
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 05 May 2021
Sec. Forensic Psychiatry
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.645927
This article is part of the Research TopicTherapeutic Process and Treatment Evaluation in Forensic Psychiatry and PrisonView all 12 articles
This study aimed to evaluate the predictive validity and reliability of the Short-Term Assessment of Risk and Treatability (START) in the context of the Japanese forensic probation service. START is a structured professional judgement guide for risk domains concerning negative behaviors such as violence, self-harm, suicide, substance abuse, unauthorized leave, victimization, and self-neglect. In this study, rehabilitation coordinators evaluated community-dwelling patients who were treated under the Medical Treatment and Supervision Act at baseline and followed-up for 6 months. The results revealed that START vulnerability scores significantly predicted self-harm, suicide, physical aggression, substance abuse, and self-neglect. START strength scores predicted physical violence and unauthorized leave. Specific risk estimates predicted physical violence and self-neglect. Risk judgement for future substance use may require adjustments for cultural differences, because of the lower prevalence in Japan. These results suggest that START offers a feasible and valid tool that allows clinicians to plan treatment and promote recovery of forensic patients in Japan.
Violence is not the only negative behavior in the prognosis of Mentally Disordered Offenders (MDOs). Suicide, self-harm, substance abuse, self-neglect, and victimization have all been found to occur at higher rates among psychiatric patients than among the general population (1–4). Risk management of these problem behaviors is a routine practice in psychiatry. Logically, risk management of such behaviors requires risk assessment tools for as many problem behaviors as there are. However, risk factors underlying different problem behaviors are known to overlap (5). A tool that can aggregate assessment items and assess the risk of worrisome outcomes for each patient would therefore be desirable.
The purpose of risk assessment in clinical practice is to guide treatment planning to support the recovery of the individual. One important perspective to support recovery in mental health is the focus on strength (6, 7). Focusing on strength has been shown to not only restore self-esteem and improve quality of life in subjects, but also improve social functioning and reduce risk behaviors (6). Strength is a protective factor that mitigates risk (8).
In the past decade, the interest in incorporating protective factors into the risk assessment and management of violence has been growing. Relevant clinical research has developed various risk measures that include protective factors, such as the Short-Term Assessment of Risk and Treatability (START) (8, 9), Structured Assessment of Violence Risk in Youth (SAVRY) (10), and Structured Assessment of Protective Factors for Violence Risk (SAPROF) (11).
The START is a risk assessment guide for a series of negative outcomes in psychiatric patients, such as violence, self-harm, suicide, self-neglect, victimization, substance abuse, and unauthorized leave. This guide was developed as a short-term risk assessment for people with mental illness, substance use, and personality disorders. Unlike traditional vulnerability-focused approaches, START assesses empirically selected dynamic factors comprising both protective factors (“strengths”) and risk factors (“vulnerabilities”), and judges the risk of seven negative outcomes occurring over a pre-determined period, as specific risk estimates (SREs). The negative outcomes of interest are: violence, self-harm, suicide, substance use, unauthorized leave, victimization, and self-neglect.
According to a systematic review of START, vulnerability score, strength score, and SREs have all been shown to have predictive validity for violent outcomes (12). With regard to outcomes other than violence, a meta-analysis suggested that although neither vulnerability nor strength scores predicted self-harm, the SRE for self-harm did offer predictive validity (12). Only one study has reported adequate predictive validities for unauthorized leave and substance use, although predictive validities for self-neglect and victimization were not significant (13).
Results from these previous studies were promising, but further evaluation may be necessary for at least two reasons. First, past studies of START were conducted in Western countries [e.g., Canada, Norway, Australia, the United Kingdom (UK), the United States, the Netherlands]. Cross-cultural generalization of START may be crucial to clarify whether the same risk and strength factors can predict negative outcomes in different cultures, such as Asian samples.
Second, most studies have examined the predictive validity of START in inpatient populations. For example, Nicholls et al. reported that case managers used START to assess patients in the community, but did not investigate its predictive validity (14). Another study tested the psychometric characteristics of START for 301 outpatient forensic psychiatric patients in the Netherlands (15). They found that for the 6-month follow-up, structured professional judgement ratings by the clinicians modestly improved the prediction of future violence beyond a summation of historical, vulnerability, and strength scores. To the best of our knowledge, no other studies have investigated the predictive validity of START in forensic outpatients.
In summary, research to date on the START has focused mainly on inpatients in Western countries. As START adopts a Structured Professional Judgement (SPJ) approach (16), the items were selected by a comprehensive review of the literature on risk factors for negative outcomes in psychiatric patients (8). Unlike actuarial risk assessments, item selection did not rely on a specific sample on which the assessment was developed. We thus expect that the predictive accuracy may be generalizable to other samples, such as Asian countries. To expand the literature on START, this study provides a first examination of the predictive validity of START in a Japanese forensic outpatient context.
