
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 18 October 2021
Sec. Public Mental Health
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.676493
This article is part of the Research Topic Sport and Psychosocial Health/Well-being after the COVID-19 Lockdown View all 11 articles
 Riyo Ueda1,2*
Riyo Ueda1,2* Takashi Okada1
Takashi Okada1 Yosuke Kita3,4
Yosuke Kita3,4 Yuri Ozawa2
Yuri Ozawa2 Hisami Inoue2
Hisami Inoue2 Mutsuki Shioda2
Mutsuki Shioda2 Yoshimi Kono2
Yoshimi Kono2 Chika Kono2
Chika Kono2 Yukiko Nakamura2
Yukiko Nakamura2 Kaoru Amemiya2
Kaoru Amemiya2 Ai Ito2
Ai Ito2 Nobuko Sugiura2
Nobuko Sugiura2 Yuichiro Matsuoka2
Yuichiro Matsuoka2 Chinami Kaiga2
Chinami Kaiga2 Masaya Kubota2
Masaya Kubota2 Hiroshi Ozawa2
Hiroshi Ozawa2Background: This study seeks to ascertain how the COVID-19 stay-at-home period has affected the quality of life (QOL) of children with neurodevelopmental disorders (NDDs) who had experienced sleep schedules alteration and clarify what psychological status predicted low QOL in children with and without altered sleep patterns.
Materials and Methods: Study participants were 86 children between 8 and 17 years of age (mean age, 11.7 years; 70 boys, 16 girls; mean intellectual quotient, 83.6). QOL was evaluated using the self-assessment KINDLR. Participants answered questions regarding depression and anxiety on a visual analog scale (VAS) for temporary mood. Their parents answered questionnaires regarding their maladaptive behaviors and differences in sleep patterns before and during the COVID-19 pandemic. The student's t-test was performed to examine the presence or absence of sleep changes in the children, which affected QOL, temporary mood, and maladaptive behaviors. Multiple or simple linear regression analyses were also performed to identify the psychogenic factors that significantly affected decreased QOL for each group with and without changes in sleep schedule.
Results: During the COVID-19 stay-at-home period, 46.5% of participants experienced changes in sleep patterns. These changes were associated with decreased QOL as well as internalized symptoms. The decreased QOL of children with sleep patterns changed was predicted by a high level of depression. In addition, low QOL in children with unchanged sleep patterns was predicted by a high level of depression and low current mood status.
Conclusions: Almost half of the participants experienced a poor sleep schedule during the stay-at-home period. These alterations in sleep patterns were associated with a low QOL. The QOL of children with a stable life schedule was affected not only by depressive tendencies but also temporary moods. Therefore, they need to live a fulfilling life to maintain their QOL. However, the QOL of children with poor sleep patterns was affected only by depressive tendencies. Hence, clinicians need to ensure that children with NDDs are well-diagnosed with depression and treated for sleep problems.
The 2019 coronavirus disease (COVID-19) pandemic has profoundly altered the way people live and work worldwide. In particular, the suspension of in-person education, extracurriculars, social activities, and routine healthcare for children severely threatens their physical and mental well-being.
In Japan, an emergency declaration was issued by the Prime Minister on April 7, 2020. Citizens were mandated to stay at home and refrain from outdoor activities until May 25, 2020. School-age children had been sent home even earlier, on March 2, 2020. Similar to caregivers around the world, Japanese parents too faced questions about how to best support their children under these conditions (1, 2).
