 31 reported between-group differences, and 10 studies reported both between- and within-group changes. Studies used a combination of tests and measures including standardized tests, self-/parent-/teacher-reported questionnaires, video coding, and observational measures to assess the impact of CMT on multiple domains including social communication, behavioral-affective, sensorimotor, cognitive, functional skills, and quality of life (see Tables 3A–C, 6). Twenty-eight studies (16 music, 3 yoga, 1 martial arts, 6 theater, 1 dance, 1 combined music and dance) reported on the inter- and intra-reliability of the assessments employed. In terms of reporting treatment effects, 28 studies reported ES for the assessed outcomes (see Tables 4A–C). We were able to use data from the original papers to calculate ES in 64 out of the total 72 studies (i.e., 89% studies). Tables 4A–C provides a comparison between ES we calculated based on data provided in the paper and ES estimates reported in the original paper, and also discusses the level of agreement between both sets of estimates. Table 6 displays our results to indicate the number of studies stratified by CMT approach where calculated ES were statistically significant (i.e., CI did not include 0). Below, we provide a narrative description of the types of measures employed and summarize the salient treatment effects from the studies included in our review across the developmental domains. Please note that each section discusses the results reported in the original papers assessing those domains followed by a summary of the results from our own ES calculations for the specific domain.
A total of 47 studies i.e., 17 Level I (7 music, 1 yoga, 3 martial arts, 4 theater, 2 dance), 15 Level II studies (6 music, 1 yoga, 2 martial arts, 4 theater, 1 dance, 1 music and dance combined) and 15 Level III studies (7 music, 2 yoga, 2 martial arts, 4 theater) assessed changes in social communication skills following CMT (refer to section Risk of Bias Assessment for definition of levels; see Table 6). The social communication outcome measures employed included standardized tests such as the ADOS, CARS, and GARS, observational measures such as the ESCS and JTAT, parent/teacher-report questionnaires such as the ATEC, SRS, VABS, and SSRS, as well as video-based coding measures of joint attention, verbalization, and turn taking (see Tables 3A–C). All except one Level II study (121) reported quantitative data on social communication outcomes following CMT interventions. Using data from original reports, we were able to calculate a total of 91 ES, specifically, 38 ES from 12 out of the total 17 level I studies, 21 ES from 11 out of total 15 level II studies, and 32 ES from 9 out of the total 15 level III studies.
Of the 17 Level I studies, three studies reported no significant changes (1 martial arts, 1 theater, 1 dance) and 14 studies (7 music, 1 yoga, 2 martial arts, 3 theater, 1 dance) reported positive effects with small to large effect sizes (ES: 0.09–4.06) within their original report. Out of the 38 ES we calculated, CI for 14 ES from 9 studies did not include 0 (5 Music, 1 yoga, 2 martial arts, 1 theater). The largest multi-site study in our review that included 364 children from 9 countries was the only study that reported only small improvements on the social affect sub-domain of the ADOS (ES: 0.03–0.2) and the social motivation and autistic mannerisms subscales of the SRS (ES: 0.04–0.02) in the experimental group following a 20-week improvisational music therapy program compared to a comparison group that received a standard-of-care intervention; however, these findings were not statistically significant at the between-group level (116).
Among all 15 Level II studies, improvements of medium sizes (ES: 0.22–0.79) in social communication outcomes were reported in the original papers by music (6), yoga (1), martial arts (2), theater (4), dance (1) and combined music and dance (1) interventions, but out of the 21 ES we calculated, only 6 ES from 3 studies (2 martial arts, 1 theater) were statistically significant (CI did not include 0). In terms of the level III studies, only 3 of the 15 studies reported small to large ES on the ADOS and SRS following theater (2) and yoga (1) interventions (see Tables 4B,C). Similarly, despite large mean ES (0.88–3.04) estimates, only 6 out of the 32 ES we calculated from the 3 Level III studies did not include 0 (2 music and 1 theater).
Overall, out of the 91 calculated ES across 47 studies, 26 ES from 15 studies (~32% studies) were statistically significant (CI did not include 0) and indicated effects that were varying in magnitude from small to large (see Tables 4A–C, 6). Specifically, there is moderately strong evidence for beneficial effects of music (5 Level I and 2 Level III studies) followed by martial arts (2 Level I and Level II studies each), with limited insufficient evidence for yoga (1 Level I study), and theater (1 Level I, 1 Level II, and 1 Level III study) interventions in promoting social communication outcomes (see Table 6). One salient finding from our ES calculations is that although all 12 theater studies assessed social communication skills, only 3 of these studies (25%) showed significant improvement (CI of ES did not include 0) in social communication despite the heavy emphasis on peer-mediated social skill training in theater-based interventions (see Table 6). Taken altogether, our review suggests that there is moderate evidence from multiple Level I studies for small-to-large-sized improvements in social communication skills following mainly music and martial arts-based approaches.
Twenty-one papers in our review assessed behavioral outcomes i.e., 8 Level I (2 music, 1 yoga, 1 martial arts, 3 theater, 1 dance), 9 Level II studies (3 music, 2 yoga, 1 martial art, 1 theater, 1 dance, and 1 combined dance and music), and 4 Level III studies (1 yoga, 1 martial arts, and 2 theater). Behavioral states were assessed using standardized scales such as the GARS, Scale for Assessment of Negative Symptoms (SANS), and Pervasive Developmental Disorder Behavioral Inventory-Children (PDDBI-C), video-based coding of on- and off- task behaviors and the amount of redirection required during training sessions, as well as using questionnaire-based measures such as the Child Behavior Checklist (CBCL), Aberrant Behavior Checklist (ABC-C), and Autism Treatment and Evaluation Checklist (ATEC) (see Tables 3A–C). A total of 18 studies reported significant effects of CMT on behavioral skills, with the remaining 3 theater-based studies (87, 124, 166) reporting non-significant effects. Only 6 of the 18 studies that reported positive effects of CMT provided ES estimates in their original report ranging from small to large in magnitude. Furthermore, we were able to calculate a total of 39 ES from 14 studies, specifically, 8 ES from 5 out of the total 8 Level I studies, 20 ES from 6 out of the total 9 Level II studies, and 11 EFs from 3 out of the total 4 Level III studies. Our own calculations based on these papers suggested mostly medium effects for CMT (note that we obtained large ES estimates for 2 studies where F-values were used to calculate ES; however, these measures are more imprecise compared to ES calculations using means and SD/SE values).
As an example of positive intervention effects, Hartshorn et al. (130) reported significant, large improvements in on-task behaviors (ES: 1.28–4.11) from an early to a late training session following their Level II 8-week music and movement intervention compared to a no-intervention control group (130). Similarly, following a Level II, 14-week, Kata martial art intervention, the experimental group showed significant, medium-sized improvements on the stereotypy subscale (ES: 0.47–0.66) of the GARS compared to a control group, with gains retained at 1 month follow-up (122). Hildebrandt et al. conducted a Level II RCT to assess the effectiveness of a 10-week manualized dance movement therapy intervention on negative symptoms using the standardized, clinician-rated SANS scale in 78 individuals with ASD. The authors concluded that although the results did not reach statistical significance at the between-group level, they found promising trends for greater symptom reduction (ES: 0.008–0.47) in the experimental group compared to the waitlist control group in overall negative symptoms as well as most subscales of the SANS (177). Overall, out of the 39 total calculated ES across 14 studies, 17 estimates calculated from 7 studies (~50% studies), specifically, 2 music (Level II), 3 yoga (1 each of Levels I, II, and III), 1 martial art (Level III), and 1 theater-based (Level I) intervention were statistically significant (CI did not include 0). Although the present state of the literature is insufficient to systematically evaluate the differing effects of various types of CMT, there is currently some consistent evidence for medium-sized, positive effects of CMT in reducing behavioral symptoms in individuals with ASD.
A total of 20 studies, i.e., 5 Level I (1 music, 3 theater, 1 dance), 6 Level II (1 music, 1 yoga, 1 theater, 2 dance, 1 music and dance combined), and 9 Level III (3 music, 2 yoga, 4 theater) studies assessed affective outcomes using questionnaires such as the Empathy/Systemizing Quotient (EQ/SQ), Brief Psychiatric Rating Scale (BPRS) Positive and Negative Affect Schedule (PANAS-C), and a computerized test such as the Multifaceted Empathy Test (MET) (see Tables 3A–C). We found that only 4 out of the 20 studies (1 yoga, 2 theater, and 1 dance) reported non-significant effects, with majority of the remaining studies suggesting small to medium-sized improvements. From the studies that reported training-related affective improvements, we were able to calculate a total of 57 ES, with 5 ES calculated from 4 out of the total 5 level I studies, 34 ES obtained from 3 out of the total 6 level II studies, and 18 ES from 4 out of the total 9 level III studies assessing changes in affective states following CMT.
Among the 5 Level I studies that indicated positive effects following CMT (1 music, 1 dance, 3 theater), largest ES estimates were reported by the 2 studies by Corbett et al. that found improvements in affect/emotion recognition and a reduction in anxiety (ES: 0.49–0.97) following a 10-week Social Emotional NeuroScience Endocrinology (SENSE) theater intervention in 8–14-year-old children with ASD (87, 165). While the Level I dance study by Koehne et al. (171) found significant improvements in emotion interference and empathy (ES: 0.31) on a computerized Multifaceted Empathy Test (MET) following a 10-week imitation- and synchronization-based group DMT in youth and adults with ASD, the single Level I music-based study by Srinivasan et al. (118) reported only within-group improvements (ES: 0.32–0.43) in levels of negative and interested affect in the group receiving rhythm therapy.
Of the 6 Level II studies (1 music, 1 yoga, 1 theater, 2 dance, and 1 combined music and dance), a majority of the studies reported small to medium positive effects on empathy, emotional synchronicity, joy, and overall psychological well-being inclusive of anxiety, depressed affect, tension, and vitality (ES: 0.31–0.68). For example, Kim et al. used a within-subject comparison cross-over design for improvisational music therapy and toy play sessions in 10 children with ASD and found that children showed greater frequencies of joyful events and mirrored emotional synchronicity (ES: 0.47–0.55) with the therapist during music therapy sessions compared to toy play sessions (101). The 9 Level III pre-post designs provided the largest variations in ES estimates ranging from small to large (0.3–1.12) across multiple studies for multiple outcomes related to anxiety, self-esteem, empathy, resiliency, emotion recognition, and enjoyment during sessions. However, out of the total 57 calculated ES across all affective outcomes from 11 studies, only 3 ES—from one Level III music and one Level I theater-based intervention (~18% studies) had a CI that did not include 0. Moreover, similar to social communication outcomes, although a majority of theater-based studies assessed affective outcomes, our calculations suggest that only 1 study found significant, non-zero effects of the intervention on affective outcomes. Overall, our review suggests that although individual studies concluded small-to-large-sized positive effects, there is at present insufficient evidence supporting the beneficial effects of CMT on affective outcomes in ASD.
