
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Psychiatry , 09 April 2021
Sec. Social Neuroscience
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.628110
 XiaoGuang Lin1
XiaoGuang Lin1 XueLing Zhang1
XueLing Zhang1 QinQin Liu1
QinQin Liu1 PanWen Zhao2
PanWen Zhao2 JianGuo Zhong3
JianGuo Zhong3 PingLei Pan4
PingLei Pan4 GenDi Wang3†
GenDi Wang3† ZhongQuan Yi2*†
ZhongQuan Yi2*†Multiple sclerosis (MS) is an immune-mediated demyelinating disease of the central nervous system. Studies have shown that MS disrupts several social cognitive abilities [including empathy and theory of mind (ToM)]. Overall ToM deficits in MS are well documented, but how the specific ToM subcomponents and empathic capacity are affected remains unclear. For this meta-analysis, we searched PubMed, Web of Science, and Embase from inception to July 2020. Effect sizes were calculated using Hedges g with a random-effects model. Thirty-three studies were included. Relative to healthy controls (HCs), patients with MS were moderately impaired in overall empathy (g = −0.67), overall ToM (g = −74), cognitive ToM (g = −0.72), and the overlapping domains of cognitive empathy/affective ToM (g = −0.79); no group differences were identified for affective empathy (g = −0.19). Compared with HCs, patients with relapsing-remitting MS (RRMS) and progressive MS were impaired in overall empathy, overall ToM, cognitive ToM, and cognitive empathy/affective ToM, without significant RRMS–progressive MS differences in impairment degree. We conducted the first meta-analytic review investigating the empathy and ToM functioning patterns in patients with MS and examined the overlapping and distinct subcomponents of these constructs. The findings suggest differential impairment of the core aspects of social cognitive processing in patients with MS, which may importantly inform the development of structured social cognitive MS interventions.
Multiple sclerosis (MS) is an immune-mediated demyelinating disease of the central nervous system (1), which is characterized by multifocal destruction of the myelin sheath and axonal loss (2, 3). Patients usually develop sensorimotor, visual, and emotional symptoms as well as cognitive impairment, leading to functional disability and reduced quality of life (QoL) (4). The precise etiology of MS remains unclear, and the prognosis is variable and unpredictable.
Cognitive impairment has been recognized as a common symptom in MS, with an estimated lifetime occurrence of 40–65% (5–7). The cognitive domains generally affected include executive functioning, information processing speed, attention, and memory (8, 9), and social cognition (10–14). Social cognition, a basic means for the individual to perceive, encode, store, retrieve, and regulate information regarding other people and the self (15), has a remarkable impact on interpersonal communication and QoL (16–19). Social cognition is a multidimensional construct, mainly involving four dimensions: empathy, theory of mind (ToM), social perception and social knowledge, and attribution bias (15, 17).
One core aspect of social cognition, i.e., empathy, refers to the ability to understand and identify the mental states of others, as well as the ability to share the feelings of others (20). It is a complex construct with multiple components, usually including affective and cognitive domains. Emotional empathy is described as “I feel your feelings” and can be regarded as primitive empathy, while cognitive empathy refers to “I understand your feelings” and can be regarded as advanced empathy (21–23). This is significant in clinical practice, as any deficit in cognitive or affective empathy can lead to atypical emotional reactions, but the clinical treatment implications differ (20, 24). Recently, several studies have assessed empathy deficits in patients with MS with inconsistent findings. For example, Realmuto et al. (25) and van der Hiele et al. (26) found no differences between patients with MS and healthy controls (HCs) in terms of empathy, whereas Kraemer et al. (27) found moderate impairment in empathy in patients with MS compared to HCs. These inconsistent findings may be related to low statistical power, as many of these studies enrolled small sample sizes. To answer important clinical questions, a quantitative meta-analysis is needed to test the magnitude and significance of empathy in MS to increase the statistical power and refine the conclusions derived from the inconsistent findings of the previous studies.
ToM, another core domain of social cognition, refers to the ability to attribute mental states (beliefs, intentions, and desires) to others and to use the attributions to understand and predict behavior (28, 29). Like empathy, ToM can also be divided into affective and cognitive components (30). Affective ToM refers to the capacity to understand others' emotional states, and cognitive ToM is the ability to infer other's thoughts, intentions, and beliefs (31). To our knowledge, two recent meta-analyses examined ToM differences between patients with MS and HCs. Cotter et al. and Bora et al. calculated the overall ToM score based on numerous different ToM tasks (a combination of affective ToM and cognitive ToM tasks) and found that patients with MS have ToM deficits (32, 33). However, it remains unclear whether these defects were attributable to only one or both subcomponents, as no specific subgroup analysis was conducted for affective and cognitive ToM.
Notably, although there are differences between cognitive empathy and affective ToM in definition (34), these two constructs are difficult to distinguish at a purely behavioral level of assessment because they both involve attribution of another's emotional states (35). Additionally, overlap between cognitive empathy and affective ToM has often been noted (24, 36, 37). Therefore, in this study, we considered cognitive empathy and affective ToM to be interchangeable.
To this end, the present study aimed to provide the first meta-analytic integration of broader empathy and ToM in MS with the affective and cognitive subcomponents of both these abilities distinguished. Moreover, specific subgroup analyses for the overlapping components (cognitive empathy and affective ToM) and separate components (cognitive ToM and affective empathy) were also conducted. Besides, considering that MS is a heterogeneous disease, with subtypes and diverse trajectories, in influx between relapse, remission, stability, and progression (38, 39), we performed subgroup analyses (including of relapsing-remitting MS [RRMS] and progressive MS (including progressive primary MS and secondary progressive MS).
In addition, studies have reported that certain clinical behavioral symptoms may have a significant relationship with social cognition (40–44). Clinically, depression and anxiety are common behavioral symptoms in patients with MS (45–50), and it has been reported that social cognitive deficits are significantly related to the severity of depressive symptoms or anxiety symptoms in some diseases (40–42, 44). So far, the exact relationship between social cognitive performance and the severity of depression or anxiety in patients with MS remains unclear. Therefore, we evaluated the effect of potential variables [such as sex (ratio of female patients in the MS group), mean age, education level, disease duration, Expanded Disability Status Scale (EDSS) score, quality assessment score, severity of depression, and severity of anxiety] on social cognition. With this meta-analysis, we hope to promote a more comprehensive and nuanced understanding of how these two core domains of social cognition are affected in MS.
This study was performed per the Preferred Reporting Items of Systematic Review and Meta-Analysis (PRISMA) guidelines (51). This protocol was prospectively registered at the International Platform of Registered Systematic Review and Meta-analysis Protocols (ID: INPLASY202070029) and has been released in the journal of Medicine (52).
A systematic literature search was conducted across the PubMed, Web of Science, and Embase databases from inception to July 2020. The following search terms were used: “multiple sclerosis” or “MS” or “clinically isolated syndrome” combined with: “social cognition” or “theory of mind” or “ToM” or “mentalizing” or “mentalizing” or “Reading the Mind in the Eyes Test” or “Faux pas task” or “False Belief” or “the Awareness of Social Inference Test” or “Virtual Assessment of Mentalising Ability” or “the Movie for the Assessment of Social Cognition” or “picture sequencing task” or “Cartoon Test” or “Hinting Test” or “Strange Stories Test” or “facial expression*” or “prosody” or “pragmatic impairment” or “non-literal language” or “sarcas*” or “lie*” or “joke*” or “empath*” or “perspective taking” or “Peer-Report Social Functioning Scale.” Furthermore, other resources, such as the reference lists of all included studies, were searched manually.
Studies were included if they met four criteria. First, the study should have compared patients with MS to a matched HC group. Second, the study should have assessed empathy performance or ToM performance using standard measures. Third, the study should have provided sufficient data to calculate the effect sizes of empathy or ToM. Fourth, the study should have been published in a peer-reviewed journal in English.
Studies were excluded for three reasons. First, if the participant overlapped with a participant in another study with a larger sample size. Second, if they lacked an HC group. Third, if they included <10 participants to ensure the reliability of the outcome (29).
Article retrieval, screening, data extraction, and quality evaluation were independently completed by two investigators. The relevant data extracted included: (a) Title information, such as first author, publication year, and title; (b) Sample characteristics from the MS and HC groups, such as sample size, sex (female and male), mean age, education level, disease duration, EDSS scores, severity of depression, and severity of anxiety; (c) For both empathy and ToM, tasks were divided into affective and cognitive subcomponents, and the classification was based on the nature of the task and the information provided by the author of the original article; (d) The data used for calculating the effect sizes of empathy or ToM. Any disagreements were first discussed between these two investigators, and further disagreements were arbitrated by a third investigator.
To assess study quality, a nine-star protocol was used based on the Newcastle-Ottawa Scale for case-control studies. Studies with ≥7 stars were considered high-quality (53).
