
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 03 January 2022
Sec. Psychopathology
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.719931
This article is part of the Research TopicComprehensive Understanding of PTSD: From Pathogenesis to InterventionView all 9 articles
 Min Peng1†
Min Peng1† Xinran Song1†
Xinran Song1† Luyu Liu1
Luyu Liu1 Weifeng Zhao1
Weifeng Zhao1 Pingmei Lai1
Pingmei Lai1 Guanglin Bao1
Guanglin Bao1 Tianyou Guo2*
Tianyou Guo2* Xiangyang Zhang3,4*
Xiangyang Zhang3,4*Background: COVID-19 pandemic is a traumatic event all over the world, and may lead to post-traumatic stress symptom (PTSS) in different population who are under the threat of novel corona virus. Therefore, the aim of our study was to compare the prevalence and risk factors of PTSS between Chinese patients with depression and non-depressed controls during the COVID-19 outbreak.
Methods: 437 depressed patients and 2,940 non-depressed controls were enrolled in this cross-sectional study between February 14 and May 9, 2020.The Impact of Events Scale-Revised (IES-R), Zung Self-Rating Depression Scale (SDS), Zung Self-Rating Anxiety Scale (SAS) and Pittsburgh Sleep Quality Index (PSQI) were used to evaluate the psychological status of all the participants.
Results: The prevalence of PTSS (IES-R ≥ 33) in depressed patients (45.08%) was higher than that in non-depressed controls (5.31%). Patients with depression were 16 times more likely to suffer from PTSS than those without depression. Correlation analyses showed that the IES-R total score was positively correlated with SDS, SAS, and PSQI scores in both depressed and non-depressed groups (Bonferroni corrected all p < 0.001). Multiple linear regression analysis showed that SAS score, and PSQI score were independently associated with IES-R total score in both depression and non-depression groups. In depressed patients, education level and duration of media exposure to COVID-19 were positively associated with PTSS, while in the non-depressed group, subjects who were married, in the 31–50 year group or with higher SDS score were more likely to develop PTSS.
Conclusions: These results indicate that the prevalence rate of PTSS in patients with depression is very higher than that in subjects without depression. PTSS are associated with a number of socio-demographic and clinical variables.
The COVID-19 pandemic is a global traumatic events (1), which has caused more than 248 million cases, and resulted in more than 5 million deaths worldwide. Nevertheless, the COVID-19 pandemic has also led to a “mental health tsunami”, including depression (2–5), anxiety (6–12), PTSS (13–17), and poor sleep quality (18–23). PTSD (or PTSS) is one of the most common mental distress among this tsunami. Numerous studies have shown that the prevalence of PTSS was high in different populations during the COVID-19 pandemic. For example, meta-analyses have estimated a combined prevalence of 6.5–42.8% for COVID-19 survivors (24), 18% (95% CI: 13–24%) for health care workers, and 12% (95% CI: 8–16%) for the general population (25). Moreover, PTSS has profound interactions with other psychiatric distress, such as depression, anxiety, and sleep quality (26, 27). For example, sleep quality is found to be a predictor variable of PTSS (28), which moderates the relationship between PTSS and anxiety (29).
The relationship between traumatic events, MDD and PTSD is complex (30). Traumatic events are a common risk factor for MDD and PTSD. MDD patients are at greater risk of PTSD than those without depression when they experience a traumatic event (31, 32). MDD patients with co-morbid PTSD tend to have a poorer prognosis (32). PTSD is a common but easily overlooked comorbidity among MDD patients in the face of global traumatic events of COVID-19. Many recent studies have focused on PTSS or PTSD during COVID-19, but these previous studies have mainly focused on COVID-19 survivors (9–11), hospital staff (3, 12–27), teachers (28), and the general population (29–33). However, few researchers have focused on PTSS co-morbidity in MDD patients during the COVID-19 pandemic (34).
Thus, although previous studies have found a high co-morbidity rate between MDD and PTSD (32), the co-morbidity rate of PTSS in MDD patients during COVID-19 and the clinical characteristics of this population are far from being fully explored. Therefore, the objectives of this study were: (1) to explore the co-morbidity rate, clinical predictors, and correlates of PTSS in MDD patients in Shenzhen, China; and (2) to identify sociodemographic or clinical factors associated with PTSS in MDD patients. In this study, we sought to identify independent risk factors for PTSS, further investigate the relationship between MDD and PTSS, develop appropriate management policies and implement practical interventions to improve PTSS in patients with depression during COVID-19.
Four hundred and thirty seven depressed patients and 2,940 non-depressed controls were enrolled in this cross-sectional study between February 14 and May 9, 2020.Our epidemiological research teams conducted the data collection. Each team included one doctor, one nurse and one data collector. Prior to the start of the study, dedicated data collectors were trained on the data collection to ensure proper data collection.
In the non-depressed control group, we used a subgroup sampling method. During the initial phase of the pandemic, prevention and control of the COVID-19 outbreak was complicated by the Chinese New Year travel rush. Individuals potentially exposed to COVID-19 virus were quarantined in Nanshan District, Shenzhen for 14 days. The Nanshan District government used epidemiological surveys to trace the chain and network of transmission of COVID-19. The epidemiological investigation was conducted by our 30 epidemiological investigation teams. Our epidemiological survey team invited all individuals who were isolated but not definitively diagnosed with COVID-19 infection to participate in this cross-sectional study in a face-to-face epidemiological survey. In the non-depressed group, we invited 3,775 subjects to participate in the survey. Four hundred and thirty seven children under the age of 18 were excluded because the sample mainly focused on those over 18 years of age. Twenty one individuals over 70 years of age were excluded because of underlying cognitive impairment. In addition, 132 subjects were excluded because they refused to participate or submitted contradictory or careless answers on the SAS or SDS. This left 3,135 subjects afterwards. Of these, 195 had SDS scores ≥50 and were excluded due to an undetermined MDD diagnosis. Finally, a total of 2,940 subjects without depressive symptoms were recruited as non-depressed controls.
In the depressed group, we recruited 437 patients with depression in the outpatient psychiatric clinics of Shenzhen Nanshan People's Hospital. Patients with depression were recruited in two ways. In the first way, psychiatrists randomly recruited 319 depressed patients during routine face-to-face consultations with our first-time patients and follow-up review patients at the psychiatric outpatient clinic of Huazhong University of Science and Technology Union Shenzhen Hospital. In the second way, the psychiatrists invited 118 depressed patients on follow-up visits to participate through the 160 web-based follow-up platform.
The inclusion criteria of patients with depression were as follows: (1) age between 18 and 70 years old; (2) SDS total score ≥ 50; (3) meeting the diagnostic criteria for Major Depressive Disorder (MDD), evaluated by psychiatrists based on ICD-10 criteria; (4) no history of serious physical diseases, such as vital organ failure, severe brain injury and severe cognitive impairment; (5) agreed to participate in this study. The inclusion criteria of non-depressed controls were as follows:(1) age between 18 and 70 years old, (2) SDS score< 50; (3) no history of serious physical diseases;(4) agreed to participate in this study.
This study was approved by the Ethics Review Committee of Huazhong University of Science and Technology Union Shenzhen Hospital. All subjects signed an informed consent form to participate in this study.
All data were collected using detailed standardized self-report questionnaires containing information on sociodemographics (e.g., age, sex, marital status, education level, occupation, history of alcohol and tobacco use, medical history, duration of media exposure to COVID-19) and mental health status. Standardized questionnaires were included in the hospital's psychological assessment system, the 160 web-based follow-up platform, and WeChat. The psychological evaluation system of the hospital was a computer-based psychological assessment system consisting of a number of psychological test scales that allowed an objective assessment of different psychological parameters. Three hundred and nineteen depressed patients were invited face-to-face by psychiatrists and filled out detailed questionnaires through our psychological assessment system. One hundred and eighteen depressed patients were invited and filled out detailed questionnaires through the 160 web-based follow-up platform. In the epidemiological survey, all our non-depressed controls were invited face-to-face. Two thousand nine hundred and forty non-depressed controls completed the questionnaire via WeChat (a social media application widely used in China) to reduce the likelihood of exposure to contaminated items. The survey was conducted at the psychiatric outpatient clinic of Huazhong University of Science and Technology Union Shenzhen Hospital, at the participants' homes or hotels.
