- 1National Clinical Research Center for Mental Disorders, Department of Psychiatry, The Second Xiangya Hospital, Central South University, Changsha, China
- 2Hunan Key Laboratory of Psychiatry and Mental Health, China National Technology Institute on Mental Disorders, Changsha, China
- 3Department of Child Psychiatry of Shenzhen Kangning Hospital, Shenzhen Mental Health Center, School of Mental Health, Shenzhen University, Shenzhen, China
Background: Prior research has found that attention deficit/hyperactivity disorder (ADHD) – particularly hyperactivity symptoms – is associated with various somatic complaints. The present study further tests the relationship between hyperactivity symptoms and somatic complaints in Chinese male adolescents and explores the underlying moderating and mediating mechanisms.
Methods: Our sample included 1,586 males (age = 12–16) recruited as part of an epidemiological study of child and adolescent mental disorders from April to July, 2014. Hyperactivity symptoms and somatic complaints were assessed with Achenbach's Child Behavior Checklist (CBCL), and the Childhood Trauma Questionnaire Short Form (CTQ-SF) and Adolescent Life Events Scale (ASLEC) were used to assess exposure to childhood trauma and recent life events.
Results: Adolescents with hyperactivity symptoms experienced more emotional abuse, physical abuse, life events, and reported more somatic complaints symptoms (p < 0.0083 or p < 0.05). Linear regression analysis showed that hyperactivity, total childhood trauma score/emotional abuse and sexual abuse and ASLEC score significantly predicted somatic complaints (all p < 0.05). Emotional abuse and life events mediated the relationship between hyperactivity symptoms and somatic complaints. Furthermore, childhood trauma moderated the path between hyperactivity symptoms and ASLEC in the moderation mediation model for predicting somatic complaints (p < 0.05).
Conclusions: Hyperactivity symptoms had a significant impact on somatic complaints among Chinese male adolescents. Furthermore, childhood trauma and life events affected the relationship between hyperactivity symptoms and somatic complaints. Interventions for somatic complaints in male adolescents with hyperactivity symptoms should thus consider history of childhood trauma and life events.
Introduction
Attention deficit/hyperactivity disorder (ADHD) is a common neurodevelopmental condition characterized by inattention and/or hyperactivity-impulsivity symptoms (1). In recent years, the prevalence of ADHD has shown an increasing trend in various countries (2, 3). A systematic review and meta-analysis of 67 studies of the Chinese population found that 6.26% of children and adolescents had ADHD (4). There is a gender difference in ADHD likelihood with a significantly higher lifetime prevalence in men than in women (5). ADHD can be comorbid with various other psychiatric conditions including conduct disorder, anxiety disorder, oppositional defiant disorder, disruptive mood dysregulation disorder, and bipolar disorder (6–10). A large proportion of children and adolescents with ADHD have at least one comorbid psychiatric disorder (11). Moreover, children and adolescents with ADHD commonly have other medical disorders and physical symptoms (12). Some studies have indicated that ADHD is associated with various somatic complaints like stomachaches and migraine (13, 14). As internalizing symptoms, such as somatic complaints, are likely to be clinically ignored in children and adolescents suffering from ADHD. Therefore, it is necessary to pay more attention to the somatic complaints associated with ADHD. As a main symptom of ADHD, hyperactivity has been reported to be related to somatic complaints. For example, a 10-year study of children's psychosomatic symptoms by Santalahti et al. indicated that psychosomatic symptoms related to hyperactivity symptoms (15). Considering that boys tend to display higher levels of hyperactivity symptoms (16, 17), the purpose of this study is to further test the relationship between hyperactivity symptoms and somatic complaints in a large sample of Chinese adolescent males.
Childhood trauma refers to emotional and physical neglect as well as physical, emotional, and sexual abuse experiences during childhood and adolescence (18). There is evidence for significant associations between childhood trauma and ADHD (19–21). Several studies have shown that children with ADHD are more likely to experience traumatic events than children without ADHD (22, 23). Children with ADHD have more academic problems, such as challenges with time management and planning (24), and exhibit more impulsive behavior than typical children (25), which somewhat increases their risk of experiencing traumatic events. A systematic review of pediatric health outcomes found that experiences of childhood adverse events are associated with somatic complaints (26). Relatedly, Achenbach et al. found that the methylation level of the transient receptor potential ankyrin 1 promotor, which is related to mechanical pain sensitivity, is influenced by childhood traumatic experiences (27). Therefore, we hypothesize that childhood trauma mediates the relationship between hyperactivity symptoms and somatic complaints.
Life events refer to stressors that typically involve danger or readjustment to resume living a normal life, and thus may influence a child's development (28, 29), such as suffering from serious illness and transferring to another school. ADHD is closely related to such life events, and people who suffer from ADHD are known to experience more conflicts and adverse life events compared to people without ADHD (30, 31). Friedrichs et al. found that adults with ADHD symptoms have an increased risk of stressful life events (32). Previous studies have found that life events increase somatic complaints. For example, a study of a population cohort in the Netherlands found that negative life events predicted functional somatic symptoms (33). Similarly, a prospective study found that higher levels of negative life events at 1 year follow-up predicted higher levels of somatic complaints (34). Life events have been shown to mediate the relationship between ADHD and physical diseases. For example, Stickley et al. found that stressful life events mediated the association between ADHD symptoms and physical diseases (35). Given these findings, we predict that life events may also mediate the relationship between hyperactivity symptoms and somatic complaints.
Prior studies have found that adversities during different life periods had interactive effects on mental health. For example, Weissman et al. reported that exposure to childhood violence affected life events related to depression during the follow-up period (36). Zhong et al. found that childhood trauma changed brain function (dorsolateral pre-frontal cortex, insula, etc.) and hypothalamic-pituitary-adrenal (HPA) axis responsiveness to stress (37). Recently, Janiri et al. reported that childhood trauma increased vulnerability to stress-related psychological distress during the coronavirus disease 2019 outbreak (38). Taken together, these studies suggest that early adverse events may influence the stress response to events that occur in the future. For this reason, the present study assumes that childhood trauma may influence the mediating effect of life events on the relationship between hyperactivity symptoms and somatic complaints.