Meta-analyses were conducted using the Stata 15.0 software package (54). The effect size (Hedges g) and 95% confidence interval (CI) were calculated to estimate differences in ToM and empathy between the MS and HC groups (55). The magnitude of Hedges g could be interpreted using Cohen d effect size conventions, and effect sizes were deemed small, moderate, or large when their values were equal to or larger than 0.2, 0.5, or 0.8, respectively (56).
When studies did not provide a total mean score on a particular measure but reported subscores (i.e., individual ToM tasks presented separately), pooled effect sizes were aggregated by computing the mean effect size (and standard error) (57). Similarly, when studies reported the effect size per subgroup [i.e., by clinical subtypes (relapsing MS and progressive MS)], data were pooled into an overall effect size (57). Meta-analyses were completed using a random-effects model, as it better accommodates heterogeneous effect distributions.
The degree of heterogeneity within effect size estimates was tested with the I2 statistic, and the degree of heterogeneity was deemed low, moderate, or large when I2 was equal to or larger than 0, 50, or 75%, respectively (58).
To assess the risk of publication bias, Egger's test was used. For this analysis, significance indicates that bias may be present [p < 0.05; (59)]. Additionally, the trim-and-fill analyses were applied, providing effect sizes adjusted for publication bias (60).
Meta-regression analyses were conducted to investigate whether demographic and clinical variables (including age, sex, education level, disease duration, and EDSS score, quality assessment score, severity of depression, and severity of anxiety) explained the variance in any of the effects identified. As a measure of severity of depression or anxiety, according to accepted cut-off scores of depression or anxiety rating scales used, studies were classified as no symptoms = 0, mild symptoms = 1, moderate symptoms = 2, severe symptoms = 3 (41, 61–63). For each of these analyses, a minimum of 10 data points was required for each relevant predictor variable and the social cognitive ability under assessment (64).
The flow chart of the study selection process is shown in Figure 1. In total, 34,365 potentially eligible articles were retrieved. After the removal of duplicates, 29,601 articles remained, which were then subjected to title and abstract screening. Of these, 43 initially met the inclusion criteria. Three of these studies did not include an HC group (65–67); another three were excluded for lack of sufficient data to calculate the effect sizes and standard errors of empathy or ToM (18, 68, 69). Four studies were excluded, as their samples overlapped with those of other studies (14, 70–72). Eventually, 33 studies with 1,568 patients with MS (mean age = 40.71 years, SD = 9.63 years, 70.4% female) and 1,283 HCs (mean age = 39.18 years, SD = 9.91 years, 65.3% female) were included in the meta-analysis [Table 1; (4, 11–13, 25–27, 46, 48, 50, 63, 73–94)].
The results of the study quality assessment are shown in Table 2. The mean score was 7.11 (SD = 0.83), and 29 of the 35 case-control studies were awarded ≥7 stars and considered of high quality.
Table 3 reports the key results from this meta-analysis. Compared to HCs, patients with MS were impaired in overall empathy, with this deficit being moderate in magnitude (g = −0.67, 95% CI [−0.84, −0.50], K = 27; see Figure 2). Patients with MS were also moderately impaired in their overall ToM ability (g = −0.74, 95% CI [−0.88, −0.61], K = 34; see Figure 3). Examining the overlapping and distinct subcomponents of these constructs revealed that MS was associated with moderate deficits in cognitive ToM (g = −0.72, 95% CI [−0.92, −0.51], K = 22; see Figure 4) and cognitive empathy/affective ToM (g = −0.79, 95% CI [−0.96, −0.62], K = 25; see Figure 5). However, no group differences were evident for affective empathy (g = −0.19, 95% CI [−0.63, 0.26], K = 3; see Figure 6). There was no heterogeneity across studies for affective empathy (I2 = 0) and moderate heterogeneity across studies for overall ToM (I2 = 70.8%), overall empathy (I2 = 74.1%), and affective ToM/cognitive empathy (I2 = 68.9%), but there was significant heterogeneity in studies for cognitive ToM (I2 = 82.3%). Egger's test was not significant for overall empathy, overall ToM, cognitive ToM, or cognitive empathy/affective ToM. Egger's test was only significant for affective empathy (p = 0.005). However, a trim-and-fill analysis did not result in imputation of any studies, and the effect size remained similar (g = −0.23, 95% CI [–0.63, 0.18]).
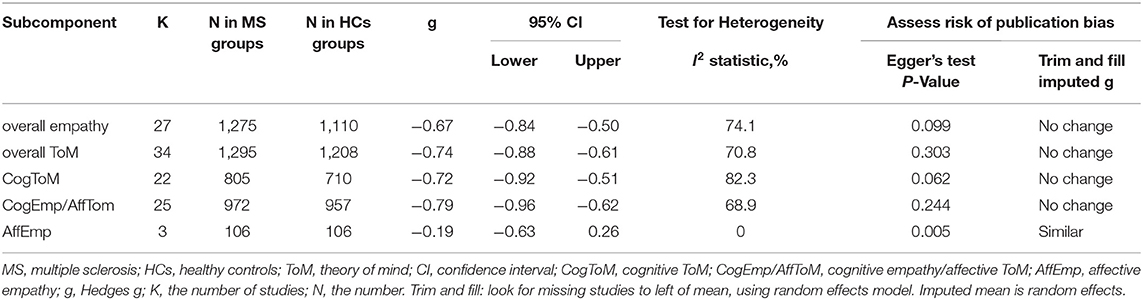
Table 3. Mean effects for ToM and empathy subcomponents comparing participants with multiple sclerosis against healthy controls and tests for publication bias.
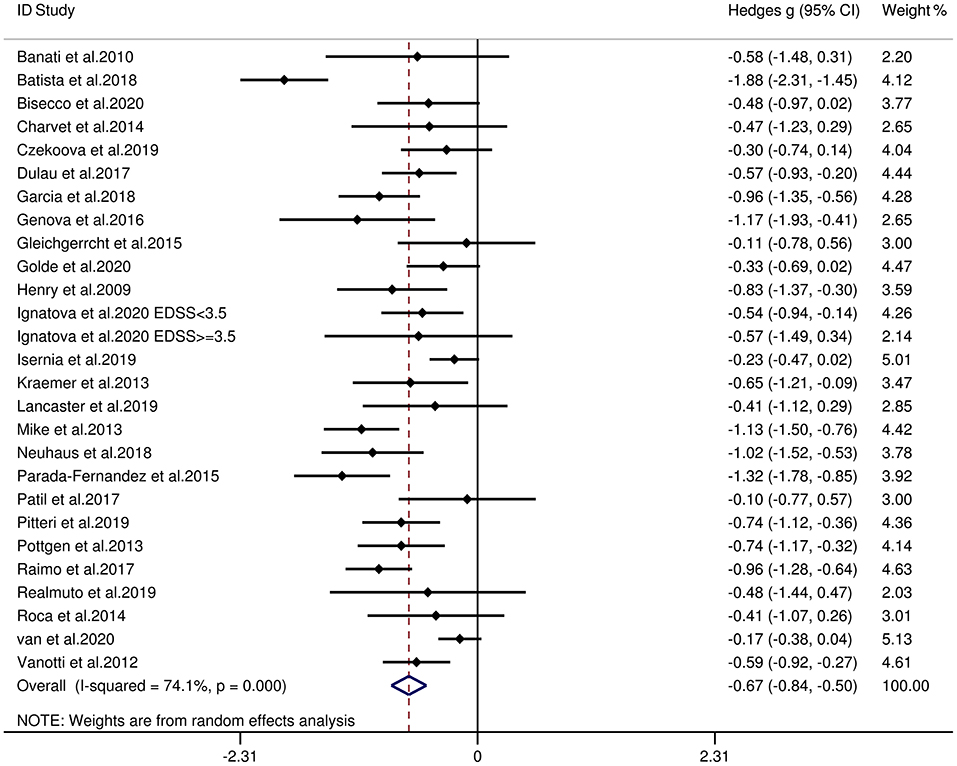
Figure 2. Forest plots showing effect size estimates (Hedges g) for overall empathy differences between MS and healthy controls. CI, confidence interval; MS, multiple sclerosis; ToM, theory of mind.
