- 1School of Nursing and Midwifery, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
- 2School of Public Health, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
Background: Depression of health care workers was related to work absences, resignations, and poor work performance, affecting the quality of patient care and the health care system. The Coronavirus disease pandemic has had an effect on the mental health of health care workers. Health care workers are facing challenges that can be stressful, overwhelming, and cause strong emotions, may put them at higher risk to develop depression. There is limited evidence that assesses health care workers' depression and its associated factors in the study area during the Coronavirus disease pandemic. Therefore this study aimed to assess depression and associated factors among health care workers in eastern Ethiopia.
Method: The cross-sectional study design was conducted from October 26th to November 15, 2020. A total of 265 health care workers from 10 health facilities participated. Patient Health Questionnaire was used for the collection of depressive symptoms. The data were analyzed by using STATA version 14 software. To assess the association between depression and the predictors Adjusted Odds Ratio along with a 95% confidence interval was estimated by using logistic regression analysis. A statistical significance was declared at p-value ≤ 0.05.
Results: Of the total 265 study participant, 176 (66.4%) and 95% CI: 60.4%, 71.8% of them reported depressive symptoms. Of 176 reported symptoms of depression 27.9, 24.1, 9.4, 3.7, and 1.1% were had minimal, mild, moderate, moderate-severe, and severe depressive symptoms respectively. The multivariable logistic regression analysis revealed the odds of depression were 2.34 times higher among female participants compared to male participants (AOR: 2.34, 95%CI: 1.09-5.02). In addition, the odds of depression for participants who perceived susceptibility to COVID-19 was 4.05 times higher among their counterpart (AOR: 4.05, 95%CI: 1.12-14.53).
Conclusions: Health care workers who experienced depression in the study was high. Health care workers' mental health needs to be protected during the COVID-19 pandemic. Female health care workers and health care workers perceived susceptibility of COVID-19 need attention.
Introduction
Since the World Health Organization (WHO) declared coronavirus disease 2019 (COVID-19) a pandemic, it became a major challenging public health problem worldwide (1). Globally, many countries have been affected by the pandemic, as of October 27, 2020; there were 43,873,412 recorded cases and 1,166,039 fatalities (1). During the same period, 93,707 cases and 1,437 fatalities were recorded in Ethiopia (2). Similarly, more than 10,000 health care workers (HCWs) in the 40 countries of Africa have been infected with corona viruses disease (COVID-19) (3).
With the ever-growing number of confirmed and suspected cases, the workload of health care workers (HCWs) has been overwhelming (4). The long and irregular hours of such continuous and heavy volumes of work have the potential to trigger depression among HCWs (5–8). Safety measures like lockdown and physical distancing recommended by the world health organizations to limit the spread of pandemics among the public, but health care workers (HCWs) are left exposed (9). Globally, the prevalence of depression among HCWs range from 18 to 72% (10–16). Also, they are burdened with emotionally challenging interactions with the sick and potentially dying persons, fearing for their and families' health, and subject to occupational overload due to staff shortages and -insufficient personal protective equipment (17).
Many studies documented as HCWs face physical exhaustion, sleep disruption, fear, emotional disturbances, feeling vulnerable, loss of control, changes in working patterns/routine, feelings of personal danger, being isolated, lacking necessary supplies to conduct their work due to the COVID-19 pandemic (4, 18–20). This may increase their risk of depression, suicide, and burnout. Depression symptoms were related to work absences resignations and poor work performance, affecting patient care and the healthcare system (15, 21).
The studies identified feeling susceptible to contracting COVID-19, family/peers encouraged face mask use, access to adequate supplies of personal protective equipment (22), females sex, severe stress (23), having a chronic disease, and suspected or confirmed with COVID-19 infection were associated with depression among health care workers during COVID-19 pandemic (24). As a result of the ongoing COVID-19 pandemic, health care workers are fronting enormous worry due to the heavy load of cases. In many cases, they work increasingly long hours, often with limited resources and uncertain infrastructure. Thus, it is important to check on the mental health of caregivers (16).
Ethiopia reported the highest number of COVID-19 confirmed cases in East Africa. The number of confirmed COVID-19 confirmed cases and new deaths are alarmingly increasing. The number of the case at the end of December was 124,265 while on April 13 it was a surge to 232, 512 which was almost double with 4 months. The number of death at the end of December was 1,923 and almost double on April 13, 2021, 3,230. Eastern part of Ethiopia is a peripheral area sharing international borders were a greater number of COVID-19-related deaths. This may overwhelming and predispose the HCW to depression (25).
The study suggests that HCWs with depression benefit from care involving medical and psychological interventions (26). World Health Organization identified protecting the mental well-being of healthcare workers caring for people with COVID-19 has been identified as crucial for the long-term capacity of the HCWs (27). There is a limited study in Ethiopia that assesses the magnitude of depression and associated factors among health care workers during COVID-19. In addition, studies revealed HCWs experiencing depression were not planning to seek help and 30% were not aware of workplace help programs. This may be due to a lack of information on the prevalence and associated factors of depression. Therefore, this study aimed to assess the magnitude of depression status and associated factors among health care workers during the COVID-19 pandemic in the Eastern part of Ethiopia.