Materials and Methods
Participants
The data for this study are drawn from a larger epidemiological study of child and adolescent mental disorders conducted between April and July, 2014 (39). Thirteen primary and high schools (including two urban middle schools, four urban primary schools, three rural middle schools, and four rural primary schools) located in two cities in Hunan province, Central China, were selected for this study. A total of 18,778 students aged 6–16 years from the selected schools participated in the study. The participants' parents were asked to complete the Achenbach's Child Behavior Checklist (CBCL). There were 17,071 valid CBCL questionnaires. A total of 3,465 students were CBCL positive based on the results of the 17,071 valid CBCL questionnaires. The 3,465 CBCL positive participants and matched 3,465 CBCL negative participants further completed the Childhood Trauma Questionnaire Short Form (CTQ-SF) and Adolescent Life Events Scale (ASLEC). Ultimately, 3,147 students aged 12–16 years completed CTQ-SF and ASLEC. The present study only analyzed results from male students (n = 1,586), for who the average age was 13.57 ± 1.29 years. Among the 1,586 male students, 521 (32.8%) reported being the only child in their family, while 1,065 (67.2%) were not. Regarding environment, 442 (27.9%) lived in a city, 340 (21.4%) lived in a town, and 804 (50.7%) lived in the countryside. Regarding socio-economic status, 254 (16.02%) reported a relatively wealthy family condition, 1,237 (78%) reported an average family economic level, and the remaining 95 (6.0%) reported that their families had financial difficulties. Children and their parents (guardians) gave informed consent. Each participating student was identified by a number to maintain their anonymity. The Ethics Committee of the Second Xiangya Hospital of Central South University approved this study.
Measures
Achenbach Child Behavior Checklist (CBCL)
The CBCL (40) is composed of three parts: a general situation scale, a social ability scale, and a behavioral problem scale. The behavioral problem scale comprises 113 items related to somatic complaints, hostile behavior, hyperactivity symptoms, etc. that are grouped into nine factors. Items are scored as 1, 2, or 3 according to the response (no such problem, an occasional problem, a common problem). Thus, a higher score indicates a more severe behavioral problem. The factor score is determined as the sum of all items comprising that factor. Items 49, 51, 54, 56, and 57 are related to somatic complaints. Items 1, 8, 10, 13, 17, 20, 41, 61, 62, and 64 are related to hyperactivity symptoms. The retest reliability was 0.77–0.79 and the criterion validity was 0.61–0.76 for the Chinese version of the CBCL (41).
Childhood Trauma Questionnaire Short Form (CTQ-SF)
The CTQ-SF is composed of 28 items that form five subscales, namely emotional abuse, physical abuse, emotional neglect, physical neglect, and sexual abuse, and three validity items (18). Emotional and physical neglect is defined as inaction during the care process that results in potential or actual harm, e.g., when emotional needs are ignored by caregivers (42). Physical abuse refers to direct beating, burns, and biting, while sexual abuse refers to cases where children and adolescents participate in sexual activities that they do not fully understand, that they cannot consent to, or that violate family roles (42). Emotional abuse refers to threatening behavior, refusal and hostile verbal abuse, or exploitation (43). The questionnaire is suitable for children and adolescents aged 12–16 (44). Participants responded to each item with a score of 1, 2, 3, 4, or 5 corresponding to the frequency they experienced the specific item (never, occasionally, sometimes, often, or always). Based on previous work, we defined an emotional abuse score ≥ 13 as moderate to severe emotional abuse, a physical abuse score ≥ 10 as moderate to severe physical abuse, a sexual abuse score ≥ 8 as moderate to severe sexual abuse, an emotional neglect score ≥ 15 as moderate to severe emotional neglect, and a physical neglect score ≥ 10 points as moderate to severe physical neglect (45). If a participant experienced any kind of moderate to severe abuse or neglect, they were considered to have experienced childhood trauma. The Chinese version of the CTQ-SF has good reliability and validity, and the Cronbach α coefficient was 0.77 (46).
Adolescent Life Events Scale (ASLEC)
The ASLEC is a 27-item scale developed in 1987 by Liu et al. based on the physiological and psychological characteristics of Chinese adolescents (47). Each item relates to a common stressor experienced by adolescents over the past 12 months and the occurrence and impact of adolescent life events are evaluated. If life events occurred, items are rated on a five-point scale based on the psychological experience of the event. A higher ASLEC score indicates greater stress reaction. Due to its simplicity, the ASLEC is widely used in China (48). The Cronbach α coefficient was 0.91 and the comparative fit index was 0.9 (49).
Statistical Analysis
Data were analyzed using SPSS version 21 statistical software (IBM). Independent sample t-tests were used to compare scores of different types of abuse /total childhood trauma, somatic complaints, and ASLEC scores between the hyperactive and non-hyperactive groups. To avoid the risk of false positive results when comparing the scores of different types of abuse/total childhood trauma, Bonferroni correction was applied for multiple testing. Relationships among hyperactivity scores, ASLEC scores, somatic complaints, and CTQ-SF scores were assessed using Pearson correlation analysis. Hyperactivity scores, ASLEC scores, and CTQ-SF dimension scores were used to predict somatic complaints via linear regression. The Process 3.2 plug-in was used for the mediation analysis (selected model 4) and moderation mediation analysis (selected model 58). The mediation analysis used the bootstrapping method with 5,000 iterations. A 95% confidence interval of the bootstrapping method that did not include 0 was considered to indicate a statistically significant difference. In line with Bonferroni correction for multiple comparison testing for the different types of abuse/total childhood trauma, p < 0.0083 (0.05/6) was selected as the level of statistical significance. For other analyses, p < 0.05 was selected as the level of statistical significance.
Results
Comparison of Somatic Complaints and Childhood Trauma Scores (All Dimensions and Total Score) Between the Hyperactive Group and Non-hyperactive Group
Emotional abuse and physical abuse scores for the hyperactive group were significantly higher than those for the non-hyperactive group (all p < 0.0083). The hyperactive group also had significantly higher ASLEC and somatic complaints scores than the non-hyperactive group (both p < 0.05; Table 1).