The Chinese version of the 20-item Zung Self-Rating Depression Scale (SDS) was adopted to access depressive symptoms. The questionnaire consists of 20 items, and each item is scored according to the Likert scale of 4 points, ranging from 1 to 4 points. According to the standard score, a cut-off value of ≥ 50 was used to identify depressive symptoms (33). This SDS cut-off score (cut-off point raw score ≥ 40, index score ≥ 50) was clinically validated with good diagnostic accuracy (sensitivity, 75%; specificity, 75.1%) (34).
Post-traumatic stress symptoms were evaluated using the Impact of Events Scale-Revised (Chinese version) (CIES-R). The questionnaire consists of 22 items, each of which is scored according to the Likert scale of 5 points, ranging from 0 to 4 points, with a total score of 0–88 (35). The IES-R contains three subscales: hyperarousal, intrusion and avoidance. The internal consistency of the CIES-R was α = 0.83–0.89 (36).
The IES-R was also categorized as normal (0–23), low levels of PTSS [(24–32); PTSD clinical concern], moderate levels [(33–36); possible diagnosis of PTSD], and extreme levels (>37) (37). A cutoff score of 33 yielded the best values in terms of diagnostic accuracy of PTSD (sensitivity, 91%; specificity, 82%) (38). In this study, the cut-off score for PTSS was based on a total score of 33 on the IES-R (39, 40).
The Chinese version of the Zung Self-Rating Anxiety Scale (SAS) was applied to evaluate anxiety related symptoms. This is a scale composed of 20 items, each of which is scored according to the Likert scale of 4 points, ranging from 1 to 4 (41).
Sleep disturbance was evaluated with the Pittsburgh sleep quality (PSQI). This scale consists of 7 sub-scales and 19 items, and each item is scored on the Likert scale of 4 points, ranging from 0 to 3 points. The 7 sub-scale scores were added up to provide a total PSQI score (42, 43).
The media exposure to COVID-19 information was evaluated by asking participates how long (≤2 h/day, 2–3 h/day, 3–4 h/day, ≥4 h/day) they spent reading or searching information (hour per day) about COVID-19 within 1 week. According to a previous study, subjects exposed to COVID-19 media for ≥4 h per day had significantly higher levels of anxiety than those who used it for ≤2 h (44). Another study showed that students exposed to COVID-19 media for ≥3 h per day had 2.13 times more acute stress symptoms than students exposed to media for <1 h per day (45). Therefore, we chose ≤2 h, 2–3 h, 3–4 h, and ≥4 h as cutoffs.
Comparisons of clinical and demographic data were conducted using χ2 analysis for categorical data and ANOVA, MANOVA for continuous data. In order to compare the prevalence of PTSS in patients with depression and non-depressed controls, χ2 test and logistic regression were used. In addition, in depression group and non-depressed control group separately, MANOVA and MANCOVA were performed to compare the differences in clinical parameters between subgroups with and without PTSS. Z-test was used for subgroup comparison. Further, Pearson correlation coefficient was calculated to evaluate the correlation between variables. Bonferroni corrections were used to adjust the p-value for multiple comparisons and correlations (α = 0.05/14 = 0.004). At last, we applied multiple regression analyses to investigate the risk factors associated with IES-R total score, including sex, age, education levels, marital status, drinking history, smoking history, SDS score, SAS score, and PSQI score. SPSS software (version 26.0) was used for statistical analysis, setting a 2-tailed p = 0.05 as the significant level.
Table 1 compares the socio-demographic and main clinical data between depressed subjects and non-depressed controls (see Table 1 for Chi-square test and MANOVA results). Compared with the non-depressed controls, the depressed patients had younger age, more women, more drinkers, and more were in non-marital status, along with higher SDS score, SAS score, PSQI score, IES-R total score and three subscale scores (all P < 0.001). After we controlled for sex, age, education and marital status, MANCOVA results showed that the differences remain significant for SDS score (F1, 3371 = 6,614.23, p < 0.001), SAS score (F1,3371 = 3,357.76, p < 0.001) and PSQI score (F1,3371 = 1,900.06, p < 0.001), IES-R total score (F1,3371 = 814.44, p < 0.001), IES-R Avoidance subscale score (F1,3371 = 305.62, p < 0.001), IES-R Intrusion subscale score(F1,3371 = 640.08, p < 0.001), IES-R Hyperarousal subscale score (F1,3371 = 1424.18, p < 0.001), between the two groups.
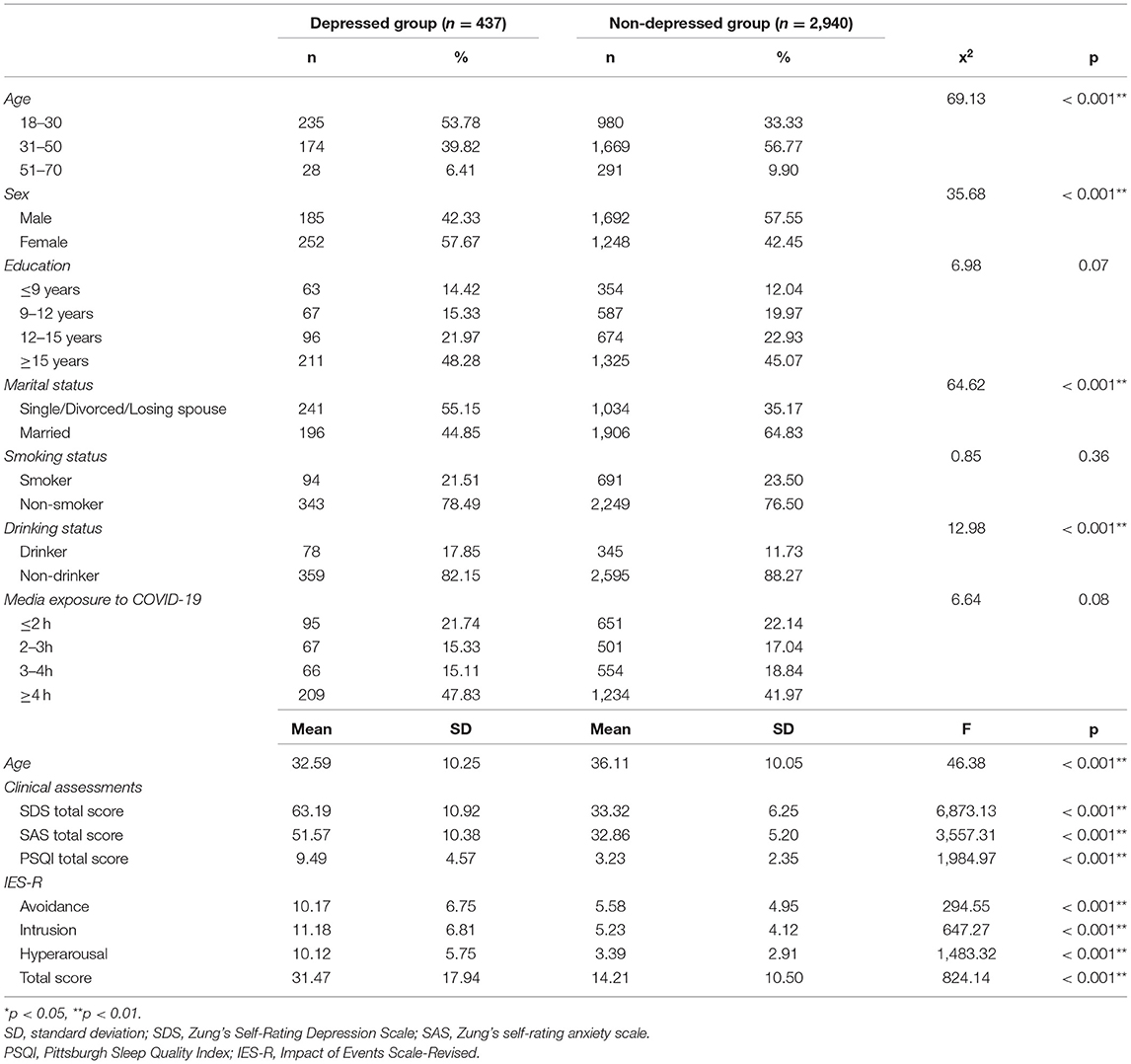
Table 1. Social demography and clinical characteristics of subjects with depression and non-depressed (x2and MANOVA).