This study comprised a 6-month prospective study of outpatients in the community in Japan under the “Act for the Medical Treatment and Supervision of Persons with Mental Disorders Who Caused Serious Harm,” commonly called the “Medical Treatment and Supervision Act (MTSA).” The follow-up period of 6 months was selected for two reasons. First, a short term was required, as START was deliberately developed to assess short-term risk and treatability. Second, the period of follow-up had to be long enough for incidents to occur, as a past study showed that the rate of reoffending within 1 year after discharge was <3% among MTSA patients (17), and cosiderably low rate. Therefore, it was assumed better to follow up for 6 months rather than three, in order to increase the chance of collecting negative incident data.
The MTSA in Japan is a forensic mental health act for Mentally Disordered Offenders (MDOs) who have committed murder, severe injury, arson, robbery, rape, or indecent assault under a state of insanity or diminished criminal responsibility. The act was passed by the parliament in 2003 and came into effect in 2005. When MDOs are introduced to the MTSA system and are mandated by the district court as warranting treatment under the MTSA, they are allocated to receive either an inpatient treatment order or an outpatient treatment order (18). The MTSA stipulates that the outpatient treatment order can last up to 3 years and be prolonged up to 5 years in total under special circumstances, but no longer. Past studies have found that the total cumulative rate of reoffending after discharge was 2.5% (1.1–3.9%) at 1 year and 7.5% (4.6–10.4%) at 3 years. The rate of serious reoffending was 0.4% (0.18–0.99%) at 1 year and 2.0% (0.4–3.6%) at 3 years (17).
Patients were included when they had been given an MTSA outpatient treatment order by the district court and were dwelling in the community.
Exclusion criteria were as follows:
1). If the outpatient treatment order was known to expire within 6 months. The maximum MTSA outpatient treatment order is 5 years. Therefore, for example, if a patients' outpatient treatment had exceeded 4.5 years, it was apparent that the outpatient treatment order would expire before 6 months.
2). When the patient was under an MTSA outpatient treatment order, but was hospitalized in a psychiatric unit under the Mental Health and Welfare Act at Time 1. The MTSA stipulates that patients can be hospitalized under the Mental Health and Welfare Act for regular psychiatric care while remaining under the MTSA outpatient treatment order. Such patients were excluded from this study as their situation could not be considered to represent “living in the community.”
The START manual was translated into Japanese by the authors with formal written consent from the original authors. The first author had experience in the SPJ scheme and participated in a START workshop by the original authors prior to the beginning of the study.
Rehabilitation coordinators (RCs) were recruited in collaboration with the Mental Health Probation Planning Office in the Ministry of Justice. RCs are forensic probation officers who provide supervision and case management of MTSA patients. RCs regularly meet with MTSA patients, and hold care coordination meetings with the participation of related caregivers and agencies in the community. RCs gather information about the patient to monitor, supervise, and coordinate treatment efforts. RCs are responsible for collating any incident reports.
Those RCs who provided informed consent to participate in the study were provided with the Japanese START manual and received 1 day of training in scoring START. All training was provided by a clinical psychologist (first author). Training was conducted in eight regions regulated by the Regional Branch Bureau of Health and Welfare in Japan. After training, RCs were able to contact the first author for clarifications pertaining to the scoring of items in START. Only two of 102 RCs were trained in the use of any SPJ instrument prior to this study.
After START training, data collection was longitudinally implemented in two parts. At Time 1, RCs were asked to score the START of patients in their caseload who met the inclusion criteria for the study. RCs were required to use the START and estimate the risks of the seven negative outcomes during the 6 months subsequent to the assessment. Completed START summary sheets were then sent to the Mental Health Probation Planning Office. RCs were asked to maintain records of challenging behaviors from patients for the next 6 months as in routine practice. This information was to be posted to the problematic behavior form. At Time 2, 6 months after Time 1, RCs sent the problematic behavior forms to the Mental Health Probation Planning Office. All data sheets were anonymized in the Mental Health Probation Planning Office before being sent to the first author for analyses.
For each eligible patient, RCs completed START, and a sociodemographic face-sheet at Time 1, and the problematic behaviors form designed specifically for this study at Time 2.
Unlike traditional vulnerability-focused approaches, START assesses 20 empirically selected dynamic factors (Table 1) in terms of both protective factors (strengths) and risk factors (vulnerabilities). Raters can add up to two case-specific items. Protective and risk factors are rated independently on three levels: 0 = minimal or no vulnerability/strength; 1 = moderate vulnerability/strength; and 2 = high vulnerability/strength. The evaluator also identifies critical vulnerabilities and key strengths, signature risk signs, medical conditions, and histories of the seven negative outcomes. Finally, the evaluator rates the risk of each outcome occurring over a predetermined period on a scale of low, medium, and high. A rating of low risk indicates no or minimal risk, moderate indicates greater than average risk, and high indicates a relatively imminent and serious threat.
START has shown practical utility when incorporated into routine practice. Nicholls et al. (19) found excellent inter-rater reliability overall (intraclass correlation coefficient, ICC2 = 0.87, p < 0.001). Doyle et al. assessed START implementation, recruiting staff members of a medium secure forensic mental health service who had participated in the START training (20). They found that START took a mean of 25 min to complete, and 82.1% of assessments were completed in ≤30 min. Another study conducted in a UK medium secure hospital found that, by the second application of START, professionals were able to complete the assessment in 11.03 min (21). START was identified as a tool supporting best practice in managing violence as well as related risks among psychiatric patients in the UK (22).