Neurodevelopmental disorders (NDDs) are a group of conditions that produce developmental impairment in personal, social, and academic functioning from the developmental period, including genetic syndromes, metabolic diseases, cerebral palsy, psychomotor delay, etc. (3). It has been warned since the beginning of the COVID-19 pandemic that children with NDDs are more likely to experience mental and physical difficulties during a disaster in comparison with typically developing children (TDC) because of their inability to adapt to unpredictable changes around them and alterations to their routines (1, 4, 5). In the Australian study, the lifestyle habits of children with NDDs worsened, especially in terms of spending more time watching TV and digital media, getting less exercise, and having a poor diet (6). Furthermore, it was revealed in several studies that both internalizing and externalizing symptoms in children with NDDs and their comorbid mental health symptoms were worse than before the COVID-19 outbreak (1, 6). In addition, one of the severe problems for caregivers was the increased psychological and social burden of parenting children (7–10). The suspension of daily rehabilitation services and the lack of alternative recreational opportunities leave these caregivers alone caring for their children, with increased childcare burden and stressors, such as lack of access to needed therapies, medical supplies, and nursing care (7–10). The concerns for their child were significantly associated with the caregivers' stress, depressive and anxious symptoms (9). Namely, in recent years, the correlation between the social status of children with NDDs and the psychological status of their parents as well as the worsening of children's psychological behaviors during the COVID-19 pandemic has been revealed, emphasizing the importance of appropriate assessment and alternative intervention for children with NDDs as one of the global public health priorities (1, 6–9, 11).
Among the many problems of children with NDDs during the COVID-19 pandemic, deterioration of sleep schedules was one of the most significant problems. Children with NDDs are prone to sleep problems, even under normal circumstances. Sleep dysfunction for children with NDDs was a common and underlying problem associated with multiple factors, including biological and genetic abnormalities (12–14). Previous studies have shown that sleep problems affect the mental problems of children with the attention-deficit hyperactive disorder (ADHD) and autism spectrum disorder (ASD) (15–17). Some neurological and psychological experts predicted sleep problems in children with NDDs, especially during the COVID-19 pandemic (4). Therefore, it is significant to identify changes in sleep patterns during the COVID-19 stay-at-home period and related factors.
Furthermore, improving the subjective indicator of children's well-being is one of the most important goals in terms of supporting children. Quality of life (QOL) describes an individual's subjective perception of their position in life, as evidenced by their physical, psychological, and social functioning (18).
In a previous study, we asked parents to respond to the questionnaire survey on changes in children's QOL and lifestyle during the COVID-19 stay-at-home period. We found that changes in children's sleep schedules were associated with reduced QOL, and decreased maladaptive behavior with a maintained QOL (19). Thus, our former study indicated the importance of adjusting the sleep schedule to maintain the QOL of children. However, many previous studies have shown that the results of parental proxy- and children's self-reports do not always match (20–23). Therefore, it is prudent to analyze the results of the children's assessment of their mental state and QOL and to clarify their detailed characteristics.
The purpose of this study was to determine, using self-assessments, how the QOL of school-age children with NDDs during the COVID-19 pandemic has been affected by changes in the sleep schedules and the psychological status that predicted low QOL in children with and without altered sleep patterns. Clarifying the relationship between children's sleep problems and QOL can help reveal focus areas for child care and its support.
We recruited 86 children who were patients at the Shimada Ryoiku Center Hachioji in May 2020. The center is a regional core outpatient clinic where children receive medical examinations, rehabilitation, and psychotherapy. Hachioji is located in the western suburbs of Tokyo. It is a commuter town with a population of 580,000 (population density 3,093/km2). Nineteen persons were infected with COVID-19 in Hachioji City (a 6.8% positivity rate in polymerase chain reaction examination for COVID-19) in May 2020.
The inclusion criteria for participants were children with NDDs, including ADHD, ASD, specific learning disorders (SLD), tic disorders, or neurodevelopmental disorders classified by DSM-5. All diagnoses were reviewed by two board-certified pediatricians, including at least one board-certified pediatric neurologist. The children were between 8 and 17 years of age, referencing the target age of the questionnaires. The exclusion criterion was children with moderate or profound intellectual disabilities through prior testing full scale intellectual quotient (FSIQ) score from the Wechsler Intelligence Scale for Children, 3rd edition or 4th edition.
In addition, the center's dedicated staff explained the study to all participants who met the above criteria while maintaining social distance in a well-ventilated large room. All parents agreed to the participation and provided written informed consent, as did the children. We collected the questionnaire from all the children who provided their informed consent.
No one refused to participate. The studies involving human participants were reviewed and approved by the Institutional Review Board of the Shimada Ryoiku Center Hachioji (Shimahachi-2001). The participants and their parents provided their written informed consent to participate in this study.
