
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 04 June 2021
Sec. Child and Adolescent Psychiatry
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.653047
This article is part of the Research Topic Full and Partial Hospitalization Interventions for Eating Disorders View all 17 articles
 Martina M. Mensi1,2
Martina M. Mensi1,2 Marika Orlandi1
Marika Orlandi1 Chiara Rogantini2
Chiara Rogantini2 Livio Provenzi1
Livio Provenzi1 Matteo Chiappedi1*
Matteo Chiappedi1* Michela Criscuolo3
Michela Criscuolo3 Maria C. Castiglioni3
Maria C. Castiglioni3 Valeria Zanna3
Valeria Zanna3 Renato Borgatti1,2 on behalf of Mondino Foundation Eating Disorders Clinical and Research Group
Renato Borgatti1,2 on behalf of Mondino Foundation Eating Disorders Clinical and Research GroupThe present study presents an investigation of family functioning in the families of adolescents with severe restrictive eating disorders (REDs) assessed before and 6 months after a multidisciplinary family treatment program that combined psychodynamic psychotherapy, parental role intervention, and triadic or family-centered interventions. Nutritional counseling and neuropsychiatric monitoring of the overall treatment and care process were also provided. Family functioning was assessed using the clinical version of the Lausanne Trilogue Play (LTPc), a semi-structured procedure for observing family dynamics, previously validated for this patient population. The LTPc is divided into four phases. In phase 1, the mother interacts with the patient while the father assumes the role of observer. In phase 2, the father plans an activity with the patient while the mother observes. In phase 3, all the family members interact. Finally, in phase 4, the parents talk while the adolescent observes. A significant change emerged in family functioning after the treatment, but only for the interactive phase 2, when the father is required to interact with the daughter while the mother silently observes. The results of this study suggest that a relatively brief multidisciplinary treatment program may significantly improve family functioning in the families of patients diagnosed with severe REDs. Although appropriate clinical trials are needed to further test the efficacy of this treatment, the results also reinforce the concept that treatment programs targeting the individual patient and both the parents should be a first-line approach in adolescents with severe REDs.
Restrictive eating disorders (REDs) are a heterogeneous group of potentially severe psychopathological conditions that have shown an increased incidence among young people in recent years, especially in the high-risk group of 15- to 19-year-old girls (1–3). REDs are thought to have a multifactorial etiology involving individual vulnerability factors influenced by biological, psychological, environmental, and family-related factors (4–8).
Among the latter, previous research has highlighted that family relations are frequently dysfunctional in the families of individuals affected by REDs (9–11). Cerniglia and his group (12), for example, underlined difficulties in respecting interpersonal boundaries, poor tolerance of conflict, and low satisfaction. Use of the clinical version of the Lausanne Trilogue Play (LTPc) (13)—a semi-structured method for observing family dynamics—may help to identify specific characteristics of a family's triadic interactions that may be linked to the patient's clinical condition. Previous LTPc studies have in fact highlighted dysfunctional interaction patterns in the families of individuals with REDs (14–16). For example, fathers were found to experience specific difficulties in maintaining a scaffolding role in relation to their daughters' development, and in providing them with support and guidance (14, 15, 17). This is line with current literature (18, 19) showing that fathers tend to disengage from caregiving. Accordingly, it has been suggested that greater affective engagement and participation in the healthcare process on the part of fathers should be encouraged (20, 21). During the last decade, the focus of family functioning research in this specific area has shifted away from the role of family-related factors in maintaining REDs to enhancement of protective family factors that may improve interventions (22). In these families, parents often tend to adapt their own lives to the RED symptoms of their daughters; for example, they may accept meal rituals in order to avoid conflicts (23). Not surprisingly, therefore engagement of the whole family in the adolescent's treatment and care process is now recognized as a key prognostic factor (4, 7, 17, 24–29).
Family-centered approaches [e.g., family-based therapy (FBT)] (30, 31) are among the most effective (type I evidence) interventions for the psychiatric care of patients with REDs (20, 32); in particular, they are considered the first-line treatment for severe cases in adolescence (25, 33, 34). Recently, FBT has also been found to be effective in the treatment of avoidant/restrictive food intake disorder (ARFID) (35). Nonetheless, the efficacy may be partial when family members are not properly engaged in the treatment and care process (26, 27), and a significant number of patients may not respond well to FBT. Another family therapy approach that has shown good evidence of effectiveness is the psychodynamic model based specifically on intrafamily relationships developed by the French group at the Montsouris Institute in Paris (18). This model focuses more on psychological issues than on eating behavior symptoms. It has been shown to be effective in reducing feeding symptoms and improving general psychopathological functioning, as measured by the Morgan–Russell Outcome Assessment Schedule (MROAS) (36) adapted for adolescent patients (37). These results suggest that improving family functioning may be an intermediate goal, important in promoting better clinical outcomes in the adolescent herself (17, 38, 39). Individual approaches, such as adolescent-focused therapy (40), can also be effective when patients are affected by more severe psychopathological conditions and when their autonomy is severely compromised. Reinstating adaptive psychological development trajectories should be considered a pivotal aim to target within the recovery process (39, 41). However, when family relationships are highly dysfunctional, individual psychotherapy can achieve only partial results; dysfunctional parenting may negatively impact the treatment and care process of adolescents with REDs, and may represent a significant obstacle to the effectiveness of individual psychotherapy (18, 41).
