
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Psychiatry , 09 February 2021
Sec. Psychopathology
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.601236
This article is part of the Research Topic Perinatal Mental Health: Expanding the Focus to the Family Context View all 30 articles
Intimate partner violence (IPV) affects individuals and families from all backgrounds, regardless of their ethnicity, socio-economic status, sexual orientation, or religion. Pregnancy and childbirth could be a time of vulnerability to violence because of changes in physical, emotional, social, and economic demands and needs. Prevalence of IPV against women during the perinatal period is increasingly researched and documented. However, evidence on IPV prevalence among intimate partners as well as on the course of IPV over the perinatal period is scarce. The purpose of this review was to provide a narrative synthesis of the existing literature regarding the prevalence estimates of IPV among intimate partners over the perinatal period. Through this review, we also gained better insight into associated factors, as well as the various forms of IPV. Of the 766 studies assessing prevalence estimates identified, 86 were included, where 80 studies focused on unidirectional IPV (i.e., perpetrated by men against women) and six studies investigated bidirectional IPV (i.e., IPV perpetrated by both partners). Most of the included studies reported lower overall prevalence rates for unidirectional IPV postpartum (range: 2–58%) compared to pregnancy (range: 1.5–66.9%). Psychological violence was found to be the most prevalent form of violence during the entire perinatal period. Studies on bidirectional IPV mostly reported women's perpetration to be almost as high as that of their partner or even higher, yet their findings need to be interpreted with caution. In addition, our results also highlighted the associated factors of IPV among partners, in which they were assimilated into a multi-level ecological model and were analyzed through an intersectional framework. Based on our findings, IPV is found to be highly prevalent during the entire perinatal period and in populations suffering from social inequalities. Further research exploring not only the occurrence, but also the motivations and the context of the bidirectionality of IPV during the perinatal period may facilitate better understanding of the detrimental consequences on partners and their families, as well as the development of effective intervention strategies. Public health prevention approaches intervening at optimal times during the perinatal period are also needed.
Intimate partner violence (IPV) affects individuals and families from various ethnic, economic, religious, or sexual backgrounds. The World Health Organization (WHO) defines IPV as “any act or behavior within a present or former intimate relationship that causes physical, psychological, or sexual harm” (1). These behaviors may pertain to (1) acts of physical violence (e.g., hitting, kicking, beating); (2) sexual violence (e.g., forced sexual intercourse, sexual coercion); (3) psychological (emotional) violence (e.g., insults, humiliation, intimidation, threats of harm); (4) controlling behavior (e.g., isolation from family and friends, monitoring movements, restricting access to financial resources, employment, education, medical care) (1, 2). With approximately a third of the women worldwide having experienced IPV during their life (3), IPV represents the most common form of violence against women. The WHO multi-country study on women's health and domestic violence against women found the prevalence of physical IPV in pregnancy to range between 1% in Japan to 28% in Peru, with the majority of sites ranging between 4 and 12% (4). An analysis of Demographic and Health Surveys and the International Violence against Women Survey found prevalence rates for IPV during pregnancy between 2% in Australia, Denmark, Cambodia, and Philippines to 13.5% in Uganda, with the majority ranging between 4 and 9% (5). Clinical studies around the world, which tend to yield higher prevalence rates but often are the only sources of information available, found the highest prevalence in Egypt with 32%, followed by India (28%), Saudi Arabia (21%), and Mexico (11%) (6). A recent review of African clinical studies reported prevalence rates of 23–40% for physical, 3–27% for sexual, and 25–49% for emotional or psychological intimate partner violence during pregnancy (7). Taking into account the variations based on the cultural background and populations investigated, prevalence of IPV could be higher in specific groups, for example, those experiencing critical life events such as the transition to parenthood, which may in turn augment and intersect with already existing factors and thus increase the risk to engage in or experience IPV.
Physical health consequences of IPV perpetrated against women have great negative consequences on the mother and her offspring, including delayed prenatal care, low birth weight (LBW), intrauterine growth retardation, preterm labor, or even miscarriage (7–11). Psychological implications of IPV during the perinatal period may be of particular importance because they may also bear adverse consequences for the mother, the child and the entire family. Depression, post-traumatic stress disorder (PTSD), anxiety, panic disorders, and substance abuse disorders have been documented as the most common psychological consequences of IPV for mothers during their pregnancy and postpartum (5, 12). Maternal depression during pregnancy is associated with an increased risk for offspring's future depression (13), whereas maternal exposure to adverse life events, such as the exposure to violence during pregnancy, has been linked to offspring autism and schizophrenia (14). Maternal PTSD during pregnancy and after childbirth could impact the offspring's hypothalamo-pituitary-adrenocortical (HPA) axis regulation (15), which in turn would result in psychological disorders such as anxiety, eating disorders, and externalizing problems during childhood and later in life (16). The gravest consequence of IPV during the perinatal period is death. Several studies found that maternal injury is a leading cause of maternal mortality; 54.3% of pregnancy-associated suicides involved intimate partner conflict, whereas 45.3% of pregnancy-related femicides were associated with pre-existing IPV victimization of women (17, 18).
Despite great advances in researching IPV, little is known about how victimization experiences may be patterned over the perinatal period (i.e., during the time frame from 1 year before to 24 months after the birth of the child), and how it may represent a period of particular vulnerability to violence. Where prevalence of IPV against women alone is increasingly researched and documented during the perinatal period, reported evidence on bidirectional IPV (i.e., perpetrated by both partners) prevalence is still scarce. Women's IPV perpetration has detrimental health consequences on both partners (19). It increases men's and women's risk for substance abuse and depression (20). While the context of violence toward men has been proven to be very different for women in that it represents defensive or retaliatory behavior, violence common to both partners can nonetheless result in a more stressful and dangerous living environment for children (21). In fact, IPV among intimate partners is associated with child maltreatment and reduced social-emotional child development (22–25). Therefore, it appears to be imperative to not only investigate prevalence estimates of IPV perpetrated against women alone, but to also improve our understanding of bidirectional IPV during pregnancy and postpartum in order to inform the ongoing process of developing effective screening and interventions for women and their families. The purpose of this review is to provide a narrative synthesis of the existing literature regarding the prevalence estimates of IPV among partners over the perinatal period as well as any associated factors. These factors will be analyzed through an intersectional approach that considers individual, family, community, and societal related factors within an ecological model.