The children were asked to self-administer the following questionnaires to assess their clinical status: Kidd-KINDLR (8–13 years) or Kiddo-KINDL R (14–17 years) (24, 25), the Depression Self-Rating Scale for Children (DSRS-C) (26), the Spence Children's Anxiety Scale (SCAS) (26, 27), and a visual analog scale (VAS) for temporary mood status in terms of percentages of the best imaginable state (28, 29). The parents assessed the maladaptive behaviors of their children using the Child Behavior Checklist (CBCL) (30). They also answered whether their children were going to bed or waking up later during the COVID-19 stay-at-home period than before.
The KINDLR items were rated on a five-point Likert scale, and the mean scores for each subscale and total items were calculated and converted to a 0–100 scale. The average values in the Kiddo-KINDLR of four subscales (physical well-being, emotional well-being, self-esteem, and family), excluding social contact and school sub-scales, were calculated to evaluate the children's QOL. Higher KINDLR scores indicate a better QOL.
Furthermore, VAS includes a graph scale on a horizontal line with endpoint 0 (the worst mood status imaginable, the picture of a crying face), mid-point 50 (intermediate mood status, the picture of a neutral face), and opposite endpoint 100 (the best mood status imaginable, the picture of a smiling face). The face scale was added to VAS to increase non-verbal explanations for children with different verbal abilities (31). After being instructed on VAS by a pediatrician, participants were asked to mark across the line on a point from (inclusive) 0 to 100, which best describes their current mood state. Higher VAS scores were associated with better mood scores and vice versa, while scores of the other questionnaires showed better symptoms at lower scores.
Statistical analysis was conducted using the JMP software, version 9.0.3 (SAS Institute Inc., Cary, NC, USA). Students t-test was performed to examine the presence or absence of sleep changes in the children, thereby affecting their QOL (KINDLR), VAS, FSIQ, externalized index, and internalized index of the CBCL. Pearson's χ2-test was used to investigate the proportional differences of the children with sleep changes between presence or absence of ADHD, ASD, and SLD, respectively. We applied a stepwise multiple or simple linear regression analysis to QOL with selective pairs to identify the psychogenic factors for each group, with and without a sleep schedule change. We began with a model that included all of the psychogenic available explanatory variables: SCAS score, DSCR-C score, externalized index and internalized index of the CBCL, and VAS score; we subsequently dropped insignificant variables based on the Akaike information criterion and the Bayesian information criterion. Significance was set at P < 0.05.
Table 1 shows the demographic parameters of the study participants. We surveyed their background and sleep schedules and assessed their QOL and mental health. There were 46 (53.5%) children with unchanged sleep schedules and 40 (46.5%) with changed sleep schedules (26 children with later bedtimes, 13 children with later bedtimes and later waking times, and one child with a later waking time than before the COVID-19 pandemic) (Table 1). None of the children took hypnotics and/or were newly diagnosed with a sleep disorder during the COVID-19 stay-at-home period.
Table 2 shows the results of the questionnaires. Among participants, 36 children (41.9%) scored above the CBCL internalized index cut-off of ≥70 points for the clinical range, and 26 children (30.2%) scored above the CBCL externalizing score cut-off of ≥70 points for the clinical range. Of the participants, 19 (22.1%) scored above the DSCR-C cut-off of ≥16 points, and another 19 (22.1%) scored above the SCAS cut-off of ≥42 points (27). The median QOL score for children was 71.2 (out of 100.0) on the KINDLR questionnaire. The median score of temporary mood for children was 55.8 out of 100.0 points on the VAS scale.
Table 3 shows the relationship between changes in sleep schedules and QOL in children during the COVID-19 stay-at-home period (deterioration = 40; unchanged = 46). Changes in sleep schedules were associated with decreased QOL and were also associated with the internalized index of CBCL. Changed sleep schedules were not associated with the externalized index and FSIQ. There was no relationship between sleep schedules and NDDs (ADHD, ASD, and SLD).