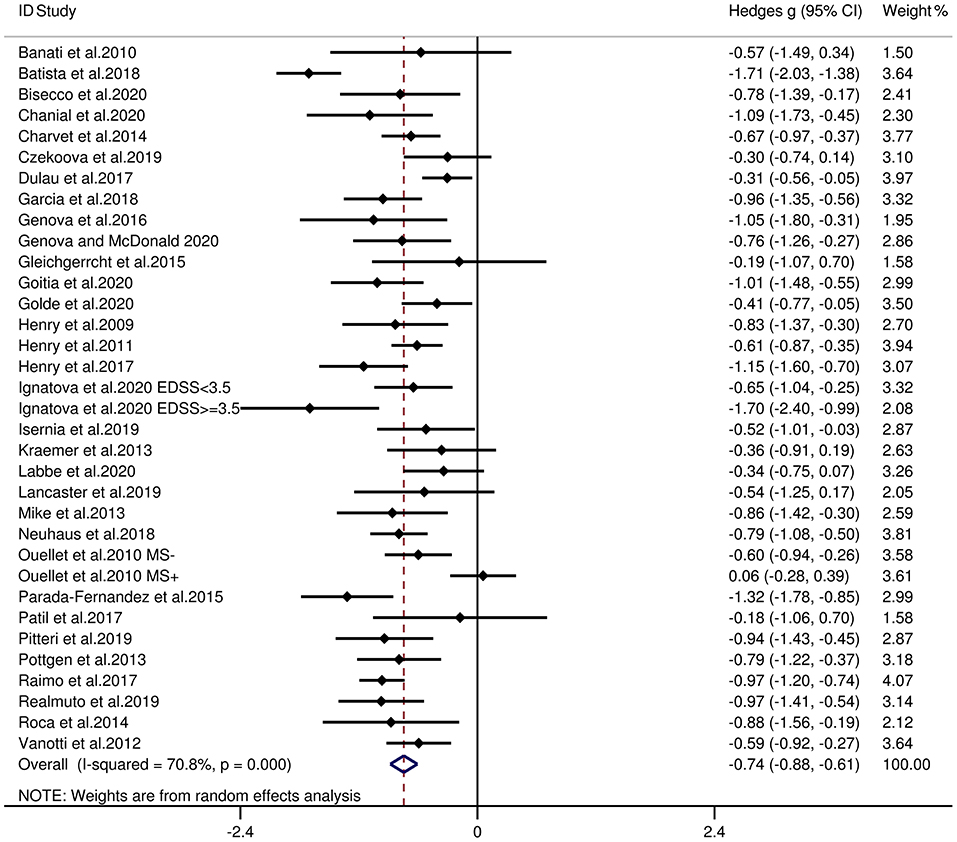
Figure 3. Forest plots showing effect size estimates (Hedges g) for overall ToM differences between MS and healthy controls. CI, confidence interval; MS, multiple sclerosis; ToM, theory of mind.
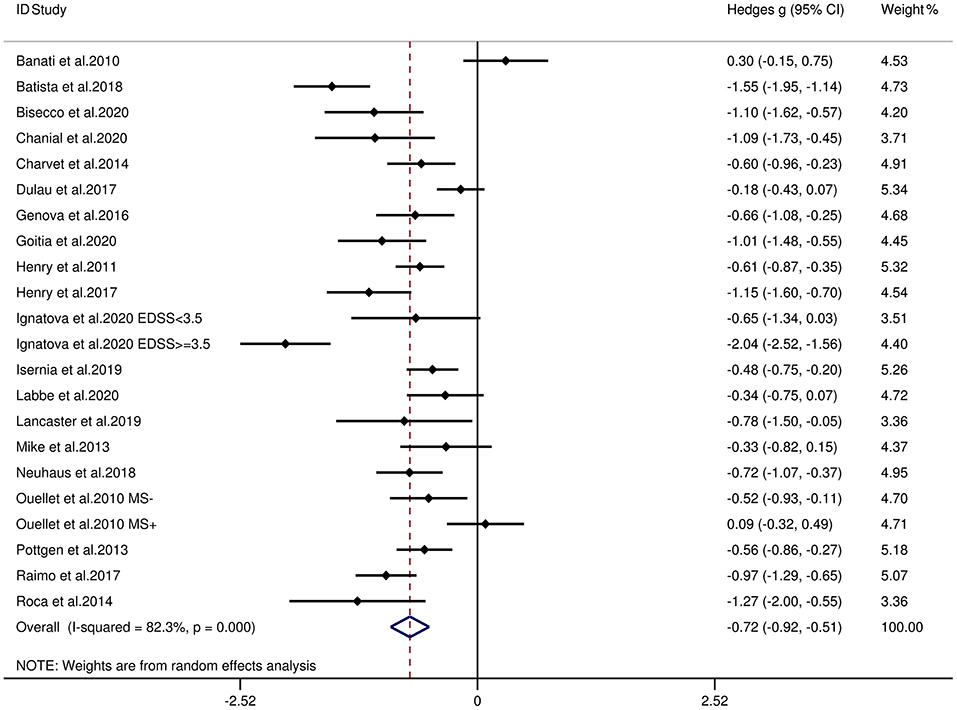
Figure 4. Forest plots showing effect size estimates (Hedges g) for cognitive ToM differences between MS and healthy controls. CI, confidence interval; MS, multiple sclerosis; ToM, theory of mind.
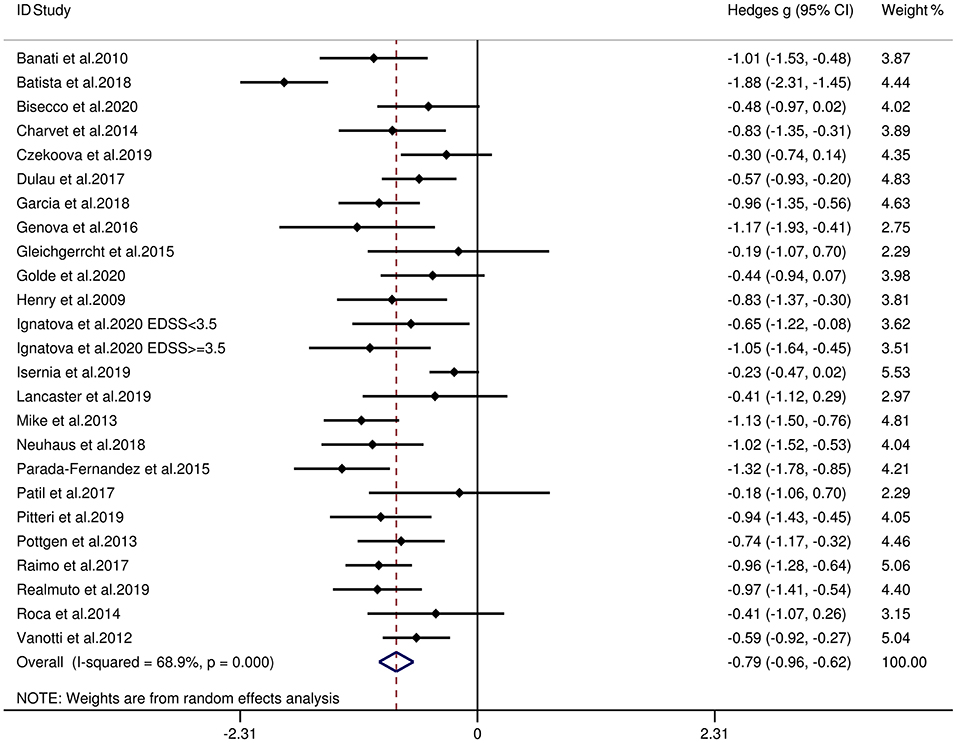
Figure 5. Forest plots showing effect size estimates (Hedges g) for cognitive empathy/affective ToM differences between MS and healthy controls. CI, confidence interval; MS, multiple sclerosis; ToM, theory of mind.
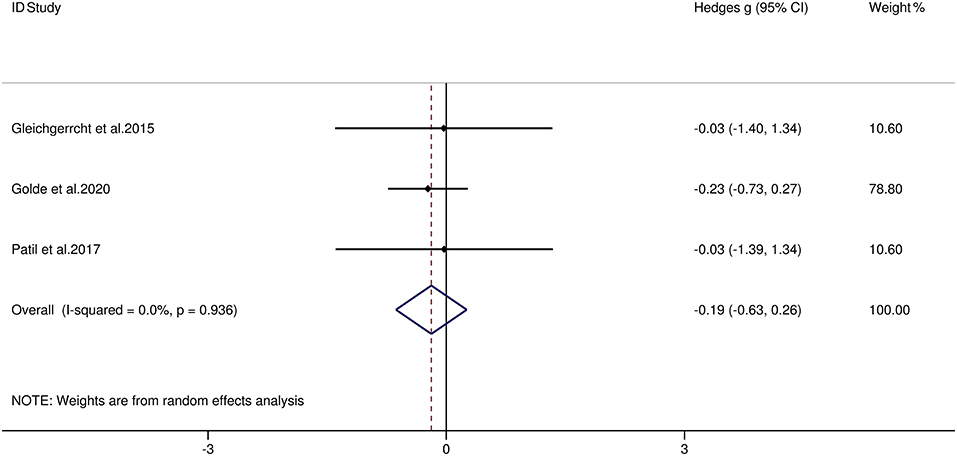
Figure 6. Forest plots showing effect size estimates (Hedges g) for affective empathy differences between MS and healthy controls. CI, confidence interval; MS, multiple sclerosis; ToM, theory of mind.