Methods and Materials
Study Setting and Period
The study was conducted among health facilities found in the Eastern Hararghe Zone, Oromia regional states found in the eastern part of Ethiopia. The East Hararghe zone has four hospitals, and 39 health centers according to the East Hararghe health bureau report (28). The study was conducted from October 25 to November 15, 2020. In 1998, the Ethiopian government established and recognized a health financing strategy that guides resources for the health sector to be organized from different sources and permits government to provide health services through its health facilities by means of a cost-sharing arrangement with users, providing services to the poor free of charge through a the fee-waiver system, as well as free provision of selected public health services (29). The Ethiopia COVID-19 public health emergency operation center (PHEOC) serves as a center for better coordinating the preparation, response, and recovery for public health emergencies. The center has been at the forefront of implementing efforts and mobilizing critical resources and lead house-to-house screenings and scaling up diagnostic testing. The center is collaboratively working with stakeholders: government agencies, partner organizations, UN agencies, embassies, hospitals, Industrial parks, and others (30).
Study Design and Source Population
Health the facilities-based cross-sectional study design was used. All health care workers include nurses, medical doctors, and allied health professionals from ten randomly selected health facilities found in the Eastern Hararghe zone were the study population. Health care workers who were on annual leave and for other activities away from health facilities during the period of data collection were excluded.
Sample Size Determination
The sample size was calculated using the formula for estimation of a single population proportion (n = [(Zα/2)2 *P(1-P)]/d2) with the assumptions of 95% confidence level, marginal error (d) of 0.05, and 50.4% the prevalence of depression among health care workers (19). The total number of the health care provider in the zone was 928 thus, after applying the finite population correction formula and adding 10% of the non-response rate, the final sample size obtained was 297.
Sampling Procedure and Sampling Technique
Two hospitals and eight health centers were selected by simple random sampling method (lottery method) from four hospitals and 39 health centers. All health care found in the selected health facilities was included.
Data Collection and Questionnaire
An interview questionnaire was developed to assess socio-demographic characteristics include; age sex, marital status, educational level, type of profession, types of health facility, and worker experiences. The 9-item Patient Health Questionnaire (PHQ-9) was used to assess depression symptoms. The questionnaire was validated and developed by the local language, Afaan Oromo and Amharic language in the Ethiopian context and it recommended for use (31, 32).
The data was collected by ten nurses. Four MSC health professionals were assigned to supervise the data collection process. Both the data collectors and supervisors were taken 2-day intensive training before the actual work about the aim of the study, procedures, data collection techniques, the art of interviewing, ways of collecting the data, and clarification. Data were collected by interview technique, since the health care providers may have limited knowledge of psychiatric symptoms. The intensive supervision was done by the principal investigator, co-investigators, and supervisors. Completeness, accuracy, and consistency of data were checked at the site of data collection throughout the data collection period. Finally, double data entry was done by two data clerks, and the consistency of the entered data was cross-checked by comparing the two separately entered data.
Measurements
The PHQ-9 is the depression module, which scores each of the nine DSM-IV criteria as 0–3 for every nine symptoms of depression, “0” not at all, “1” several days “2” more than half the days “3” nearly every day. Scoring was done by counting the number of boxes checked in a column. Multiply that number by the value indicated above, then add the subtotal to produce a total score. PHQ-9 total score for the nine items ranges from 0 to 27. Scores of zero, 1–4, 5–9, 10–14, 15–19, and 20–27 represent cut-points for no depression symptoms, minimal, mild, moderate, moderately severe, and severe depression, respectively (33). For logistic regression analysis we have categorized based on the PHQ-9 recommendation cut off point for depression, > 10 and coded as “1” and cut-off point ≤ 10 coded as “0.”
The age of the mother was recorded based on maternal response later and was grouped as 19–29 and ≥ 30 with codes 1 and 2, respectively, for analysis. Work experience was grouped <5 and ≥5 years with codes 1 and 2, respectively for analysis. Perceived susceptibility refers to a person's subjective perception of the risk of acquiring an illness or disease. Perceived severity refers to the subjective assessment of the severity of a health problem and its potential consequences (34). This study data for perceived susceptible was collected by interview using a single question “How likely do you think it is that you will develop COVID-19 during your providing care?” liker scale of five were used and labeled as “Strong unlikely,” “unlikely,” “Neutral,” “likely,” and “Strongly likely” and coded with 1, 2, 3, 4, and 5 respectively. For logistic regression analysis, we categorize as strong unlikely, unlikely, and neutral as no perceived susceptible, no susceptible coded as “1” and susceptible coded as “2.” With a similar pattern. Data for perceived severity was collected by interview using question with a single question “Getting COVID-19 in the future worries me and It is important for me to prevent getting.” Likert scale of five was used and labeled as “Strong unlikely,” “unlikely,” “Neutral,” “likely,” and “Strongly likely” and coded with 1, 2, 3, 4, and 5, respectively. For logistic regression analysis, we categorize as strong unlikely, unlikely, and neutral as no perceived susceptible, no susceptible coded as “1” and susceptible coded as “2.”