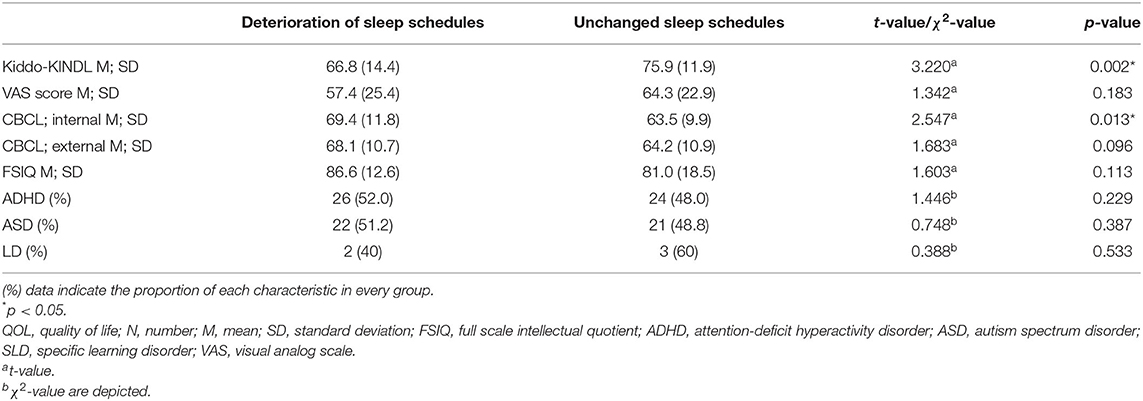
Table 3. Relationship between changes in sleep schedules and QOL changes in children during the COVID-19 stay-at-home period.
Table 4 shows the psychological factors that significantly predicted the QOL of children. Stepwise multiple regression analysis for children with changed sleep schedules showed that higher DSCR-C scores were associated with lower KINDLR scores. In children with unchanged sleep schedules, higher DSCR-C scores, and lower VAS scores were associated with lower KINDLR scores.
To our knowledge, this was the first study to reveal the relationship between changed sleep patterns in children with NDDs and their QOL during the COVID-19 stay-at-home period, based on the results of self-assessment by children. Changed sleep patterns were associated with decreased QOL and internalized symptoms of children with NDDs. The decreased QOL of children with changed sleep patterns was predicted by high levels of depression. In addition, low QOL in children with unchanged sleep patterns was predicted by high levels of depression and low current mood status.
Results indicate that changed sleep patterns were associated with decreased QOL in our previous study. In previous studies, children with ADHD and ASD were prone to sleep problems, affecting their QOL, even when they were not facing a crisis (15–17). A Turkish study during the COVID-19 pandemic indicated that severe sleep disorders led to highly increased ASD symptoms (32). In our previous study, QOL of children in parent proxy-reports also decreased with changes in sleep during the COVID-19 stay-at-home period (19). Despite a weak correlation of the same domain in both reports in a previous study (20), the similarity of the results in self-report and proxy-report was clarified in this study. Conversely, there was no relationship between VAS scores and changes in sleep patterns in this study. Since the sleep schedule is not related to temporary mood status during daytime (VAS), it is recommended that parents and clinical practitioners monitor children's sleep conditions.
In addition, changed sleep patterns were associated with maladaptive behavior in children during the COVID-19 pandemic. In previous studies, internalizing symptoms were associated with problematic sleep behaviors in children with comorbid ASD or ADHD, even in non-emergency situations (33, 34). During the COVID-19 stay-at-home period in Italy, it was revealed that ASD children had more intense and frequent disruptive behavior, although there was no mention of the relationship between sleep problems and maladaptive behavior (1). A similar relationship was also clarified during the stay-at-home periods in the present study.
In summary, the relationship between sleep schedule change and low QOL, and between sleep schedule change and internalized symptoms in children with NDDs, during the COVID-19 stay-at-home period tended to be the same as before the COVID-19 pandemic.
The decreased QOL of children with changed sleep patterns was predicted by high levels of depression. Furthermore, low QOL in children with unchanged sleep patterns was predicted by high levels of depression and low current mood status. As in previous studies, the prediction of low QOL was associated with increased depressive symptoms, regardless of sleep problems (35–37). Furthermore, in children with unchanged sleep patterns, worse temporary mood status was also a predictor of lower QOL. A positive relationship between temporary mood status and QOL in children having unchanged sleep patterns is affected by sleep invoked sufficient emotional adjustment (38).