A systematic search of the available literature was performed in March 2020 from the following databases: PubMed, Embase via Ovid, CINAHL, and Scopus. The search strategy was developed according to the PICO model to determine search concepts and types of studies. The keywords (and their combinations) adopted for the research are the following: perinatal, perinatal women, perinatal men, perinatal couple, intimate partner violence, IPV, domestic violence, spousal abuse, prevalence, observational studies. Separate searches for each primary database combined Medical Subject Subheadings (MeSH) terms and key text words with the Boolean operators (AND) and (OR), accordingly. The full list of search terms for PubMed can be found in Appendix A.
All publications in English, German, and Arabic languages that appeared between 2000 and 2020 have been considered. For studies to be included in this review, the search was international and had to include a sample that refers to IPV victims affected by it during the perinatal period (i.e., the time frame from 1 year before to 24 months after the birth of the child). The target population were intimate partners, regardless of the nature of their intimate relationship. Only empirical quantitative studies such as cohort, case-control, and cross-sectional studies were included. Qualitative studies were excluded. We considered IPV the primary outcome for this review.
A flowchart of the search and inclusion process is presented in Figure 1. The search provided a total of 766 articles. After removing duplicates, a total of 632 papers were collected and imported into a web-based tool, Rayyan QCRI (26). The abstracts of these articles were checked, in which 546 abstracts demonstrated no relevance for this review and were excluded. Assessment of eligibility of the 102 full-text articles lead to exclusion of 16 articles because they did not report the relationship to perpetrators (i.e., being an intimate partner or a natal family member, etc.), nor did they provide any prevalence estimates. The remaining 86 studies will be described in the results section.
A qualitative approach was employed in synthesizing the results. Since prevalence studies of IPV tend to be highly heterogeneous and violence definitions tend to vary among research settings, we did not consider conducting any quantitative analyses for this review. The relevant data were tabulated in a data extraction form that was developed. Prevalence estimates of IPV among intimate partners, as well as associated factors relevant for IPV during the perinatal period were constructed. For each paper, we extracted and systematized the following information: author and year of publication; setting (e.g., clinical- or population-based); study design; sample size (e.g., final sample, response rate); the directionality of IPV (i.e., uni- or bidirectional); overall IPV prevalence estimates (i.e., during pregnancy, postpartum, or both); and its types (i.e., physical, sexual, psychological, economic). In addition, we also considered population characteristics and associated factors significant to IPV prevalence when available, using a multi-level ecological model where each factor is assimilated into the following levels: (a) the individual level, which represents the biolo- gical and personal history of the individuals; (b) family level, which represents factors relating to the immediate context where abuse took place; (c) community level, which represents factors relating to the formal or informal social institutions or structures in which violent relationships are embedded; and (d) societal level, which represents factors relating to gender inequality, religious or cultural belief systems, societal norms, and economic or social policies (10, 27).
An overview of the study selection process can be found in Figure 1. Eighty-six studies met the inclusion criteria (28–113). The majority of the studies were cross-sectional (n = 75) and few used longitudinal designs (n = 11). The studies originated from 35 countries, published in English, and recruited only women (n = 90,895) (Appendix B). Eighty of the included studies investigated violence against women where the perpetrator was their current or former intimate partner. Six studies explored bidirectional perpetration of IPV, in which women can be both perpetrators as well as victims. Three terms were used to describe the violence, i.e., IPV, Gender-Based Violence (GBV), and Domestic Violence (DV). We excluded studies that reported perpetrators other than intimate partners, such as family members, since the aim of the present review was to summarize and describe the prevalence of violence perpetrated by intimate partners, as well as to investigate what factors were associated with the prevalence of IPV during the perinatal period.
According to the results from the included studies, we found that IPV prevalence estimates were reported either during pregnancy (n = 60) or during the postpartum period (n = 5). Further, some studies reported comparable estimates during both pregnancy and the postpartum period (n = 9), whereas others reported estimates during the entire perinatal period (n = 2) (Table 1).
The overall IPV prevalence during pregnancy ranged from 1.5 to 66.9%, being highest in Kenya (96) and lowest in Sweden (54). During pregnancy, prevalence of psychological violence was the most prevalent form of violence and ranged from 1% in Sweden (54) to 81% in South Africa (53), followed by physical violence, ranging from 0.4% in Sweden (54) to 60.6% in Uganda (44). Sexual violence was reported in 40 studies, with a range between 0.1 and 39.4%. Prevalence estimates for economic violence were reported in two studies only: in Nigeria with 6.8% (72) and in India with 37% (59).
Moreover, the overall IPV prevalence during the 1st year postpartum ranged from 2% in Sweden (102) to 58% in Iran (32). One study reported prevalence estimates within 2 years postpartum (28) for overall IPV (37%) as well as other forms of violence i.e., physical violence (31%), psychological violence (28%), and sexual violence (6%). One study reported estimates of IPV at 3, 6, 12, 18, and 24 months postpartum, with the overall IPV prevalence rate being highest at the earliest measurement point after birth, i.e., 3 months postpartum (21,3, 16, 17.7, 17.7, 12.8%, respectively) (66). In Iran, a study reported IPV prevalence estimates for physical (25%) and psychological violence (35%) during the first 48 h after delivery.
