- 1Department of Sport Rehabilitation, Shanghai University of Sport, Shanghai, China
- 2Rehabilitation Therapy Center, Luoyang Orthopedic Hospital of Henan Province, Luoyang, China
- 3Department of Rehabilitation Medicine, Shanghai Shangti Orthopedic Hospital, Shanghai, China
Background: While most previous studies regarding patients with chronic low back pain (CLBP) mainly focused on pain, disability, psychological damage, and intervention measures, the effect of CLBP on personal space remains unclear. The study aimed to assess the personal space of patients with CLBP and healthy controls, explored the differences between the two groups, and examined whether pain, dysfunction, anxiety, and depression affected the personal space regulation.
Methods: The cross-sectional study recruited 24 patients with CLBP and 24 healthy controls at Shanghai Shangti Orthopedic Hospital and Shanghai University of Sport, Shanghai, China, from December 2018 to January 2019. A stop-distance paradigm was applied to measure the comfortable and uncomfortable distance under four conditions. A self-rating anxiety scale (SAS) and a self-rating depression scale (SDS) were used to examine the anxiety and depression levels of all participants. The pain intensity and dysfunction in the CLBP group were evaluated by the numeric rating scale and Roland-Morris questionnaire (RMDQ), respectively.
Results: When approaching another individual or when being approached, the interpersonal distance under all the conditions in the CLBP group significantly differed from that in the healthy control group with larger space distances (p < 0.01). Gender had a significant main effect on the regulation of personal space in patients with CLBP (p < 0.05). The average pain intensity, scores on RMDQ, SAS, and SDS had a significant positive correlation with the interpersonal distance under the Same or Opposite Gender condition (p < 0.05).
Conclusion: People with CLBP show an atypical personal space behavior and indeed have a greater interpersonal distance to strangers. The higher the pain intensity, dysfunction, anxiety, and depression, the greater the interpersonal distance in patients with CLBP. In the future, the effect and underlying neural mechanisms of pain and negative emotions on social withdrawal in patients should be examined.
Introduction
Low back pain (LBP) is defined as pain that occurs between the inferior border of the ribs and the buttock wrinkles, which may be accompanied by lower limb pain or related neurological symptoms (1, 2). Most LBP cases tend to subside within the first 6 weeks (3), while approximately 10% of them will develop into chronic low back pain (CLBP) (4, 5). CLBP, a type of LBP that lasts or fluctuates for more than three months (6), is the most common chronic pain disease that causes clinical, public health, and social problems in the world (7). Normally, 51–80% of adults suffer from CLBP at some point in their lives (8, 9). It also causes a huge economic loss ranging from 12.2 billion to 90.6 billion (6). In addition to pain and impaired function, CLBP limits leisure activities, social activities, and public engagements as well (10). Pain could negatively impact social relationships, such as poor relationships between children and peers (11) and reduced marital satisfaction between partners (12). Furthermore, the associations between CLBP with interpersonal relationships, social withdrawal, and psychological distress, such as depression and loneliness, have been demonstrated (13–15).
Since humans are fully socialized creatures and spend almost 80% of their waking time with other people (16), sociality plays a vital role in their physical and mental health (17). Generally, the lack of sociality is expressed as increased personal space, including increased interpersonal distance, social withdrawal, social isolation, and subjective feelings of loneliness (17, 18). When individuals lack contact with society, they feel social isolation and loneliness and experience social withdrawal. Insufficient social connections and following loneliness might produce pain and depression and result in a higher risk of cardiovascular disease, sleep disorders, suicidal tendencies, and degenerative dementia (17, 19–21). Individuals with social withdrawal likely show poor physical and psychological health. Additionally, a meta-analysis on social relationships and death risk has revealed that the odds ratio of increased mortality due to loneliness is 1.45, which is about twice that caused by obesity (21, 22).
Personal space refers to the perceived comfortable and safe area around individuals. Individuals normally experience discomfort and anxiety if it is intruded (23). During social interaction, they can automatically adjust the distance between themselves and others. Meanwhile, the ability to maintain proper interpersonal distance is conducive to positive and successful social interactions (24). Many studies have explored the adjustment of interpersonal distance among different groups of people. Lough et al. (25) investigated the differences in personal space adjustment between patients with Williams syndrome and typically developing peers. The findings suggested that patients with Williams syndrome more likely invade others' personal space and maintain a shorter interpersonal distance. Furthermore, Rubinsten et al. (26) studied the effect of deficiencies in spatial cognition on personal space regulation and reported that patients with developmental dyscalculia were less efficient in allocating spatial attention and had difficulties in adjusting personal space. Studies have shown that some patients with special diseases lack flexibility in personal space adjustment. It is an important aspect that reflects the social vulnerability profile (25). While a large number of studies regarding on CLBP mainly focused on pain, disability, psychological damage, and intervention measures (27–30), the effect of CLBP on social behavior remains unclear. In other words, it is still unsure whether patients with CLBP can normally adjust their personal space.
The study aimed to assess the personal space of patients with CLBP and healthy controls; explore the differences between the two groups; and examine whether pain, dysfunction, anxiety, and depression affected the personal space regulation in patients with CLBP. It is hypothesized that individuals with CLBP avoid to be too close to strangers and have a greater personal space than healthy controls; pain, dysfunction, anxiety, and depression negatively impact interpersonal distance; and patients with CLBP experience social withdrawal in daily life.
Methods
Participants
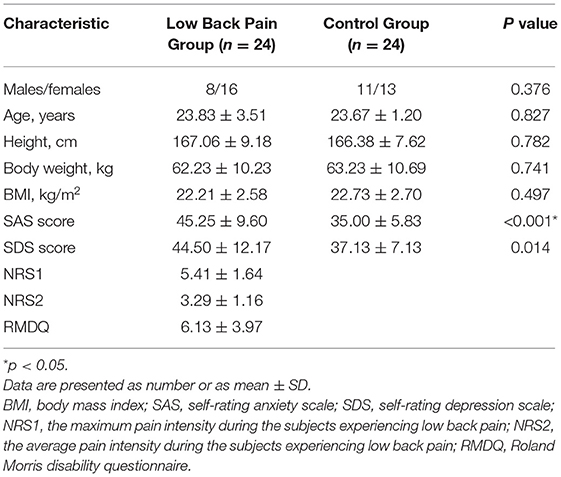
According to a previous study by Lough et al. (25), the sample size that can be calculated by G*Power should have 21 participants in each group (α = 0.05, d = 0.8, and power = 80%). In the present study, 24 patients with CLBP and 24 healthy adults were recruited between December 2018 and January 2019 from the Shanghai Shangti Orthopedic Hospital and Shanghai University of Sport, Shanghai, China. The CLBP group (≥18, average 23.83 ± 3.51 years old) and the control group (≥18, average 23.67 ± 1.20 years old) matched in terms of age (23.67 vs. 23.83 years), gender ratio (45.83% vs. 33.33% male), height (166.38 vs. 167.06 cm), body weight (63.23 vs. 62.23 kg), and body mass index (BMI, 22.73 vs. 22.21 kg/m2) (Table 1). All the participants met the inclusion and exclusion criteria, and they were instructed to abstain from alcohol or drugs for 24 h before the experiment. The healthy controls were included on the basis of the following criteria: (1) age over 18 years, (2) no chronic or acute pain in the body, and (3) able to communicate and understand the instructions well. They were excluded in accordance with the following criteria: (1) a history of neurologic or psychiatric disorders, (2) a history of substance use and abuse, (3) currently taking anti-depressants or analgesics, and (4) pregnant or lactating. The subjects with CLBP were included on the basis of the following criteria: (1) age over 18 years, (2) pain in the back area from below the costal margin to the gluteal fold and lasting at least 12 weeks with an average pain intensity of 3 or greater on an 11-point numerical rating scale in the previous week, (3) no other pain or pain unrelated to the lower back and no dysfunction in the body, and (4) able to communicate and understand the instructions well. The subjects with CLBP were excluded in accordance with the following criteria: (1) low back pain caused by intervertebral disk diseases, paravertebral infection or tumor, spinal diseases or injury, and visceral diseases, (2) a history of neurologic or psychiatric disorders, (3) a history of substance use and abuse, (4) currently taking anti-depressants or analgesics; and (5) pregnant or lactating.
