- 1Schizophrenia Research Foundation, Chennai, India
- 2Department of Psychiatry, Sri Ramachandra Institute of Higher Education and Research, Chennai, India
Background: The importance of physical health among persons with schizophrenia is well-established. Studies from developed and developing countries indicated a strong association between cardiovascular diseases and schizophrenia, while evidence from India is scattered and in its infancy. Hence, the aims of the study were to collate available studies from India on cardiovascular diseases among persons with schizophrenia, identify knowledge gaps and challenges, and discuss recommendations to improve clinical care and research on cardiovascular diseases among persons with schizophrenia in India.
Materials and methods: A comprehensive literature review of Indian studies on cardiovascular diseases and schizophrenia was conducted to collate and synthesise available knowledge.
Results: Several risk factors for cardiovascular disease predominated among persons with schizophrenia. Metabolic syndrome and obesity were the key factors that were reported. Knowledge gaps were identified with respect to the prevalence of cardiovascular diseases among persons with schizophrenia. Sparse research in interventions to prevent and reduce the impact of cardiovascular diseases among persons with schizophrenia was noted.
Conclusion: Targeted efforts are needed at the clinic, community, and policy levels to understand the impact of cardiovascular diseases among persons with schizophrenia. Robust and feasible interventions targeting cardiovascular diseases and its varied risk factors in persons with schizophrenia, that can be implemented in tertiary mental health services, need to be developed and tested.
Introduction
Cardiovascular diseases (CVD) are the leading cause of morbidity and mortality in India (1). Serious mental disorders (SMD), comprising of schizophrenia spectrum disorders and bipolar disorders, also contribute as major causes of morbidity worldwide (2) and in India (3). Among the serious mental disorders, CVD morbidity and mortality is more pronounced among schizophrenia spectrum disorders. In the National Mental Health Survey in 2016, the prevalence of schizophrenia spectrum disorders was found to be 0.8% in India (4). This translates to a huge number of people being affected by schizophrenia spectrum disorders in India.
While global literature has shown a strong association between cardiovascular diseases and schizophrenia, evidence from India is scattered and still in its infancy. Hence, the aims of this paper were to: (1) To comprehensively review the available literature on the interface of cardiovascular health and schizophrenia from India; and (2) To use the information from this scoping review to identify gaps and put forth evidence-informed recommendations to improve management of cardiovascular health among persons with schizophrenia in India.
Materials and Methods
Search Strategy
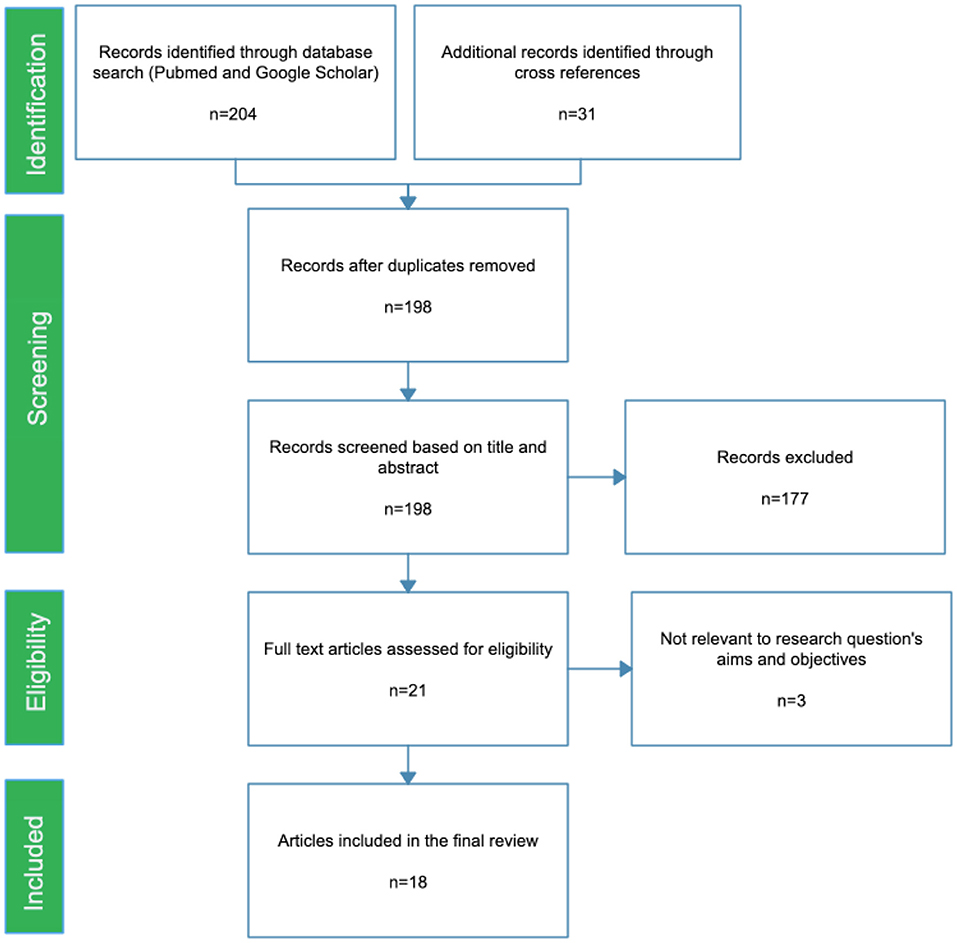
We conducted a scoping review for published articles, up to October 2020. The electronic databases used were PubMed and Google Scholar, using Medical Subject Headings (MESH) terms in combinations: schizophrenia OR psychosis AND “cardiovascular disease” OR “metabolic syndrome” OR diabetes OR hypertension AND India OR Indian, to identify the relevant research publications. Cross references from the articles were retrieved and grey literature were also screened for relevant articles (Figure 1).