This study excluded case-specific items from the analysis, because these were specific to individuals and not comparable between patients. Total scores on strength and vulnerability items were prorated to account for up to four missing items in accordance with the START manual (8). According to the recommendation in the START manual, assessments with more than five or more missing item data were excluded (8).
Outcome measures were problematic behaviors exhibited by the patient. Data collection was operationalized by asking RCs to write down the problematic behaviors and then to categorize each event into one of the following: self-harm, suicide, physical violence, substance abuse, victimization, self-neglect, unauthorized leave, or other challenging behaviors (free description). Data for other challenging behaviors (e.g., water intoxication) were not included in this study.
Data on age, sex, diagnosis (International Classification of Diseases, 10th edition (ICD-10) (23), index offense, and length of MTSA outpatient treatment were collected at Time 1. The information in patient records were transferred into the dataset. The diagnoses were decided by certified psychiatrists who implemented the court-ordered mental health examination for 3 months. The ICD-10 system is used for MTSA diagnoses. The mental health examination report was submitted to the district court to be reviewed in the process of making decisions about the case. In rare instances where the main diagnosis is proven to be different during the MTSA treatment, the diagnosis is renewed accordingly in the official patient records.
Receiver operating characteristic (ROC) analyses were used to examine the predictive validity of START Vulnerability and Strength scores, and SREs for the different challenging behavior incidents in the 6 months following the Time 1 evaluation. ROC analysis has been widely used in violence prediction research due to its independence from base rates (24). To quantify the ROC, area under the ROC curve (AUC) was calculated. Strength scores were inverted when conducting ROC analyses to compare predictive validity to the total vulnerability score and specific risk estimates. Spearman's rho between the START vulnerability score, strength score, and the number and type of problematic challenging behaviors was calculated. Cronbach's alpha was used to measure the internal consistency of START items. All analyses were conducted using SPSS version 21.0 software (IBM corporation, Armonk, NY).
In total, 102 RCs (57.6% of the total number of RCs in Japan at Time 1) were recruited to the study, of whom 18 were excluded owing to an absence of eligible patients in their caseload (Figure 1). At Time 1, a total of 235 START assessments were completed by 84 RCs. By Time 2, 6 months after initial assessment, two RCs declined to participate in the study, resulting in a decrease of six START assessments. Another START assessment was excluded due to a patient moving to another prefecture. As a result, 228 pairs of START assessment and problematic behavior forms were obtained. Based on the exclusion criterion of START assessments with more than five missing item scores, four patients were further excluded from the analysis based on recommendations in the START manual (8). Another 43 assessments were excluded as the client was hospitalized under the Mental Health and Welfare Act at Time 1. As a result, 181 pairs of START assessments from Time 1 and problematic behavior forms from Time 2, were analyzed in this study.
Table 2 shows descriptive characteristics of the study. The 181 eligible study subjects comprised predominantly men (79%) with a mean age of 43 years (range 24–86 years). The most frequent ICD-10 diagnosis was F2, schizophrenia (n = 141; 77.9%). The second most frequent was F1 (n = 19; 10.5%), Mental and Behavioral Disorders due to Psychoactive Substance Use. Concerning the index offense, murder, injury, and arson made up to ~90% of the total number. At Time 1, the average length of MTSA outpatient treatment was 14.46 months [standard deviation (SD) = 8.66 months]. Overall, the study sample did not significantly differ from the national MTSA sample in terms of distributions of gender, age at Time 1, diagnosis, or index offense (25).
In 6 months, 42 patients (23.2%) showed at least one START negative outcome (Table 3). The most commonly observed negative outcome was self-neglect, in 24 patients (13.2%). The least common risk outcomes were self-harm and victimization [two patients (1.10%) each]. No participants were rated as high risk for victimization or unauthorized leave. Mean vulnerability score was 12.52 (SD = 7.40) and mean strength score was 23.55 (SD = 7.90). Vulnerability score correlated negatively with strength score (Spearman's rho = −0.55, p < 0.01).
Table 4 shows the predictive accuracy (AUC) of baseline START assessment scores for problematic behaviors in the 6 months after scoring. An AUC > 0.71 was considered as a large effect, 0.64~0.70 as medium, and 0.56~0.63 as small (26).
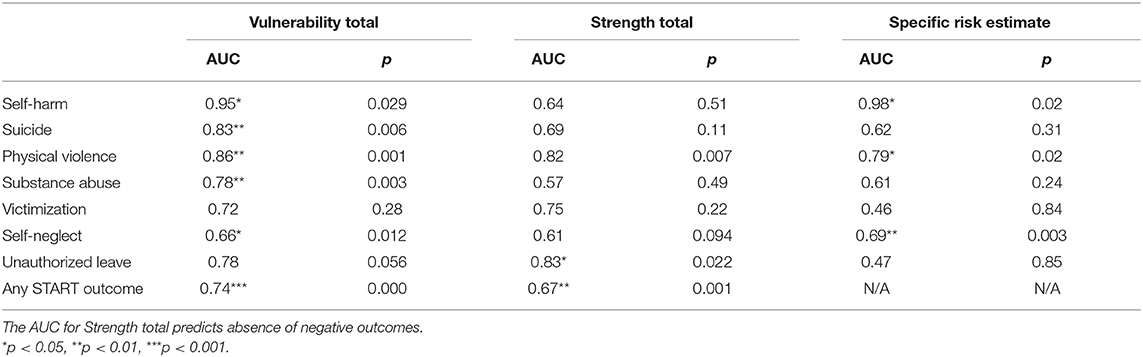
Table 4. Predictive accuracy (AUC) of baseline START assessment scores for problematic incidents in 6 months (n = 181).