The Ethics Committee of Shanghai University of Sport approved this study. All the subjects voluntarily participated and signed their written informed consent forms.
Assessment
Before participating in the study, all the subjects completed a questionnaire on the following details: basic information, CLBP evaluation, and psychological evaluation (healthy subjects only completed basic information and psychological evaluation).
In CLBP evaluation, a numeric rating scale (NRS, 0–10, where 0 indicated “no pain at all,” and 10 denoted “the worst imaginable pain”) was used to assess the maximum and average pain intensity (NRS1 and NRS2) of the patients who experienced CLBP in the past 3 days. It is a valid, reliable, has good test-rest reliability (intraclass correlation coefficient, ICC = 0.991), excellent responsiveness (area under the curve, AUC = 0.880), and is often preferred tool to measure the severity of pain (31, 32). The dysfunction related to CLBP was examined with the Roland-Morris questionnaire (RMDQ), which is frequently utilized to measure the specific functional status of the back (33). RMDQ includes 24 items scored as 0 or 1, where 1 indicates that an item is applicable to the subjects, and 0 denotes that an item is not applicable. The total score range is 0 (no disability) to 24 (the highest possible disability). It has good test-retest reliability (ICC = 0.855), responsiveness (AUC = 0.868), internal consistency, construct validity, and face and content validity (32, 34).
In psychological evaluation, all the subjects were examined with a self-rating anxiety scale (SAS) and a self-rating depression scale (SDS). These scales are used to quantify the anxiety and depression level of the subjects. Each scale has 20 items with a score of 1–4 (1 = never, 2 = often, 3 = sometimes, and 4 = always). The normalized score is equal to the total score (ranging from 20 to 80) multiplied by 1.25 (SAS: 20–44 = normal range, 45–59 = mild anxiety, 60–74 = moderate anxiety, 75–80 = severe anxiety; SDS: 20–49 = normal range, 50–59 = mild depression, 60–69 = moderate depression, 70–80 = severe depression) (35). Cronbach's coefficients of the Chinese version of the SAS and SDS used in this study are 0.931 and 0.784, respectively (36). The SAS is significantly correlated with the Taylor Manifest Anxiety Scale (r = 0.30), and the correlation between the SDS and the Beck Depression Inventory is 0.68 (37). Both scales have good internal consistency, reliability, and validity (36). The SAS and the SDS yield convincing results of anxiety and depression assessment, and they are widely applied to different areas, such as rehabilitation, psychiatry, and oncology (38, 39).
Procedure
In social interaction, people can automatically regulate interpersonal distance. With high validity and reliability, a stop-distance paradigm is frequently applied to measure the preferred interpersonal distance under various conditions (25, 40). At the beginning of a task, a subject and the experimenter faced each other at a distance of 3 m. Four conditions were set: two of them involved completing a task with an unfamiliar person of the same gender (the experimenter was the same gender as the subject), and the two other conditions were undertaken with an unfamiliar person of the opposite gender (the experimenter was the opposite gender as the subject).
Under the first condition, the unfamiliar experimenter (same gender) slowly walked toward the subject until he or she reached the distance, where the subject would normally maintain a stranger; this distance was denoted as the comfortable distance (CD1; Figure 1). Thereafter, the unfamiliar experimenter (same gender) continued to move toward the subject and stopped at the distance, where the subject felt uncomfortable; this distance was indicated as the uncomfortable distance (UD1; Figure 1). Afterward, the procedure was repeated, but the subject walked toward the unfamiliar experimenter (same gender) and stopped again at comfortable (CD3; Figure 1) and uncomfortable distances (UD3; Figure 1). The task was repeated, but an unfamiliar experimenter of the opposite gender was involved this time (comfortable distance: CD2 and CD4; uncomfortable distances: UD2 and UD4; Figure 1). Toe-to-toe distances were tested three times under each condition and recorded using a digital laser measurer (Bosch GLM 30C). The average of being approached by the same-gender experimenter and the opposite-gender experimenter and approaching them was taken as the outcome measure (41, 42). Different experimenters were randomly assigned under each condition to avoid familiarity effects (17).
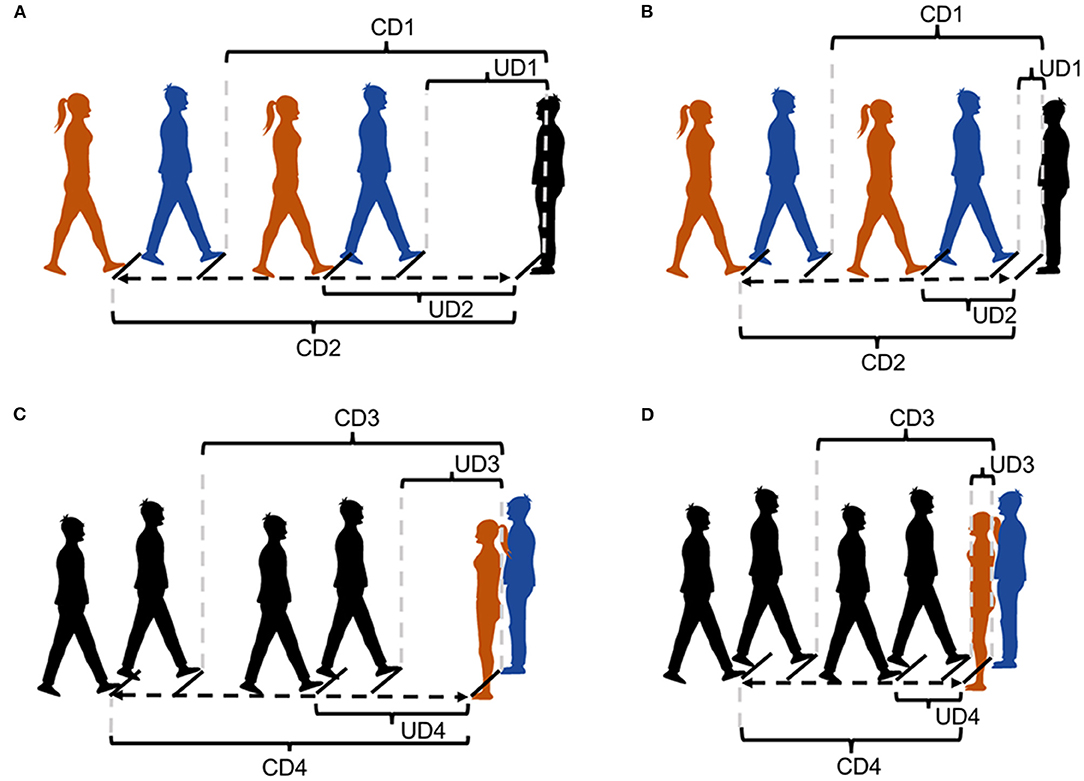
Figure 1. Stop-distance paradigm. (A) The interpersonal distance between participant with CLBP and experimenter under the condition of being approached. (B) The interpersonal distance between health control and experimenter under the condition of being approached. (C) The interpersonal distance between participant with CLBP and experimenter under the condition of active approach. (D) The interpersonal distance between health control and experimenter under the condition of active approach. Black figures: the participant. Blue figures: the experimenters (the same gender as the participant). Red figures: the experimenters (the opposite gender as the participant). CD1: The comfortable distance between the participant and the experimenter (same gender) under the condition of being approached. CD2: The comfortable distance between the participant and the experimenter (opposite gender) under the condition of being approached. UD1: The uncomfortable distance between the participant and the experimenter (same gender) under the condition of being approached. UD2: The uncomfortable distance between the participant and the experimenter (opposite gender) under the condition of being approached. CD3: The comfortable distance between the participant and the experimenter (same gender) under the condition of active approach. CD4: The comfortable distance between the participant and the experimenter (opposite gender) under the condition of active approach. UD3: The uncomfortable distance between the participant and the experimenter (same gender) under the condition of active approach. UD4: The uncomfortable distance between the participant and the experimenter (opposite gender) under the condition of active approach.