In summary, the QOL of children with a stable life schedule was affected not only by depressive tendencies but also temporary moods. Therefore, they need to live a fulfilling life to maintain their QOL. However, the QOL of children with poor sleep patterns was affected only by depressive tendencies. Hence, it is important for clinicians that children with NDDs are correctly diagnosed with depression and treated for sleep problems.
In addition, the telerehabilitation (online rehabilitation) and online medical service for children with NDDs were constructed in several countries during the prolonged COVID-19 pandemic to continue care and adequate support to children and their families (39–41) and to ensure that the human rights of children with NDDs are protected, even during the emergency (42). It has been paying attention because of its ability to at least partially reduce the risk of hopelessness and loneliness, including anxious and depressive feelings related to the COVID-19 emergency. Since telecommunication in the medical field can be expected to improve the depression and well-being of children with NDDs, it is essential to build and improve the system in Japan.
The first of the study's limitations relates to the sample size of patients analyzed, which was small, even though the questionnaire collection rate was 100%. It was because there were a limited number of participants due to the single-center study. The second is that it is unclear whether the QOL of children was lower during the COVID-19 pandemic than before because the QOL of children with NDDs is usually significantly lower than that of the general child population (18, 36, 43). Third, the clinical characteristics of the children who participated in this study might differ from those throughout Japan because there were regional differences in infectious disease pandemics based on population density. Forth, it was impossible to accurately diagnose sleep disorders, as there were no interviews by doctors regarding children's sleep patterns and no sleep diaries from which to glean information. In the future, longitudinal studies analyzing sleep diaries of children with NDDs gain a clearer understanding of sleep disorders.
Among the study sample, 46.5% of children with NDDs had changed sleep patterns during the COVID-19 stay-at-home period. Of these, 19 children (22.1%) also showed a high tendency for depression and anxiety, respectively. Changed sleep patterns were associated with decreased QOL and internalized symptoms. The decreased QOL of children with changed sleep patterns was predicted by high depression. In addition, low QOL in children with unchanged sleep patterns was predicted by high levels of depression and low current mood status.
Since the adjustment of sleep schedule was associated with depressive states improvement and also their QOL, it is recommended that clinicians focus on children's regular sleep schedule as manifested during the COVID-19 stay-at-home period. The QOL and psychiatric status had to be evaluated by self-report as much as possible. Furthermore, it is necessary for children's keeping regular sleep schedules to maintain a system for linkage of education, welfare services, and medical care even in critical situations.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Institutional Review Board of the Shimada Ryoiku Center Hachioji (Shimahachi-2001). Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
RU, TO, and HO decided on the conception and design of the study. YO, HI, MS, YKo, CKo, YN, KA, AI, NS, YM, CKa, MK, and HO jointly carried out the acquisition of data (participant collection and data curation). RU and YKi performed the data analysis. RU wrote the manuscript. TO supervised this work and assisted with the writing of the manuscript. All the authors have approved the final article.