On the basis of these premises, and with a view to identifying a suitable treatment for patients with severe REDs, a multidisciplinary family therapy approach integrating the models by Godart et al. (18) and Fitzpatrick et al. (40) was developed at two university tertiary care services in Italy. The treatment program we developed combines principles from various models of intervention (i.e., psychodynamic psychotherapy, parental role intervention, and triadic or family-centered interventions). We also provided nutritional counseling and neuropsychiatric monitoring of the overall process, including the effects of any pharmacological therapy. The aim of the present study was to look for significant pre-post differences in family functioning in the families of adolescent patients with severe REDs who underwent a 6-month (± two) multidisciplinary treatment program. Family functioning was assessed before and after the treatment using the LTPc procedure (13). Greater understanding of how family functioning may improve after a relatively brief multidisciplinary family treatment program may further inform effective interventions for these patients and their families. LTPc score changes are related to changes in family members' abilities to get involved in the game, to adhere to their assigned role in the different phases of it (and therefore, when necessary, to stand back), and to support others' ideas. Score changes may also be linked to greater emotional participation and exchange, as well as improved gaze triangulation.
Sixty-seven families of adolescent patients diagnosed with REDs were assessed for eligibility between July 2017 and October 2020 at the Child Neurology and Psychiatry Unit of the IRCCS Mondino Foundation (Pavia, Italy) and at the Child and Adolescent Neuropsychiatry Unit of the Bambino Gesù Children's Hospital (Rome, Italy). Patients were considered eligible for the study if they were 11–18 years old and if they had a diagnosis of RED (including restrictive and binge-eating/purging subtypes of anorexia nervosa, ARFID, atypical anorexia nervosa, other specified feeding or eating disorders with restrictive characteristics). Diagnoses were made according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) criteria (42). Patients were excluded from the study if they presented at least one of the following: psychotic disorders, intellectual disability, neurological disorders (e.g., epilepsy), or other psychiatric comorbidities with an organic substrate (e.g., celiac disease, Wilson's disease). Single-parent families and individuals partially unable to understand Italian were also considered ineligible. Finally, to avoid interrupting or modifying ongoing therapies, we also excluded patients who were already receiving psychotherapy at a secondary-level service. The study was approved by the Ethics Committee of the Policlinico San Matteo in Pavia, Italy (P-20170016006). All the enrolled patients and their parents provided written informed consent to participate in the study. Figure 1 illustrates the flow chart of the participant selection process.
The patients were interviewed by a trained child neuropsychiatrist, who collected clinical and socio-demographic data. To confirm the RED diagnosis and verify the presence of any comorbidities, the semi-structured DSM-based K-SADS interview (43) was administered to the patients and their parents. Furthermore, the absence of intellectual disabilities was verified through administration of the age-appropriate Wechsler intelligence scale: WISC-IV (44) or WAIS-IV (45). To evaluate family functioning, the LTPc procedure (13) was used twice, before (T0) and after the treatment (T1). Every LTPc session, performed in a dedicated room, was videotaped and subsequently coded independently by two raters, who had first received specific training.
The treatment lasted 6 (±2) months and involved a multidisciplinary team (Figure 2), as the main international guidelines suggest that the care of patients affected by REDs should be entrusted to a team of medical, social, and rehabilitation healthcare professionals (24, 46).
Our multidisciplinary team comprised an expert neuropsychiatrist, a neuropsychiatry resident, psychotherapists, a psychiatric rehabilitation specialist, an educator, and a nurse.
The integrated treatment model (see Supplementary Material) consisted of at least 24 sessions of psychodynamic psychotherapy for the adolescent patient, scheduled once a week and conducted in an individual or group setting (40, 47, 48), at least 12 parental role intervention sessions (49, 50), and at least 12 treatment sessions focusing on triadic or family interaction. The parental role sessions took place every other week, alternating with the triadic or family interventions. The first session with the parents always involved the use of video feedback, which allows parents to work directly on their own limits and resources, favors the development of the ability to reflect on the relationship (mentalization), and significantly improves the therapeutic alliance (51–53).