Statistical Analyses
Differences in demographical and clinical data between the two groups were explored with a chi-square test, an independent sample t-test, and a Wilcoxon rank-sum test. We performed a normality test on all data and normal transformation when necessary. The difference in the interpersonal distance under various conditions between the CLBP and control groups was analyzed through an independent sample t-test. Two-way ANOVA was performed to examine the significant effect of the Approach Direction (being approached or approaching) and Gender (same or opposite gender) on interpersonal distance based on adjusted analysis. Age, body weight, height, and BMI were included in adjusted analysis as baseline covariates. Further associations between interpersonal distance and different clinical indicators (SAS, SDS, NRS1, NRS2, and RMDQ) were tested by using the Pearson correlation test with Benjamini-Hochberg adjustment for multiple testing. Adjusted p < 0.05 was considered as statistical significance.
Results
Stop-Distance Paradigm
Being Approached by an Unfamiliar Experimenter
Under the Same Gender condition, the average CD1 between the subjects and an unfamiliar experimenter was 81.97 ± 25.25 cm in the CLBP group and 61.49 ± 16.11 cm in the control group, and they had average UD1 of 44.15 ± 16.77 and 32.01 ± 8.75 cm, respectively (Figures 1A,B). Under the Opposite Gender condition, the average CD2 was 94.17 ± 28.61 cm in the CLBP group and 71.44 ± 15.17 cm in the control group, and they had average UD2 of 53.69 ± 20.40 and 41.21 ± 9.29 cm, respectively (Figures 1A,B). When the subject was approached by the experimenter, the distance under all the conditions in the CLBP group significantly differed from that in the healthy control group with larger space distances (CD1: t = 3.350, p = 0.002; UD1: t = 3.251, p = 0.002; CD2: t = 3.496, p = 0.001; UD2: t = 3.208, p = 0.003; Figure 2A).
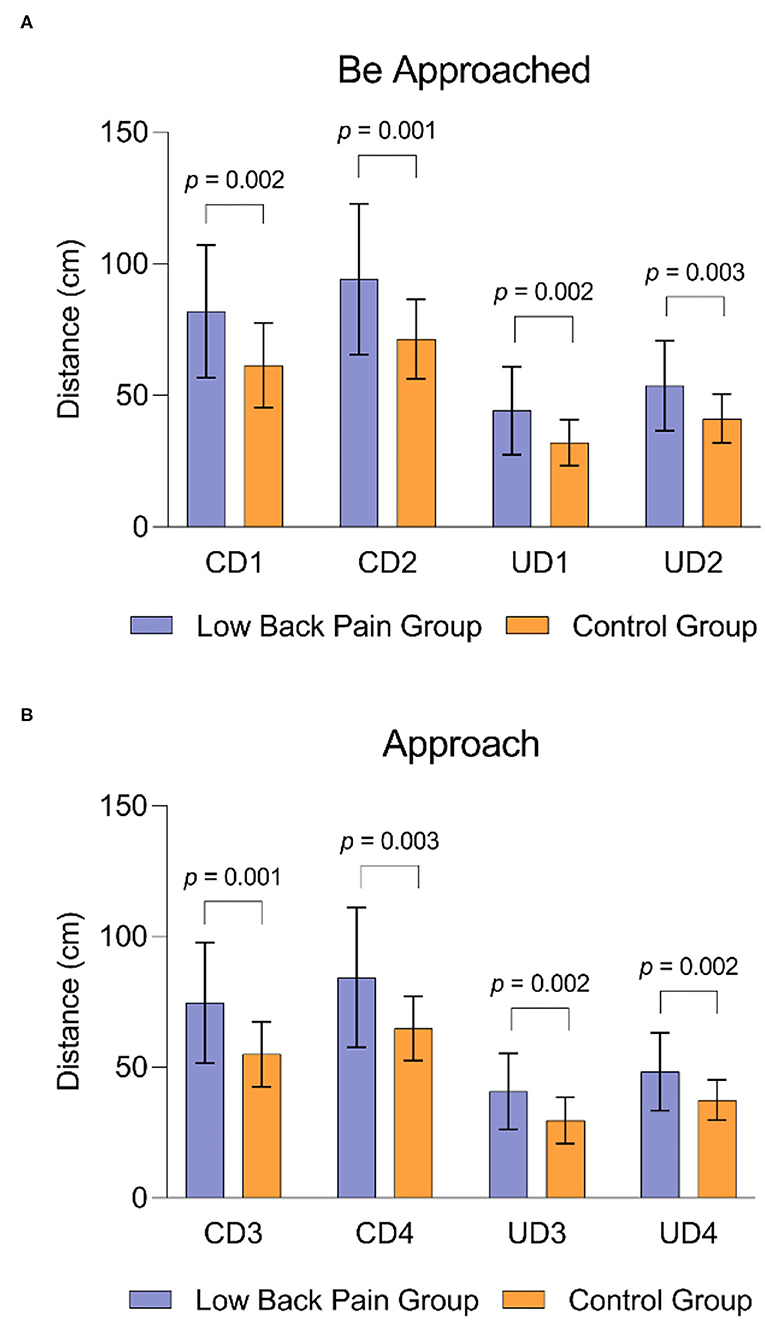
Figure 2. The difference in interpersonal distance across the CLBP and control group. (A) The difference in interpersonal distance across the CLBP and control group under the condition of being approached. (B) The difference in interpersonal distance across the CLBP and control group under the condition of active approach.
Approaching an Unfamiliar Experimenter
Under the Same Gender condition, the average CD3 between the subjects and an unfamiliar experimenter was 74.63 ± 23.09 cm in the CLBP group and 55.02 ± 12.40 cm in the control group, and they had average UD3 of 40.75 ± 14.51 and 29.68 ± 8.91 cm, respectively (Figures 1C,D). Under the Opposite Gender condition, the average CD4 was 84.34 ± 26.84 cm in the CLBP group and 64.86 ± 12.35 cm in the control group, and they had average UD4 of 48.31 ± 14.91 and 37.47 ± 7.71 cm, respectively (Figures 1C,D). When the subject approached the experimenter, the distance under all the conditions in the CLBP group significantly differed from that in the healthy control group with larger space distances (CD3: t = 3.734, p = 0.001; UD3: t = 3.258, p = 0.002; CD4: t = 3.229, p = 0.003; UD4: t = 3.216, p = 0.002; Figure 2B).
Factors Affecting Personal Space
Approach Direction or Gender
Comfortable Distance
The Approach Direction significantly affected the control group but not the CLBP group [F(1,93) = 5.187, p = 0.025; = 0.053; Table 2]. The result indicated that the subjects maintained a larger interpersonal distance when they were approached by the experimenter compared with that when they approached actively the experimenter. Gender also had a significant main effect [F(1,93) = 11.943, p = 0.001; = 0.114], as participants showed a greater distance with the experimenter of the opposite gender compared with that of the experimenter of the same gender in the healthy control group. However, no significant interaction between Approach Direction and Gender was observed [F(1,88) < 0.001, p = 0.991; < 0.001]. In addition, the Same- and Opposite-Gender subgroups significantly differed in terms of the comfortable distance when they were being approached or actively approaching the experimenter (Being Approached: t = −2.203, p = 0.033; Approaching: t = −2.756, p = 0.008). No significant difference in the distance of the Being Approach subgroup and the Approaching subgroup under the Same or Opposite Gender condition (Same Gender: t = 1.559, p = 0.126; Opposite Gender: t = 1.646, p = 0.167).