This work was supported partly by the Meiji Yasuda Mental Health Foundation, Japan (Grant Number 2020-1-007 to RU) and the Intramural Research Grant for Neurological and Psychiatric Disorders of NCNP, Japan (1–4 and 2–7 to TO).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Colizzi M, Sironi E, Antonini F, Ciceri ML, Bovo C, Zoccante L. Psychosocial and behavioral impact of COVID-19 in autism spectrum disorder: an online parent survey. Brain Sci. (2020) 10:341. doi: 10.3390/brainsci10060341
2. Wang C, Zhao H. The impact of COVID-19 on anxiety in chinese university students. Front Psychol. (2020) 11:1168. doi: 10.3389/fpsyg.2020.01168
3. Morris-Rosendahl DJ, Crocq M-A. Neurodevelopmental disorders—the history and future of a diagnostic concept. Dialogues Clin Neurosci. (2020) 22:65–72. doi: 10.31887/DCNS.2020.22.1/macrocq
4. Becker SP, Gregory AM. Editorial perspective: perils and promise for child and adolescent sleep and associated psychopathology during the COVID-19 pandemic. J Child Psychol Psychiatry. (2020) 61:757–9. doi: 10.1111/jcpp.13278
5. Ameis SH, Lai MC, Mulsant BH, Szatmari P. Coping, fostering resilience, and driving care innovation for autistic people and their families during the COVID-19 pandemic and beyond. Mol Autism. (2020) 11:61. doi: 10.1186/s13229-020-00365-y
6. Masi A, Mendoza Diaz A, Tully L, Azim SI, Woolfenden S, Efron D, et al. Impact of the COVID-19 pandemic on the well-being of children with neurodevelopmental disabilities and their parents. J Paediatr Child Health. (2021) 57:631–6. doi: 10.1111/jpc.15285
7. Provenzi L, Grumi S, Borgatti R. Alone with the kids: tele-medicine for children with special healthcare needs during COVID-19 emergency. Front Psychol. (2020) 11:2193. doi: 10.3389/fpsyg.2020.02193
8. Houtrow A, Harris D, Molinero A, Levin-Decanini T, Robichaud C. Children with disabilities in the United States and the COVID-19 pandemic. J Pediatr Rehabil Med. (2020) 13:415–24. doi: 10.3233/PRM-200769
9. Grumi S, Provenzi L, Gardani A, Aramini V, Dargenio E, Naboni C, et al. Rehabilitation services lockdown during the COVID-19 emergency: the mental health response of caregivers of children with neurodevelopmental disabilities. Disabil Rehabil. (2021) 43:27–32. doi: 10.1080/09638288.2020.1842520
10. Faccioli S, Lombardi F, Bellini P, Costi S, Sassi S, Pesci MC. How did Italian adolescents with disability and parents deal with the COVID-19 emergency? Int J Environ Res Public Health. (2021) 18:1687. doi: 10.3390/ijerph18041687
11. Boyle CA, Fox MH, Havercamp SM, Zubler J. The public health response to the COVID-19 pandemic for people with disabilities. Disabil Health J. (2020) 13:100943. doi: 10.1016/j.dhjo.2020.100943
12. Mazzone L, Postorino V, Siracusano M, Riccioni A, Curatolo P. The relationship between sleep problems, neurobiological alterations, core symptoms of autism spectrum disorder, and psychiatric comorbidities. J Clin Med. (2018) 7:102. doi: 10.3390/jcm7050102
13. Mogavero F, Jager A, Glennon JC. Clock genes, ADHD and aggression. Neurosci Biobehav Rev. (2018) 91:51–68. doi: 10.1016/j.neubiorev.2016.11.002
14. Ballester P, Richdale AL, Baker EK, Peiro AM. Sleep in autism: a biomolecular approach to aetiology and treatment. Sleep Med Rev. (2020) 54:101357. doi: 10.1016/j.smrv.2020.101357
15. Sung V, Hiscock H, Sciberras E, Efron D. Sleep problems in children with attention-deficit/hyperactivity disorder: prevalence and the effect on the child and family. Arch Pediatr Adolesc Med. (2008) 162:336–42. doi: 10.1001/archpedi.162.4.336
16. Green JL, Sciberras E, Anderson V, Efron D, Rinehart N. Association between autism symptoms and functioning in children with ADHD. Arch Dis Child. (2016) 101:922–8. doi: 10.1136/archdischild-2015-310257