The prevalence of PTSS (IES-R ≥ 33, possible diagnosis of PTSD) was significantly higher in the depressed group (45.08%, 95%CI: 40.4–49.8%, 197/437) than in the non-depressed control group (5.31%, 95%CI: 4.5–6.1%, 156/2,940) (x2 = 642.99, P < 0.001).
Moreover, logistic regression analysis showed that the depressed group was 16 times more likely to have PTSS than the non-depressed group (IES-R ≥ 33) (x2 = 457.79, P < 0.001; odds ratio = 16.00; 95%CI: 12.25–20.89).
In addition, the IES-R total score in the depression group (31.47 ± 17.94) was significantly higher than that in the non-depressed control group (14.21 ± 10.50) (x2 = 824.14, p < 0.001). We further analyzed data of the depressed and non-depressed groups respectively, using occupation as a subgroup variable. The results showed no significant differences on IRS-R total scores and three subscores between different occupational groups (including peasants, workers, teachers, health care workers, staffs, self-employed, military personnels, freelancers, domestic workers, other workers and unemployed).
Among patients with depression, compared with the non-PTSS subgroup, the PTSS subgroup had higher education, more time exposure to COVID-19 media coverage and higher SDS score, IES-R total and all three subscores, SAS score, PSQI score (all P < 0.05) (see Chi-square test and MANOVA results in Table 2). After adjusting for covariates including age, gender, education, and marital status, there were no significant differences in SDS scores (F1,431 = 40.18, P < 0. 001, Bonferroni corrected), SAS scores (F1,431 = 91.82, P < 0.001, Bonferroni corrected), PSQI scores (F1,431 = 56.36, P < 0.001, Bonferroni-corrected), IES-R total score (F1,431 = 838.65, P < 0.001, Bonferroni-corrected), IES-R avoidance subscale score (F1,431 = 627.08, P < 0.001, Bonferroni-corrected), IES-R interference subscale score (F1,431 = 529.99, P < 0.001, Bonferroni corrected), and IES-R overanxiety subscale scores (F1,431 = 551.80, P < 0.001, Bonferroni corrected), between the two subgroups (α = 0.05/14 = 0.004).
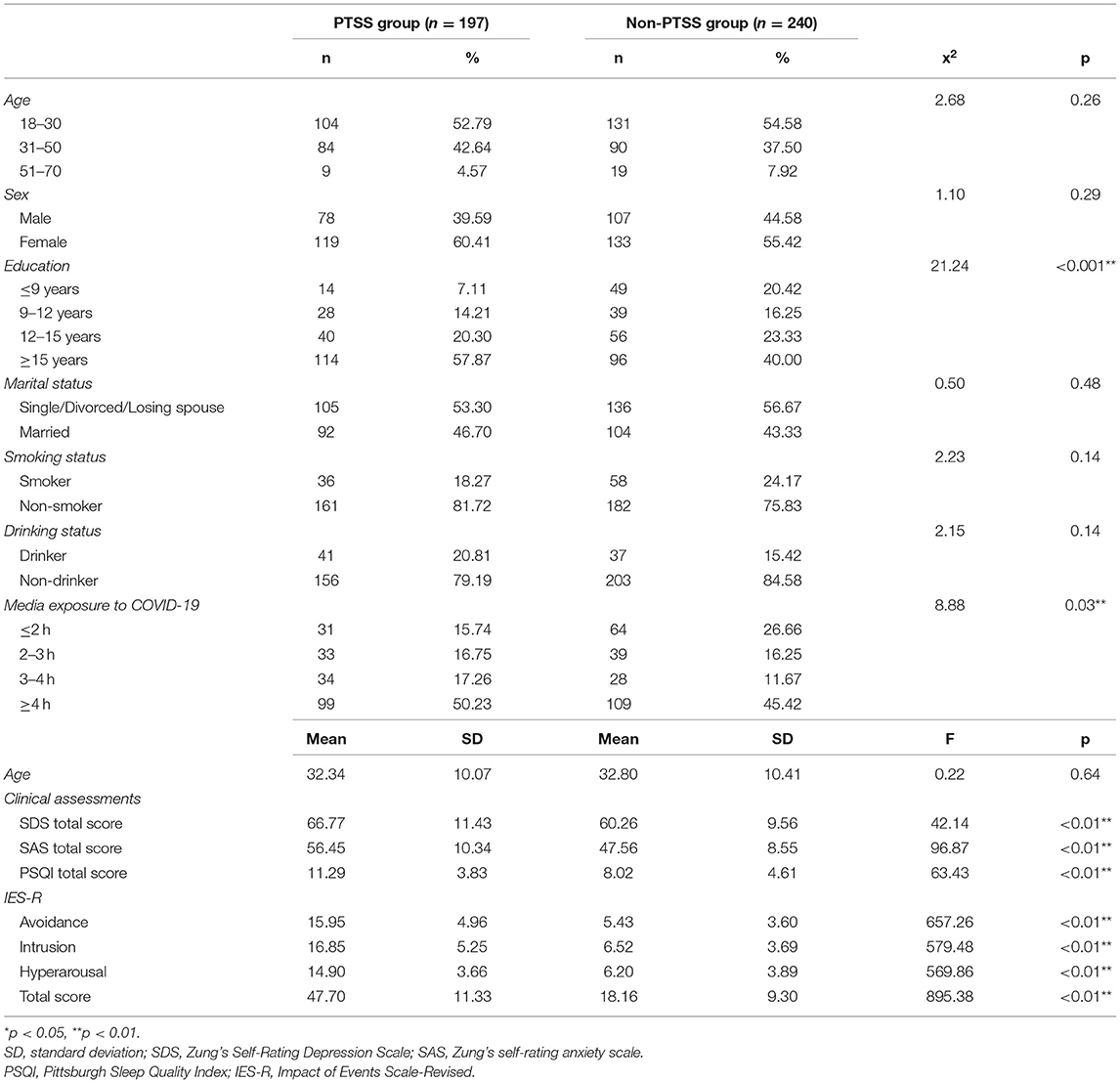
Table 2. Social demography and clinical characteristics of depressed subjects with PTSS and without-PTSS (IES-R ≥ 33) (x2 and MANOVA).
Correlation analyses revealed that IES-R total score was significantly associated with education levels (r = 0.229, P < 0.001), media exposure to COVID-19 (r = 0.114, p = 0.017), SDS score (r = 0.418, P < 0.001), SAS score (r = 0.553, P < 0.001), and PSQI score (r = 0.457, p < 0.001) (Detailed results of correlation analyses are provided in Table 3). Further, education, SDS score, SAS score, and PSQI score passed the Bonferroni correction (α = 0.05/14 = 0.004).
