
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CLINICAL TRIAL article
Front. Psychiatry, 26 February 2021
Sec. Psychological Therapies
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.624876
 Marcelo Trombka1,2,3,4,5,6*
Marcelo Trombka1,2,3,4,5,6* Marcelo Demarzo7
Marcelo Demarzo7 Daniel Campos8,9
Daniel Campos8,9 Sonia B. Antonio7
Sonia B. Antonio7 Karen Cicuto7
Karen Cicuto7 Ana L. Walcher1,2,3,4
Ana L. Walcher1,2,3,4 Javier García-Campayo9
Javier García-Campayo9 Zev Schuman-Olivier5,6
Zev Schuman-Olivier5,6 Neusa S. Rocha1,2,3,4
Neusa S. Rocha1,2,3,4Background: Police officers' high-stress levels and its deleterious consequences are raising awareness to an epidemic of mental health problems and quality of life (QoL) impairment. There is a growing evidence that mindfulness-based interventions are efficacious to promote mental health and well-being among high-stress occupations.
Methods: The POLICE study is a multicenter randomized controlled trial (RCT) with three assessment points (baseline, post-intervention, and 6-month follow-up) where police officers were randomized to mindfulness-based health promotion (MBHP) (n = 88) or a waiting list (n = 82). This article focuses on QoL, depression and anxiety symptoms, and religiosity outcomes. Mechanisms of change and MBHP feasibility were evaluated.
Results: Significant group × time interaction was found for QoL, depression and anxiety symptoms, and non-organizational religiosity. Between-group analysis showed that MBHP group exhibited greater improvements in QoL, and depression and anxiety symptoms at both post-intervention (QoL d = 0.69 to 1.01; depression d = 0.97; anxiety d = 0.73) and 6-month follow-up (QoL d = 0.41 to 0.74; depression d = 0.60; anxiety d = 0.51), in addition to increasing non-organizational religiosity at post-intervention (d = 0.31). Changes on self-compassion mediated the relationship between group and pre-to-post changes for all QoL domains and facets. Group effect on QoL overall health facet at post-intervention was moderated by mindfulness trait and spirituality changes.
Conclusion: MBHP is feasible and efficacious to improve QoL, and depression and anxiety symptoms among Brazilian officers. Results were maintained after 6 months. MBHP increased non-organizational religiosity, although the effect was not sustained 6 months later. To our knowledge, this is the first mindfulness-based intervention RCT to empirically demonstrate these effects among police officers. Self-compassion, mindfulness trait, and spirituality mechanisms of change are examined.
Clinical Trial Registration: www.ClinicalTrials.gov. identifier: NCT03114605.
Policing is a high-stress occupation (1, 2), ranking as one of the most psychologically dangerous professions worldwide (3, 4). Different from other vulnerable occupations, officers repeatedly face dangerous, unpredictable, and potentially traumatic situations (e.g., exposure to human misery and death, shooting, critical incidents, and life-changing errors with emotional cost). Dealing with verbal and physical aggression, having to use force to restrain, giving evidence in court, and high-speed driving are examples of operational stressors (4). Organizational stressors often include hierarchical and bureaucratic structures which can perpetuate discrimination, sexism, and racism; poor communication; long and irregular shifts; new recruit hazing and cultural assimilation; hostile public image; and inadequate resources (4–6). Exposure to acute and chronic stressors are associated with a myriad of negative consequence for officers' mental health, physical health, and quality of life (QoL).
When compared to the general population, officers exhibit higher rates of depression (7), anxiety (8), burnout (9), alcohol abuse (10), post-traumatic stress disorder (PTSD) (11), and suicide (12). Police perceived work stress predicts depression and anxiety symptoms (7, 13). For instance, the prevalence of depression among officers is nearly twice as high as the general population (14). Half of all completed suicides are related to depressive and other mood disorders (15). Anxiety disorders more than double the risk of suicide attempts, and a combination of depression and anxiety greatly increases the risk by 17 (16, 17). Recent data show that in the USA, more officers die from suicide than in the line of duty (18). Poor mental health can be deleterious to physical health. Indeed, officers have elevated risks for diabetes, obesity, cardiovascular disease, and sudden cardiac death (19–21). Brazilian Police mental health scenario is also alarming, with a high prevalence of stress, depression, anxiety, and PTSD (6, 22–24). Crime rate in Brazil is high and exposure to violence is associated with occupational stress, burnout, and suicide (23, 25–28). The 2019 Brazilian Public Annual Report evidenced the same pattern as the USA: more officers died from suicide than at work (29).
Work-related stress, accompanied by a culture where display of emotion is often viewed as a sign of weakness (30), pays a toll on multiple work and life dimensions. Officers experiencing high levels of stress and fatigue are less efficient and prone to absenteeism, uncontrolled anger toward suspects, impaired judgment and decision-making (31, 32); increased implicit racial bias (33), including the decision to shoot (34); and to use excessive force (35, 36). Disruptive family relationships and marital troubles are another facet of the pernicious consequences of stress (37, 38). QoL is a broad-ranging concept, affected in a complex way by the person's physical health, psychological state, level of independence, social relationships, and their relationships to salient features of their environment (39). Perceived stress levels are negatively associated with QoL and explain up to 34% of its variability (40). Two studies evidenced significant associations between Brazilian police stress and QoL deficits in the social, affective, professional, and health areas (6, 23). Extensive literature associate religiosity and its dimensions (i.e., organizational, non-organizational, intrinsic) with psychological health and QoL (41–43). It is negatively related to stress among officers and can be an effective coping tool for occupational stress (44, 45).
The last two decades have seen a dramatic increase in the scientific research and popular interest about mindfulness. Mindfulness can be defined as an innate meta-awareness capacity to attend to present-moment experience while avoiding entanglement in cognitive biases with an orientation of curiosity, openness, and acceptance (46). It can be enhanced by simple meditative attentional practices, as well as through structured training programs such as mindfulness-based interventions (MBIs). MBIs are group-based weekly classes composed of meditation practices, such as the body scan, mindful movement, and sitting and walking meditation; experiential inquiry-based learning process; and exercises to develop insight (47). MBIs implicitly teach self-compassion, which is composed of three interacting components: self-kindness (i.e., being kind and understanding toward oneself in instances of perceived inadequacy or suffering vs. self-judgment), a sense of common humanity (i.e., perceiving one's experiences as part of the larger human experience vs. isolation), and mindfulness itself (i.e., holding one's painful thoughts and feelings in balanced awareness vs. over identification with suffering or avoidance/disconnection) (48). Mindfulness training (MT) may regulate how the individual appraises stress and increase secondary appraisals of approach-oriented coping resources, thus reducing stress reactivity. A process of enhanced self-regulation is established by synergistic systems of attention/cognitive control, emotional regulation, and self-related processes (49, 50).
Meta-analyses indicate that MBIs decrease stress (51), depression and suicidal ideation (52, 53), anxiety and burnout (53, 54), and increases QoL (55) and spirituality (56). MBIs have been shown to be feasible and to lead to improved health outcomes in non-clinical populations at the workplace (57), including several high-stress occupations, such as the military (58–62), healthcare providers (63), firefighters (64), and inner-city teachers (65). Published in 2016, a single-arm pilot study pioneered the field of MT within law enforcement officers (LEOs), suggesting positive effects following mindfulness-based resilience training (MBRT)—an 8-week mindfulness-based stress reduction (MBSR) adaptation designed to enhance resilience for LEOs in the context of stressors inherent to policing—on outcomes such as perceived stress, burnout, emotional intelligence, and mental and physical health (66). Since then, three other trials have replicated and extended those benefits (67–69).
With the development of positive psychiatry, specialty scope incorporates—along with the treatment of mental illness—psychosocial interventions targeting those at high risk of developing mental or physical illness, and goals encompass increased well-being and positive psychosocial characteristics (e.g., resilience, spirituality, religiosity) (70). Two reviews concluded that randomized controlled trials (RCTs) are needed to clarify the role of psychosocial interventions for stress management and mental health/well-being promotion among police officers (71, 72). In light of these findings, the burden of high-stress levels and mental health problems epidemic in the police, plus aforementioned MBIs' salutary effects, further empirical evaluation of MBIs' impact on that vulnerable population is needed. The POLICE (imPact Of a mindfuLness-based Intervention on burnout and quality of life in poliCE officers) study is a multicenter RCT evaluating the efficacy of mindfulness-based health promotion (MBHP) to promote police officers' QoL and mental health at post-intervention and after 6 months. As designated at the research protocol manuscript (73), our hypothesis is that officers allocated to MBHP, compared with a waiting list (WL), will show enhancement on QoL and reduction on burnout symptoms (primary outcomes), besides improvement on several mental health measures (secondary outcomes). We also investigated primary outcomes of potential mechanisms of change through mediation and moderation analysis. Mediators clarify how/why intervention works, while moderators identify whom or under what conditions interventions have effects (74). The POLICE study design overcomes previous studies' limitations such as absence of control group/follow-up or small sample sizes.
A detailed description of POLICE study Materials and Methods is available at the research protocol manuscript (73).
The POLICE study was a multicentric, parallel, two-armed RCT with three assessment points: baseline, post-intervention, and 6-month follow-up (73). Participants were randomized to MBHP—an 8-week MBI—or a WL control group. The clinical trial protocol was prepared in accordance with SPIRIT 2013 statement (75) and was approved by the centers' ethical committees. Figure 1 shows the CONSORT flow diagram through the study.
Police officers working at two major Brazilian cities were recruited from 2016 to 2018.
(1) Civil Police. The study center in Porto Alegre was located at the Police Hall of the State of Rio Grande do Sul. Civil Police main duties are to oversee public order and security, adopt measures necessary to avoid danger or injury to persons and public or private property, and ensure the administration of criminal offenses, including execution of arrest warrants and requisitions requested by the judicial branch.
(2) Civil Guard. The study center in São Paulo was located at the headquarters of Unifesp Santo Amaro. Civil Guard fundamental duties include the protection of goods, services, and municipal facilities, as well as patrolling areas and preventive policing.