The vulnerability score significantly predicted occurrences of self-harm (AUC = 0.95, p = 0.03), suicide (AUC = 0.83, p < 0.01), physical violence (AUC = 0.85, p < 0.01), and substance abuse (AUC = 0.78, p < 0.01) with a large effect size. Feedback from participating RCs revealed the difficulty of assessing the intent to die for a given suicide/self-harm event. We therefore produced a composite self-harm/suicide outcome and the AUC by vulnerability score was 0.86 (n = 7, p < 0.01).
The Strength score significantly predicted only the non-occurrence of physical violence (AUC = 0.82, p < 0.01) and unauthorized leave (AUC = 0.82, p < 0.01).
SREs significantly predicted self-harm (AUC = 0.98, p < 0.05) and physical violence (AUC = 0.79, p < 0.01) with a large effect size, and self-neglect with a medium effect size (AUC = 0.69, p < 0.01), but not suicide, substance abuse, victimization, or unauthorized leave.
Both vulnerability score and strength score were predictive of “any START negative outcomes” with a medium to large effect size (AUC = 0.74, p < 0.01 for vulnerability score; AUC = 0.67, p < 0.01 for strength score).
Vulnerability score correlated significantly with total number of incidents (Spearman's rho = 0.34, p < 0.01) and total types of incidents (Spearman's rho = 0.37, p < 0.01). Strength score also correlated significantly with the total number of incidents (Spearman's rho = −0.23, p < 0.01) and total types of incidents (Spearman's rho = −0.24, p < 0.01).
Cronbach's alpha for the standard 20 START items was 0.90 for vulnerability items and 0.91 for strength items.
This study appears to be the first to examine the validity of START in a prospective forensic sample living in the community and to explore the utility of START in Japan. Little research of this nature has been conducted outside North America and Europe.
START vulnerability score, strength score, and specific risk estimates all showed significant and high predictive validity for physical violence in the 6-month follow-up period. Past studies have consistently found that START was predictive of physical violence in 3–12 months (12, 27–32). START risk/vulnerability items for judging physical violence risk may thus also be generalizable to MDOs in Japan.
Vulnerability score showed predictive validity for both self-harm and suicide within 6 months, whereas strength score did not. O'Shea et al. (33) analyzed the predictive validity of START in an inpatient setting by combining self-harm and suicide, because their outcome data were derived from progress notes with a flag “self-harm/suicide” (33). This may reflect the difficulty in terms of clinical reality for distinguishing between deliberate self-harm with no intent to die and attempted suicide with intention to die (34). If this is true in inpatient settings, it is reasonable to assume that the difficulty would be larger in the community, where direct observation of patients' behaviors is much lower.
Our results found significant and sufficient AUCs in a 6-month follow-up period for the combined item of self-harm/suicide. Bearing in mind the significant and persistent risk of suicide following deliberate self-harm (35), relaxing the intention criteria may be more feasible in clinical settings, to judge combined risk estimates for self-harm/suicide. This is particularly true where the treated population consists primarily of individuals with psychosis, since these individuals are approximately six times more likely to die by suicide after a prior incident of deliberate self-harm (36).
Vulnerability scores, but not strength scores, were sufficiently predictive of substance abuse at 6 months. The vulnerability score outperformed the specific risk estimate for substance abuse. The distribution of risk estimates for substance use in this study was 162 patients with low risk (89.5%), 16 patients with medium risk (8.8%), and three patients with high risk (1.7%). However, actual incidents of substance abuse comprised nine cases (5%) in the 6-month follow-up period. This means that RCs tended to judge patients to be at a higher risk than they actual were (Fisher's exact test p = 0.004).
Past studies have documented that substance use tends to be a chronic condition where most patients need repeated treatment efforts (37). Therefore, when a patient is found to have a history of substance abuse, RCs might tend to consider and weigh this as evidence of elevated risk of further substance use. However, Japan has a low rate of drug use compared to other Western countries, such as the UK and European countries. For instance, according to a 2004 report from the World Health Organization, the 12-month prevalence of drug use disorders among male 15 years or older was 0.01% in Japan, markedly lower than the 1.29% in the UK and 1.14% in Canada (38). Our results suggest that the impact of historical substance use on future use may be mitigated in Japan because of the lower availability of drugs.