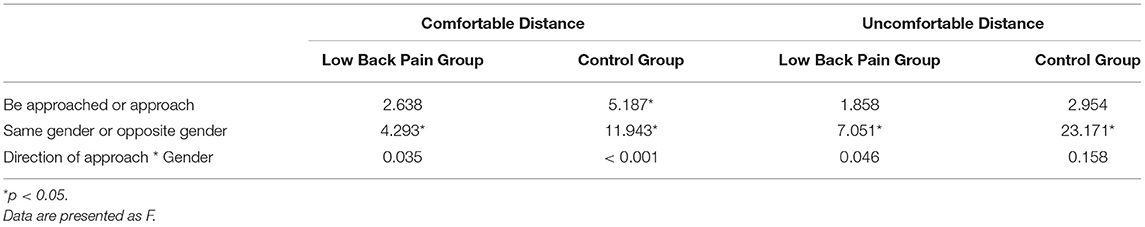
Table 2. The effect of the Approach Direction (being approached or approaching) and Gender (same or opposite gender) on interpersonal distance.
In the CLBP group, Gender showed a significant main effect [F(1,93) = 4.293, p = 0.041; = 0.044]. However, the Approach Direction had no significant main effect [F(1,93) = 2.638, p = 0.108; = 0.028], and no significant interaction was observed between the two factors [F(1,88) = 0.003, p = 0.960; < 0.001]. Statistical analysis revealed no significant difference between the Same- and Opposite-Gender subgroups or Being Approached and Approaching subgroups (Being Approached: t = −1.609, p = 0.114; Approaching: t = −1.375, p = 0.176; Same Gender: t = 1.068, p = 0.291; Opposite Gender: t = 1.280, p = 0.228).
Uncomfortable Distance
Gender had a significant main effect in the control and CLBP groups [control group: F(1,93) = 23.171, p < 0.001; = 0.199; CLBP group: F(1,93) = 7.051, p = 0.009; = 0.070; Table 2]. The result showed that the subject had a closer distance with the experimenter of the same gender than that of the opposite gender. However, Approach Direction had no significant main effect [control group: F(1,93) = 2.954, p = 0.089; = 0.031; CLBP group: F(1,93) = 1.858, p = 0.176; = 0.020], and the two factors also had no significant interaction [control group: F(1,88) = 0.019, p = 0.892; < 0.001; CLBP group: F(1,88) = 0.002, p = 0.962; < 0.001]. In the healthy control group, the Same- and Opposite-Gender subgroups significantly differed when they were being approached or actively approaching the experimenter (approached: t = −3.531, p = 0.001; approaching: t = −3.239, p = 0.002). The distance maintained by the Opposite-Gender subgroup was constantly larger than that maintained by the Same-Gender subgroup. The Being Approach subgroup and the Approaching subgroup did not significantly differ in terms of uncomfortable distance under the Same or Opposite Gender conditions (Same Gender: t = 0.914, p = 0.366; Opposite Gender: t = 1.517, p = 0.136). In the CLBP group, no significant difference was observed between the Same- and Opposite-Gender subgroups or the Being Approached and Approaching subgroups (Being approached: t = −2.117, p = 0.040; Approaching: t = −1.936, p = 0.059; Same Gender: t = 0.764, p = 0.449; Opposite Gender: t = 1.188, p = 0.241).
Clinical Variables
The results of the correlation analysis between clinical factors (SAS, SDS, NRS1, NRS2, and RMDQ) and interpersonal distance are shown in Figures 3–6.
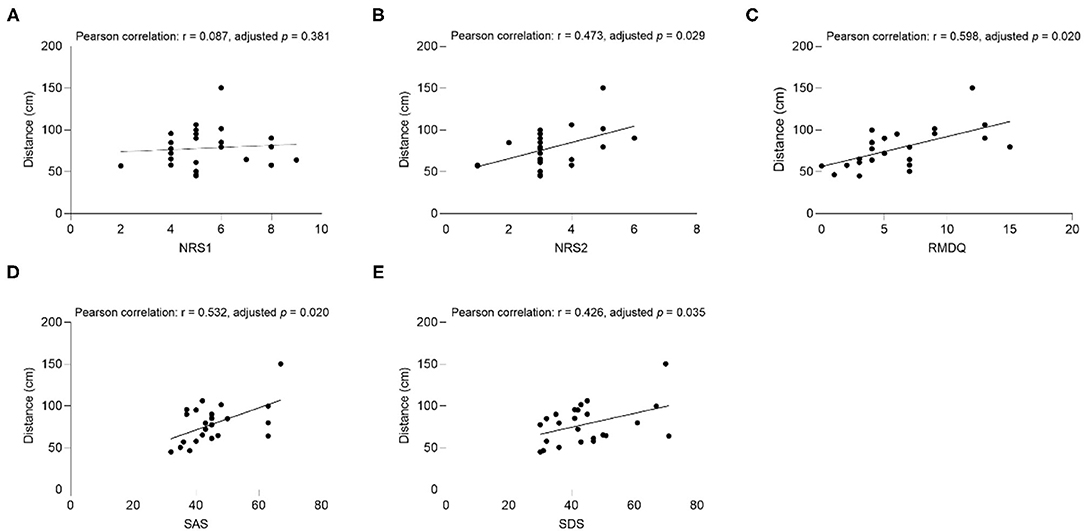
Figure 3. The correlation between comfortable distance and (A) NRS1, (B) NRS2, (C) RMDQ, (D) SAS, (E) SDS in CLBP group under the Same Gender condition. NRS1, the maximum pain intensity during the subjects experiencing low back pain; NRS2, the average pain intensity during the subjects experiencing low back pain; RMDQ, Roland-Morris questionnaire; SAS, self-rating anxiety scale; SDS, self-rating depression scale.
Comfortable Distance
In the CLBP group, NRS2 (Pearson correlation: r = 0.473, adjusted p = 0.029), RMDQ (Pearson correlation: r = 0.598, adjusted p = 0.020), SAS (Pearson correlation: r = 0.532, adjusted p = 0.020), SDS (Pearson correlation: r = 0.426, adjusted p = 0.035), and comfortable distance had significant positive associations when the subjects were the same gender as the experimenter (Figure 3). RMDQ (Pearson correlation: r = 0.534, adjusted p = 0.020), SAS (Pearson correlation: r = 0.467, p = 0.028), and distance had significant positive associations when the gender of the subjects and the experimenter were not the same (Figure 4). In the healthy control group, no clinical factors were significantly related to the interpersonal distance under various conditions.
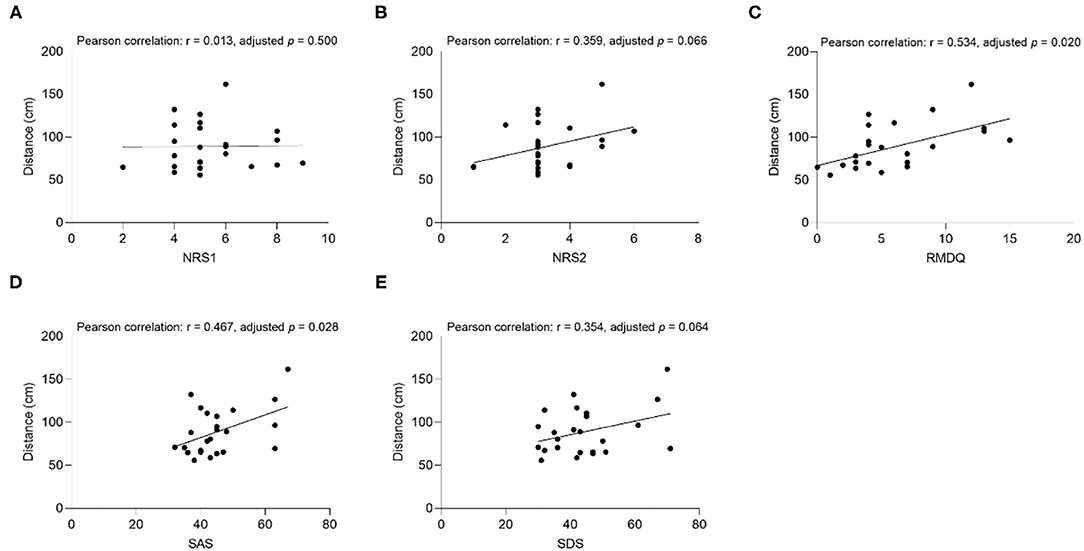
Figure 4. The correlation between comfortable distance and (A) NRS1, (B) NRS2, (C) RMDQ, (D) SAS, (E) SDS in CLBP group under the Opposite Gender condition. NRS1, the maximum pain intensity during the subjects experiencing low back pain; NRS2, the average pain intensity during the subjects experiencing low back pain; RMDQ, Roland-Morris questionnaire; SAS, self-rating anxiety scale; SDS, self-rating depression scale.
