- 1Department of Psychiatry, Dalhousie University, Halifax, NS, Canada
- 2Department of Psychology & Neuroscience, Dalhousie University, Halifax, NS, Canada
- 3Department of Psychology, St. Francis Xavier University, Antigonish, NS, Canada
- 4Department of Psychiatry, Université de Montréal, Montréal, PQ, Canada
Background: Fifteen to 25-year-olds are the age group most likely to misuse prescription drugs. Few studies have tested theory-driven models of adolescent risk for prescription drug misuse. Moreover, rarely are distinct pathways to different forms of prescription drug misuse considered.
Methods: We tested mediational paths from personality to mental health symptoms to prescription drug misuse, informed by etiological models of addiction. We specified pathways from particular personality traits to unique forms of prescription drug misuse via specific mental health symptoms. We used semi-longitudinal data collected across two waves of the Co-Venture Trial. Our sample included students from 31 Canadian high schools tested in Grade 9 (n = 3,024) and again in Grade 10 (n = 2,869; 95% retention). Personality (hopelessness, anxiety sensitivity, impulsivity, sensation seeking) was assessed in Grade 9. Mental health symptoms (depression, anxiety, ADHD, conduct disorder) and prescription drug misuse (opioids, sedatives/tranquilizers, stimulants) were assessed at both time points.
Results: Consistent with the negative affect regulation model, hopelessness was specifically associated with opioid misuse via depressive symptoms, and anxiety sensitivity was specifically associated with sedative/tranquilizer misuse via anxiety symptoms. Consistent with positive affect regulation, sensation seeking was directly associated with stimulant misuse. Consistent with the psychological dysregulation model, impulsivity was associated with stimulant misuse via ADHD symptoms. And consistent with the deviance proneness model, impulsivity was also associated with unconstrained (i.e., all three forms of) prescription drug misuse via conduct disorder symptoms.
Conclusions: Screening for adolescents high in hopelessness, anxiety sensitivity, sensation seeking, or impulsivity and providing them with personality-matched cognitive-behavioral interventions may be helpful in preventing or mitigating prescription drug misuse. Our results point to the specific mental health symptoms that are important to target in each of these personality-matched interventions.
Introduction
The National Survey on Drug Use and Mental Health defines prescription drug (PD) misuse as use of PDs “in any way that a doctor did not direct you to use them” including (a) use without a prescription of one's own; (b) use in greater amounts, for longer, or more often than prescribed; or (c) use in any other way that was not prescribed by a physician (1). Many young people consider PDs to be less harmful than illicit drugs (2). Due to their potency, potential for addiction, and overdose potential, however, PD misuse can be injurious or even fatal (3).
Of any age group, 15–25-year-olds are the most likely to misuse PDs (1). After cannabis, PDs are the drugs most commonly misused by North American adolescents (1, 4). One study showed that among adolescents aged 12–17, 5% reported past year PD misuse (5). PDs are readily accessible to adolescents through legitimate medical prescriptions (6), diversion (7, 8), and online pharmacies (9, 10). These trends are concerning for several reasons. First, prescription opiate misuse increases risk for serious injury (11), respiratory depression, and death (12). Moreover, the prevalence of adolescent misuse of sedatives/tranquilizers, including novel designer benzodiazepines, is significantly increasing (13–15), co-use with opioids is common (16), and sedative/tranquilizer-related deaths increased by 137% from 2007 to 2016 (17). Stimulant misuse is associated with adverse short-term (e.g., headaches, sleep problems, academic difficulties) and long-term effects [e.g., decreased likelihood of college graduation; (18)]. Adolescent-onset PD misuse is linked with elevated substance use disorder rates in adulthood (18, 19).
While several risk and protective factors for adolescent PD misuse have been identified [see review by (20)], few studies have tested theoretical models of adolescent risk for PD misuse (21). And although the predictors of PD misuse may vary considerably by drug class (22), little work has examined unique pathways to specific forms of PD misuse. One potential risk factor that may help fill both these identified gaps is personality: specific traits may present risk for particular classes of PD misuse via unique theory-informed pathways.
Personality as a Risk Factor
Personality is a robust predictor of addictive behavior [e.g., (23)]. Internalizing and externalizing traits have been reliably associated with an increased susceptibility for alcohol and illicit substance misuse in adolescence (24). Pihl and Peterson (25) developed a model that delineates four such traits. The first two traits in this model are internalizing. Hopelessness (HOP) involves the trait-like tendency to expect aversive events but not desirable ones (26, 27). Anxiety sensitivity (AS) involves the fear of anxiety-related sensations, due to an unrealistic expectation that such sensations will have catastrophic consequences (28). In adolescents, both HOP and AS are associated with coping motives for substance use (29). Young people high in these traits tend to preferentially misuse depressant drugs (30, 31). In adults, HOP uniquely predicts opioid dependence and AS uniquely predicts anxiolytic dependence (30, 32). The specificity of these paths has yet to be tested in adolescents.
The remaining two traits in Pihl and Peterson's (25) model are externalizing. Impulsivity (IMP), or impulsiveness, is the tendency to act without sufficient forethought (33). IMP has been associated with a pattern of polysubstance use (34, 35). Deficits in response inhibition make high IMP teens more susceptible to early experimentation and to later compulsive substance use (36). Sensation seeking (SS), or novelty seeking (37), involves the desire for novel and intense stimulation (38). High SS substance users are sensitive to the rewarding properties of drugs (39) and tend to specifically misuse stimulants (40) to study, stay awake/alert, “get high,” “party,” and experiment (41).
Traits from Pihl and Peterson's (25) four-factor personality vulnerability model have proven useful in predicting adolescent alcohol (42) and illicit drug use (43, 44), emerging adult PD use (31, 45), and adult PD use (30). This model has yet to be applied to adolescent PD misuse.
Etiological Models of Addiction
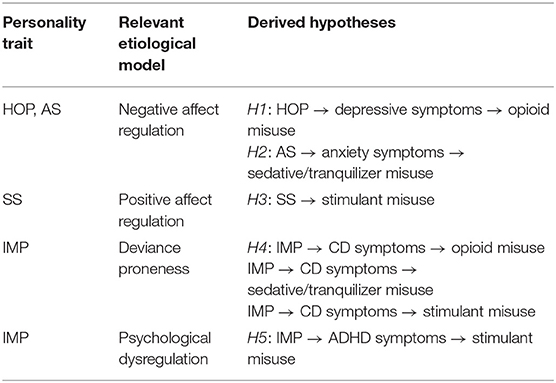
Theoretically, these four traits exert their influence on substance use via negative and positive affect regulation, deviance proneness, and/or psychological dysregulation processes (39). The models most relevant to linking HOP, AS, SS, and IMP with PD misuse are described below (see also Table 1). These theoretical models have informed the mediators in the hypothesized paths from personality to PD misuse.
Affect Regulation Models
Affect regulation models theorize that drugs are taken to regulate emotions—either for negative reinforcement (i.e., a drug's ability to relieve negative affect) or positive reinforcement (i.e., a drug's hedonic effects) (31). Negative affect regulation involves PD use to avoid or control negative emotional states whereas positive affect regulation involves PD use to increase positive emotional states. This dichotomy is in keeping with McCabe et al.'s (46) work on PD misuse motives, which suggests that PDs are misused for self-medication (negative affect regulation) or recreation (positive affect regulation).
Negative Affect Regulation
Individuals high in HOP or AS are theoretically most prone to PD misuse for negative affect regulation (29). First, those high in HOP are thought to misuse opioids to control or avoid symptoms of depression. High HOP adults preferentially misuse opioids over other substances (30–32). HOP also predicts adolescent depression (47), and depression increases risk of PD misuse (21). The negative affect regulation model suggests that depressive symptoms should mediate HOP's specific effect on opioid misuse.
Those high in AS are also theoretically prone to PD misuse for negative affect regulation but through a distinct pathway. Specifically, they are thought to misuse sedatives/tranquilizers to control or avoid anxiety symptoms. High AS adults preferentially misuse anxiolytics over other substances (30, 31). AS incrementally predicts anxiety disorder symptoms in children and adolescents (48, 49) and anxiety disorders are associated with increased risk for sedative/tranquilizer misuse (50). In sum, the negative affect regulation model supports two distinct and specific pathways: HOP to opioid misuse via depressive symptoms vs. AS to sedative/tranquilizer misuse via anxiety symptoms.
Positive Affect Regulation
Stimulants activate mesolimbic dopamine activity and increase positive mood (51). High SS individuals are theoretically most prone to stimulant misuse for positive affect regulation. SS is robustly related to sensitivity to drug reward (39) and to enhancement motivated substance use (31). High SS individuals preferentially misuse stimulants (32, 40). The positive affect regulation model suggests this is because SS underlies sensitivity to stimulant reinforcement (52). The positive affect regulation model suggests a direct pathway from SS to stimulant misuse that is not mediated through mental health symptoms.
Deviance Proneness Model
Another model relevant to understanding PD misuse is the deviance proneness model (53). High IMP individuals are thought to be prone to a broad, unconstrained pattern of PD misuse (opioid, sedative/tranquilizer, and stimulant), occurring amidst other “deviant” or antisocial behaviors. IMP is associated with comorbid addictive and antisocial behaviors (54). IMP in elementary school students is concurrently and prospectively associated with conduct problems (55). Conduct disorder (CD) symptom severity is associated with greater substance involvement (56), including unconstrained PD misuse (57), in adolescence. The deviance proneness model suggests that CD symptoms mediate IMP's effect on unconstrained PD misuse (i.e., all three types of PD misuse).
Psychological Dysregulation Model
The psychological dysregulation model is an alternative model for explaining the specific link of IMP to stimulant misuse. Individuals high in IMP are most prone to PD misuse resulting from an adverse environment triggering a heritable tendency toward psychological dysregulation (58). ADHD is an externalizing disorder characterized by high IMP (59). Individuals with ADHD (60) or high IMP levels (24) are more likely to misuse stimulants. While only 4% of 10–18-year-olds endorse past-month stimulant misuse (61), 14% of 4–17-year-olds with ADHD endorse past-2-week stimulant misuse (62). IMP's effect on stimulant misuse may be attributable, at least in part, to an inability to inhibit pre-potent responses (63). ADHD symptoms are associated with stimulant misuse even after controlling for prescribed use (64). The psychological dysregulation model suggests that symptoms of ADHD mediate IMP's specific effect on stimulant misuse.