Participants meeting the following inclusion criteria were enrolled: (1) active police officers; (2) 21–65 years old; (3) availability to attend eight sessions; (4) willingness to participate voluntarily. Exclusion criteria included (1) previous involvement in any MBI or regular mindfulness practice over the last 3 months, or one of the following diagnosis, assessed by the Mini International Neuropsychiatric Interview (MINI): (2) major depressive episode (current); (3) manic or hypomanic episode (current); (4) psychotic syndrome (current or past); (5) substance use disorder (past 12 months, except tobacco); (6) risk of suicide.
The POLICE study was advertised within the two Police Institutions using the internet, social media, and posters. Officers who showed interest contacted the research team by phone or email and were initially screened. Potential participants had a face-to-face interview scheduled where they were provided detailed information about the study and inclusion/exclusion criteria were assessed. Eligible volunteers filled the informed consent form and were randomly assigned to MBHP or WL by an independent researcher who were unaware of the characteristics of the study and was not involved in the trial or had access to study data. Randomization was implemented using sealed envelopes. Officers allocated to the WL group did not receive any intervention for 6 months. After the 6-month assessment, MBHP was offered for all participants randomized to the WL group. Officers received authorization from the Police Institutions to attend the program which happened during working hours. Due to the nature of the intervention, the POLICE study was single-blind—the outcomes assessment was blind, albeit participants were aware of their group assignment. While we initially planned to randomize 160 participants (allowing for up to 20% loss to follow-up) to detect a moderate effect size (Cohen's d = 0.05) with a power of 0.80 and an alpha of 0.05, from the 194 participants screened, 170 officers met enrollment criteria and were randomized. We defined participants as external police officers if during the study they were exerting operational activities and as internal police officers if their contact with civilians was done inside police agencies or they were assigned to administrative roles.
MBHP (76) is an 8-week MBI based on the MBSR model (77). It was adapted to suit the context and needs of primary healthcare and national and local health systems, developing a framework that supports the learning process to individuals from distinctive cultural and educational backgrounds. MBHP was designed to address human universal vulnerabilities, not focusing on any specific health condition. It has been applied since 2009 by Mente Aberta—Brazilian Center for Mindfulness and Health Promotion, and by the University of Zaragoza in Spain. There is a strong emphasis on informal mindfulness practices, such as walking, eating, exercising, talking, and doing housework. Concepts of radical acceptance (78), values clarification (79), and positive psychology (80) are heavily emphasized. Session six is conducted in silence for the purpose of deepening the practice. Besides MBSR core practices, psychoeducational activities and practices from mindfulness-based cognitive therapy (MBCT) and Breathworks curriculum are introduced (i.e., 3-min breathing space; “primary and secondary suffering;” “hello-thanks-goodbye thought”) (81, 82). Compassion training techniques are also included (equanimity in the condition of human suffering, receiving affection and showing affection to oneself). This rigorous training follows the British and Brazilian guidelines for good practices of mindfulness (83, 84). MBHP groups started with an average of 21 officers. One interventionist led the MBHP groups in Porto Alegre and one led the MBHP groups in São Paulo. MBHP core curriculum content is described in Table 1.
The POLICE study had three assessment points, which occurred during the 2 weeks before the intervention, the 2 weeks following the intervention, and 6 months after the intervention. Participants allocated to the WL filled the surveys on the same timeline. Surveys were answered on the Survey Monkey Software (http://surveymonkey.com). When computers or tablets were not available, participants answered using pen and paper and the data were transcribed via single entry to the password-protected software. Primary and secondary outcomes were previously reported (73). This article will specifically report the findings related to QoL, anxiety and depression symptoms, and religiosity. We will also address MBHP feasibility and the possible role of mediators (i.e., mindfulness trait, decentering, self-compassion, and spirituality) and moderators (i.e., sex, age, number of sessions, mindfulness trait, decentering, self-compassion, and spirituality) to post-intervention QoL improvement as formerly proposed (73). Because the Connor-Davidson-25 Scale of Resilience (CD-RISC-25) was not applied to all participants, we excluded resilience from our mediation and moderation analysis.
Twenty-six-item instrument that produces scores for four domains related to QoL: physical health, psychological, social relationships, and environment, besides overall QoL and general health facets. WHOQOL-BREF Portuguese version exhibits strong psychometric properties (85). Cronbach's α in the present sample was physical health, α = 0.79; psychological, α = 0.84; social relationships, α = 0.79; and environment, α = 0.76.
Fourteen-item scale that quantifies the severity of anxiety (HADS-A) and depressive symptoms (HADS-D) in community and hospital settings. HADS Portuguese version shows good psychometric properties (86). Cronbach's α in the present sample was 0.81 for HADS-A and 0.78 for HADS-D.
Five-item instrument capturing three dimensions of religiosity: organizational religiosity (OR), non-organizational religiosity (NOR), and intrinsic religiosity (IR). The NOR subscale measures private religious activities (e.g., prayer, meditation, Scripture study), while the OR subscale involves public religious activities. IR subscale assesses the degree of personal religious commitment or motivation, pursuing religion as an ultimate end in itself (43). DUREL Portuguese version presents high internal consistency and discriminant validity (87). Cronbach's α in the present study was 0.88.
Fifteen-item scale designed to assess a core characteristic of dispositional mindfulness. MAAS Portuguese version has adequate reliability and validity (88). Cronbach's α in the present study was 0.96.
Twenty-six-item instrument measuring six components of self-compassion. Portuguese SCS version exhibits good psychometric properties (89). Cronbach's α in the present study was 0.81.
Thirty-four-item scale evaluating QoL domains of spirituality, religiosity, and personal beliefs. WHOQOL-SRPB-BREF Portuguese version shows strong psychometric properties (90). Cronbach's α in the present study was 0.88.
Group differences at baseline on demographic data and outcome variables were evaluated using χ2-tests for categorical variables and Student's t-test for continuous data. Intention-to-treat (ITT) mixed-models analyses without any ad hoc imputation were used to account for missing data with the restricted maximum likelihood estimation (REML) (91), rather than repeated measures ANOVA described in the original protocol based on the authors' recommendation and due to the amount of missing data. The mixed-model approach is appropriate for RCTs with multiple time points and pre-only to post-only designs, it does not assume that the last measurement is stable, it does not involve any substitution of missing values with supposed or estimated values, it is conducted using all available observations (92, 93), and it is robust to violations of distributional assumptions (94). A linear mixed model for each primary and secondary outcome measure was implemented with time (pre, post, and follow-up) as within-group factor and group (WL and MBHP) as between-group factor using the MIXED procedure with a random intercept for subject. An identity covariance structure was specified to model the covariance structure of the intercept. Wald statistic (or Z-test) was conducted to test the residual error variance estimation and the null hypothesis of homogeneity of residuals (95, 96). Significant effects were followed up with pairwise contrasts adjusted by Bonferroni correction. These statistical tests have shown their robustness regardless of violations of the required assumptions when group sizes are equal (97). Results are reported in line with conventional ANOVA, as mixed-model repeated measures, according to studies that used this approach for repeated measures designs (98, 99). Effect sizes (Cohen's d) and the 95% CI were calculated for within- and between-group comparisons, based on Botella and Sanchez-Meca, and Cumming and Calin-Jageman recommendations (100, 101). Mediation hypothesis was tested by bootstrap regression analysis using the Preacher and Hayes approach (PROCESS) (Model 4) (102). The pre-to-post changes in mindfulness (MAAS), decentering (EQ), self-compassion (SCS), and spirituality (WHOQOL-SRPB-BREF) were included as proposed mediators between group and QoL outcome. Separate moderation analyses were conducted for WHOQOL-BREF using the Bootstrapping PROCESS (model 1). Independent moderation models were tested for each proposed mediator: sex, age, number of sessions, and pre-to-post changes on mindfulness (MAAS), decentering (EQ), self-compassion (SCS), and spirituality (WHOQOL-SRPB-BREF). Significant moderation was followed up by significant interaction between the independent variable (X) (group: WL vs. MBHP) and the dependent variable (Y) (pre-to-post changes in WHOQOL-BREF). Statistical analyses were performed using the IBM SPSS version 23 for Windows.
Descriptive statistics and sociodemographic characteristics of participants are shown in Table 2. No statistically significant differences between groups were found on any sociodemographic data, or on primary and secondary outcomes at baseline.
We randomized 87.6% (n = 170 out of 194) of officers assessed for eligibility. Due to reported lack of time, four individuals did not start the intervention. Participants who were randomized to the MBHP arm and started the intervention (n = 84) attended a mean of 6.44 (SD 2.14) of eight weekly sessions, 82.1% (n = 69) attended at least four sessions, and 69% (n = 58) at least six sessions. Eight-week assessment was completed by 75.3% (n = 128) and 6-month follow-up was answered by 71.2% (n = 121) of the enrolled sample.
Results for the WHOQOL-BREF showed a significant group × time interaction effect in all QoL domains—physical health [F(2,252.59) = 13.83; p < 0.001], psychological [F(2,245.89) = 20.36; p < 0.001], social relationships [F(2,248.25) = 9.02; p < 0.001], and environment [F(2,250.096) = 15.20; p < 0.001], the overall QoL facet [F(2,251.98) = 7.51; p < 0.01), and general health facet [F(2,254.216) = 5.10; p < 0.05]. Within-group comparisons revealed a significant pre-to-post and pre-to 6-month follow-up changes in MBHP group for physical health [F(2,251.67) = 18.65; p < 0.001], psychological [F(2,244.84) = 19.12; p < 0.001], social relationship [F(2,247.02) = 12.72; p < 0.001], environment [F(2,248.77) = 18.67; p < 0.001], overall QoL [F(2,249.20) = 9.13; p < 0.001], and general health [F(2,252.38) = 15.16; p < 0.001]. No significant changes were found in WL group except for pre-to-post reductions on the psychological domain (Table 3).