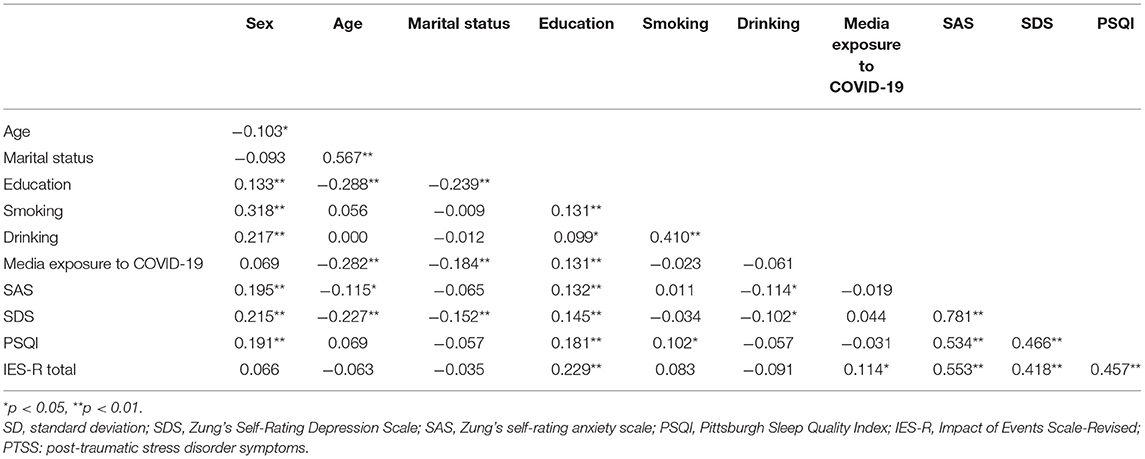
Table 3. Correlations between demographic characteristics and clinical variables of depressed group.
Further multiple regression analyses were used to examine the relationship between IES-R scores and other variables in the depression group. The covariates in these stepwise forward input models included those with Ps<0.1 in univariate analyses, including age, gender, education, media exposure to COVID-19, SDS, SAS, and PSQI scores. The results of the multiple linear regression analysis are presented in Table 4. Multiple linear regression analysis showed that education level (β = 0.122, t = 3.121, p = 0.002), media exposure COVID-19 (β = 0.118, t = 3.068, p = 0.002), SAS score (β = 0.498, t = 7.759, P < 0.001), and PSQI score (β = 0.217, t = 4.747, P < 0.001) remained associated with the total IES-R score.
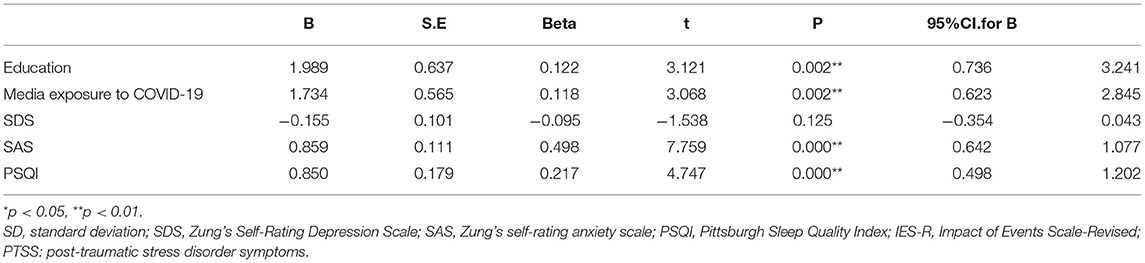
Table 4. Multiple regression results of IES-R total score and related variables among depressed group.
In the non-depressed control group, the PTSS subgroup was older and had higher SDS scores, SAS scores and PSQI scores, and IES-R total and subscale scores compared to the non-PTSS subgroup (all P < 0.05) (see Chi-square test and MANOVA results in Table 5). After adjusting for covariates including age, gender, education, and marital status, differences remained significant for SDS scores (F1,2934 = 107.11, P < 0. 001, Bonferroni correction), SAS scores (F1,2934 = 142.67, P < 0.001, Bonferroni correction), PSQI scores (F1,2934 = 113.05, P < 0.001, Bonferroni corrected), IES-R total score (F1,2934 = 1,222.74, P < 0.001, Bonferroni corrected), IES-R avoidance subscale score (F1,2934 = 858.85, P < 0.001, Bonferroni corrected), and between two subgroups of IES-R intrusion subscale scores (F1,2934 = 917.70, P < 0.001, Bonferroni corrected) and IES-R overanxiety subscale scores (F1,2934 = 783.55, P < 0.001, Bonferroni corrected).
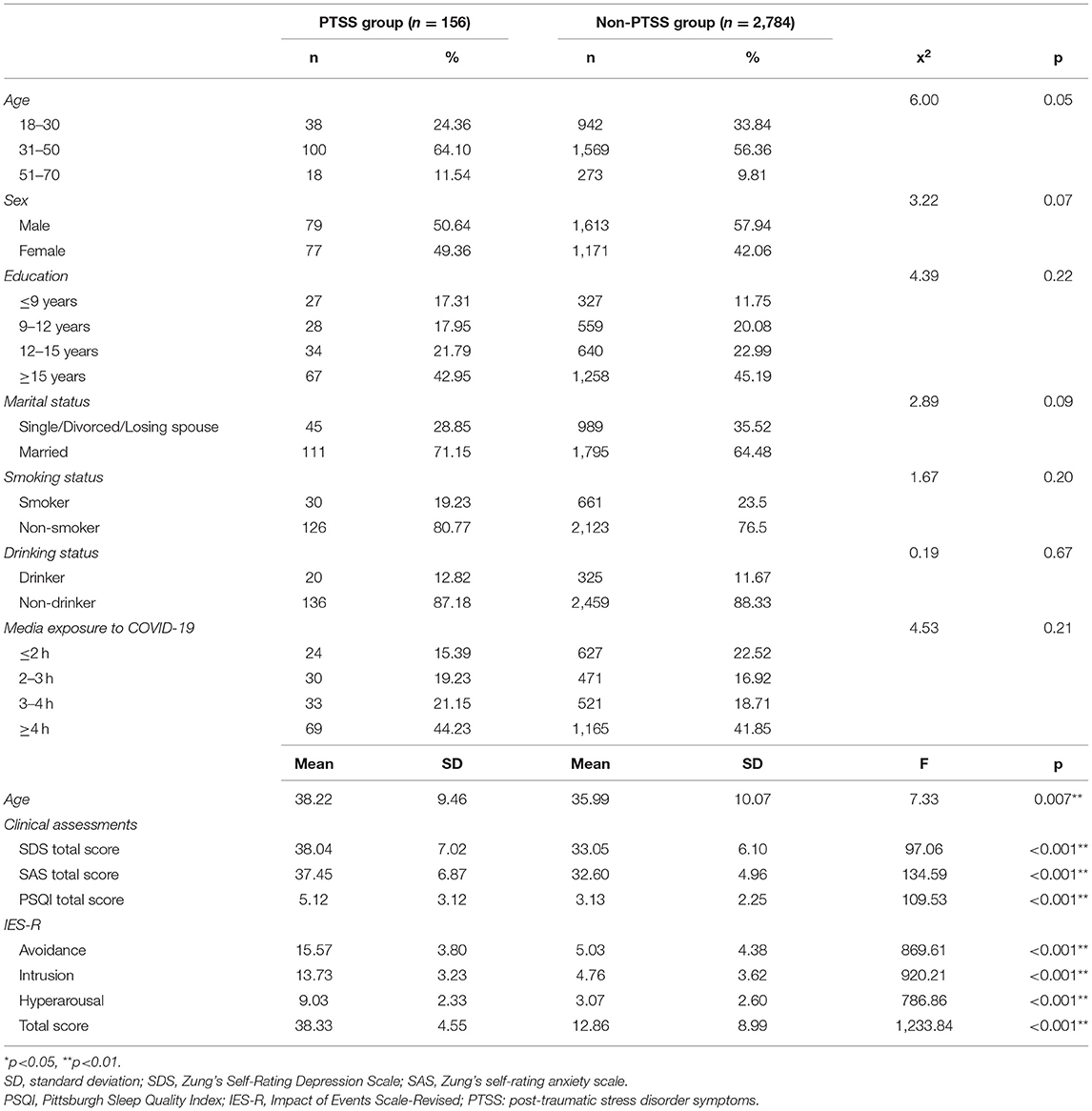
Table 5. Social demography and clinical characteristics of non-depressed subjects with PTSS and without-PTSS (IES-R ≥ 33) (x2 and MANOVA).