Objectives
Nargiso et al. (20) reviewed 50 articles on adolescent PD misuse and identified the following limitations. First, most studies were cross-sectional. Second, non-demographic risk factors (e.g., personality, mental health symptoms) were understudied. Third, there was a lack of specificity regarding predictors of misuse across PD classes. The present study sought to address these limitations by examining predictors of different forms of PD misuse (i.e., opioid, sedative/tranquilizer, stimulant) in a large sample of Canadian adolescents, tested prospectively in Grades 9 and 10 through a “semi-longitudinal design.” In this design, one part is longitudinal (i.e., tests of personality to mental health symptoms and personality to PD misuse) and the other part is cross-sectional (i.e., tests of mental health symptoms to PD misuse). We used a broad definition of PD misuse in the present study, involving use of a PD in any way not directed by a physician (1).
See Table 1 for a summary of our hypotheses. Based on the theories described above, we hypothesized that: in keeping with the negative affect regulation model, (H1) Grade 9 HOP would specifically predict Grade 10 opioid misuse via Grade 10 depressive symptoms, and (H2) Grade 9 AS would specifically predict Grade 10 sedative/tranquilizer misuse via Grade 10 anxiety symptoms; in keeping with the positive affect regulation model, (H3) Grade 9 SS would directly predict Grad 10 stimulant misuse; in keeping with the deviance proneness model, (H4) Grade 9 IMP would predict Grade 10 opioid misuse, sedative tranquilizer misuse, and stimulant use, all via Grade 10 CD symptoms; and in keeping with the psychological dysregulation model, (H5) Grade 9 IMP would also predict Grade 10 stimulant misuse via Grade 10 ADHD symptoms.
Methods
The present study's data was archival. It was collected as part of the Co-Venture Trial (65) examining the longer-term efficacy of personality-targeted substance misuse prevention. Assenting students from 31 high schools (public and private; English and French) in Montreal, Canada participated. Data was collected annually (during the fall and spring terms) beginning in September 2012. A web-based platform (Delosis Ltd., London, U.K.) was used to survey students during regular class times. At baseline, students were in Grade 7. The present study used data collected prospectively in Grade 9 (September 2014-May 2015) and Grade 10 (September 2015-May 2016). Risk increases as adolescents transition from middle to high school (66). In Canada, high school normally runs from Grades 9-12 (67). We therefore excluded Grade 7-8 (i.e., middle school) data. Ethical approval was granted by Sainte-Justine Hospital's Research Ethics Board (approval number = 2012-396, 3427) and by each administrative school board.
Participants
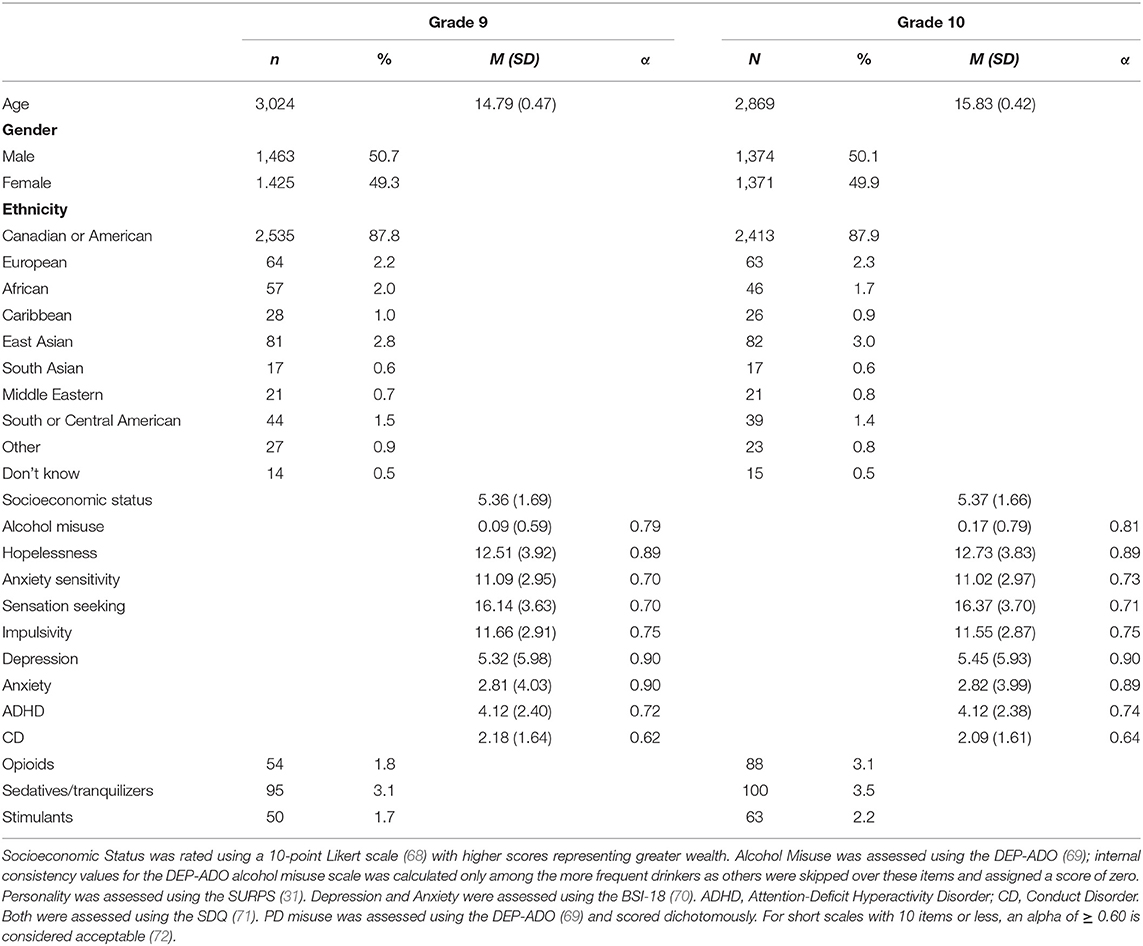
Sample sizes were n = 3,024 in Grade 9 and n = 2,869 of these same students in Grade 10 (5% attrition). See Table 2 for sample characteristics.
Measures
Personality
The 23-item Substance Use Risk Profile Scale (SURPS; 30) was used to assess personality as part of the Co-Venture Trial. The SURPS has four subscales: HOP (7 items; “I feel that I'm a failure”), AS (5 items; “It is frightening to feel dizzy or faint”), SS (6 items; “I like doing things that frighten me a little”), and IMP (5 items; “I usually act without stopping to think”). Participants responded using a 5-point Likert scale (1 strongly disagree to 5 strongly agree). Following reverse scoring of certain negatively keyed items, subscale scores were generated by summing component items. The SURPS was chosen for use in the large-scale Co-Venture survey given its brevity and its strong psychometric properties in both English (43) and French (73). These include acceptable to good internal consistency, factorial validity, convergent and discriminant validity (e.g., with similar personality measures), and concurrent, predictive, and incremental validity in relation to substance use and substance-related problems in youth [e.g., (31, 43, 74)]. In the present sample, the subscales were internally consistent (see Table 2).
Internalizing Symptoms
The 18-item Brief Symptom Inventory-18 [BSI-18; (70)] was used to assess depression and anxiety symptoms. It measures past-week psychological distress. In this study, only the Depression (6 items; “feeling blue”) and Anxiety (6 items; “nervousness or shakiness inside”) subscales were used. Participants responded using a 5-point Likert Scale (0 not at all to 4 extremely often). Subscale scores were generated by summing component items. The BSI-18 has strong psychometric properties in both English (75) and French (76). In our sample, the subscales were internally consistent (see Table 2).
Externalizing Symptoms
The 25-item Youth Self-Report Strengths and Difficulties Questionnaire (SDQ; 73) was used to assess ADHD and CD symptoms. It measures symptoms over the past 6-months. In this study, only the Hyperactivity/Inattention (5 items; “restless, cannot sit still for long”) and Conduct Problems (5 items; “often accused of lying or cheating”) subscales were used (77). The remaining subscales were excluded as they pertain instead to prosocial (Prosocial Behavior) and internalizing (Emotional Symptoms, Peer Relationship Problems) behaviors (77). Participants responded using a 3-point Likert Scale (0 not true to 2 certainly true). Following reverse scoring of certain items, subscale scores were generated by summing component items. The SDQ has strong psychometric properties in both English (78) and French (79). In our sample, the subscales were internally consistent (see Table 2).
Prescription Drug Misuse
A modified and validated version of the Detection of Alcohol and Drug Problems in Adolescents (DEP-ADO; 77) assessed lifetime PD misuse for: (1) Opioids: e.g., “Codeine, Demerol, Morphine, Percodan, Methadone, Darvon, Opium, Dilaudid, or Talwin”; (2) sedatives: e.g., “barbiturates, sedatives, downers, or sleeping pills like Seconal and Quaaludes”; (3) tranquilizers: e.g., “Valium, Librium, or Ativan”; and (4) stimulants: e.g., “stimulants, speed, methamphetamine, amphetamine, or Benzedrine.” Participants responded using a 6-point frequency scale (0 never to 5 every day). To deal with zero-inflation, items were scored dichotomously (i.e., 1 = had used that PD class, 0 = had not). In keeping with our previous research (45), sedatives and tranquilizers were collapsed into a single category. The DEP-ADO has strong psychometrics and is available in both English (69) and French (80). It was developed for and validated with adolescents aged 14-17 years (i.e., Grades 9–11). It has a strong test-retest reliability (r =0.94), acceptable to good internal consistency (Cronbach's alpha =0.61–0.86), and content, convergent, and criterion-related validity (sensitivity =0.84; specificity =0.91) (69).
Alcohol Misuse
Alcohol misuse was also assessed using the modified DEP-ADO (69). This scale includes 10 yes/no items that pertain to lifetime issues with: physical health, psychological health, familial relationships, intimate relationships, academics, finances, delinquency, risky behavior, alcohol tolerance, and treatment seeking, attributable to one's alcohol use. This sole focus on alcohol was a change from the original DEP-ADO which asked these items for alcohol and other drugs combined (69). Items were summed to create a 0–10 total score. Only those indicating a frequency of drinking greater than or equal to “weekends or once or twice during the week” on a previous DEP-ADO item were asked these alcohol misuse items; the others were skipped over these items and automatically assigned an alcohol misuse score of 0. In the present sample, the alcohol misuse scale was internally consistent (see Table 2).