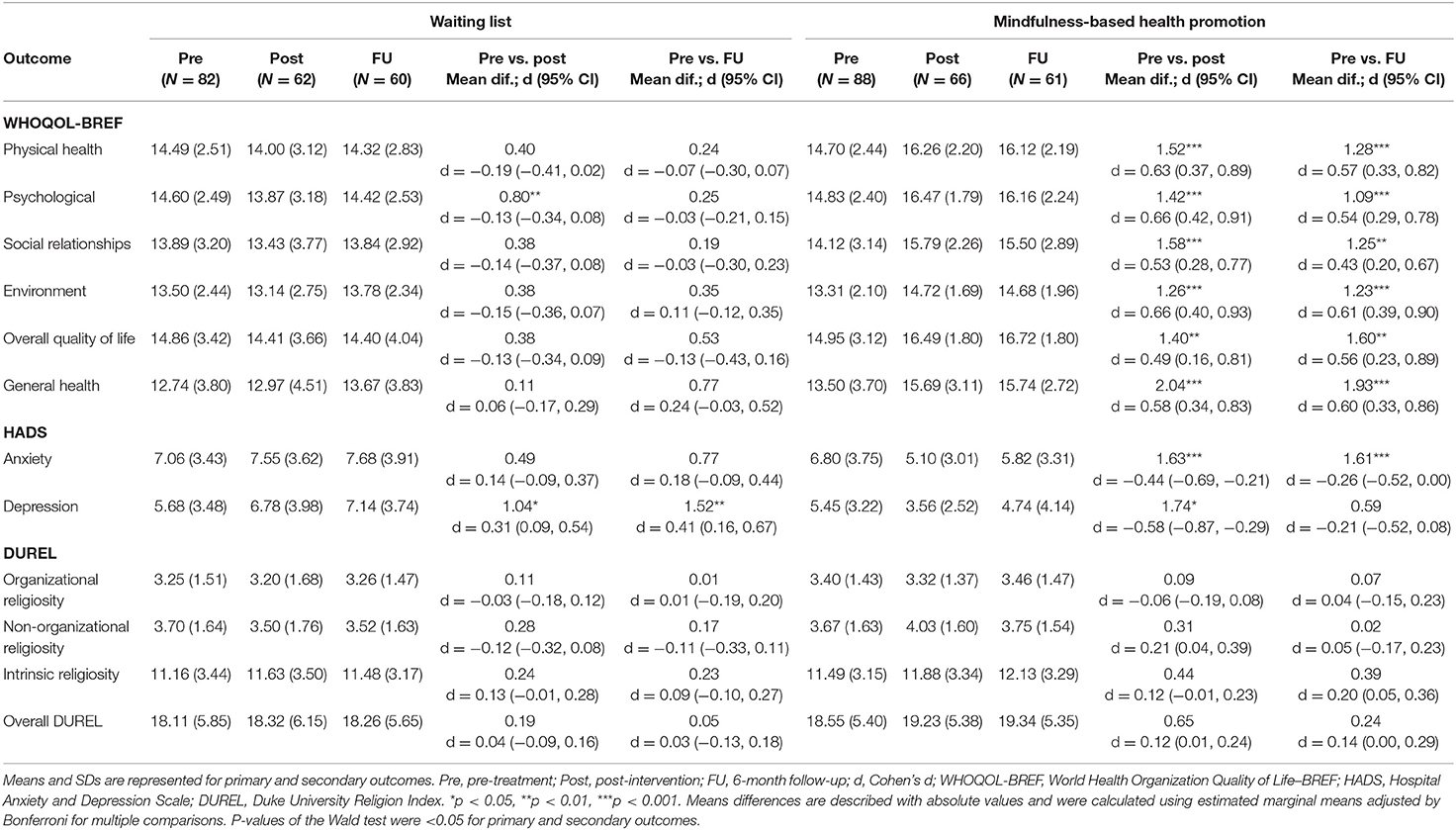
Table 3. Means, SDs, and within-group effect sizes for primary and secondary outcomes at pre-, post-intervention, and 6-month follow-up.
Between-group comparisons showed significant differences between groups, indicating higher scores in the MBHP group at post and 6-month follow-up compared with the WL control group across all domains and facets (Table 4).
Additional mixed-model analyses showed that the type of work (i.e., internal vs. external) was not a significant covariate for WHOQOL-BREF domains and facets (F-values from 0.019 to 1.563; all ps > 0.05).
A significant group × time interaction effect was found for both HADS subscales, Depression [F(2,247.44) = 12.52; p < 0.001] and Anxiety [F(2,167.70) = 12.76; p < 0.001], and statistically significant differences between groups were found at post and 6-month follow-up, showing lower scores in the MBHP group compared with the WL group for both depression and anxiety subscales (Table 4). At pre-intervention, 32 (18.9%) and 52 (30.8%) participants scored above HADS-D and HADS-A cut-off (≥8), whereas at post-intervention, 20 (16.2%) and 27 (22.3%) officers scored above the cut-off, respectively. When considering the MBHP group, 16 (18.2%) and 29 (32.9%) valid responses were above HADS-D and HADS-A cut-off scores at pre-intervention, and 3 (4.7%) and 8 (12.7%) at post-intervention, respectively. Type of work was not a significant covariate for depression [F(1,163.46) = 0.13; p > 0.05] and anxiety [F(1,162.30) = 0.05; p > 0.05] subscales.
For DUREL, results showed only a significant interaction effect on non-organizational religiosity subscale [F(2,241.62) = 3.51; p < 0.05]. Specifically, between-group comparison revealed statistically significant differences at post where the MBHP reported higher scores compared with the WL group (Table 4). Type of work (i.e., internal vs. external) was not a significant covariate for DUREL measure (F-values from 0.023 to 0.867; all ps > 0.05).
Mediation results showed a significant indirect effect of MBHP on the change of QoL outcome through the change of self-compassion scores (SCSs) from pre-to-post intervention (Figure 2). Specifically, the total score of the SCS remained as the only significant mediator for pre-to-post changes on physical health [b = 0.94 (0.33), Ba CI 95% [0.34, 1.70]; R2 = 0.25], psychological [b = 1.33 (0.32), Ba CI 95% [0.78, 2.03]; R2 = 0.47], social relationships [b = 1.31 (0.37), Ba CI 95% [0.67, 2.16]; R2 = 0.26], environment [b = 0.75 (0.26), Ba CI 95% [0.29, 1.32]; R2 = 0.26], overall QoL [b = 1.27 (0.40), Ba CI95% [0.54, 2.18]; R2 = 0.22], and general health [b = 1.15 (0.38), Ba CI 95% [0.45, 1.89]; R2 = 0.18].
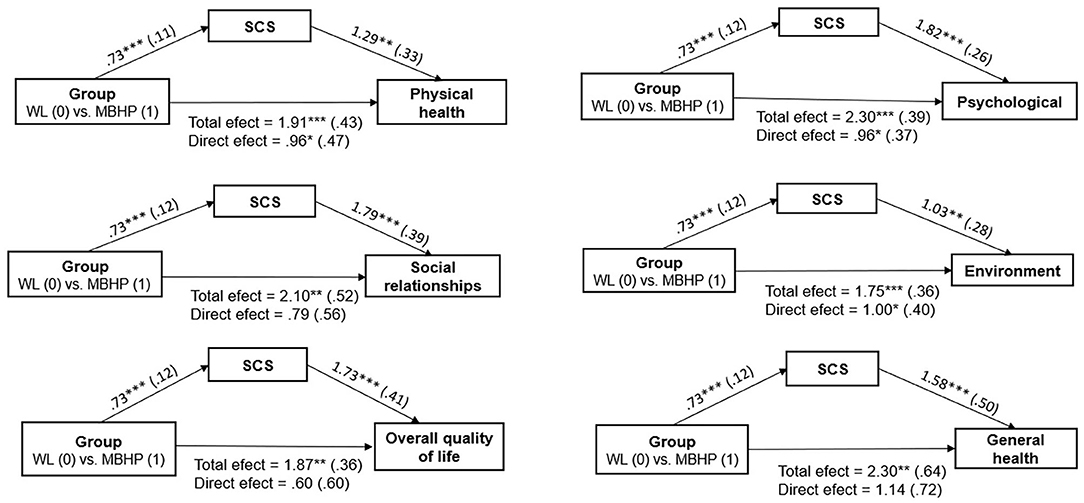
Figure 2. Mediation analyses for pre-to-post changes on quality of life (WHOQOL-BREF). SCS, Self-Compassion Scale. All coefficients represent unstandardized beta coefficients (standard errors in parentheses). Mediators and dependent variables are pre-to-post changes. *p < 0.05; **p < 0.01; ***p < 0.001.
Moderation was demonstrated by a significant interaction effect for general health facet, indicating that the relationship between the group and the pre-to-post change on the general health score was independently moderated by the pre-to-post change in MAAS [b = 1.28 (0.61), 95% CI [0.67, 2.49], t = 2.09, p < 0.05] and spirituality scores (WHOQOL-SRPB-BREF) [b = 0.098 (0.04), 95% CI [0.012, 0.18], t = 2.25, p < 0.05]. Specifically, increases on MAAS [b = 3.64 (1.02), 95% CI [1.63, 5.66], t = 3.59, p < 0.01] and spirituality (WHOQOL-SRPB-BREF) [b = 0.3.26 (0.86), 95% CI [1.55, 4.96], t = 3.78, p < 0.01] at post significantly moderated the group effect for general health. Sex, age, number of sessions, and changes in self-compassion and decentering scores were not yielded as significant moderators.
To the extent of our knowledge, we demonstrated the first empirical evidence grounded on a RCT that among police officers, an 8-week MBI (1) enhances all QoL domains and facets, (2) reduces depression symptoms, (3) decreases anxiety symptoms, (4) maintains QoL and mental health benefits after 6 months, (5) increases non-organizational religiosity, (6) has self-compassion as an important mechanism of action which mediates the improvement in all QoL domains and facets, and (7) is feasible in the Brazilian police environment.
Participants randomized to receive MBHP demonstrated greater levels of self-reported QoL at post-intervention than the WL group across its multiple domains and facets with medium to large effect sizes. Notably, at 6-month follow-up, the difference between groups across all QoL domains and facets remained significant indicating medium effect sizes. As expected, the psychological domain was the one that showed the largest effect size magnitude between groups both at post-intervention and at 6-month follow-up. These findings are consistent with Grupe et al.'s (68) single-arm study with 30 LEOs who exhibited increased psychological well-being after 8 weeks of MT and with Christopher et al.'s (66) pioneering single-arm pilot (n = 43) that reported increased LEO global mental health following MBRT. Noteworthy, a study by the UK College of Policing suggests that online mindfulness resources improve officers' well-being (103). Our results are in accordance with the literature that indicates MT's positive impact in QoL and well-being across different populations (55, 81, 104), including military and war veterans (58, 62, 105, 106).