Table 4 reports the key results from this meta-analysis. Relative to HCs, patients with RRMS exhibited low impairment in overall empathy (g = −0.43, 95% CI [−0.57, −0.29], K = 17), and moderate impairment in overall ToM ability (g = −0.67, 95% CI [−0.82, −0.52], K = 20). Examining the overlapping and distinct subcomponents of these constructs revealed that RRMS was associated with significant and large-sized deficits in cognitive ToM (g = −0.83, 95% CI [−1.17, −0.50], K = 11) and cognitive empathy/affective ToM (g = −0.59, 95% CI [−0.77, −0.41], K = 15). However, no group differences were evident for affective empathy (g = −0.19, 95% CI [−0.63, 0.26], K = 3). There was no heterogeneity across studies for affective empathy (I2 = 0), low heterogeneity across studies for overall empathy (I2 = 39.1%), and moderate heterogeneity across studies for overall ToM (I2 = 53.3%) and affective ToM/cognitive empathy (I2 = 52.2%), but there was significant variation among studies for cognitive ToM (I2 = 85.4%). Egger's test was not significant for overall ToM, overall empathy, cognitive ToM, or affective ToM/cognitive empathy. Egger's test was only significant for affective empathy. However, a trim-and-fill analysis did not result in imputation of any studies, and the effect size remained similar.
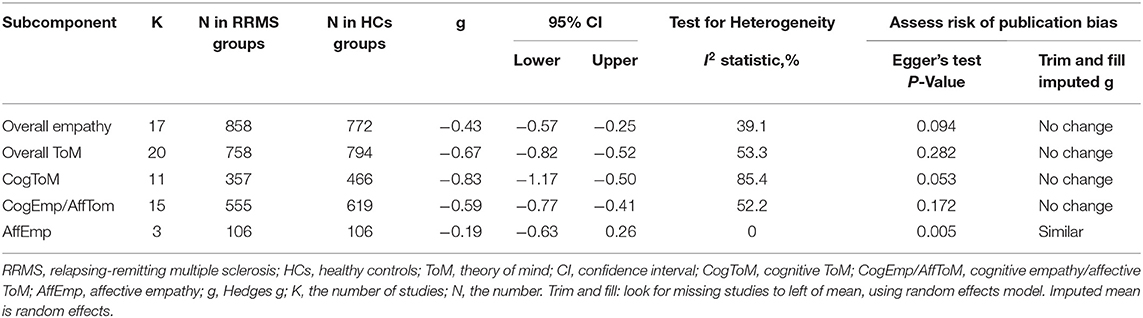
Table 4. Mean effects for ToM and empathy subcomponents comparing participants with relapsing-remitting multiple sclerosis against healthy controls and tests for publication bias.
Table 5 reports the key results from this meta-analysis. Relative to HCs, patients with progressive MS exhibited a moderate-sized deficit in overall empathy (g = −0.50, 95% CI [−0.73, −0.27], K = 4), overall ToM ability (g = −0.75, 95% CI [−1.08, −0.41], K = 7, cognitive ToM (g = −0.72, 95% CI [−1.15, −0.29], K = 6), and affective ToM/cognitive empathy (g = −0.50, 95% CI [−0.73, −0.27], K = 4). No analysis for affective empathy was conducted, as no such studies were included in the meta-analysis. There was no heterogeneity across studies for overall empathy (I2 = 0) and affective ToM/cognitive empathy (I2 = 0) and moderate heterogeneity across studies for overall ToM (I2 = 65%), but there was significant variation among studies for cognitive ToM (I2 = 75.5%). Egger's test was not significant for overall ToM, overall empathy, cognitive ToM, or affective ToM/cognitive empathy.
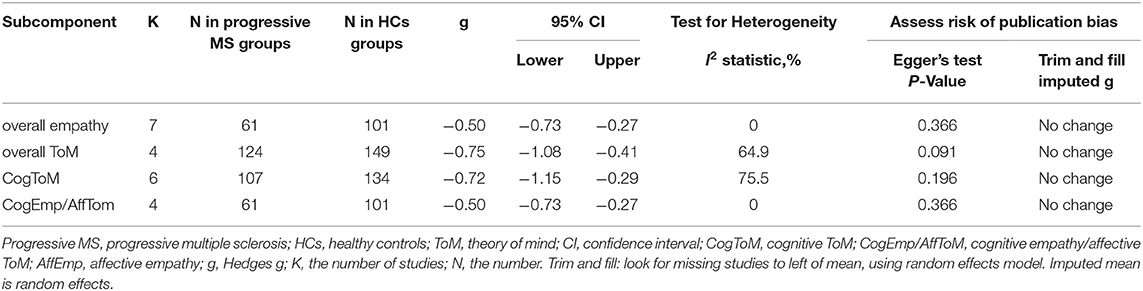
Table 5. Mean effects for ToM and empathy subcomponents comparing participants with progressive multiple sclerosis against healthy controls and tests for publication bias.
Table 6 reports the key results from this meta-analysis. Relative to patients with progressive MS, patients with RRMS showed no difference in overall empathy (g = 0.21, 95% CI [−0.23, 0.65], K = 2), overall ToM (g = 0.11, 95% CI [−0.09, 0.31], K = 3), cognitive ToM (g = 0.05, 95% CI [−0.14, 0.24], K = 3), and affective ToM/cognitive empathy (g = 0.21, 95% CI [−0.23, 0.65], K = 2). No analysis for affective empathy was conducted, as no such studies were included in this meta-analysis. There was low heterogeneity across studies for overall ToM (I2 = 23.7%) and cognitive ToM (I2 = 15.4%) and moderate heterogeneity across studies for overall empathy (I2 = 63.2%) and cognitive empathy/affective ToM (I2 = 63.2%). Egger's test was not significant for overall ToM and cognitive ToM.
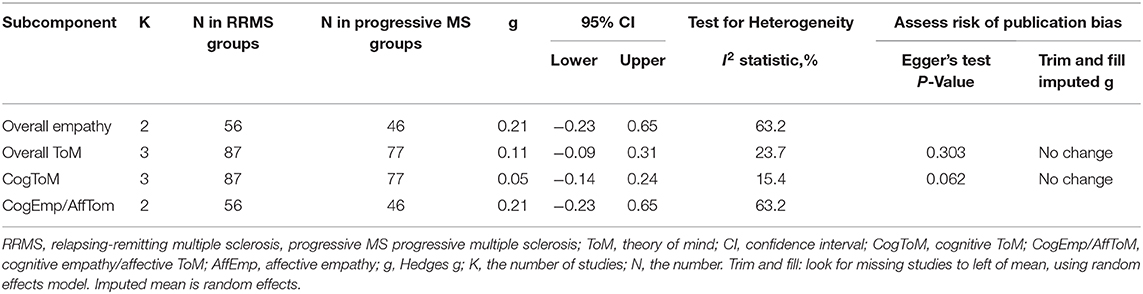
Table 6. Mean effects for ToM and empathy subcomponents comparing participants with relapsing-remitting multiple sclerosis against progressive multiple sclerosis and tests for publication bias.
Meta-regression analyses showed that the included variables did not account for significant variance across studies. The variables (age, sex, education level, disease duration, EDSS score, quality assessment score, severity of depression, and severity of anxiety) did not account for significant variance in overall empathy(p = 0.871, 0.218, 0.582, 0.996, 0.712, 0.318, 0.671, and 0.871, respectively), overall ToM (p = 0.825, 0.341, 0.832, 0.245, 0.527, 0.535, 0.068, and 0.224, respectively), cognitive ToM (p = 0.961, 0.418, 0.89, 0.997, 0.831, 0.098, 0.423, NA, respectively), or cognitive empathy/affective ToM (p = 0.548, 0.516, 0.61, 0.634, 0.549, 0.589, 0.48, and 0.872, respectively). No meta-regression analyses were conducted for the severity of anxiety in cognitive ToM, as fewer than 10 studies contributed to the data for this subcomponent.
To our knowledge, this was the first meta-analysis to investigate the patterns of empathy and ToM functioning in patients with MS. The meta-analysis included 33 studies, with combined samples of 1,568 individuals with MS and 1,283 HCs. Relative to the HC group, the MS group showed moderate impairments in both overall empathy (g = −0.67) and overall ToM (g = −0.74). Among the overlapping and distinct subcomponents of these constructs, MS was associated with moderate impairment in cognitive ToM (g = −0.72) and cognitive empathy/affective ToM (g = −0.79), but no significant difference was found in affective empathy. Subgroup analyses showed that compared with the HCs, patients with RRMS and progressive MS were both impaired in overall empathy, overall ToM, cognitive ToM, and cognitive empathy/affective ToM, and there was no statistical difference between RRMS and progressive MS in the degree of impairment. Meta-regression analysis indicated that the examined variables (age, sex, education level, disease duration, EDSS score, quality assessment score, severity of depression, and severity of anxiety) did not affect the magnitude of the effect sizes observed.