Statistical Analyses
Sample descriptive statistics were first calculated in SPSS 20.0. T-tests and chi square tests were used to compare baseline (Grade 9) characteristics of those retained (n = 2,869) vs. lost to follow-up (n = 155) in Grade 10. Correlations were specified between the personality, mental health, and PD misuse variables. The hypothesized model was then run in MPlus 7.11 (81). Because our dependent variables were categorical, a robust weighted least squares approach was used [ESTIMATOR = WLSMV; (82)]. Missing data was handled using pairwise deletion such that only those with data at both timepoints were used in hypothesis testing. We controlled for school and for Grade 9 mental health and PD misuse. Our model therefore accounts for new users. We also controlled for age, sex, ethnicity, and socioeconomic status (68), given their known effects on PD misuse (20, 83). Because high-intensity drinking is associated with PD misuse (84), we controlled for alcohol misuse as assessed on the DEP-ADO. These covariates were regressed onto all the outcome variables.
Standard indices were used to assess model fit. RMSEA ≤ 0.05 and CFI/TLI ≥0.95 indicate good fit. RSMEA ≤ 0.08 and CFI/TLI ≥0.90 indicate adequate fit (85). Since chi-square values are often significant when the sample size is large (86), we did not interpret the chi-square as a fit statistic. Instead, we used the χ2/df ratio where a value <3.0 indicates good fit. Significant effects were detected at a 95% confidence interval. Bootstrapped confidence intervals were used to determine the significance of indirect effects (i.e., significant if the confidence intervals did not cross zero).
Results
Sociodemographic Features
On average, students were 14.8 (SD = 0.5) years of age in Grade 9. There was a relatively equal split of the sample across gender at both waves. Most students were middle class and of Canadian or American descent (see Table 2).
Personality
Sample mean scores on the four subscales of the SURPS were relatively consistent with norms on the measure from a previously tested sample of adolescents (31). Scores remained relatively stable from Grade 9 to Grade 10 (see Table 2).
Mental Health
Sample mean scores on the BSI-18 measure of internalizing mental health symptoms indicated that levels of anxiety and depression symptoms were both relatively low, on average, in our non-clinical sample at baseline (Grade 9), with depression symptom scores somewhat higher than anxiety symptom scores overall. Sample mean scores on the SDQ measure of externalizing mental health symptoms similarly indicated that levels of ADHD and CD symptoms were both relatively low, on average, in our non-clinical sample at baseline (Grade 9), with ADHD symptom scores somewhat higher than CD symptoms scores overall. Scores remained relatively stable on all four measures of mental health symptoms from Grade 9 to Grade 10 (see Table 2).
Substance Misuse
In Grade 10, lifetime PD misuse rates were: 3% for opioids, 4% for sedatives/tranquilizers, and 2% for stimulants (see Table 2). Rates of misuse of each type of PD rose between Grade 9 and Grade 10 with the sharpest increase observed for opioid misuse. Levels of alcohol misuse also rose between Grade 9 and Grade 10 (see Table 2).
Comparison of Students Retained vs. Lost to Follow-Up
T-tests and chi-square tests suggested that, at baseline (Grade 9), those who were later lost to follow-up (Grade 10) were older, more likely to attend certain schools, and endorsed more personality vulnerability (HOP, SS, IMP), mental health symptoms (depression, CD, ADHD), alcohol misuse, and PD misuse.
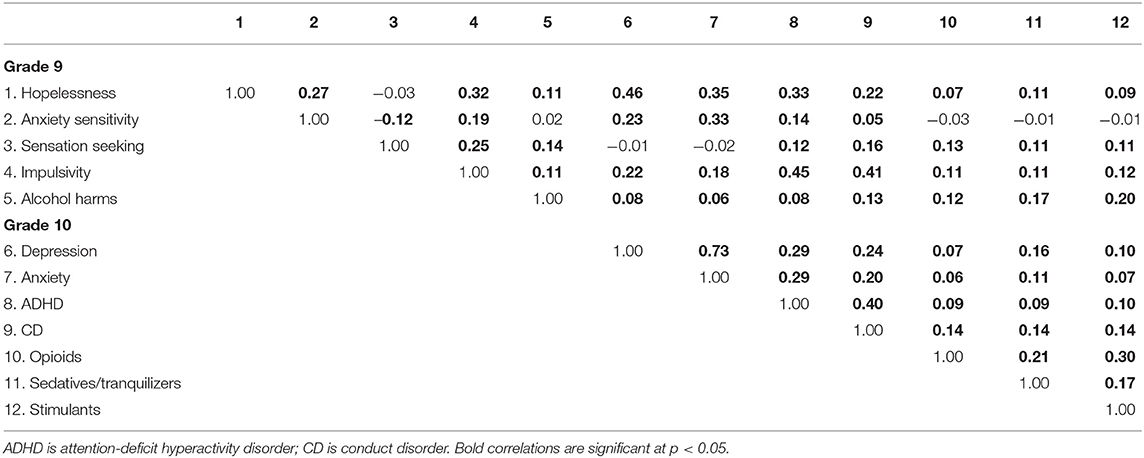
Correlations
Bivariate correlations between study variables are displayed in Table 3. With respect to correlations between Grade 9 personality and Grade 10 mental health symptoms, HOP was most strongly associated with depressive symptoms, AS was most strongly associated with anxiety symptoms, and IMP and SS were most strongly associated with ADHD and CD symptoms (with IMP showing much stronger associations than SS in this regard). With respect to correlations between Grade 10 mental health symptoms and Grade 10 PD misuse, the strongest correlations were between CD symptoms with all three forms of PD misuse, anxiety and depressive symptoms with sedative/tranquilizer misuse, and ADHD symptoms with stimulant misuse. Grade 9 alcohol misuse was significantly associated with all Grade 9 personality factors save AS, with all four measures of Grade 10 mental health symptoms, and with all three forms of PD misuse in Grade 10, underlining the importance of alcohol misuse as a covariate.
Hypothesis Tests
Our hypothesized model (see Figure 1) showed good fit across fit indices: χ2(71) = 158.07, p < 0.001; χ2/df = 2.23; RMSEA =0.02, 90% CI [0.02, 0.03]; CFI =0.98; TLI =0.96. Indirect effects are reported in Table 4.
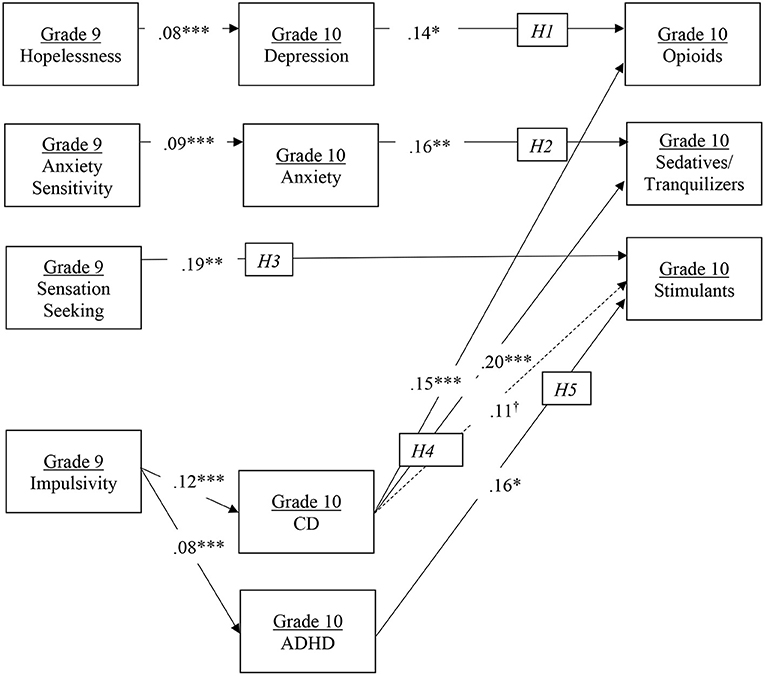
Figure 1. Model results. H1-H5 represent numbered hypotheses. Solid arrows represent statistically significant hypothesized pathways; dotted arrows represent hypothesized but non-significant pathways. Numbers represent standardized coefficients. *p < 0.05, **p < 0.01, ***p < 0.001. †represents marginal significance at p = 0.06.
Grade 9 HOP significantly predicted Grade 10 depressive symptoms which in turn were significantly associated with Grade 10 opioid misuse. Consistent with H1, the indirect effect was statistically significant (p < 0.05). Grade 9 AS significantly predicted Grade 10 anxiety symptoms which in turn were significantly associated with Grade 10 sedative/tranquilizer misuse. Consistent with H2, the indirect effect was statistically significant (p < 0.01).
Consistent with H3, the direct path from Grade 9 SS to Grade 10 stimulant misuse was statistically significant. Grade 9 IMP significantly predicted Grade 10 CD symptoms which in turn were significantly associated with Grade 10 opioid and sedative/tranquilizer misuse and marginally associated with Grade 10 stimulant misuse (p = 0.06). Consistent with H4, all three indirect effects were statistically significant (p < 0.05 for opioid and stimulant misuse; p < 0.01 for sedative/tranquilizer misuse). Grade 9 IMP also significantly predicted Grade 10 ADHD symptoms which were in turn associated with Grade 10 stimulant misuse. Consistent with H5, the indirect effect was statistically significant (p < 0.05).
Tests of Pathway Specificity
To determine the specificity of the HOP to opioid misuse pathway via depression symptoms [H1] and the AS to sedative/tranquilizer misuse pathway via anxiety symptoms [H2], we examined modification indices (MIs). These indicated that the inclusion of paths from AS to depression (MI: 0.23) and HOP to anxiety (MI: 2.47) did not improve model fit (values > 3.84 indicate that the model would be improved). Thus, for the sake of model parsimony, these were not added to the model.
Discussion
Main Findings
In the present study, we sought to address the limitations of the extant literature on adolescent PD misuse, as outlined by Nargiso et al. (20). We applied the four-factor personality vulnerability model (25) to understanding risk for misuse of specific classes of PDs in adolescents. Moreover, we applied different theoretical models of addiction (39) to understanding specific pathways from personality to adolescents' future PD misuse, as mediated through specific sets of mental health symptoms.