Finally, nutritional counseling was provided, as well as neuropsychiatric monitoring of the progress of the treatment, to allow introduction or adjustment of pharmacological therapy as needed, as in the case of comorbid depressive or anxious symptoms. Further details on the intervention are reported in Supplementary Material.
The LTPc is a standardized and well-validated observation-based method used in clinical and research settings to assess dysfunctional patterns in triadic or family interactions (13). The procedure requires parents and daughter to pretend that they are planning a weekend where the adolescent daughter stays home alone. The pretend play is divided into four phases. In phase 1, the mother interacts with the patient while the father assumes the role of observer. In phase 2, the father plans the activity with the patient while the mother observes. In phase 3, all the family members interact with each other. Finally, in phase 4, the parents talk together, while the adolescent assumes the role of observer. The entire process is videotaped and lasts ~15 min.
The LTPc coding system used in this study has been explained in previous publications (14, 52, 54, 55). Essentially, it considers four aspects of interaction (i.e., participation, organization, focal attention, affective contact), which are rated, in each phase, on a three-point Likert scale (0 = dysfunctional; 1 = partially functional; 2 = functional). On this basis, descriptions of each family member's interactive contribution and of the overall family functioning are obtained. The total family score, which identifies one of four types of family alliance, is the sum of the scores recorded by each family member in each phase (13).
The statistical analyses were conducted using IBM SPSS Version 21 for Windows. Descriptive statistics were calculated for each variable. To test for stability, we adopted the mean-level change method (56) and rank-order consistency method (57). To assess mean differences in LTPc scores, separate paired sample t-tests were computed for each LTPc phase (1, mother-daughter; 2, father-daughter; 3, triadic interaction; 4, parental pair).
Table 1 reports the descriptive statistics for this sample. Eighteen 11- to 17-year-old girls (M = 14.64 years, SD = 1.47) who were being cared for in day-hospital settings participated in the study with their parents. Eleven girls came from the Child Neurology and Psychiatry Unit of the IRCCS Mondino Foundation in Pavia (61.11%) and seven from the Child and Adolescent Neuropsychiatry Unit of the Bambino Gesù Children's Hospital in Rome (38.89%). Two of the 18 pairs of parents were divorced (11.10%). The average duration of symptoms prior to clinical referral was 13.32 months (SD = 11.33). The severity of the patients' clinical conditions was assessed using the MROAS and coded as: 0 = good outcome, 1 = intermediate outcome, and 2 = poor outcome. These outcomes were distributed as follows: 25.4% good, 44.1% intermediate, and 30.5% poor. At baseline (T0), the average percentage of weight loss reported by the patients was 22.02% (SD = 11.15), and their average BMI was 13.1 kg/m2 (SD = 18.74) (range: 11.91–32.11 kg/m2). The median pre-treatment percentile BMI was 1.2. Within the sample, 28 of 67 patients were using medications before T0 (i.e., 6.9% were taking antipsychotics, 58.6% antidepressants, 6.9% benzodiazepines, and 27.6% a combination of antipsychotics and antidepressants). The total family score in phase 2 (father–daughter) showed a statistically significant positive change from T0 to T1 (see Table 2). No significant differences emerged for the other LTPc phases.
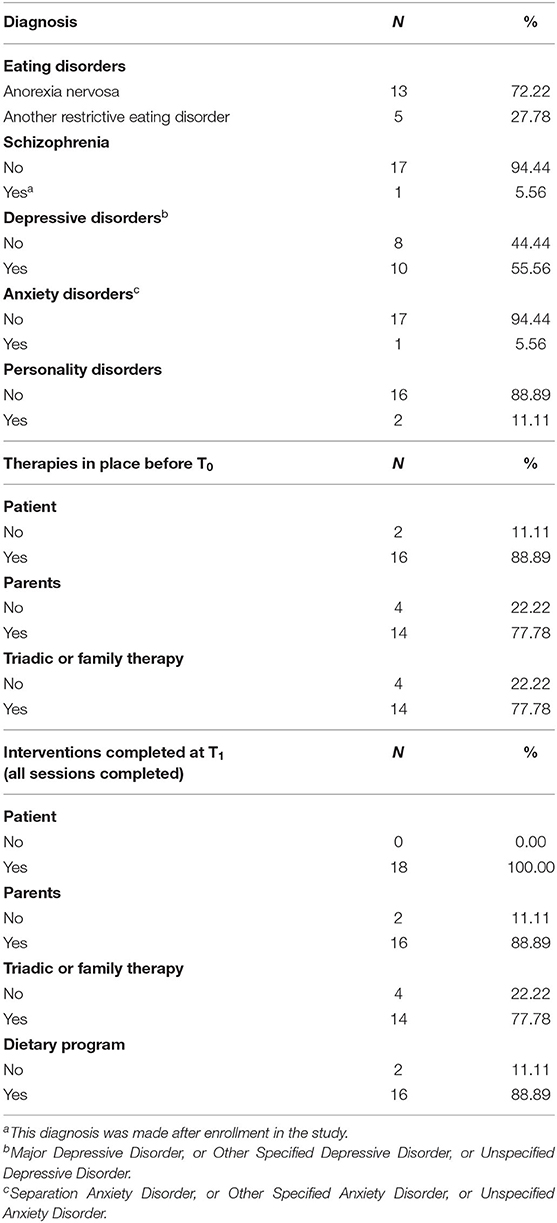
Table 1. Descriptive statistics: patients' baseline diagnoses and therapies both before and during the multidisciplinary treatment program.