Studies reporting prevalence estimates of IPV both during pregnancy as well as at follow-ups during the postpartum period provided comparable estimates before and after childbirth. A study from Nepal reported a decrease of prevalence rates from pregnancy to 6–10 weeks postpartum for overall (26.2–20%), physical (9.4–4.8%), and sexual IPV (16–7.3%) with an exception for psychological violence, where the prevalence rate remained the same (15%) (40). A study from Bangladesh reported a slight decrease in prevalence estimates for overall (66.4–63.6%), physical (35–32.2%), and sexual IPV (18.5–15.5%) during the first 6 months postpartum compared to the time during pregnancy. However, psychological violence was reported to have significantly increased from 18.5 to 60.8% during the first 6 months postpartum compared to the time during pregnancy (68). In Iran, a study reported increased prevalence estimates for overall (42–53.3%), physical (10–14.7%), psychological (33–42.7%), and sexual IPV (17.3–25%) during 6–18 months postpartum compared to the time during pregnancy (91).
A South African study also reported a decrease in prevalence rates, where overall IPV decreased from 21.3–17.7% during the first 9 months postpartum compared to the time during pregnancy. Prevalence estimates for physical (8.7%), psychological (16.6%), and sexual violence (3%) only occurred during pregnancy (62). Furthermore, a study from Tanzania reported higher prevalence rates during pregnancy for physical (12.4%, 5.2%), psychological (31%, 17.8%), sexual (9%, 3.8%), and economic violence (48.4%, 11.4%) compared to the first 9 months postpartum (84). Prevalence rates for overall (3.7–25.6%) and sexual IPV (0.1–0.5%) were reported to increase postpartum in comparison to the time during pregnancy, whereas physical (14%, 4.3%) and psychological violence (32.9%, 25%) seemed to be higher during pregnancy (87). In Nigeria, a study reported a 20% decrease in overall IPV prevalence (0.8%) during the first 6 weeks postpartum compared to the time during pregnancy (20.8%). Further four studies reported prevalence estimates of IPV during pregnancy and postpartum without providing any comparable estimates before and after childbirth (46, 61, 70, 106) (Table 1).
Lastly, prevalence estimates during the entire perinatal period, where no differentiation between before and after childbirth was made, were reported in two studies. A study in England found only psychological and physical violence to be prevalent, with 24 and 9.6%, respectively (81). Another study from Ghana reported psychological violence as most prevalent with 34%, followed by 17% for physical violence, and 15% for sexual violence (108).
Only six studies investigated bidirectionality of IPV. In the studies focused on bidirectional IPV, two of these studies were during pregnancy (37, 89), one study was during the postpartum period (46), and three studies were during both pregnancy and the postpartum period (42, 58, 66) (Table 2).
Few studies presented the prevalence of IPV victimization and perpetration during the perinatal period over time (Table 2). At baseline (i.e., during pregnancy), a range between 8.5 and 67.7% of women endorsed at least one instance of IPV victimization and 9.4–72.2% endorsed at least one instance of IPV perpetration. At follow-up (i.e., during postpartum), a range between 12.3 and 54.1% of women endorsed at least one instance of IPV victimization and 7.4–64.8% endorsed at least one instance of IPV perpetration. After childbirth, two studies suggest that prevalence of IPV perpetration declined for about 10% (58, 66), whereas Charles & Perreira (41) reported around 20% increase in prevalence (42). In regard to IPV victimization, only Hellmuth et al. (66) reported around 10% increase in prevalence estimates, while others suggest a decrease in prevalence rates for <20% (42, 58). In addition, it was noted that although there is a percentage of women endorsed perpetrating some form of violence against their intimate partners during the perinatal period, it was not clear if this violence was reciprocal or not. Only one longitudinal study (66) reported no reciprocity of IPV perpetration endorsed by women (i.e., 12% during pregnancy and 7% during postpartum). Reciprocity of violence within couples was defined as the endorsement of both perpetration of violence against their partner and victimization of violence by their partner (Table 3) (46).
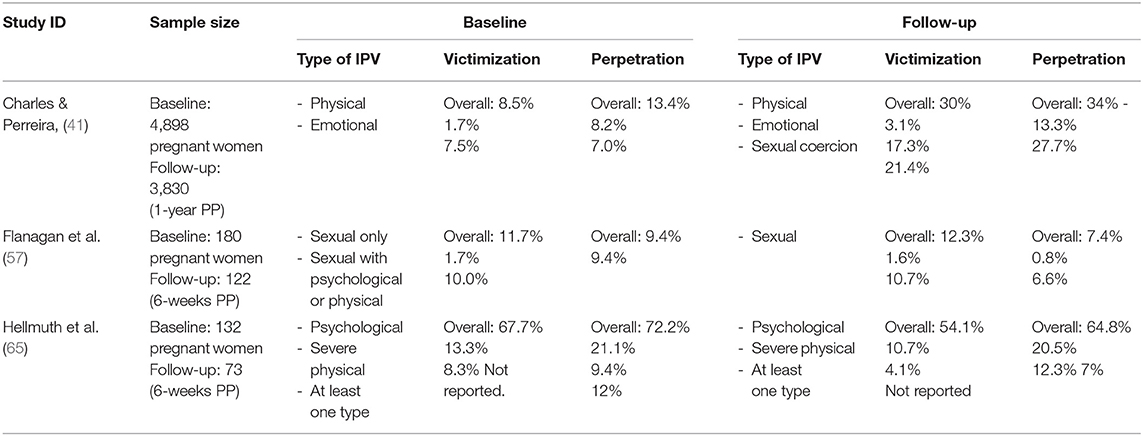
Table 3. Prevalence of types of bidirectional IPV during the perinatal period at baseline and follow-up.