For overall empathy, a moderate effect size was found (g = −0.67). When focusing on the subcomponents of empathy, patients with MS were found to have moderate impairment in cognitive empathy; however, there was no difference in affective empathy. The quantitative findings support the conclusions of previous qualitative studies, indicating that cognitive and affective empathy are separate and have different requirements for effortful processing (81, 83, 90). Specifically, cognitive empathy/affective ToM, requiring attention and time, is a slow and laborious process, while affective empathy, operating with minimal conscious awareness, is an automatic and spontaneous response (95). Therefore, these two empathic components may present different challenges for patients with MS. As affective empathy has low cognitive requirements, it might be expected that this ability remains relatively preserved in MS. This disconnection between the cognitive and affective subcomponents of empathy has been confirmed in several other neurological diseases. For example, in patients with Alzheimer's disease, there was a moderate-sized deficit in cognitive empathy/affective ToM, but no impairment in affective empathy (96). Patients with Parkinson's disease, compared to HCs, PD had significant impairment in cognitive empathy/affective ToM, but no group differences were identified in affective empathy (97). However, the findings should be interpreted with caution in this meta-analysis due to the limited number of included studies contributing to the effect size of affective empathy (K = 3).
The results pertaining to overall ToM impairment supported the findings of Bora et al. (32) and Cotter et al. (33), showing that overall ToM is moderately impaired in MS. When considering the sub-components of ToM, some previous studies have suggested that the domains of cognitive and affective ToM are dissociated, and the function of cognitive empathy/affective ToM in MS is conserved, but cognitive ToM is impaired (74, 85, 88, 93). However, findings from the current quantitative meta-analysis do not support this suggestion, which showed that patients of MS had moderate impairment in both cognitive and affective ToM and their degrees of defect were close (g = −0.72 and g = −0.79, respectively). This impairment may be related to white matter (WM) damage in MS. On the macro-structure, ToM impairment is associated with T1 and T2 lesions (65, 71, 88); on the microstructure, ToM impairment is shown to be related to the disconnection with the social brain network caused by diffuse normal-appearing white matter damage in MS, especially in tracts of limbic pathways (uncinate fasciculus, fornix) and callosal interhemispheric fibers (corpus callosum, tapetum) (72), which play a key role in social and communication skills or emotional processing (98–100). In addition, gray matter (GM) pathology is considered to have an important role in ToM impairment. GM atrophy was found in the cingulate, orbitofrontal, cerebellar cortex, and insula decreased was found (65, 66, 72), which are involved in cognitive and affective ToM network (101). Several studies based on magnetic resonance imaging (MRI) have found that amygdala atrophy is the main predictor of ToM impairment in MS (66, 72). Besides, one resting-state functional MRI study found that there was an association between ToM impairment and functional connectivity changes in the default mode network, executive network, and limbic network in MS (74).
In the subgroup meta-analyses, the results showed that compared with HCs, patients with RRMS and progressive MS were impaired in overall empathy, overall ToM, cognitive ToM, and cognitive empathy/affective ToM, and there was no statistical difference between RRMS and progressive MS in overall empathy, overall ToM, cognitive ToM, and cognitive empathy/affective ToM. This result is inconsistent with the previous quantitative results of Bora et al., which indicated that social cognition tended to be more impaired in progressive MS in comparison to RRMS. However, it should be noted that the aforementioned Bora et al. study calculated a social cognition score based on numerous very different ToM tasks and facial emotion recognition tasks (another core domain of social cognition). Besides, due to the limited number of included studies contributing to the comparison between RRMS and progressive MS (K = 3 in this study, K = 5 in the study by Bora et al.), we should cautiously interpret the results.
Our meta-analysis findings may contribute to the development of cognitive rehabilitation for MS. Several studies have shown that cognitive rehabilitation intervention may have a positive impact on MS symptoms (102–104). In particular, depression symptoms, anxiety, fatigue, pain, physical vitality, and sleep quality improved significantly after most of the cognitive rehabilitation intervention (104–107). Besides, studies have shown that cognitive rehabilitation can improve the cognitive function in patients with MS, mainly focusing on general cognitive functions such as memory, executive function, attention, and processing speed (102, 104, 108–112). However, there are few studies about how the cognitive interventions affect social cognitive in MS. Our meta-analytic findings can broaden the theoretical understanding of MS, which may help improve or formulate cognitive intervention strategies.
The current meta-analysis has some limitations. First, although 33 studies were included in this meta-analysis, only three contributed to the mean effect size for affective empathy between patients with MS and HCs. In addition, only three studies provided data comparing RRMS and progressing MS; hence, more research in this area is needed in the future. Second, we only included cross-sectional studies, while more longitudinal studies are needed to investigate the dynamic changes in empathy and ToM function in patients of MS. Third, although we investigated some demographic and clinical variables (including age, sex, education level, disease duration, EDSS scores, severity of depression, and severity of anxiety) that may affect empathy and ToM function, other factors [such as prior substance abuse or some other behavioral symptoms (including apathy, inflexible, obsessive, sometimes with flattened affect, suspiciousness, etc.)] were not examined due to the limited data available in the original studies (67, 113, 114). Further studies are required to comprehensively elucidate the potential effects of these factors on empathy- and ToM-associated features in MS. Fifth, there was heterogeneity between the individual tasks for the assessment of ToM or empathy, and further development of standardized batteries for ToM/empathy assessment in MS is needed. For example, the Measurement and Treatment Research to Improve Cognition in Schizophrenia Cognition in Schizophrenia (MATRICS) Consensus Cognitive Battery (MCCB) (115), which makes it possible to standardize the evaluation of cognitive outcomes in schizophrenia, may also be adapted for MS.
The results of this meta-analysis suggest that patients with MS exhibited moderate impairment in broad constructs of ToM and empathy and the ToM subcomponents (cognitive ToM and affective ToM/cognitive empathy), but no significant impairment in affective empathy. These quantitative results suggest a differential impairment of the core aspects of social cognitive (including empathy and ToM) processing in patients with MS, which may greatly inform the development of structured social cognitive interventions in MS.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
ZY and GW: study design and critical revision of the manuscript. XL, XZ, QL, PZ, JZ, and PP: analysis and interpretation of data. XL and XZ: drafting of the manuscript. All authors: approval of the final version for submission.
This work was supported by Jiangsu Commission of Health (LGY20180390).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We thank all the authors of the studies included. This protocol was prospectively registered at the International Platform of Registered Systematic Review and Meta-analysis Protocols (ID: INPLASY202070029) and has been released in the journal of Medicine (52).
1. Rolf L, Muris AH, Theunissen R, Hupperts R, Damoiseaux J, Smolders J. Vitamin D(3) supplementation and the IL-2/IL-2R pathway in multiple sclerosis: attenuation of progressive disturbances? J Neuroimmunol. (2018) 314:50–7. doi: 10.1016/j.jneuroim.2017.11.007
2. Buchanan RJ, Minden SL, Chakravorty BJ, Hatcher W, Tyry T, Vollmer T. A pilot study of young adults with multiple sclerosis: demographic, disease, treatment, and psychosocial characteristics. Disabil Health J. (2010) 3:262–70. doi: 10.1016/j.dhjo.2009.09.003
3. Motl RW, Sandroff BM, Kwakkel G, Dalgas U, Feinstein A, Heesen C, et al. Exercise in patients with multiple sclerosis. Lancet Neurol. (2017) 16:848–56. doi: 10.1016/s1474-4422(17)30281-8
4. Henry A, Tourbah A, Chaunu MP, Rumbach L, Montreuil M, Bakchine S. Social cognition impairments in relapsing-remitting multiple sclerosis. J Int Neuropsychol Soc. (2011) 17:1122–31. doi: 10.1017/s1355617711001147
5. Benedict RH, Cookfair D, Gavett R, Gunther M, Munschauer F, Garg N, et al. Validity of the minimal assessment of cognitive function in multiple sclerosis (MACFIMS). J Int Neuropsychol Soc. (2006) 12:549–58. doi: 10.1017/s1355617706060723
6. Sanfilipo MP, Benedict RH, Weinstock-Guttman B, Bakshi R. Gray and white matter brain atrophy and neuropsychological impairment in multiple sclerosis. Neurology. (2006) 66:685–92. doi: 10.1212/01.wnl.0000201238.93586.d9
7. Chalah MA, Ayache SS. Deficits in social cognition: an unveiled signature of multiple sclerosis. J Int Neuropsychol Soc. (2017) 23:266–86. doi: 10.1017/s1355617716001156