The aim of the present study was to assess post-treatment changes in family functioning among families of adolescents with severe REDs who underwent a multidisciplinary 6-month treatment program. We observed a significant change in the family functioning score for the LTPc phase 2, in which the father interacts with his daughter while the mother acts as a silent observer. This suggests that the fathers, when playing an active role, could improve dyadic family functioning. This finding is consistent with the idea, emerging from previous pioneering studies, that encouraging paternal involvement can improve patient outcomes (20, 21). In the families of girls affected by REDs, fathers tend to be disengaged from the caregiving role. Although this may be merely a defensive reaction to their daughter's illness, it can lead to a less affective bond and influence the quality of family interactions and the patient's outcome (15, 58). It can be speculated that the treatment model here proposed had more effect on the fathers than on the other members of the triad. In line with the current literature (59, 60), the results of our study therefore support the clinical indication of promoting affective engagement and participation of all family members, including fathers, in the care of adolescent patients, especially those with REDs (18, 19). A growing body of literature indeed suggests that therapeutic approaches to severe REDs in adolescence should include the promotion of paternal—and not only maternal—participation (20, 21, 61), in order to enhance the parents' alliance and improve the quality of triadic interactions. Paternal involvement and warmth have been shown to be fundamental for patient outcomes, and fathers who tend to draw back and remain emotionally and concretely detached need to be encouraged and supported (18, 20, 21, 62).
We did not find a similar change in maternal interactive behavior after the treatment. As others have pointed out (63–65), mothers are usually more involved in their daughters' afflictions. It is likely that a more prolonged family treatment would be needed in order to change dysfunctional interactive patterns in mothers. However, it can also be speculated that when fathers prove able to play a more active role, this may be due in part to mothers managing to give them more space (15).
We also found no post-treatment change in the functioning of the parental pair. This is in line with the fact that our treatment model, based on a psycho-pedagogical approach, was designed to strengthen the parental role rather than address relational dynamics (such as conflict and conflict management) between the parents themselves (66). Consequently, we were not surprised that the functioning of the parental pair remained unchanged after the treatment.
Finally, the treatment was not found to change triadic functioning. We can assume that a 6-month treatment is not long enough to modify interactions at the triadic level.
The lack of impact of the treatment on triadic functioning could also be explained by the fact that dyadic relations were highly impaired in our sample of adolescents; these were indeed patients whose psychopathological conditions were severe enough to warrant intervention by tertiary-level services.
This study has some limitations. First, the relatively small sample size (due to the need to include only triads with complete data and to the exclusion of patients already receiving psychotherapy) limits the generalizability of the findings. Future research in larger samples is needed. Second, we focused on REDs because the families of patients affected by these conditions frequently show dysfunctional family relations (15, 67). Future studies should investigate whether our results extend to other eating disorders. Finally, in line with the descriptive aim of this study, no control groups were included. Future research is warranted to address the relative effect of this multidisciplinary treatment program compared with care as usual and with other family- or patient-centered interventions.
Since the psychopathological organization underlying REDs can vary, the therapeutic approach should be tailored to the specific features of the single patient. In particular, in the most severe cases, particular attention should be paid to parental (dyadic) and triadic or family interactions, but psychotherapy for patients only (individual or group) may also be very useful. We strongly suggest that a flexible therapeutic approach allowing integrated interventions (psychodynamic psychotherapy for patients, support for the parental role, and triadic or family intervention) might better meet the needs of the most impaired patients referred to tertiary care services. The LTPc may help clinicians to improve their understanding of dysfunctional family interactions and even uncover potential protective factors that might be further exploited to enhance the efficacy of the family intervention in RED patients (15). In addition, performing the LTPc after the treatment may assist the clinical decision-making process. For example, its findings may support the decision to continue with the current treatment or allow the treatment to be tailored to the needs of the family, perhaps suggesting a less-intensive program of treatment in order to obtain a better balance of family psychological and economic resources.