MBHP presented efficacy to decrease depression symptoms at post-intervention and at 6-month follow-up, displaying large and medium effect sizes, respectively. These results are in line with Grupe et al. (68) pre–post pilot findings that exhibited a trend level decrease on depression symptoms with medium effect size after MT. Individuals allocated to receive MBHP also showed reduced levels of anxiety when compared with the control group both at post-intervention and at 6-month follow-up with medium effect sizes. While Christopher et al.'s (67) rigorous RCT that enrolled 61 LEOs did not find a significant reduction on anxiety symptoms, the authors stated that the small sample size and type II error could explain the findings given that the trial main aim was to explore MBRT feasibility and acceptability. Our results resonate with the aforementioned Grupe et al. pilot (68) that showed a salient reduction in anxiety symptoms after MT which persisted after 5 months. Furthermore, a growing body of evidence denotes MT's declining effects on depression symptoms among military personnel (107–110).
Whereas, the scientific literature is still not clear about how long MBI effects last, its psychological benefits tend to decrease over time (111, 112). Previous studies with MBIs and police personnel mental health follow-up have mixed results (67, 68). Persistent salutary effects of MHBP after 6 months should be highlighted; however, the study design does not illuminate its longstanding impact as prolonged follow-up was not performed. The WL within-group significant reductions in QoL psychological domain after 8 weeks and the increment in depression symptoms after 8 weeks and at 6-month follow-up (Table 3) could be explained as a consequence of dealing with new stressors intrinsic to the police activity without mindfulness skills or due to the nocebo effect and frustration, disappointment, and anger about not being offered MBHP immediately (113).
Police officers' QoL and mental health impairment represented in the baseline assessment lower scores when compared with populational national and international samples might have contributed to the intervention impact (85, 114–116). For instance, the poor mental health of our non-clinical sample is expressed by the average score of 7.06 on HADS-Anxiety (Table 3), close to the ≥8 cut-off score that presents sensitivity and specificity for anxiety disorders of ~0.8 (117). Exposure to extensive criminality, low wages, long and irregular shifts, inadequate training, lack of equipment, corruption, hostile public image, bureaucracy, and rigid hierarchy, in addition to hazing, discrimination, sexism, and racism within departments, may represent Brazilian police work-related stressors that possibly explain these findings (6, 23, 118, 119). Inasmuch as organizational conditions affect the Police Institution as a whole, it explains why the covariate analysis showed that internal and external police officers equivalently benefit from the intervention. Brazilian police scientific literature de facto demonstrates that stress levels are similar between officers exerting operational or administrative roles (120, 121), in line with international data pointing that organizational stressors may be more challenging than operational experiences (122).
The significant interaction effect and difference between groups on non-organizational (private) religiosity at post-intervention can be attributed to the possibility that many participants considered mindfulness meditation a private religious activity and/or MT led participants to increase private religious activities such as other types of meditation, prayer, etc. MBHP, such as MBSR, is a secular behavioral medicine intervention that teaches skills addressed to reduce universal human suffering where spiritual themes are not explicitly explored. That being said, MBIs can enhance transcendence and awareness of interconnectedness in which oneself is not seen as separate from everyday activities, other people, or the world (123); thus, studies consistently have been suggesting that it might lead to increments in spirituality/religiosity (56, 124–126). MBHP components of values clarification and compassion/loving-kindness practices for oneself and others potentially contributed to this finding. It is also important to mention that Brazil is a highly religious country (predominantly catholic) where 90% of the population identify with a spiritual or religious group (127), and in our sample, that proportion was ~80%.
The hypothesis that self-compassion could mediate QoL improvement was confirmed for all QoL domain and facets. Self-compassion has empirically shown to mediate MBI's effects on mental health and well-being (128–133). It is associated with a wide variety of positive outcomes related to psychological well-being and QoL (e.g., life satisfaction, positive affect, social connectedness, flourishing) (48, 134–137) and inversely associated with psychopathology (i.e., depression, anxiety, stress, suppression of unwanted thoughts, self-criticism, shame, anger) (137–141). Emotional regulation deficits and experiential avoidance are linked to depression, anxiety, and a lower QoL (142, 143). Denial, suppression, and avoidance of negative emotions are emotional regulation strategies commonly used by officers and those who are able to identify their feelings and be present to moment-to-moment experience show better mental health (144–146). The police toughness culture combined with exposure to uncontrollable situations, violence, and potentially traumatic situations results in high levels of shame, guilt, isolation, self-critical thinking, anger, and trauma-related disorders (2, 11, 146–148); therefore, self-compassion emerges as a crucial skill to be learned and cultivated. First-generation MBIs (i.e., MBSR, MBCT) did not explicitly teach self-compassion skills, but they are interwoven into the mindfulness instructions (e.g., “whenever you notice that the mind has wandered off, bring it back with gentleness and kindness”) (149, 150). In addition to implicit teaching, MBHP curriculum (73, 76) includes didactive teaching on compassion (e.g., fears of compassion), formal practices of compassion/loving kindness for oneself and informal practices (i.e., attention for self-compassion in routine activity), providing explicit opportunities for inner compassion cultivation.
Mindfulness trait and spirituality group effect moderation for WHOQOL-BREF general health facet pre–post changes are consistent with the literature that associates both characteristics with self-regulated behavior (151–153) and better health (154–157) in a variety of settings, including policing (69, 146, 158). Alsubaie et al.'s systematic review of MBCT and MBSR (159) concluded that global change in mindfulness are linked to better health outcomes. Historically, it should be remembered that MBSR—the first MBI—was developed in 1979 for people with chronic health conditions with the intention to create a vehicle for the effective training of medical patients in relatively intensive mindfulness meditation and its immediate applications to stress, pain, and illness (77). The fact that the number of sessions attended did not moderate the effect on QoL is aligned with Carmody and Baer's review (160) demonstrating no significant correlation between number of in-class MBSR hours and mean effect size. Moreover, our research group had previously suggested that an abbreviated MBI (four sessions) may have a similar efficacy to a standard MBI (eight sessions) in a non-clinical population (161).
The findings indicate that MBHP is feasible among Brazilian police officers. Randomization process was successful considering that baseline characteristics were similar in both groups. Initial dropout rate was low, and most of the participants accepted the randomization and completed the assessments. MBI's “completion” has been defined as attending four or more sessions (112). In view of these criteria, our completion rate was high and comparable with previous MBI studies (162), including within the police (67, 68).
The empirical results reported herein should be considered in the light of some limitations. Our sample was composed predominantly of female officers (Table 2) working at two of the most violent cities in the world (119). We used a waitlist control design rather than an active control intervention. While there are ethical advantages to a waitlist design because it allows for the provision of care to research participants who are seeking help while permitting a non-intervention evaluation, such design may overestimate intervention effects (163). Finally, single data entry may be associated with errors within the registry and a MIXED procedure with a random intercept for subject was conducted but test for random slope was not considered. The POLICE study has several strengths including the relevance and potential societal impact of applying MBIs within the police environment and its design—a multicenter RCT with follow-up assessment. RCTs are the “gold standard” in evidence-based medicine and the only type of study able to establish causation. Other key strengths are the sample size that allowed us to detect differences between groups and the focus on mental health/quality of life promotion and prevention of psychological suffering. Given mental illness' emotional, physical, economic, and social cost, a balanced approach between early intervention strategies and treatment is needed, consonant with preventive medicine and positive psychiatry (70, 164).
The POLICE study makes an important contribution to the emerging field of MT for police mental health and QoL. Although on its infancy, results from the first trials are promising. Qualitative studies are needed to understand officers' attitudes, feelings, and behaviors toward MT in greater depth (e.g., language attunement; potential obstacles and resistances related to police norms and customs; impact on family life). Occupational health literature suggests that physical exercise, MBIs, cognitive-behavioral therapy, and change in organizational practices promote mental health and well-being with no particular superiority, although more rigorous evaluations are needed (165). Future police RCTs should use active control interventions. Long-term follow-up, cost-effectiveness data, cross-cultural research, and replication on male samples will play a pivotal role for the field expansion. Complementary neurobiological, cognitive, behavioral, and psychometric measures addressing mechanisms (e.g., attentional/cognitive control, emotional regulation, interoceptive awareness, rumination) and a wide scope of outcomes, encompassing health and well-being; workplace (e.g., interpersonal relationships, absenteeism, safety, leadership, return on investment); societal (e.g., mental capital, ethics, impact on civilians); and effective policing (e.g., impulse control, working memory, task performance) perspectives should be on the research agenda. Importantly, if mindfulness and loving-kindness meditation could reduce implicit racial bias (166, 167), its impact in decreasing officers' stereotype-biased judgments and behaviors would warrant further investigation. “Stepped-care” and “low intensity–high volume” approaches (168) can increase accessibility and facilitate the nurturing of “Mindful Police Departments.” Evidence-based programs designed for cultivation and embodiment of self-compassion skills such as mindful self-compassion (169) and compassion cultivation training (170) or the interweaving of self-compassion practices in MT are auspicious. Rigorous research will inform and guide procedures, public policy decision-making, and systematic real-world implementation of MT for Police Institutions around the globe, nourishing the conditions for officers' physical, emotional, and mental fitness, and contributing to the judicious and mindful use of police power and authority, which could benefit society as a whole.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The study was approved by HCPA and UNIFESP Research Ethics Committees under number 60406416.9.1001.5327. The patients/participants provided their written informed consent to participate in this study.
MT, MD, and NR were responsible for manuscript writing, co-conceptualized, designed the study, and obtained funding. DC were responsible for statistical analysis and manuscript writing. MD, SA, and KC coordinated the study at São Paulo center. SA was particularly involved in the implementation and conduction of the project at this site. MT and NR coordinated the study implementation and conduction at Porto Alegre center. KC and AW were responsible for data curation. JG-C and ZS-O commented and critically reviewed the manuscript for important intellectual content. All authors read and approved the final manuscript.