Taken altogether, we found only limited evidence from 26% studies (8 out of 31 studies) that were mainly Level II and Level III studies with high risk-of-bias for beneficial effects of yoga, music, martial arts, theater, and dance on behavioral-affective outcomes in ASD (see Table 6).
Of the three studies that assessed sensory skills using either questionnaires (Short sensory Profile, Questionnaire of movement therapy) or video coding-based measures, 2 Level II studies reported moderate-sized positive effects following dance and music interventions on children's body awareness and their negative response to touch (77, 130), with the 3rd theater-based study (Level III) reporting non-significant effects (124). We could calculate only 2 ES from 2 out of 2 Level II studies of which only 1 ES from a Level II music study did not include 0. Specifically, an 8-week intervention of music-based movement therapy led to improvements in children's negative response to touch (ES: 0.59) during training sessions compared to a waitlist control group (130). Although Koch et al., reported moderate improvements in awareness of body movement (ES: 0.62) after a 7-week long manualized DMT intervention, the CI of the calculated ES included 0 [(77); see Tables 4A–C]. Given the few studies that have assessed effects of CMT on sensory outcomes, at present, there is insufficient evidence to make definitive conclusions on the effects of CMT approaches on sensory outcomes in ASD.
Fifteen studies that assessed motor outcomes, i.e., 5 Level I (1 music, 2 yoga, 2 martial arts), 6 Level II studies (2 music, 1 yoga, 1 martial arts, 1 dance, 1 music and dance combined), and 4 Level III studies (2 music, 1 yoga, 1 martial arts) used standardized tests such as the Bruininks-Oseretsky Test of Motor Performance-2nd Edition (BOT-2), Movement Assessment Battery-2nd Edition (MABC), and the Korperkoordinationstest fur Kinder (KTK), questionnaires such as the ATEC and imitation test battery, as well as observation-based quantitative measures such as posturography, and video-coding for imitation and interpersonal synchrony. Out of the 8 studies that reported ES estimates, five studies (1 music, 1 yoga, 2 martial arts, 1 music and dance combined) reported medium-to-large positive effects of CMT and 3 music-based studies (1 Level I, 1 Level II, and 1 Level III; see Tables 2A,B) reported non-significant effects on motor skills following intervention (120, 138, 140). However, even among the clinical trials, 3 studies (27, 150, 157) reported only within-group effects suggesting that the positive effects were perhaps not robust enough to attain statistical significance at the between-group level. We were able to calculate a total of 18 ES, i.e., 10 ES from 4 out of the total 5 Level I studies, 5 ES from 1 out of the total 6 Level II studies and 3 ES from 2 out of the total 4 Level III studies assessing motor outcomes.
Large effects were obtained from the Level I study by Sarabzadeh et al. (158) on ball skills and balance subscales (ES: 3.14–3.16) assessed using the standardized MABC-2 test after a 6-week Tai Chi Chuan martial arts-based intervention. Similarly, the single Level II dance intervention that assessed motor outcomes reported improvements in the Korperkoordinations test fur Kinder (KTK) test (ES: 0.88–2.63), a measure of neuromuscular coordination including balance and agility, following an 8-week traditional Greek dance program in 5 children with ASD (85). Of the 3 studies that employed quantitative measures to assess motor outcomes, Garcia et al. in a Level III study reported large improvements in moderate-to-vigorous physical activity levels (MVPA) (ES: 0.97) using Actigraph GT9X accelerometers following a judo intervention in children with ASD (127). The other Level I and II studies reported improved static and dynamic balance and reduced postural sway during an eyes closed single leg balance task, respectively (ES: 0.5–5.34), following a 10-week Kata and an 8-week Taekwondo intervention in children with ASD, respectively (157, 159). Overall, out of the 18 ES calculated from 7 studies, CI for 8 ES calculated from 4 Level I studies (2 yoga, 2 martial arts) and 1 Level II study (music) did not include 0 (~71% studies). Therefore, there seems to be limited, yet very promising evidence from mainly Level I studies for medium-to-large sized improvements in motor outcomes following martial arts and yoga-based interventions in ASD.
Therefore, altogether across the sensorimotor domain, there is limited evidence from around 28% studies (5 out of 18 studies, i.e., 4 Level I and 1 Level II) which showed improvements in assessed outcomes following predominantly yoga and martial arts interventions (see Table 6).
The 6 Level I studies (2 yoga, 4 martial arts) that assessed cognition used EEG measures to record neural activity, computerized tests such as the Go-No-Go and the Hearts and flowers test, as well as questionnaires such as the ATEC to report medium to large ES for improvements in executive functioning, visual memory, cognitive awareness, and brain activation patterns following CMT (104, 148, 152, 154, 155, 161) (see Tables 3A,B, 6). For instance, Chan et al. reported large improvements in self-control (ES: 0.84), indicated by a reduction in the # of rule violations during a Tower of London task following a Nei Yang Gong martial arts intervention compared to a control group that received progressive muscle relaxation (154). Similarly, following a 13-week mixed martial arts intervention, Phung and Goldberg reported improvements in accuracy (ES: 0.83–1.01) on the computerized Hearts and Flowers executive functioning test (104). Of the 22 ES we could calculate from the 6 studies, the CI of 14 ES from 4 Level I studies (2 yoga, 2 martial arts) did not include zero (~66% studies) (see Table 6). We found some disagreements between reported and calculated ES (see Tables 4A–C for details) (104, 154); however, our overall assessment suggests limited promising evidence for medium-to-large sized improvements in cognitive skills following martial arts and yoga-based interventions.
Three studies assessed activities of daily living and QOL using self- and family-report questionnaires such as the World Health Organization-Five Well-being Index (WHO-5), the WHO Disability Assessment Scale (WHODAS) and the Functional Independence Measure (FIM). Of these, 1 study each of Level I and II, respectively (1 music and 1 dance + EAT) [(116, 174); see Tables 3A–C, 6] reported non-significant between-group effects on QOL and functional participation, whereas a single Level III study found medium-sized within-group improvements in QOL following a yoga-based intervention (146). Specifically, de Bruin et al., reported medium-sized improvements in QOL in adolescents with ASD measured on the WHO-5 well-being index (ES: 0.55–0.63) following a 9-week mindfulness training intervention (146). Although Souza-Santos et al., reported non-significant between-group differences, they found within-group improvements in the dance and combined dance and equine-assisted therapy intervention groups on the Functional Independence Measure (FIM) and WHO Disability Assessment Scale (WHODAS) (174). Based on reported data, we could only calculate 6 within-group ES from a single Level II study. Our calculations confirmed the findings from Souza-Santos et al. (174) with within-group ES estimates ranging from 0.64 to 0.73 and their CI not inclusive of 0. However, overall, at present, there is insufficient evidence to indicate any benefits from CMT on functional participation and QOL of individuals with ASD.
Sixteen (4 Level I, 6 Level II, 6 Level III) out of the 72 papers assessed effects of CMT on other domains including, (1) physiological parameters such as sleep, gastrointestinal (GI) problems, heart rate variability, and cortisol levels, (2) training-specific skills such as musical abilities and mindful awareness, and (3) cost effectiveness of provided interventions and parent-reported adverse effects (see Tables 3A–C, 6). A combination of quantitative measures such as ECG recordings and salivary cortisol levels, standardized tests, and patient/caregiver-report questionnaires were used to assess these miscellaneous outcomes. For instance, Corbett et al. assessed the effects of theater-based interventions on salivary cortisol levels, a marker for physiological stress, in 3 separate studies, 2 of which were Level III pre-post designs and one was a Level I RCT (87, 124, 126). While theater interventions had large within-group effects (ES: 0.73–2.55) for reducing cortisol levels in participants during and after the intervention (124, 126), the effects were not strong enough to attain significance at the between-group level (87). A single Level II study also reported significant medium-sized effects (ES: 0.3–0.64) on a questionnaire-based assessment of sleep and GI problems in children with ASD following a 90-day yoga training program (147). Two Level III studies that assessed training-specific musical skills reported mostly large effects (ES: 1.13–2.67) on musical vocal behaviors, rhythmic imitation of musical patterns, turn taking within musical contexts, instrument playing, and singing following music therapy sessions (129, 131). No statistically significant effects were demonstrated on mindful awareness and heart rate variability following CMT (151). Three studies reported positive trends in qualitative data on parent/teacher and participant satisfaction, feasibility of implementation, and social validity of CMT (116, 140, 166).
We were able to calculate a total of 66 ES from 7 studies, i.e., 9 ES from 2 out of the total 4 Level I studies, 31 ES from 1 out of the total 5 Level II studies and 26 ES from 4 out of the total 6 Level III studies. Out of these 66 calculated ES, 8 ES from 2 Level I studies (1 yoga, 1 theater) and 12 ES from 4 Level III studies (2 music, 2 theater) suggested mostly medium-to-large-sized effects on assessed outcomes (see Tables 4A–C, 6). Overall, there is preliminary evidence from mostly within-group designs supporting the effectiveness of music therapies in enhancing children's musical skills and theater-based interventions in improving salivary cortisol levels and reducing stress in individuals with ASD.
The efficacy and utility of any therapy depends not only on the effects assessed during and immediately following the intervention, but more importantly on the carryover of training effects into real-world settings beyond the duration of the training. Only 17 (7 Level I, 7 Level II, 3 Level III studies) out of the 72 studies assessed the short- and long-term effects of CMT through follow-up (FU) testing that was conducted between 2 weeks and 12 months post-intervention. Of the 17 papers, only 9 (2 music, 1 yoga, 3 martial arts, 3 theater) studies found sustained improvements in outcomes at FU. The music studies (116, 140) that compared rock drumming and improvisational music therapy, respectively, with standardized care found improvements in social and motor outcomes at 2 weeks and 12 months FU, respectively (see Table 3A). Three martial arts-based studies from a single group of authors found retention of positive improvements on behavioral and social communication outcomes at 1-month FU (see Table 3B) (86, 122, 153). Sustained improvements were also seen following the SENSE theater and SDARI interventions in social communication and behavioral domains (see Table 3C) at 1.5- and 2-months post-intervention respectively (163, 165). The only study in the review that conducted multiple FU sessions (at 3, 6, and 12 months) assessed the effects of a drama-based intervention on social communication and behavioral outcomes (170). However, the study only reported outcomes at the final FU visit and suggested sustained improvements in autism severity and emotion recognition at 12 months post-intervention compared to baseline values (170). Lastly, 1 yoga-based intervention study found sustained improvements in executive functioning at 1.5 months post intervention compared to the posttest and baseline measures (152). On the other hand, 8 studies (3 music, 1 yoga, 1, martial arts, 1 theater, 2 dance) found that the immediate beneficial effects of CMT were not sustained at FU (87, 134, 136, 137, 146, 172, 173). Overall, although 9 of the 17 papers claimed sustained beneficial effects of CMT in individuals with ASD, our calculations suggested that only 4 out of the 22 calculated ES (ES: −0.79–0.71) from a Level II yoga and a Level III theater-based intervention study (152, 170) were statistically significant (i.e., CI did not include 0). Thus, there is currently insufficient evidence for short-to-long-term sustained benefits following CMT in individuals with ASD.