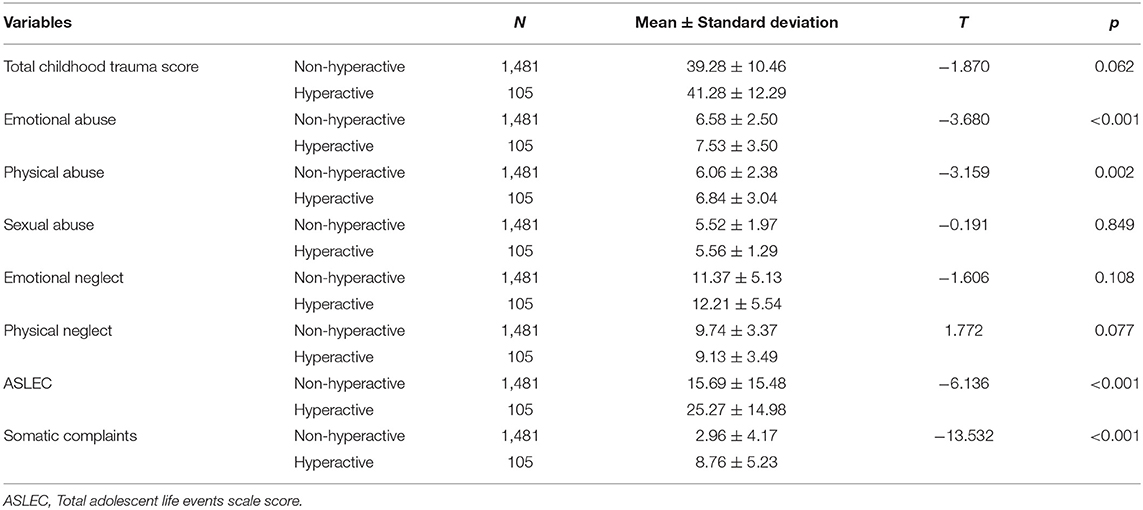
Table 1. Comparison of various childhood abuse scores, total ASLEC score, and somatic complaints between the hyperactive and non-hyperactive groups.
Correlation Analysis of All Relevant Scores
As shown in Table 2, hyperactivity score was positively related to scores for emotional abuse, physical abuse, sexual abuse, emotional neglect, ASLEC, and somatic complaints (r = 0.088–0.534, all p < 0.01). Hyperactivity score was negatively related to physical neglect score (r = −0.049, p < 0.05). Somatic complaints score was positively related to scores for emotional abuse, physical abuse, sexual abuse, emotional neglect, and ASLEC (r = 0.096–0.255, all p < 0.01). The total childhood trauma score was positively related to scores for hyperactivity, emotional abuse, physical abuse, sexual abuse, emotional neglect, physical neglect, ASLEC, and somatic complaints (r = 0.136–0.767, all p < 0.01).

Table 2. Correlations among scores for hyperactivity, childhood trauma, ASLEC, and somatic complaints (n = 1,586).
Linear Regression Model for Predicting Somatic Complaints
The results of linear regression analysis including hyperactivity, different types of childhood trauma, and life events showed that hyperactivity score (β = 0.492, p < 0.001), emotional abuse score (β = 0.119, p < 0.001), sexual abuse score (β = 0.062, p = 0.011), and ASLEC score (β = 0.06, p = 0.011) significantly predicted somatic complaints (Table 3A).
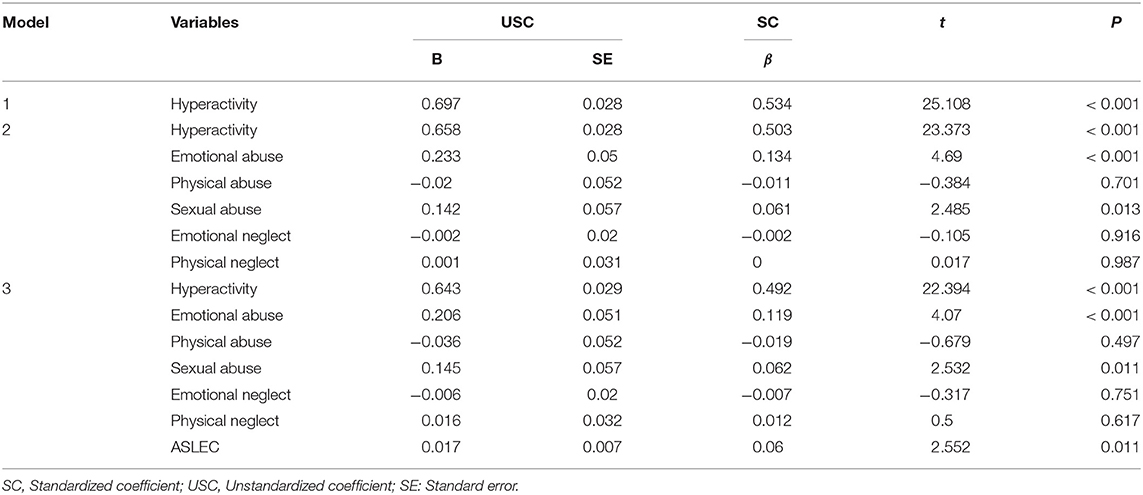
Table 3A. Linear regression analysis for hyperactivity, different types of childhood trauma, and life events predicting somatic complaints.
The results of linear regression analysis including hyperactivity, severity of childhood trauma (total childhood trauma score), and life events showed that hyperactivity score (β = 0.497, p < 0.001), total score of childhood trauma (β = 0.1, p < 0.001), and ASLEC score (β = 0.081, p < 0.001) significantly predicted somatic complaints (Table 3B).
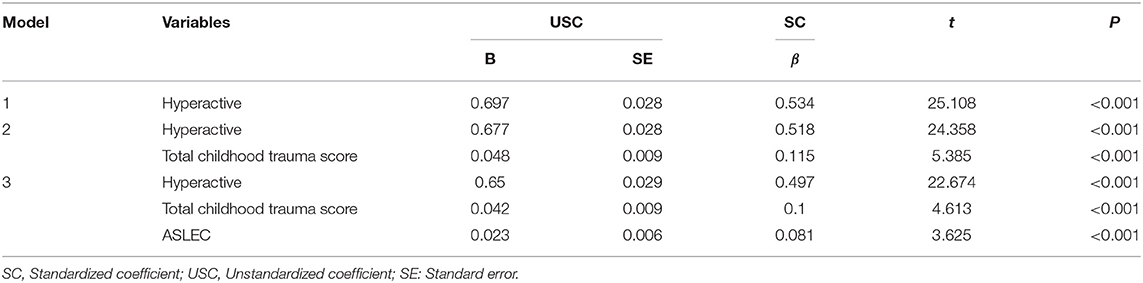
Table 3B. Linear regression analysis for hyperactivity, severity of childhood trauma, and life events predicting somatic complaints.