17. Knuppel A, Telleus GK, Jakobsen H, Lauritsen MB. Quality of life in adolescents and adults with autism spectrum disorder: results from a nationwide Danish survey using self-reports and parental proxy-reports. Res Dev Disabil. (2018) 83:247–59. doi: 10.1016/j.ridd.2018.09.004
18. Danckaerts M, Sonuga-Barke EJ, Banaschewski T, Buitelaar J, Dopfner M, Hollis C, et al. The quality of life of children with attention deficit/hyperactivity disorder: a systematic review. Eur Child Adolesc Psychiatry. (2010) 19:83–105. doi: 10.1007/s00787-009-0046-3
19. Ueda R, Okada T, Kita Y, Ozawa Y, Inoue H, Shioda M, et al. The quality of life of children with neurodevelopmental disorders and their parents during the coronavirus disease 19 emergency in Japan. Sci Rep. (2021) 11:3042. doi: 10.1038/s41598-021-82743-x
20. Alamolhoda M, Farjami M, Bagheri Z, Ghanizadeh A, Jafari P. Assessing whether child and parent reports of the KINDL questionnaire measure the same constructs of quality of life in children with attention-deficit hyperactivity disorder. Health Qual Life Outcomes. (2021) 19:19. doi: 10.1186/s12955-020-01649-w
21. Burrows CA, Usher LV, Becker-Haimes EM, McMahon CM, Mundy PC, Jensen-Doss A, et al. Profiles and correlates of parent-child agreement on social anxiety symptoms in youth with autism spectrum disorder. J Autism Dev Disord. (2018) 48:2023–37. doi: 10.1007/s10803-018-3461-9
22. Kalvin CB, Marsh CL, Ibrahim K, Gladstone TR, Woodward D, Grantz H, et al. Discrepancies between parent and child ratings of anxiety in children with autism spectrum disorder. Autism Res. (2020) 13:93–103. doi: 10.1002/aur.2220
23. Lee YC, Yang HJ, Lee WT, Teng MJ. Do parents and children agree on rating a child's HRQOL? A systematic review and Meta-analysis of comparisons between children with attention deficit hyperactivity disorder and children with typical development using the PedsQLTM. Disabil Rehabil. (2019) 41:265–75. doi: 10.1080/09638288.2017.1391338
24. Hatta K, Hosozawa M, Tanaka K, Shimizu T. Exploring traits of autism and their impact on functional disability in children with somatic symptom disorder. J Autism Dev Disord. (2019) 49:729–37. doi: 10.1007/s10803-018-3751-2
25. Sano F, Kanemura H, Tando T, Goto Y, Hosaka H, Sugita K, et al. Depressive symptoms contribute to quality of life in children with epilepsy. Eur J Paediatr Neurol. (2014) 18:774–9. doi: 10.1016/j.ejpn.2014.08.002
26. Kawahara K, Ushijima H, Usami M, Takebayashi M. No associations of psychological symptoms and suicide risk with disaster experiences in junior high school students 5 years after the 2011 great east japan earthquake and tsunami. Neuropsychiatr Dis Treat. (2020) 16:2377–87. doi: 10.2147/ndt.S269835
27. Muris P, Schmidt H, Merckelbach H. Correlations among two self-report questionnaires for measuring DSM-defined anxiety disorder symptoms in children: the screen for child anxiety related emotional disorders and the Spence Children's Anxiety Scale. Pers Individ Diff. (2000) 28:333–46. doi: 10.1016/S0191-8869(99)00102-6
28. Kreindler D, Levitt A, Woolridge N, Lumsden CJ. Portable mood mapping: the validity and reliability of analog scale displays for mood assessment via hand-held computer. Psychiatry Res. (2003) 120:165–77. doi: 10.1016/s0165-1781(03)00196-3
29. Kim JH, Park EC, Yoo KB, Park S. The association between short or long sleep times and Quality of Life (QOL): results of the Korea National Health and Nutrition Examination Survey (KNHANES IV-V). J Clin Sleep Med. (2015) 11:625–34. doi: 10.5664/jcsm.4772
30. Achenbach TM, Rescorla L. Manual for the ASEBA School-Age Forms & Profiles: An Integrated System of Multi-Informant Assessment. Burlington, VT: ASEBA. (2001).