Creative movement therapies have been an ongoing topic of study over the past 3 decades. Within CMT approaches, the effects of music- and yoga-based therapies have been studied since the 1990s and 2000s, whereas dance, theater, and martial arts have been studied only more recently over the past decade. Given that this area of study is still in its infancy, there is presently lack of rigorous, definitive evidence supporting the use of CMT approaches within the standard-of-care clinical practice in ASD. There have been a few reviews in the past assessing the individual effectiveness of music, yoga, martial arts, theater, and dance approaches in individuals with ASD. Despite the common underlying theoretical framework and the key intervention ingredients across these different approaches, to date, there has been no umbrella review that has systematically compiled evidence across different types of CMT approaches in individuals with ASD. Our paper addresses this critical gap by providing a comprehensive review of the literature through August 2021, supplemented with a critical risk of bias assessment on different CMT approaches as applied to individuals with ASD. By conducting both a narrative literature synthesis and a quantitative review through calculation of ES estimates of treatment effects, we are able to systematically compare and contrast the efficacy of different types of CMT approaches in individuals with ASD.
Of the total 72 studies, we were able to calculate within- and/or between-group ES estimates for around 89% studies (23 music, 7 yoga, 16 martial arts, 10 theater, and 7 dance, 1 music and dance) of which around 45% studies (N = 29) showed statistically significant, non-zero effects of CMT on assessed outcomes across domains. Specifically, we found evidence for (1) medium- to large-sized improvements in social communication skills from over 30% of the studies (mostly Levels I and II) that assessed these outcomes, (2) medium-sized improvements in the behavioral domain from around 33% studies (mostly Levels II and III) that assessed these skills, (3) medium-to-large improvements in motor outcomes from around 33% studies (mostly Level 1) that assessed movement performance, and (4) medium-to-large improvements in cognitive skills from over 65% (all Level I) of the studies that assessed this domain. In comparison, we found limited evidence to date for the positive impact of CMT on sensory, affective, and functional participation domains. In terms of CMT types, our review suggests that there is presently strongest evidence for the beneficial effects of music-based therapies in promoting social communication skills (5 out of 7 Level I music studies), followed by limited, yet positive evidence for both martial arts and yoga in promoting motor and cognitive skills (2 Level I studies for each approach for each domain), and for martial arts in promoting social communication skills (2 out of 3 Level I studies). Below we summarize the potential mechanisms of change for individual CMT approaches.
Our literature search revealed the largest number of studies for music-based interventions compared to all other CMT approaches, with around 40% studies reporting significant improvements (ES: 0.02–4.11) in measured outcomes. Specifically, 35% studies (N = 7) showed improvements of varying sizes in social communication skills (ES: 0.02–4.06) and around 38% (N = 3) studies suggested large improvements in behavioral-affective outcomes (ES: 1.28–4.11).
Previous literature in the field of music and autism suggests that children with ASD particularly enjoy musical experiences, and in fact have enhanced musical perception skills (53, 178). From a brain imaging standpoint, there is substantial evidence that musical practice promotes multimodal integration by activating long range connections that simultaneously engage the auditory, visual, somatosensory, motor, and premotor areas as well as brain networks such as the mirror neuron system that are especially dysfunctional in ASD (52, 101, 106). Given the considerable overlap between brain substrates underlying speech and music, and the overall structural similarity between music and language, it has also been argued that musical training can in fact lead to enhanced speech processing in individuals with ASD (52). Overall, there is considerable behavioral and neuroimaging evidence to support the mechanisms for beneficial effects of music-based training in ASD (179).
Our review findings of consistent improvements in social communication skills following music therapies is not surprising given that such activities are based in rhythm, melody, and harmony, and involve components of singing, listening, music making with instruments, moving to the beat of the music, and spontaneous improvisation, all of which provide abundant opportunities for practice of social communication skills such as turn taking, joint attention, imitation, and verbal communication (53). Several of the reviewed studies also provided opportunities for flexibility and child-led activities during training that probably fostered children's engagement and led to better outcomes (4, 6, 27, 118, 119, 135). Although authors also hypothesized that musical training provides a non-intimidating context that may contribute to a reduction in off-task behaviors, stereotypes, and other repetitive behaviors in participants (130, 131), there is presently a need for more rigorous, high-quality research to support the use of music-based approaches in improving behavioral impairments in ASD. Moreover, music making using different types of instruments challenges the fine motor and cognitive systems as it typically involves complex, sequential, and precise finger and hand movements that require intricate motor planning and execution (53). Although the current evidence on the effects of music-based interventions on sensorimotor and cognitive skills is scant, this is definitely an area that deserves further attention.
Taken altogether, although music therapy approaches have the strongest evidence among other CMT approaches, there is a clear need for more research to assess the multisystem effects of these interventions on primary and secondary comorbidities in ASD.
Yoga-based interventions fall under the category of holistic mind-body therapies and are based on principles and techniques of yogic practice that date back several millennia to ancient India. Yoga and mindfulness practice has been postulated to have physical, mental, and spiritual effects (180, 181). Studies included in our review evaluated the effects of yoga practice on behavioral, social communication, and motor skills as well as on physiological parameters, with very few studies assessing effects on affective control, cognitive, and functional skills. We were able to calculate ES estimates from around 55% of all yoga studies; nevertheless, a majority of the studies indicated medium-to-large improvements (ES: 0.43–2.66) in measured outcomes. Our analyses indicated promising beneficial effects in behavioral regulation (N = 3, ES: 0.43–2.66), motor (N = 2, ES: 0.76–2.66), and cognitive skills (N = 2, ES: 0.91–1.42) following yoga-based interventions.
Yoga-based programs emphasize the practice of breathing control and mindful body awareness that may help individuals with ASD manage their behavioral and mood/affective symptoms (88, 145, 148, 150). Moreover, the practice of static and dynamic postures that focus on improving balance, core muscle strength, flexibility, and body awareness may impact the sensorimotor systems (150) and also have physiological effects on digestion, sleep, and HR variability (88, 145, 148); see Table 5 for components). Yoga and mindful awareness have also been found to help with attention regulation, memory, and executive control (152, 154, 155). Additionally, the only study that provided mindfulness training to adolescents with ASD and their caregivers found improved quality of parent-child interactions as evidenced by decreased parental stress and improved behavioral regulation (146). Despite extensive evidence for the whole-body effects of yoga in healthy individuals (182–184), our review suggests that the use of yoga-based interventions in ASD is presently an under-researched topic that deserves greater systematic investigation.
Around 56% of reviewed martial arts-based studies reported significant small-to-large improvements in measured outcomes (ES: 0.29–5.34), specifically in social communication (N = 4, ES: 1.13–1.15), cognitive (N = 2, ES: 0.42–1.19), and motor (N = 2; ES: 3.14–5.34) domains. Moreover, improvements in the cognitive domain i.e., in executive functioning, which includes working memory, flexible thinking, and inhibitory control are supported by high-quality Level I studies [(104, 154, 161); see Table 6]. This is not surprising given the heavy emphasis in martial arts training on discipline, structured practice of multistep action sequences, and movement precision, all of which require focused attention, motor planning, task switching, and working memory (75, 104, 123, 154, 159).
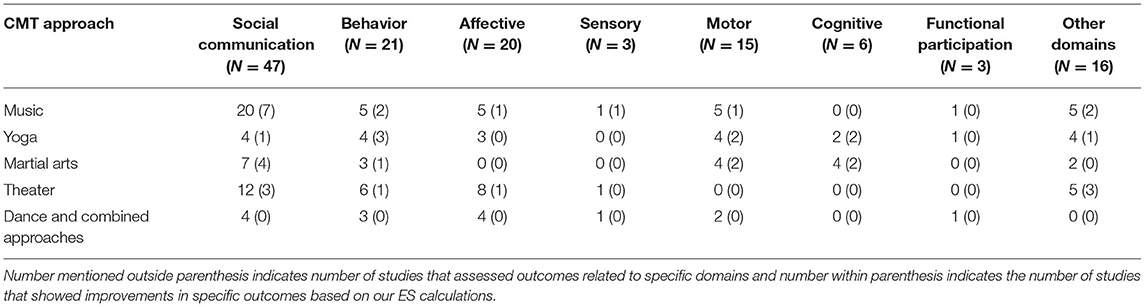
TABLE 6. Summary of reviewed studies that assessed specific domains and number of studies that showed improvements based on ES calculations.
The reviewed studies also suggested the potential for martial arts training to impact socialization, behavior, and motor skills. For instance, martial art training led to improved synthesis and metabolism of neurotransmitters oxytocin, serotonin, and dopamine (75, 122). In fact, disturbed metabolism in these very neurotransmitter systems is thought to underlie the social dysfunction and stereotypies commonly seen in individuals with ASD (75, 122, 153). Similarly, high-energy, dynamic, martial art movement routines are thought to physically resemble stereotypical movements characteristic in ASD, perhaps serving as a functional “substitute” for repetitive behaviors, while still providing the same level of sensory input and reinforcement (75, 122). Although there is presently evidence from only 2 Level I studies, it seems plausible that martial arts training may also have effects on the sensorimotor system through practice of poses and action sequences that require good postural control, balance, multi-limb coordination, strength, agility, and optimal processing in the vestibular- and tactile-proprioceptive systems (104, 158). Our review of the existing literature suggests that among all CMT approaches, martial arts-based therapies seem to have the strongest evidence at present for promoting multisystem development in social communication, behavior, motor, and cognitive domains.
Although a majority of theater-based studies assessed social communication and behavioral-affective outcomes, only around 42% (i.e., 2 Level I, 1 Level 1 and 2 Level III studies) of reviewed studies reported medium-to-large improvements (ES: 0.56–2.55) across these domains as well as a reduction in cortisol levels (ES: 0.73–2.55) following theater training. In fact, 2 of these studies were conducted by the same research group (126, 165). The reviewed theater studies typically provided training in a group format emphasizing interactions with peer models, specialized instructors, teachers, and other staff (87). Such a socially embedded and interactive context may provide plenty of opportunities for individuals with ASD to practice critical social communication skills such as joint attention, turn taking, perspective taking, and dialogue delivery, while also learning to recognize and express subtle socio-emotional cues related to facial expressions, voice intonation, and body language. It is therefore surprising to see a lack of statistically significant effects in support of enhanced social communication and behavioral-affective skills following theater training. A salient difference between theater and other CMT approaches is the average session duration, with theater interventions on an average lasting for much longer, i.e., around 2.9 h/session (see Table 5). It remains to be seen if the long duration of intervention sessions impacted abilities of individuals with ASD to sustain engagement during the training program. Overall, despite the highly interactive nature of theater, at present, there is insufficient evidence to support the use of theater-based training to facilitate social communication and behavioral-affective skills in individuals with ASD.