Study Selection
In this scoping review, we included peer reviewed studies, including original research and reviews, that reported on: (1) Prevalence/incidence of cardiovascular disorders in persons with schizophrenia; (2) Etiological and risk factors associated with cardiovascular disorders among persons with schizophrenia; and (3) Intervention/management of cardiovascular disorders among persons with schizophrenia. The inclusion criteria were: (1) Articles on cardiovascular disease and metabolic syndrome—prevalence, risk factors, and interventions for persons with schizophrenia, and studies conducted in India. Commentaries and perspectives were excluded from this review.
Data Analysis
The research studies obtained from electronic databases were screened according to the inclusion and exclusion criteria. The selected studies were then categorised under relevant sub-headings pertaining to cardiovascular risk.
Results
Studies Included
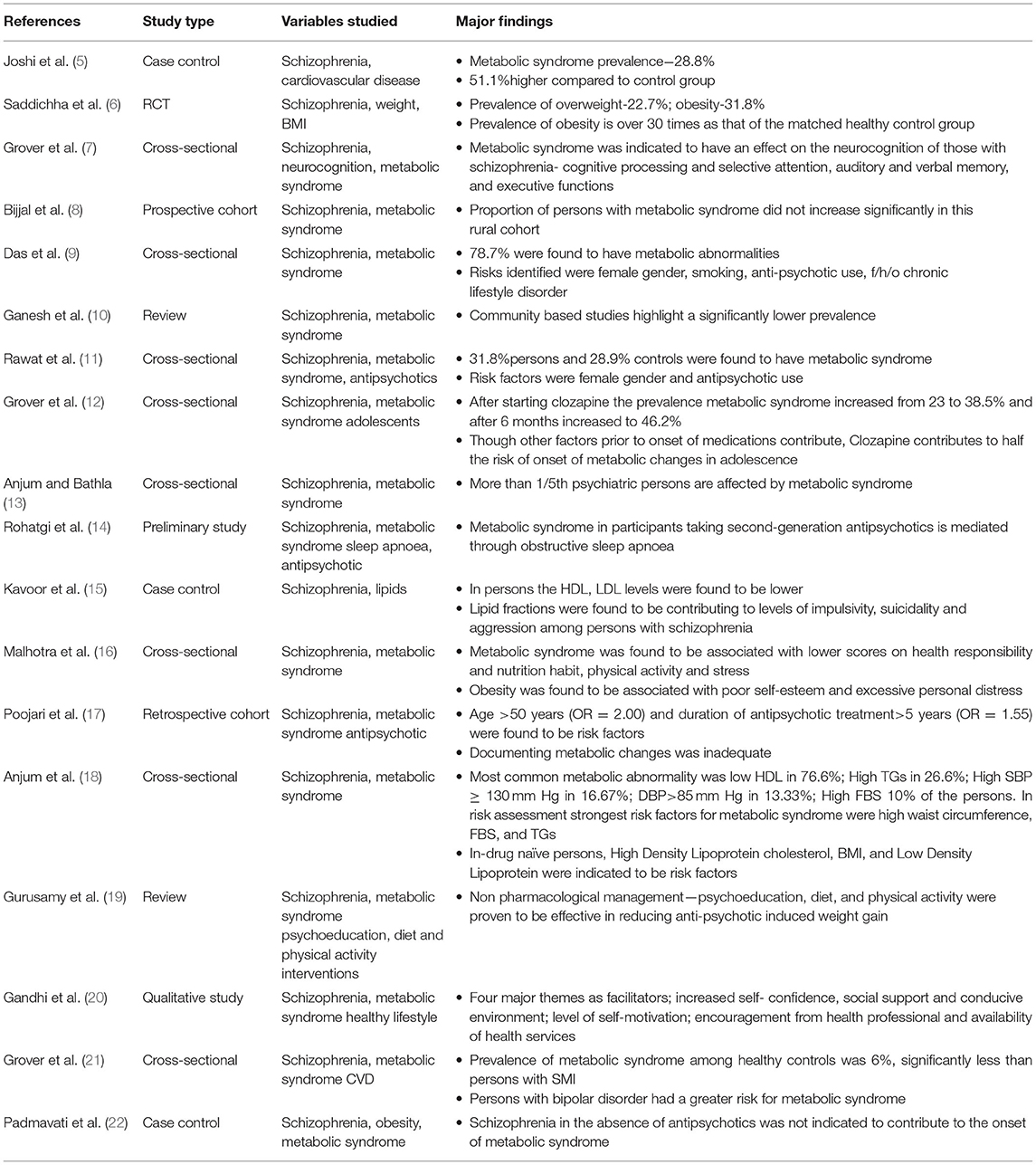
The search Identified 198 unique articles. Of these, 177 articles were excluded as they were not found to satisfy the inclusion and exclusion criteria during the title and abstract search. The remaining 21 research articles were reviewed as full text articles 18 articles were found to be eligible to be included in the current review. All of the studies included in this review, along with their main findings, are given in Table 1.