8. Jongen PJ, Ter Horst AT, Brands AM. Cognitive impairment in multiple sclerosis. Minerva Med. (2012) 103:73–96.
9. Miller E, Morel A, Redlicka J, Miller I, Saluk J. Pharmacological and non-pharmacological therapies of cognitive impairment in multiple sclerosis. Curr Neuropharmacol. (2018) 16:475–83. doi: 10.2174/1570159x15666171109132650
10. Phillips LH, Henry JD, Scott C, Summers F, Whyte M, Cook M. Specific impairments of emotion perception in multiple sclerosis. Neuropsychology. (2011) 25:131–6. doi: 10.1037/a0020752
11. Neuhaus M, Bagutti S, Yaldizli Ö, Zwahlen D, Schaub S, Frey B, et al. Characterization of social cognition impairment in multiple sclerosis. Eur J Neurol. (2018) 25:90–6. doi: 10.1111/ene.13457
12. Pitteri M, Genova H, Lengenfelder J, DeLuca J, Ziccardi S, Rossi V, et al. Social cognition deficits and the role of amygdala in relapsing remitting multiple sclerosis patients without cognitive impairment. Mult Scler Relat Disord. (2019) 29:118–23. doi: 10.1016/j.msard.2019.01.030
13. Genova HM, McDonald S. Social cognition in individuals with progressive multiple sclerosis: a pilot study using TASIT-S. J Int Neuropsychol Soc. (2020) 26:539–44. doi: 10.1017/s1355617719001371
14. Isernia S, Cabinio M, Pirastru A, Mendozzi L, Di Dio C, Marchetti A, et al. Theory of mind network in multiple sclerosis: a double disconnection mechanism. Soc Neurosci. (2020) 15:544–57. doi: 10.1080/17470919.2020.1766562
15. Green MF, Horan WP, Lee J. Social cognition in schizophrenia. Nat Rev Neurosci. (2015) 16:620–31. doi: 10.1038/nrn4005
16. Rao SM, Leo GJ, Ellington L, Nauertz T, Bernardin L, Unverzagt F. Cognitive dysfunction in multiple sclerosis. II Impact on employment and social functioning. Neurology. (1991) 41:692–6. doi: 10.1212/wnl.41.5.692
17. Green MF, Penn DL, Bentall R, Carpenter WT, Gaebel W, Gur RC, et al. Social cognition in schizophrenia: an NIMH workshop on definitions, assessment, and research opportunities. Schizophr Bull. (2008) 34:1211–20. doi: 10.1093/schbul/sbm145
18. Krause M, Wendt J, Dressel A, Berneiser J, Kessler C, Hamm AO, et al. Prefrontal function associated with impaired emotion recognition in patients with multiple sclerosis. Behav Brain Res. (2009) 205:280–5. doi: 10.1016/j.bbr.2009.08.009
19. Bora E, Walterfang M, Velakoulis D. Theory of mind in Parkinson's disease: a meta-analysis. Behav Brain Res. (2015) 292:515–20. doi: 10.1016/j.bbr.2015.07.012
20. Henry JD, von Hippel W, Molenberghs P, Lee T, Sachdev PS. Clinical assessment of social cognitive function in neurological disorders. Nat Rev Neurol. (2016) 12:28–39. doi: 10.1038/nrneurol.2015.229
21. Wondra JD, Ellsworth PC. An appraisal theory of empathy and other vicarious emotional experiences. Psychol Rev. (2015) 122:411–28. doi: 10.1037/a0039252
22. Bartochowski Z, Gatla S, Khoury R, Al-Dahhak R, Grossberg GT. Empathy changes in neurocognitive disorders: a review. Ann Clin Psychiatry. (2018) 30:220–32.
23. Chen J. Empathy for distress in humans and rodents. Neurosci Bull. (2018) 34:216–36. doi: 10.1007/s12264-017-0135-0
24. Dvash J, Shamay-Tsoory SG. Theory of mind and empathy as multidimensional constructs. Top Langu Disord. (2014) 34:282–95. doi: 10.1097/TLD.0000000000000040
25. Realmuto S, Dodich A, Meli R, Canessa N, Ragonese P, Salemi G, et al. Moral Cognition and multiple sclerosis: a neuropsychological study. Archiv Clin Neuropsychol. (2019) 34:319–26. doi: 10.1093/arclin/acy047
26. van der Hiele K, van Egmond EEA, Jongen PJ, van der Klink JJL, Beenakker EAC, van Eijk JJJ, et al. Empathy in multiple sclerosis–correlates with cognitive, psychological and occupational functioning. Mult Scler Relat Disord. (2020) 41:102036. doi: 10.1016/j.msard.2020.102036
27. Kraemer M, Herold M, Uekermann J, Kis B, Wiltfang J, Daum I, et al. Theory of mind and empathy in patients at an early stage of relapsing remitting multiple sclerosis. Clin Neurol Neurosurg. (2013) 115:1016–22. doi: 10.1016/j.clineuro.2012.10.027
28. McDonald S, Flanagan S. Social perception deficits after traumatic brain injury: interaction between emotion recognition, mentalizing ability, and social communication. Neuropsychology. (2004) 18:572–9. doi: 10.1037/0894-4105.18.3.572
29. Leppanen J, Sedgewick F, Treasure J, Tchanturia K. Differences in the theory of mind profiles of patients with anorexia nervosa and individuals on the autism spectrum: a meta-analytic review. Neurosci Biobehav Rev. (2018) 90:146–63. doi: 10.1016/j.neubiorev.2018.04.009
30. Yi Z, Zhao P, Zhang H, Shi Y, Shi H, Zhong J, et al. Theory of mind in Alzheimer's disease and amnestic mild cognitive impairment: a meta-analysis. Neurol Sci. (2020) 41:1027–39. doi: 10.1007/s10072-019-04215-5
31. Heitz C, Noblet V, Phillipps C, Cretin B, Vogt N, Philippi N, et al. Cognitive and affective theory of mind in dementia with Lewy bodies and Alzheimer's disease. Alzheimers Res Ther. (2016) 8:10. doi: 10.1186/s13195-016-0179-9
32. Bora E, Özakbaş S, Velakoulis D, Walterfang M. Social cognition in multiple sclerosis: a meta-analysis. Neuropsychol Rev. (2016) 26:160–72. doi: 10.1007/s11065-016-9320-6
33. Cotter J, Firth J, Enzinger C, Kontopantelis E, Yung AR, Elliott R, et al. Social cognition in multiple sclerosis: a systematic review and meta-analysis. Neurology. (2016) 87:1727–36. doi: 10.1212/wnl.0000000000003236
34. Singer T. The neuronal basis and ontogeny of empathy and mind reading: review of literature and implications for future research. Neurosci Biobehav Rev. (2006) 30:855–63. doi: 10.1016/j.neubiorev.2006.06.011
35. Bensalah L, Caillies S, Anduze M. Links among cognitive empathy, theory of mind, and affective perspective taking by young children. J Genet Psychol. (2016) 177:17–31. doi: 10.1080/00221325.2015.1106438
36. Shamay-Tsoory SG, Aharon-Peretz J, Perry D. Two systems for empathy: a double dissociation between emotional and cognitive empathy in inferior frontal gyrus versus ventromedial prefrontal lesions. Brain. (2009) 132(Pt 3):617–27. doi: 10.1093/brain/awn279
37. Preckel K, Kanske P, Singer T. On the interaction of social affect and cognition: empathy, compassion and theory of mind. Curr Opin Behav Sci. (2018) 19:1–6. doi: 10.1016/j.cobeha.2017.07.010
38. Jacques F, Lublin F. Defining the clinical course of multiple sclerosis: the 2013 revisions. Neurology. (2015) 84:963. doi: 10.1212/01.wnl.0000462309.76486.c5
39. Martin SJ, Mcglasson S, Hunt D, Overell J. Cerebrospinal fluid neurofilament light chain in multiple sclerosis and its subtypes: a meta-analysis of case–control studies. J Neurol Neurosurg Psychiatry. (2019) 90:1059–67. doi: 10.1136/jnnp-2018-319190
40. Achim AM, Ouellet R, Lavoie MA, Vallières C, Jackson PL, Roy MA. Impact of social anxiety on social cognition and functioning in patients with recent-onset schizophrenia spectrum disorders. Schizophr Res. (2013) 145:75–81. doi: 10.1016/j.schres.2013.01.012
41. Bora E, Berk M. Theory of mind in major depressive disorder: a meta-analysis. J Affect Disord. (2016) 191:49–55. doi: 10.1016/j.jad.2015.11.023
42. Bora E, Kose S. Meta-analysis of theory of mind in anorexia nervosa and bulimia nervosa: a specific Impairment of cognitive perspective taking in anorexia nervosa? Int J Eat Disord. (2016) 49:739–40. doi: 10.1002/eat.22572
43. Gkika S, Wittkowski A, Wells A. Social cognition and metacognition in social anxiety: a systematic review. Clin Psychol Psychother. (2018) 25:10–30. doi: 10.1002/cpp.2127
44. Alvi T, Kouros CD, Lee J, Fulford D, Tabak BA. Social anxiety is negatively associated with theory of mind and empathic accuracy. J Abnorm Psychol. (2020) 129:108–13. doi: 10.1037/abn0000493
45. Lima FS, Simioni S, Bruggimann L, Ruffieux C, Dudler J, Felley C, et al. Perceived behavioral changes in early multiple sclerosis. Behav Neurol. (2007) 18:81–90. doi: 10.1155/2007/674075
46. Ouellet J, Scherzer PB, Rouleau I, Métras P, Bertrand-Gauvin C, Djerroud N, et al. Assessment of social cognition in patients with multiple sclerosis. J Int Neuropsychol Soc. (2010) 16:287–96. doi: 10.1017/s1355617709991329
47. Mavrogiorgou P, Bethge M, Luksnat S, Nalato F, Juckel G, Brüne M. Social cognition and metacognition in obsessive–compulsive disorder: an explorative pilot study. Eur Archiv Psychiatry Clin Neurosci. (2016) 266:209–16. doi: 10.1007/s00406-016-0669-6
48. Henry A, Tourbah A, Chaunu MP, Bakchine S, Montreuil M. Social cognition abilities in patients with different multiple sclerosis subtypes. J Int Neuropsychol Soc. (2017) 23:653–64. doi: 10.1017/S1355617717000510
49. Misir E, Bora E, Akdede BB. Relationship between social-cognitive and social-perceptual aspects of theory of mind and neurocognitive deficits, insight level and schizotypal traits in obsessive-compulsive disorder. Compreh Psychiatry. (2018) 83:1–6. doi: 10.1016/j.comppsych.2018.02.008
50. Ignatova VG, Surchev JK, Stoyanova TG, Vassilev PM, Haralanov LH, Todorova LP. Social cognition impairments in patients with multiple sclerosis: comparison with grade of disability. Neurol India. (2020) 68:94–8. doi: 10.4103/0028-3886.279700
51. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
52. Lin X, Zhang X, Liu Q, Zhao P, Zhong J, Pan P, et al. Empathy and theory of mind in multiple sclerosis: a protocol for systematic review and meta-analysis. Medicine. (2020) 99:e21773. doi: 10.1097/MD.0000000000021773
53. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. (2010) 25:603–5. doi: 10.1007/s10654-010-9491-z
54. Masi A, Quintana DS, Glozier N, Lloyd AR, Hickie IB, Guastella AJ. Cytokine aberrations in autism spectrum disorder: a systematic review and meta-analysis. Mol Psychiatry. (2015) 20:440–6. doi: 10.1038/mp.2014.59
55. Hedges LV. Distribution theory for glass's estimator of effect size and related estimators. J Educ Stats. (1981) 6:107–28.