Although all individual reports (N = 8; 2 Level I, 6 Level II) concluded positive effects of dance-based therapies, our ES calculations from data reported in 6 papers suggested that none of the ES were statistically significant. This was the singular approach where studies recruited participants across the lifespan from 14 to 65 years. The wide age-range might have added to the variability of data, undermining the effects reported in these studies. Dance is an embodied experience incorporating elements of complex coordination, motor planning, and balance that may provide individuals with ASD opportunities to express their emotions through fluid bodily movements and to engage in mirrored practice during group choreography (172, 173). Despite the potential for promising effects on multiple systems through the very embodied nature of the experience, the current evidence on dance therapy in ASD is very limited. We call for future research to fully explore the use of dance-based interventions in individuals with ASD. We specifically recommend that future studies assess the effects of dance approaches on participants within a narrower age range.
Based on the studies reviewed, we suggest intervention guidelines for clinicians working with individuals with ASD in terms of assessments and interventions pertaining to CMT approaches. In terms of assessment measures, we recommend that clinicians use a combination of domain-specific standardized tests, observational measures, parent report questionnaires/interviews, and video coding to assess the impact of CMT approaches on multiple systems (see Tables 3A–C). Ultimately, the choice of assessment tools will depend upon multiple factors including the domains assessed as well as participant characteristics such as age, autism severity, functional level, receptive and expressive communication, and intellectual abilities. From our own experience, we recommend that objective clinician-based assessment tools be supplemented with parent reports to allow assessment of the individual's skills across a variety of structured and naturalistic activities and environments. We also recommend that researchers collect video data of testing and training sessions that can be scored at a later time by unbiased coders, thereby again allowing an evaluation of multiple snapshots of target behaviors across a variety of settings such as the lab, home, school, etc.
In terms of treatment, Table 5 provides a summary of our suggested intervention guidelines for the different CMT training approaches in terms of FITT principles (Frequency, Intensity, Time, Type). Note that our guidelines are based on the reviewed literature, specifically, training programs that led to appreciable improvements in assessed treatment outcomes. The choice of CMT approach should ultimately depend on the preferences of the individual with ASD/their family. Clinicians should choose the approach that their client is most excited about and that they are comfortable delivering. Moreover, based on the evidence from this review, we recommend that there is at present, most consistent evidence from high-quality studies with low risk of bias for enhancements in social communication skills following music and martial arts interventions, and in motor and cognitive skills following yoga and martial arts practice. There is need for more systematic research to support the use of theater and dance-based approaches in the plan of care of individuals with ASD.
To administer CMT interventions to their clients with ASD, allied health professionals may need to consult with certified instructors and work collaboratively with them to tailor interventions to their client/family's needs. Moreover, several studies reported using common training strategies derived from conventional ASD treatments such as ABA, PECS, TEACHH, etc. while delivering CMT approaches with individuals with ASD. While structured practice will be an integral part of every CMT-based session, we strongly recommend that clinicians reserve time during sessions for free play and improvisation that will afford individuals with ASD opportunities for creative movement exploration and self-expression. Although there is a need for more rigorous research in this field, our review certainly suggests that CMT approaches involve embodied experiences that engage multiple systems/domains, are fun and engaging, and may provide individuals with ASD a variety of activity options fostering lifelong learning and creative expression.
Around 75% of the reviewed studies employed between-group designs; however, <50% of the total studies were RCTs which are considered the gold standard for intervention efficacy research. There is a need for greater methodological rigor of clinical trials to reduce risk of bias by ensuring random and concealed assignment of participants to intervention and control groups, blinding of therapists and assessors, ensuring baseline similarity between groups prior to group assignment, and employing intention-to-treat analyses when possible. Since RCTs require significant amount of financial and personnel-related resources and are not always feasible to conduct in clinical settings, several studies in our review used pre-post designs. Our risk of bias assessment for pre-post designs indicated a need for better justification of sample sizes using power analyses, administration of tests at multiple times to obtain stable estimates of the child's behavior at baseline and post-intervention, better assessment and reporting of validity and reliability of selected outcome measures, and blinding of assessors to ensure unbiased estimates of participant performance.
Overall, across all study designs, we recommend that future studies provide more information on sample characteristics within the original report including measures of autism severity, IQ levels, as well as functional skills assessed using parent questionnaires such as the VABS. This is crucial since, the effects of CMT approaches might differ across participants based on these above-mentioned characteristics. Interestingly, a very small proportion of the reviewed studies included participants with intellectual disability and similarly even fewer studies recruited youth and adults with ASD, suggesting a need for more research with these subject demographics. In terms of study quality, future studies should report on steps taken to assess and ensure treatment fidelity during intervention delivery.
Among reviewed CMT approaches, the greatest quantity of evidence is for music-based interventions; there is therefore, a need for more rigorous research on other CMT approaches as well as efforts directed toward replication of the effects of music-based therapies on multiple systems in ASD using large sample size studies. Specifically, our review suggests that yoga- and martial arts-based therapies may be promising to promote multisystem development in individuals with ASD. Although reviewed studies assessed a variety of outcomes, the most frequently assessed domains included social communication and behavioral skills. Given the embodied nature of CMT approaches and their proposed mechanism of action on multiple systems, it would be important for future studies to holistically assess other developmental domains including sensorimotor, affective, and cognitive systems that also present as significant challenges for individuals with ASD. Moreover, researchers should go beyond the impairment domain and begin assessing the impact of CMT approaches on function and participation of individuals with ASD. In order to understand the carryover effects of CMT approaches, studies will need to assess treatment effects both in terms of short-term effects i.e., immediately following intervention completion, as well as the long term maintenance of training-related gains at follow-up. Finally, we urge that authors include their data within the original reports to enable calculation of ES estimates for measured outcomes and meta-analytic analyses.
Although we used a comprehensive search strategy (see Appendix 1) to identify eligible studies, it is possible that we may have missed relevant research. For the purposes of our review, we only included clinical trials and pre-post study designs with the exclusion of case studies, narrative reports, and other types of qualitative reports. We also excluded conference proceedings and unpublished theses and dissertations from this review. Finally, we limited our review to only articles published in English. Although our original intention was to restrict our review to studies that used CMT approaches in individuals with ASD, there were a few papers (N = 5) in our review that recruited mixed samples, thereby adding to the heterogeneity of the sample. In terms of intervention components, several studies reported using training strategies derived from conventional, evidence based ASD treatments while delivering CMT to participants. Therefore, at present, the literature does not allow us to tease apart the true effects of the key ingredients of the CMT approaches themselves vs. those of the training strategies used in conjunction with the CMT approaches. In a related vein, a majority of the studies did not report on acceptability, implementation feasibility, cost-effectiveness, etc. of interventions. The extent of the literature does not presently allow the development of clinical practice guidelines for the ASD population; instead, the suggested treatment guidelines reported in our paper are based only on the reviewed studies and the dosing parameters that led to gains in measured outcomes in the reviewed studies.
Our systematic review aimed at providing a comprehensive summary of the literature through August 2021 on the effects of various types of CMT approaches for individuals with ASD. Our search identified a total of 72 articles that used music, yoga, martial arts, theater, and dance-based intervention programs in 1,939 number of individuals with ASD between 3 and 65 years. Our quantitative synthesis of the published literature suggested strong and consistent evidence for small-to-large improvements in social communication skills following music and martial arts training as well as medium-to-large sized improvements in motor and cognitive skills following martial arts and yoga training. Presently, there is limited evidence in support of theater and dance-based approaches as well as the utility of all CMT approaches in improving affective, sensorimotor, and functional participation skills in individuals with ASD. Our review offers future directions for research examining the effects of CMT approaches in ASD as well as provides intervention guidelines for clinicians to incorporate CMT approaches in their plan of care for their clients with ASD.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
SS was responsible for conception of the manuscript. WCS, AB, and SS were involved in project design. NA and SS finalized and coded the articles and were responsible for data extraction and analyses. NA and SS put together the first draft of the manuscript. All authors were involved in proof reading and editing of the manuscript prior to submission.
AB's research was supported by a Clinical Neuroscience Award from the Dana Foundation and multiple grants from the National Institutes of Health (Grant #s: 1S10OD021534-01, P20 GM103446, 1R01-MH125823-01). SS's efforts on this project were supported through multiple internal grants from the University of Connecticut: Scholarship Facilitation Fund (SFF), Research Excellence Program (REP) Award, and a seed grant from the Institute for Collaboration on Health, Intervention, and Policy (InCHIP).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We would like to thank undergraduate students Emma Burleigh, Nitya Yelamanchili, Pranati Mathur, Amber Bardsley, and Gaganjot Bedi at the University of Connecticut who assisted in the initial screening of the literature, coding of a subset of the studies to establish reliability with the authors, and data entry into Excel. The authors would like to thank librarian Jill Livingston who was at the University of Connecticut at the time this review was conducted for her help in designing the search strategy and conducting the comprehensive search across multiple databases.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.722874/full#supplementary-material
1. Knopf A. Autism prevalence increases from 1 in 60 to 1 in 54: CDC. Brown Univ Child Adolescent Behav Lett. (2020) 36:4. doi: 10.1002/cbl.30470
2. Maenner MJ, Shaw KA, Baio J, Washington A, Patrick M, DiRienzo M, et al. Prevalence of autism spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2016. MMWR Surveill Summ. (2020) 69:1–12. doi: 10.15585/mmwr.ss6903a1
3. Young RL, Rodi ML. Redefining autism spectrum disorder using DSM-5: the implications of the proposed DSM-5 criteria for autism spectrum disorders. J Autism Dev Disord. (2014) 44:758–65. doi: 10.1007/s10803-013-1927-3
4. *Srinivasan SM, Eigsti I, Gifford T, Bhat AN. The effects of embodied rhythm and robotic interventions on the spontaneous and responsive verbal communication skills of children with autism spectrum disorder (ASD): A further outcome of a pilot randomized controlled trial. Res Autism Spectrum Disord. (2016) 27:73–87. doi: 10.1016/j.rasd.2016.04.001
5. Wetherby AM, Woods JJ. Early social interaction project for children with autism spectrum disorders beginning in the second year of life: a preliminary study. Topics Early Childhood Special Educ. (2006) 26:67–82. doi: 10.1177/02711214060260020201
6. *Srinivasan SM, Eigsti I, Neelly L, Bhat AN. The effects of embodied rhythm and robotic interventions on the spontaneous and responsive social attention patterns of children with autism spectrum disorder (ASD): A pilot randomized controlled trial. Res Autism Spectrum Disord. (2016) 27:54–72. doi: 10.1016/j.rasd.2016.01.004
7. Dawson G, Bernier R, Ring RH. Social attention: a possible early indicator of efficacy in autism clinical trials. J Neurodev Disord. (2012) 4:1–12. doi: 10.1186/1866-1955-4-11
8. Mundy P, Crowson M. Joint attention and early social communication: implications for research on intervention with autism. J Autism Dev Disord. (1997) 27:653–76. doi: 10.1023/A:1025802832021
9. American Psychiatric Association. DSM-5 Diagnostic Classification. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC (2013). p. 10.