This work was supported by CAPES Brasil - Coordenação de Aperfeiçoamento de Pessoal de Nível Superior under Grant 88882.346691 – Finance Code 001; by Hospital de Clínicas de Porto Alegre Research Incentive Fund and by Mente Aberta - Brazilian Center for Mindfulness and Health Promotion.
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the funders.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Anderson GS, Litzenberger R, Plecas D. Physical evidence of police officer stress. Policing. (2002) 25:399–420. doi: 10.1108/13639510210429437
2. Violanti JM, Charles LE, Virginia W, Mccanlies E, Hartley TA, Baughman P. Police stressors and health: a state-of-the-art review. Policing. (2017) 40:642–56. doi: 10.1108/PIJPSM-06-2016-0097
3. Axel BM, Valle J. South Florida's approach to police stress management. Police Stress. (1979) 1:13–4.
4. Collins PA, Gibbs ACC. Stress in police officers: a study of the origins, prevalence and severity of stress-related symptoms within a county police force. Occup Med. (2003) 53:256–64. doi: 10.1093/occmed/kqg061
5. Kop N, Euwema M. Burnout, job stress and violent behaviour among Dutch police officers. Work Stress. (2010) 13:37–41. doi: 10.1080/02678379950019789
6. Lipp M, Costa KR, Nunes V. Estresse, qualidade de vida e estressores ocupacionais de policiais [Police stress, quality of life and occupational stressors]. Psicol Org Trabalho. (2017) 17:46–53. doi: 10.17652/rpot/2017.1.12490
7. Wang Z, Inslicht SS, Metzler TJ, Henn-Haase C, McCaslin SE, Tong H, et al. A prospective study of predictors of depression symptoms in police. Psychiatry Res. (2010) 175:211–6. doi: 10.1016/j.psychres.2008.11.010
8. Violanti J, Mnatskanova A, Michael A, Tara H, Desta F, Penelope B, et al. Associations of stress, anxiety, and resiliency in police work. Occup Environ Med. (2014) 71(Suppl. 1):A3. doi: 10.1136/oemed-2014-102362.8
9. McCarty WP, Skogan WG. Job-related burnout among civilian and sworn police personnel. Police Q. (2013) 16:66–84. doi: 10.1177/1098611112457357
10. Gershon RRM, Lin S, Li X. Work stress in aging police officers. J Occup Environ Med. (2002) 44:160–7. doi: 10.1097/00043764-200202000-00011
11. Hartley TA, Violanti JM, Sarkisian K, Andrew ME, Burchfiel CM. PTSD symptoms among police officers: associations with frequency, recency, and types of traumatic events. Int J Emerg Mental Health. (2013) 15:241–53.
12. O'Hara AF, Violanti JM, Levenson RL, Clark RG. National police suicide estimates: web surveillance study III. Int J Emerg Mental Health. (2013) 15:31–8.
13. Berg AM, Hem E, Lau B, Ekeberg Ø. An exploration of job stress and health in the Norwegian police service: a cross sectional study. J Occup Med Toxicol. (2006) 1:1–9. doi: 10.1186/1745-6673-1-26
14. Hartley TA, Burchfiel CM, Fekedulegn D, Andrew ME, Violanti JM. Health disparities in police officers: comparisons to the U.S. general population. Int J Emerg Mental Health. (2011) 13:211–20.
15. Bachmann S. Epidemiology of suicide and the psychiatric perspective. Int J Environ Res Public Health. (2018) 15:1425. doi: 10.3390/ijerph15071425
16. Sareen J, Cox BJ, Afifi TO, De Graaf R, Asmundson GJG, Ten Have M, et al. Anxiety disorders and risk for suicidal ideation and suicide attempts: a population-based longitudinal study of adults. Arch General Psychiatry. (2005) 62:1249–57. doi: 10.1001/archpsyc.62.11.1249
17. Bolton JM, Cox BJ, Afifi TO, Enns MW, Bienvenu OJ, Sareen J. Anxiety disorders and risk for suicide attempts: findings from the Baltimore epidemiologic catchment area follow-up study. Depression Anxiety. (2008) 25:477–81. doi: 10.1002/da.20314
18. Heyman M, Dill J, Robert Douglas N. The Ruderman White Paper on Mental Health and Suicide of First Responders (2018). Available online at: https://rudermanfoundation.org/white_papers/police-officers-and-firefighters-aremore-likely-to-die-by-suicide-than-in-line-of-duty (accessed April 29, 2020).
19. Joseph PN, Violanti JM, Donahue R, Andrew ME, Trevisan M, Burchfiel CM, et al. Police work and subclinical atherosclerosis. J Occup Environ Med. (2009) 51:700–7. doi: 10.1097/JOM.0b013e3181a02252
20. Ramey SL, Downing NR, Franke WD. Milwaukee police department retirees. AAOHN J. (2009) 57:448–53. doi: 10.3928/08910162-20091019-02
21. Mccraty R, Atkinson M. Resilience training program reduces physiological and psychological stress in police officers. Glob Adv Health Med. (2012) 1:44–66. doi: 10.7453/gahmj.2012.1.5.013
22. Correia AR, Dunningham W. Estimativa da ocorrência de transtorno do estresse pós- traumático em policiais militares da Bahia [Estimate of the occurrence of post-traumatic stress disorder in military police from Bahia]. Rev Brasil Neurol Psiquiatria. (2016) 20:187–216.
23. Lipp M. Stress and quality of life of senior Brazilian police officers. Spanish J Psychol. (2009) 12:593–603. doi: 10.1017/S1138741600001967
24. Gonçalves T, Silva B. Estresse, depressão e ansiedade: um enfoque sobre a saúde mental do policial militar [Stress, depression and anxiety: a focus on mental health of military police] (Graduation thesis). Academia da Polícia Militar de Goiás. Goiânia (2018).
25. Coleta A. Fatores de estresse ocupacional e coping entre policiais civis [Occupational stress factors and coing among civil police]. Psico USF. (2008) 13:59–68. doi: 10.1590/S1413-82712008000100008
26. Coelho Alves JS, Bendassolli PF, Guedes Gondim SM. Emotional labor and burnout: a study with the military police. Avances Psicol Lationamericana. (2017) 35:459–72. doi: 10.12804/revistas.urosario.edu.co/apl/a.4505
27. Mariano BD, Brambilla BB. Uma análise crítica sobre suicídio policial [A Critical Analysis on Police Suicide]. São Paulo: Ouvidoria da Polícia do Estado de São Paulo (2019).
28. Numbeo. Crime Index by Country 2020. (2020). Available online at: https://www.numbeo.com/crime/rankings_by_country.jsp (accessed December 21, 2020)
29. Bueno S, Lima RS. Brazillian 13th Public Security Annual Report. São Paulo Observatório de Segurança Pública - OSP (2019).
31. Covey TJ, Shucard JL, Violanti JM, Lee J, Shucard DW. The effects of exposure to traumatic stressors on inhibitory control in police officers: a dense electrode array study using a Go/NoGo continuous performance task. Int J Psychophysiol. (2013) 87:363–75. doi: 10.1016/j.ijpsycho.2013.03.009
32. Rajaratnam SMW, Barger LK, Lockley SW, Shea SA, Wang W, Landrigan CP, et al. Sleep disorders, health, and safety in police officers. JAMA. (2011) 306:2567–78. doi: 10.1001/jama.2011.1851
33. James L. The stability of implicit racial bias in police officers. Police Q. (2017) 21:1–23. doi: 10.1177/1098611117732974
34. Ma DS, Correll J, Wittenbrink B, Bar-anan Y, Sriram N, Nosek BA, et al. When fatigue turns deadly : the association between fatigue and racial bias in the decision to shoot. (2013) 35:515–24. doi: 10.1080/01973533.2013.840630
35. Waggoner LB, Grant DA, Van Dongen HPA, Belenky G, Vila B. A combined field and laboratory design for assessing the impact of night shift work on police officer operational performance. Sleep. (2012) 35:1575–7. doi: 10.5665/sleep.2214
36. Euwema MC. Occupational stress and the use of force by Dutch police officers. Crim Justice Behav. (2015) 28:631–52. doi: 10.1177/009385480102800505
37. Martinussen M, Richardsen AM, Burke RJ. Job demands, job resources, and burnout among police officers. J Crim Justice. (2007) 35:239–49. doi: 10.1016/j.jcrimjus.2007.03.001
38. Alexander DA, Walker LG. A study of methods used by Scottish police officers to cope with work-induced stress. Stress Med. (1994) 10:131–8. doi: 10.1002/smi.2460100210
39. The World Health Organization quality of life assessment (WHOQOL): position paper from the World Health Organization. Soc Sci Med. (1995) 41:1403–9. doi: 10.1016/0277-9536(95)00112-K
40. Alexopoulos EC, Palatsidi V, Tigani X, Darviri C. Exploring stress levels, job satisfaction, and quality of life in a sample of police officers in Greece. Safety Health Work. (2014) 5:210–5. doi: 10.1016/j.shaw.2014.07.004
41. Moreira-Almeida A, Neto FL, Koenig HG. Religiousness and mental health: a review. Rev Brasil Psiquiatria. (2006) 28:242–50. doi: 10.1590/S1516-44462006005000006
42. Abdala GA, Kimura M, Koenig HG, Reinert KG, Horton K. Religiosity and quality of life in older adults: literature review. J Aging Phys Activity. (2014) 2:25–51. doi: 10.19141/2237-3756/lifestyle.v2.n2.p25-51
43. Koenig HG, Büssing A. The Duke University Religion Index (DUREL): a five-item measure for use in epidemological studies. Religions. (2010) 1:78–85. doi: 10.3390/rel1010078
44. Sigler RT, Thweatt DR. Religiosity and stress for police officers. J Police Crim Psychol. (1997) 12:13–24. doi: 10.1007/BF02813807
45. Benefiel M, Fry LW, Geigle D. Advances in Workplace Spirituality: Theory, Research and Application. Charlotte, NC: IAP Information Age Publishing (2012).