Major Findings
Search results indicate that there is a dearth of studies on the interface of CVD and schizophrenia from India, the majority of the studies have examined the prevalence of metabolic syndrome and its association with CVD and the clinical outcomes in persons with schizophrenia.
Metabolic Syndrome Among Persons With SMD
Reported literature indicates that standard methods of defining metabolic syndrome have been adopted in the studies, facilitating the comparison and generalizability of the findings. The prevalence of metabolic syndrome among persons with schizophrenia varies in studies from India. In a study conducted in Assam, 78.7% of persons with schizophrenia were found to have metabolic abnormalities (9).There is a higher prevalence amongst persons with mental illness than healthy controls (21). In a recent review by Ganesh et al., pooled prevalence of metabolic syndrome in persons with schizophrenia was 29.83%, and the meta-analysis showed an OR = 3.03 for prevalence in persons with schizophrenia when compared to normal controls and drug-naïve persons had a pooled prevalence of 11.86% (10).
Modifiable lifestyle factors seem to contribute largely by affective quality of life, self-esteem, and increasing distress to the occurrence of metabolic syndrome (16). Some risk factors identified were female gender, antipsychotic use, high BP in men, age > 30 years (13), fasting blood sugar, and triglycerides (18, 23).
Monitoring of metabolic parameters was indicated to be inadequate (17). In drug naïve persons with schizophrenia, high density lipoprotein cholesterol, BMI, and low density lipoprotein were indicated to be risk factors for metabolic syndrome (18).
The presence of metabolic syndrome was also found to impact multiple factors such as neurocognition of persons with schizophrenia (7), while lipid fractions were found to be associated with levels of impulsivity, suicidality, and aggression (15) in persons with schizophrenia. It is further indicated that the presence of mental illness with co-morbid CVD is found to lead to productivity loss (24).
Olanzapine was found to have the greatest weight gain, followed by risperidone and haloperidol (5.1, 4.1, and 2.8 kg), respectively (6). Though other factors contribute to the onset of metabolic changes, clozapine use contributed largely, as after starting clozapine the prevalence of metabolic syndrome increased from 23 to 38.5% and after 6 months increased to 46.2% (12). A study from north India indicates that obstructive sleep apnoea may be a mediating factor for metabolic syndrome with persons on second generation antipsychotics (14). At the same time, Padmavati et al. found low prevalence of obesity and metabolic syndrome among never treated persons with schizophrenia (22). Similarly, the proportion of persons with metabolic syndrome did not increase significantly in this rural cohort, despite the fact that nearly three-fourths of the persons were initiated on second-generation antipsychotics (8).
Prevalence of Obesity Among Persons With SMD
The prevalence of overweight individuals was 22.7% and obesity at 31.8%. It was found that at times the difference of prevalence of metabolic syndrome is up to 30 times greater in persons with mental illness when compared to controls (6).
Interventions for CVD Among Persons With SMD
Some methods to reduce weight gain due to medications that were proven to be effective were—reducing body mass index, reducing waist circumference, lower blood glucose levels, and interventions by dieticians and nurses (19).Other facilitators to improve healthy lifestyle behaviours were increased self-confidence, social support, and conducive environment; level of self-motivation; encouragement from health professional, and availability of health services (20).
Discussion
The aims of our study were to synthesise the available information on the interface of schizophrenia and cardiovascular diseases in India through a scoping review of available studies from India, to understand the gaps in the understanding of cardiac diseases in the Indian context and to discuss a potential way forward to improve clinical care and research for CVD among persons with schizophrenia.
Two important risk factors identified have been metabolic syndrome and obesity, both of which could be intervened with. Most of the studies from India have concentrated on the risk factors for CVD such as metabolic syndrome and anti-psychotic medications among persons with schizophrenia (10). There is sparse research on interventions that can prevent the syndrome or manage the components after they manifest (25), despite evidence of effective management using therapeutic lifestyle approaches and targeted pharmacological interventions in the general population (26).
Obesity is a critical factor associated with an increased risk of developing cardiovascular disease. Several meta-analyses have documented the increased prevalence of obesity in persons with mental disorders in general (27).
In India, a large proportion of the population is affected by obesity (28) and the prevalence of obesity in India varies due to various socio-demographic factors. According to an ICMR-INDIAB study in 2015 (29), the prevalence rate of obesity and central obesity varies from 11.8 to 31.3% and 16.9 to 36.3%, respectively. Several meta-analyses have documented the increased prevalence of obesity in persons with mental disorders in general (27) but very few studies from India. This implies the need for more data on obesity, especially central obesity. This becomes important given that there are few intervention studies that cite body weight and patterning as outcome variables in the general population (30) and virtually none in persons with schizophrenia.
Global literature recognises that over three quarters of deaths from heart disease happen in LMIC with 4–5 persons dying of a heart attack or a stroke (31). These outcomes would be avoidable if there was more awareness of the conditions and the ways to control risk factors through lifestyle interventions and drug treatment where necessary (32). In the Indian context too, cardiovascular diseases are the leading cause of mortality, the estimated prevalence being 54.4 million (33). CVDs with ischemic heart disease and stroke responsible for >80% are the cause of one in four deaths (34). These diseases tend to affect persons in the most productive years of their lives and result in catastrophic social and economic consequences.