Mediation Analysis for the Relationship Between Hyperactivity and Somatic Complaints
Based on the hypotheses described earlier, model 4 of the Process 3.2 plug-in was used to further examine the mediating effects of childhood trauma and life events on the relationship between somatic complaints and hyperactivity. The results showed that life events and emotional abuse mediated the relationship between hyperactivity and somatic complaints (the 95% confidence interval of bootstrapping did not include 0) in the mediation model; however, the severity of childhood trauma (total childhood trauma score) did not mediate the relationship between hyperactivity and somatic complaints (the 95% confidence interval of bootstrapping included 0) in the mediation model (Tables 4A,B).

Table 4A. Test of the indirect path for different types of childhood trauma and life events mediating the relationship between hyperactivity and somatic complaints.

Table 4B. Test of the indirect path for the severity of childhood trauma and life events mediating the relationship between hyperactivity and somatic complaints.
Moderation Mediation Analysis for the Relationship Between Hyperactivity and Somatic Complaints
If a participant experienced any type of moderate to severe abuse or neglect, they were considered to have experienced childhood trauma. Based on our hypotheses, model 58 of the Process 3.2 plug-in was used to examine whether childhood trauma moderated two paths (hyperactivity → life events and life events → somatic complaints) in the mediation model. In the moderated mediation model, hyperactivity was treated as an independent variable, somatic complaints were treated as the dependent variable, life events were treated as a mediator, and the presence/absence of childhood trauma was treated as a moderator.
The results showed that childhood trauma moderated the path between hyperactivity and life events (p = 0.0076; see Figures 1, 2); however, childhood trauma did not moderate the path between life events and somatic complaints (p = 0.8802; see Figure 1) in the mediation analysis of the relationship between hyperactivity and somatic complaints. Furthermore, life events mediated the relationship between hyperactivity and somatic complaints in persons with/without childhood trauma (the 95% confidence interval of bootstrapping did not include 0; Table 5).
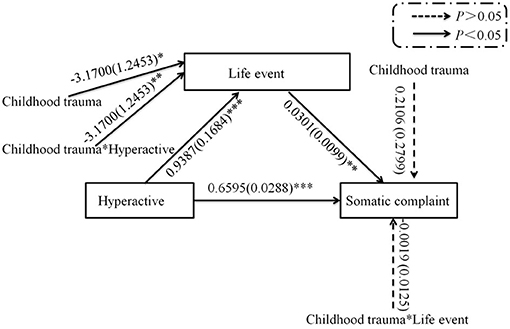
Figure 1. Path of moderation mediation analysis for the relationship between hyperactivity and somatic complaints. *p < 0.05, **p < 0.01, ***p < 0.001.

Figure 2. Childhood trauma moderated the relationship between hyperactivity and life events in moderation mediation analysis. CT, Childhood trauma.

Table 5. Test of the indirect path for the relationship between hyperactivity and somatic complaints in exposed and non-exposed childhood trauma populations in moderation mediation analysis.
Discussion
The present study is a cross-sectional study to explore the relationship between hyperactivity symptoms and somatic complaints, and the first to explore the mediating and moderating influences of recent life events and childhood trauma, in male adolescents. We found that, compared to non-hyperactive male adolescents, hyperactive male adolescents suffered more emotional abuse, physical abuse, and life events. Previous studies have found similar results in children with ADHD (50, 51). For instance, children with ADHD have higher exposure to childhood trauma than those without ADHD (52). Correlational analysis revealed that hyperactivity symptoms were associated with life events and all dimensions of childhood trauma. Hyperactive teenagers are more likely to be criticized, bullied, or injured (53), this might because they tend to violate social norms and often exhibit impulsive behavior. Additionally, parental or teacher criticism is more commonly accompanied by physical violence and verbal abuse than sexual abuse in China (54). This may partly explain the results that hyperactive male adolescents experienced more emotional and physical abuse than non-hyperactive male adolescents, while experiencing no significant difference in sexual abuse and neglect.
There is evidence that adolescents with ADHD have significantly higher somatic complaints scores than control adolescents (55, 56). Similar to previous research findings, the present study found that adolescents who screened positively for hyperactivity problems had more somatic complaints than those who screened negatively. Furthermore, correlation analysis found that somatic complaints were significantly correlated with hyperactivity symptoms as well as with childhood trauma and life events. Among adults in the general population, somatic complaints are strongly associated with reporting of past negative events (e.g., loss and abuse) (57). As expected, and consistent with previous studies (26, 58), the current study found that, among male adolescents, exposure to childhood maltreatment or adversity was correlated with somatic complaints. Notably, physical neglect was not significantly correlated with somatic complaints. It is possible that parental neglect of children's physical needs can lead to children ignoring physical discomfort or rarely complaining about physical discomfort, as such complains do not receive their parents' attention.
Previous studies of children and adolescents have found that ADHD symptoms are significantly related to somatic complaints (59) and that migraines and recurrent abdominal pain are more common in ADHD adolescents than healthy control (14). The linear regression found that hyperactivity symptoms are positively associated with somatic complaints in male adolescents. Moreover, life events, as well as childhood trauma, were found to be an important factor for somatic complaints. Growing evidence indicates that childhood trauma is associated with a significantly increased risk of medical disorders (60) and somatic complaints in adults (61, 62), that childhood adversity is associated with somatic complaints in adolescents (26), and that childhood maltreatment scores predict somatic complaints (63, 64). Our linear regression analysis further showed that emotional abuse and sexual abuse positively predicted somatic complaints, while physical abuse, emotional neglect, and physical neglect did not. Although the results for physical abuse, emotional neglect, and physical neglect showed no predictive effect in the statistical analysis, this does not mean that they have no predictive effect on somatic complaints. For instance, Ibeziako et al. found that neglect affected the range of pain sites in pediatric patients with somatic symptoms and related disorders (65). Longitudinal research is needed to verify this relationship. For boys with somatic complaints, it is necessary to teach them how to effectively cope with the adverse effects of childhood trauma, especially emotional and sexual abuse, and to cope with the challenges of hyperactivity symptoms and life events. It is well-known that stress spikes during adolescence (66). Teens who vent their emotions to close peers but do not receive supportive responses have more somatic complaints (67). Somatic complaints may be an adolescent means of coping with stress or negative emotions due to recent adversities.