There is a limited consistency in reporting the prevalence of types of IPV victimization or perpetration across the perinatal period. For example, Bahrami-Vazir and colleagues (45) investigated the prevalence of subcategories of IPV perpetration during pregnancy, such as psychological (58%), sexual (30%), or physical violence (22%) (37). Similarly, Charles & Perreira (42) reported only the prevalence rates of physical violence (1.7%) and emotional violence (7.5%) experienced by pregnant women. They also reported prevalence rates of subcategories of IPV during postpartum, such as physical (3.1%) and emotional violence (17.3%), as well as controlling behavior (21.4%). Other authors categorized IPV types based on severity. In Hellmuth et al.'s (65), women who participated during pregnancy reported experiences of severe physical violence (8.3%) and minor psychological violence (13.3%) (66), while another study found that women during postpartum endorsed victimization of minor physical violence (17.5%) and severe physical violence (7.9%) (46). Mohammad-Alizadeh-Charandabi et al. (88) compared prevalence of IPV between age groups, i.e., adolescents (15–19 years of age) and young adults (20–29 years of age) (89). They found that, during pregnancy, sexual IPV victimization was significantly more common in both adolescents and adults, conversely, psychological IPV perpetration was significantly more common than victimization only among the adolescents.
In the following, we focus on associated factors found to be significantly related to IPV either during pregnancy or during the postpartum period. Other studies reported factors during both pregnancy and the postpartum period, whereas even others reported estimates during the entire perinatal period.
In pregnancy, 45 studies investigated associated factors of IPV (Table 4).
At the individual level, risk factors were either related to victims or perpetrators of IPV. Victim-related factors such as pregnant women's lower education (30, 32, 34, 36, 43, 51, 54, 63, 95, 98, 112, 113), younger age (35, 36, 51, 53, 64, 72, 76, 92), unemployment (52, 53, 72, 98), or being self-employed (62), marital status (30, 38, 53, 64), mental health issues (34, 38), alcohol use (38), drug use (64, 77), having previous experience of IPV (92, 103, 110), and having witnessed or been a victim of physical violence during childhood (34, 43, 54, 55, 64, 76, 77, 98, 100) were all associated with higher victimization of IPV. Inappropriate utilization of prenatal care services for pregnant women (40) constituted another significant association, whereas early initiation of antenatal care could be considered a protective factor (35). Moreover, dowry demand (67, 98), low ability for decision-making as well as low self-esteem (68, 97) were also associated with increased risk for IPV. Perpetrator-related factors related to IPV included perpetrator's younger age (34, 78, 96, 103, 104), lower education (35, 50, 57, 97, 104), substance use, including alcohol (34–36, 43, 44, 51, 52, 68, 77, 78, 96, 98, 103, 104, 112, 113), unemployment (34, 50, 57, 59, 72, 112), and having witnessed or been a victim of physical violence during childhood (100).
At the family level, factors such as those relating to marriage, family life, conflict within the family, family's living conditions are explored and included at this level. Partner's control of woman's reproductive health (103) like husband's prohibition of contraception use (44, 108), having previous abortion experience (78), multigravidity (56, 70, 93), multiparity (36, 68, 77, 78, 93, 98, 109), and low parity (72) were significantly associated with increased IPV victimization for women. Financial factors were explored in six studies. IPV increased when the family had financial distress/insufficient income (53–55, 57, 100), or when the women were the providers and the ones responsible for the family's income (34). Further factors like accusations of extramarital affair by husbands (98) or polygamous marriages (33, 76, 95) were explored and found to be statistically significant. A number of studies found the risk of violence increased by undesired pregnancy (53, 54, 93, 97), the pressure on pregnant women to have a male child (70, 93), and by being forced into marriage (32). In contrast, results of Azene et al. (34) indicated that women choosing their husband on their own, i.e., without relying on their family, is associated with IPV in pregnancy (35).
At the community level, factors relating to the extended family, family's residency, and the nature of marriage are explored and included. Pregnant women being related to their husbands more distantly, as well as their less frequent communication with their natal family (43) were found to be a significant factor for increasing IPV. Living in rural areas (35, 68) such as tea plantation sectors in Sri Lanka (91), and lack of social support (92, 98, 104) were found to increase the odds of experiencing IPV. On the contrary, urban residency (36, 63, 93) was also linked to IPV. However, in another study, urban residency was found to be a protective factor against IPV (30), see Table 4.
At the societal level, factors relating to the cultural context are heavily influenced by the social, religious, and political systems and should be included at this level. Pregnant women with a certain ethnicity such as being Jewish women of Sephardic descent, (57), being non-Caucasian (30, 33), with an immigrant status (30), being HIV-positive (48, 49) and having an HIV-positive child (48), or belonging to a certain religion, i.e., Catholic, Muslim, or Hindu (56, 59, 91), as well as endorsing a higher degree of religiosity (religious vs. non-religious) were at higher risk for IPV (57). Studies found that women who endorsed violence supporting attitude were also at risk for experiencing IPV (43, 52, 77, 104).
During the postpartum period, three studies investigated associated factors of IPV (28, 31, 102).
At the individual level and as victim-related factors, IPV risk was significantly higher for younger mothers and those unable to fully meet the sexual expectations of their husbands (31). Institutional delivery opposed to home birth was found to be a protective factor against IPV (28).
At the family level, unplanned pregnancy (31, 102), husband being disappointed about infant gender (i.e., having female children) (31), and having more than one child (102) were significantly related to IPV, see Table 2.
During both pregnancy and the postpartum period, six studies investigated associated factors with IPV (39, 45, 60, 61, 90, 94). Victim-related factors at the individual level included history of IPV (39, 61, 90), women who have lower education (90), and women reporting regular alcohol use during pregnancy and puerperium (94). One study reported higher risk of IPV for employed women (45). As for perpetrator-related factors, one study reported husband's alcohol use (45).