56. Cohen J. Statistical Power Analysis for the Behavioural Sciences. New York, NY: Academic Press (1988).
57. Velikonja T, Fett AK, Velthorst E. Patterns of nonsocial and social cognitive functioning in adults with autism spectrum disorder: a systematic review and meta-analysis. JAMA Psychiatry. (2019) 76:135–51. doi: 10.1001/jamapsychiatry.2018.3645
58. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.1186
59. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
60. Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. (2000) 56:455–63. doi: 10.1111/j.0006-341x.2000.00455.x
61. Spielberger CD. STAI Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologist Press (1970).
62. Beck AT, Steer RA. Beck Depression Inventory: Manual. Vol. 8. San Antonio TX: Harcourt Brace Jovanovich (1996). p. 77–100.
63. Banati M, Sandor J, Mike A, Illes E, Bors L, Feldmann A, et al. Social cognition and Theory of Mind in patients with relapsing-remitting multiple sclerosis. Eur J Neurol. (2010) 17:426–33. doi: 10.1111/j.1468-1331.2009.02836.x
64. Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Chichester: Cochrane book series (2009).
65. Chalah MA, Kauv P, Lefaucheur JP, Hodel J, Créange A, Ayache SS. Theory of mind in multiple sclerosis: a neuropsychological and MRI study. Neurosci Lett. (2017) 658:108–13. doi: 10.1016/j.neulet.2017.08.055
66. Ciampi E, Uribe-San-Martin R, Vásquez M, Ruiz-Tagle A, Labbe T, Cruz JP, et al. Relationship between social cognition and traditional cognitive impairment in progressive multiple sclerosis and possible implicated neuroanatomical regions. Multiple Scler Relat Disord. (2018) 20:122–8. doi: 10.1016/j.msard.2018.01.013
67. Genova HM, Lancaster K, Lengenfelder J, Bober CP, DeLuca J, Chiaravalloti ND. Relationship between social cognition and fatigue, depressive symptoms, and anxiety in multiple sclerosis. J Neuropsychol. (2020) 14:213–25. doi: 10.1111/jnp.12185
68. Krämer M, Brauner S, Herold M, Diehl RR, Dziobek I, Berlit P. theory of mind, perception of affective prosody and empathy in secondary progressive multiple sclerosis. Aktuelle Neurol. (2014) 41:208–16. doi: 10.1055/s-0034-1370029
69. Fabri TL, Datta R, O'Mahony J, Bar-Or A, Yeh EA, Arnold DL. Memory and identification of emotional expression in pediatric-onset multiple sclerosis. Multiple Scler J. (2018) 24:340–1. doi: 10.1177/1352458518798590
70. Henry A, Bakchine S, Maarouf A, Chaunu MP, Rumbach L, Magnin E, et al. Facial emotion recognition and faux pas interpretation in multiple sclerosis. Brain Impairment. (2015) 16:158–72. doi: 10.1017/BrImp.2015.33
71. Batista S, Alves C, D'Almeida OC, Afonso A, Félix-Morais R, Pereira J, et al. Disconnection as a mechanism for social cognition impairment in multiple sclerosis. Neurology. (2017) 89:38–45. doi: 10.1212/WNL.0000000000004060
72. Batista S, d'Almeida OC, Afonso A, Freitas S, Macário C, Sousa L, et al. Impairment of social cognition in multiple sclerosis: amygdala atrophy is the main predictor. Multiple Scler. (2017) 23:1358–66. doi: 10.1177/1352458516680750
73. Batista S, Freitas S, Afonso A, Macário C, Sousa L, Cunha L, et al. Theory of mind and executive functions are dissociated in multiple sclerosis. Arch Clin Neuropsychol. (2018) 33:541–51. doi: 10.1093/arclin/acx101
74. Bisecco A, Altieri M, Santangelo G, Di Nardo F, Docimo R, Caiazzo G, et al. Resting-state functional correlates of social cognition in multiple sclerosis: an explorative study. Front Behav Neurosci. (2020) 13:276. doi: 10.3389/fnbeh.2019.00276
75. Chanial C, Basaglia-Pappas S, Jacqueline S, Boulange A, Gourdon C, Donya S, et al. Assessment of implicit language and theory of mind in multiple sclerosis. Ann Phys Rehabil Med. (2020) 63:111–5. doi: 10.1016/j.rehab.2019.08.005
76. Charvet LE, Cleary RE, Vazquez K, Belman AL, Krupp LB. Social cognition in pediatric-onset multiple sclerosis (MS). Multiple Scler. (2014) 20:1478–84. doi: 10.1177/1352458514526942
77. Czekóová K, Shaw DJ, Saxunová K, Dufek M, Mareček R, Vaníček J, et al. Impaired self-other distinction and subcortical gray-matter alterations characterize socio-cognitive disturbances in multiple sclerosis. Front Neurol. (2019) 10:525. doi: 10.3389/fneur.2019.00525
78. Dulau C, Deloire M, Diaz H, Saubusse A, Charre-Morin J, Prouteau A, et al. Social cognition according to cognitive impairment in different clinical phenotypes of multiple sclerosis. J Neurol. (2017) 264:740–8. doi: 10.1007/s00415-017-8417-z
79. García M, Rueda DS, Rosenbaum K, Cassará FP, Sinay V, Torralva T, et al. The reduced version of the reading the mind in the eyes test. It's utility in evaluating complex emotion recognition in relapsing remitting multiple sclerosis. Neurology. (2018) 90.