10. Reese RM, Richman DM, Belmont JM, Morse P. Functional characteristics of disruptive behavior in developmentally disabled children with and without autism. J Autism Dev Disord. (2005) 35:419–28. doi: 10.1007/s10803-005-5032-0
11. Leekam SR, Prior MR, Uljarevic M. Restricted and repetitive behaviors in autism spectrum disorders: a review of research in the last decade. Psychol Bull. (2011) 137:562. doi: 10.1037/a0023341
12. Maskey M, Warnell F, Parr JR, Le Couteur A, McConachie H. Emotional and behavioural problems in children with autism spectrum disorder. J Autism Dev Disord. (2013) 43:851–9. doi: 10.1007/s10803-012-1622-9
13. Dominick KC, Davis NO, Lainhart J, Tager-Flusberg H, Folstein S. Atypical behaviors in children with autism and children with a history of language impairment. Res Dev Disabil. (2007) 28:145–62. doi: 10.1016/j.ridd.2006.02.003
14. Hartley S, Sikora D, McCoy R. Prevalence and risk factors of maladaptive behaviour in young children with autistic disorder. J Intellectual Disability Res. (2008) 52:819–29. doi: 10.1111/j.1365-2788.2008.01065.x
15. Diamond A. The early development of executive functions. In: Bialystok E, Craik FIM, editors. (2006) 1:70–95. doi: 10.1093/acprof:oso/9780195169539.003.0006
16. Van Eylen L, Boets B, Steyaert J, Wagemans J, Noens I. Executive functioning in autism spectrum disorders: influence of task and sample characteristics and relation to symptom severity. Eur Child Adolesc Psychiatry. (2015) 24:1399–417. doi: 10.1007/s00787-015-0689-1
17. Lai CLE, Lau Z, Lui SS, Lok E, Tam V, Chan Q, et al. Meta-analysis of neuropsychological measures of executive functioning in children and adolescents with high-functioning autism spectrum disorder. Autism Res. (2017) 10:911–39. doi: 10.1002/aur.1723
18. Van Etten HM, Kaur M, Srinivasan SM, Cohen SJ, Bhat A, Dobkins KR. Increased prevalence of unusual sensory behaviors in infants at risk for, and teens with, autism spectrum disorder. J Autism Dev Disord. (2017) 47:3431–45. doi: 10.1007/s10803-017-3227-9
19. Kaur M, Srinivasan SM, Bhat AN. Comparing motor performance, praxis, coordination, and interpersonal synchrony between children with and without Autism Spectrum Disorder (ASD). Res Dev Disabil. (2018) 72:79–95. doi: 10.1016/j.ridd.2017.10.025
20. Srinivasan SM, Bhat AN. Differences in object sharing between infants at risk for autism and typically developing infants from 9 to 15 months of age. Infant Behav Dev. (2016) 42:128–41. doi: 10.1016/j.infbeh.2015.12.003
21. Srinivasan SM, Bhat AN. Differences in means-end exploration between infants at risk for autism and typically developing infants in the first 15 months of life. Dev Psychobiol. (2019) 61:203–15. doi: 10.1002/dev.21810
22. Bhat AN. Is motor impairment in autism spectrum disorder distinct from developmental coordination disorder? A report from the SPARK study. Phys Ther. (2020) 100:633–44. doi: 10.1093/ptj/pzz190
23. Leekam SR, Nieto C, Libby SJ, Wing L, Gould J. Describing the sensory abnormalities of children and adults with autism. J Autism Dev Disord. (2007) 37:894–910. doi: 10.1007/s10803-006-0218-7
24. Donnellan AM, Hill DA, Leary MR. Rethinking autism: implications of sensory and movement differences for understanding and support. Front Integr Neurosci. (2013) 6:124. doi: 10.3389/fnint.2012.00124
25. Provost B, Crowe TK, Acree K, Osbourn PL, McClain C. Sensory behaviors of preschool children with and without autism spectrum disorders. N Zeal J Occupational Ther. (2009) 56:9. doi: 10.3316/informit.108115167044231
26. Shield A, Knapke K, Henry M, Srinivasan S, Bhat A. Impaired praxis in gesture imitation by deaf children with autism spectrum disorder. Autism Dev Lang Impairments. (2017) 2:2396941517745674. doi: 10.1177/2396941517745674
27. *Srinivasan SM, Kaur M, Park IK, Gifford TD, Marsh KL, Bhat AN. The effects of rhythm and robotic interventions on the imitation/praxis, interpersonal synchrony, and motor performance of children with autism spectrum disorder (ASD): a pilot randomized controlled trial. Autism Res Treatment. (2015) 1–18. doi: 10.1155/2015/736516
28. Marsh KL, Isenhower RW, Richardson MJ, Helt M, Verbalis AD, Schmidt RC, et al. Autism and social disconnection in interpersonal rocking. Front Integr Neurosci. (2013) 7:4. doi: 10.3389/fnint.2013.00004
29. Downey R, Rapport MJ. Motor activity in children with autism: a review of current literature. Pediatr Phys Ther. (2012) 24:2–20. doi: 10.1097/PEP.0b013e31823db95f
30. Green D, Baird G, Barnett AL, Henderson L, Huber J, Henderson SE. The severity and nature of motor impairment in Asperger's syndrome: a comparison with specific developmental disorder of motor function. J Child Psychol Psychiatry. (2002) 43:655–68. doi: 10.1111/1469-7610.00054
31. Provost B, Lopez BR, Heimerl S. A comparison of motor delays in young children: autism spectrum disorder, developmental delay, and developmental concerns. J Autism Dev Disord. (2007) 37:321–8. doi: 10.1007/s10803-006-0170-6
32. Manjiviona J, Prior M. Comparison of Asperger syndrome and high-functioning autistic children on a test of motor impairment. J Autism Dev Disord. (1995) 25:23–39. doi: 10.1007/BF02178165
33. Miyahara M, Tsujii M, Hori M, Nakanishi K, Kageyama H, Sugiyama T. Brief report: motor incoordination in children with Asperger syndrome and learning disabilities. J Autism Dev Disord. (1997) 27:595–603. doi: 10.1023/A:1025834211548
34. Hilton C, Wente L, LaVesser P, Ito M, Reed C, Herzberg G. Relationship between motor skill impairment and severity in children with Asperger syndrome. Res Autism Spectrum Disord. (2007) 1:339–49. doi: 10.1016/j.rasd.2006.12.003
35. Provost B, Heimerl S, Lopez BR. Levels of gross and fine motor development in young children with autism spectrum disorder. Phys Occup Ther Pediatr. (2007) 27:21–36. doi: 10.1080/J006v27n03_03
36. Green D, Charman T, Pickles A, Chandler S, Loucas T, Simonoff E, et al. Impairment in movement skills of children with autistic spectrum disorders. Dev Med Child Neurol. (2009) 51:311–6. doi: 10.1111/j.1469-8749.2008.03242.x
37. Ming X, Brimacombe M, Wagner GC. Prevalence of motor impairment in autism spectrum disorders. Brain Dev. (2007) 29:565–70. doi: 10.1016/j.braindev.2007.03.002
38. Dewey D, Cantell M, Crawford SG. Motor and gestural performance in children with autism spectrum disorders, developmental coordination disorder, and/or attention deficit hyperactivity disorder. J Int Neuropsychol Soc. (2007) 13:246–56. doi: 10.1017/S1355617707070270
39. MacDonald M, Lord C, Ulrich DA. The relationship of motor skills and social communicative skills in school-aged children with autism spectrum disorder. Adapted Phys Activity Q. (2013) 30:271–82. doi: 10.1123/apaq.30.3.271
40. Iverson JM. Early motor and communicative development in infants with an older sibling with autism spectrum disorder. J Speech Lang Hearing Res. (2018) 61:2673–84. doi: 10.1044/2018_JSLHR-L-RSAUT-18-0035
41. Licari MK, Alvares GA, Varcin K, Evans KL, Cleary D, Reid SL, et al. Prevalence of motor difficulties in autism spectrum disorder: analysis of a population-based cohort. Autism Res. (2020) 13:298–306. doi: 10.1002/aur.2230
42. Sipes M, Matson JL, Horovitz M. Autism spectrum disorders and motor skills: the effect on socialization as measured by the Baby and Infant Screen for Children with aUtIsm Traits (BISCUIT). Dev Neurorehabil. (2011) 14:290–6. doi: 10.3109/17518423.2011.587838
43. Pusponegoro HD, Efar P, Soebadi A, Firmansyah A, Chen H, Hung K. Gross motor profile and its association with socialization skills in children with autism spectrum disorders. Pediatrics Neonatol. (2016) 57:501–7. doi: 10.1016/j.pedneo.2016.02.004
44. Mody M, Shui A, Nowinski L, Golas S, Ferrone C, O'Rourke J, et al. Communication deficits and the motor system: exploring patterns of associations in autism spectrum disorder (ASD). J Autism Dev Disord. (2017) 47:155–62. doi: 10.1007/s10803-016-2934-y
45. Craig F, Crippa A, Ruggiero M, Rizzato V, Russo L, Fanizza I, et al. Characterization of Autism Spectrum Disorder (ASD) subtypes based on the relationship between motor skills and social communication abilities. Human Movement Sci. (2021) 77:102802. doi: 10.1016/j.humov.2021.102802
46. Bhat AN. Motor impairment increases in children with autism spectrum disorder as a function of social communication, cognitive and functional impairment, repetitive behavior severity, and comorbid diagnoses: a SPARK study report. Autism Res. (2021) 14:202–19. doi: 10.1002/aur.2453
47. Bhat AN, Srinivasan SM, Woxholdt C, Shield A. Differences in praxis performance and receptive language during fingerspelling between deaf children with and without autism spectrum disorder. Autism. (2018) 22:271–82. doi: 10.1177/1362361316672179
48. MacDonald M, Lord C, Ulrich D. The relationship of motor skills and adaptive behavior skills in young children with autism spectrum disorders. Res Autism Spectrum Disord. (2013) 7:1383–90. doi: 10.1016/j.rasd.2013.07.020
49. Travers BG, Bigler ED, Duffield TC, Prigge MD, Froehlich AL, Lange N, et al. Longitudinal development of manual motor ability in autism spectrum disorder from childhood to mid-adulthood relates to adaptive daily living skills. Dev Sci. (2017) 20:e12401. doi: 10.1111/desc.12401
50. Günal A, Bumin G, Huri M. The effects of motor and cognitive impairments on daily living activities and quality of life in children with autism. J Occupational Ther Schools Early Intervention. (2019) 12:444–54. doi: 10.1080/19411243.2019.1604286
51. Srinivasan S, Bhat A. Differences in caregiver behaviors of infants at-risk for autism and typically developing infants from 9 to 15 months of age. Infant Behav Dev. (2020) 59:101445. doi: 10.1016/j.infbeh.2020.101445
52. McCleery JP, Elliott NA, Sampanis DS, Stefanidou CA. Motor development and motor resonance difficulties in autism: relevance to early intervention for language and communication skills. Front Integr Neurosci. (2013) 7:30. doi: 10.3389/fnint.2013.00030
53. Bhat AN, Srinivasan S. A review of “music and movement” therapies for children with autism: embodied interventions for multisystem development. Front Integr Neurosci. (2013) 7:22. doi: 10.3389/fnint.2013.00022
54. Bhat AN, Landa RJ, Galloway JC. Current perspectives on motor functioning in infants, children, and adults with autism spectrum disorders. Phys Ther. (2011) 91:1116–29. doi: 10.2522/ptj.20100294
55. Lovaas OI. Behavioral treatment and normal educational and intellectual functioning in young autistic children. J Consult Clin Psychol. (1987) 55:3. doi: 10.1037/0022-006X.55.1.3
56. Mesibov GB, Shea V, Schopler E. The TEACCH Approach to Autism Spectrum Disorders. Springer Science & Business Media (2005).