At the family level, longer duration of marriage (39), and insufficient income (45, 60, 90) constituted risk factors (see Table 2).
At the community level, controlling behavior of the mother-in-law was associated with higher victimization of IPV (39). At the societal level, belonging to an ethnic minority (e.g., Janajati ethnicity in Nepal) (39, 61, 90) and being HIV-positive (94) were found to be associated with increased IPV victimization.
Among the studies examining bidirectional perpetration, four of them investigated associated factors of IPV (Table 5).
In pregnancy and at the individual level, intimate partners' dissatisfaction with their own employment status constituted an associated variable for bidirectional IPV during pregnancy (37).
During the postpartum period and at the individual level, insufficient prenatal and postpartum medical care, lower education and/or insecure employment status of mothers were reported to be associated factors (46).
At the family level, unwanted pregnancy was found to be associated with bidirectional IPV, as well as not living with a partner, or living in a household with more than one child younger than 5 years of age (46).
At the societal level, Moaes et al. (45) also reported that black adolescent mothers were at higher risk to experience IPV.
During both pregnancy and the postpartum period and at the individual level, maternal stress due to unwanted pregnancy and feeling unsafe in one's neighborhood, lower education status, partner's substance use was associated with higher prevalence rates of bidirectional IPV. Also, IPV during pregnancy was a strong predictor of violence after childbirth, especially in constellations where both partners perpetrated violence against each other reciprocally (42). Hellmuth et al. (65) reported associated factors for reciprocal IPV, such as reported alcohol abuse in partners as well as stress and depression.
At the family level, family structure was strongly associated with interpersonal violence, i.e., women who were single or uninvolved with their previous partner at the time of their child's birth were four times more likely to have been involved in a violent relationship during pregnancy (42). Lower dyadic adjustment (i.e., a process with consequences that can be identified with the rate of a couple's problematic conflicts, interpersonal tensions, individual anxiety, marital satisfaction, coherence, integrity, and collaboration about important problems) (115) was found to be an associated factor (66).
At the societal level, Hispanic and other mothers in relation to white mothers were more likely to experience or perpetrate violence and abuse during pregnancy (42).
Our review aimed at examining prevalence estimates of IPV victimization and perpetration over the perinatal period. Moreover, we were interested in associated factors as well as the various forms of IPV during this period.
The narrative synthesis of relevant data revealed that most of the included studies reported on IPV during pregnancy with overall prevalence rates ranging from 1.5 to 66.9%. Less research concentrated on IPV during the postpartum period. Here, overall prevalence estimates ranged from 2 to 58%. The considerable variation of prevalence estimates found is indicative of considerable between-study variation. Hence, included studies were conducted in heterogeneous countries and investigated diverse populations with different cultural backgrounds and gender role distributions among women and men. Also, definitions of IPV, methods, and time of measurement differed markedly. Gazmararian et al. (113) already pointed out that such factors may affect prevalence estimates of IPV in pregnancy (116). Therefore, our results indicate that between-study variation could be of influence across the entire perinatal period.
Of special interest are studies reporting prevalence estimates during both pregnancy and the postpartum period. Here, the course of IPV over the perinatal period could be examined. Most of the included studies reported lower overall IPV prevalence rates postpartum compared to pregnancy. At first glance, this finding seems counterintuitive, as pregnancy clearly does not prevent the occurrence of intimate partner violence, regardless of its many negative health implications for women and their unborn child. Our findings add to the conflicting evidence of whether intimate partner violence increases or decreases during pregnancy (117). However, factors associated with IPV in this period ought to be considered when trying to explain this finding. In fact, a study found that prevalence estimates of IPV during pregnancy could be higher because expectant mothers may think staying with the violent partner is the safer option for their unborn child. Lost energy, low self-esteem, and hoping that the violence ends after the pregnancy constitute further possible reasons (54). Various forms of IPV were found including psychological, physical, sexual, and economic violence. Here, again prevalence rates, as well as types of IPV under investigation differed markedly across studies. Psychological violence was found to be the most prevalent form. This is consistent with previous research (7). The included studies focused primarily on psychological, physical, and sexual violence, while economic violence had been investigated by two studies only. This however could disregard the consequences of this type of violence and its relevant inclusion within the definition of IPV. As economic violence is often used as a controlling mechanism as part of a larger pattern of intimate partner violence (118). Despite the broad consensus that IPV, by definitions, includes all forms of sexual violence (119), an Iranian study (71) stated clearly the exclusion of questions on sexual violence and marital rape from their investigations due to cultural reasons (p. 8). This is an indication that sexual violence might be under researched in some contexts and prevalence rates could be even higher in reality (27).
Despite the clear research focus on unidirectional IPV, six of the included studies investigated bidirectional IPV among partners in pregnancy and/or postpartum. However, these data were solely based on women's reports. The results of these studies show the prevalence of IPV perpetration of women to be almost as high as or even higher than their victimization both during and after pregnancy. This is similar to the findings based on the two path-breaking national family violence surveys conducted by Straus & Gelles (119) which suggest gender symmetry of IPV, indicating that women are as likely to perpetrate violence as men. However, it is argued that women tend to overestimate their violence against their partners (120). This could be attributed to “their likelihood to remember their own aggression because it is deemed less appropriate and less acceptable for women than for men and thus takes on the more memorable quality of a forbidden act or one that is out of character” [(121): p. 405]. In addition to overestimating their own violence, women may also tend to underestimate their partner's violence given the norms of domestic life, which frequently find women discounting, downplaying, or normalizing their partner's violent behavior (120). Furthermore, these studies reported missing information regarding the context of the violence perpetrated by women. This could be due to the instrument used in most of the bidirectional studies (i.e., CTS-2), which has been assumed to be framing the occurrence of violence within the context of conflict resolution, which is of crucial importance in international settings where multiple populations are under examination at once (122). Most importantly, CTS-2 provides limited information about the context, initiation pattern, severity, intention, and motivation of abuse that many researchers consider central features of IPV (122). Research has consistently indicated that women's IPV perpetration is motivated mostly in self-, or in their children's defense, rather than driven by control and/or punishing motives (120, 123). Therefore, further enhanced research needs to be done to not only identify the occurrence, but also the context of the violence perpetrated by women during the perinatal period, in order to improve our understanding of the implications of this violence on their partners and their families.