46. Segal ZV, Williams JMG, Teasdale JD. Mindfulness-Based Cognitive Therapy for Depression: A New Approach to Preventing Relapse. New York, NY: Guilford Press (2002).
47. Crane RS, Brewer J, Feldman C, Kabat-Zinn J, Santorelli S, Williams JMG, et al. What defines mindfulness-based programs? The warp and the weft. Psychol Med. (2016) 47:990–9. doi: 10.1017/S0033291716003317
48. Neff KD. Development and validation of a scale to measure self-compassion. Self Identity. (2003) 2:223–50. doi: 10.1080/15298860309027
49. Hölzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, Ott U. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspect Psychol Sci. (2011) 6:537–59. doi: 10.1177/1745691611419671
50. Schuman-Olivier Z, Trombka M, Lovas DA, Brewer JA, Vago DR, Gawande R, et al. Mindfulness and behavior change. Harvard Rev Psychiatry. (2020) 28:371–94. doi: 10.1097/HRP.0000000000000277
51. Khoury B, Sharma M, Rush SE, Fournier C. Mindfulness-based stress reduction for healthy individuals: a meta-analysis. J Psychosomatic Res. (2015) 78:519–28. doi: 10.1016/j.jpsychores.2015.03.009
52. Khoury B, Lecomte T, Fortin G, Masse M, Therien P, Bouchard V, et al. Mindfulness-based therapy: a comprehensive meta-analysis. Clin Psychol Rev. (2013) 33:763–71. doi: 10.1016/j.cpr.2013.05.005
53. Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: a meta-analytic review. J Consult Clin Psychol. (2010) 78:169–83. doi: 10.1037/a0018555
54. Luken M, Sammons A. Systematic review of mindfulness practice for reducing job burnout. Am J Occup Ther. (2016) 70:7002250020p1–10. doi: 10.5014/ajot.2016.016956
55. Demarzo MMP, Cuijpers P, Zabaleta-del-olmo E, Mahtani KR, Vellinga A, Vicens C. The efficacy of mindfulness-based interventions in primary care: a meta-analytic review. Ann Fam Med. (2015) 13:573–82. doi: 10.1370/afm.1863
56. Chiesa A, Serretti A. Mindfulness-based stress reduction for stress management in healthy people: a review and meta-analysis. J Alternative Complement Med. (2009) 15:593–600. doi: 10.1089/acm.2008.0495
57. Vonderlin R, Biermann M, Bohus M, Lyssenko L. Mindfulness-based programs in the workplace: a meta-analysis of randomized controlled trials. Mindfulness. (2020) 11:1579–98. doi: 10.1007/s12671-020-01328-3
58. Bijlsma T, Muis S, van Tilborg A. Mindfulness in the Dutch military train your brain. In: Rocha Á, Guarda T, editors. Developments and Advances in Defense and Security. Singapore: Springer (2018). p. 155–79.
59. Jha AP, Morrison AB, Parker SC, Stanley EA. Practice is protective: mindfulness training promotes cognitive resilience in high-stress cohorts. Mindfulness. (2017) 8:46–58. doi: 10.1007/s12671-015-0465-9
60. Jha AP, Stanley EA, Kiyonaga A, Wong L, Gelfand L. Examining the protective effects of mindfulness training on working memory capacity and affective experience. Emotion. (2010) 10:54–64. doi: 10.1037/a0018438
61. Johnson DC, Thom NJ, Stanley EA, Haase L, Simmons AN, Shih PAB, et al. Modifying resilience mechanisms in atrisk individuals: a controlled study of mindfulness training in marines preparing for deployment. Am J Psychiatry. (2014) 171:844–53. doi: 10.1176/appi.ajp.2014.13040502
62. Zimmermann F. Mindfulness-based practices as a resource for health and well-being. Med Acupuncture. (2015) 27:349–59. doi: 10.1089/acu.2014.1080
63. Irving JA, Dobkin PL, Park J. Cultivating mindfulness in health care professionals: a review of empirical studies of mindfulness-based stress reduction (MBSR). Complement Ther Clin Prac. (2009) 15:61–6. doi: 10.1016/j.ctcp.2009.01.002
64. Kaplan JB, Bergman AL, Christopher M, Bowen S, Hunsinger M. Role of resilience in mindfulness training for first responders. Mindfulness. (2017) 8:1373–80. doi: 10.1007/s12671-017-0713-2
65. Meiklejohn J, Phillips C, Freedman ML, Griffin ML, Biegel G, Roach A, et al. Integrating mindfulness training into K-12 education: fostering the resilience of teachers and students. Mindfulness. (2012) 3:291–307. doi: 10.1007/s12671-012-0094-5
66. Christopher MS, Goerling RJ, Rogers BS, Hunsinger M, Baron G, Bergman AL, et al. A pilot study evaluating the effectiveness of a mindfulness-based intervention on cortisol awakening response and health outcomes among law enforcement officers. J Police Crim Psychol. (2016) 31:15–28. doi: 10.1007/s11896-015-9161-x
67. Christopher MS, Hunsinger M, Goerling LRJ, Bowen S, Rogers BS, Gross CR, et al. Mindfulness-based resilience training to reduce health risk, stress reactivity, and aggression among law enforcement officers: a feasibility and preliminary efficacy trial. Psychiatry Res. (2018) 264:104–15. doi: 10.1016/j.psychres.2018.03.059
68. Grupe DW, McGehee C, Smith C, Francis AD, Mumford JA, Davidson RJ. Mindfulness training reduces PTSD symptoms and improves stress-related health outcomes in police officers. J Police Crim Psychol. (2019) 1–14. doi: 10.31231/osf.io/jk4e6
69. Krick A, Felfe J. Who benefits from mindfulness? The moderating role of personality and social norms for the effectiveness on psychological and physiological outcomes among police officers. J Occup Health Psychol. (2020) 25:99–112. doi: 10.1037/ocp0000159
70. Jeste DV, Palmer BW, Rettew DC, Boardman S. Positive psychiatry: its time has come. J Clin Psychiatry. (2015) 76:675–83. doi: 10.4088/JCP.14nr09599
71. Peñalba V, McGuire H, Leite JR. Psychosocial interventions for prevention of psychological disorders in law enforcement officers. Cochrane Database System Rev. (2008) 16:CD005601. doi: 10.1002/14651858.CD005601.pub2
72. Patterson GT, Chung IW, Swan PW. Stress management interventions for police officers and recruits: a meta-analysis. J Exp Criminol. (2014) 10:487–513. doi: 10.1007/s11292-014-9214-7
73. Trombka M, Demarzo M, Bacas DC, Antonio SB, Cicuto K, Salvo V, et al. Study protocol of a multicenter randomized controlled trial of mindfulness training to reduce burnout and promote quality of life in police officers: the POLICE study. BMC Psychiatry. (2018) 18:1–9. doi: 10.1186/s12888-018-1726-7
74. Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Arch General Psychiatry. (2002) 59:877–83. doi: 10.1001/archpsyc.59.10.877
75. Chan AW, Tetzlaff JM, Altman DG. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Internal Med. (2013) 158:200–7. doi: 10.7326/0003-4819-158-3-201302050-00583
76. Demarzo M, Garcia-Campayo J. Manual Prático de Mindfulness: Curiosidade e Aceitação [Mindfulness Practical Manual: Curiosity and Acceptance]. São Paulo: Pallas Athena (2015).
77. Kabat-Zinn J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain and Illness New York, NY: Delacorte Press (1990).
78. Dimeff L, Linehan MM. Dialectical behavior therapy in a nutshell. California Psychol. (2001) 34:10–3.
79. Luciano JV, Guallar JA, Aguado J, López-Del-Hoyo Y, Olivan B, Magallón R, et al. Effectiveness of group acceptance and commitment therapy for fibromyalgia: a 6-month randomized controlled trial (EFFIGACT study). Pain. (2014) 155:693–702. doi: 10.1016/j.pain.2013.12.029
80. Ciarrochi J, Kashdan TB. Mindfulness, Acceptance, and Positive Psychology. The Seven Foundations of Well-Being. Oakland, CA: The Context Press (2013).
81. Kuyken W, Hayes R, Barrett B, Byng R, Dalgleish T, Kessler D, et al. The effectiveness and cost-effectiveness of mindfulness-based cognitive therapy compared with maintenance antidepressant treatment in the prevention of depressive relapse/recurrence: results of a randomised controlled trial (The PREVENT study). Health Technol Assessment. (2015) 19:1–123. doi: 10.3310/hta19730
82. Cusens B, Duggan GB, Thorne K, Burch V. Evaluation of the breathworks mindfulness-based pain management programme: effects on well-being and multiple measures of mindfulness. Clin Psychol Psychother. (2009) 17:1. doi: 10.1002/cpp.653
83. British Association for Mindfulness-Based Approaches. Good Practice Guidance for Teachers. (2015). Available online at: https://bamba.org.uk/ (accessed April 26, 2020).
84. Brazilian Center for Mindfulness and Health Promotion. (2015). Available online at: https://mindfulnessbrasil.com/formacao/formacao-modular/boas-praticas (accessed April 26, 2020).
85. Fleck MP, Louzada S, Xavier M, Chachamovich E, Vieira G, Santos L, et al. Application of the Portuguese version of the abbreviated instrument of quality life WHOQOL-bref. Rev Saude Publica. (2000) 34:178–83. doi: 10.1590/S0034-89102000000200012
86. Botega NJ, Bio MR, Zomignani MA, Garcia C, Pereira WA. Mood disorders among inpatients in ambulatory and validation of the anxiety and depression scale HAD. Rev Saúde Pública. (1995) 29:355–63. doi: 10.1590/S0034-89101995000500004
87. Lucchetti G, Lucchetti ALG, Peres MF, Leão FC, Moreira-Almeida A, Koenig HG. Validation of the Duke Religion Index: DUREL (Portuguese Version). J Religion Health. (2012) 51:579–86. doi: 10.1007/s10943-010-9429-5
88. de Barros VV, Kozasa EH, Souza de ICW, Ronzani TM. Validity evidence of the Brazilian version of the Mindful Attention Awareness Scale (MAAS). Psicologia. (2015) 28:87–95. doi: 10.1590/1678-7153.201528110
89. Souza LK, Hutz CS. Adaptation of the Self-Compassion Scale for use in Brazil: evidences of construct validity. Temas Psicol. (2016) 24:159–72. doi: 10.9788/TP2016.1-11
90. Zimpel RR, Panzini RG, Bandeira DR, Fleck MP, da Rocha NS. Psychometric properties of the whoqol-srpb bref, Brazilian Portuguese version. Brazil J Psychiatry. (2019) 41:411–8. doi: 10.1590/1516-4446-2018-0083
91. Chakraborty H, Gu H. A Mixed Model Approach for Intent-to-Treat Analysis in Longitudinal Clinical Trials With Missing Values. Research Triangle Park: RTI Press (2009).