The results of our mediation analysis firstly showed only emotional abuse and life events mediated the relationship between hyperactivity symptoms and somatic complaints, whereas emotional neglect, sexual abuse, physical neglect, and physical abuse did not. Moreover, total scores of childhood trauma did not have a mediating role in the analysis. This means that the effect of hyperactivity symptoms on somatic complaints is partly through emotional abuse and life events. Among male adolescents who have experienced recent life events or emotional abuse, hyperactivity symptoms may lead to more problematic somatic complaints. The reason for this pattern may be that emotional abuse in the CTQ includes blatant belittling and humiliation, and male adolescents with hyperactivity symptoms are more likely to be criticized and to experience shame for their disorderly behavior. Shame is a mechanism through which emotional abuse can lead to somatic complaints (61). Notably, Rajindrajith et al. found that emotional abuse was significantly associated with constipation in children, and that children with constipation with a history of emotional abuse had a higher somatization index compared to those with a history of sexual abuse and physical abuse (68). Emotional abuse may have a greater impact on children's somatic complaints than other forms of childhood trauma. Currently, there is no evidence of a relationship between physical abuse or physical neglect and somatic complaints (69). Considering that a previous study found a synergistic effect of childhood trauma and life events on behavioral problems (70), interventions relevant to both childhood trauma and life events are needed to reduce somatic complaints of male adolescents with hyperactivity symptoms. Our results also suggest that male adolescents with ADHD who have experienced emotional abuse may present with more somatic complaints. For such ADHD adolescents, psychotherapy could focus on childhood trauma (especially emotional abuse) and life events, and clinical treatment may need to focus not just on somatic complaints, but also on the impact of childhood trauma and life events. Reducing the occurrence of emotional abuse and life events, and improving the environment of adolescents are of great importance for the health of adolescents.
Lastly, this study found a moderating role of childhood trauma in the mediation model for hyperactivity symptoms → life events. This finding is consistent with our hypothesis that male adolescents with hyperactivity symptoms and a history of childhood trauma exposure would have more somatic complaints when experiencing recent life events. However, the mechanism for this relationship is unclear. It could be linked to post-traumatic changes in brain function or HPA axis responsiveness to stress (37). Based on the findings described above, interventions to address somatic complaints in male adolescents with hyperactivity symptoms should consider the effects of trauma and life events alone, and the interaction between childhood traumatic experiences and life events should be addressed.
Limitations
This study is subject to several limitations. First, as this is a cross-sectional study with recall bias, further study is needed to explore causal relationships. Second, this study only examined the influence of childhood trauma and life events on the relationship between hyperactivity symptoms and somatic complaints in the general population. For applications in ADHD, this relationship needs to be tested in ADHD patients. Third, there may be some overlap between childhood trauma and life events that occur in adolescence, which may impact the results of this study. Fourth, the childhood trauma measure used in this study only investigated severity, and did not consider age at the time of trauma or frequency of trauma, which may affect the results. Fifth, it is well-known that self-evaluation is suitable for assessing internalizing behaviors; however, for externalizing behaviors (like hyperactivity), external evaluation is better. This may affect the validity or reliability of the results.
Conclusion
Hyperactivity symptoms, childhood trauma, and life events were all found to impact somatic complaints among male adolescents. This study firstly found that emotional abuse and life events mediated the relationship between hyperactivity symptoms and somatic complaints, and that childhood trauma had moderating effects on the path between hyperactivity symptoms and life events in the mediation model for predicting somatic complaints. In light of these findings, interventions to address somatic complaints among male adolescents with hyperactivity symptoms should consider the impact of childhood trauma and life events.
Data Availability Statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding authors.
Ethics Statement
The studies involving human participants were reviewed and approved by The Ethics Committee of the Second Xiangya Hospital of Central South University. Children and their parents (guardians) gave informed consent.
Author Contributions
SW and TY was responsible for writing the manuscript. YH was responsible for data processing and writing the manuscript. XC participated in the design, investigation, and evaluation of the study. XL participated in the design, investigation, and evaluation of the study and contributed to critical revision. JL participated in the investigation and contributed to critical revision. All authors have read and approved the manuscript.
Funding
This study was supported by the National Science and Technology Support Plan - Epidemiological Investigation of Mental Disorders among Chinese Children and Adolescents (Grant No. 2012BAI01B02), Science and Technology Innovation Committee of Shenzhen (JCYJ20190809155019338), Guangdong Basic and Applied Basic Research Foundation (2019A1515110047), and Hunan Provincial Innovation Foundation for Postgraduates (Grant No. CX2019159).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Association AP. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). Washington, DC: American Psychiatric Pub (2013).