57. Bondy AS, Frost LA. The picture exchange communication system. Focus Autistic Behav. (1994) 9:1–19. doi: 10.1177/108835769400900301
58. Wieder S, Greenspan SI. Engaging Autism: using the floortime approach to help children Relate, Communicate, and Think. Cambridge, MA: Da Capo Lifelong Books (2006).
59. Prizant BM, Wetherby AM, Rubin E, Laurent AC, Rydell PJ. The SCERTS Model: A Comprehensive Educational Approach for Children With Autism Spectrum Disorders, Vol. 1. Washington, DC: Paul H Brookes Publishing (2006).
60. Dawson G, Rogers S, Munson J, Smith M, Winter J, Greenson J, et al. Randomized, controlled trial of an intervention for toddlers with autism: the Early Start Denver Model. Pediatrics. (2010) 125:e17–23. doi: 10.1542/peds.2009-0958
61. Schreibman L, Koegel RL. Fostering self-management: parent-delivered pivotal response training for children with autistic disorder. In: Hibbs ED, Jensen PS, editors. Psychosocial Treatments for Child and Adolescent Disorders: Empirically Based Strategies for Clinical Practice. American Psychological Association (1996). p. 525–52. doi: 10.1037/10196-020
62. Steiner AM, Gengoux GW, Klin A, Chawarska K. Pivotal response treatment for infants at-risk for autism spectrum disorders: a pilot study. J Autism Dev Disord. (2013) 43:91–102. doi: 10.1007/s10803-012-1542-8
63. Hyman SL, Levy SE, Myers SM, Council on Children With Disabilities Section on Developmental and Behavioral Pediatrics. Identification, evaluation, and management of children with autism spectrum disorder. Pediatrics. (2020) 145:1–71. doi: 10.1542/peds.2019-3448
64. Wickstrom J, Dell'Armo K, Salzman E, Hooker JL, Delehanty A, Bishop S, et al. Systematic review: recommendations for rehabilitation in ASD and ID from clinical practice guidelines. medRxiv. (2021) 7:1–30. doi: 10.1101/2021.04.05.21254892
65. Maglione MA, Gans D, Das L, Timbie J, Kasari C, Technical Expert Panel, et al. Nonmedical interventions for children with ASD: recommended guidelines and further research needs. Pediatrics. (2012) 130(Suppl. 2):S169–78. doi: 10.1542/peds.2012-0900O
66. Trimble KA. A quantitative correlational study of race and access to services for preschool age children with autism spectrum disorder. ProQuest Dissertations Publishing (2021) 2531530198:1–81.
67. Schreibman L, Dawson G, Stahmer AC, Landa R, Rogers SJ, McGee GG, et al. Naturalistic developmental behavioral interventions: empirically validated treatments for autism spectrum disorder. J Autism Dev Disord. (2015) 45:2411–28. doi: 10.1007/s10803-015-2407-8
68. Smith T. What is evidence-based behavior analysis? Behav Analyst. (2013) 36:7–33. doi: 10.1007/BF03392290
69. Virues-Ortega J, Julio FM, Pastor-Barriuso R. The TEACCH program for children and adults with autism: a meta-analysis of intervention studies. Clin Psychol Rev. (2013) 33:940–53. doi: 10.1016/j.cpr.2013.07.005
70. Rogers SJ, Vismara LA. Evidence-based comprehensive treatments for early autism. J Clin Child Adolescent Psychol. (2008) 37:8–38. doi: 10.1080/15374410701817808
71. Wong C, Odom SL, Hume KA, Cox AW, Fettig A, Kucharczyk S, et al. Evidence-based practices for children, youth, and young adults with autism spectrum disorder: a comprehensive review. J Autism Dev Disord. (2015) 45:1951–66. doi: 10.1007/s10803-014-2351-z
72. Paul R, Sutherland D. Enhancing early language in children with autism spectrum disorders. In: Volkmar FR, Paul R, Klin A, Cohen D, editors. Handbook of Autism and Pervasive Developmental Disorders: Assessment, Interventions, and Policy. John Wiley & Sons, Inc (2005). p. 946–76. doi: 10.1002/9780470939352.ch11
73. Klein N, Kemper KJ. Integrative approaches to caring for children with autism. Curr Problems Pediatric Adolescent Health Care. (2016) 46:195–201. doi: 10.1016/j.cppeds.2015.12.004
74. Geretsegger M, Holck U, Bieleninik Ł, Gold C. Feasibility of a trial on improvisational music therapy for children with autism spectrum disorder. J Music Ther. (2016) 53:93–120. doi: 10.1093/jmt/thv038
75. Zou L, Xiao Z, Wang H, Wang C, Hu X, Shu Y. Martial arts for health benefits in children and youth with autism spectrum disorder: a systematic review. Archives of Budo. (2017) 13:79–92.
76. Miller A, Vernon T, Wu V, Russo K. Social skill group interventions for adolescents with autism spectrum disorders: a systematic review. Rev J Autism Dev Disord. (2014) 1:254–65. doi: 10.1007/s40489-014-0017-6
77. Koch S, Kunz T, Lykou S, Cruz R. Effects of dance movement therapy and dance on health-related psychological outcomes: a meta-analysis. Arts Psychother. (2014) 41:46–64. doi: 10.1016/j.aip.2013.10.004
78. Takahashi H, Matsushima K, Kato T. The effectiveness of dance/movement therapy interventions for autism spectrum disorder: a systematic review. Am J Dance Ther. (2019) 41:55–74. doi: 10.1007/s10465-019-09296-5
79. Martin M. Moving on the spectrum: dance/movement therapy as a potential early intervention tool for children with Autism Spectrum Disorders. Arts Psychother. (2014) 41:545–53. doi: 10.1016/j.aip.2014.10.003
80. LaGasse AB, Hardy MW. Rhythm, movement, and autism: using rhythmic rehabilitation research as a model for autism. Front Integr Neurosci. (2013) 7:19. doi: 10.3389/fnint.2013.00019
81. Srinivasan SM, Su W, Cleffi C, Bhat AN. From social distancing to social connections: insights from the delivery of a clinician-caregiver co-mediated telehealth-based intervention in young children with autism spectrum disorder. Front Psychiatry. (2021) 12:247. doi: 10.3389/fpsyt.2021.700247
82. Su W, Srinivasan S, Cleffi C, Bhat A. Short report on research trends during the COVID-19 pandemic and use of telehealth interventions and remote brain research in children with autism spectrum disorder. Autism. (2021) 25:1816–22. doi: 10.1177/13623613211004795
83. Bhat A, Su W, Cleffi C, Srinivasan S. A hybrid clinical trial delivery model in the COVID-19 era. Phys Ther. (2021) 101:pzab116. doi: 10.1093/ptj/pzab116
84. Kaur M, Gifford T, Marsh KL, Bhat A. Effect of robot–child interactions on bilateral coordination skills of typically developing children and a child with autism spectrum disorder: a preliminary study. J Motor Learn Dev. (2013) 1:31–7. doi: 10.1123/jmld.1.2.31
85. *Arzoglou D, Tsimaras V, Kotsikas G, Fotiadou E, Sidiropoulou M, Proios M, et al. The effect of [alpha] tradinional dance training program on neuromuscular coordination of individuals with autism. J Phys Educ Sport. (2013) 13:563. doi: 10.7752/jpes.2013.04088
86. *Bahrami F, Movahedi A, Marandi SM, Sorensen C. The effect of karate techniques training on communication deficit of children with autism spectrum disorders. J Autism Dev Disord. (2016) 46:978–86. doi: 10.1007/s10803-015-2643-y
87. *Corbett BA, Blain SD, Ioannou S, Balser M. Changes in anxiety following a randomized control trial of a theatre-based intervention for youth with autism spectrum disorder. Autism. (2017) 21:333–43. doi: 10.1177/1362361316643623
88. *Koenig KP, Buckley-Reen A, Garg S. Efficacy of the Get Ready to Learn yoga program among children with autism spectrum disorders: a pretest–posttest control group design. Am J Occupational Ther. (2012) 66:538–46. doi: 10.5014/ajot.2012.004390
89. Healy S, Nacario A, Braithwaite RE, Hopper C. The effect of physical activity interventions on youth with autism spectrum disorder: a meta-analysis. Autism Res. (2018) 11:818–33. doi: 10.1002/aur.1955
90. Srinivasan S, Bhat A. The effect of robot-child interactions on social attention and verbalization patterns of typically developing children and children with autism between 4 and 8 years. Autism. (2013) 3:1–8. doi: 10.4172/2165-7890.1000111
92. Marsh KL, Richardson M, Schmidt RC. Social connection through joint action and interpersonal coordination. Top Cogn Sci. (2009) 1:320–39. doi: 10.1111/j.1756-8765.2009.01022.x
93. Overy K, Molnar-Szakacs I. Being together in time: musical experience and the mirror neuron system. Music Perception. (2009) 26:489–504. doi: 10.1525/mp.2009.26.5.489
94. Minshew NJ, Williams DL. The new neurobiology of autism: cortex, connectivity, and neuronal organization. Arch Neurol. (2007) 64:945–50. doi: 10.1001/archneur.64.7.945
95. Courchesne E, Pierce K, Schumann CM, Redcay E, Buckwalter JA, Kennedy DP, et al. Mapping early brain development in autism. Neuron. (2007) 56:399–413. doi: 10.1016/j.neuron.2007.10.016
96. Belmonte MK, Allen G, Beckel-Mitchener A, Carper RA, Webb SJ. Autism and abnormal development of brain connectivity. J Neurosci. (2004) 24:9228–31. doi: 10.1523/JNEUROSCI.3340-04.2004
97. Lense MD, Camarata S. PRESS-play: musical engagement as a motivating platform for social interaction and social play in young children with ASD. Music Sci. (2020) 3:2059204320933080. doi: 10.1177/2059204320933080
98. *Dvir T, Lotan N, Viderman R, Elefant C. The body communicates: movement synchrony during music therapy with children diagnosed with ASD. Arts Psychother. (2020) 69:101658. doi: 10.1016/j.aip.2020.101658
99. Quintin E. Music-evoked reward and emotion: relative strengths and response to intervention of people with ASD. Front Neural Circuits. (2019) 13:49. doi: 10.3389/fncir.2019.00049
100. Sharda M, Tuerk C, Chowdhury R, Jamey K, Foster N, Custo-Blanch M, et al. Music improves social communication and auditory–motor connectivity in children with autism. Translational Psychiatry. (2018) 8:1–13. doi: 10.1038/s41398-018-0287-3
101. *Kim J, Wigram T, Gold C. Emotional, motivational and interpersonal responsiveness of children with autism in improvisational music therapy. Autism. (2009) 13:389–409. doi: 10.1177/1362361309105660
102. Wimpory DC, Nash S. Musical interaction therapy-therapeutic play for children with autism. Child Lang Teach Ther. (1999) 15:17–28. doi: 10.1177/026565909901500103
103. Katagiri J. The effect of background music and song texts on the emotional understanding of children with autism. J Music Ther. (2009) 46:15–31. doi: 10.1093/jmt/46.1.15
104. *Phung JN, Goldberg WA. Promoting executive functioning in children with autism spectrum disorder through mixed martial arts training. J Autism Dev Disord. (2019) 49:3669–84. doi: 10.1007/s10803-019-04072-3
105. Geretsegger M, Elefant C, Mössler KA, Gold C. Music therapy for people with autism spectrum disorder. Cochrane Database Systematic Rev. (2014) 6:1–22. doi: 10.1002/14651858.CD004381.pub3
106. Moseley AM, Herbert RD, Sherrington C, Maher CG. Evidence for physiotherapy practice: a survey of the Physiotherapy Evidence Database (PEDro). Austr J Physiother. (2002) 48:43–9. doi: 10.1016/S0004-9514(14)60281-6
107. National Institutes of Health. National Institutes of Health Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies [Internet]. Bethesda, National Heart, Lung and Blood Institute (2016).