Data Analysis
Double data entry was made using the Epidata 3.1 software. Then after validation was done the data exported to the STATA statistical package version 14 for further analysis. Descriptive statistics were used to summarize the variable. Continuous variables like age and work experience were first transformed into categorical variables before analyzed. Initially, the crude odds ratio (COR) along with a 95% confidence interval was estimated to assess the association between each independent variable and the outcome variable. Multicollinearity was tested using the Variance Inflation Factor (VIF) test and the tolerance test. No multicollinearity problem was found. The Hosmer-Lemeshow goodness-of-fit tests were used to test for model fitness (35). The logistic regression model was used to assess the association between predictor variables and the outcome variable depression symptoms. Adjusted Odds Ratio (AOR) along with a 95% confidence interval was estimated to assess the strength of the association. Statistical significance was declared at a p-value ≤ of 0.05.
Ethical Consideration
The study was approved by the Haramaya University, College of Health and Medical Sciences Institutional Health Research Ethics Review Committee (IHRERC) with a reference number of IHRERC/230/2020. The permission and agreement consent was obtained from East Hararghe Zone, participating District health bureau, and health care facilities office prior to the study. The study participant was informed about the purpose of the study, their right to refuse, and written and signed voluntary consent was obtained prior to data collection. To maintain confidentiality, interviews were conducted in a separate room and all information obtained in this study was handled with anonymity. Based on the interpretation and recommendation of PHQ-9 author HCWs who had depression symptoms were referred to the psychiatric unit for further diagnosis and management who had moderate, moderate-severe, and severe symptoms.
Results
Socio-Demographic Characteristics and COVID-19 Related Perception of the Respondents
Of 297 total sample size, 265 health care workers participated in this study with a response rate of 89.22%. The reason for non-participation 13 (0.59%) were due to annual leave and 19 (0.71%) were due to additional assignments away from health facilities. The mean (±SD) age of HCWs was 29.29 (±6.40) years. The mean (±SD) HCWs work experience was 6.25 (±4.98) years. Of these, 161 (60.75%) were working in the inpatient department, the majorities 118 (44.53%) were nurses in the profession, and more than two-thirds of 183 (69.06%) were married. After categorizing, 202 (76.23%) and 222 (83.77%) respondents were perceived as susceptible and perceived severe to COVID-19, respectively (Table 1).
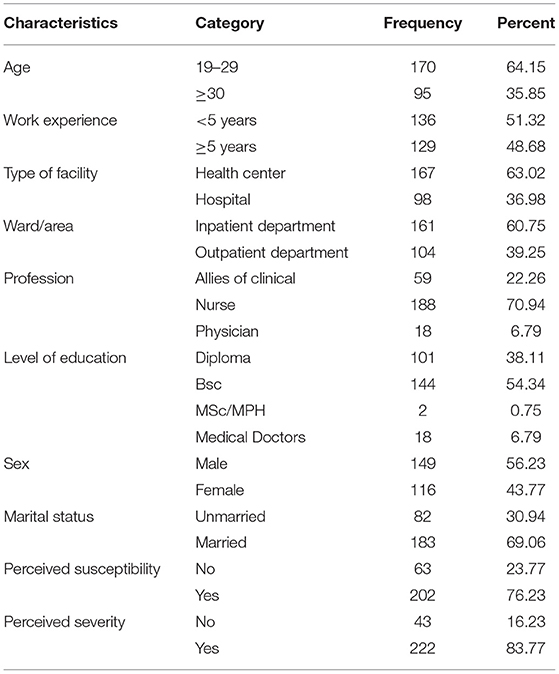
Table 1. Socio-demographic characteristics and COVID-19 related perception of respondents in in Eastern Hararghe zone, Oromia region, Eastern Ethiopia, 2020.
Participants Response to PHQ-9 Questions
More than half, 148 (55.85%) of respondents not at all had interest or pleasure in doing things over the past 2 weeks. Two third 174 (65.66%) of the respondents not at all feeling down, depressed, or hopeless, feeling tired 171 (64.53%) and trouble concentrating on things, such as reading the newspaper or watching television 173 (65.28%) over the past 2 weeks (Table 2).
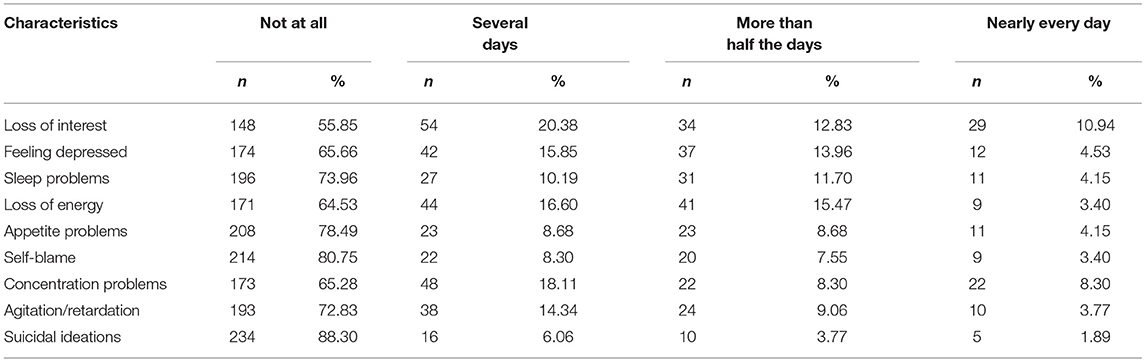
Table 2. Response of the participant to each depression question by health care workers in Eastern Hararghe zone, Oromia region, Eastern Ethiopia, 2020.