Different personality traits showed effects on specific types of PD misuse through unique sets of mental health symptoms, consistent with different theoretical models of addiction, namely the negative and positive affective regulation, deviance proneness, and psychological dysregulation models. Two internalizing personality traits (HOP and AS) followed a negative affect regulation model for predicting specific PD misuse, while SS (an externalizing trait) followed a positive affect regulation model. First, depressive symptoms mediated the relationship between HOP and future opiate misuse. Second, anxiety symptoms mediated the relationship between AS and future tranquilizer misuse. While both these paths are consistent with negative affect regulation, they suggest that high HOP adolescents may be using opiates to self-medicate their depressive symptoms—while high AS teens may be using tranquilizers to self-medicate their anxiety symptoms. Third, SS was predictive of future stimulant misuse suggesting high SS adolescents may be using stimulants to enhance positive affect. This suggests that adolescents high in HOP and AS are prone to PD misuse via negative affect regulation pathways while those high in SS are prone to PD misuse via a positive affect regulation pathway. Fourth, CD symptoms mediated the relationship between IMP and future opiate, sedative/tranquilizer, and stimulant misuse, consistent with a deviance proneness pathway. Unlike the other three traits, IMP therefore seems to be a more general predictor of PD misuse, rather than a specific predictor of a particular form of PD misuse. Higher IMP adolescents appear to more prone to misusing PDs indiscriminately—in the same way that they are prone to engaging in broadband antisocial behaviors. Finally, ADHD symptoms also mediated IMP's effect in the case of future stimulant misuse. We have suggested that this unique personality-to-PD misuse pathway may represent self-medication of psychological dysregulation. In the next section, we look at each of these main findings in relation to the extant literature.
Comparison With the Literature
H1 predicted that HOP would specifically predict future opioid misuse via depressive symptoms. This hypothesis, informed by the negative affect regulation model, was supported through a significant indirect effect from Grade 9 HOP to Grade 10 opioid misuse 1 year later as mediated through Grade 10 depressive symptoms. Depression has been identified as the mental health issue most strongly related to opioid misuse (odds ratios from 1.2 to 4.3) (87). Zullig and Divin (88) found that students who endorsed HOP, depression, and suicidality were 1.18–1.43 times more likely to misuse opioids. Opioids possess psychic pain-numbing properties (89), which may make them particularly attractive to high HOP adolescents—who are prone to depression and may be looking to dull their psychological pain. Our mediational findings are consistent with a mechanism where HOP confers risk for opioid misuse in adolescence via negative affect regulation. More specifically, high HOP adolescents may be self-medicating their depressive symptoms by misusing opioids. Given that opioids are prescribed for the management of physical pain (89) but not for the management of depression (90), any use of opioids for depression self-medication would be considered opioid misuse since it would involve taking the medication for a non-prescribed purpose (91). To help establish the specificity of this HOP risk pathway to opioid use, we tested an additional personality to PD misuse pathway informed by the negative affect regulation model involving AS (i.e., H2).
H2 predicted that AS would specifically predict future sedative/tranquilizer misuse via anxiety symptoms. This hypothesis, also informed by the negative affect regulation model, was supported through a significant indirect effect from Grade 9 AS to Grade 10 sedative/tranquilizer misuse 1 year later as mediated through Grade 10 anxiety symptoms. While sedatives/tranquilizers are commonly prescribed for anxiety (92), the relevant DEP-ADO items (69) specify use “without a prescription,” suggesting that high AS adolescents may be taking non-prescribed sedatives/tranquilizers that they have obtained from family, friends, dealers, or online pharmacies (15) to self-medicate their anxiety symptoms. Taken together, support for H1-2 suggests that there are two distinct negative affect regulation paths from personality to PD misuse. The first is specific to opioid misuse through HOP and the self-medication of depression, and the second specific to sedative/tranquilizer misuse through AS and the self-medication of anxiety. Furthermore, modification indices indicated that the inclusion of paths from AS-to-depression and HOP-to-anxiety did not improve model fit, providing further evidence of the specificity of these pathways.
Informed by the positive affect regulation model, H3 predicted that SS would lead to future stimulant misuse. This hypothesis was supported through a direct path from Grade 9 SS to Grade 10 stimulant misuse. SS is strongly related to sensitivity to positive reinforcement and enhancement motives (31). It predicts substance misuse (93) that is driven by a need for positive affect and psycho-stimulation (29). Previously, we found that SS predicted undergraduate stimulant misuse (45). Other studies also support a robust association between SS and adolescent alcohol misuse (74). Finn et al. (94) found that SS was both directly linked to alcohol problems as well as indirectly linked through alcohol use and positive alcohol expectancies. Castellanos-Ryan et al. (95) concluded that SS's effect on binge drinking was mediated by a reward response bias. Thus, SS likely confers risk for adolescent stimulant misuse as well as excessive drinking via a positive affect regulation pathway. Taken together, the support for H1-H3 suggests that three distinct affect regulation paths predict PD misuse in adolescence: two involving negative affect regulation (i.e., HOP to depression to opioid misuse and AS to anxiety to sedative/tranquilizer misuse) and one involving positive affect regulation (i.e., SS to stimulant misuse).
Unlike the specific associations of each of HOP, AS and SS with particular forms of PD misuse, we expected IMP to have a more general association with PD misuse, including future opioid, sedative/tranquilizer, and stimulant misuse. H4 predicted that Grade 9 IMP would be associated with all three forms of PD misuse in Grade 10 via Grade 10 CD symptoms. These hypotheses, informed by the deviance proneness model, and IMP's centrality as a characteristic of CD (59, 96), were all supported in tests of indirect effects. This pattern is in keeping with previous research with other substances. Mackie et al. (93), for instance, found that IMP predicted adolescent alcohol use via CD symptoms. This result also replicates and extends prior research linking CD symptoms to unconstrained PD misuse in adolescents, including misuse of opioids (97) and stimulants (64). IMP's relationship with substance misuse is motivationally undefined (31) in that it is more reflective of a general inability to inhibit behavior (98). IMP is associated with deficits in response execution and inhibition (95). Poor response inhibition is a risk factor for both CD (99) and substance misuse (100). Paths from IMP to both CD and alcohol problems are also partially mediated by deficient response inhibition (94, 95). In sum, we know that high IMP adolescents struggle to regulate and inhibit their impulses. This makes them more vulnerable to deviance (including CD and PD misuse). Our results are consistent with the idea that IMP confers risk for broadband PD misuse (including all three types of PD misuse) via a general proneness toward deviance in adolescence.
In addition to these general IMP to CD symptoms to PD misuse pathways, H5 predicted a second indirect pathway specifically linking IMP to later stimulant misuse via ADHD symptoms. This hypothesis, informed by the psychological dysregulation model, was supported by a significant indirect effect from Grade 9 IMP to Grade 10 stimulant misuse via Grade 10 ADHD symptoms. IMP is a prominent symptom of ADHD (101) for which stimulants are prescribed (102). Previously, we showed that IMP was concurrently associated with both medically sanctioned stimulant use and stimulant misuse in university students (45). Prescription stimulants are classified as Schedule III under the Canadian Controlled Drugs and Substances Act (S.C. 1996, C. 19) due to their high potential for misuse (103). Their use is legal only when prescribed by a licensed practitioner and taken by the person for whom they were prescribed. For those high in IMP, availability is the best motivational predictor of misuse (34). Adolescents who report symptoms of ADHD are more likely to have stimulant prescriptions, which they can then misuse [e.g., by taking their stimulants in greater amounts or more often than prescribed, via non-intended routes, for non-prescribed reasons, and/or with contraindicated substances; (91)]. While rates of stimulant misuse are relatively low in general adolescent samples, rates are much higher among adolescents who: have symptoms of ADHD, have ADHD diagnoses, are receiving treatment for ADHD, or have stimulant prescriptions (104). Interestingly, some research suggests that the young people most likely to misuse prescription stimulants are those with markers of a possible mental health disorder (e.g., ADHD) but without a formal diagnosis or prescription (105). Our results suggest that some young people may misuse stimulants to cope with their ADHD-related disorganization, poor time management, forgetfulness, and distractibility (64). Thus, in adolescence, IMP may confer risk for stimulant misuse, in part, via self-medication of psychological dysregulation—a form of self-medication that is theoretically distinct from the self-medication of negative affect pathways described above for AS and HOP.
Strengths and Limitations
Our study has several important strengths. These include the large sample size, inclusion of both French- and English-speaking students, the longitudinal component (personality to mental health symptoms and personality to PD misuse paths) over a 1-year follow-up across the developmentally challenging transition to high school, the excellent retention rate (95%), the control of baseline levels of mediators and outcomes in all models, and the theoretically driven hypotheses. Moreover, the topic of the paper is likely to be of interest to both a general and specialty audience of mental health professionals, particularly those that work with youth.
These findings should be interpreted in the context of several potential study limitations. First, we measured personality in Grade 9—and mental health symptoms and PD misuse in Grade 10. As such, the final pathways in our semi-longitudinal model (from mental health symptoms to PD misuse) were cross-sectional. Methodologically, we set up our semi-longitudinal model in this manner because H1-H3 pertain to self-medication. We considered assessing PD misuse in Grade 11, in a three-wave design, but this would have meant testing whether students misused PDs to cope with the mental health symptoms they had reported a year earlier. We wanted to measure mental health symptoms and PD misuse in closer proximity. Self-medication models posit that the mental health-to-PD misuse relationship is unidirectional (50). There are data, however, that suggest that it may be bidirectional. PD misuse, for example, has been shown to exacerbate students' mental health symptoms (106). Our data do not allow us to compare these possibilities and our model does not allow for causal inference. Nonetheless, mediation analyses with even partially cross-sectional data can be a useful starting point (107) and our model had the advantage of being semi-longitudinal (i.e., where part of the design was longitudinal—specifically personality to mental health symptoms and personality to PD misuse). To demonstrate reliability and address these limitations, however, our model should be replicated in a fully longitudinal design that uses shorter (e.g., 6 month) lags between waves. Future research could also use ecological momentary assessment to examine these relationships day-to-day [e.g., (108)].
A second potential limitation pertains to our measure of PD misuse. The DEP-ADO was chosen because it is standardized, has been demonstrated reliable and valid in the measurement of Canadian high school students' substance use (69), and can be use with both English- and French-speaking Québécois adolescents (73). Despite these strengths, the DEP-ADO has some shortcomings. For example, we assessed each type of PD misuse with a single item, introducing measurement error. It also provides little information about students' means of access (e.g., diversion sources, online pharmacies), administration routes, or motives for use. Moreover, different definitions of PD misuse abound (109), and it has been suggested that none of the instruments published to date can adequately assess PD misuse (110). When improved PD misuse measurement tools become available, our model should be replicated. This would reduce measurement error, allowing for a more accurate and refined test of personality's effects on PD misuse generally and on specific classes of PD misuse specifically.