Making cultural adjustments when deciding on the impact of substance use may also be necessary for making clinical judgements regarding future violence in Japan. Past studies have repeatedly documented an effect of substance use on an elevated risk of violence in psychosis (39, 40). However, a recent study by Imai et al. (41) examined 420 Japanese patients with schizophrenia who had committed violent acts immediately prior to an emergency admission to a psychiatric hospital. Substance abuse and antisocial episodes were not recognized as significant violence-associated factors in that study. They speculated that this result was related to the markedly low rate of drug use in Japan (41). Taken together, evaluators in Japan should consider making cultural adjustments in weighing the impact of substance use when making clinical risk judgements. This is possible with START, which adopts an SPJ approach to risk assessment, where risks are estimated not by the total score, but by clinical judgements.
Inverted strength scores were predictive of future unauthorized leave, although vulnerability scores were not. This discrepancy could be attributed to the ambiguous definition of unauthorized leave in the community setting. For example, reported incidents have included temporary unauthorized leave (failing to report leaving) from a group home and unexplained disappearance for days where contact was impossible. Such instances of unauthorized leave may remain undetected in cases of independent living or when occurring between care coordination meetings.
Self-neglect was observed in 24 patients (13.3%), representing the most common START negative outcome in the study sample. Self-neglect was predicted by the vulnerability score and specific risk estimate, but not by the strength score. This was different from the observations of O'Shea et al. (12) who studied the predictive validity of START with inpatients and found neither vulnerability nor strength score predicted self-neglect. On the other hand, Marriott et al. reported different results that self-neglect in psychosis was predicted by both vulnerability score and strength score (42). As noted by Marriott et al. (42), the predictive validity of START for self-neglect may be influenced by the type of community setting. Our results may be reflective of Japanese MDOs residing in the community.
Only two incidents (1.1%) of victimization were reported in our sample during the 6-month follow-up. Neither START vulnerability score nor strength score predicted their occurrence. These low rates can be interpreted as follows: The first is the underreporting of victimization. According to the International Crime Victims Survey by the United Nations Interregional Crime and Justice Research Institute in 2000, the yearly prevalence of victimization in 1999 was 15.2% in Japan (43). When also considering that victimization is higher for people with severe mental illness than for the general population (44, 45), the extent of underreporting in our sample is apparent. The second interpretation is that the compulsory nature of MTSA outpatient treatment may have served to protect against supervision. This aligns with a review of the effects of compulsory community treatment by Kisely et al. (46), who found that people receiving compulsory community treatment were less likely to be victims of violent or non-violent crime. They speculated that the effect may be due to the intensity of treatment or its compulsory nature (46).
One of the assumptions of START is that risks overlap between negative outcomes (8). Vulnerability score correlated significantly with total number and types of START negative outcomes. Among the 42 patients who exhibited at least one START negative outcome within 6 months, 14 patients (34.14%) exhibited two or more types of START negative outcomes, supporting the assumption that risks overlap.
Japanese versions of START items exhibited high internal consistency (>0.90), comparable to those in past Western studies (19, 27, 47).
The fact that strength scores only showed moderately significant correlations with vulnerability scores suggests that START strengths do not merely represent the vulnerability/risk measure repeated and expressed in the opposite direction. This differed from the results described by Abidin et al. (27), where START vulnerability and strength scores were strongly and inversely correlated (r = −0.947) (27).
Strength score showed predictive validity only for physical violence and unauthorized leave. This was much less than that for the vulnerability score, which showed predictive validity for five of the seven outcomes. Two reasons may play roles in this difference. First, the vagueness of some START strength items may originate from the “lack of conceptual certitude around the relationship between protective and risk factors” (48). This reasoning may be supported by previous findings that assessment tools with separate items and unambiguous definitions for protective factors, such as SAPROF and SAVRY, tend to perform better in demonstrating incremental validity (49–51). Second, strength scores may be more predictive of positive results, such as job attainment and personal recovery, than merely non-negative results such as absence of violence. Our results may thus indicate the clinical utility of strength items as more relevant than risk estimates in guiding treatment planning.
This study shows several limitations that merit consideration when interpreting the results. First, inter-rater reliability was not determined in this study. All data were collected during the routine forensic probation practice of RCs, and it is not standard practice for MTSA patients to have two or more RCs in charge. Second, negative outcome data were collected from a single source, the RCs. Past studies have shown that detection of violence during follow-up increased steadily when combining methods (52). Our RCs obtained knowledge of forensic patients not only from direct contact with the patients in question, but also through care coordination meetings where multiple agencies and disciplines discuss the case. However, negative outcomes may still have been underreported. Aggression against psychiatric patients has been reported to show a tendency to be underreported (53), and the same conditions may have been present in the present study. This is important because the current study gathered outcome data for outpatients in the community, which is different from inpatient settings where outcome information is readily accessible and a strong obligation to record negative events is present. Future studies should ideally use collateral information on negative outcomes. Third, although the sample size of this study was the largest to date in validating risk assessment among forensic outpatients in Japan, the sample size was still too small to detect meaningful calculation of AUCs for victimization and unauthorized leave. Finally, although this study extended the evaluation of START to the outpatient population, the results remain limited to forensic psychiatric outpatients under MTSA in the community. The predictive validity of START in both forensic inpatients and general psychiatric patients in Japan remains unknown and is a target for future studies.