Results of the correlation analyses are summarized in Table 6. Correlation analysis revealed that IES-R total score was significantly associated with sex (r = 0.040, p = 0.031), age (r = 0.057, p = 0.002), marital status (r = 0.056, p = 0.002), media exposure to COVID-19 (r = 0.060, p = 0.001), SDS score (r = 0.326, p < 0.001), SAS score (r = 0.305 p < 0.001), and PSQI score (r = 0.345, p < 0.001).Further, age, marital status, media exposure to COVID-19, SDS score, SAS score and PSQI score passed the Bonferroni correction (α = 0.05/14 = 0.004).
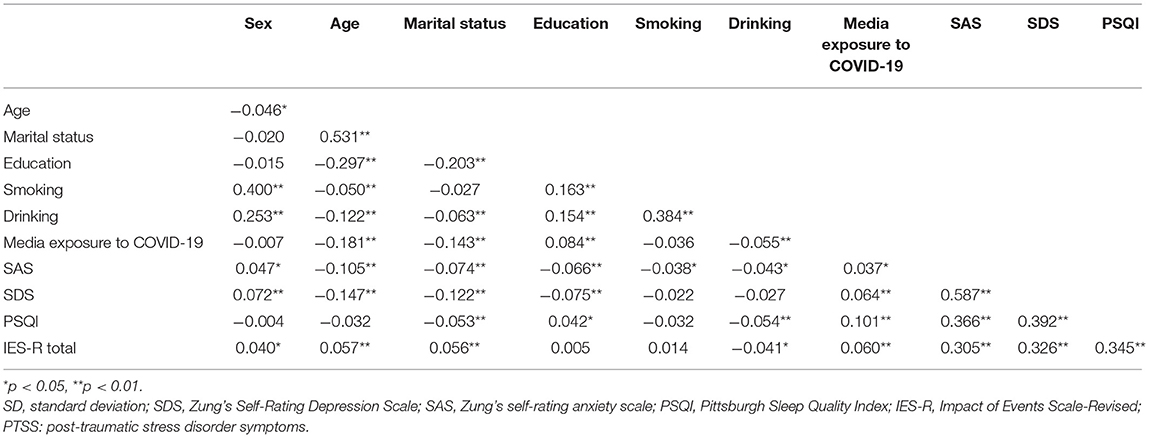
Table 6. Correlations between demographic characteristics and clinical variables of non-depressed group.
In addition, we used multiple linear regression analysis to examine the relationship between IES-R scores and other variables in the non-depressed group. The covariates in these stepwise forward input models included those with Ps<0.1 in univariate analyses, including age, gender, marital status, SDS, SAS, and PSQI scores. The results of the multiple linear regression analysis are presented in Table 7. Multiple linear regression showed that age (β = 0.072, t = 3.648, P < 0.001), marital status (β = 0.062, t = 3.125, p = 0.002), SDS score (β = 0.175, t = 8.203, P < 0. 001), SAS score (β = 0.127, t = 6.062, P < 0.001) and PSQI scores (β = 0.235, t = 12.744, P < 0.001) remained correlated with total IES-R scores.
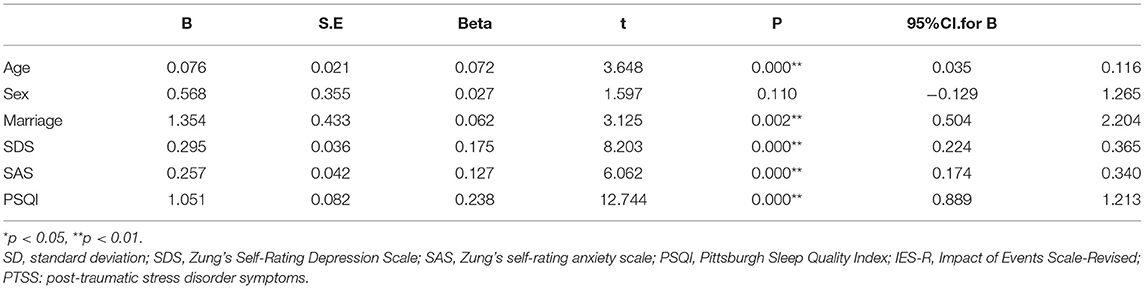
Table 7. Multiple regression results of IES-R total score and related variables among non-depressed group.
The main purpose of this research is to explore the co-morbidity rate, clinical predictive factors and correlations of PTSS among MDD patients. There were the following main findings in this study. (1) During the initial stage of COVID-19, there was a high co-morbidity rate of PTSS in MDD patients (45.08%). (2) In patients with depression and non-depressed controls, SDS score, SAS score, and PSQI score were significantly correlated with PTSS. (3) In patients with depression, people with higher education and more time exposure to COVID-19 media coverage were more likely to suffer from PTSS. (4) In non-depressed controls, married subjects and 31~50-year age group were more likely to suffer from PTSS.
In this study, we found a co-morbidity rate of 45.08% (197/437) for PTSS in MDD patients, much higher than in non-depressed controls (5.31%, 156/2,940). Because few studies have focused on PTSS comorbidity in MDD patients during the COVID-19 pandemic, we compared our results with other populations during the COVID-19 pandemic and with several studies prior to the COVID-19 pandemic. When compared with other populations during the COVID-19 pandemic, we found a significantly higher prevalence of PTSS among MDD patients in our sample (45.08%, 95% CI: 40.4–49.8%) than among adolescent MDD patients in China (34.4%) (46) and among COVID-19 survivors during the COVID-19 pandemic (18.66%, 95% CI: 11.98–25.34%) (47), health care workers (28.0%, 95% CI: 9.5–59.0%) (48) and general population (12.8%) (49). Compared with other studies before the COVID-19 pandemic, our 45.08% prevalence was similar to the co-occurrence of depressive symptoms and PTSS 3 months after the 2016 Salt Lake City tornado (44.94%) (50) and close to the global prevalence estimates of MDD and PTSD in the pre-pandemic Meta-analysis of COVID-19 (52%). In addition, we found that depressed patients were 16 times more likely to have PTSS than non-depressed patients. This result suggests that during the COVID-19 pandemic, patients with MDD were more likely to experience severe psychological distress and PTSS than non-depressed controls and some other high-risk populations.
Despite the high rate of comorbidity of posttraumatic stress symptoms and depression, the underlying mechanisms are far from being fully understood. One hypothesis proposes that the high comorbidity rate may be the result of common susceptibility factors, including biological factors, such as certain brain regions, certain specific genetic polymorphisms, etc. For example, the insular (i.e., insular cortex) has been associated with both PTSD and depression. Furthermore, previous studies have shown genetic correlations of 0.71 to 0.80 between PTSD and depression phenotypes (51). Some specific genetic polymorphisms have been shown to be associated with high rates of combined PTSD and MDD (51). For example, the 5-hydroxytryptamine transporter-linked polymorphic region (5-HTTLPR) has been suggested as a possible candidate gene to regulate emotional responses to traumatic events. the interaction between 5HTTLPR mutations and stressful life events can predict depression and PTSD (46, 47). The A1 allele encoding a type 2 dopaminergic receptor is associated with the comorbidity of PTSD and depression (46). Carriers of the G allele of the OXTR rs53576 gene are more likely to have co-morbid PTSD-depression (48). Defects in the GRK-βarrestin2 machinery would lead to excessive CRF (1) receptor signaling, resulting in PTSD and co morbid PTSD (49). In addition, meta-analysis showed that subjects with specific alleles of the FKBP5 gene were more likely to develop MDD and PTSD (50). Thus, many factors may make depressed subjects more likely to develop PTSD, but further research is needed to explore additional possibilities.