Third, our sampling was limited. While our study was bolstered by its large sample size, this increases the likelihood that small effects will be statistically significant. And some of our effects were relatively small in magnitude, calling for evaluation of their clinical significance (see below). In addition, the students who did not complete our Grade 10 measures were more likely to report Grade 9 personality vulnerability, mental health symptoms, and alcohol and PD misuse, and were more likely to come from specific schools. Some of these results are in keeping with previous studies, in which adolescents lost to follow up were more likely to be involved in drug use and other deviant behavior (111–113). Moreover, we controlled effects of school in our analyses. It still bears noting, however, as samples and findings can be biased when the individuals who drop out differ substantially from those who are retained (114).
Finally, while the use of our brief personality measure [SURPS; (31)] allowed for brevity in the context of a large-scale survey, it did not allow for nuanced assessment of the components of each of our traits. For example, the longer Childhood Anxiety Sensitivity Index (115) would have allowed for examination of the relative contributions of the AS Physical, Social/Control, and Psychological concerns dimensions (116) to the anxiety symptom mediated pathway to sedative/tranquilizer misuse observed in the present study. Similarly, the longer Barratt Impulsiveness Scale (117) would have allowed for examination of the relative contributions of the Attentional, Motor, and Non-planning Impulsiveness components (118) to the CD and ADHD symptom mediated pathways to PD misuse observed in the present study.
Future Research Directions
The present study focused on the mediating effects of mental health symptoms. Motives for PD misuse were not assessed. Bennett and Holloway (119) have concluded that opioids, sedatives/tranquilizers, and stimulants tend to be misused in one of two ways. PDs are misused for self-medication of mental health (e.g., more sleep, less anxiety) or physical health (e.g., to manage a pre-existing illness) problems. They are also misused for pleasure (e.g., to party, get high, or experiment). Boyd et al. (22) and McCabe et al. (46) have published measures of motives for PD misuse. Negatively and positively reinforcing motives are both associated with increased PD misuse frequency (120). Follow-up studies might test whether personality predicts specific motives for PD misuse just as personality predicts specific motives for alcohol use (121). Previously, in the alcohol field, we found chained mediation from personality to mental health symptoms, to drinking motives, to alcohol outcomes (122). The results of the present study suggest that a four-variable chained mediational model might be equally applicable to PD misuse. For example, HOP may predict opioid misuse via symptoms of depression and in turn self-medication motives.
There are also several other areas of future research that are worthy of investigation in the field of personality and PD misuse risk more broadly. First, given that online marketplaces are an accessible source of PDs for young people [e.g., largely uncontrolled, not requiring a prescription, allowing for anonymous access; (123, 124)], and thus a significant public health concern, we need more information on the types of adolescents who are accessing PDs via these sites. While the demographic characteristics of the typical customers of such online marketplaces have been identified [i.e., young, male, Caucasian; (125)], we have not yet identified their personality or mental health characteristics, which would be helpful for targeting prevention efforts. Second, given the well-established role of social influence in young people's drug misuse [e.g., (126)] and emerging data concerning online drug forums and social networking sites where those experimenting with psychotropics, including PDs, share drug-related information (9), it would be interesting to study whether involvement in such communities might be related to personality. For example, are these experimenters or “psychonauts” higher in sensation seeking? Finally, personality and mental health factors may be relevant when it comes to pre-marketing assessment trials of the abuse liability of new prescription drugs. Current practices in this regard have been criticized for excluding those with a previous history of drug misuse or addiction [e.g., (8)]. Given the present findings of significant links of four factor personality model traits and mental health symptoms to different forms of PD misuse, there could be utility to testing a new compound's abuse potential using these more substance-misuse prone individuals in pre-marketing assessment trials to get at the compound's truer abuse liability.
Clinical Implications
Our model suggests that treatment of opioid misuse in adolescents might benefit from a specific targeting of HOP and IMP youth. Cognitive-behavioral therapy (CBT) could benefit teens high in HOP, by teaching them to better cope with their symptoms of depression (127). Motivational approaches could benefit antisocial teens high in IMP, by increasing their future-oriented thinking and teaching them to weigh the short vs. long term consequences of their behavior (128). Because we substantiated paths from IMP to CD symptoms, to opioid, sedative/tranquilizer, and stimulant misuse—a focus on this personality factor would theoretically reduce misuse of a variety of types of PDs. The results of our specificity tests further suggest that treatments of sedative/tranquilizer misuse be targeted toward youth high in AS and include techniques drawn from CBT for anxiety (128). To treat stimulant misuse, our model suggests we should be targeting adolescents high in externalizing traits. Those high in SS could be encouraged to pursue other stimulating yet prosocial activities (129). “Alternate rebellions” including hair dyeing, getting a tattoo, or getting a piercing (130) are safer activities that might meet these adolescents' need for excitement. In contrast, psychologically dysregulated, high-IMP teens could be trained in behavioral ADHD-management techniques (131).
Treating PD misuse is, of course, important. But, given the ongoing PD crisis in North America (132), preventing it is critical. Adolescent overdoses from prescription opioids rose 95% from 1999 to 2016 (133). The likelihood of reporting PD misuse during adolescence, increases with age (83), as we saw across each PD type from Grade 9 to 10 in our sample. Research has shown that PD misuse rates rise consistently between Grade 8–12 and ages 12–17 (134). Thus, prevention efforts geared toward at-risk youth are especially vital. Our results suggest that identifying high personality-risk adolescents (i.e., those high in HOP, AS, SS, or IMP) would benefit both early intervention and targeted prevention strategies for PD misuse.
Personality-matched interventions have effectively reduced illicit drug use in adolescence (135) and PD misuse in adulthood (136). The present study was embedded within a larger trial, which evaluated the longer-term efficacy of the Preventure Program (65). This personality-matched prevention program targets teens with elevated four-factor trait scores (25). It is rooted in the cognitive-behavioral model and incorporates psycho-educational and motivational interviewing components. When applied to alcohol and illicit drug use, the Preventure Program has resulted in delayed onset and reduced escalation of misuse (65). Our study suggests that personality is related to PD misuse in a similar manner to its relations with alcohol and illicit drug use, through mental health symptoms. Thus, personality-matched interventions may have the potential to reduce PD misuse and even prevent PD uptake, if administered prior to PD misuse onset. Our results suggest that the Preventure Program should next be investigated in relation to its utility in targeting adolescent PD misuse.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
Ethical approval was granted by Sainte-Justine Hospital's Research Ethics Board and each administrative school board. The consent process varied across schools. Some schools opted for active consent where written informed consent to participate in the study was provided by the participants' legal guardian/next of kin. Other schools opted for a passive consent procedure where legal guardians/next of kin were fully informed about the study and they declined if they did not consent for their adolescent to participate. All adolescents provided their assent prior to participating.
Author Contributions
SS and AC wrote the manuscript with input from all co-authors. KT ran the statistical analyses. MA assisted with database management. The data collection was coordinated by PC as part of the CoVenture trial. All authors assisted with conceptualization of the model and interpretation of the results.
Funding
Data collection was funded by a grant to PC for the CoVenture trial from the Canadian Institutes of Health Research (Grant #: FRN: 114887). Conduct of this study was also supported by a grant to PC for the CUSP Trial from the Canadian Institutes of Health Research (Grant #: PJT155914). SS and PC are funded through Tier 1 Canada Research Chairs. AC conducted this work as a part of her dissertation research at Dalhousie under the supervision of SS and she was supported through a doctoral fellowship from the Social Sciences and Humanities Research Council of Canada. KT was funded through a Jules Leger Research Chair at Saint Francis Xavier University.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Substance Abuse and Mental Health Services Administration (SAMHSA) (2015). Results From the 2014 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: Department of Health and Human Services.
2. Manchikanti L. Prescription drug abuse: what is being done to address this new drug epidemic? Testimony before the subcommittee on criminal justice, drug policy, human resources. Pain Phys. (2006) 9:287–321.
3. National Advisory Committee on Prescription Drug Misuse. First Do No Harm: Responding to Canada's Prescription Drug Crisis. Ottawa, ON: Canadian Centre on Substance Abuse (2013).
4. Centre for Addiction and Mental Health. Drug use Among Ontario Students: Highlights from the Ontario Student Drug Use and Health Survey (1977-2017). Toronto, ON: Centre for Addition and Mental Health (2017).
5. Miech R, Schulenberg J, Johnston L, Bachman J, O'Malley P, Patrick M. Monitoring the Future National Adolescent Drug Trends in 2017: Findings Released. Ann Arbor, MI: Institute for Social Research, The University of Michigan (2017).
6. Miech R, Johnston L, O'Malley PM, Keyes KM, Heard K. Prescription opioids in adolescence and future opioid misuse. Pediatrics. (2015) 136:e1169–77. doi: 10.1542/peds.2015-1364
7. Boyd CJ, McCabe SE, Cranford JA. Prescription drug abuse and diversion among adolescents in a southeast Michigan school district. Arch Pediatr Adolesc Med. (2007) 161:276–81. doi: 10.1001/archpedi.161.3.276
8. Schifano. F, Papanti GD, Orsolini L, Corkery JM. The consequences of drug misuse on post-marketing surveillance. Exp Rev Clin Pharmacol. (2016) 9:867–71. doi: 10.1080/17512433.2016.1178571
9. Chiappini S, Schifano F. What about “pharming”: issues regarding the misuse of prescription and over-the-counter drugs. Brain Sci. (2020) 10:736. doi: 10.3390/brainsci10100736
10. Monteith S, Glenn T. Searching online to buy commonly prescribed psychiatric drugs. Psychiatry Res. (2018) 260:248–54. doi: 10.1016/j.psychres.2017.11.037
11. Pulver A, Davison C, Parpia A, Purkey E, Pickett W. Nonmedical use of prescription opioids and injury risk among youth. J Child Adolesc Substance Abuse. (2016) 25:522–9. doi: 10.1080/1067828X.2015.1115795
12. Compton WM, Volkow ND. Major increases in opioid abuse in the United States: concerns and strategies. Drug Alcohol Dependence. (2006) 81:103–7. doi: 10.1016/j.drugalcdep.2005.05.009
13. Carrasco-Garrodo P, Jimenez-Trujillo I, Hernandez-Barrera V, Garcia-Gomez-Heras S, Alonso-Fernandez N, Palacios-Cena D. Trends in the misuse of tranquilizers, sedatives, and sleeping pills by adolescents in Spain. J Adolesc Health. (2018) 63:709–16. doi: 10.1016/j.jadohealth.2018.04.003
14. Ford JA. The prescription drug problem we are missing: risks associated with the misuse of tranquilizers and sedatives. J Adolesc Health. (2018) 63:665–6. doi: 10.1016/j.jadohealth.2018.09.007
15. Orsolini L, Corkery JM, Chiappini S, Guirguis A, Vento A, DeBerandis D, et al. ‘New/designer benzodiazepines': an analysis of the literature and psychonauts' trip reports. Curr Neuropharmacol. (2020) 18:809–37. doi: 10.2174/1570159X18666200110121333
16. Schepis TS, West BT, Teter CJ, McCabe SE. Prevalence and correlates of coingestion of prescription tranquilizers and other psychoactive substances by US high school seniors: results from a national survey. Addict Behav. (2016) 52:8–12. doi: 10.1016/j.addbeh.2015.08.002
17. Centres for Disease Control and Prevention National Centre for Health Statistics. Multiple cause of death 1999-2018. CDC WONDER Online Database. Centres for Disease Control and Prevention, National Centre for Health Statistics (2020).