The present study has major implications in terms of the dissemination of START in forensic psychiatric practice in the community. We were able to demonstrate via a prospective study design that START is an assessment tool that can be applied in Japan, a non-Western country. To conclude, this study advances our understanding regarding the utilization of START by clinicians in planning treatment for patients that will not only reduce the risks of negative outcomes, but also enhance strengths to promote recovery in the community.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The study protocol was approved by the Ethics Committee of the National Center of Neurology and Psychiatry. All RCs provided written informed consent to participate in the research. Patients were notified of the study by posters in local probation offices and were guaranteed the right to opt out if they had any reservations about participating in the research. None of the participants opted out during the study period.
AK conceived and designed the present study. AK and MK collected data. AK, TK, and CF analyzed the data. AK drafted and revised the manuscript. AK and CF supervised the study. All authors approved the final manuscript.
This study was supported by National Center of Neurology and Psychiatry Intramural Research Grants for Neurological and Psychiatric Disorders (No. 24-3 and No. 1-3).
AK receive royalties from texts or books she has published on risk assessment.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We are deeply grateful to all participants and the regional Rehabilitation Coordinators who collaborated in the data collection.
1. Kooyman I, Dean K, Harvey S, Walsh E. Outcomes of public concern in schizophrenia. Br J Psychiatry Suppl. (2007) 50:s29–36. doi: 10.1192/bjp.191.50.s29
2. Hunt GE, Large MM, Cleary M, Lai HMX, Saunders JB. Prevalence of comorbid substance use in schizophrenia spectrum disorders in community and clinical settings, 1990-2017: systematic review and meta-analysis. Drug Alcohol Depend. (2018) 191:234–58. doi: 10.1016/j.drugalcdep.2018.07.011
3. Jayatilleke N, Hayes RD, Chang CK, Stewart R. Acute general hospital admissions in people with serious mental illness. Psychol Med. (2018) 48:2676–83. doi: 10.1017/S0033291718000284
4. Yates K, Lång U, Cederlöf M, Boland F, Taylor P, Cannon M, et al. Association of psychotic experiences with subsequent risk of suicidal ideation, suicide attempts, and suicide deaths: a systematic review and meta-analysis of longitudinal population studies. JAMA Psychiatry. (2019) 76:180–9. doi: 10.1001/jamapsychiatry.2018.3514
5. Wilkins N, Myers L, Kuehl T, Bauman A, Hertz M. Connecting the dots: state health department approaches to addressing shared risk and protective factors across multiple forms of violence. J Public Health Manag Pract. (2018) 24(Suppl. 1):S32–41. doi: 10.1097/PHH.0000000000000669
6. Xie H. Strengths-based approach for mental health recovery. Iranian J Psychiatry Behav Sci. (2013) 7:5–10.
7. Isaacs AN, Sutton K, Beauchamp A. PERSPECTIVES: recovery oriented services for persons with severe mental illness can focus on meeting needs through care coordination. J Mental Health Policy Econ. (2020) 23:55–60.
8. Webster CD, Martin ML, Brink J, Nicholls TL, Desmarais SL. Manual for the Short-Term Assessment of Risk and Treatability. Coquitlam, BC: British Columbia Mental Health and Addiction Services (2009).
9. Webster CD, Martin ML, Brink J, Nicholls TL, Middleton C. The Short-Term Assessment of Risk and Treatability (START). Coquitlam, BC: Forensic Psychiatric Services Commission. (2004).
10. Borum R, Bartel P, Forth A. Manual for the Structured Assessment for Violence Risk in Youth (SAVRY). Odessa, FL: Psychological Assessment Resources (2006).
11. de Vogel V, de Ruiter C, Bouman Y, de Vries Robbe M. SAPROF. Guidelines for the Assessment of Protective Factors for Violence Risk. Utrecht: Forum Educatief (2009).