Level of Depression of Participants
According to the cut-off defined by PHQ-9 the level of depression of respondents were calculated. Of the total 265 interviewed, 176 (66.4%, 95%CI: 60.4%-71.8%) of them reported at least one depressive symptom. Of respondents who had symptoms of depression, 74 (27.92%) had minimal, 64 (24.15%) had mild depression, 9.43% moderate depression, 3.77% had moderate severe depression, and 1.13% had severe depression (Figure 1).
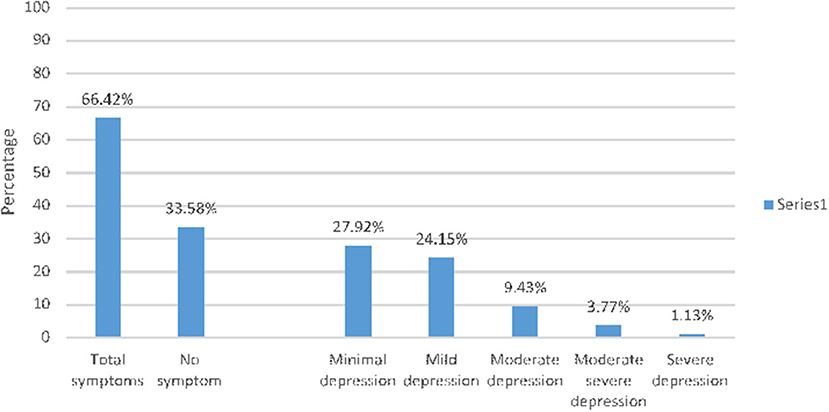
Figure 1. Level of depression among health care workers in Eastern Hararghe zone, Oromia region, Eastern Ethiopia, 2020.
Predictors of Depression
The multivariable logistic regression analysis revealed the odds of depression was 2.34 times higher among female participants compared to male participants (AOR: 2.34, 95%CI: 1.09-5.02). In addition, the odds of depression for participants who perceived susceptibility to COVID-19 was 4.05 times higher among their counterpart (AOR: 4.05, 95%CI: 1.12-14.53) (Table 3).
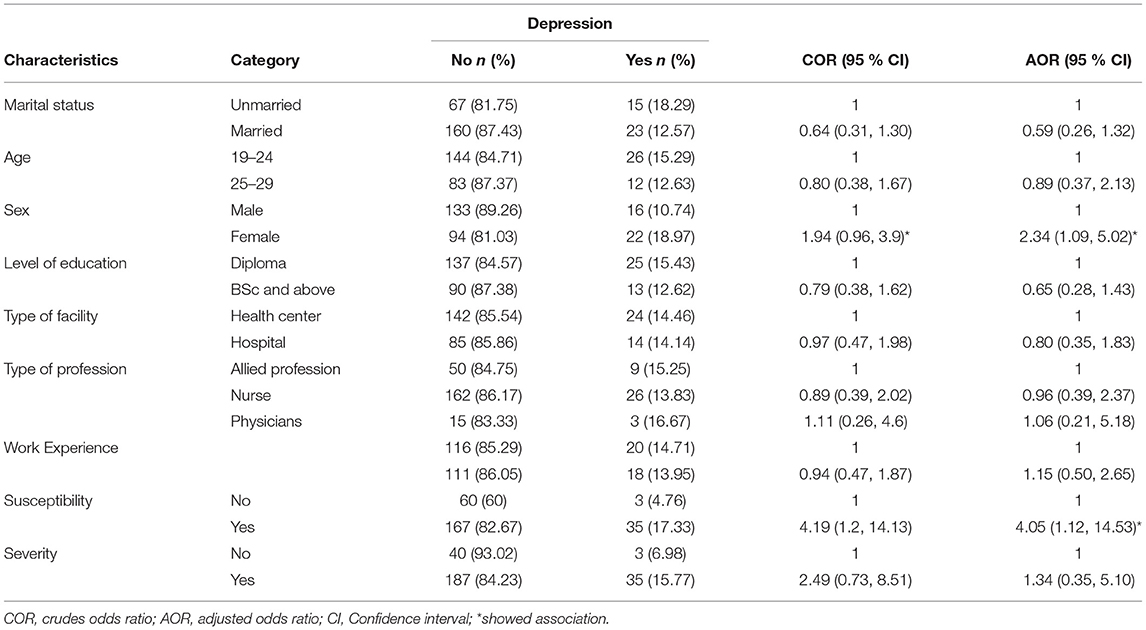
Table 3. Factors associated with the depression of health care workers in Eastern Hararghe zone, Oromia region, Eastern Ethiopia, 2020.
Discussion
In this study, overall, 176 (66.42%) of the study participants have had at least one depression symptoms. Factors significantly associated with depression symptoms were being a female and perceived susceptibility to COVID-19.
The depression symptoms reported in this study were high. This may due to, Ethiopia is one of the low-income countries which left HCWs with high fear of COVID-19 due to lack of personal protective equipment (PPE) and shortage of human power to handle ever-increasing the case (14, 36). This may result in fears and concerns for self, family members, problems with children and spouses, and difficulties entailed in working at home are some of the stressors during the Covid-19 pandemic (37). As some bodies experience stress, adrenal glands make and release cortisol hormone into the bloodstream. Prolonged elevated cortisol level leads to the manifestation of depression (38–40) and minimize the body immunity (41). Health care providers at higher risk of experiencing severe disease and even may fatal. ICN confirms 1,500 nurses have died from COVID-19 in 44 countries and estimates that healthcare worker COVID-19 fatalities worldwide could be more than 20,000 as of October 28, 2020 (42). Without addressing mental health services, we risk not having a workforce left to care for us.