18. McCabe SE, Veliz P, Wilens TE, Schulenberg JE. Adolescents' prescription stimulant use and adult functional outcomes: a national prospective study. J Am Acad Child Adolesc Psychiatry. (2017) 56:226–33. doi: 10.1016/j.jaac.2016.12.008
19. McCabe SE, Veliz P, Boyd CJ, Schulenberg JE. Medical and nonmedical use of prescription sedatives and anxiolytics: adolescents' use and substance use disorder symptoms in adulthood. Addict Behav. (2017) 65:296–301. doi: 10.1016/j.addbeh.2016.08.021
20. Nargiso JE, Ballard EL, Skeer MR. A systematic review of risk and protective factors associated with nonmedical use of prescription drugs among youth in the United States: a social ecological perspective. J Stud Alcohol Drugs. (2015) 76:5–20. doi: 10.15288/jsad.2015.76.5
21. Ford JA, Reckdenwald A, Marquardt B. Prescription drug misuse and gender. Subst Use Misuse. (2014) 49:842–51. doi: 10.3109/10826084.2014.880723
22. Boyd CJ, McCabe SE, Cranford JA, Young A. Adolescents' motivations to abuse prescription medications. Pediatrics. (2006) 118:2472–80. doi: 10.1542/peds.2006-1644
23. Cloninger CR, Bohman M, Sigvardsson S. Childhood personality predicts alcohol abuse in young adults. Alcohol Clin Experi Res. (1988) 12:494–505. doi: 10.1111/j.1530-0277.1988.tb00232.x
24. Conrod PJ. Personality-targeted interventions for substance use and misuse. Curr Addiction Rep. (2016) 3:426–36. doi: 10.1007/s40429-016-0127-6
25. Pihl RO, Peterson JB. Alcoholism: the role of different motivational systems. J Psychiatry Neurosci. (1995) 20:372–96.
26. Abramson LY, Metalsky GI, Alloy LB. Hopelessness depression: a theory-based subtype of depression. Psychol Rev. (1989) 96:358–72. doi: 10.1037/0033-295X.96.2.358
28. Taylor S. Anxiety Sensitivity: Theory, Research, and Treatment of the Fear of Anxiety. New York, NY: Routledge (2014). doi: 10.4324/9781410603326
29. Comeau N, Stewart SH, Loba P. The relations of trait anxiety, anxiety sensitivity, and sensation seeking to adolescents' motivations for alcohol, cigarette, marijuana use. Addict Behav. (2001) 26:803–25. doi: 10.1016/S0306-4603(01)00238-6
30. Conrod PJ, Pihl RO, Stewart SH, Dongier M. Validation of a system of classifying female substance abusers on the basis of personality and motivational risk factors for substance abuse. Psychol Addict Behav. (2000) 14:243. doi: 10.1037/0893-164X.14.3.243
31. Woicik PA, Stewart SH, Pihl RO, Conrod PJ. The substance use risk profile scale: a scale measuring traits linked to reinforcement-specific substance use profiles. Addict Behav. (2009) 34:1042–55. doi: 10.1016/j.addbeh.2009.07.001
32. Mahu IT, Conrod PJ, Barrett SP, Sako A, Swansburg J, Lawrence M. Specificity of personality relationships to particular forms of concurrent substance use among opiate agonist therapy clients. Addict Behav. (2019) 98:106056. doi: 10.1016/j.addbeh.2019.106056
33. Dawe S, Loxton NJ. The role of impulsivity in the development of substance use and eating disorders. Neurosci Biobehav Rev. (2004) 28:343–51. doi: 10.1016/j.neubiorev.2004.03.007
34. Hecimovic K, Barrett SP, Darredeau C, Stewart SH. Cannabis use motives and personality risk factors. Addict Behav. (2014) 39:729–32. doi: 10.1016/j.addbeh.2013.11.025
35. Moody L, Franck C, Hatz L, Bickel WK. Impulsivity and polysubstance use: a systematic comparison of delay discounting in mono-, dual, and tri-substance use. Exp Clin Psychopharmacol. (2016) 24:30–7. doi: 10.1037/pha0000059
36. Castellanos-Ryan N, Struve M, Whelan R, Banaschewski T, Barker GJ, Bokde AL, et al. Neural and cognitive correlates of the common and specific variance across externalizing problems in young adolescence. Am J Psychiatry. (2014) 171:1310–9. doi: 10.1176/appi.ajp.2014.13111499
37. Cloninger CR, Svrakic DM, Pryzbeck TR. A psychobiological model of temperament and character. Arch Gene Psychiatry. (1993) 50:975–90. doi: 10.1001/archpsyc.1993.01820240059008
38. Zuckerman M. Biological Expressions and Biosocial Bases of Sensation Seeking. New York, NY: Press Syndicate of the University of Cambridge (1994).
39. Castellanos-Ryan N, Conrod P. Personality and substance misuse: evidence for a four-factor model of vulnerability. In: Vester JC, Brady K, Galanter M, Conrod P, editors. Drug Abuse and Addiction in Medical Illness: Causes, Consequences, Treatment. New York, NY: Springer (2012). p. 47–62. doi: 10.1007/978-1-4614-3375-0_4
40. Herman-Stahl MA, Krebs CP, Kroutil LA, Heller DC. Risk and protective factors for nonmedical use of prescription stimulants and methamphetamine among adolescents. J Adolesc Health. (2006) 39:374–80. doi: 10.1016/j.jadohealth.2006.01.006
41. Yudko E, Lozhkina O, Fouts A. A comprehensive review of the psychometric properties of the drug abuse screening test. J Subst Abuse Treatment. (2007) 32:189–98. doi: 10.1016/j.jsat.2006.08.002
42. Stewart SH, McGonnell M, Wekerle C, Adlaf E. Associations of personality with alcohol use behaviour and alcohol problems in adolescents receiving child welfare services. Int J Mental Health Addict. (2011) 9:492–506. doi: 10.1007/s11469-011-9339-0
43. Castellanos-Ryan N, O'Leary-Barrett M, Sully L, Conrod P. Sensitivity and specificity of a brief personality screening instrument in predicting future substance use, emotional, behavioural problems. Alcohol Clin Experi Res. (2013) 37:E281–90. doi: 10.1111/j.1530-0277.2012.01931.x
44. Mahu IT, Doucet C, O'Leary-Barrett M, Conrod PJ. Can cannabis use be prevented by targeting personality risk in schools? Twenty-four-month outcome of the Adventure trial on cannabis use: a cluster-randomized controlled trial. Addiction. (2015) 110:1625–33. doi: 10.1111/add.12991
45. Chinneck A, Thompson K, Mahu IT, Davis-MacNevin P, Dobson K, Stewart SH. Personality and prescription drug use/misuse among first year undergraduates. Addict Behav. (2018) 87:122–30. doi: 10.1016/j.addbeh.2018.07.001
46. McCabe SE, Boyd CJ, Teter CJ. Subtypes of nonmedical prescription drug misuse. Drug Alcohol Depend. (2009) 102:63–70. doi: 10.1016/j.drugalcdep.2009.01.007
47. Joiner TR. A test of the hopelessness theory of depression in youth psychiatric inpatients. J Clin Child Psychol. (2000) 19:231–42. doi: 10.1207/S15374424jccp2902_3
48. Knapp AA, Blumenthal H, Mischel ER, Badour CL, Leen-Feldner EW. Anxiety sensitivity and its factors in relation to generalized anxiety disorder among adolescents. J Abnormal Child Psychol. (2015) 44:233–44. doi: 10.1007/s10802-015-9991-0
49. McLaughlin EN, Stewart SH, Taylor S. Childhood anxiety sensitivity index factors predict unique variance in DSM-IV anxiety disorder symptoms. Cognit Behav Ther. (2007) 36:210–9. doi: 10.1080/16506070701499988
50. Becker WC, Fiellin DA, Desai RA. Non-medical use, abuse, and dependence on sedatives and tranquilizers among U.S. adults: psychiatric and socio-demographic correlates. Drug Alcohol Depend. (2007) 90:280–7. doi: 10.1016/j.drugalcdep.2007.04.009
51. Seeman P, Madras B. Methylphenidate elevates resting dopamine which lowers the impulse-triggered release of dopamine: a hypothesis. Behav Brain Res. (2002) 130:79–83. doi: 10.1016/S0166-4328(01)00435-1
52. Miller ME, Badger GJ, Heil SH, Higgins ST, Sigmon SC. Associations between sensation seeking and d-amphetamine reinforcement. Am J Addict. (2015) 24:435–42. doi: 10.1111/ajad.12226
53. Sher KJ, Slutske WS. Disorders of impulse control. In: Stricker GA, Widiger T, editors. Handbook of Psychology. New York, NY: Wiley (2003). p. 195–228. doi: 10.1002/0471264385.wei0808
54. Castellanos-Ryan N, Conrod P. Personality correlates of the common and unique variance across conduct disorder and substance misuse symptoms in adolescence. J Abnormal Child Psychol. (2011) 39:563–76. doi: 10.1007/s10802-010-9481-3
55. López-Romero L, Romero E, Andershed H. Conduct problems in childhood and adolescence: developmental trajectories, predictors, and outcomes in a six-year follow-up. Child Psychiatry Human Dev. (2015) 46:762–73. doi: 10.1007/s10578-014-0518-7
56. Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gene Psychiatry. (2003) 60:837–44. doi: 10.1001/archpsyc.60.8.837
57. Khoddam R, Leventhal AM. Alternative and complementary reinforcers as mechanisms linking adolescent conduct problems and substance use. Exp Clin Psychopharmacol. (2016) 24:376–89. doi: 10.1037/pha0000088
58. Tarter RE, Kirisci L, Mezzich A, Cornelius JR, Pajer K, Vanyukov M, et al. Neurobehavioral disinhibition in childhood predicts early age at onset of substance use disorder. Am J Psychiatry. (2003) 160:1078–85. doi: 10.1176/appi.ajp.160.6.1078
59. American Psychiatric Association (APA). Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Arlington, VA: American Psychiatric Association (2013). doi: 10.1176/appi.books.9780890425596
60. Cassidy TA, Varughese S, Russo L, Budman SH, Eaton TA, Butley SF. Nonmedical use and diversion of ADHD stimulants among U.S. adults ages 18-49: a national internet survey. J Attent Disord. (2015) 19:630–40. doi: 10.1177/1087054712468486
61. Cottler LB, Striley CW, Lasopa SO. Assessing prescription stimulant use, misuse, and diversion among youth 10-18 years of age. Curr Opin Psychiatry. (2013) 26:511–9. doi: 10.1097/YCO.0b013e3283642cb6
62. Sawyer MG, Reece CE, Sawyer ACP, Johnson S, Lawrence D, Zubrick SR. The prevalence of stimulant and antidepressant use by Australian children and adolescents with attention-deficit/hyperactivity disorder and major depressive disorder: a national survey. J Child Adolesc Psychopharmacol. (2017) 27:177–84. doi: 10.1089/cap.2016.0017
63. Logan GD. On the ability to inhibit thought and action: a user guide to the stop signal paradigm. In: Dagenback D, Carr HT, editors. Inhibitory Processes in Attention, Memory, Language. San Diego, CA: Academic Press (1994). p. 189–239.