The raw data supporting the conclusions of this article will be made available upon reasonable requests to the corresponding author.
The present study was reviewed and approved by Ethics Committee of the Policlinico San Matteo in Pavia, Italy (P-20170016006). Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
MM designed the study. MO, CR, MCr, MCC, and VZ collected data. LP conducted statistical analyses. MCh and RB provided scientific supervision. All authors contributed to the drafting of the manuscript and agreed on the final version to be submitted for publication.
This study was supported by Italian Ministry of Health (Ricerca Corrente 2020).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Authors are thankful to the colleagues of the Child Neurology and Psychiatry Unit and to the patients and their parents who took part in this study.
Luca Capone, Chiara Coci, Elisabetta Zerbi, Alice Busca, Maria Sabella, Lucia Racioppi.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.653047/full#supplementary-material
1. Smink FRE, Van Hoeken D, Hoek HW. Epidemiology of eating disorders: incidence, prevalence and mortality rates. Curr Psychiatry Rep. (2012) 14:406–14. doi: 10.1007/s11920-012-0282-y
2. Hoek HW. Review of the worldwide epidemiology of eating disorders. Curr Opin Psychiatry. (2016) 29:336–9. doi: 10.1097/YCO.0000000000000282
3. Keski-Rahkonen A, Mustelin L. Epidemiology of eating disorders in Europe: prevalence, incidence, comorbidity, course, consequences, and risk factors. Curr Opin Psychiatry. (2016) 29:340–5. doi: 10.1097/YCO.0000000000000278
4. National Collaborating Centre for Mental Health (UK). Eating Disorders: Core Interventions in the Treatment and Management of Anorexia Nervosa, Bulimia Nervosa and Related Eating Disorders. Leicester: British Psychological Society (2004).
5. Rikani AA, Choudhry Z, Choudhry AM, Ikram H, Asghar MW, Kajal D, et al. A critique of the literature on etiology of eating disorders. Ann Neurosci. (2013) 20:157–61. doi: 10.5214/ans.0972.7531.200409
6. Gutiérrez T, Espinoza P, Penelo E, Mora M, González ML, Rosés R, et al. Association of biological, psychological and lifestyle risk factors for eating disturbances in adolescents. J Health Psychol. (2015) 20:839–49. doi: 10.1177/1359105315577302
7. Lock J, La Via MC. Practice parameter for the assessment and treatment of children and adolescents with eating disorders. J Am Acad Child Adolesc Psychiatry. (2015) 54:412–25. doi: 10.1016/j.jaac.2015.01.018
8. Dell'Osso L, Abelli M, Carpita B, Pini S, Castellini G, Carmassi C, et al. Historical evolution of the concept of anorexia nervosa and relationships with orthorexia nervosa, autism, and obsessive-compulsive spectrum. Neuropsychiatr Dis Treat. (2016) 12:1651–60. doi: 10.2147/NDT.S108912
9. McDermott BM, Batik M, Roberts L, Gibbon P. Parent and child report of family functioning in a clinical child and adolescent eating disorders sample. Aust N Z J Psychiatry. (2002) 36:509–14. doi: 10.1046/j.1440-1614.2002.01043.x
10. Gillett KS, Harper JM, Larson JH, Berrett ME, Hardman RK. Implicit family process rules in eating-disordered and non-eating- disordered families. J Marital Fam Ther. (2009) 35:159–74. doi: 10.1111/j.1752-0606.2009.00113.x
11. Sim LA, Homme JH, Lteif AN, Vande Voort JL, Schak KM, Ellingson J. Family functioning and maternal distress in adolescent girls with anorexia nervosa. Int J Eat Disord. (2009) 42:531–9. doi: 10.1002/eat.20654
12. Cerniglia L, Cimino S, Tafà M, Marzilli E, Ballarotto G, Bracaglia F. Family profiles in eating disorders: family functioning and psychopathology. Psychol Res Behav Manag. (2017) 10:305–12. doi: 10.2147/PRBM.S145463
13. Malagoli Togliatti M, Mazzoni S. Osservare, valutare, e sostenere la relazione genitori-figli. Il Lausanne Trilogue Play clinico (Observe, evaluate, and support the parent-child relationship. The clinical Lausanne Trilogue Play). Milano: Raffaello Cortina Editore (2006).