2. Rydell M, Lundström S, Gillberg C, Lichtenstein P, Larsson H. Has the attention deficit hyperactivity disorder phenotype become more common in children between 2004 and 2014? Trends over 10 years from a Swedish general population sample. J Child Psychol Psychiatry. (2018) 59:863–71. doi: 10.1111/jcpp.12882
3. Xu G, Strathearn L, Liu B, Yang B, Bao W. Twenty-year trends in diagnosed attention-deficit/hyperactivity disorder among US children and adolescents, 1997-2016. JAMA Netw Open. (2018) 1:e181471. doi: 10.1001/jamanetworkopen.2018.1471
4. Wang T, Liu K, Li Z, Xu Y, Liu Y, Shi W, et al. Prevalence of attention deficit/hyperactivity disorder among children and adolescents in China: a systematic review and meta-analysis. BMC Psychiatry. (2017) 17:32. doi: 10.1186/s12888-016-1187-9
5. Cortese S, Faraone SV, Bernardi S, Wang S, Blanco C. Gender differences in adult attention-deficit/hyperactivity disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). J Clin Psychiatry. (2016) 77:e421–8. doi: 10.4088/JCP.14m09630
6. Banaschewski T, Brandeis D, Heinrich H, Albrecht B, Brunner E, Rothenberger A. Association of ADHD and conduct disorder–brain electrical evidence for the existence of a distinct subtype. J Child Psychol Psychiatry. (2003) 44:356–76. doi: 10.1111/1469-7610.00127
7. D'Agati E, Curatolo P, Mazzone L. Comorbidity between ADHD and anxiety disorders across the lifespan. Int J Psychiatry Clin Pract. (2019) 23:238–44. doi: 10.1080/13651501.2019.1628277
8. Mulraney M, Schilpzand EJ, Hazell P, Nicholson JM, Anderson V, Efron D, et al. Comorbidity and correlates of disruptive mood dysregulation disorder in 6-8-year-old children with ADHD. Eur Child Adolesc Psychiatry. (2016) 25:321–30. doi: 10.1007/s00787-015-0738-9
9. Noordermeer SDS, Luman M, Greven CU, Veroude K, Faraone SV, Hartman CA, et al. Structural brain abnormalities of attention-deficit/hyperactivity disorder with oppositional defiant disorder. Biol Psychiatry. (2017) 82:642–50. doi: 10.1016/j.biopsych.2017.07.008
10. Perroud N, Cordera P, Zimmermann J, Michalopoulos G, Bancila V, Prada P, et al. Comorbidity between attention deficit hyperactivity disorder (ADHD) and bipolar disorder in a specialized mood disorders outpatient clinic. J Affect Disord. (2014) 168:161–6. doi: 10.1016/j.jad.2014.06.053
11. Reale L, Bartoli B, Cartabia M, Zanetti M, Costantino MA, Canevini MP, et al. Comorbidity prevalence and treatment outcome in children and adolescents with ADHD. Eur Child Adolesc Psychiatry. (2017) 26:1443–57. doi: 10.1007/s00787-017-1005-z
12. Muskens JB, Velders FP, Staal WG. Medical comorbidities in children and adolescents with autism spectrum disorders and attention deficit hyperactivity disorders: a systematic review. Eur Child Adolesc Psychiatry. (2017) 26:1093–103. doi: 10.1007/s00787-017-1020-0
13. Egger HL, Costello EJ, Erkanli A, Angold A. Somatic complaints and psychopathology in children and adolescents: stomach aches, musculoskeletal pains, and headaches. J Am Acad Child Adolesc Psychiatry. (1999) 38:852–60. doi: 10.1097/00004583-199907000-00015
14. Kutuk MO, Tufan AE, Guler G, Yalin OO, Altintas E, Bag HG, et al. Migraine and associated comorbidities are three times more frequent in children with ADHD and their mothers. Brain Dev. (2018) 40:857–64. doi: 10.1016/j.braindev.2018.06.001
15. Santalahti P, Aromaa M, Sourander A, Helenius H, Piha J. Have there been changes in children's psychosomatic symptoms? A 10-year comparison from Finland. Pediatrics. (2005) 115:e434–42. doi: 10.1542/peds.2004-1261
16. Gaub M, Carlson CL. Gender differences in ADHD: a meta-analysis and critical review. J Am Acad Child Adolesc Psychiatry. (1997) 36:1036–45. doi: 10.1097/00004583-199708000-00011
17. Rucklidge JJ. Gender differences in attention-deficit/hyperactivity disorder. Psychiatr Clin North Am. (2010) 33:357–73. doi: 10.1016/j.psc.2010.01.006
18. Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. (2003) 27:169–90. doi: 10.1016/S0145-2134(02)00541-0
19. Stern A, Agnew-Blais J, Danese A, Fisher HL, Jaffee SR, Matthews T, et al. Associations between abuse/neglect and ADHD from childhood to young adulthood: a prospective nationally-representative twin study. Child Abuse Negl. (2018) 81:274–85. doi: 10.1016/j.chiabu.2018.04.025
20. Capusan AJ, Kuja-Halkola R, Bendtsen P, Viding E, McCrory E, Marteinsdottir I, et al. Childhood maltreatment and attention deficit hyperactivity disorder symptoms in adults: a large twin study. Psychol Med. (2016) 46:2637–46. doi: 10.1017/S0033291716001021
21. González RA, Vélez-Pastrana MC, McCrory E, Kallis C, Aguila J, Canino G, et al. Evidence of concurrent and prospective associations between early maltreatment and ADHD through childhood and adolescence. Soc Psychiatry Psychiatr Epidemiol. (2019) 54:671–82. doi: 10.1007/s00127-019-01659-0
22. Sari Gokten E, Saday Duman N, Soylu N, Uzun ME. Effects of attention-deficit/hyperactivity disorder on child abuse and neglect. Child Abuse Negl. (2016) 62:1–9. doi: 10.1016/j.chiabu.2016.10.007
23. Schilpzand EJ, Sciberras E, Alisic E, Efron D, Hazell P, Jongeling B, et al. Trauma exposure in children with and without ADHD: prevalence and functional impairment in a community-based study of 6-8-year-old Australian children. Europ Child Adolesc Psychiatry. (2018) 27:811–9. doi: 10.1007/s00787-017-1067-y
24. Sibley MH, Altszuler AR, Morrow AS, Merrill BM. Mapping the academic problem behaviors of adolescents with ADHD. Sch Psychol Q. (2014) 29:422–37. doi: 10.1037/spq0000071