Uncomfortable Distance
The results showed that the uncomfortable distance had a significant positive correlation with RMDQ (Pearson correlation: r = 0.454, adjusted p = 0.026), SAS (Pearson correlation: r = 0.571, adjusted p = 0.020), and SDS (Pearson correlation: r = 0.532, adjusted p = 0.020) under the Same Gender condition of the CLBP group (Figure 5). The correlation of SAS (Pearson correlation: r = 0.570, adjusted p = 0.020), and SDS (Pearson correlation: r = 0.457, p = 0.027) under the Opposite Gender condition was significantly positive (Figure 6). In the healthy control group, all the clinical factors and the interpersonal distance were not significantly correlated under different conditions.
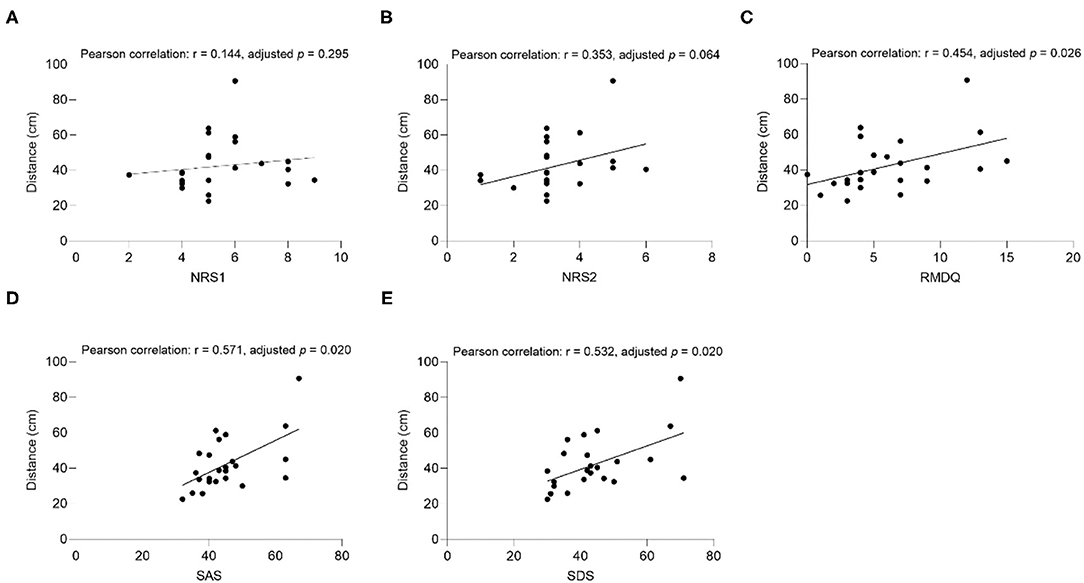
Figure 5. The correlation between uncomfortable distance and (A) NRS1, (B) NRS2, (C) RMDQ, (D) SAS, (E) SDS in CLBP group under the Same Gender condition. NRS1, the maximum pain intensity during the subjects experiencing low back pain; NRS2, the average pain intensity during the subjects experiencing low back pain; RMDQ, Roland-Morris questionnaire; SAS, self-rating anxiety scale; SDS, self-rating depression scale.
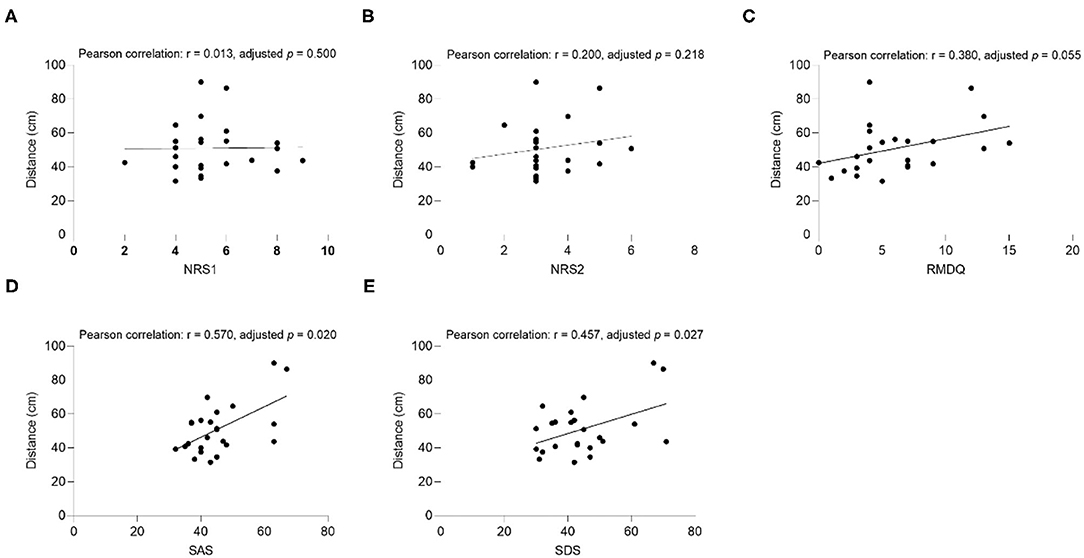
Figure 6. The correlation between uncomfortable distance and (A) NRS1, (B) NRS2, (C) RMDQ, (D) SAS, (E) SDS in CLBP group under the Opposite Gender condition. NRS, numerical rating scale; RMDQ, Roland-Morris questionnaire; SAS, self-rating anxiety scale; SDS: self-rating depression scale.
Discussion
The results revealed that the individuals with CLBP generally showed a greater personal space than the healthy controls. When approaching a stranger or when being approached, the patients kept a greater interpersonal distance from the stranger of the same gender or opposite gender. Meanwhile, the interpersonal distance between patients and the stranger of the same gender was shorter than that between patients and the stranger of the opposite gender. Furthermore, the higher the pain intensity, dysfunction, anxiety, and depression, the greater the interpersonal distance in patients with CLBP.
The Effect of CLBP on the Personal Space
The individuals with CLBP showed a significantly greater personal space than the healthy controls, which indicated that patients with CLBP consciously avoided further contact with others and expressed greater social withdrawal. This phenomenon has also been reported in patients suffering from other pain. For example, Lutzman et al. (43) found that single elderly people with physical pain felt a greater loneliness and showed a lower social integration than those without pain. Furthermore, Stout et al. (44) showed that women who experienced more intense and frequent pain during intercourse could suffer from more loneliness and depression. In the task of Cyberball social exclusion, participants who received endotoxin experienced worse social disconnection than participants who received the same volume of saline (45). These studies pointed out the relationship between physical pain and social withdrawal. One possible explanation for this phenomenon is that physical pain restricts individuals from participating in social activities and maintaining interpersonal relationships. Another one is that patients try to hide their pain by minimizing contact with the outside world, thereby producing social withdrawal and loneliness. To explain further, CLBP often negatively affects self-perception, which is patients are ashamed of difficulties in performing daily living activities and they are often misunderstood by others due to the absence of obvious signs or symptoms. Therefore, they cannot reasonably manage their social interactions (46). Furthermore, from the perspective of neural mechanisms, this phenomenon is probably due to the dependence of physical pain and social pain on a shared neural circuit (47–49). As an important area responsible for processing unpleasant and negative emotions related to social events or physical pain (48), the pregenual anterior cingulate cortex (pACC), for instance, is responsible for accepting physical pain regulation and gives a change in social pain. Similarly, the activation of the dorsal anterior cingulate cortex (dACC) decreases with the pain subsides, thereby reducing social pain (49).