Risk factors for IPV during the perinatal period may often be similar to risk factors for IPV in general. Still, given that pregnancy and the postpartum period are times that may demand increased relationship commitment and the resources needed, shedding more light on some risk factors are likely to be important here. Our narrative review revealed that most of the risk factors relating to unidirectional IPV were detected in studies focusing on IPV during pregnancy. Victim- and perpetrator-related factors at the individual level constituted both younger age and lower socioeconomic status, as well as having experienced or witnessed physical violence during childhood. This is found to be consistent with previous research (4, 7, 27). For the victimized pregnant women alone, early initiation of antenatal care (ANC) was found to be a protective factor for IPV. This could be attributed to the early detection and intervention of IPV, which possibly prevented further victimization (124). The same could be said for women who give birth in clinical settings vs. women who give birth at home, where their IPV victimization is found to decrease postpartum. Associated factors such as alcohol and drug use, insufficient utilization of prenatal care services, and reduced ability in decision-making as well as low self-esteem were also found to increase the risk of being victimized. However, previous research shows that such factors would rather be considered as consequences, where a multitude of pregnancy-specific health behaviors, as well as damaged self-image are common implications of IPV (125). Furthermore, a study reported that partners' sexual dissatisfaction could place mothers at higher risk for IPV postpartum. This could be attributed to the fact that the women are not as sexually available as their partners would like them to be, especially during this period. The patriarchal structure of some cultural contexts, which endorse the idea that a woman should be ready to satisfy her partner's sexual desires under any circumstances and at any cost could explain the higher risk for IPV victimization. This may suggest that the more patriarchal the societies the more such factors might play a role in the occurrence of IPV (27, 126). Family level related factors consisted of unplanned and undesired pregnancies, having multiple abortions, multigravidity, as well as having more (or fewer) than two children. As previous research pointed out, such factors could be considered as consequences of IPV, where some would be attributed to the partner's control over the woman's reproductive health or injury caused by assaultive episodes (27, 125, 127). Of relevant associated factors to IPV were the pressure on women to have a male child, which increased women's risk for victimization during pregnancy, as well as partners' disappointment with the child's gender (i.e., being female), which contributed to increased risk for victimization postpartum. These findings are consistent with previous evidence (27). Associated factors with bidirectional IPV were found to be similar to those regarding unidirectional IPV. Of special interest, women who perpetrated violence had partners with poorer dyadic adjustment, greater depression and stress levels, as well as greater severity of reported alcohol abuse compared to women who did not perpetrate IPV. Although causal attributions cannot be made here, further research is warranted to identify detrimental outcomes that are key indicators of mental, emotional, and physical health.
The studies included have traditionally identified individual characteristics and features of the social context that may be important for understanding violence against women. This scope of analysis often overlooks the power dynamic and impact of overlapping identities that are shaping the living realities of individuals and pushing them to the margins of society. An intersectional approach analyzes these identities, which could help enhance our understanding of how they coexist and shape individuals' lives in the community. Here, the findings reveal the interrelatedness of the factors mentioned thus far with the factors at the societal level like ethnicity (e.g., Jewish, African, or Hispanic women), having immigrant status, being HIV-positive, or having an HIV-positive child) indicate that the intersectionality lens is of essential importance in the context of our review. Instead of viewing characteristics such as age, socioeconomic status, class, gender, or race individually or as parts of an individual (128), an intersectional perspective views the influence of these characteristics as a process within a structural context of overlapping and interlocking identities. Such factors therefore appear not only to predispose pregnant women and mothers to IPV but it may worsen pre-existing violence. For example, as an immigrant woman, in addition to being confronted with gender inequalities, she is also faced with structural violence (i.e., injustices embedded in economic, political and cultural structures) of the host society (30). Consequently, IPV is a more complex problem for immigrant women and has serious consequences based on their social identities. As a person with a Jewish, African, or Hispanic racial identity, she faces racial discrimination (racism). As a woman, she faces sexism, which includes gender inequality, prejudice, stereotyping, or discrimination based on gender. Another form of discrimination would be social classism, which is discrimination based on a person's economic position in society that is determined mainly by income, educational attainment, financial security, and other criteria. Race is proven to influence social class standing. Likewise, gender and class are related because women continue to be underrepresented in high-level and highly paid positions but overrepresented in low-paying jobs (129, 130). Her multiple interlocked identities of race, gender, and class determine her lived experiences of violence. This implies that power relations intersect to produce specific vulnerabilities for specific groups in specific contexts. Moreover, new insights on the intersecting inequities resulting from different systems of domination (e.g., racism, sexism, classism), and varying forms of discrimination at community and societal levels (e.g., medical care, education, or employment) can help in highlighting the need for tailored prevention and intervention strategies for IPV (131).
Strengths of this review lie in the systematic search for relevant literature, the systematic process of data extraction, and its focus on prevalence estimates of IPV and its varying forms among partners, as well as their associated factors. Nonetheless, some limitations ought to be considered. Due to the narrative design of the review, no meta-analyses of the reported IPV prevalence estimates were conducted. Therefore, no pooled estimates were presented. Our hypothesis that the considerable variation of prevalence estimates found is attributable to between-study variation was not tested.