We also found that PTSS level was positively correlated with depression level, which is consistent with previous study showing that initial levels of PTSS predicted depressive symptoms (52).
Despite the SDS score, our study identified several other common correlates for PTSS in both patients with depression and non-depressed controls. We found that the IES-R total score was positively associated with SAS score in both depression and non-depression groups, which was consistent with previous studies on breast cancer survivors (53). Another study on American adolescents also showed that anxiety was the most common psychiatric comorbidities in hospitalized adolescent patients with PTSS (54).
Furthermore, this study illustrated that PTSS were significantly positively correlated with poor sleep quality both in depression and non-depression groups, which was in accordance with previous studies, showing that subjects with better sleep quality reported fewer PTSS during COVID-19. Another study also showed that pre-deployment sleep quality was a predictive feature of post-deployment PTSD in active-duty army (55). Recent studies have shown that the relationship between sleep disorders and PTSD is bidirectional (56). Patients with sleep disturbances prior to a traumatic event are more likely to develop PTSD after exposure to a traumatic event (57). Poor sleep quality is a common symptom and feature of PTSD (56) and a predictor of poor PTSD prognosis (58).
Recent studies have shown that the frequency of exposure to social media was positively associated with acute stress symptoms and anxiety during COVID-19 (44). For example, Ma et al. found that students exposed to COVID-19 media for ≥3 h per day were 2.13 times more likely to have acute stress symptoms than those exposed to media for <1 h per day (59). Ni et al. reported that subjects exposed to COVID-19 media for ≥4 hours per day had significantly higher levels of anxiety than those who used it for ≤2 hours (44). In the present study, by subgroup comparison, we found that subjects exposed to COVID-19 media ≤2 h per day had a significantly lower incidence of PTSS than those exposed for 3–4 h per day (P < 0.05). Furthermore, our multiple linear regression also showed that media exposure to COVID-19 was a predictor of PTSS in the depression group, so we further confirmed that the duration of social media exposure in COVID-19 was also associated with PTSS in depressed patients.
We also found that people with higher education were more vulnerable to PTSS in the depressed group, which is consistent with previous observational studies on Nibel traumatized patients, indicating that subjects with high school education or above are more vulnerable to PTSD (60). However, there was no significant correlation between PTSS and education level in the non-depressed control group.
Further, we found that non-depressed subjects between the ages of 31 and 50 years reported more PTSS. Previous studies have demonstrated that age is an effective risk factor for PTSD. For example, Zhang et al. reported that after the 512 Wenchuan earthquake in China, the 30 40-years-old age group reported more PTSD than other age groups (61). Also, Koirala et al. observed that the 31–45-years-old age group was susceptible to PTSD (60), and Divsalar et al. also observed similar results 12 years after the Bam earthquake in Iran (62). Our results are consistent with those previous results. In addition, our study also found that married respondents were more likely to suffer from PTSS than single respondents in non-depressed respondents, which was in accordance with previous research among war veterans (63).
Some of the limitations of our study need to be addressed. First, given this study was cross-sectional, it cannot infer the causality between PTSS and related risk factors. Further studies of prospective longitudinal designs are needed to confirm the association observed in this study. Second, as all participants were enrolled from Shenzhen, China. The level of exposure to COVID-19 in this region is relatively low (462 cases of COVID-19 as of May 9, 2020). Therefore, we should be cautious in extrapolating these findings to other regions and further studies in other ethnic populations are needed. Third, this is a scale-based study. IES-R was used to quantify PTSS. However, PTSD diagnosis have not been established. The lack of PTSD diagnosis may also limit the effectiveness of this study. Fourth, we had 30 epidemiological study groups, and because the data collected went directly into the electronic database, we could not distinguish whether there were differences in the data collected by the different epidemiological study groups. Fifth, the sample size of this study was moderate, which may limit its generalizability.
In conclusion, our results show that during the COVID-19 outbreak, the prevalence of PTSS in the MDD patients was very high (45.08%), and patients with depression were 16 times more likely to suffer from PTSS that those without depression. Our findings in this study have certain clinical implications, showing that nearly half of MDD patients may have PTSS during the COVID-19 pandemic, even if they did not report a severe traumatic event. Previous studies have indicated that MDD patients with PTSS may have a worse prognosis (32). Therefore, the results of this study remind us that such patients should be identified as early as possible, and we can then better predict the course and prognosis of these patients and further optimize their treatment options.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
This study was approved by the Ethics Review Committee of Huazhong University of Science and Technology Union Shenzhen Hospital. The patients/participants provided their written informed consent to participate in this study.
MP, XZ, and TG designed the study. MP, XS, LL, WZ, PL, GB, and TG participated in the data collection. MP analyzed the data and drafted the manuscript. XZ revised the manuscript. All authors contributed to and approved the final manuscript.
This study was supported by National Natural Science Foundation of China, Grant/Award Number: 31871115.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Forte G, Favieri F, Tambelli R, Casagrande M. COVID-19 Pandemic in the Italian Population: Validation of a Post-Traumatic Stress Disorder Questionnaire and Prevalence of PTSD Symptomatology. Int J Environ Res Public Health, (2020). 17:2020. doi: 10.3390/ijerph17114151
2. Rajkumar RP. COVID-19 and mental health: A review of the existing literature. Asian J Psychiatr. (2020) 52:102066. doi: 10.1016/j.ajp.2020.102066
3. Smith K, Ostinelli E, Cipriani A. Covid-19 and mental health: a transformational opportunity to apply an evidence-based approach to clinical practice and research. Evid Based Ment Health. (2020) 23:45–6. doi: 10.1136/ebmental-2020-300155
4. Webb L. Covid-19 lockdown: a perfect storm for older people's mental health. J Psychiatr Ment Health Nurs. (2020) 28:300. doi: 10.1111/jpm.12644
5. Tsamakis K, Rizos E, A JM, Chaidou S, Kympouropoulos S, Spartalis E, et al. COVID-19 pandemic and its impact on mental health of healthcare professionals. Exp Ther Med. (2020) 19:3451–3. doi: 10.3892/etm.2020.8646