In the stop-distance task, the gender played a vital role in personal space regulation in both groups, which suggested that the distance between individuals of the same gender was shorter than that between individuals of the opposite gender. The gender difference could be explained by neural mechanisms. The activation of the amygdala in children when encountering opposite-gender faces is significantly stronger than when interacting with same-gender faces (50). The amygdala is activated during close contact with others, thereby maintaining the minimum distance between people (40). This early development of gender differences has potential long-term effects that is individuals prefer to choose the same-gender playmates rather than the opposite-gender (50), which is a possible reason for participants showed shorter interpersonal distances when facing the same gender in this study.
Other Factors for Personal Space
Pain intensity, dysfunction, anxiety, and depression negatively affected the personal space regulation of patients with CLBP, which means the serious health problems are associated with increased interpersonal distance. From the perspective of pain intensity, individuals with CLBP who are afraid of pain likely develop catastrophic pain cognitions to avoid activities that might irritate more serious pain and harm. The presence of the avoidance behaviors subsequently leads to increased disability and depression, which in turn increases pain intensity (51). Pain and disability limit social participation in patients with CLBP. In terms of anxiety and depression, previous studies have reported that increased negative emotions can be accompanied by loneliness and social separation (17). People with high anxiety usually adopt an avoidant coping strategy in social interactions (52). Similarly, depressive symptoms could reduce people's social interaction time, and people with depressive symptoms tend to stay away from social networks and be isolated (53). Overall, individuals with anxiety, depression, or anxiety-depressive comorbidities show severe social dysfunction (54). As can be seen, the anxiety and depression symptoms in patients with CLBP may further reduce social interaction. There are some possible reasons why anxiety and depression negatively affect personal space. The first one is that the signal transduction of the brain reward system, which is closely related to the amygdala, in patients with anxiety or depression is impaired. It makes patients think that the rewards from social interaction are fewer and express social avoidance and withdrawal (54, 55). Another reason could be that the basolateral amygdala complex (BLA) exhibits hyperactivity in anxiety disorders and decreases social interaction by activating the BLA- medial prefrontal cortex projection (56).
As can be seen, the amygdala plays a key role in emotional disorders (e.g., depression, anxiety) and social behaviors. Additionally, considering its bilateral activation is correlated with the perceived pain intensity (57), the amygdala may be also a key brain area that regulates the social interaction in patients with CLBP and can be used to interpret the appearance of social withdrawal. It has been demonstrated that patients with CLBP have functional and structural changes in various brain regions, including the amygdala that belongs to the emotion-related circuitry (58–60). Resting-state functional magnetic resonance imaging (fMRI) has shown the increased activation of the amygdala in patients with CLBP (58, 61). Rodriguez-Raecke et al. (62) reported that the activation of the amygdala in patients with CLPB or depression increases during pain stimulation, and depression and pain seem to reinforce each other clinically. The pain and negative emotions in patients with CLBP could be connected through the amygdala, which is directly related to personal space regulation. Consequently, when CLBP or chronic pain occurs, the plasticity of the central nervous system changes, and the amygdala, a part of the cognitive-affective system of the “pain matrix,” is activated. Patients experience emotional disorders and atypical social behavior, which appears a larger personal space than that in healthy people.
Interestingly, the results showed that there is no association between maximum pain intensity during CLBP and personal space. One possible reason is that the maximum pain intensity during CLBP does not have a continuous and stable effect, which might indicate a limited effect of pain on the regulation of personal space in social communication. In the future, studies should explore whether immediate painful stimulation affects the size of personal space.
Limitations
Few studies have explored the effect of CLBP on personal space. This study provided new insight into the personal space management for patients with CLBP, which is practically significant. However, the limitations in the study should be considered. First, the sample size was relatively small. In future experiments, more subjects should be recruited to improve the credibility of experimental results. From the perspective of participant recruitment, a wider age range and more occupational types should be considered to more comprehensively show the results. Second, a stop-distance paradigm as an artificial task may fail to completely and accurately reflect social behavior in real life. As such, tasks that can more validly reflect the personal space during real social interactions should be established. Third, this study only investigated the changes in interpersonal distance between patients with CLBP and strangers. Further studies should examine whether the interpersonal distance between patients and familiar people will be different from healthy controls. Fourth, other factors that may affect social behavior and personal space, such as employment status, socioeconomic status, were not collected in the study. These factors could be considered and included in the next step of research.
Clinical Implications and Future Research
Our results revealed that the association of CLBP with social withdrawal is worthy to be focused on. This study offered a novel method for assessing the psychosocial status in patients with CLBP. Pain and disability are the most prominent symptoms in CLBP, which makes most patients seek medical attention. Psychosocial problems, which are often overlooked, play an important role in physical and mental health. As such, the psychosocial problems in patients with CLBP should be explored. Medical staff should consider potential social withdrawal and reduced social interactions. They should also formulate the corresponding psychosocial interventions to help patients smoothly reintegrate into society. Additionally, the effect and underlying neural mechanisms of pain and negative emotions on social withdrawal in patients should be examined. In the future, a larger sample size, more realistic social tasks, and more task models (such as those determining whether the interpersonal distance between patients with CLBP and familiar people will be different from healthy controls) will be needed to explore the effect of CLBP on psychosocial status.
Conclusion
People with CLBP show an atypical personal space behavior, indeed have a greater interpersonal distance to strangers and reduced social interactions. The increased anxiety, depression, average pain intensity, and dysfunction in CLBP are related to the greater personal space and more severe social withdrawal. The changes of personal space are one of the manifestations of social behavior. CLBP reduces the connection and interaction between individuals and society and produces social withdrawal and loneliness. In addition to alleviating pain and dysfunction in clinic, social and psychological problems in patients with CLBP during recovery should be explored to accurately identify the difficulties that need improvement. Further research can enhance our understanding of psychosocial changes in patients with CLBP and provide the evidence for the implementation of psychological rehabilitation.
Data Availability Statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding authors.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Committee of Shanghai University of Sport. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
L-MW, BW, and X-QW conceived and designed the study. L-MW, BW, C-CC, JW, and M-SP collected the data. L-MW and BW analyzed and interpreted the data. L-MW drafted the manuscript. BW, Z-JZ, and X-QW revised the manuscript for important intellectual content. All authors discussed the results, commented on the manuscript, and approved the final manuscript.
Funding
This work was supported by Fok Ying-Tong Education Foundation of China (161092), Scientific and Technological Research Program of the Shanghai Science and Technology Committee (19080503100), Shanghai Key Lab of Human Performance (Shanghai University of Sport) (11DZ2261100), Science and Technology Commission of Shanghai Municipality (21S31902400), and Project of Science Research of Traditional Chinese Medicine of Henan Province of China (2019ZY1028).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
CLBP, chronic low back pain; LBP, low back pain; BMI, body mass index; NRS, numerical rating scale; RMDQ, Roland-Morris questionnaire; SAS, self-rating anxiety scale; SDS, self-rating depression scale; AUC, area under the curve; ICC, intraclass correlation coefficient; pACC, pregenual anterior cingulate cortex; dACC, dorsal anterior cingulate cortex; fMRI, functional magnetic resonance imaging.