25. Nandagopal JJ, Fleck DE, Adler CM, Mills NP, Strakowski SM, DelBello MP. Impulsivity in adolescents with bipolar disorder and/or attention-deficit/hyperactivity disorder and healthy controls as measured by the Barratt Impulsiveness Scale. J Child Adolesc Psychopharmacol. (2011) 21:465–8. doi: 10.1089/cap.2010.0096
26. Oh DL, Jerman P, Silvério Marques S, Koita K, Purewal Boparai SK, Burke Harris N, et al. Systematic review of pediatric health outcomes associated with childhood adversity. BMC Pediatr. (2018) 18:83. doi: 10.1186/s12887-018-1037-7
27. Achenbach J, Rhein M, Gombert S, Meyer-Bockenkamp F, Buhck M, Eberhardt M, et al. Childhood traumatization is associated with differences in TRPA1 promoter methylation in female patients with multisomatoform disorder with pain as the leading bodily symptom. Clin Epigenetics. (2019) 11:126. doi: 10.1186/s13148-019-0731-0
28. Villalonga-Olives E, Rojas-Farreras S, Vilagut G, Palacio-Vieira JA, Valderas JM, Herdman M, et al. Impact of recent life events on the health related quality of life of adolescents and youths: the role of gender and life events typologies in a follow-up study. Health Qual Life Outcomes. (2010) 8:71. doi: 10.1186/1477-7525-8-71
29. Kraan T, Velthorst E, Smit F, de Haan L, van der Gaag M. Trauma and recent life events in individuals at ultra high risk for psychosis: review and meta-analysis. Schizophr Res. (2015) 161:143–9. doi: 10.1016/j.schres.2014.11.026
30. Semeijn EJ, Comijs HC, Kooij JJ, Michielsen M, Beekman AT, Deeg DJ. The role of adverse life events on depression in older adults with ADHD. J Affect Disord. (2015) 174:574–9. doi: 10.1016/j.jad.2014.11.048
31. Counts CA, Nigg JT, Stawicki JA, Rappley MD, von Eye A. Family adversity in DSM-IV ADHD combined and inattentive subtypes and associated disruptive behavior problems. J Am Acad Child Adolesc Psychiatry. (2005) 44:690–8. doi: 10.1097/01.chi.0000162582.87710.66
32. Friedrichs B, Igl W, Larsson H, Larsson JO. Coexisting psychiatric problems and stressful life events in adults with symptoms of ADHD–a large Swedish population-based study of twins. J Atten Disord. (2012) 16:13–22. doi: 10.1177/1087054710376909
33. Bonvanie IJ, Janssens KA, Rosmalen JG, Oldehinkel AJ. Life events and functional somatic symptoms: a population study in older adolescents. Br J Psychol. (2017) 108:318–33. doi: 10.1111/bjop.12198
34. Walker LS, Garber J, Greene JW. Somatic complaints in pediatric patients: a prospective study of the role of negative life events, child social and academic competence, and parental somatic symptoms. J Consult Clin Psychol. (1994) 62:1213–21. doi: 10.1037/0022-006X.62.6.1213
35. Stickley A, Koyanagi A, Takahashi H, Ruchkin V, Inoue Y, Kamio Y. Attention-deficit/hyperactivity disorder and physical multimorbidity: a population-based study. Eur Psychiatry. (2017) 45:227–34. doi: 10.1016/j.eurpsy.2017.07.010
36. Weissman DG, Lambert HK, Rodman AM, Peverill M, Sheridan MA, McLaughlin KA. Reduced hippocampal and amygdala volume as a mechanism underlying stress sensitization to depression following childhood trauma. Depress Anxiety. (2020) 37:916–25. doi: 10.1002/da.23062
37. Zhong X, Ming Q, Dong D, Sun X, Cheng C, Xiong G, et al. Childhood maltreatment experience influences neural response to psychosocial stress in adults: an fMRI study. Front Psychol. (2019) 10:2961. doi: 10.3389/fpsyg.2019.02961
38. Janiri D, Moccia L, Dattoli L, Pepe M, Molinaro M, De Martin V, et al. Emotional dysregulation mediates the impact of childhood trauma on psychological distress: first Italian data during the early phase of COVID-19 outbreak. Aust N Z J Psychiatry. (2021) 9:4867421998802. doi: 10.1177/0004867421998802
39. Shen YM, Chan BSM, Liu JB, Zhou YY, Cui XL, He YQ, et al. The prevalence of psychiatric disorders among students aged 6~ 16 years old in central Hunan, China. BMC Psychiatry. (2018) 18:243. doi: 10.1186/s12888-018-1823-7
40. Achenbach, Thomas M. Empirically based assessment and taxonomy: applications to clinical research. Psychol Assess. (1995) 7:261–74. doi: 10.1037/1040-3590.7.3.261
41. Su LY, Li XR, Luo XR, Wan GB, Yang ZW. The norms of Achenbach Child Behaviour Checklist in Hunan province(in Chinese version). Chin J Clin Psychol. (1996) 4:24–8.
42. Gonzalez D, Bethencourt Mirabal A, McCall JD. Child Abuse and Neglect. StatPearls. Treasure Island, FL: StatPearls Publishing LLC (2021).
43. Li ET, Carracher E, Bird T. Linking childhood emotional abuse and adult depressive symptoms: the role of mentalizing incapacity. Child Abuse Negl. (2020) 99:104253. doi: 10.1016/j.chiabu.2019.104253
44. Bernstein DP, Ahluvalia T, Pogge D, Handelsman L. Validity of the Childhood Trauma Questionnaire in an adolescent psychiatric population. J Am Acad Child Adolesc Psychiatry. (1997) 36:340–8. doi: 10.1097/00004583-199703000-00012
45. Bernstein D, Fink L, Bernstein D. Childhood Trauma Questionnaire: a retrospective self-report manual (1998).
46. Zhao XF, Zhang YL, Li LF, Zhou YF, Li HZ, Yang SC. Reliability and validity of the Chinese version of childhood trauma questionnaire (in Chinese version). Chin J Clin Rehab. (2005) 20:105–7.
47. Liu XC, Liu LQ, Yang J, Chai FX, Wang AZ M, SL, et al. The adolescent self-rating life events checklist and its reliability and validity (in Chinese version). Chin J Clin Psychol. (1997) 5:34–6.
48. Xin XH, Yao SQ. Validity and reliability of the Adolescent Self-rating Life Events Checklist in middle school students (in Chinese version). Chin Ment Health J. (2015) 29:355–60.
49. Chen H, Jia CX, Liu XC. Psychometric properties and application of Adolescent Self-Rating Life Events Checklist(ASLEC) (in Chinese version). Chin J Public Health. (2016) 32:1116–9.