6. Liu Y, Chen H, Zhang N, Wang X, Fan Q, Zhang Y, et al. Anxiety and depression symptoms of medical staff under COVID-19 epidemic in China. J Affect Disord. (2021) 278:144–8. doi: 10.1016/j.jad.2020.09.004
7. van der Velden PG, Contino C, Das M, van Loon P, Bosmans MWG. Anxiety and depression symptoms, and lack of emotional support among the general population before and during the COVID-19 pandemic. A prospective national study on prevalence and risk factors. J Affect Disord. (2020) 277:540–8. doi: 10.1016/j.jad.2020.08.026
8. Elhai JD, Yang H, McKay D, Asmundson GJG. COVID-19 anxiety symptoms associated with problematic smartphone use severity in Chinese adults. J Affect Disord. (2020) 274:576–82. doi: 10.1016/j.jad.2020.05.080
9. Arafa A, Mohammed Z, Mahmoud O, Elshazley M, Ewis A. Depressed, anxious, and stressed: What have healthcare workers on the frontlines in Egypt and Saudi Arabia experienced during the COVID-19 pandemic? J Affect Disord. (2021) 278:365–71. doi: 10.1016/j.jad.2020.09.080
10. Liguori C, Pierantozzi M, Spanetta M, Sarmati L, Cesta N, Iannetta M, et al. Depressive and anxiety symptoms in patients with SARS-CoV2 infection. J Affect Disord. (2021) 278:339–40. doi: 10.1016/j.jad.2020.09.042
11. Li Q, Miao Y, Zeng X, Tarimo CS, Wu C, Wu J. Prevalence and factors for anxiety during the coronavirus disease (2019). (COVID-19) epidemic among the teachers in China. J Affect Disord. (2020) 277:153–8. doi: 10.1016/j.jad.2020.08.017
12. Zhang X-R, Huang Q-M, Wang X-M, Cheng X, Li Z-H, Wang Z-H, et al. Prevalence of anxiety and depression symptoms, and association with epidemic-related factors during the epidemic period of COVID-19 among 123,768 workers in China: A large cross-sectional study. J Affect Disord. (2020) 277:495–502. doi: 10.1016/j.jad.2020.08.041
13. Qiu D, Li Y, Li L, He J, Ouyang F, Xiao S. Infectious disease outbreak and post-traumatic stress symptoms: a systematic review and meta-analysis. Front Psychol. (2021) 12:668784. doi: 10.3389/fpsyg.2021.668784
14. Liang L, Gao T, Ren H, Cao R, Qin Z, Hu Y, et al. Post-traumatic stress disorder and psychological distress in Chinese youths following the COVID-19 emergency. J Health Psychol. (2020). 25:1164–75. doi: 10.1177/1359105320937057
15. Allan SM, Bealey R, Birch J, Cushing T, Parke S, Sergi G, et al. The prevalence of common and stress-related mental health disorders in healthcare workers based in pandemic-affected hospitals: a rapid systematic review and meta-analysis. Eur J Psychotraumatol. (2020) 11:1810903. doi: 10.1080/20008198.2020.1810903
16. Yuan Y, Liu ZH, Zhao YJ, Zhang Q, Zhang L, Cheung T, et al. Prevalence of post-traumatic stress symptoms and its associations with quality of life, demographic and clinical characteristics in COVID-19 survivors during the post-COVID-19 era. Front Psychiatry. (2021). 12:665507. doi: 10.3389/fpsyt.2021.665507
17. Zhao YJ, Jin Y, Rao WW, Li W, Zhao N, Cheung T, et al. The prevalence of psychiatric comorbidities during the SARS and COVID-19 epidemics: a systematic review and meta-analysis of observational studies. J Affect Disord. (2021) 287:145–57. doi: 10.1016/j.jad.2021.03.016
18. Amra B, Salmasi M, Soltaninejad F, Sami R, Nickpour M, Mansourian M, et al. Healthcare workers' sleep and mood disturbances during COVID-19 outbreak in an Iranian referral center. Sleep Breath. (2021) 25:2197–204. doi: 10.1007/s11325-021-02312-4
19. Helito AC, Lindoso L, Sieczkowska SM, Astley C, Queiroz LB, Rose N, et al. Poor Sleep quality and health-related quality of life impact in adolescents with and without chronic immunosuppressive conditions during COVID-19 quarantine. Clinics (São Paulo). (2021) 76:e3501. doi: 10.6061/clinics/2021/e3501
20. Fu L, Fang Y, Luo D, Wang B, Xiao X, Hu Y, et al. Pre-hospital, in-hospital and post-hospital factors associated with sleep quality among COVID-19 survivors 6 months after hospital discharge: cross-sectional survey in five cities in China - CORRIGENDUM. BJPsych Open. (2021) 7:e214. doi: 10.1192/bjo.2021.1051
21. Wu XY, You JH, Li AJ, He Z, Huang C, Prevalence Prevalence and risk factors of anxiety depression and sleeping disturbances in china during the COVID-19 outbreak: a web-based cross-sectional study. Psychol Health Med. (2021) 1–9. doi: 10.1080/13548506.2021.2003829
22. Liu Y, Wang X, Sun P, Zhang Q, Zhang C, Shen Y, et al. Sleep disturbance and anxiety symptom among public during the second wave of COVID-19 in Beijing: A web-based cross-sectional survey. J Affect Disord. (2021) 298:80–5. doi: 10.1016/j.jad.2021.10.068
23. Yilmaz M, Kiraç Y, Sahin MK. Sleep quality and related factors in a sample of Turkish healthcare workers during the COVID-19 pandemic: A cross-sectional study. Int J Clin Pract. (2021) 75:e14813. doi: 10.1111/ijcp.14813
24. Schou TM, Joca S, Wegener G, Bay-Richter C. Psychiatric and neuropsychiatric sequelae of COVID-19 - A systematic review. Brain Behav Immun. (2021) 97:328–48. doi: 10.1016/j.bbi.2021.07.018
25. Salehi M, Amanat M, Mohammadi M, Salmanian M, Rezaei N, Saghazadeh A, et al. The prevalence of post-traumatic stress disorder related symptoms in Coronavirus outbreaks: A systematic-review and meta-analysis. J Affect Disord. (2021) 282:527–38. doi: 10.1016/j.jad.2020.12.188
26. Pollock A, Campbell P, Cheyne J, Cowie J, Davis B, McCallum J, et al. Interventions to support the resilience and mental health of frontline health and social care professionals during and after a disease outbreak, epidemic or pandemic: a mixed methods systematic review. Cochrane Database Syst Rev. (2020) 11:Cd013779. doi: 10.1002/14651858.CD013779
27. Liang Y, Wu K, Zhou Y, Huang X, Zhou Y, Liu Z. Mental health in frontline medical workers during the (2019). novel coronavirus disease epidemic in China: A comparison with the general population. Int J Environ Res Public Health. (2020). 17:6550. doi: 10.3390/ijerph17186550
28. Liu N, Zhang F, Wei C, Jia Y, Shang Z, Sun L, et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: Gender differences matter. Psychiatry Res. (2020) 287:112921. doi: 10.1016/j.psychres.2020.112921
29. McNett S, Lind MJ, Brown RC, Hawn S, Berenz EC, Brown E, et al. Sleep quality moderates the relationship between anxiety sensitivity and PTSD symptoms in combat-exposed veterans. Behav Sleep Med. (2021). 19:208–20. doi: 10.1080/15402002.2020.1726749
30. Mundy J, Hübel C, Gelernter J, Levey D, Murray RM, Skelton M, et al. Psychological trauma and the genetic overlap between posttraumatic stress disorder and major depressive disorder. Psychol Med. (2021) 1–10. doi: 10.1017/S0033291721000830
31. Radell ML, Hamza EA, Moustafa AA. Depression in post-traumatic stress disorder. Rev Neurosci. (2020) 31:703–22. doi: 10.1515/revneuro-2020-0006
32. Rytwinski NK, Scur MD, Feeny NC, Youngstrom EA. The co-occurrence of major depressive disorder among individuals with posttraumatic stress disorder: a meta-analysis. J Trauma Stress. (2013) 26:299–309. doi: 10.1002/jts.21814
33. Zung WW. A SELF-RATING DEPRESSION SCALE. Arch Gen Psychiatry. (1965) 12:63–70. doi: 10.1001/archpsyc.1965.01720310065008
34. Jokelainen J, Timonen M, Keinänen-Kiukaanniemi S, Härkönen P, Jurvelin H, Suija K. Validation of the Zung self-rating depression scale (SDS) in older adults. Scand J Prim Health Care. (2019) 37:353–7. doi: 10.1080/02813432.2019.1639923
35. Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom Med. (1979) 41:209–18. doi: 10.1097/00006842-197905000-00004
36. Wu KK, Chan KS. The development of the Chinese version of Impact of Event Scale–Revised (CIES-R). Soc Psychiatry Psychiatr Epidemiol. (2003) 38:94–8. doi: 10.1007/s00127-003-0611-x
37. Hao F, Tan W, Jiang L, Zhang L, Zhao X, Zou Y, et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav Immun. (2020). doi: 10.1016/j.bbi.2020.04.069
38. Creamer M, Bell R, Failla S. Psychometric properties of the impact of event scale - revised. Behav Res Ther. (2003) 41:1489–96. doi: 10.1016/j.brat.2003.07.010
39. Chatzittofis A, Karanikola M, Michailidou K, Constantinidou A. Impact of the COVID-19 pandemic on the mental health of healthcare workers. Int J Environ Res Public Health. (2021) 18:1435. doi: 10.3390/ijerph18041435
40. Rousseau AF, Minguet P, Colson C, Kellens I, Chaabane S, Delanaye P, et al. Post-intensive care syndrome after a critical COVID-19: cohort study from a Belgian follow-up clinic. Ann Intensive Care. (2021) 11:118. doi: 10.1186/s13613-021-00910-9
41. Zung WW. A rating instrument for anxiety disorders. Psychosomatics. (1971) 12:371–9. doi: 10.1016/S0033-3182(71)71479-0
42. Buysse DJ, Reynolds CF. 3rd, Monk TH, Berman SR, and Kupfer DJ, The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
43. Mollayeva T, Thurairajah P, Burton K, Mollayeva S, Shapiro CM, Colantonio A. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: A systematic review and meta-analysis. Sleep Med Rev. (2016) 25:52–73. doi: 10.1016/j.smrv.2015.01.009
44. Ni MY, Yang L, Leung CM. C, Li N, Yao XI, Wang Y, et al. Mental Health, Risk Factors, and Social Media Use During the COVID-19 Epidemic and Cordon Sanitaire Among the Community and Health Professionals in Wuhan, China: Cross-Sectional Survey. JMIR Ment Health. (2020) 7:e19009. doi: 10.2196/19009
45. Ma Z, Zhao J, Li Y, Chen D, Wang T, Zhang Z, et al. Mental health problems and correlates among 746 217 college students during the coronavirus disease 2019 outbreak in China. Epidemiol Psychiatr Sci. (2020) 29:e181. doi: 10.1017/S2045796020000931
46. Auxéméry Y. Posttraumatic stress disorder (PTSD) as a consequence of the interaction between an individual genetic susceptibility, a traumatogenic event and a social context. Encephale. (2012) 38:373–80. doi: 10.1016/j.encep.2011.12.003
47. Maul S, Giegling I, Fabbri C, Corponi F, Serretti A, Rujescu D. Genetics of resilience: Implications from genome-wide association studies and candidate genes of the stress response system in posttraumatic stress disorder and depression. Am J Med Genet B Neuropsychiatr Genet. (2020) 183:77–94. doi: 10.1002/ajmg.b.32763
48. Cao C, Wang L, Wu J, Li G, Fang R, Liu P, et al. Association between the OXTR rs53576 genotype and latent profiles of post-traumatic stress disorder and depression symptoms in a representative sample of earthquake survivors. Anxiety Stress Coping. (2020) 33:140–7. doi: 10.1080/10615806.2019.1695604
49. Hauger RL, Olivares-Reyes JA, Dautzenberg FM, Lohr JB, Braun S, Oakley RH. Molecular and cell signaling targets for PTSD pathophysiology and pharmacotherapy. Neuropharmacology. (2012) 62:705–14. doi: 10.1016/j.neuropharm.2011.11.007
50. Wang Q, Shelton RC, Dwivedi Y. Interaction between early-life stress and FKBP5 gene variants in major depressive disorder and post-traumatic stress disorder: A systematic review and meta-analysis. J Affect Disord. (2018) 225:422–8. doi: 10.1016/j.jad.2017.08.066
51. Zhang F, Rao S, Cao H, Zhang X, Wang Q, Xu Y, et al. Genetic evidence suggests posttraumatic stress disorder as a subtype of major depressive disorder. J Clin Invest. (2021). doi: 10.1172/JCI145942
52. Peng M, Mo B, Liu Y, Xu M, Song X, Liu L, et al. Prevalence, risk factors and clinical correlates of depression in quarantined population during the COVID-19 outbreak. J Affect Disord. (2020) 275:119–24. doi: 10.1016/j.jad.2020.06.035
53. Vazquez D, Rosenberg S, Gelber S, Ruddy KJ, Morgan E, Recklitis C, et al. Posttraumatic stress in breast cancer survivors diagnosed at a young age. Psychooncology. (2020). doi: 10.1002/pon.5438
54. Eskander N, Vadukapuram R, Zahid S, Ashraf S, Patel RS. Post-traumatic stress disorder and suicidal behaviors in american adolescents: analysis of 159,500 psychiatric hospitalizations. Cureus. (2020) 12:e8017. doi: 10.7759/cureus.8017
55. Schultebraucks K, Qian M, Abu-Amara D, Dean K, Laska E, Siegel C, et al. Pre-deployment risk factors for PTSD in active-duty personnel deployed to Afghanistan: a machine-learning approach for analyzing multivariate predictors. Mol Psychiatry. (2020). doi: 10.1038/s41380-020-0789-2
56. Richards A, Kanady JC, Neylan TC. Sleep disturbance in PTSD and other anxiety-related disorders: an updated review of clinical features, physiological characteristics, and psychological and neurobiological mechanisms. Neuropsychopharmacology. (2020) 45:55–73. doi: 10.1038/s41386-019-0486-5
57. Wang HE, Campbell-Sills L, Kessler RC, Sun X, Heeringa SG, Nock MK, et al. Pre-deployment insomnia is associated with post-deployment post-traumatic stress disorder and suicidal ideation in US Army soldiers. Sleep. (2019) 42. doi: 10.1093/sleep/zsy229
58. Brownlow JA, McLean CP, Gehrman PR, Harb GC, Ross RJ, Foa EB. Influence of sleep disturbance on global functioning after posttraumatic stress disorder treatment. J Trauma Stress. (2016) 29:515–21. doi: 10.1002/jts.22139
59. Ma L, Mazidi M, Li K, Li Y, Chen S, Kirwan R, et al. Prevalence of mental health problems among children and adolescents during the COVID-19 pandemic: A systematic review and meta-analysis. J Affect Disord. (2021) 293:78–89. doi: 10.1016/j.jad.2021.06.021
60. Koirala R, Søegaard EGI, Ojha SP, Hauff E, Thapa SB. Trauma related psychiatric disorders their correlates in a clinical sample: A cross-sectional study in trauma affected patients visiting a psychiatric clinic in Nepal. PLoS ONE. (2020) 15:e0234203. doi: 10.1371/journal.pone.0234203
61. Zhang Y, Ho SM. Risk factors of posttraumatic stress disorder among survivors after the 512 Wenchuan earthquake in China. PLoS ONE. (2011) 6:e22371. doi: 10.1371/journal.pone.0022371
62. Divsalar P, Dehesh T. Prevalence and predictors of post-traumatic stress disorder and depression among survivors over 12 years after the bam earthquake. Neuropsychiatr Dis Treat. (2020) 16:1207–16. doi: 10.2147/NDT.S252730
Keywords: post-traumatic stress disorder, PTSD, posttraumatic stress symptom, PTSS, depression, COVID-19, prevalence, correlates
Citation: Peng M, Song X, Liu L, Zhao W, Lai P, Bao G, Guo T and Zhang X (2022) Comparison of Prevalence and Risk Factors of PTSS Between Chinese Patients With Depression and Non-depressed Controls During COVID-19 Outbreak. Front. Psychiatry 12:719931. doi: 10.3389/fpsyt.2021.719931
Received: 03 June 2021; Accepted: 06 December 2021;
Published: 03 January 2022.
Edited by:
Wanhong Zheng, West Virginia University, United StatesReviewed by:
Benedetto Vitiello, University of Turin, ItalyCopyright © 2022 Peng, Song, Liu, Zhao, Lai, Bao, Guo and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tianyou Guo, Z3R5b3UxNjhAMTI2LmNvbQ==; Xiangyang Zhang, emhhbmd4eUBwc3ljaC5hYy5jbg==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.