References
1. Dionne CE, Dunn KM, Croft PR, Nachemson AL, Buchbinder R, Walker BF, et al. A consensus approach toward the standardization of back pain definitions for use in prevalence studies. Spine (Phila Pa 1976). (2008) 33:95–103. doi: 10.1097/BRS.0b013e31815e7f94
2. Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, et al. What low back pain is and why we need to pay attention. Lancet. (2018) 391:2356–67. doi: 10.1016/S0140-6736(18)30480-X
3. da CMCL, Maher CG, Hancock MJ, McAuley JH, Herbert RD, Costa LO. The prognosis of acute and persistent low-back pain: a meta-analysis. CMAJ. (2012) 184:E613–24. doi: 10.1503/cmaj.111271
4. van Tulder M, Koes B, Bombardier C. Low back pain. Best Pract Res Clin Rheumatol. (2002) 16:761–75. doi: 10.1053/berh.2002.0267
5. Balagué F, Mannion AF, Pellisé F, Cedraschi C. Non-specific low back pain. Lancet. (2012) 379:482–91. doi: 10.1016/S0140-6736(11)60610-7
6. Last AR, Hulbert K. Chronic low back pain: evaluation and management. Am Fam Physician. (2009) 79:1067–74.
7. Manchikanti L, Singh V, Datta S, Cohen SP, Hirsch JA. Comprehensive review of epidemiology, scope, and impact of spinal pain. Pain Physician. (2009) 12:E35–70. doi: 10.36076/ppj.2009/12/E35
8. Berman BM, Langevin HM, Witt CM, Dubner R. Acupuncture for chronic low back pain. N Engl J Med. (2010) 363:454–61. doi: 10.1056/NEJMct0806114
9. Shanthanna H, Gilron I, Rajarathinam M, AlAmri R, Kamath S, Thabane L, et al. Benefits and safety of gabapentinoids in chronic low back pain: a systematic review and meta-analysis of randomized controlled trials. PLoS Med. (2017) 14:e1002369. doi: 10.1371/journal.pmed.1002369
10. Bushnell DM, Blum SI, Liedgens H, Martin ML, Freynhagen R, Wallace M, et al. Mixed-methods development of a new patient-reported outcome instrument for chronic low back pain: part 2-The Patient Assessment for Low Back Pain-Impacts (PAL-I). Pain. (2018) 159:2066–75. doi: 10.1097/j.pain.0000000000001309
11. Forgeron PA, King S, Stinson JN, McGrath PJ, MacDonald AJ, Chambers CT. Social functioning and peer relationships in children and adolescents with chronic pain: a systematic review. Pain Res Manag. (2010) 15:27–41. doi: 10.1155/2010/820407
12. Leonard MT, Cano A, Johansen AB. Chronic pain in a couples context: a review and integration of theoretical models and empirical evidence. J Pain. (2006) 7:377–90. doi: 10.1016/j.jpain.2006.01.442
13. Dionne CE. Psychological distress confirmed as predictor of long-term back-related functional limitations in primary care settings. J Clin Epidemiol. (2005) 58:714–8. doi: 10.1016/j.jclinepi.2004.12.005
14. Krein SL, Metreger T, Kadri R, Hughes M, Kerr EA, Piette JD, et al. Veterans walk to beat back pain: study rationale, design and protocol of a randomized trial of a pedometer-based internet mediated intervention for patients with chronic low back pain. BMC Musculoskelet Disord. (2010) 11:205. doi: 10.1186/1471-2474-11-205
15. Yokota J, Fukutani N, Nin K, Yamanaka H, Yasuda M, Tashiro Y, et al. Association of low back pain with presenteeism in hospital nursing staff. J Occup Health. (2019) 61:219–26. doi: 10.1002/1348-9585.12030
16. Hawkley LC, Cacioppo JT. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med. (2010) 40:218–27. doi: 10.1007/s12160-010-9210-8
17. Ben Simon E, Walker MP. Sleep loss causes social withdrawal and loneliness. Nat Commun. (2018) 9:3146. doi: 10.1038/s41467-018-05377-0
18. Williams LE, Bargh JA. Keeping one's distance: the influence of spatial distance cues on affect and evaluation. Psychol Sci. (2008) 19:302–8. doi: 10.1111/j.1467-9280.2008.02084.x
19. Pressman SD, Cohen S, Miller GE, Barkin A, Rabin BS, Treanor JJ. Loneliness, social network size, and immune response to influenza vaccination in college freshmen. Health Psychol. (2005) 24:297–306. doi: 10.1037/0278-6133.24.3.297
20. Barger SD, Messerli-Bürgy N, Barth J. Social relationship correlates of major depressive disorder and depressive symptoms in Switzerland: nationally representative cross sectional study. BMC Public Health. (2014) 14:273. doi: 10.1186/1471-2458-14-273
21. Cacioppo S, Capitanio JP, Cacioppo JT. Toward a neurology of loneliness. Psychol Bull. (2014) 140:1464–504. doi: 10.1037/a0037618
22. Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. (2010) 7:e1000316. doi: 10.1371/journal.pmed.1000316
23. Perry A, Rubinsten O, Peled L, Shamay-Tsoory SG. Don't stand so close to me: a behavioral and ERP study of preferred interpersonal distance. Neuroimage. (2013) 83:761–9. doi: 10.1016/j.neuroimage.2013.07.042
24. Gessaroli E, Santelli E, di Pellegrino G, Frassinetti F. Personal space regulation in childhood autism spectrum disorders. PLoS One. (2013) 8:e74959. doi: 10.1371/journal.pone.0074959
25. Lough E, Flynn E, Riby DM. personal space regulation in williams syndrome: the effect of familiarity. J Autism Dev Disord. (2016) 46:3207–15. doi: 10.1007/s10803-016-2864-8
26. Rubinsten O, Korem N, Perry A, Goldberg M, Shamay-Tsoory S. Different neural activations for an approaching friend versus stranger: linking personal space to numerical cognition. Brain Behav. (2020) 10:e01613. doi: 10.1002/brb3.1613
27. Ferrari S, Chiarotto A, Pellizzer M, Vanti C, Monticone M. Pain self-efficacy and fear of movement are similarly associated with pain intensity and disability in Italian patients with chronic low back pain. Pain Pract. (2016) 16:1040–7. doi: 10.1111/papr.12397
28. Oliveira DS, Vélia Ferreira Mendonça L, Sofia Monteiro Sampaio R, Manuel Pereira Dias de Castro-Lopes J, Ribeiro de Azevedo LF. The impact of anxiety and depression on the outcomes of chronic low back pain multidisciplinary pain management-a multicenter prospective cohort study in pain clinics with one-year follow-up. Pain Med. (2019) 20:736–46. doi: 10.1093/pm/pny128
29. Wu B, Zhou L, Chen C, Wang J, Hu L, Wang X. Effects of exercise induced hypoalgesia and its neural mechanisms. Med Sci Sports Exerc. (2021). doi: 10.1249/MSS.0000000000002781 [Epub ahead of print].