This work contributes to the literature by providing prevalence estimates of IPV among intimate partners as well as its associated factors during the perinatal period. Higher prevalence estimates were reported during pregnancy, with an overall IPV prevalence ranging from 1.5 to 66.9%, followed by an overall IPV prevalence of 2–58% during the postpartum period. Psychological violence was found to be the most prevalent form during the entire perinatal period compared to physical or sexual violence. Our results also highlighted the relationship between IPV and the varying associated factors, which relate to the different levels of the ecological model, suggesting a complex pattern of intersecting factors, which could put pregnant and/or postpartum women or partners at greater risk for IPV victimization. Studies regarding bidirectional perpetration of IPV during the perinatal period have been explored, yet their findings need to be interpreted with caution. Further research exploring not only the occurrence, but also the motivations and the contexts of the bidirectionality of IPV during the perinatal period may facilitate better understanding of the detrimental consequences on partners and their families, as well as better understanding of the detrimental consequences on partners and their families, as well as the development of effective intervention strategies. Public health prevention approaches intervening at optimal times during the perinatal period, are also needed. As a future outlook, as part of the recently started INVITE study (study on INtimate partner VIolence Treatment prEferences), our research group will generate a more comprehensive view of intervention preferences and barriers reported by postpartum women, who could be exposed to IPV and/or suffer from mental health problems.
AM, NA, MK, and SG-N designed and conceptualized the present study. AM and NA developed the search strategies. AM, NA, MK, AP, and FT conducted manuscript screening, data extraction, and wrote the first draft of the manuscript. SG-N supervised data extraction and drafting of the manuscript. AM, NA, MK, and SG-N contributed to the manuscript revision. All authors read and approved the submitted version.
No funding was provided for this work but SGN is a management committee member of COST action CA18211.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.601236/full#supplementary-material
1. World Health Organization. Understanding and Addressing Violence Against Women: Intimate Partner Violence. (2012). Available online at: https://apps.who.int/iris/bitstream/handle/10665/77432/WHO_RHR_12.36_eng.pdf (accessed August 10, 2020).
2. Van Gelder N, Peterman A, Potts A, O'Donnell M, Thompson K, Shah N, et al. COVID-19: reducing the risk of infection might increase the risk of intimate partner violence. EClinicalMedicine. (2020) 21:100348. doi: 10.1016/j.eclinm.2020.100348
3. Devries KM, Mak JYT, Garcia-Moreno C, Petzold M, Child JC, Falder G, et al. The global prevalence of intimate partner violence against women. Science. (2013) 340:1527–8. doi: 10.1126/science.1240937
4. García-Moreno C, Jansen AFMH, Watts C, Ellsberg M, Heise L. WHO Multi-Country Study on Women's Health and Domestic Violence Against Women. (2005). Available online at: http://dspace.ceid.org.tr/xmlui/bitstream/handle/1/93/ekutuphane4.1.6.4.pdf?sequence=1&isAllowed=y (accessed August 10, 2020).
5. Devries KM, Kishor S, Johnson H., Stöckl H, Bacchus LJ, Garcia-Moreno C, et al. Intimate partner violence during pregnancy: analysis of prevalence data from 19 countries. Reprod Health Matters. (2010) 18:158–70. doi: 10.1016/S0968-8080(10)36533-5
6. Campbell JC. Health consequences of intimate partner violence. Lancet. (2002) 359:1331–6. doi: 10.1016/S0140-6736(02)08336-8
7. Shamu S, Abrahams N, Temmerman M, Musekiwa A, Zarowsky C. A systematic review of African studies on intimate partner violence against pregnant women: prevalence and risk factors. PLoS ONE. (2011) 6:e17591. doi: 10.1371/journal.pone.0017591
8. World Health Organization. Preventing Intimate Partner and Sexual Violence Against Women: Taking Action and Generating Evidence. (2010). Available online at: https://apps.who.int/iris/bitstream/handle/10665/44350/9789275716359_por.pdf (accessed August 10, 2020).
9. Bonomi AE, Thompson RS, Anderson M, Reid RJ, Carrell D, Dimer JA., et al. Intimate partner violence and women's physical, mental, and social functioning. Am J Prev Med. (2006) 30:458–66. doi: 10.1016/j.amepre.2006.01.015
10. Heise L, Ellsberg M, Gottmoeller M. A global overview of gender-based violence. Int J Gynecol Obstet. (2002) 78:S5–14. doi: 10.1016/S0020-7292(02)00038-3
11. United Nations Office on Drugs and Crime. Global Study on Homicide: Gender-Related Killing of Women and Girls. (2018). Available online at: https://www.unodc.org/documents/data-and-analysis/GSH2018/GSH18_Gender-related_killing_of_women_and_girls.pdf (accessed August 10, 2020).