50. Zou S, Yu W, Liang S, Ma X, Li D, Bian Y, et al. The association between child abuse and emotional and behavioral problems in Chinese school-aged boys with attention deficit hyperactivity disorder. J Nerv Ment Dis. (2019) 207:869–74. doi: 10.1097/NMD.0000000000001041
51. Brown NM, Brown SN, Briggs RD, Germán M, Belamarich PF, Oyeku SO. Associations between adverse childhood experiences and adhd diagnosis and severity. Acad Pediatr. (2017) 17:349–55. doi: 10.1016/j.acap.2016.08.013
52. Gul H, Gurkan CK. Child maltreatment and associated parental factors among children with ADHD: a comparative study. J Atten Disord. (2018) 22:1278–88. doi: 10.1177/1087054716658123
53. Spinks AB, Nagle C, Macpherson AK, Bain C, McClure RJ. Host factors and childhood injury: the influence of hyperactivity and aggression. J Dev Behav Pediatr. (2008) 29:117–23. doi: 10.1097/DBP.0b013e318163c3b0
54. Fang X, Fry DA, Ji K, Finkelhor D, Chen J, Lannen P, et al. The burden of child maltreatment in China: a systematic review. Bull World Health Organ. (2015) 93:176–85C. doi: 10.2471/BLT.14.140970
55. Oncü B, Oner O, Oner P, Erol N, Aysev A, Canat S. Symptoms defined by parents' and teachers' ratings in attention-deficit hyperactivity disorder: changes with age. Can J Psychiatry. (2004) 49:487–91. doi: 10.1177/070674370404900711
56. Cho S-C, Kim B-N, Kim J-W, Rohde LA, Hwang J-W, Chungh D-S, et al. Full syndrome and subthreshold attention-deficit/hyperactivity disorder in a Korean community sample: comorbidity and temperament findings. Eur Child Adolesc Psychiatry. (2009) 18:447–57. doi: 10.1007/s00787-009-0755-7
57. Garnefski N, van Rood Y, de Roos C, Kraaij V. Relationships between traumatic life events, cognitive emotion regulation strategies, and somatic complaints. J Clin Psychol Med Settings. (2017) 24:144–51. doi: 10.1007/s10880-017-9494-y
58. Shanahan L, Zucker N, Copeland WE, Bondy CL, Egger HL, Costello EJ. Childhood somatic complaints predict generalized anxiety and depressive disorders during young adulthood in a community sample. Psychol Med. (2015) 45:1721–30. doi: 10.1017/S0033291714002840
59. Chen T-J, Ji C-Y, Wang S-S, Lichtenstein P, Larsson H, Chang Z. Genetic and environmental influences on the relationship between ADHD symptoms and internalizing problems: a Chinese twin study. Am J Med Genet B Neuropsychiatr Genet. (2016) 171:931–7. doi: 10.1002/ajmg.b.32411
60. Nemeroff CB. Paradise lost: the neurobiological and clinical consequences of child abuse and neglect. Neuron. (2016) 89:892–909. doi: 10.1016/j.neuron.2016.01.019
61. Kealy D, Rice SM, Ogrodniczuk JS, Spidel A. Childhood trauma and somatic symptoms among psychiatric outpatients: Investigating the role of shame and guilt. Psychiatry Res. (2018) 268:169–74. doi: 10.1016/j.psychres.2018.06.072
62. Easton SD, Kong J. Mental health indicators fifty years later: a population-based study of men with histories of child sexual abuse. Child Abuse Negl. (2017) 63:273–83. doi: 10.1016/j.chiabu.2016.09.011
63. Sesar K, Zivcić-Bećirević I, Sesar D. Multi-type maltreatment in childhood and psychological adjustment in adolescence: questionnaire study among adolescents in Western Herzegovina Canton. Croat Med J. (2008) 49:243–56. doi: 10.3325/cmj.2008.2.243
64. Bonvanie IJ, van Gils A, Janssens KAM, Rosmalen JGM. Sexual abuse predicts functional somatic symptoms: an adolescent population study. Child Abuse Negl. (2015) 46:1–7. doi: 10.1016/j.chiabu.2015.06.001
65. Ibeziako P, Randall E, Vassilopoulos A, Choi C, Thomson K, Ribeiro M, et al. Prevalence, patterns, and correlates of pain in medically hospitalized pediatric patients with somatic symptom and related disorders. J Acad Consult Liaison Psychiatry. (2021) 62:46–55. doi: 10.1016/j.psym.2020.05.008
66. Hartman CA, Rommelse N, van der Klugt CL, Wanders RBK, Timmerman ME. Stress exposure and the course of ADHD from childhood to young adulthood: comorbid severe emotion dysregulation or mood and anxiety problems. J Clin Med. (2019) 8:1824. doi: 10.3390/jcm8111824
67. Parr NJ, Zeman J, Braunstein K, Price N. Peer emotion socialization and somatic complaints in adolescents. J Adolesc. (2016) 50:22–30. doi: 10.1016/j.adolescence.2016.04.004
68. Rajindrajith S, Devanarayana NM, Lakmini C, Subasinghe V, de Silva DG, Benninga MA. Association between child maltreatment and constipation: a school-based survey using Rome III criteria. J Pediatr Gastroenterol Nutr. (2014) 58:486–90. doi: 10.1097/MPG.0000000000000249
69. Rueness J, Myhre Md MC, Strøm IF, Wentzel-Larsen T, Dyb G, Thoresen S. Child abuse and physical health: a population-based study on physical health complaints among adolescents and young adults. Scand J Public Health. (2020) 48:511–8. doi: 10.1177/1403494819848581
Keywords: hyperactivity symptoms, trauma, life events, somatic complaints, male adolescents
Citation: Wu S, Yang T, He Y, Cui X, Luo X and Liu J (2021) Association Between Hyperactivity Symptoms and Somatic Complaints: Mediating and Moderating Mechanisms in Childhood Trauma and Life Events Among Chinese Male Adolescents. Front. Psychiatry 12:630845. doi: 10.3389/fpsyt.2021.630845
Received: 18 November 2020; Accepted: 10 August 2021;
Published: 16 September 2021.
Edited by:
Jean Marc Guile, University of Picardie Jules Verne, FranceReviewed by:
Stéphanie Bioulac, Centre Hospitalier Universitaire de Bordeaux, FranceHeejeong Yoo, Seoul National University, South Korea
Copyright © 2021 Wu, Yang, He, Cui, Luo and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jianbo Liu, amlhbmJvbGl1QGFsaXl1bi5jb20=; Xuerong Luo, bHVveHVlcm9uZ0Bjc3UuZWR1LmNu
†These authors have contributed equally to this work and share first authorship
 Shuxian Wu
Shuxian Wu Tingyu Yang1,2†
Tingyu Yang1,2† Yuqiong He
Yuqiong He Xilong Cui
Xilong Cui Xuerong Luo
Xuerong Luo