30. Zheng K, Chen C, Yang S, Wang X. Aerobic exercise attenuates pain sensitivity: an event-related potential study. Front Neurosci. (2021) 15:1217. doi: 10.3389/fnins.2021.735470
31. Bendinger T, Plunkett N. Measurement in pain medicine. BJA Educ. (2016) 16:310–5. doi: 10.1093/bjaed/mkw014
32. Yao M, Xu B-P, Li Z-J, Zhu S, Tian Z-R, Li D-H, et al. A comparison between the low back pain scales for patients with lumbar disc herniation: validity, reliability, and responsiveness. Health Qual Life Outcomes. (2020) 18:175–175. doi: 10.1186/s12955-020-01403-2
33. Chiarotto A, Maxwell LJ, Terwee CB, Wells GA, Tugwell P, Ostelo RW. Roland-Morris disability questionnaire and Oswestry disability index: which has better measurement properties for measuring physical functioning in nonspecific low back pain? Systematic Review and Meta-Analysis. Phys Ther. (2016) 96:1620–37. doi: 10.2522/ptj.20150420
34. Igwesi-Chidobe CN, Obiekwe C, Sorinola IO, Godfrey EL. Assessing self-reported disability in a low-literate population with chronic low back pain: cross-cultural adaptation and psychometric testing of Igbo Roland Morris disability questionnaire. Disabil Rehabil. (2019) 41:948–57. doi: 10.1080/09638288.2017.1416185
35. Yu S, Zhao Q, Wu P, Qin M, Huang H, Cui H, et al. Effect of anxiety and depression on the recurrence of paroxysmal atrial fibrillation after circumferential pulmonary vein ablation. J Cardiovasc Electrophysiol. (2012) 23(Suppl. 1):S17–23. doi: 10.1111/j.1540-8167.2012.02436.x
36. Yang M, He P, Xu X, Li D, Wang J, Wang Y, et al. Disrupted rhythms of life, work and entertainment and their associations with psychological impacts under the stress of the COVID-19 pandemic: a survey in 5854 Chinese people with different sociodemographic backgrounds. PLoS ONE. (2021) 16:e0250770. doi: 10.1371/journal.pone.0250770
37. Dunstan DA, Scott N, Todd AK. Screening for anxiety and depression: reassessing the utility of the Zung scales. BMC Psychiatry. (2017) 17:329–329. doi: 10.1186/s12888-017-1489-6
38. Kirkby R, Al Saif A, el-din Mohamed G. Validation of an Arabic translation of the Zung self-rating depression scale. Ann Saudi Med. (2005) 25:205–8. doi: 10.5144/0256-4947.2005.205
39. Yue T, Li Q, Wang R, Liu Z, Guo M, Bai F, et al. Comparison of Hospital Anxiety and Depression Scale (HADS) and Zung Self-Rating Anxiety/Depression Scale (SAS/SDS) in evaluating anxiety and depression in patients with psoriatic arthritis. Dermatology. (2020) 236:170–8. doi: 10.1159/000498848
40. Kennedy DP, Gläscher J, Tyszka JM, Adolphs R. Personal space regulation by the human amygdala. Nat Neurosci. (2009) 12:1226–7. doi: 10.1038/nn.2381
41. Holt DJ, Cassidy BS, Yue X, Rauch SL, Boeke EA, Nasr S, et al. Neural correlates of personal space intrusion. J Neurosci. (2014) 34:4123–34. doi: 10.1523/JNEUROSCI.0686-13.2014
42. Perry A, Nichiporuk N, Knight RT. Where does one stand: a biological account of preferred interpersonal distance. Soc Cogn Affect Neurosci. (2016) 11:317–26. doi: 10.1093/scan/nsv115
43. Lutzman M, Sommerfeld E, Ben-David S. (2020). Loneliness and social integration as mediators between physical pain and suicidal ideation among elderly men. Int Psychogeriatr. (2005) 33:453–59. doi: 10.1017/S104161022000112X
44. Stout ME, Meints SM, Hirsh AT. Loneliness mediates the relationship between pain during intercourse and depressive symptoms among young women. Arch Sex Behav. (2018) 47:1687–96. doi: 10.1007/s10508-017-1138-7
45. Eisenberger NI, Inagaki TK, Mashal NM, Irwin MR. Inflammation and social experience: an inflammatory challenge induces feelings of social disconnection in addition to depressed mood. Brain Behav Immun. (2010) 24:558–63. doi: 10.1016/j.bbi.2009.12.009
46. Bailly F, Foltz V, Rozenberg S, Fautrel B, Gossec L. The impact of chronic low back pain is partly related to loss of social role: A qualitative study. Joint Bone Spine. (2015) 82:437–41. doi: 10.1016/j.jbspin.2015.02.019
47. Eisenberger NI, Lieberman MD, Williams KD. Does rejection hurt? An FMRI study of social exclusion. Science. (2003) 302:290–2. doi: 10.1126/science.1089134
48. Xu X, Zuo X, Wang X, Han S. Do you feel my pain? Racial group membership modulates empathic neural responses. J Neurosci. (2009) 29:8525–9. doi: 10.1523/JNEUROSCI.2418-09.2009
49. Zhang M, Zhang Y, Kong Y. Interaction between social pain and physical pain. Brain Sci Adv. (2019) 5:265–73. doi: 10.26599/BSA.2019.9050023
50. Telzer EH, Flannery J, Humphreys KL, Goff B, Gabard-Durman L, Gee DG, et al. “The cooties effect”: amygdala reactivity to opposite- versus same-sex faces declines from childhood to adolescence. J Cogn Neurosci. (2015) 27:1685–96. doi: 10.1162/jocn_a_00813
51. Bunzli S, Smith A, Schütze R, Lin I, O'Sullivan P. making sense of low back pain and pain-related fear. J Orthop Sports Phys Ther. (2017) 47:628–36. doi: 10.2519/jospt.2017.7434
52. Raffety BD, Smith RE, Ptacek JT. Facilitating and debilitating trait anxiety, situational anxiety, and coping with an anticipated stressor: a process analysis. J Pers Soc Psychol. (1997) 72:892–906. doi: 10.1037/0022-3514.72.4.892
53. Elmer T, Stadtfeld C. Depressive symptoms are associated with social isolation in face-to-face interaction networks. Sci Rep. (2020) 10:1444–1444. doi: 10.1038/s41598-020-58297-9
54. Saris IMJ, Aghajani M, van der Werff SJA, van der Wee NJA, Penninx BWJH. Social functioning in patients with depressive and anxiety disorders. Acta Psychiatr Scand. (2017) 136:352–61. doi: 10.1111/acps.12774
55. Germine LT, Garrido L, Bruce L, Hooker C. Social anhedonia is associated with neural abnormalities during face emotion processing. Neuroimage. (2011) 58:935–45. doi: 10.1016/j.neuroimage.2011.06.059
56. Felix-Ortiz AC, Burgos-Robles A, Bhagat ND, Leppla CA, Tye KM. Bidirectional modulation of anxiety-related and social behaviors by amygdala projections to the medial prefrontal cortex. Neuroscience. (2016) 321:197–209. doi: 10.1016/j.neuroscience.2015.07.041
57. Bornhövd K, Quante M, Glauche V, Bromm B, Weiller C, Büchel C. Painful stimuli evoke different stimulus-response functions in the amygdala, prefrontal, insula and somatosensory cortex: a single-trial fMRI study. Brain. (2002) 125(Pt 6):1326–36. doi: 10.1093/brain/awf137
58. Hashmi JA, Baliki MN, Huang L, Baria AT, Torbey S, Hermann KM, et al. Shape shifting pain: chronification of back pain shifts brain representation from nociceptive to emotional circuits. Brain. (2013) 136(Pt 9):2751–68. doi: 10.1093/brain/awt211
59. Kregel J, Meeus M, Malfliet A, Dolphens M, Danneels L, Nijs J, et al. Structural and functional brain abnormalities in chronic low back pain: a systematic review. Semin Arthritis Rheum. (2015) 45:229–37. doi: 10.1016/j.semarthrit.2015.05.002
60. Zhang B, Jung M, Tu Y, Gollub R, Lang C, Ortiz A, et al. Identifying brain regions associated with the neuropathology of chronic low back pain: a resting-state amplitude of low-frequency fluctuation study. Br J Anaesth. (2019) 123:e303–11. doi: 10.1016/j.bja.2019.02.021
61. Baliki MN, Geha PY, Apkarian AV, Chialvo DR. Beyond feeling: chronic pain hurts the brain, disrupting the default-mode network dynamics. J Neurosci. (2008) 28:1398–403. doi: 10.1523/JNEUROSCI.4123-07.2008
Keywords: interpersonal distance, personal space, low back pain, stop-distance, social behavior
Citation: Weng L-M, Wu B, Chen C-C, Wang J, Peng M-S, Zhang Z-J and Wang X-Q (2021) Association of Chronic Low Back Pain With Personal Space Regulation. Front. Psychiatry 12:719271. doi: 10.3389/fpsyt.2021.719271
Received: 23 June 2021; Accepted: 24 November 2021;
Published: 15 December 2021.
Edited by:
Susanne Fischer, University of Zurich, SwitzerlandReviewed by:
Francesco Monaco, Azienda Sanitaria Locale Salerno, ItalyMohsen Khosravi, Zahedan University of Medical Sciences, Iran
Copyright © 2021 Weng, Wu, Chen, Wang, Peng, Zhang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhi-Jie Zhang, c3BvcnRzcHRAMTYzLmNvbQ==; Xue-Qiang Wang, cWlhbmc4OTdAMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Lin-Man Weng
Lin-Man Weng Bao Wu1†
Bao Wu1† Chang-Cheng Chen
Chang-Cheng Chen Meng-Si Peng
Meng-Si Peng Zhi-Jie Zhang
Zhi-Jie Zhang Xue-Qiang Wang
Xue-Qiang Wang