108. Sackett DL, Straus SE, Richardson WS. Evidence-Based Medicine: How to Practice and Teach EBM. Edinburgh: Churchill Livingstone (2000).
109. Hedges LV. Distribution theory for Glass's estimator of effect size and related estimators. J Educ Stat. (1981) 6:107–28. doi: 10.3102/10769986006002107
111. Huedo-Medina T, Johnson B. Estimating the Standardized Mean Difference Effect Size and Its Variance From Different Data Sources: A Spreadsheet. Storrs, CT: Authors (2011).
113. Cohen J. The Effect Size. Statistical Power Analysis for the Behavioral Sciences 4th ed. New York, NY (1988). p. 77–83.
114. Page P. Beyond statistical significance: clinical interpretation of rehabilitation research literature. Int J Sports Phys Ther. (2014) 9:726–36.
115. Sullivan GM, Feinn R. Using effect size—or why the P value is not enough. J Graduate Med Educ. (2012) 4:279. doi: 10.4300/JGME-D-12-00156.1
116. *Bieleninik Ł, Geretsegger M, Mössler K, Assmus J, Thompson G, Gattino G, et al. Effects of improvisational music therapy vs enhanced standard care on symptom severity among children with autism spectrum disorder: the TIME-A randomized clinical trial. JAMA. (2017) 318:525–35. doi: 10.1001/jama.2017.9478
117. *Mossler K, Schmid W, Assmus J, Fusar-Poli L, Gold C. Attunement in music therapy for young children with autism: revisiting qualities of relationship as mechanisms of change. J Autism Dev Disord. (2020) 50:3921–34. doi: 10.1007/s10803-020-04448-w
118. *Srinivasan SM, Park IK, Neelly LB, Bhat AN. A comparison of the effects of rhythm and robotic interventions on repetitive behaviors and affective states of children with autism spectrum disorder (ASD). Res Autism Spectrum Disord. (2015) 18:51–63. doi: 10.1016/j.rasd.2015.07.004
119. *Kim J, Wigram T, Gold C. The effects of improvisational music therapy on joint attention behaviors in autistic children: a randomized controlled study. J Autism Dev Disord. (2008) 38:1758. doi: 10.1007/s10803-008-0566-6
120. *Radhakrishna S. Application of integrated yoga therapy to increase imitation skills in children with autism spectrum disorder. Int J Yoga. (2010) 3:26–30. doi: 10.4103/0973-6131.66775
121. *Radhakrishna S, Nagarathna R, Nagendra HR. Integrated approach to yoga therapy and autism spectrum disorders. J Ayurveda Integr Med. (2010) 1:120–4. doi: 10.4103/0975-9476.65089
122. *Bahrami F, Movahedi A, Marandi SM, Abedi A. Kata techniques training consistently decreases stereotypy in children with autism spectrum disorder. Res Dev Disabil. (2012) 33:1183–93. doi: 10.1016/j.ridd.2012.01.018
123. *Phung JN, Goldberg WA. Mixed martial arts training improves social skills and lessens problem behaviors in boys with Autism Spectrum Disorder. Res Autism Spectrum Disord. (2021) 83:101758. doi: 10.1016/j.rasd.2021.101758
124. *Corbett BA, Gunther JR, Comins D, Price J, Ryan N, Simon D, et al. Brief report: theatre as therapy for children with autism spectrum disorder. J Autism Dev Disord. (2011) 41:505–11. doi: 10.1007/s10803-010-1064-1
125. *Ioannou S, Key AP, Muscatello RA, Klemencic M, Corbett BA. Peer actors and theater techniques play pivotal roles in improving social play and anxiety for children with autism. Front Psychol. (2020) 11:908. doi: 10.3389/fpsyg.2020.00908
126. *Corbett BA, Swain DM, Coke C, Simon D, Newsom C, Houchins-Juarez N, et al. Improvement in social deficits in autism spectrum disorders using a theatre-based, peer-mediated intervention. Autism Research. (2014) 7:4–16. doi: 10.1002/aur.1341
127. *Garcia JM, Leahy N, Rivera P, Renziehausen J, Samuels J, Fukuda DH, et al. Brief report: preliminary efficacy of a judo program to promote participation in physical activity in youth with autism spectrum disorder. J Autism Dev Disord. (2019) 50:1–7. doi: 10.1007/s10803-019-04338-w
128. *Rivera P, Renziehausen J, Garcia JM. Effects of an 8-week Judo program on behaviors in children with autism spectrum disorder: a mixed-methods approach. Child Psychiatry Human Dev. (2020) 51:734–41. doi: 10.1007/s10578-020-00994-7
129. *Edgerton CL. The effect of improvisational music therapy on the communicative behaviors of autistic children. J Music Ther. (1994) 31:31–62. doi: 10.1093/jmt/31.1.31
130. *Hartshorn K, Olds L, Field T, Delage J, Cullen C, Escalona A. Creative movement therapy benefits children with autism. Early Child Dev Care. (2001) 166:1–5. doi: 10.1080/0300443011660101
131. *Boso M, Emanuele E, Minazzi V, Abbamonte M, Politi P. Effect of long-term interactive music therapy on behavior profile and musical skills in young adults with severe autism. J Alternative Complementary Med. (2007) 13:709–12. doi: 10.1089/acm.2006.6334
132. *Gattino GS, Riesgo RdS, Longo D, Leite JCL, Faccini LS. Effects of relational music therapy on communication of children with autism: a randomized controlled study. Nordic J Music Ther. (2011) 20:142–54. doi: 10.1080/08098131.2011.566933
133. *Hillier A, Greher G, Poto N, Dougherty M. Positive outcomes following participation in a music intervention for adolescents and young adults on the autism spectrum. Psychol Music. (2012) 40:201–15. doi: 10.1177/0305735610386837
134. *Wan CY, Bazen L, Baars R, Libenson A, Zipse L, Zuk J, et al. Auditory-motor mapping training as an intervention to facilitate speech output in non-verbal children with autism: a proof of concept study. PLoS ONE. (2011) 6:e25505. doi: 10.1371/journal.pone.0025505
135. *Thompson G, McFerran K, Gold C. Family-centred music therapy to promote social engagement in young children with severe autism spectrum disorder: a randomized controlled study. Child Care Health Dev. (2014) 40:840–52. doi: 10.1111/cch.12121
136. *LaGasse AB. Effects of a music therapy group intervention on enhancing social skills in children with autism. J Music Ther. (2014) 51:250–75. doi: 10.1093/jmt/thu012
137. *Ghasemtabar SN, Hosseini M, Fayyaz I, Arab S, Naghashian H, Poudineh Z. Music therapy: an effective approach in improving social skills of children with autism. Adv Biomed Res. (2015) 4:1–8. doi: 10.4103/2277-9175.161584
138. *Yoo GE, Kim SJ. Dyadic drum playing and social skills: implications for rhythm-mediated intervention for children with autism spectrum disorder. J Music Ther. (2018) 55:340–75. doi: 10.1093/jmt/thy013
139. *Willemin T, Litchke LG, Liu T, Ekins C. Social emotional effects of Drumtastic®: a dyadic within-group drumming pilot program for children with autism spectrum disorder. Int J Special Educ. (2018) 33:94–103.
140. *Lowry RG, Hale BJ, Draper SB, Smith MS. Rock drumming enhances motor and psychosocial skills of children with emotional and behavioral difficulties. Int J Dev Disabilities. (2019) 65:152–61. doi: 10.1080/20473869.2018.1429041
141. *Stephen S. Impact of music therapy program in improving social skills of children with autism. Turkish J Physiother Rehabil. (2020) 32:2.