The finding was consistent with those reported in a study conducted in Poland 70.7% (43). However, it was higher than studies finding in china at 54.65% (4) and 44.37% (44). This is may be due to Ethiopia is one of the developing countries which left HCWs with high fear of COVID-19 due to lack of personal protective equipment (PPE) and shortage of human power to handle ever increasing the case (14, 36) and low preparedness to compact the pandemic (36, 45, 46). In contrast, it was lower than a study finding in Egypt were 77.2% (23) participants had symptoms of depression. This difference might be due to contextual differences.
Regarding symptoms of depression, majority 24.15% participants had mild a symptom of depression followed by moderate 9.43%, severe 3.77% and 3 extremely severe. This was almost in line with study finding in the United Kingdom where 32.1% participants had mild, 17% moderate, 8.9% moderate severe and 5.7% (47) had severe symptoms of depression, respectively. But, it was relatively lower than study finding in Pakistan, 18.18% mild, 20.91% moderate, 40.91% severe and 11.81% participants had extremely severe symptoms of depression (16). Also, it was lower than study finding in India, 7.3% had severe symptoms of depression (48). This difference may be due to high fear for contacting the infection as a result of insufficient PPE, and low preparedness to compact the pandemic (36, 45, 46).
The study showed depression were associated with female health care workers. This is supported by studies conducted in China (19, 49), Iran (24), Egypt (23), and Ethiopia (50). Women are among the highly vulnerable population groups during a pandemic due to disrupt the food system and other economic activities. A study in India showed COVID-19 case fatality rate among men were 2.9 and 3.3% among women (51). Study showed that, there was a gender difference in stress and coping styles, numerous studies have determined that women find themselves in stressful circumstances more often than men, and their coping style is more emotion-focused than that of men (52). Social roles also seem relevant in the stressful life experiences of women, especially in low-income countries. There can be sex differences in the use of coping strategies which is important for the mitigation of depressive symptoms (53). The study shows that certain psychological and social determinants were associated with increased depressive symptoms, women are disadvantageous in a low-income country, COVID-19 enhances the vulnerability to the mental health challenge (54). Measures must be put into place to ensure the protection of women on the frontlines while reducing COVID-19 deaths and adverse health effects among displaced populations.
Perceived susceptibility (perception of the risk of acquiring COVID-19) was associated with participants who had symptoms of depression. This is consistent with the study finding in China (22, 55). Perceived susceptibility may be related to shortages of personal protective equipment (PPE) or other essential equipment, low community role in practice to protect themselves and the play their role in mitigating the transmission including to the health care worker (56). Contradicting of belief in susceptibility, with the low accessibility of protective measure, less concern of the community and the health manager may put health care providers at risk of experiencing depressive symptoms. Health care may also face moral dilemmas in decision-making around the provision of care with limited resources (6).
Depression symptoms were related to work absences and reduced work performance. The study investigated that workers with depression may benefit from care involving medical and psychological interventions (26). World Health Organization identified protecting the mental well-being of healthcare workers caring for people with COVID-19 has been recognized as crucial for the long-term capacity of the health workforce (27). However, most health care workers experiencing depression were not planning to seek help and not aware of workplace help plan (26). Prioritizing the well-being of health care workers must be at the forefront of the action plan to tackle the coming wave of this pandemic. We suggested that comprehensive psychological assistance should be provided to support the mental well-being of healthcare workers.
The trend of the number of COVID-19 confirmed cases in Ethiopia revealed that another wave of the pandemic is happening. The current increment in the number of COVID-19 cases may be attributed to the spread of the disease in the community due to relaxation of public health and social measures (PHSM) and fatigue around adhering to PSHM measures compounded by a high risk of importation variants of concern (VOC) (30). Urgent and effective community based intervention may reduce the pressure on mental health of the health care workers.
Strengths, Limitations, and Future Directions
The study conducted in multiple health care facilities including Hospitals and Health Centers found in town and rural areas. We never used design effect to increase the power due to budget constraints. However, the cross-sectional the study is important to be aware of the predictive, there is generally no evidence of a temporal relationship between exposure and outcome because the exposure and outcome are simultaneously assessed. The study includes only depressive symptoms, other mental health problems were not included. This study also not include staff who had contact with COVID-19 patients. We suggest a study that includes health professionals who had contact with COVID-19 patients, assessment of other mental health problems, longitudinal studies that assess the prolonged implication on HCWs need further investigation and more sample size. Finally, unaccounted and residual confounding could have had an effect on the association found.
Conclusion
The magnitude of health care workers experienced depression was high. Health care workers' mental health needs to be protected during the COVID-19 pandemic. Female health care workers, and health care workers perceived susceptibility of COVID-19 need attention.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, if officially requested without reservation.
Ethics Statement
The study was reviewed and approved by the Institutional Health Research Ethics Review Committee of the Colleges of Health and Medical Sciences, Haramaya University. Written consent was obtained from each participants before commencement of data collection. To maintain confidentiality, interviews were conducted in a separate room and all information obtained in this study was handled with anonymity.