92. Gueorguieva R, Krystal JH. Move over ANOVA: progress in analyzing repeated-measures data and its reflection in papers published in the archives of general psychiatry. Arch General Psychiatry. (2004) 61:310–7. doi: 10.1001/archpsyc.61.3.310
93. Salim A, Mackinnon A, Christensen H, Griffiths K. Comparison of data analysis strategies for intent-to-treat analysis in pre-test-post-test designs with substantial dropout rates. Psychiatry Res. (2008) 160:335–45. doi: 10.1016/j.psychres.2007.08.005
94. Schielzeth H, Dingemanse NJ, Nakagawa S, Westneat DF, Allegue H, Teplitsky C, et al. Robustness of linear mixed-effects models to violations of distributional assumptions. Methods Ecol Evolut. (2020) 11:1141–52. doi: 10.1111/2041-210X.13434
97. Schmider E, Ziegler M, Danay E, Beyer L, Bühner M. Is it really robust? Reinvestigating the robustness of ANOVA against violations of the normal distribution assumption. Methodology. (2010) 6:147–51. doi: 10.1027/1614-2241/a000016
98. Mahoney AEJ, Mackenzie A, Williams AD, Smith J, Andrews G. Internet cognitive behavioural treatment for obsessive compulsive disorder: a randomised controlled trial. Behav Res Ther. (2014) 66:99–106. doi: 10.1016/j.brat.2014.09.012
99. Newby JM, Mewton L, Andrews G. Transdiagnostic versus disorder-specific internet-delivered cognitive behaviour therapy for anxiety and depression in primary care. J Anxiety Disord. (2017) 16:25–34. doi: 10.1016/j.janxdis.2016.06.002
100. Botella J, Sanchez-Meca J. Meta-análisis en Ciencias Sociales y de la Salud. Madrid: Síntesis (2015).
101. Cumming G, Calin-Jageman R. Introduction to the New Estatistics: Estimation, Open Science, and Beyond. New York, NY: Routledge (2017).
102. Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirekt effects in simple mediation models. Behav Res Methods Instruments Comput. (2004) 36:717–31. doi: 10.3758/BF03206553
103. Fitzhugh H, Michaelides G, Anglia E, Connolly S, Anglia E, Daniels K, et al. Mindfulness in Policing. A Randomised Controlled Trial of Two Online Mindfulness Resources Across Five Forces in England and Wales. Coventry: UK College of Policing Report (2019).
104. Vibe M, Bjørndal A, Tipton E, Hammerstrøm K. Mindfulness based stress reduction (MBSR) for improving health, quality of life, and social functioning in adults. Campbell Syst Rev. (2017) 13:1–264. doi: 10.4073/csr.2017.11
105. Azad E. The effectiveness of mindfulness training in improving the quality of life of the war victims with post traumatic stress disorder (PTSD). Iran J Psychiatry. (2014) 9:228–36.
106. Polusny MA, Erbes CR, Thuras P, Moran A, Lamberty GJ, Collins RC, et al. Mindfulness-based stress reduction for posttraumatic stress disorder among veterans: a randomized clinical trial. JAMA. (2015) 314:456–65. doi: 10.1001/jama.2015.8361
107. Serpa JG, Taylor SL, Tillisch K. Mindfulness-based stress reduction (MBSR) reduces anxiety, depression, and suicidal ideation in veterans. Med Care. (2014) 52(12 Suppl. 5):S19–24. doi: 10.1097/MLR.0000000000000202
108. Jasbi M, Sadeghi Bahmani D, Karami G, Omidbeygi M, Peyravi M, Panahi A, et al. Influence of adjuvant mindfulness-based cognitive therapy (MBCT) on symptoms of post-traumatic stress disorder (PTSD) in veterans-results from a randomized control study. Cogn Behav Ther. (2018) 47:431–46. doi: 10.1080/16506073.2018.1445773
109. Kluepfel L, Ward T, Yehuda R, Dimoulas E, Smith A, Daly K. The evaluation of mindfulness-based stress reduction for veterans with mental health conditions. J Holistic Nurs. (2013) 31:248–55. doi: 10.1177/0898010113495975
110. Meland A, Ishimatsu K, Pensgaard AM, Wagstaff A, Fonne V, Garde AH, et al. Impact of mindfulness training on physiological measures of stress and objective measures of attention control in a military helicopter unit. Int J Aviation Psychol. (2015) 25:191–208. doi: 10.1080/10508414.2015.1162639
111. Solhaug I, de Vibe M, Friborg O, Sørlie T, Tyssen R, Bjørndal A, et al. Long-term mental health effects of mindfulness training: a 4-year follow-up study. Mindfulness. (2019) 10:1661–72. doi: 10.1007/s12671-019-01100-2
112. Lo F, Arendt M, Ørnbøl E, Fink P, Mindfulness- WH. Mindfulness-based stress reduction and mindfulness-based cognitive therapy - a systematic review of randomized controlled trials. Acta Psychiatr Scand. (2011) 124:102–19. doi: 10.1111/j.1600-0447.2011.01704.x
113. Furukawa TA, Noma H, Caldwell DM, Honyashiki M, Shinohara K, Imai H, et al. Waiting list may be a nocebo condition in psychotherapy trials: a contribution from network meta-analysis. Acta Psychiatrica Scand. (2014) 130:181–92. doi: 10.1111/acps.12275
114. Demarzo MM, Andreoni S, Sanches N, Perez S, Fortes SG-CJ. Mindfulness-Based Stress Reduction (MBSR) in perceived stress and quality of life: an open, uncontrolled study in a Brazilian healthy sample. Explore. (2014) 10:118–20. doi: 10.1016/j.explore.2013.12.005
115. Skevington SM, Lotfy M, O'Connell KA. The World Health Organization's WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial a Report from the WHOQOL Group. Qual Life Res. (2004) 13:299–310. doi: 10.1023/B:QURE.0000018486.91360.00
116. Hawthorne G, Herrman H, Murphy B. Interpreting the WHOQOL-Bref: preliminary population norms and effect sizes. Social Indicat Res. (2006) 77:37–59. doi: 10.1007/s11205-005-5552-1
117. Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale: an updated literature review. J Psychosomatic Res. (2002) 52:69–77. doi: 10.1016/S0022-3999(01)00296-3
118. Couto G, Brito EDAG, Vasconcelos-Silva A, Lucchese R. Saúde mental do policial militar: Relações interpessoais e estresse no exercício profissional [Military police mental health: interpersonal relationships and stress in professional practice]. Psicol Argumento. (2017) 30:185–94. doi: 10.7213/psicol.argum.5896
119. Numbeo. Crime Index by City 2020. (2020). Available online at: https://www.numbeo.com/crime/rankings.jsp (accessed April 15, 2020).
120. Carvalho AL, Cury AA, Garcia RC. Prevalence of bruxism and emotional stress and the association between them in Brazilian police officers. Brazilian Oral Res. (2008) 22:31–5. doi: 10.1590/S1806-83242008000100006
121. Anchieta VCC, Galinkin AL. Policiais civis: representando a violência [civil police officers: representing violence]. Psicol Sociedade. (2005) 17:29–37. doi: 10.1590/S0102-71822005000100005
122. Garbarino S, Magnavita N, Elovainio M, Heponiemi T, Ciprani F, Cuomo G, et al. Police job strain during routine activities and a major event. Occup Med. (2011) 61:395. doi: 10.1093/occmed/kqr058
123. Wallace BA, Shapiro SL. Mental balance and well-being: building bridges between Buddhism and Western psychology. Am Psychol. (2006) 61:690–701. doi: 10.1037/0003-066X.61.7.690
124. Garland SN, Carlson LE, Cook S, Lansdell L, Speca M. A non-randomized comparison of mindfulness-based stress reduction and healing arts programs for facilitating post-traumatic growth and spirituality in cancer outpatients. Support Care Cancer. (2007) 15:949–61. doi: 10.1007/s00520-007-0280-5
125. Henderson VP, Clemow L, Massion AO, Hurley TG. The effects of mindfulness-based stress reduction on psychosocial outcomes and quality of life in early-stage breast cancer patients : a randomized trial. Breast Cancer Res Treat. (2012) 131:99–109. doi: 10.1007/s10549-011-1738-1
126. Crescentini C, Urgesi C, Campanella F, Eleopra R, Fabbro F. Effects of an 8-week meditation program on the implicit and explicit attitudes toward religious/spiritual self-representations. Conscious Cogn. (2014) 30:266–80. doi: 10.1016/j.concog.2014.09.013