14. Balottin L, Mannarini S, Mensi MM, Chiappedi M, Gatta M. Triadic interactions in families of adolescents with anorexia nervosa and families of adolescents with internalizing disorders. Front Psychol. (2017) 7:e02046. doi: 10.3389/fpsyg.2016.02046
15. Mensi MM, Balottin L, Rogantini C, Orlandi M, Galvani M, Figini S, et al. Focus on family functioning in anorexia nervosa: new perspectives using the Lausanne Trilogue Play. Psychiatry Res. (2020) 288:112968. doi: 10.1016/j.psychres.2020.112968
16. Criscuolo M, Laghi F, Mazzoni S, Castiglioni MC, Vicari S, Zanna V. How do families of adolescents with anorexia nervosa coordinate parenting? J Child Fam Stud. (2020) 29:2542–51. doi: 10.1007/s10826-020-01740-2
17. Balottin L, Mannarini S, Mensi MM, Chiappedi M, Balottin U. Are family relations connected to the quality of the outcome in adolescent anorexia nervosa? An observational study with the Lausanne Trilogue Play. Clin Psychol Psychother. (2018) 25:785–96. doi: 10.1002/cpp.2314
18. Godart N, Berthoz S, Curt F, Perdereau F, Rein Z, Wallier J, et al. A randomized controlled trial of adjunctive family therapy and treatment as usual following inpatient treatment for anorexia nervosa adolescents. PLoS ONE. (2012) 7:e28249. doi: 10.1371/journal.pone.0028249
19. Duclos J, Dorard G, Berthoz S, Curt F, Faucher S, Falissard B, et al. Expressed emotion in anorexia nervosa: what is inside the “black box”? Compr Psychiatry. (2014) 55:71–9. doi: 10.1016/j.comppsych.2013.10.002
20. Couturier J, Kimber M, Szatmari P. Efficacy of family-based treatment for adolescents with eating disorders: a systematic review and meta-analysis. Int J Eat Disord. (2013) 46:3–11. doi: 10.1002/eat.22042
21. Horesh N, Sommerfeld E, Wolf M, Zubery E, Zalsman G. Father-daughter relationship and the severity of eating disorders. Eur Psychiatry. (2015) 30:114–20. doi: 10.1016/j.eurpsy.2014.04.004
22. Holtom-Viesel A, Allan S. A systematic review of the literature on family functioning across all eating disorder diagnoses in comparison to control families. Clin Psychol Rev. (2014) 34:29–43. doi: 10.1016/j.cpr.2013.10.005
23. Sepulveda AR, Kyriacou O, Treasure J. Development and validation of the accommodation and enabling scale for eating disorders (AESED) for caregivers in eating disorders. BMC Health Serv Res. (2009) 9:171. doi: 10.1186/1472-6963-9-171
24. American Psychiatric Association. American Psychiatric Association Practice Guidelines for the Treatment of Psychiatric Disorders: Compendium 2006. American Psychiatric Publishing (2006).
25. Hay P, Chinn D, Forbes D, Madden S, Newton R, Sugenor L, et al. Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for the treatment of eating disorders. Aust N Z J Psychiatry. (2014) 48:977–1008. doi: 10.1177/0004867414555814
26. Espie J, Eisler I. Focus on anorexia nervosa: modern psychological treatment and guidelines for the adolescent patient. Adolesc Health Med Ther. (2015) 6:9. doi: 10.2147/ahmt.s70300
27. Herpertz-Dahlmann B. Adolescent eating disorders: update on definitions, symptomatology, epidemiology, and comorbidity. Child Adolesc Psychiatr Clin N Am. (2015) 24:177–96. doi: 10.1016/j.chc.2014.08.003
28. Zanna V, Castiglioni MC, Criscuolo M, Chianello I, Elisei M, Cinelli G, et al. Day-Hospital multifocal integrated treatment for anorexia nervosa in adolescents: a one-year follow-up. J Child Fam Stud. (2017) 26:1460–71. doi: 10.1007/s10826-017-0666-z
29. Brockmeyer T, Friederich HC, Schmidt U. Advances in the treatment of anorexia nervosa: a review of established and emerging interventions. Psychol Med. (2018) 48:1228–56. doi: 10.1017/S0033291717002604
30. Le Grange D, Eisler I. Family Interventions in Adolescent Anorexia Nervosa. Child Adolesc Psychiatr Clin N Am. (2009) 18:159–73. doi: 10.1016/j.chc.2008.07.004
31. Murray SB, Le Grange D. Family therapy for adolescent eating disorders: an update. Curr Psychiatry Rep. (2014) 16:447. doi: 10.1007/s11920-014-0447-y