Author Contributions
YD and BB conceived and designed the paper, involved in data collection, performed the statistical analysis, interpret the results, and wrote and reviewed the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was financially supported by Oromia Regional State Health (Ref No. BEFO/yccHar4/3926), Bureau, Ethiopia.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to thank Oromia Regional State Health Bureau for financial support, the study participants, for their generosity spent many hours responding to questionnaires. We wish to acknowledge the sterling contributions of our field workers, administrators, and data personnel and other staff who contributed to the data collection.
References
1. WHO. Coronavirus Disease (COVID-19) Pandemic. (2020). Avaliable at https://www.worldometers.info/coronavirus/ (accessed October 27, 2020).
2. FMOH. Coronavirus Update, Ethiopia Gov't Covid-19 Control Center. (2020). Avaliable at https://www.google.com/aclk?sa=L&ai=DChcSEwjymdTJ39TsAhWDse0KHRmlAn0YABAAGgJkZw&sig=AOD64_170o6wqY2KWtnMgjJsH3mh9HGCew&q&adurl&ved=2ahUKEwiSzMvJ39TsAhXFRxUIHarnDz8Q0Qx6BAgMEAE (accessed October 27, 2020).
3. WHO. Over 10 000 Health Workers in Africa Infected With COVID-19. (2020). Avaliable at https://www.afro.who.int/news/over-10-000-health-workers-africa-infected-covid-19 (accessed October 27, 2020).
4. Zhan YX, Zhao SY, Yuan J, Liu H, Liu YF, Gui LL, et al. Prevalence and influencing factors on fatigue of first-line nurses combating with COVID-19 in China: a descriptive cross-sectional study. Curr Med Sci. (2020) 40:625–35. doi: 10.1007/s11596-020-2226-9
5. Cai Z, Cui Q, Liu Z, Li J, Gong X, Liu J, et al. Nurses endured high risks of psychological problems under the epidemic of COVID-19 in a longitudinal study in Wuhan China. J Psychiatr Res. (2020) 131:132–7. doi: 10.1016/j.jpsychires.2020.09.007
6. da Silva FCT, Neto MLR. Psychiatric symptomatology associated with depression, anxiety, distress, and insomnia in health professionals working in patients affected by COVID-19: a systematic review with meta-analysis. Progr Neuropsychopharmacol Biol Psychiatry. (2020) 2020:110057. doi: 10.1016/j.pnpbp.2020.110057
7. Khanal P, Devkota N, Dahal M, Paudel K, Joshi D. Mental health impacts among health workers during COVID-19 in a low resource setting: a cross-sectional survey from Nepal. Global Health. (2020) 16:89. doi: 10.1186/s12992-020-00621-z
8. Li Q, Chen J, Xu G, Zhao J, Yu X, Wang S, et al. The psychological health status of healthcare workers during the COVID-19 outbreak: a cross-sectional survey study in Guangdong, China. Front Public Health. (2020) 8:562885. doi: 10.3389/fpubh.2020.562885
9. Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med. (2020) 27:taaa020. doi: 10.1093/jtm/taaa020
10. Blake H, Bermingham F, Johnson G, Tabner A. Mitigating the psychological impact of COVID-19 on healthcare workers: a digital learning package. Int J Environ Res Public Health. (2020) 17:. doi: 10.3390/ijerph17092997
11. Liang Y, Wu K, Zhou Y, Huang X, Zhou Y, Liu Z. Mental health in frontline medical workers during the 2019 novel coronavirus disease epidemic in China: a comparison with the general population. Int J Environ Res Public Health. (2020) 17:6551. doi: 10.3390/ijerph17186550
12. Alshekaili M, Hassan W, Al Said N, Al Sulaimani F, Jayapal SK, Al-Mawali A, et al. Factors associated with mental health outcomes across healthcare settings in Oman during COVID-19: frontline versus non-frontline healthcare workers. BMJ open. (2020) 10:e042030. doi: 10.1136/bmjopen-2020-042030
13. Amin F, Sharif S, Saeed R, Durrani N, Jilani D. COVID-19 pandemic- knowledge, perception, anxiety and depression among frontline doctors of Pakistan. BMC Psychiatry. (2020) 20:459. doi: 10.1186/s12888-020-02864-x
14. Chen J, Liu X, Wang D, Jin Y, He M, Ma Y, et al. Risk factors for depression and anxiety in healthcare workers deployed during the COVID-19 outbreak in China. Soc Psychiatry Psychiatr Epidemiol. (2020) 1:1–9. doi: 10.1007/s00127-020-01954-1
15. Gill S, Hao D, Hirte H, Campbell A, Colwell B. Impact of COVID-19 on Canadian medical oncologists and cancer care: Canadian Association of Medical Oncologists survey report. Curr Oncol. (2020) 27:71–4. doi: 10.3747/co.27.6643