Gaps
The gaps in the current knowledge of the status of cardiac health in persons with schizophrenia need to be explored in depth. The association between cardiac disease and mental illnesses has been well-documented with the existing world literature providing relevant insights (35).
The scoping review that we undertook however, demonstrates the limited literature in the Indian context. This finding needs to be understood from several angles. First, it appears that the focus of research has been related largely to metabolic syndrome—taking into context the role of psychotropic medications. Secondly, mental health services are largely delivered in mental health settings, limiting the scope of physical health screening, although the incorporation of psychiatric services at a general hospital psychiatric unit has been documented historically and is within the scope of the National Mental Health program (36). However, despite making mental health services more accessible, several limitations bring about inadequate utilisation of this facility for general medical care for the persons. With increasing emphasis on the primary care provider's role in promoting preventive care, lifestyle changes, and patient self-management, services for the chronically mentally ill persons from the mainstream has become more marginalised (37). Thirdly, there is sufficient evidence that people with schizophrenia are less likely to be screened for lifestyle factors, insufficiently tested for baseline physical parameters or receive standard levels of care for chronic diseases (38). Other factors that limit treatment for cardiac and other physical comorbidities include stigma and diagnostic overshadowing (39). This also limits the possibility of undertaking collaborative research for the study of medical morbidity in persons with severe mental illnesses, explaining the sparse data that is available, despite the increased prevalence of chronic disease and mental illnesses.
Existing literature has several implications. Persons, clinicians and the health care system all play a role in mitigating the multiple factors that are associated with poor physical health in persons with serious mental illnesses. Most persons with schizophrenia receive psychiatric services as out-persons. While many receive medication, social, and rehabilitative services, most either do not receive or access medical care. For persons with serious mental illness, negotiating a separate, complex, medical health care system can be challenging (40). While integrated services offering both mental and medical care at the same location, sometimes even by the same clinician, can overcome systems-based barriers, it also implies that the mental health service system must be able to recognise the comorbidity early and take steps to manage it through referral pathways or collaborative care.
Recommendations
Clinical
Various factors have been identified to contribute to poor cardiovascular health from previous studies. One of the major factors contributing to poor physical health among persons with SMD is lifestyle risk factors (41). Persons with SMD are more likely to smoke, even after comparison with lower socioeconomic status (42). Persons with SMD are also less likely to exercise (43), have diets higher in fat and lower in fibre (44), and are more prone to substance misuse (45). Depressive symptoms (46) and antipsychotic medications (47) have also been implicated to play a role towards poor physical health among persons with SMD. Previous research has highlighted that the mental health professionals are poor in identifying and treating physical health disorders including cardiovascular diseases in persons with SMD (48–50). Improper recording of cardiovascular risk factors and inadequate action are done to intervene to improve these risk factors (49). The stigma of mental illness may be another hurdle that prevents persons from receiving the appropriate and timely treatment (50).
In the recent World Health Organization (WHO) guidelines on managing physical health conditions in persons with severe mental disorders, recommendations are suggested to address important areas such as tobacco cessation, weight management, substance use disorders, cardiovascular disease and cardiovascular risk, diabetes mellitus, HIV/AIDS, and other infectious diseases (tuberculosis, hepatitis B/C) (51).
Physical health screening such as historical review of physical health symptoms and existing chronic disease status and review and follow up of weight, waist circumference, and body mass index are highly recommended to identify CVD risks and diseases early in persons with SMD (52). The recent India Hypertension Control Initiative (IHCI) advocates for regular blood pressure checking for all the persons and caregivers visiting any health facility and initiation of medications at the facility itself rather than referring to experts to prevent delay and drop-out from taking medications (53). Guideline based laboratory assessment of blood glucose, lipid profile, renal functions and ECG monitoring are to be added (51).
As mental health professionals are found to be less involved in the physical health care of persons with SMD (54), additional training to the mental health professionals are needed with respect to advice on safe exercises and diet. At the systems level, efforts must be made to record history of mental illnesses in the data base of the National Hypertension control program (55), to bring in a holistic care for non-communicable disorders in India.
Research
Though literature indicates a well-established need for focus on physical health in persons with mental illness, little progress has been made in understanding the implementation barriers in a developing country such as India. The economic disparity in our nation coupled with lack of awareness may contribute largely to multiple comorbid physical problems that may easily go undetected. Due to cultural barriers in India, persons often do not report their concerns freely unless probed by a professional. Due to their difficulty to verbalise their ailments, their pain behaviour, discomfort may often be overshadowed by their psychiatric ailments.
There are a dearth of trained mental health professionals in India, which results in the existing professionals being over burdened with patient load. This may often lead to an oversight while attending to a patient whose physical ailments are not reported specifically by a patient or caregiver. There is a lack of access to medical records across health care professionals which further widens the gap and hinders collaborative care.
Healthy lifestyle behaviours are not common knowledge in rural parts of India. With the easy availability of fast foods and low priced packaged food there has also been an increase in consumption of fatty foods across the nation (56). This coupled with the existing diet in underdeveloped areas which often lack nutritive value may facilitate poor physical health (57). Sedentary lifestyles are perpetuated by a lack of education regarding exercising, lack of access to parks, gymnasiums etc. (58). Non pharmacological interventions to improve motivation and lifestyle behaviours may not suffice unless the model is tailored for rural areas, as implementation barriers are specific and vary widely from region to region (59).