80. Genova HM, Cagna CJ, Chiaravalloti ND, DeLuca J, Lengenfelder J. Dynamic assessment of social cognition in individuals with multiple sclerosis: a pilot study. J Int Neuropsychol Soc. (2016) 22:83–8. doi: 10.1017/S1355617715001137
81. Gleichgerrcht E, Tomashitis B, Sinay V. The relationship between alexithymia, empathy and moral judgment in patients with multiple sclerosis. Eur J Neurol. (2015) 22:1295–303. doi: 10.1111/ene.12745
82. Goitia B, Bruno D, Abrevaya S, Sedeño L, Ibáñez A, Manes F, et al. The relationship between executive functions and fluid intelligence in multiple sclerosis. PLoS ONE. (2020) 15:e0231868. doi: 10.1371/journal.pone.0231868
83. Golde S, Heine J, Pöttgen J, Mantwill M, Lau S, Wingenfeld K, et al. Distinct Functional connectivity signatures of impaired social cognition in multiple sclerosis. Front Neurol. (2020) 11:507. doi: 10.3389/fneur.2020.00507
84. Henry JD, Phillips LH, Beatty WW, McDonald S, Longley WA, Joscelyne A, et al. Evidence for deficits in facial affect recognition and theory of mind in multiple sclerosis. J Int Neuropsychol Soc. (2009) 15:277–85. doi: 10.1017/S1355617709090195
85. Isernia S, Baglio F, d'Arma A, Groppo E, Marchetti A, Massaro D. Social mind and long-lasting disease: focus on affective and cognitive theory of mind in multiple sclerosis. Front Psychol. (2019) 10:218. doi: 10.3389/fpsyg.2019.00218
86. Labbe TP, Zurita M, Montalba C, Ciampi EL, Cruz JP, Vasquez M, et al. Social cognition in multiple sclerosis is associated to changes in brain connectivity: a resting-state fMRI study. Multiple Scler Relat Disord. (2020) 45:102333. doi: 10.1016/j.msard.2020.102333
87. Lancaster K, Stone EM, Genova HM. Cognitive but not affective theory of mind deficits in progressive MS. J Int Neuropsychol Soc. (2019) 25:896–900. doi: 10.1017/s1355617719000584
88. Mike A, Strammer E, Aradi M, Orsi G, Perlaki G, Hajnal A, et al. Disconnection mechanism and regional cortical atrophy contribute to impaired processing of facial expressions and theory of mind in multiple sclerosis: a structural MRI study. PLoS ONE. (2013) 8:e82422 doi: 10.1371/journal.pone.0082422
89. Parada-Fernández P, Oliva-Macías M, Amayra I, López-Paz JF, Lázaro E, Martínez Ó, et al. Accuracy and reaction time in recognition of facial emotions in people with multiple sclerosis. Rev Neurol. (2015) 61:433–40. doi: 10.33588/rn.6110.2015225
90. Patil I, Young L, Sinay V, Gleichgerrcht E. Elevated moral condemnation of third-party violations in multiple sclerosis patients. Soc Neurosci. (2017) 12:308–29. doi: 10.1080/17470919.2016.1175380
91. Pöttgen J, Dziobek I, Reh S, Heesen C, Gold SM. Impaired social cognition in multiple sclerosis. J Neurol Neurosurg Psychiatry. (2013) 84:523–8. doi: 10.1136/jnnp-2012-304157
92. Raimo S, Trojano L, Pappacena S, Alaia R, Spitaleri D, Grossi D, et al. Neuropsychological correlates of theory of mind deficits in patients with multiple sclerosis. Neuropsychology. (2017) 31:811–21. doi: 10.1037/neu0000372
93. Roca M, Manes F, Gleichgerrcht E, Ibáñez A, González De Toledo ME, Marenco V, et al. Cognitive but not affective theory of mind deficits in mild relapsing-remitting multiple sclerosis. Cognit Behav Neurol. (2014) 27:25–30. doi: 10.1097/WNN.0000000000000017
94. Vanotti S, Rojas G, Allegri R, Caceres F. How behavioral and quality of life changes affect social cognition in multiple sclerosis patients. Neurology. (2012) 78:P02.042. doi: 10.1212/WNL.78.1
95. Yu CL, Chou TL. A dual route model of empathy: a neurobiological prospective. Front Psychol. (2018) 9:2212. doi: 10.3389/fpsyg.2018.02212
96. Demichelis OP, Coundouris SP, Grainger SA, Henry JD. Empathy and theory of mind in Alzheimer's disease: a meta-analysis. J Int Neuropsychol Soc. (2020) 26:963–77. doi: 10.1017/s1355617720000478
97. Coundouris SP, Adams AG, Henry JD. Empathy and theory of mind in Parkinson's disease: a meta-analysis. Neurosci Biobehav Rev. (2020) 109:92–102. doi: 10.1016/j.neubiorev.2019.12.030
98. Paul LK, Brown WS, Adolphs R, Tyszka JM, Richards LJ, Mukherjee P, et al. Agenesis of the corpus callosum: genetic, developmental and functional aspects of connectivity. Nat Rev Neurosci. (2007) 8:287–99. doi: 10.1038/nrn2107
99. Von Der Heide RJ, Skipper LM, Klobusicky E, Olson IR. Dissecting the uncinate fasciculus: disorders, controversies and a hypothesis. Brain. (2013) 136(Pt 6):1692–1707. doi: 10.1093/brain/awt094
100. Downey LE, Mahoney CJ, Buckley AH, Golden HL, Henley SM, Schmitz N, et al. White matter tract signatures of impaired social cognition in frontotemporal lobar degeneration. Neuroimage Clin. (2015) 8:640–51. doi: 10.1016/j.nicl.2015.06.005
101. Abu-Akel A, Shamay-Tsoory S. Neuroanatomical and neurochemical bases of theory of mind. Neuropsychologia. (2011) 49:2971–84. doi: 10.1016/j.neuropsychologia.2011.07.012
102. O'Brien AR, Chiaravalloti N, Goverover Y, Deluca J. Evidenced-based cognitive rehabilitation for persons with multiple sclerosis: a review of the literature. Arch Phys Med Rehabil. (2008) 89:761–9. doi: 10.1016/j.apmr.2007.10.019
103. Pagnini F, Bosma CM, Phillips D, Langer E. Symptom changes in multiple sclerosis following psychological interventions: a systematic review. BMC Neurol. (2014) 14:222. doi: 10.1186/s12883-014-0222-z
104. Sesel AL, Sharpe L, Naismith SL. Efficacy of psychosocial interventions for people with multiple sclerosis: a meta-analysis of specific treatment effects. Psychother Psychosom. (2018) 87:105–11. doi: 10.1159/000486806
105. Mitolo M, Venneri A, Wilkinson ID, Sharrack B. Cognitive rehabilitation in multiple sclerosis: a systematic review. J Neurol Sci. (2015) 354:1–9. doi: 10.1016/j.jns.2015.05.004
106. van den Akker LE, Beckerman H, Collette EH, Twisk JW, Bleijenberg G, Dekker J, et al. Cognitive behavioral therapy positively affects fatigue in patients with multiple sclerosis: results of a randomized controlled trial. Mult Scler. (2017) 23:1542–53. doi: 10.1177/1352458517709361
107. Chalah MA, Ayache SS. Cognitive behavioral therapies and multiple sclerosis fatigue: a review of literature. J Clin Neurosci. (2018) 52:1–4. doi: 10.1016/j.jocn.2018.03.024
108. Fink F, Rischkau E, Butt M, Klein J, Eling P, Hildebrandt H. Efficacy of an executive function intervention programme in MS: a placebo-controlled and pseudo-randomized trial. Mult Scler. (2010) 16:1148–51. doi: 10.1177/1352458510375440
109. Mattioli F, Stampatori C, Zanotti D, Parrinello G, Capra R. Efficacy and specificity of intensive cognitive rehabilitation of attention and executive functions in multiple sclerosis. J Neurol Sci. (2010) 288:101–5. doi: 10.1016/j.jns.2009.09.024
110. Mattioli F, Stampatori C, Scarpazza C, Parrinello G, Capra R. Persistence of the effects of attention and executive functions intensive rehabilitation in relapsing remitting multiple sclerosis. Mult Scler Relat Disord. (2012) 1:168–73. doi: 10.1016/j.msard.2012.06.004
111. Hanssen KT, Beiske AG, Landrø NI, Hofoss D, Hessen E. Cognitive rehabilitation in multiple sclerosis: a randomized controlled trial. Acta Neurol Scand. (2016) 133:30–40. doi: 10.1111/ane.12420
112. Lincoln NB, Bradshaw LE, Constantinescu CS, Day F, Drummond AE, Fitzsimmons D, et al. Cognitive rehabilitation for attention and memory in people with multiple sclerosis: a randomized controlled trial (CRAMMS). Clin Rehabil. (2020) 34:229–41. doi: 10.1177/0269215519890378
113. Kratz AL, Braley TJ, Foxen-Craft E, Scott E, Murphy JF III, Murphy SL. How do pain, fatigue, depressive, and cognitive symptoms relate to well-being and social and physical functioning in the daily lives of individuals with multiple sclerosis? Arch Phys Med Rehabil. (2017) 98:2160–6. doi: 10.1016/j.apmr.2017.07.004
114. Henry A, Tourbah A, Camus G, Deschamps R, Mailhan L, Castex C, et al. Anxiety and depression in patients with multiple sclerosis: the mediating effects of perceived social support. Mult Scler Relat Disord. (2019) 27:46–51. doi: 10.1016/j.msard.2018.09.039
Keywords: multiple sclerosis, empathy, theory of mind, meta-analysis, cognitive, affective
Citation: Lin X, Zhang X, Liu Q, Zhao P, Zhong J, Pan P, Wang G and Yi Z (2021) Empathy and Theory of Mind in Multiple Sclerosis: A Meta-Analysis. Front. Psychiatry 12:628110. doi: 10.3389/fpsyt.2021.628110
Received: 13 November 2020; Accepted: 18 March 2021;
Published: 09 April 2021.
Edited by:
Philipp Kanske, Technische Universität Dresden, GermanyReviewed by:
Katja Koelkebeck, LVR Hospital Essen, GermanyCopyright © 2021 Lin, Zhang, Liu, Zhao, Zhong, Pan, Wang and Yi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: ZhongQuan Yi, eWl6aG9uZ3F1YW5AMTYzLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.