16. Sandesh R, Shahid W, Dev K, Mandhan N, Shankar P, Shaikh A, et al. Impact of COVID-19 on the mental health of healthcare professionals in Pakistan. Cureus. (2020) 12:e8974. doi: 10.7759/cureus.8974
17. Huang JZ, Han M, Luo T, Ren A, Zhou X. Mental health survey of 230 medical staff in a tertiary infectious disease hospital for COVID-19. Chin J Ind Hyg Occup Dis. (2020) 38:E001. doi: 10.3760/cma.j.cn121094-20200219-00063
18. Dong Z-Q, Ma J, Hao Y-N, Shen X-L, Liu F, Gao Y, et al. The social psychological impact of the COVID-19 pandemic on medical staff in China: a cross-sectional study. Eur Psychiatry. (2020) 63:e65. doi: 10.1192/j.eurpsy.2020.59
19. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
20. An Y, Yang Y, Wang A, Li Y, Zhang Q, Cheung T, et al. Prevalence of depression and its impact on quality of life among frontline nurses in emergency departments during the COVID-19 outbreak. J Affect Disord. (2020) 276:312–5. doi: 10.1016/j.jad.2020.06.047
21. Dobson H, Malpas CB, Burrell AJ, Gurvich C, Chen L, Kulkarni J, et al. Burnout and psychological distress amongst Australian healthcare workers during the COVID-19 pandemic. Aust Psychiatry. (2020) 29:26–30. doi: 10.1177/1039856220965045
22. Lam SC, Arora T, Grey I, Suen LKP, E.Huang Y-z, Li D, et al. Perceived risk and protection from infection and depressive symptoms among healthcare workers in mainland China and Hong Kong during COVID-19. Front Psychiatry. (2020) 11:686. doi: 10.3389/fpsyt.2020.00686
23. Elkholy H, Tawfik F, Ibrahim I, Salah El-din W, Sabry M, Mohammed S, et al. Mental health of frontline healthcare workers exposed to COVID-19 in Egypt: a call for action. Int J Soc Psychiatry. (2020) 2020:1–10. doi: 10.1177/0020764020960192
24. Pouralizadeh M, Bostani Z, Maroufizadeh S, Ghanbari A, Khoshbakht M, Alavi SA, et al. Anxiety and depression and the related factors in nurses of Guilan University of Medical Sciences hospitals during COVID-19: a web-based cross-sectional study. Int J Afr Nurs Sci. (2020) 13:100233. doi: 10.1016/j.ijans.2020.100233
25. Alene KA, Gelaw YA, Fetene DM, Koye DN, Melaku YA, Gesesew H, et al. COVID-19 in Ethiopia: a geospatial analysis of vulnerability to infection, case severity and death. BMJ Open. (2021) 11:e044606. doi: 10.1136/bmjopen-2020-044606
26. Lerner D, Adler DA, Rogers WH, Lapitsky L, McLaughlin T, Reed J. Work performance of employees with depression: the impact of work stressors. Am J Health Promot. (2010) 24:205–13. doi: 10.4278/ajhp.090313-QUAN-103
27. WHO. Mental Health and Psychosocial Considerations During the COVID-19 Outbreak. (2020). Available online: https://www.who.int/docs/default-source/coronaviruse/mental-health-considerations.pdf (accessed April 17, 2020).
30. M.o.Ethiopia Health. National Public Health Emergency Operation Center (PHEOC), ETHIOPIA COVID-19 Pandemic Perepardness and Response in Ethiopia. Wkly Bul WHO Epi Week. Addis Abeba (2021) 12.
31. Degefa M, Dubale B, Bayouh F, Ayele B, Zewde Y. Validation of the PHQ-9 depression scale in Ethiopian cancer patients attending the oncology clinic at Tikur Anbessa specialized hospital. BMC Psychiatry. (2020) 20:1–7. doi: 10.1186/s12888-020-02850-3
32. Woldetensay YK, Belachew T, Tesfaye M, Spielman K, Biesalski HK, Kantelhardt EJ, et al. Validation of the Patient Health Questionnaire (PHQ-9) as a screening tool for depression in pregnant women: Afaan Oromo version. PLoS ONE. (2018) 13:e0191782. doi: 10.1371/journal.pone.0191782
33. Beck AT, Steer RA, William RB, Ranieri F. Comparison of Beck Depression Inventories-IA and-II in Psychiatric Outpatients. J Persen Assess. (1996) 67:588–97. doi: 10.1207/s15327752jpa6703_13
34. Rosenstock IM. The health belief model and preventive health behavior. Health Educ Monogr. (1974) 2:354–86. doi: 10.1177/109019817400200405
35. Midi H, Sarkar SK, Rana S. Collinearity diagnostics of binary logistic regression model. J Interdisc Math. (2010) 13:253–67. doi: 10.1080/09720502.2010.10700699
36. FMOH National Comprehensive Covid19 Management Handbook. (2020). Avaliable at: http://www.moh.gov.et/ejcc/en/node/196 (accessed October 27, 2020).
37. Levkovich I, Shinan-Altman S. Impact of the COVID-19 pandemic on stress and emotional reactions in Israel: a mixed-methods study. Int Health. (2020). doi: 10.21203/rs.3.rs-30346/v1. [Epub ahead of print].