64. Van Eck K, Markle RS, Flory K. Do conduct problems and sensation seeking moderate the association between ADHD and three types of stimulant use in a college population? Psychol Addict Behav. (2012) 26:939–47. doi: 10.1037/a0027431
65. O'Leary-Barrett M, Mâsse R, Pihl R, Stewart SH, Séguin JR, Conrod P. A cluster-randomised controlled trial evaluating the effects of delaying onset of adolescent substance abuse on cognitive development and addiction following a selective, personality-targeted intervention program: the Co-Venture trial. Addiction. (2017) 112:1871–81. doi: 10.1111/add.13876
66. McIntosh K, Flannery KB, Sugai G, Braun DH, Cochrane KL. Relationships between academics and problem behaviour in the transition from middle school to high school. J Positive Behav Intervent. (2008) 10:243–55. doi: 10.1177/1098300708318961
67. Our Kids. Canadian Provincial Grade Levels: Comparing the Education and Grade Levels of Provinces in Canada. (2019). Available online at: https://www.ourkids.net/school/canadian-province-grade-levels (accessed April 13, 2021).
68. Currie CE, Elton RA, Todd J, Platt S. Indicators of socioeconomic status for adolescents: the WHO health behaviour in school-aged children survey. Health Educ Res. (1997) 12:385–97. doi: 10.1093/her/12.3.385
69. Landry M, Tremblay J, Guyon L, Bergeron J, Brunelle N. La grille de dépistage de la consommation problématique d'alcool et de drogues chez les adolescents et les adolescents (DEP-ADO): développement et qualités psychométriques. Drogues Santé Soc. (2004) 3:20–37. doi: 10.7202/010517ar
70. Derogatis LR. BSI 18, Brief Symptom Inventory 18: Administration, Scoring and Procedures Manual. Minneapolis, MN: National Computer Systems (2001). doi: 10.1037/t07502-000
71. Goodman R. The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry. (1997) 38:581–6. doi: 10.1111/j.1469-7610.1997.tb01545.x
72. Lowenthal KM. An Introduction to Psychological Tests and Scales. 2nd ed. Hove: Psychology Press (2004).
73. Castonguay-Jolin L, Perrier-Ménard E, Castellanos-Ryan N, Parent S, Vitaro F, Tremblay RE, et al. Validation de la traduction française de la SURPS pour une population d'adolescents québécois. Canad J Psychiatry. (2013) 58:538–45. doi: 10.1177/070674371305800909
74. Krank M, Stewart SH, O'Connor R, Woicik PB, Wall AM, Conrod PJ. Structural, concurrent, and predictive validity of the substance use profile scale in early adolescence. Addict Behav. (2011) 36:37–46. doi: 10.1016/j.addbeh.2010.08.010
75. Lancaster MA, McCrea MA, Nelson LD. Psychometric properties and normative data for the Brief Symptom Inventory-18 (BSI-18) in high school and collegiate athletes. Clin Neuropsychol. (2016) 31:321–33. doi: 10.1080/13854046.2016.1138504
76. Perrudet-Badoux A. Évaluation des désordres psychologiques dans une population d'asmathiques à l'aide du Brief Symptom Inventory (DSI). Psychol Med. (1987) 19:2457–60.
77. Goodman A, Lamping DL, Ploubidis GB. When to use broader internalizing and externalizing subscales instead of the hypothesized five subscales on the Strengths and Difficulties Questionnaire (SDQ): Data from British parents, teachers, and children. J Abnormal Child Psychol. (2010) 38:1179–91. doi: 10.1007/s10802-010-9434-x
78. He JP, Burstein M, Schmitz A, Merikangas KR. The Strengths and Difficulties Questionnaire (SDQ): the structure and scale validation in U.S. adolescents. J Abnormal Child Psychol. (2013) 41:583–95. doi: 10.1007/s10802-012-9696-6
79. Capron C, Thérond C, Duyme M. Psychometric properties of the French version of the self-report and teacher Strengths and Difficulties Quesionnaire (SDQ). Eur J Psychol Assessment. (2007) 23:79–88. doi: 10.1027/1015-5759.23.2.79
80. Bernard M, Bolognini M, Plancherel B, Chinet L, Laget J, Stephan P, et al. French validity of two substance-use screening tests among adolescents: a comparison of the CRAFT and DEP-ADO. J Substance Use. (2005) 10:385–95. doi: 10.1080/14659890412331333050
82. Muthén B. Bayesian Analysis in MPlus: A Brief Introduction. (2010). Available online at: www.statmodel.com/download/IntroBayesVersion (accessed April 13, 2021).
83. Milner LA, Ham LS, Zamboanga BL. Adolescents misusing prescription drugs: who's the riskiest users of them all? J Substance Use. (2014) 19:68–74. doi: 10.3109/14659891.2012.734541
84. McCabe SE, Veliz P, Patrick ME. High-intensity drinking and nonmedical use of prescription drugs: results from a national survey of 12th grade students. Drug Alcohol Depend. (2017) 178:372–9. doi: 10.1016/j.drugalcdep.2017.05.038
85. Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Eq Model A Multidiscipl J. (1999) 6:1–55. doi: 10.1080/10705519909540118
86. Curran PJ, West SG, Finch JF. The robustness of test statistics to non-normality and specification error in confirmatory factor analysis. Psychol Methods. (1996) 1:16–29. doi: 10.1037/1082-989X.1.1.16
87. Amari E, Rehm J, Goldner E, Fischer B. Nonmedical prescription opioid use and mental health and pain comorbidities: a narrative review. Canad J Psychiatry. (2011) 56:495–501. doi: 10.1177/070674371105600808
88. Zullig KJ, Divin AL. The association between non-medical prescription drug use, depressive symptoms, and suicidality among college students. Addict Behav. (2012) 37:890–9. doi: 10.1016/j.addbeh.2012.02.008
89. Smith K, Mattick RP, Bruno R, Nielsen S, Cohen M, Campbell G, et al. Factors associated with the development of depression in chronic non-cancer pain patients following the onset of opioid treatment for pain. J Affect Disord. (2015) 184:72–80. doi: 10.1016/j.jad.2015.05.049
90. Singh N, Reece J. Psychotherapy, pharmacotherapy, and their combination for adolescents with major depressive disorder: a meta-analysis. Austr Educat Dev Psychol. (2014) 31:47–65. doi: 10.1017/edp.2013.20
91. Haydon E, Monga B, Rehm J, Adlah E, Fischer B. Prescription drug abuse in Canada and the diversion of prescription drugs into the illicit drug market. Canad J Public Health. (2006) 96:459–61. doi: 10.1007/BF03405190
92. Bisaga A, Mariani JJ. Benzodiazepines and other sedatives and hypnotics. In: Galanter M, Kleber HD, Brady TK, editors. The American Psychiatric Publishing Textbook of Substance Abuse Treatment. 5th edn. Arlington, VA: American Psychiatric Publishing Inc. (2015). p. 239–62. doi: 10.1176/appi.books.9781615370030.mg17
93. Mackie CJ, Castellanos-Ryan N, Conrod PJ. Personality moderates the longitudinal relationship between psychological symptoms and alcohol in adolescents. Alcohol Clin Experi Res. (2011) 35:703–16. doi: 10.1111/j.1530-0277.2010.01388.x
94. Finn PR, Sharkansky EJ, Brandt KM, Turcotte N. The effects of familial risk, personality, and expectancies on alcohol use and abuse. J Abnormal Psychol. (2000) 109:122–33. doi: 10.1037/0021-843X.109.1.122
95. Castellanos-Ryan N, Rubia K, Conrod PJ. Response inhibition and reward response bias mediate the predictive relationships between impulsivity and sensation seeking and common and unique variance in conduct disorder and substance misuse. Alcohol Clin Experi Res. (2011) 35:140–55. doi: 10.1111/j.1530-0277.2010.01331.x
96. Thompson LL, Whitmore EA, Raymond KM, Crowley TJ. Measuring impulsivity in adolescents with serious substance and conduct problems. Assessment. (2006) 13:3–15. doi: 10.1177/1073191105282247
97. Morioka CK, Howard DE, Caldeira KM, Wang MQ, Arria AM. Affective dysregulation predicts incident non-medical prescription analgesic use among college students. Addict Behav. (2018) 76:328–34. doi: 10.1016/j.addbeh.2017.08.034
98. Finn PR, Mazas C, Jutus A, Steinmetz JE. Early-onset alcoholism with conduct disorder: Go/no-go learning deficits, working memory capacity, and personality. Alcohol Clin Experi Res. (2002) 26:186–206. doi: 10.1111/j.1530-0277.2002.tb02524.x
99. Herba CM, Tranah T, Rubia K, Yule W. Conduct problems in adolescence: three domains of inhibition and effect of gender. Dev Neurosci. (2006) 24:11017–22. doi: 10.1207/s15326942dn3002_2
100. Li CS, Huang C, Constable RT, Sinha R. Imaging response inhibition in a stop-signal task: neural correlates independent of signal monitoring and post-response processing. J Neurosci. (2006) 26:186–92. doi: 10.1523/JNEUROSCI.3741-05.2006
101. Barkley RA, Murphy KR, Fischer M. ADHD in Adults: What the Science Says. New York, NY: Guilford Press (2008).
102. Solanto MV, Arnsten AFT, Castellanos FX. (Eds.). Stimulant Drugs and ADHD: Basic and Clinical Neuroscience. New York, NY: Oxford University Press (2001).