12. O'Shea LE, Dickens GL. Short-term assessment of risk and treatability (START): systematic review and meta-analysis. Psychol Assess. (2014) 26:990–1002. doi: 10.1037/a0036794
13. Braithwaite E, Charette Y, Crocker A, Reyes A. The predictive validity of clinical ratings of the Short-Term Assessment of Risk and Treatability (START). Int J Forensic Mental Health. (2010) 9:271–81. doi: 10.1080/14999013.2010.534378
14. Nicholls TL, Petersen KL, Brink J, Webster CD. A clinical and risk profile of forensic psychiatric patients: Treatment team STARTs in a Canadian service. Int J Forensic Mental Health. (2011) 10:187–99. doi: 10.1080/14999013.2011.600234
15. Troquete NA, van den Brink RH, Beintema H, Mulder T, van Os TW, Schoevers RA, et al. Predictive validity of the Short-Term Assessment of Risk and Treatability for violent behavior in outpatient forensic psychiatric patients. Psychol Assess. (2015) 27:377–91. doi: 10.1037/a0038270
16. Hart SD, Douglas KS, Guy LS. The structured professional judgement approach to violence risk assessment: Origins, nature, and advances. In: Boer DP, editor. The Wiley Handbook on the Theories, Assessment and Treatment of Sexual Offending. Wiley-Blackwell (2016). p.643–66. doi: 10.1002/9781118574003.wattso030
17. Nagata T, Tachimori H, Nishinaka H, Takeda K, Matsuda T, Hirabayashi N. Mentally disordered offenders discharged from designated hospital facilities under the medical treatment and supervision act in Japan: Reoffending and readmission. Crim Behav Ment Health. (2019) 29:157–67. doi: 10.1002/cbm.2117
18. Fujii C, Fukuda Y, Ando K, Kikuchi A, Okada T. Development of forensic mental health services in Japan: working towards the reintegration of offenders with mental disorders. Int J Ment Health Syst. (2014) 8:21. doi: 10.1186/1752-4458-8-21
19. Nicholls TL, Brink J, Desmarais SL, Webster CD, Martin ML. The Short-Term Assessment of Risk and Treatability (START): a prospective validation study in a forensic psychiatric sample. Assessment. (2006) 13:313–27. doi: 10.1177/1073191106290559
20. Doyle M, Lewis G, Brisbane M. Implementing the Short-Term Assessment of Risk and Treatability (START) in a forensic mental health service. Psyhiatric Bulletin. (2008) 32:406–8. doi: 10.1192/pb.bp.108.019794
21. Quinn R, Miles H, Kinane C. The Validity of the Short-Term Assessment of Risk and Treatability (START) in a UK medium secure forensic mental health service. Int J Forensic Mental Health. (2013) 12:215–24. doi: 10.1080/14999013.2013.832714
23. World Health Organization. ICD-10: International Statistical Classification of Diseases and Related Health Problems: Tenth Revision. 2nd ed. World Health Organization (2004). Available online at: https://apps.who.int/iris/handle/10665/42980
24. Rice ME, Harris GT. Violent recidivism: assessing predictive validity. J Consult Clin Psychol. (1995) 63:737–48. doi: 10.1037/0022-006X.63.5.737
25. Ando K, Soshi T, Nakazawa K, Noda T, Okada T. Risk factors for problematic behaviors among forensic outpatients under the medical treatment and supervision act in Japan. Front Psychiatry. (2016) 7:144. doi: 10.3389/fpsyt.2016.00144
26. Rice ME, Harris GT. Comparing effect sizes in follow-up studies: ROC Area, Cohen's d, and r. Law Hum Behav. (2005) 29:615–20. doi: 10.1007/s10979-005-6832-7
27. Abidin Z, Davoren M, Naughton L, Gibbons O, Nulty A, Kennedy HG. Susceptibility (risk and protective) factors for in-patient violence and self-harm: prospective study of structured professional judgement instruments START and SAPROF, DUNDRUM-3 and DUNDRUM-4 in forensic mental health services. BMC Psychiatry. (2013) 13:197. doi: 10.1186/1471-244X-13-197
28. Desmarais SL, Nicholls TL, Wilson CM, Brink J. Using dynamic risk and protective factors to predict inpatient aggression: reliability and validity of START assessments. Psychol Assess. (2012) 24:685–700. doi: 10.1037/a0026668
29. Dickens GL, O'Shea LE. How short should short-term risk assessment be? Determining the optimum interval for START reassessment in a secure mental health service. J Psychiatr Ment Health Nurs. (2015) 22:397–406. doi: 10.1111/jpm.12232
30. O'Shea LE, Dickens GL. Predictive validity of the START for unauthorised leave and substance abuse in a secure mental health setting: a pseudo-prospective cohort study. Int J Nurs Stud. (2015) 52:970–9. doi: 10.1016/j.ijnurstu.2015.02.007
31. Troquete NA, van den Brink RH, Beintema H, Mulder T, van Os TW, Schoevers RA, et al. Risk assessment and shared care planning in out-patient forensic psychiatry: cluster randomised controlled trial. Br J Psychiatry. (2013) 202:365–71. doi: 10.1192/bjp.bp.112.113043
32. Wilson CM, Desmarais SL, Nicholls T, Brink J. The role of client strengths in assessments of violence risk using the short-term assessment of risk and treatability (START). Int J Forensic Mental Health. (2010) 9:282–93. doi: 10.1080/14999013.2010.534694
33. O'Shea LE, Picchioni MM, Dickens GL. The predictive validity of the short-term assessment of risk and treatability (START) for multiple adverse outcomes in a secure psychiatric inpatient setting. Assessment. (2016) 23:150–62. doi: 10.1177/1073191115573301
34. Gray NS, Benson R, Craig R, Davies H, Fitzgerald S, Huckle P, et al. The Short-Term Assessment of Risk and Treatability (START): a prospective study of inpatient behavior. Int J Forensic Mental Health. (2011) 14:132–46. doi: 10.1080/14999013.2011.631692
35. Hawton K, Zahl D, Weatherall R. Suicide following deliberate self-harm: long-term follow-up of patients who presented to a general hospital. Br J Psychiatry. (2003) 182:537–42. doi: 10.1192/bjp.182.6.537
36. Runeson B, Haglund A, Lichtenstein P, Tidemalm D. Suicide risk after nonfatal self-harm: a national cohort study, 2000-2008. J Clin Psychiatry. (2016) 77:240–6. doi: 10.4088/JCP.14m09453
37. Dennis M, Scott CK. Managing addiction as a chronic condition. Addict Sci Clin Pract. (2007) 4:45–55. doi: 10.1151/ascp074145
38. World Health Organization. Atlas on Substance Use 2010: Resources for the Prevention and Treatment of Substance Use Disorders 2010. World Health Organization (2017).