38. Dinan TG. Glucocorticoids and the genesis of depressive illness a psychobiological model. Br J Psychiatry. (1994) 164:365–71. doi: 10.1192/bjp.164.3.365
39. Cowen P. Cortisol, serotonin and depression: all stressed out? Br J Psychiatry. (2002) 180:99–100. doi: 10.1192/bjp.180.2.99
40. Hannibal KE, Bishop MD. Chronic stress, cortisol dysfunction, and pain: a psychoneuroendocrine rationale for stress management in pain rehabilitation. Phys Therapy. (2014) 94:1816–25. doi: 10.2522/ptj.20130597
41. Glacer R, Kiecolt-Glacer JK, Stout JC, Tarr KL, Speicher CE, Holliday JE. Stress-related impairments in cellular immunity. Psychiatry Res. (1985) 16:233–9. doi: 10.1016/0165-1781(85)90111-8
43. Wańkowicz P, Szylińska A, Rotter I. Assessment of mental health factors among health professionals depending on their contact with COVID-19 patients. Int J Environ Res Public Health. (2020) 17:5849. doi: 10.3390/ijerph17165849
44. Que J, Le Shi JD, Liu J, Zhang L, Wu S, Gong Y, et al. Psychological impact of the COVID-19 pandemic on healthcare workers: a cross-sectional study in China. Gen Psychiatry. (2020) 33:e100259. doi: 10.1136/gpsych-2020-100259
45. Mulu GB, Kebede WM, Worku SA, Mittiku YM, Ayelign B. Preparedness and responses of healthcare providers to combat the spread of COVID-19 Among North Shewa Zone Hospitals, Amhara, Ethiopia, 2020. Infect Drug Resist. (2020) 13:3171. doi: 10.2147/IDR.S265829
46. WHO. Technical Guidance on Infection Prevention and Control During the Coronavirus (COVID-19) Outbreak for the Western Pacific Region. Avaliable at: https://www.who.int/westernpacific/emergencies/covid-19/technical-guidance/infection-prevention-control (accessed October 27, 2020).
47. Jia R, Ayling K, Chalder T, Massey A, Broadbent E, Coupland C, et al. Mental health in the UK during the COVID-19 pandemic: cross-sectional analyses from a community cohort study. BMJ Open. (2020) 10:e040620. doi: 10.1136/bmjopen-2020-040620
48. Pandey U, Corbett G, Mohan S, Reagu S, Kumar S, Farrell T, et al. Anxiety, depression and behavioural changes in junior doctors and medical students associated with the coronavirus pandemic: a cross-sectional survey. J Obstetr Gynaecol India. (2020) 1–5. doi: 10.1007/s13224-020-01366-w
49. Zhu Z, Xu S, Wang H, Liu Z, Wu J, Li G, et al. COVID-19 in Wuhan: immediate psychological impact on 5062 health workers. MedRxiv [Preprint]. (2020). doi: 10.1101/2020.02.20.20025338
50. Kemal J, Berhanu S, Tinsae GA, Mukemil A. COVID-19 pandemic and self-reported symptoms of depression, anxiety, and stress among health care workers in Ethiopia. Neuropsychiatr Dis Treat. (2020) 17:1363–73. doi: 10.21203/rs.3.rs-62244/v1
51. Joe W, Kumar A, Rajpal S, Mishra U, Subramanian S. Equal risk, unequal burden? Gender differentials in COVID-19 mortality in India. J Global Health Sci. (2020) 2:e17. doi: 10.35500/jghs.2020.2.e17
52. Sibley CG, Overall NC. Modeling the hierarchical structure of attachment representations: A test of domain differentiation. Person Ind Differ. (2008) 44:238–49. doi: 10.1016/j.paid.2007.08.003
53. Kelly MM, Tyrka AR, Price LH, Carpenter LL. Sex differences in the use of coping strategies: predictors of anxiety and depressive symptoms. Depress Anxiety. (2008) 25:839–46. doi: 10.1002/da.20341
54. Skapinakis P, Bellos S, Oikonomou A, Dimitriadis G, Gkikas P, Perdikari E, et al. Depression and its relationship with coping strategies and illness perceptions during the COVID-19 lockdown in Greece: a cross-sectional survey of the population. Depress Res Treat. (2020) 2020:3158954. doi: 10.1155/2020/3158954
55. Ying Y, Ruan L, Kong F, Zhu B, Ji Y, Lou Z. Mental health status among family members of health care workers in Ningbo, China, during the coronavirus disease 2019 (COVID-19) outbreak: a cross-sectional study. BMC Psychiatry. (2020) 20:379. doi: 10.1186/s12888-020-02784-w
Keywords: health worker, depression, COVID-19, eastern, Ethiopia, pandemic
Citation: Yadeta TA, Dessie Y and Balis B (2021) Magnitude and Predictors of Health Care Workers Depression During the COVID-19 Pandemic: Health Facility-Based Study in Eastern Ethiopia. Front. Psychiatry 12:654430. doi: 10.3389/fpsyt.2021.654430
Received: 16 January 2021; Accepted: 19 May 2021;
Published: 15 July 2021.
Edited by:
Paul Alfred Vöhringer, Harvard University, United StatesReviewed by:
Minale Tareke, Bahir Dar University, EthiopiaSamir Al-Adawi, Sultan Qaboos University, Oman
Copyright © 2021 Yadeta, Dessie and Balis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tesfaye Assebe Yadeta, dGVzZmF5ZS5hc3NiQGdtYWlsLmNvbQ==
 Tesfaye Assebe Yadeta
Tesfaye Assebe Yadeta Yadeta Dessie
Yadeta Dessie Bikila Balis1
Bikila Balis1