127. IBGE Demographic Census (2010). Available online at: https://censo2010.ibge.gov.br/ (accessed April 24, 2020).
128. Kuyken W, Watkins E, Holden E, White K, Taylor RS, Byford S, et al. How does mindfulness-based cognitive therapy work? Behav Res Ther. (2010) 48:1105–12. doi: 10.1016/j.brat.2010.08.003
129. Velden AM, Kuyken W, Wattar U, Crane C, Pallesen KJ, Dahlgaard J, et al. A systematic review of mechanisms of change in mindfulness-based cognitive therapy in the treatment of recurrent major depressive disorder. Clin Psychol Rev. (2015) 37:26–39. doi: 10.1016/j.cpr.2015.02.001
130. Sevel LS, Finn MTM, Smith RM, Ryden AM, McKernan LC. Self-compassion in mindfulness-based stress reduction: an examination of prediction and mediation of intervention effects. Stress Health. (2020) 36:88–96. doi: 10.1002/smi.2917
131. Campos D, Cebolla A, Quero S, Bretón-López J, Botella C, Soler J, et al. Meditation and happiness: mindfulness and self-compassion may mediate the meditation-happiness relationship. Personal Individual Differ. (2016) 93:80–5. doi: 10.1016/j.paid.2015.08.040
132. Sünbül ZA, Malkoç A. A mindful pathway to flourishing: mediating effects of self-compassion and valued living in college students. Eur J Educ Stud. (2018) 5:174–85. doi: 10.5281/zenodo.140708
133. Keng SL, Smoski MJ, Robins CJ, Ekblad AG, Brantley JG. Mechanisms of change in mindfulness-based stress reduction: self-compassion and mindfulness as mediators of intervention outcomes. J Cogn Psychother. (2012) 26:270–80. doi: 10.1891/0889-8391.26.3.270
134. Baer RA, Lykins ELB, Peters JR. Mindfulness and self-compassion as predictors of psychological wellbeing in long-term meditators and matched nonmeditators. J Positive Psychol. (2012) 7:230–8. doi: 10.1080/17439760.2012.674548
135. Satici SA, Uysal R, Akin A. Investigating the relationship between flourishing and self-compassion:A structural equation modeling approach. Psychol Belgica. (2013) 53:85–99. doi: 10.5334/pb-53-4-85
136. Yang Y, Zhang M, Kou Y. Self-compassion and life satisfaction: the mediating role of hope. Personal Individual Differ. (2016) 98:91–5. doi: 10.1016/j.paid.2016.03.086
137. Neff K, Kirkpatrick K, Rude S. Self-compassion and adaptive psychological functioning. J Res Personal. (2007) 41:139–54. doi: 10.1016/j.jrp.2006.03.004
138. Arimitsu K, Hofmann SG. Cognitions as mediators in the relationship between self-compassion and affect. Personal Individual Differ. (2015) 74:41–8. doi: 10.1016/j.paid.2014.10.008
139. Krieger T, Holtforth MG. Self-compassion in depression : associations with depressive symptoms, Rumination, and Avoidance in Depressed Outpatients. Behav Ther. (2013) 44:501–13. doi: 10.1016/j.beth.2013.04.004
140. Leary MR, Tate EB, Adams CE, Allen AB, Hancock J. Self-compassion and reactions to unpleasant self-relevant events : the implications of treating oneself kindly. J Pers Soc Psychol. (2007) 92:887–904. doi: 10.1037/0022-3514.92.5.887
141. Neff K. Self-compassion: an alternative conceptualization of a healthy attitude toward oneself. Self Identity. (2003) 2:85–101. doi: 10.1080/15298860309032
142. Berking M, Meier C. Enhancing emotion-regulation skills in police officers : results of a pilot controlled study. Behav Ther. (2010) 41:329–39. doi: 10.1016/j.beth.2009.08.001
143. Hayes SC, Strosahl K, Wilson KG, Bissett RT, Pistorello J, Toarmino D, et al. Measuring experiential avoidance: a preliminary test of a working model. Psychol Record. (2004) 54:553–78. doi: 10.1007/BF03395492
144. Amaranto E, Steinberg J, Castellano C, Mitchell R. Police stress interventions. Brief Treat Crisis Intervent. (2003) 3:47–53. doi: 10.1093/brief-treatment/mhg001
145. Pogrebin MR, Poole ED. Emotion management: a study of police response to tragic events. In: Flaherty MG, Ellis C, editors. Social Perspectives on Emotion. Greenwich, CT: Elsevier Science/JAI Press (1995). p. 149–68.
146. Williams V, Ciarrochi J, Deane FP. On being mindful, emotionally aware, and more resilient: longitudinal pilot study of police recruits. Austral Psychol. (2010) 45:274–82. doi: 10.1080/00050060903573197
147. Chopko BA, Palmieri PA, Adams RE. Associations between police stress and alcohol use: implications for practice. J Loss Trauma Int Perspect Stress Coping. (2013) 18:482–97. doi: 10.1080/15325024.2012.719340
148. Komarovskaya I, Maguen S, Mccaslin SE, Metzler TJ, Madan A, Brown AD, et al. The impact of killing and injuring others on mental health symptoms among police officers. J Psychiatric Res. (2011) 45:1332–6. doi: 10.1016/j.jpsychires.2011.05.004
149. Kirschner H, Kuyken W, Wright K, Roberts H, Brejcha C, Karl A. Soothing your heart and feeling connected: a new experimental paradigm to study the benefits of self-compassion. Clin Psychol Sci. (2019) 7:545–65. doi: 10.1177/2167702618812438
150. Brito-Pons G, Campos D, Cebolla A. Implicit or explicit compassion? Effects of compassion cultivation training and comparison with mindfulness-based stress reduction. Mindfulness. (2018) 9:1494–508. doi: 10.1007/s12671-018-0898-z
151. Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Personal Social Psychol. (2003) 84:822–48. doi: 10.1037/0022-3514.84.4.822
152. Brownson C. Self-regulation: an “active ingredient” in the spirituality-health relationship (Indianapolis, IN: Undergraduate Honors Thesis Collection) (2012).
153. Aldwin CM, Park CL, Jeong YJ, Nath R. Differing pathways between religiousness, spirituality, and health: a self-regulation perspective. Psychol Religion Spiritual. (2014) 6:9–21. doi: 10.1037/a0034416
154. Prazak M, Critelli J, Martin L, Miranda V, Purdum M, Powers C. Mindfulness and its role in physical and psychological health. Appl Psychol Health Well Being. (2012) 4:91–105. doi: 10.1111/j.1758-0854.2011.01063.x
155. Musick MA, Traphagan JW, Koenig HG, Larson DB. Spirituality in physical health and aging. J Adult Dev. (2000) 7:73–86. doi: 10.1023/A:1009523722920
156. Lawler-Row KA, Elliott J. The role of religious activity and spirituality in the health and well-being of older adults. J Health Psychol. (2009) 14:43–52. doi: 10.1177/1359105308097944
157. Charles GL, Travis F, Smith J. Policing and spirituality: their impact on brain integration and consciousness. J Manage Spiritual Religion. (2014) 11:230–44. doi: 10.1080/14766086.2014.887479
158. Bergman AL, Christopher MS, Bowen S. Changes in facets of mindfulness predict stress and anger outcomes for police officers. Mindfulness. (2016) 7:851–8. doi: 10.1007/s12671-016-0522-z
159. Alsubaie M, Abbott R, Dunn B, Dickens C, Keil TF, Henley W, et al. Mechanisms of action in mindfulness-based cognitive therapy (MBCT) and mindfulness-based stress reduction (MBSR) in people with physical and/or psychological conditions: a systematic review. Clin Psychol Rev. (2017) 55:74–91. doi: 10.1016/j.cpr.2017.04.008
160. Carmody J, Baer RA. How long does a mindfulness-based stress reduction program need to be? A review of class contact hours and effect sizes for psychological distress. J Clin Psychol. (2009) 65:627–38. doi: 10.1002/jclp.20555
161. Demarzo M, Montero-Marin J, Puebla-Guedea M, Navarro-Gil M, Herrera-Mercadal P, Moreno-González S, et al. Efficacy of 8- and 4-session mindfulness-based interventions in a non-clinical population: a controlled study. Front Psychol. (2017) 8:1343. doi: 10.3389/fpsyg.2017.01343
162. Morone NE, Greco CM, Weiner DK. Mindfulness meditation for the treatment of chronic low back pain in older adults: a randomized controlled pilot study. Pain. (2008) 134:310–9. doi: 10.1016/j.pain.2007.04.038
163. Cunningham JA, Kypri K, McCambridge J. Exploratory randomized controlled trial evaluating the impact of a waiting list control design. BMC Med Res Methodol. (2013) 13:150. doi: 10.1186/1471-2288-13-150
164. Verweij M. What is preventive medicine? Can Family Phys. (2000) 20:13–23. doi: 10.1007/978-94-015-9365-6_2
165. Hesketh R, Strang L, Pollitt A, Wilkinson B. What Do We Know About the Effectiveness of Workplace Mental Health Interventions? London: The Policy Institute; King's College London (2020).
166. Lueke A, Gibson B. Mindfulness meditation reduces implicit age and race bias: the role of reduced automaticity of responding. Soc Psychol Personal Sci. (2014) 6:1–8. doi: 10.1177/1948550614559651
167. Stell AJ, Farsides T. Brief loving-kindness meditation reduces racial bias, mediated by positive other-regarding emotions. Motivation Emotion. (2015) 40:140–7. doi: 10.1007/s11031-015-9514-x
168. Demarzo M, Cebolla A, Garcia-Campayo J. The implementation of mindfulness in healthcare systems: a theoretical analysis. General Hospital Psychiatry. (2015) 37:166–71. doi: 10.1016/j.genhosppsych.2014.11.013
169. Neff K, Germer C. The Mindful Self-Compassion Workbook: A Proven Way to Accept Yourself, Build Inner Strength, and Thrive. New York, NY: Guilford Publications (2018).
Keywords: mindfulness, police officer, quality of life, depression, anxiety, religiosity, well-being, self-compassion
Citation: Trombka M, Demarzo M, Campos D, Antonio SB, Cicuto K, Walcher AL, García-Campayo J, Schuman-Olivier Z and Rocha NS (2021) Mindfulness Training Improves Quality of Life and Reduces Depression and Anxiety Symptoms Among Police Officers: Results From the POLICE Study—A Multicenter Randomized Controlled Trial. Front. Psychiatry 12:624876. doi: 10.3389/fpsyt.2021.624876
Received: 01 November 2020; Accepted: 21 January 2021;
Published: 26 February 2021.
Edited by:
Angela Fang, University of Washington, United StatesReviewed by:
Sverre Urnes Johnson, University of Oslo, NorwayCopyright © 2021 Trombka, Demarzo, Campos, Antonio, Cicuto, Walcher, García-Campayo, Schuman-Olivier and Rocha. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marcelo Trombka, bWFyY2Vsb3Ryb21ia2FAZ21haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.