Economic difficulties often dictate the quality of care, time of reaching out for health care (60), urgency of care, and implementation of the health care plan (61). Even when diagnosed an asymptomatic individual with a comorbid SMI often does not implement a regimented care plan due to economic constraints (16). When individuals from underprivileged sectors are faced with economic constraints, there is often a trade-off made between immediate respite from their fatiguing lives and long term investment for health care. Often the latter is neglected till the health concern is of imminent nature. This may also stem from their health beliefs and lack of knowledge of the trajectory of illness. Various challenges and recommendations to improve cardiovascular health and diseases among persons with serious mental disorders is provided in Table 2.
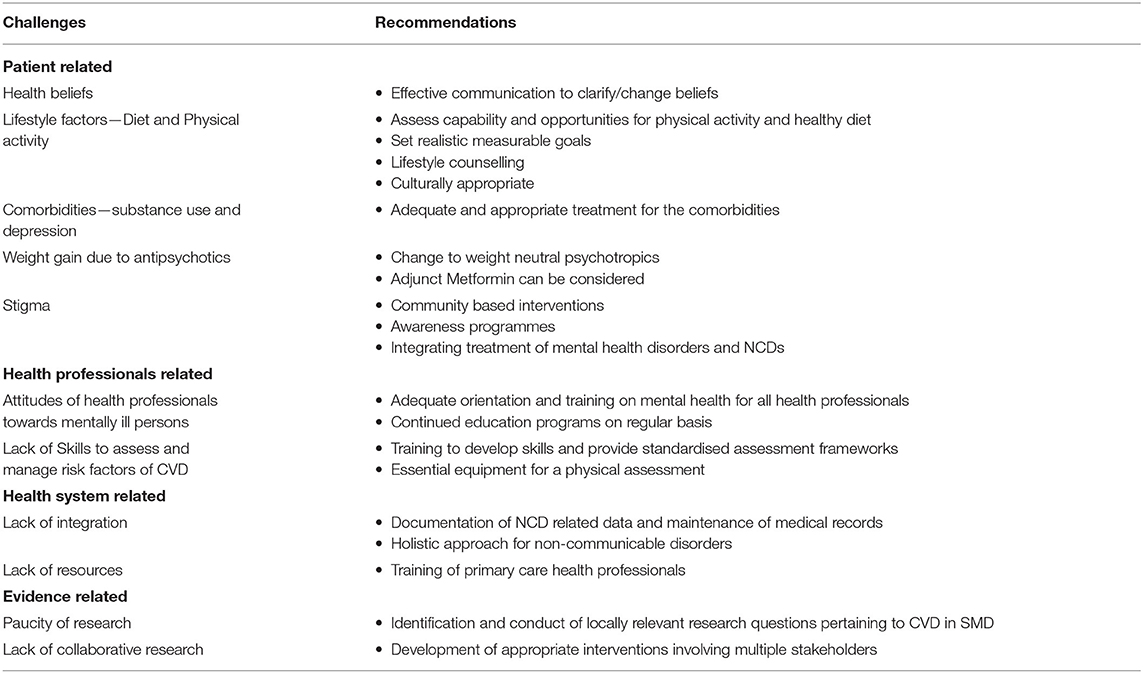
Table 2. Challenges and recommendations to improve cardiovascular health and diseases among persons with schizophrenia.
Strengths and Limitations
This study, through a comprehensive review on cardiovascular health and diseases among persons with serious mental disorders from India, outlines the knowledge gaps and recommendations based on the existing evidence. At the same time, this study is not without limitations. Most of the studies from India on CVD and schizophrenia are heterogenous and have compared various parameters. Given the limited number of studies providing adequate information on CVD and schizophrenia, risk of bias and high heterogeneity, the review findings are unlikely to be valid among different settings in India. Further, a lack of studies from communities and wide age groups could skew our results.
Conclusion
The high incidence of cardiovascular diseases among persons with schizophrenia are a major public health concern worldwide and in India. Better understanding of the magnitude of the problem and various biological, psychological, and social factors contributing in the interplay between cardiovascular diseases and schizophrenia is much needed from India to develop cost-effective, scalable, and culturally appropriate interventions to prevent and/or reduce the impact of cardiovascular disease among persons with schizophrenia.
Author Contributions
RP and VR planned, designed the manuscript, and wrote the first draft of the manuscript. SB did the scoping review of the manuscript and wrote the review section. SK and VR did secondary data analysis. SK and SB commented on the draft and contributed to the subsequent drafts. All authors approved the final manuscript and agreed to submit for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Prabhakaran D, Jeemon P, Roy A. Cardiovascular diseases in India: current epidemiology and future directions. Circulation. (2016) 133:1605–20. doi: 10.1161/CIRCULATIONAHA.114.008729
2. Parks J, Svendsen D, Singer P, Foti ME, Mauer B. Morbidity and Mortality in People With Serious Mental Illness. Alexandria, VA: National Association of State Mental Health Program Directors (NASMHPD) Medical Directors Council (2006). p. 1–87.