103. Kollins SH. Abuse liability of medications used to treat attention-deficit/hyperactivity disorder (ADHD). Am J Addict. (2007) 16:35–44. doi: 10.1080/10550490601082775
104. Weyandt L, Oster D, Marraccini ME, Gudmundsdottir B, Munro B, Mattinez-Zavras B, et al. Pharmacological interventions for adolescents and adults with ADHD: stimulant and nonstimulant medications and misuse of prescription stimulants. Psychol Res Behav Manage. (2014) 7:223–49. doi: 10.2147/PRBM.S47013
105. Arria AM, DuPont RL. Nonmedical prescription stimulant use among college students: why we need to do something and what we need to do. J Addict Dis. (2010) 29:417–26. doi: 10.1080/10550887.2010.509273
106. Soule M, Connery HS. Co-occurring substance use disorders. In: Tse J, Volpp YS, editors. A Case-Based Approach to Public Psychiatry. New York, NY: Oxford University Press (2018). p. 155–61. doi: 10.1093/med/9780190610999.003.0020
107. Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York, NY: Guilford Publications. (2013).
108. Serre F, Fatseas M, Debrabant R, Alexandre J.-M., Auriacombe M, et al. Ecological momentary assessment in alcohol, tobacco, cannabis, and opiate dependence: a comparison of feasibility and validity. Drug Alcohol Depend. (2012) 126:118–23. doi: 10.1016/j.drugalcdep.2012.04.025
109. Barrett SP, Meisner JR, Stewart SH. What constitutes prescription drug misuse? Problems and pitfalls of current conceptualizations. Curr Drug Abuse Rev. (2008) 1:255–62. doi: 10.2174/1874473710801030255
110. Smith SM, Paillard F, McKeown A, Burke LB, Edwards RR, Katz NP, et al. Instruments to identify prescription medication misuse, abuse, and related events in clinical trials: an ACTTION systematic review. J Pain. (2015) 16:389–441. doi: 10.1016/j.jpain.2015.01.009
111. Tebes JK, Snow DL, Arthur MW. Panel attrition and external validity in the short-term follow-up study of adolescent substance use. Evaluat Rev. (1992) 16:151–70. doi: 10.1177/0193841X9201600203
112. Snow DL, Tebes JK, Arthur MW. Panel attrition and external validity in adolescent substance use research. J Consult Clin Psychol. (1992) 60:804–7. doi: 10.1037/0022-006X.60.5.804
113. Brook JS, Cohen P, Gordon AS. Impact of attrition in a sample in a longitudinal study of adolescent drug use. Psychol Rep. (1983) 53:375–8. doi: 10.2466/pr0.1983.53.2.375
114. Boys A, Marsden J, Stillwell G, Hatchings K, Griffiths P, Farrell M. Minimizing attrition in longitudinal research: practical applications from a cohort of adolescent drinking. J Adolesc. (2003) 26:363–73. doi: 10.1016/S0140-1971(03)00011-3
115. Silverman WK, Fleisig W, Rabian B, Peterson RA. Childhood anxiety sensitivity index. J Clin Child Psychol. (1991) 20:162–8. doi: 10.1207/s15374424jccp2002_7
116. Walsh TM, Stewart SH, McLaughlin E, Comeau N. Gender differences in Childhood anxiety sensitivity index (CASI) dimensions. J Anxiety Disord. (2004) 18:695–706. doi: 10.1016/S0887-6185(03)00043-4
117. Barratt ES. Anxiety and impulsiveness related to psychomotor efficiency. Perceptual Motor Skills. (1959) 9:191–8. doi: 10.2466/pms.1959.9.3.191
118. Patton JH, Stanford MS, Barrett ES. Factor structure of the barratt impulsiveness scale. J Clin Psychol. (1995) 51:768–74. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1
119. Bennett T, Holloway K. Motives for illicit prescription drug use among university students: a systematic review and meta-analysis. Int J Drug Policy. (2017) 44:12–22. doi: 10.1016/j.drugpo.2017.02.012
120. Kelly BC, Rendina HJ, Vuolo M, Wells BE, Parsons JT. A typology of prescription drug misuse: a latent class approach to differences and harms. Drug Alcohol Rev. (2015) 34:211–20. doi: 10.1111/dar.12192
121. Cooper ML, Frone MR, Russell M, Mudar P. Drinking to regulate positive and negative emotions: a motivational model of alcohol use. J Personal Soc Psychol. (1995) 69:990–1005. doi: 10.1037/0022-3514.69.5.990
122. Chinneck A, Thompson K, Dobson KS, Stuart H, Teehan M, Stewart SH, et al. Neurotic personality traits and risk for adverse alcohol outcomes: Chained mediation through emotional disorder symptoms and drinking to cope. Substance Use Misuse. (2018) 53:173–4. doi: 10.1080/10826084.2018.1432647
123. Orsolini L, Papanti D, Corkery J, Schifano F. An insight into the deep web: why it matters for addiction psychiatry? Human Psychopharmacol Clin Experi. (2017) 32:e2573. doi: 10.1002/hup.2573
124. Shifano F, Chiappini S, Corkery JM, Guirguis A. Abuse of prescription drugs in the context of novel psychoactive substances (NPS): a systematic review. Brain Sci. (2018) 8:73. doi: 10.3390/brainsci8040073
125. Orsolini L, Francesconi G, Papanti D, Giergetti A, Schifano F. Profiling online recreational/prescription drugs' customers and overview of drug vending virtual marketplaces. Hum Psychopharmacol Clin Exp. (2015) 30:302–18. doi: 10.1002/hup.2466
126. Bartel SJ, Sherry SB, Smith MM, Glowacka M, Speth TA, Stewart SH. Social influences on binge drinking in emerging adults: which social network members matter most? Substance Abuse. (2020) 41:480–4. doi: 10.1080/08897077.2019.1709604
127. Colognori DB, Herzig K, Reigada LC, Leiby A, Warner CM. Cognitive-behavioural therapy for youth with functional somatic and internalizing symptoms. In: Anbar RD, editor. Functional Symptoms in Pediatric Disease: A Clinical Guide. Berlin: Springer Science and Business Media (2014). p. 269–84. doi: 10.1007/978-1-4939-1974-1_19
128. Conrod PJ, Stewart SH, Comeau N, Maclean AM. Preventative efficacy of cognitive behavioural strategies to the motivational bases of alcohol misuse in at-risk youth. J Clin Child Adolesc Psychol. (2006) 35:490–504. doi: 10.1207/s15374424jccp3504_6
129. Herie MA, Watkin-Merek L. Structured Relapse Prevention: An outpatient Counselling Approach. 2nd ed. Toronto, ON: Centre for Addiction and Mental Health (2006).
130. Linehan MM. DBT Skills Training Manual. Module. 4: Distress Tolerance Skills. Handouts and Worksheets. 2nd ed. New York, NY: Guilford Press (2015).
131. Antshel KM, Olszewski AK. Cognitive behavioural therapy for adolescents with ADHD Child. Adolesc Psychiatric Clin North Am. (2014) 23:825–42. doi: 10.1016/j.chc.2014.05.001
132. Fischer B, Keates A, Bühringer G, Reimer J, Rehm J. Non-medical use of prescription opioids and prescription opioid-related harms: why so markedly higher in North America compared to the rest of the world? Addiction. (2014) 109:177–81. doi: 10.1111/add.12224
133. Gaither JR, Shabanova V, Leventhal JM. US national trends in pediatric deaths from prescription and illicit opioids, 1999-2016. JAMA Network Open. (2018) 1:e186558. doi: 10.1001/jamanetworkopen.2018.6558
134. Johnston LD, O'Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future National Survey Results on Drug Use 1975–2009: Volume II. College Students and Adults Ages 19-50. Bethesda, MD: National Institute on Drug Abuse (2010).
135. Conrod PJ, Castellanos-Ryan N, Strang J. Brief, personality-targeted coping skills intervention and survival as a non-drug user over a 2-year period during adolescence. Arch Gene Psychiatry. (2010) 67:85–93. doi: 10.1001/archgenpsychiatry.2009.173
Keywords: adolescents, personality risk, prescription drug misuse, anxiety sensitivity, hopelessness, sensation seeking, impulsivity, mental health symptoms
Citation: Stewart SH, Chinneck A, Thompson K, Afzali MH, Nogueira-Arjona R, Mahu IT and Conrod PJ (2021) Personality to Prescription Drug Misuse in Adolescents: Testing Affect Regulation, Psychological Dysregulation, and Deviance Proneness Pathways. Front. Psychiatry 12:640766. doi: 10.3389/fpsyt.2021.640766
Received: 12 December 2020; Accepted: 17 March 2021;
Published: 27 April 2021.
Edited by:
Fabrizio Schifano, University of Hertfordshire, United KingdomReviewed by:
Georgios Demetrios Kotzalidis, Sapienza University of Rome, ItalyLaura Orsolini, University of Hertfordshire, United Kingdom
Copyright © 2021 Stewart, Chinneck, Thompson, Afzali, Nogueira-Arjona, Mahu and Conrod. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sherry H. Stewart, c3N0ZXdhcnRAZGFsLmNh
 Sherry H. Stewart
Sherry H. Stewart Annie Chinneck
Annie Chinneck Kara Thompson3
Kara Thompson3 Raquel Nogueira-Arjona
Raquel Nogueira-Arjona Ioan T. Mahu
Ioan T. Mahu Patricia J. Conrod
Patricia J. Conrod