32. Fisher CA, Skocic S, Rutherford KA, Hetrick SE. Family therapy approaches for anorexia Nervosa. Cochrane Database Syst Rev. (2019) 2019:CD004780. doi: 10.1002/14651858.CD004780.pub4
33. Le Grange D, Lock J, Loeb K, Nicholls D. Academy for eating disorders position paper: the role of the family in eating disorders. Int J Eat Disord. (2010) 43:1–5. doi: 10.1002/eat.20751
34. Lock J. Evaluation of family treatment models for eating disorders. Curr Opin Psychiatry. (2011) 24:274–9. doi: 10.1097/YCO.0b013e328346f71e
35. Lock J, Robinson A, Sadeh-Sharvit S, Rosania K, Osipov L, Kirz N, et al. Applying family-based treatment (FBT) to three clinical presentations of avoidant/restrictive food intake disorder: similarities and differences from FBT for anorexia nervosa. Int J Eat Disord. (2019) 52:439–46. doi: 10.1002/eat.22994
36. Morgan HG, Hayward AE. Clinical assessment of anorexia nervosa. The Morgan-Russell outcome assessment schedule. Br J Psychiatry. (1988) 152:367–71. doi: 10.1192/bjp.152.3.367
37. Jeammet P, Brechon G, Payan C, Gorge A, Fermanian J. Le devenir de l'anorexie mentale: une étude prospective de 129 patients évalués au moins 4 ans après leur première admission [The outcome of anorexia nervosa: a prospective study of 129 patients evaluated at least 4 years after their first admission]. Psychiatr l'Enfant. (1991) 34:381–442.
38. Wallin U, Kronvall P. Anorexia nervosa in teenagers: change in family function after family therapy, at 2-year follow-up. Nord J Psychiatry. (2002) 56:363–9. doi: 10.1080/080394802760322132
39. Ciao AC, Accurso EC, Fitzsimmons-Craft EE, Lock J, Le Grange D. Family functioning in two treatments for adolescent anorexia nervosa. Int J Eat Disord. (2015) 48:81–90. doi: 10.1002/eat.22314
40. Fitzpatrick KK, Moye A, Hoste R, Lock J, Le Grange D. Adolescent focused psychotherapy for adolescents with anorexia nervosa. J Contemp Psychother. (2010) 40:31–9. doi: 10.1007/s10879-009-9123-7
41. Wallis A, Miskovic-Wheatley J, Madden S, Rhodes P, Crosby RD, Cao L, et al. How does family functioning effect the outcome of family based treatment for adolescents with severe anorexia nervosa? J Eat Disord. (2017) 5:55. doi: 10.1186/s40337-017-0184-9
42. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association (2013).
43. Kaufman J, Birmaher B, Axelson D, Pereplitchikova F, Brent D, Ryan N. Schedule for Affective Disorders and Schizophrenia for School-Aged Children: Present and Lifetime Version (K-SADS-PL) DSM-5. New Heaven, CT: Child and Adolescent Research and Education (2016).
44. Wechsler D. Wechsler Intelligence Scale for Children-Fourth Edition (WISC-IV). 4th ed. Firenze: Giunti Organizzazioni Speciali (2003).
45. Wechsler D. Wechsler Adult Intelligence Scale-Fourth edition (WAIS-IV). 4th ed. Firenze: Giunti Organizzazioni Speciali (2008).
46. National Institute for Clinical Excellence (NICE). Eating disorders: recognition and treatment. Full Guidel. (2017) 62:656–62.
47. Foulkes SH. Introduzione alla psicoterapia gruppoanalitica. Roma: Edizioni Universitaria Romane (1991).
49. Hughes EK, Sawyer SM, Loeb KL, Le Grange D. Parent-focused treatment. In: Loeb KL, editor. Family Therapy for Adolescent Eating and Weight Disorders: New Applications. Milton Park, UK: Routledge (2015). p. 59–71.
50. Duclos J, Dorard G, Cook-Darzens S, Curt F, Faucher S, Berthoz S, et al. Predictive factors for outcome in adolescents with anorexia nervosa: to what extent does parental expressed emotion play a role? Jiménez-Murcia S, editor. PLoS ONE. (2018) 13:e0196820. doi: 10.1371/journal.pone.0196820
51. Zelenko M, Benham A. Videotaping as a therapeutic tool in psychodynamic infant- parent therapy. Infant Ment Health J. (2000) 21:192–203. doi: 10.1002/1097-0355(200007)21:3<>1.0.CO;2-G
52. Mazzoni S, Lavadera AL. Le Jeu Trilogique de Lausanne (LTP) en clinique: application dans le contexte d'interventions de soutien à la relation parents-enfants [1] | Cairn.info. In: Favez N, Frascarolo-Moutinot F, and Tissot H, editors. Naître et grandir au sein de la triade: Le développement de l'alliance familiale. Bruxelles: De Boeck Supérieur (2013). p. 193–210.