3. Sagar R, Dandona R, Gururaj G, Dhaliwal R, Singh A, Ferrari A, et al. The burden of mental disorders across the states of India: the Global Burden of Disease Study 1990–2017. Lancet Psychiatry. (2020) 7:148–61. doi: 10.1016/S2215-0366(19)30475-4
4. Gururaj G, Varghese M, Benegal V, Rao GN, Pathak K, Singh L, et al. National Mental Health Survey of India, 2015-16: Summary. Bengaluru: National Institute of Mental Health and Neurosciences (2016).
5. Joshi KB, Nillawar A, Thorat A. Cardiovascular disease risk in schizophrenia patients: a case control study. J Clin Diagn Res. (2013) 7:2694. doi: 10.7860/JCDR/2013/7592.3734
6. Saddichha S, Manjunatha N, Ameen S, Akhtar S. Effect of olanzapine, risperidone, and haloperidol treatment on weight and body mass index in first-episode schizophrenia patients in India: a randomized, double-blind, controlled, prospective study. J Clin Psychiatry. (2007) 68:1793. doi: 10.4088/JCP.v68n1120
7. Grover S, Padmavati R, Sahoo S, Gopal S, Nehra R, Ganesh A, et al. Relationship of metabolic syndrome and neurocognitive deficits in patients with schizophrenia. Psychiatry Res. (2019) 278:56–64. doi: 10.1016/j.psychres.2019.05.023
8. Bijjal S, Ganesh S, Rawat VS, Agarwal V, Reddy KS, Devi NR, et al. Six months' course and outcome of metabolic abnormalities in a cohort of patients with schizophrenia in rural India. Schizophr Res. (2018) 201:415–6. doi: 10.1016/j.schres.2018.05.016
9. Das D, Bora K, Baruah B, Konwar G. Prevalence and predictors of metabolic syndrome in schizophrenia patients from Assam. Indian J Psychiatry. (2017) 59:228. doi: 10.4103/psychiatry.IndianJPsychiatry_64_16
10. Ganesh S, Ashok AH, Kumar CN, Thirthalli J. Prevalence and determinants of metabolic syndrome in patients with schizophrenia: a systematic review and meta-analysis of Indian studies. Asian J Psychiatry. (2016) 22:86–92. doi: 10.1016/j.ajp.2016.05.006
11. Rawat VS, Ganesh S, Bijjal S, Reddy KS, Agarwal V, Devi R, et al. Prevalence and predictors of metabolic syndrome in patients with schizophrenia and healthy controls: a study in rural South Indian population. Schizophr Res. (2018) 192:102–7. doi: 10.1016/j.schres.2017.04.039
12. Grover S, Hazari N, Chakrabarti S, Avasthi A. Metabolic disturbances, side effect profile and effectiveness of clozapine in adolescents. Indian J Psychol Med. (2016) 38:224. doi: 10.4103/0253-7176.183091
13. Anjum S, Bathla M. A comparative study of prevalence and predictors of metabolic syndrome in various psychiatric disorders in state of Haryana: more than 30 years Vs. less than 30 years. Diabetes Metab Syndr. (2019) 13:510–6. doi: 10.1016/j.dsx.2018.11.002
14. Rohatgi R, Gupta R, Ray R, Kalra V. Is obstructive sleep apnea the missing link between metabolic syndrome and second-generation antipsychotics: preliminary study. Indian J Psychiatry. (2018) 60:478–84. doi: 10.4103/psychiatry.IndianJPsychiatry_105_18
15. Kavoor AR, Mitra S, Kumar S, Sisodia AK, Jain R. Lipids, aggression, suicidality and impulsivity in drug-naïve/drug-free patients of schizophrenia. Asian J Psychiatry. (2017) 27:129–36. doi: 10.1016/j.ajp.2017.03.002
16. Malhotra N, Kulhara P, Chakrabarti S, Grover S. Lifestyle related factors & impact of metabolic syndrome on quality of life, level of functioning & self-esteem in patients with bipolar disorder & schizophrenia. Indian J Med Res. (2016) 143:434. doi: 10.4103/0971-5916.184284
17. Poojari PG, Khan SA, Shenoy S, Acharya LD, Shetty S, Bose S, et al. Identification of risk factors and metabolic monitoring practices in patients on antipsychotic drugs in South India. Asian J Psychiatry. (2020) 53:102186. doi: 10.1016/j.ajp.2020.102186
18. Anjum S, Bathla M, Panchal S, Singh GP, Singh M. Metabolic syndrome in drug naïve schizophrenic patients. Diabetes Metab Syndr Clin Res Rev. (2018) 12:135–40. doi: 10.1016/j.dsx.2017.11.006
19. Gurusamy J, Gandhi S, Damodharan D, Ganesan V, Palaniappan M. Exercise, diet and educational interventions for metabolic syndrome in persons with schizophrenia: a systematic review. Asian J Psychiatry. (2018) 36:73–85. doi: 10.1016/j.ajp.2018.06.018
20. Gandhi S, Gurusamy J, Ragupathy SK, Damodharan D, Ganesan V, Marimuthu P. Healthy lifestyle behavior and personal control in people with schizophrenia with healthy controls: a cross-sectional comparative study. Asian J Psychiatry. (2019) 45:95–8. doi: 10.1016/j.ajp.2019.09.008
21. Grover S, Nebhinani N, Chakrabarti S, Avasthi A, Basu D, Kulhara P, et al. Cardiac risk factors and metabolic syndrome in patients with schizophrenia admitted to a general hospital psychiatric unit. Indian J Psychiatry. (2014) 56:371–6. doi: 10.4103/0019-5545.146520
22. Padmavati R, McCreadie RG, Tirupati S. Low prevalence of obesity and metabolic syndrome in never-treated chronic schizophrenia. Schizophr Res. (2010) 121:199–202. doi: 10.1016/j.schres.2010.05.010
23. Grover S, Aggarwal M, Chakrabarti S, Dutt A, Avasthi A, Kulhara P, et al. Prevalence of metabolic syndrome in bipolar disorder: an exploratory study from North India. Prog Neuropsychopharmacol Biol Psychiatry. (2012) 36:141–6. doi: 10.1016/j.pnpbp.2011.10.013
24. Fathima FN, Kahn JG, Krishnamachari S, Ekstrand M. Productivity losses among individuals with common mental illness and comorbid cardiovascular disease in rural Karnataka, India. Int J Noncommun Dis. (2019) 4:86–92. doi: 10.4103/jncd.jncd_17_19
25. Yogaratnam J, Biswas N, Vadivel R, Jacob R. Metabolic complications of schizophrenia and antipsychotic medications-an updated review. East Asian Arch Psychiatry. (2013) 23:21–8.