31. Lorish CD, Maisiak R. The Face Scale: a brief, nonverbal method for assessing patient mood. Arthritis Rheum. (1986) 29:906–9. doi: 10.1002/art.1780290714
32. Türkoglu S, Uçar HN, Çetin FH, Güler HA, Tezcan ME. The relationship between chronotype, sleep, and autism symptom severity in children with ASD in COVID-19 home confinement period. Chronobiol Int. (2020) 37:1207–13. doi: 10.1080/07420528.2020.1792485
33. Reynolds KC, Patriquin M, Alfano CA, Loveland KA, Pearson DA. Parent-reported problematic sleep behaviors in children with comorbid autism spectrum disorder and attention-deficit/hyperactivity disorder. Res Autism Spectr Disord. (2017) 39:20–32. doi: 10.1016/j.rasd.2017.04.003
34. Sannar EM, Palka T, Beresford C, Peura C, Kaplan D, Verdi M, et al. Sleep problems and their relationship to maladaptive behavior severity in psychiatrically hospitalized children with Autism Spectrum Disorder (ASD). J Autism Dev Disord. (2018) 48:3720–6. doi: 10.1007/s10803-017-3362-3
35. Armstrong D, Lycett K, Hiscock H, Care E, Sciberras E. Longitudinal associations between internalizing and externalizing comorbidities and functional outcomes for children with ADHD. Child Psychiatry Hum Dev. (2015) 46:736–48. doi: 10.1007/s10578-014-0515-x
36. Jonsson U, Alaie I, Lofgren Wilteus A, Zander E, Marschik PB, Coghill D, et al. Annual Research Review: Quality of life and childhood mental and behavioural disorders - a critical review of the research. J Child Psychol Psychiatry. (2017) 58:439–69. doi: 10.1111/jcpp.12645
37. Oakley BF, Tillmann J, Ahmad J, Crawley D, San Jose Caceres A, Holt R, et al. How do core autism traits and associated symptoms relate to quality of life? Findings from the Longitudinal European Autism Project. Autism. (2020) 22, 774–83. doi: 10.1177/1362361320959959
38. Walker MP. The role of sleep in cognition and emotion. Ann N Y Acad Sci. (2009) 1156:168–97. doi: 10.1111/j.1749-6632.2009.04416.x
39. Provenzi L, Grumi S, Gardani A, Aramini V, Dargenio E, Naboni C, et al. Italian parents welcomed a telehealth family-centred rehabilitation programme for children with disability during COVID-19 lockdown. Acta Paediatr. (2020). 110:194–6. doi: 10.1111/apa.15636
40. Provenzi L, Borgatti R. Potentials of telerehabilitation for families of children with special health care needs during the coronavirus disease 2019 emergency. JAMA Pediatr. (2021) 175:105. doi: 10.1001/jamapediatrics.2020.2351
41. Conti E, Chericoni N, Costanzo V, Lasala R, Mancini A, Prosperi M, et al. Moving toward telehealth surveillance services for toddlers at risk for autism during the COVID-19 pandemic. Front Psychiatry. (2020) 11:565999. doi: 10.3389/fpsyt.2020.565999
42. Schiariti V. The human rights of children with disabilities during health emergencies: the challenge of COVID-19. Dev Med Child Neurol. (2020) 62:661. doi: 10.1111/dmcn.14526
Keywords: COVID-19, children, neurodevelopmental disorders, quality of life, depression
Citation: Ueda R, Okada T, Kita Y, Ozawa Y, Inoue H, Shioda M, Kono Y, Kono C, Nakamura Y, Amemiya K, Ito A, Sugiura N, Matsuoka Y, Kaiga C, Kubota M and Ozawa H (2021) Psychological Status Associated With Low Quality of Life in School-Age Children With Neurodevelopmental Disorders During COVID-19 Stay-At-Home Period. Front. Psychiatry 12:676493. doi: 10.3389/fpsyt.2021.676493
Received: 05 March 2021; Accepted: 23 September 2021;
Published: 18 October 2021.
Edited by:
Rochelle Eime, Victoria University, AustraliaReviewed by:
Livio Provenzi, Neurological Institute Foundation Casimiro Mondino (IRCCS), ItalyCopyright © 2021 Ueda, Okada, Kita, Ozawa, Inoue, Shioda, Kono, Kono, Nakamura, Amemiya, Ito, Sugiura, Matsuoka, Kaiga, Kubota and Ozawa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Riyo Ueda, dWVkYXJpeW9AbmNucC5nby5qcA==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.