53. Keren M. Using the LTP in an infant mental health unit. In: Leipzig, Germany: Paper presented at the World Association for Infant Mental Health, 12th World Congress. Leipzig (2010).
54. Lavadera AL, Laghi F, Togliatti MM, Malagoli Togliatti M, Togliatti MM. Assessing family coordination in divorced families. Am J Fam Ther. (2011) 39:277–91. doi: 10.1080/01926187.2010.539479
55. Mazzoni S, Lavadera AL, Di Benedetto R, Criscuolo M, Mangano C. Parenting coalitions: coparenting and toddler's interactive styles. Psicologia Clinica dello Sviluppo. (2015) 19:79–100. doi: 10.1449/79740
56. Ashton MC. Individual Differences and Personality. 3rd ed. London: Academic Press (2017). p. 1–416.
57. Roberts BW, DelVecchio WF. The rank-order consistency of personality traits from childhood to old age: a quantitative review of longitudinal studies. Psychol Bull. (2000) 126:3–25. doi: 10.1037/0033-2909.126.1.3
58. Balottin U, Ferri M, Racca M, Rossi M, Rossi G, Beghi E, et al. Psychotherapy versus usual care in pediatric migraine and tension-type headache: a single-blind controlled pilot study. Ital J Pediatr. (2014) 40:6. doi: 10.1186/1824-7288-40-6
59. Duhig AM, Phares V, Birkeland RW. Involvement of fathers in therapy: a survey of clinicians. Prof Psychol Res Pract. (2002) 33:389–95. doi: 10.1037//0735-7028.33.4.389
60. Hecker LL. Where is dad?: 21 ways to involve fathers in family therapy. J Fam Psychother. (1991) 2:31–45. doi: 10.1300/j085V02N02_03
61. Jones CJ, Leung N, Harris G. Father-daughter relationship and eating psychopathology: the mediating role of core beliefs. Br J Clin Psychol. (2006) 45:319–30. doi: 10.1348/014466505X53489
62. Hay P, Mitchison D, Collado AEL, González-Chica DA, Stocks N, Touyz S. Burden and health-related quality of life of eating disorders, including avoidant/restrictive food intake disorder (ARFID), in the Australian population. J Eat Disord. (2017) 5:1–10. doi: 10.1186/s40337-017-0149-z
63. Kyriacou O, Treasure J, Schmidt U. Understanding how parents cope with living with someone with anorexia nervosa: modelling the factors that are associated with carer distress. Int J Eat Disord. (2008) 41:233–42. doi: 10.1002/eat.20488
64. Whitney J, Murphy T, Landau S, Gavan K, Todd G, Whitaker W, et al. A practical comparison of two types of family intervention: an exploratory RCT of family day workshops and individual family work as a supplement to inpatient care for adults with anorexia nervosa. Eur Eat Disord Rev. (2012) 20:142–50. doi: 10.1002/erv.1076
65. Anastasiadou D, Medina-Pradas C, Sepulveda AR, Treasure J. A systematic review of family caregiving in eating disorders. Eat Behav. (2014) 15:464–77. doi: 10.1016/j.eatbeh.2014.06.001
66. Criscuolo M, Marchetto C, Chianello I, Cereser L, Castiglioni MC, Salvo P, et al. Family functioning, coparenting, and parents' ability to manage conflict in adolescent anorexia nervosa subtypes. Fam Syst Heal. (2020) 38:151–61. doi: 10.1037/fsh0000483
Keywords: adolescence, eating disorders, family functioning, Lausanne Trilogue Play, family therapy, multi-professional treatment
Citation: Mensi MM, Orlandi M, Rogantini C, Provenzi L, Chiappedi M, Criscuolo M, Castiglioni MC, Zanna V and Borgatti R (2021) Assessing Family Functioning Before and After an Integrated Multidisciplinary Family Treatment for Adolescents With Restrictive Eating Disorders. Front. Psychiatry 12:653047. doi: 10.3389/fpsyt.2021.653047
Received: 13 January 2021; Accepted: 16 April 2021;
Published: 04 June 2021.
Edited by:
Enrica Marzola, University of Turin, ItalyReviewed by:
Jennifer Couturier, McMaster University, CanadaCopyright © 2021 Mensi, Orlandi, Rogantini, Provenzi, Chiappedi, Criscuolo, Castiglioni, Zanna and Borgatti. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Matteo Chiappedi, bWF0dGVvLmNoaWFwcGVkaUB1bmlwdi5pdA==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.