142. *Schmid L, DeMoss L, Scarbrough P, Ripple C, White Y, Dawson G. An investigation of a classroom-based specialized music therapy model for children with autism spectrum disorder: voices together using the VOICSS™ method. Focus Autism Other Dev Disabil. (2020) 35:176–85. doi: 10.1177/1088357620902505
143. *Rabeyron T, Del Canto JR, Carasco E, Bisson V, Bodeau N, Vrait F, et al. A randomized controlled trial of 25 sessions comparing music therapy and music listening for children with autism spectrum disorder. Psychiatry Res. (2020) 293:113377. doi: 10.1016/j.psychres.2020.113377
144. *Cibrian FL, Madrigal M, Avelais M, Tentori M. Supporting coordination of children with ASD using neurological music therapy: a pilot randomized control trial comparing an elastic touch-display with tambourines. Res Dev Disabil. (2020) 106:103741. doi: 10.1016/j.ridd.2020.103741
145. *Rosenblatt LE, Gorantla S, Torres JA, Yarmush RS, Rao S, Park ER, et al. Relaxation response–based yoga improves functioning in young children with autism: a pilot study. J Alternative Complementary Med. (2011) 17:1029–35. doi: 10.1089/acm.2010.0834
146. *de Bruin EI, Blom R, Smit FM, van Steensel FJ, Bögels SM. MYmind: mindfulness training for youngsters with autism spectrum disorders and their parents. Autism. (2015) 19:906–14. doi: 10.1177/1362361314553279
147. *Narasingharao K, Pradhan B, Navaneetham J. Efficacy of structured yoga intervention for sleep, gastrointestinal and behaviour problems of ASD children: an exploratory study. J Clin Diagn Res. (2017) 11:VC01–6. doi: 10.7860/JCDR/2017/25894.9502
148. *Sotoodeh MS, Arabameri E, Panahibakhsh M, Kheiroddin F, Mirdoozandeh H, Ghanizadeh A. Effectiveness of yoga training program on the severity of autism. Complementary Ther Clin Prac. (2017) 28:47–53. doi: 10.1016/j.ctcp.2017.05.001
149. *Litchke LG, Liu T, Castro S. Effects of multimodal mandala yoga on social and emotional skills for youth with autism spectrum disorder: an exploratory study. Int J Yoga. (2018) 11:59–65. doi: 10.4103/ijoy.IJOY_80_16
150. *Kaur M, Bhat A. Creative yoga intervention improves motor and imitation skills of children with autism spectrum disorder. Phys Ther. (2019) 99:1520–34. doi: 10.1093/ptj/pzz115
151. *Vidyashree HM, Maheshkumar K, Sundareswaran L, Sakthivel G, Partheeban PK, Rajan R. Effect of yoga intervention on short-term heart rate variability in children with autism spectrum disorder. Int J Yoga. (2019) 12:73–7. doi: 10.4103/ijoy.IJOY_66_17
152. *Tanksale R, Sofronoff K, Sheffield J, Gilmour J. Evaluating the effects of a yoga-based program integrated with third-wave cognitive behavioral therapy components on self-regulation in children on the autism spectrum: a pilot randomized controlled trial. Autism. (2021) 25:995–1008. doi: 10.1177/1362361320974841
153. *Movahedi A, Bahrami F, Marandi SM, Abedi A. Improvement in social dysfunction of children with autism spectrum disorder following long term Kata techniques training. Res Autism Spectrum Disord. (2013) 7:1054–61. doi: 10.1016/j.rasd.2013.04.012
154. *Chan AS, Sze SL, Siu NY, Lau EM, Cheung M. A Chinese mind-body exercise improves self-control of children with autism: a randomized controlled trial. PLoS ONE. (2013) 8:e68184. doi: 10.1371/journal.pone.0068184
155. *Chan AS, Han YM, Sze SL, Lau EM. Neuroenhancement of memory for children with autism by a mind–body exercise. Front Psychol. (2015) 6:1893. doi: 10.3389/fpsyg.2015.01893
156. *Figueiredo A, Avelar-Rosa B, Quaresma AM, Pinho J. Karate in children with neurodevelopmental disorders: an exploratory study. Rev Artes Marciales Asiáticas. (2016) 11:138–9. doi: 10.18002/rama.v11i2s.4209
157. *Kim Y, Todd T, Fujii T, Lim JC, Vrongistinos K, Jung T. Effects of Taekwondo intervention on balance in children with autism spectrum disorder. J Exerc Rehabil. (2016) 12:314–9. doi: 10.12965/jer.1632634.317
158. *Sarabzadeh M, Azari BB, Helalizadeh M. The effect of six weeks of Tai Chi Chuan training on the motor skills of children with Autism Spectrum Disorder. J Bodywork Movement Ther. (2019) 23:284–90. doi: 10.1016/j.jbmt.2019.01.007
159. *Ansari S, Hosseinkhanzadeh AA, AdibSaber F, Shojaei M, Daneshfar A. The effects of aquatic versus Kata techniques training on static and dynamic balance in children with autism spectrum disorder. J Autism Dev Disord. (2020) 51:1–7. doi: 10.1007/s10803-020-04785-w
160. *AdibSaber F, Shojaei M, Daneshfar A, Hossein Khanzadeh A. The effect of kata techniques training on sleep habits in boys with autism spectrum disorder. J Child Ment Health. (2021) 7:111–27. doi: 10.52547/jcmh.7.4.8
161. *Greco G, de Ronzi R. Effect of Karate training on social, emotional, and executive functioning in children with autism spectrum disorder. J Phys Educ Sport. (2020) 20:1637–45. doi: 10.7752/jpes.2020.04223
162. *Tabeshian R, Nezakat-Alhosseini M, Movahedi A, Zehr EP, Faramarzi S. The effect of Tai Chi Chuan training on stereotypic behavior of children with autism spectrum disorder. J Autism Dev Disord [Internet]. (2021) 1–7. doi: 10.1007/s10803-021-05090-w
163. *Lerner MD, Mikami AY, Levine K. Socio-dramatic affective-relational intervention for adolescents with Asperger syndrome & high functioning autism: Pilot study. Autism. (2011) 15:21–42. doi: 10.1177/1362361309353613
164. *Lerner MD, Mikami AY. A preliminary randomized controlled trial of two social skills interventions for youth with high-functioning autism spectrum disorders. Focus Autism Other Dev Disabil. (2012) 27:147–57. doi: 10.1177/1088357612450613
165. *Corbett BA, Key AP, Qualls L, Fecteau S, Newsom C, Coke C, et al. Improvement in social competence using a randomized trial of a theatre intervention for children with autism spectrum disorder. J Autism Dev Disord. (2016) 46:658–72. doi: 10.1007/s10803-015-2600-9
166. *Guli LA, Semrud-Clikeman M, Lerner MD, Britton N. Social Competence Intervention Program (SCIP): a pilot study of a creative drama program for youth with social difficulties. Arts Psychother. (2013) 40:37–44. doi: 10.1016/j.aip.2012.09.002
167. *Kim A, Stembridge S, Lawrence C, Torres V, Miodrag N, Lee J, et al. Neurodiversity on the stage: the effects of inclusive theatre on youth with autism. Int J Educ Soc Sci. (2015) 2:27–39.
168. *Reading S, Reading J, Padgett RJ, Reading S, Pryor P. The use of theatre to develop social and communication behaviors for students with autism. J Speech Pathol Ther. (2015) 1:1–8. doi: 10.4172/2472-5005.1000102
169. *Naniwadekar K, Ravi A, Sreevidya M. Impact of drama as a therapy for teaching social-communication skills on children with ASD. Int J Educ Psychol Res. (2016) 5:48–51.
170. *Beadle-Brown J, Wilkinson D, Richardson L, Shaughnessy N, Trimingham M, Leigh J, et al. Imagining Autism: feasibility of a drama-based intervention on the social, communicative and imaginative behaviour of children with autism. Autism. (2018) 22:915–27. doi: 10.1177/1362361317710797
171. *Koehne S, Behrends A, Fairhurst MT, Dziobek I. Fostering Social Cognition through an Imitation- and Synchronization-Based Dance/Movement Intervention in Adults with Autism Spectrum Disorder: A Controlled Proof-of-Concept Study. Psychother Psychosom. (2016) 85:27–35. doi: 10.1159/000441111
172. *Hildebrandt MK, Koch SC, Fuchs T. “We dance and find each other” 1: Effects of dance/movement therapy on negative symptoms in autism spectrum disorder. Behav Sci. (2016) 6:24. doi: 10.3390/bs6040024
173. *Mastrominico A, Fuchs T, Manders E, Steffinger L, Hirjak D, Sieber M, et al. Effects of dance movement therapy on adult patients with autism spectrum disorder: a randomized controlled trial. Behav Sci. (2018) 8:61. doi: 10.3390/bs8070061
174. *Souza-Santos C, dos Santos JF, Azevedo-Santos I, Teixeira-Machado L. Dance and equine-assisted therapy in autism spectrum disorder: crossover randomized clinical trial. Clin Neuropsychiatry J Treat Evaluation. (2018) 15:284–90.
175. *Aithal S, Karkou VV, Makris S, Karaminis T, Powell J. A dance movement psychotherapy intervention for the wellbeing of children with autism spectrum disorders: a pilot intervention study. Front Psychol. (2021) 12:2672. doi: 10.3389/fpsyg.2021.588418
176. *Mateos-Moreno D, Atencia-Doña L. Effect of a combined dance/movement and music therapy on young adults diagnosed with severe autism. Arts Psychother. (2013) 40:465–72. doi: 10.1016/j.aip.2013.09.004
177. *Koch SC, Mehl L, Sobanski E, Sieber M, Fuchs T. Fixing the mirrors: a feasibility study of the effects of dance movement therapy on young adults with autism spectrum disorder. Autism. (2015) 19:338–50. doi: 10.1177/1362361314522353
178. Heaton P, Williams K, Cummins O, Happé FG. Beyond perception: musical representation and on-line processing in autism. J Autism Dev Disord. (2007) 37:1355–60. doi: 10.1007/s10803-006-0283-y
179. Wan CY, Schlaug G. Music making as a tool for promoting brain plasticity across the life span. Neuroscientist. (2010) 16:566–77. doi: 10.1177/1073858410377805
180. Goldberg L. Yoga Therapy for Children With Autism and Special Needs. WW Norton & Company (2013).
181. Galantino ML, Galbavy R, Quinn L. Therapeutic effects of yoga for children: a systematic review of the literature. Pediatr Phys Ther. (2008) 20:66–80. doi: 10.1097/PEP.0b013e31815f1208
182. D'souza C, Avadhany S. Effects of yoga training and detraining on physical performance measures in prepubertal children–a randomized trial. Indian J Physiol Pharmacol. (2014) 58:61–8.
184. Nayak NN, Shankar K. Yoga: a therapeutic approach. Phys Med Rehabil Clin N Am. (2004) 15:783–98, vi. doi: 10.1016/j.pmr.2004.04.004
*^Note: All citations with an “*” indicate that these studies were included in our systematic review.
Keywords: creative movement, music, dance and movement, yoga, theater, martial arts, autism spectrum disorder (ASD), interventions
Citation: Amonkar N, Su W-C, Bhat AN and Srinivasan SM (2021) Effects of Creative Movement Therapies on Social Communication, Behavioral-Affective, Sensorimotor, Cognitive, and Functional Participation Skills of Individuals With Autism Spectrum Disorder: A Systematic Review. Front. Psychiatry 12:722874. doi: 10.3389/fpsyt.2021.722874
Received: 09 June 2021; Accepted: 30 September 2021;
Published: 18 November 2021.
Edited by:
Cheryl Dissanayake, La Trobe University, AustraliaReviewed by:
Kathryn K. Chadman, Institute for Basic Research in Developmental Disabilities (IBR), United StatesCopyright © 2021 Amonkar, Su, Bhat and Srinivasan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sudha M. Srinivasan, c3VkaGEuc3Jpbml2YXNhbkB1Y29ubi5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.