39. Boles SM, Miotto K. Substance abuse and violence: a review of the literature. Aggression Violent Behav. (2003) 8:155–74. doi: 10.1016/S1359-1789(01)00057-X
40. Swartz MS, Swanson JW, Hiday VA, Borum R, Wagner HR, Burns BJ. Violence and severe mental illness: the effects of substance abuse and nonadherence to medication. Am J Psychiatry. (1998) 155:226–31.
41. Imai A, Hayashi N, Shiina A, Sakikawa N, Igarashi Y. Factors associated with violence among Japanese patients with schizophrenia prior to psychiatric emergency hospitalization: a case-controlled study. Schizophr Res. (2014) 160:27–32. doi: 10.1016/j.schres.2014.10.016
42. Marriott R, O'Shea LE, Picchioni MM, Dickens GL. Predictive validity of the Short-Term Assessment of Risk and Treatability (START) for multiple adverse outcomes: the effect of diagnosis. Psychiatry Res. (2017) 256:435–43. doi: 10.1016/j.psychres.2017.07.009
43. Kesteren J, Mayhew P, Nieuwbeerta P. Criminal Victimisation in Seventeen Industrialised Countries: Key-findings from the 2000 International Crime Victims Survey. The Hague: Ministry of Justice (2000).
44. Anderson F, Howard L, Dean K, Moran P, Khalifeh H. Childhood maltreatment and adulthood domestic and sexual violence victimisation among people with severe mental illness. Soc Psychiatry Psychiatr Epidemiol. (2016) 51:961–70. doi: 10.1007/s00127-016-1244-1
45. Khalifeh H, Moran P, Borschmann R, Dean K, Hart C, Hogg J, et al. Domestic and sexual violence against patients with severe mental illness. Psychol Med. (2015) 45:875–86. doi: 10.1017/S0033291714001962
46. Kisely SR, Campbell LA, O'Reilly R. Compulsory community and involuntary outpatient treatment for people with severe mental disorders. Cochrane Database Syst Rev. (2017) 3:CD004408. doi: 10.1002/14651858.CD004408.pub5
47. Nonstad K, Nesset MB, Kroppan E, Petersen TW, Nottestad JA, Almvik R, et al. Predictive validity and other psychometric properties of the Short-Term Assessment of Risk and Treatability (START) in a Norwegian high secure hospital. Int J Forensic Mental Health. (2010) 9:294–9. doi: 10.1080/14999013.2010.534958
48. O'Shea LE, Dickens GL. Role of assessment components and recent adverse outcomes in risk estimation and prediction: use of the Short Term Assessment of Risk and Treatability (START) in an adult secure inpatient mental health service. Psychiatry Res. (2016) 240:398–405. doi: 10.1016/j.psychres.2016.04.068
49. de Vries Robbé M, de Vogel V, de Spa E. Protective factors for violence risk in forensic psychiatric patients: a retrospective validation study of the SAPROF. Int J Forensic Mental Health. (2011) 10:178–86. doi: 10.1080/14999013.2011.600232
50. Lodewijks HP, de Ruiter C, Doreleijers TA. The impact of protective factors in desistance from violent reoffending: a study in three samples of adolescent offenders. J Interpersonal Violence. (2010) 25:568–87. doi: 10.1177/0886260509334403
51. Lodewijks HP, Doreleijers TA, de Ruiter C, Borum R. Predictive validity of the Structured Assessment of Violence Risk in Youth (SAVRY) during residential treatment. Int J Law Psychiatry. (2008) 31:263–71. doi: 10.1016/j.ijlp.2008.04.009
52. Steadman HJ, Mulvey EP, Monahan J, Robbins PC, Appelbaum PS, Grisso T, et al. Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Arch Gen Psychiatry. (1998) 55:393–401. doi: 10.1001/archpsyc.55.5.393
Keywords: short-term assessment of risk and treatability (START), risk assessment, predictive validity, strength, structured professional judgement, forensic, outpatient
Citation: Kikuchi A, Soshi T, Kono T, Koyama M and Fujii C (2021) Validity of Short-Term Assessment of Risk and Treatability in the Japanese Forensic Probation Service. Front. Psychiatry 12:645927. doi: 10.3389/fpsyt.2021.645927
Received: 24 December 2020; Accepted: 06 April 2021;
Published: 05 May 2021.
Edited by:
Thomas Masterman, Karolinska Institutet (KI), SwedenReviewed by:
Marije E. Keulen-de Vos, Forensic Psychiatric Center de Rooyse Wissel, NetherlandsCopyright © 2021 Kikuchi, Soshi, Kono, Koyama and Fujii. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Akiko Kikuchi, b2tpa3VAYi1zdGFyLmpw
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.