27. Daré LO, Bruand P-E, Gérard D, Marin B, Lameyre V, Boumédiène F, et al. Co-morbidities of mental disorders and chronic physical diseases in developing and emerging countries: a meta-analysis. BMC Public Health. (2019) 19:304. doi: 10.1186/s12889-019-6623-6
28. Ahirwar R, Mondal PR. Prevalence of obesity in India: a systematic review. Diabetes Metab Syndr Clin Res Rev. (2019) 13:318–21. doi: 10.1016/j.dsx.2018.08.032
29. Pradeepa R, Anjana RM, Joshi SR, Bhansali A, Deepa M, Joshi PP, et al. Prevalence of generalized & abdominal obesity in urban & rural India-the ICMR-INDIAB Study (Phase-I)[ICMR-INDIAB-3]. Indian J Med Res. (2015) 142:139. doi: 10.4103/0971-5916.164234
30. Shrivastava U, Fatma M, Mohan S, Singh P, Misra A. Randomized control trial for reduction of body weight, body fat patterning, and cardiometabolic risk factors in overweight worksite employees in Delhi, India. J Diabetes Res. (2017) 2017:7254174. doi: 10.1155/2017/7254174
31. World Health Organization. Cardiovascular Diseases (CVDs). Fact Sheet N 317. January, 2015. Geneva (2015).
32. World Health Organization. Hearts: Technical Package for Cardiovascular Disease Management in Primary Health Care (2020).
33. Prabhakaran D, Jeemon P, Sharma M, Roth GA, Johnson C, Harikrishnan S, et al. The changing patterns of cardiovascular diseases and their risk factors in the states of India: the Global Burden of Disease Study 1990–2016. Lancet Global Health. (2018) 6:e1339–51. doi: 10.1016/S2214-109X(18)30407-8
34. Abdul-Aziz AA, Desikan P, Prabhakaran D, Schroeder LF. Tackling the burden of cardiovascular diseases in India: the essential diagnostics list. Circulations. (2019) 12:e005195. doi: 10.1161/CIRCOUTCOMES.118.005195
35. Correll CU, Solmi M, Veronese N, Bortolato B, Rosson S, Santonastaso P, et al. Prevalence, incidence and mortality from cardiovascular disease in patients with pooled and specific severe mental illness: a large-scale meta-analysis of 3,211,768 patients and 113,383,368 controls. World Psychiatry. (2017) 16:163–80. doi: 10.1002/wps.20420
36. Chadda RK, Sood M. General hospital psychiatry in India: history, scope, and future. Indian J Psychiatry. (2018) 60(Suppl. 2):S258–63. doi: 10.4103/psychiatry.IndianJPsychiatry_435_17
37. Misra S, Ganzini L. Medical care for patients with severe and persistent mental illness. J Gen Internal Med. (2006) 21:1207. doi: 10.1111/j.1525-1497.2006.00619.x
38. Deh M, Correll CU, Bobes J, Cetkovich-Bakmas M, Cohen D, Asai I, et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry. (2011) 10:52–77. doi: 10.1002/j.2051-5545.2011.tb00014.x
39. Jones S, Howard L, Thornicroft G. 'Diagnostic overshadowing': worse physical health care for people with mental illness. Acta Psychiatr Scand. (2008) 118:169–71. doi: 10.1111/j.1600-0447.2008.01211.x
40. Lawrence D, Kisely S. Inequalities in healthcare provision for people with severe mental illness. J Psychopharmacol. (2010) 24:61–8. doi: 10.1177/1359786810382058
41. Brown S, Birtwistle J, Roe L, Thompson C. The unhealthy lifestyle of people with schizophrenia. Psychol Med. (1999) 29:697–701. doi: 10.1017/S0033291798008186
42. Jeste DV, Gladsjo JA, Lindamer LA, Lacro JP. Medical comorbidity in schizophrenia. Schizophr Bull. (1996) 22:413–30. doi: 10.1093/schbul/22.3.413
43. Glover CM, Ferron JC, Whitley R. Barriers to exercise among people with severe mental illnesses. Psychiatr Rehabil J. (2013) 36:45. doi: 10.1037/h0094747
44. Barre LK, Ferron JC, Davis KE, Whitley R. Healthy eating in persons with serious mental illnesses: understanding and barriers. Psychiatr Rehabil J. (2011) 34:304. doi: 10.2975/34.4.2011.304.310
45. Winklbaur B, Ebner N, Sachs G, Thau K, Fischer G. Substance abuse in patients with schizophrenia. Dial Clin Neurosc. (2006) 8:37. doi: 10.31887/DCNS.2006.8.1/bwinklbaur
46. Osborn DP. Topics in review: the poor physical health of people with mental illness. Western J Med. (2001) 175:329. doi: 10.1136/ewjm.175.5.329
47. Kurzthaler I, Fleischhacker WW. The clinical implications of weight gain in schizophrenia. J Clin Psychiatry. (2001) 62(Suppl. 7):32–7.
48. Koran LM, Sox HC, Marton KI, Moltzen S, Sox CH, Kraemer HC, et al. Medical evaluation of psychiatric patients: I. results in a state mental health system. Arch Gen Psychiatry. (1989) 46:733–40. doi: 10.1001/archpsyc.1989.01810080063007
49. Kendrick T. Cardiovascular and respiratory risk factors and symptoms among general practice patients with long-term mental illness. Br J Psychiatry. (1996) 169:733–9. doi: 10.1192/bjp.169.6.733
50. Phelan M, Stradins L, Morrison S. Physical health of people with severe mental illness: can be improved if primary care and mental health professionals pay attention to it. BMJ. (2001) 322:443. doi: 10.1136/bmj.322.7284.443
51. World Health Organization. Management of Physical Health Conditions in Adults With Severe Mental Disorders: WHO Guidelines (2018).
52. Taylor DM, Barnes TR, Young AH. The Maudsley Prescribing Guidelines in Psychiatry. Chichester: John Wiley & Sons (2018).
53. Krishna A, Pathni AK, Sharma B, Shivashankar R, Shrivastava S, Hering D. A perspective of private health care providers in the state of Madhya Pradesh on adopting key strategies of the India hypertension control initiative. J Clin Hypertens. (2020) 22:1321–7. doi: 10.1111/jch.13944
54. Bressington D, Badnapurkar A, Inoue S, Ma HY, Chien WT, Nelson D, et al. Physical health care for people with severe mental illness: the attitudes, practices, and training needs of nurses in three Asian countries. Int J Environ Res Public Health. (2018) 15:343. doi: 10.3390/ijerph15020343
55. Raina S. From NHM to NPCDCS: epidemiological transition and need for a National Program for diabetes in India. J Metab Syndr. (2016) 5:2167–09431000204. doi: 10.4172/2167-0943.1000204
56. Gupta A, Kapil U, Singh G. Consumption of junk foods by school-aged children in rural Himachal Pradesh, India. Indian J Public Health. (2018) 62:65–7. doi: 10.4103/ijph.IJPH_343_16
57. Colles SL, Singh S, Kohli C, Mithal A. Dietary beliefs and eating patterns influence metabolic health in type 2 diabetes: a clinic-based study in urban North India. Indian J Endocrinol Metab. (2013) 17:1066. doi: 10.4103/2230-8210.122626
58. Chandra A, Nongkynrih B. Facilitators and barriers of physical activity in prevention and control of ncd a qualitative study in North India. J Trop Med Health. (2019) 3:1–4. doi: 10.29011/JTMH-144
59. Andrade C. Cardiometabolic risks in schizophrenia and directions for intervention, 2: nonpharmacological interventions. J Clin Psychiatry. (2016) 77:964–7. doi: 10.4088/JCP.16f11060
60. Yerramilli S, Bipeta R. Economics of mental health: part I-economic consequences of neglecting mental health-an Indian perspective. Arch Mental Health. (2012) 13:80.
Keywords: cardiovascular diseases, risk factors, interventions, India, schizophrenia
Citation: Padmavati R, Kantipudi SJ, Balasubramanian S and Raghavan V (2021) Cardiovascular Diseases and Schizophrenia in India: Evidence, Gaps, and Way Forward. Front. Psychiatry 12:639295. doi: 10.3389/fpsyt.2021.639295
Received: 08 December 2020; Accepted: 03 May 2021;
Published: 24 June 2021.
Edited by:
Sri Mahavir Agarwal, University of Toronto, CanadaReviewed by:
VIjay Kumar, National Institute of Mental Health and Neurosciences (NIMHANS), IndiaVenkataram Shivakumar, National Institute of Mental Health and Neurosciences (NIMHANS), India
Rishikesh Behere, KEM Hospital Research Centre, India
Copyright © 2021 Padmavati, Kantipudi, Balasubramanian and Raghavan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ramachandran Padmavati, cGFkbWF2YXRpQHNjYXJmaW5kaWEub3Jn; Vijaya Raghavan, dmlqYXlhcmFnaGF2YW5Ac2NhcmZpbmRpYS5vcmc=
 Ramachandran Padmavati
Ramachandran Padmavati Suvarna Jyothi Kantipudi
Suvarna Jyothi Kantipudi Suhavana Balasubramanian1
Suhavana Balasubramanian1 Vijaya Raghavan
Vijaya Raghavan