12. Rose L, Alhusen J, Bhandari S, Soeken K, Marcantonio K, Bullock L, et al. Impact of intimate partner violence on pregnant women's mental health: mental distress and mental strength. Issues Ment Health Nurs. (2010) 31:103–11. doi: 10.3109/01612840903254834
13. Plant DT, Pariante CM, Sharp D, Pawlby S. Maternal depression during pregnancy and offspring depression in adulthood: Role of child maltreatment. Br J Psychiatry Suppl. (2015) 207:213–20. doi: 10.1192/bjp.bp.114.156620
14. Klengel T, Dias BG, Ressler KJ. Models of intergenerational and transgenerational transmission of risk for psychopathology in mice. Neuropsychopharmacology. (2016) 41:219–31. doi: 10.1038/npp.2015.249
15. Yehuda R, Bell A, Bierer LM, Schmeidler J. Maternal, not paternal, PTSD is related to increased risk for PTSD in offspring of Holocaust survivors. J Psychiatr Res. (2008) 42:1104–11. doi: 10.1016/j.jpsychires.2008.01.002
16. Schury K, Koenig AM, Isele D, Hulbert AL, Krause S, Umlauft M, et al. Alterations of hair cortisol and dehydroepiandrosterone in mother-infant-dyads with maternal childhood maltreatment. BMC Psychiatry. (2017) 17:213. doi: 10.1186/s12888-017-1367-2
17. Campbell JC, Glass N, Sharps PW, Laughon K, Bloom T. Intimate partner homicide: review and implications of research and policy. Trauma Violence Abuse. (2007) 8:246–69. doi: 10.1177/1524838007303505
18. Palladino CL, Singh V, Campbell J, Flynn H, Gold K. Homicide and suicide during the perinatal period: findings from the National Violent Death Reporting System. Obstet Gynecol. (2011) 118:1056. doi: 10.1097/AOG.0b013e31823294da
19. Hines DA, Douglas EM. Alcohol and drug abuse in men who sustain intimate partner violence. Aggress Behav. (2012) 38:31–46. doi: 10.1002/ab.20418
20. Coker AL, Davis KE, Arias I, Desai S, Sanderson M, Brandt HM, et al. Physical and mental health effects of intimate partner violence for men and women. Am J Prev Med. (2002) 23:260–8. doi: 10.1016/s0749-3797(02)00514-7
21. Sullivan TP, Meese KM, Swan SC, Mazure CM, Snow DL. Precursors and correlates of women's violence: Child abuse traumatization, victimization of women, avoidance coping, and psychological symptoms. Psychol Women Q. (2005) 29:290–301. doi: 10.1111/j.1471-6402.2005.00223.x
22. Garthus-Niegel S, Ayers S, Martini J, Von Soest T, Eberhard-Gran M. The impact of postpartum post-traumatic stress disorder symptoms on child development: a population-based, 2-year follow-up study. Psychol Med. (2016) 47:161–70. doi: 10.1017/S003329171600235X
23. Schechter DS, Moser DA, Aue T, Gex-Fabry M, Pointet VC, Cordero MI, et al. Maternal PTSD and corresponding neural activity mediate effects of child exposure to violence on child PTSD symptoms. PLoS ONE. (2017) 12:e0181066. doi: 10.1371/journal.pone.0181066
24. Polte C, Junge C, von Soest T, Seidler A, Eberhard-Gran M, Garthus-Niegel S. Impact of maternal perinatal anxiety on social-emotional development of 2-year-olds, a prospective study of Norwegian mothers and their offspring. Matern Child Health J. (2019) 23:386–96. doi: 10.1007/s10995-018-2684-x
25. Junge C, Garthus-Niegel S, Slinning K, Polte C, Simonsen TB, Eberhard-Gran M. The impact of perinatal depression on children's social-emotional development: a longitudinal study. Matern Child Health J. (2017) 21:607–15. doi: 10.1007/s10995-016-2146-2
26. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. (2016) 5:210. doi: 10.1186/s13643-016-0384-4
27. Mojahed A, Alaidarous N, Shabta H, Hegewald J, Garthus-Niegel S. Intimate partner violence against women in the Arab countries: a systematic review of risk factors. Trauma Violence Abuse. (2020) doi: 10.1177/1524838020953099
28. Ahmad J, Khan ME, Mozumdar A, Varma DS. Gender-based violence in rural Uttar Pradesh, India: Prevalence and association with reproductive health behaviors. J Interpers Violence. (2016) 31:3111–28. doi: 10.1177/0886260515584341
29. Alhusen JL, Marguerite BL, Bullock L, Sharps P. Intimate partner violence, substance use, and adverse neonatal outcomes among urban women. J Pediatr. (2013) 136:471–6. doi: 10.1016/j.jpeds.2013.01.036
30. Almeida FSJ, Coutinho EC, Duarte JC, Chaves CMB, Nelas PAB, Amaral OP, et al. Domestic violence in pregnancy: prevalence and characteristics of the pregnant woman. J Clin Nurs. (2017) 26:2417–25. doi: 10.1111/jocn.13756
31. Amiri M, Mohammad-Alizadeh-Charandabi S, Mirghafourvand M, Farshbaf-Khalili A, Ranjbar F. Intimate partner violence during the first year after childbirth in an urban area of Iran: prevalence and its predictors. Int J Womens Health Reprod Sci. (2018) 6:491–8. doi: 10.15296/ijwhr.2018.81
32. Arslantaş H, Adana F, Ergin F, Gey N, Biçer N, Kiranşal N. Domestic violence during pregnancy in an Eastern City of Turkey: a field study. J Interpers Violence. (2012) 27:1293–313. doi: 10.1177/0886260511425248
33. Ashimi AO, Amole TG. Prevalence and predictors for domestic violence among pregnant women in a rural community Northwest, Nigeria. Niger Med J. (2015) 56:118. doi: 10.4103/0300-1652.150696
34. Azene ZN, Yeshita HY, Mekonnen FA. Intimate partner violence and associated factors among pregnant women attending antenatal care service in Debre Markos town health facilities, Northwest Ethiopia. PLoS ONE. (2019) 14:e0218722. doi: 10.1371/journal.pone.0218722
35. Babua BV, Kar SK. Abuse against women in pregnancy: a population-based study from Eastern India. WHO South East Asia J Public Health. (2012) 1:133–43. doi: 10.4103/2224-3151.206926
36. Bahrami-Vazir E, Mohammad-Alizadeh-Charandabi S, Ghelichkhani F, Mohammadi A, Mirghafourvand M. Intimate partner abuse among couples during pregnancy and its predictors as reported by pregnant women visiting governmental health care centres in Tabriz, Iran. J Biosoc Sci. (2020) 52:400–11. doi: 10.1017/S002193201900052X
37. Bernstein M, Phillips T, Zerbe A, McIntyre JA, Brittain K, Petro G, et al. Intimate partner violence experienced by HIV-infected pregnant women in South Africa: a cross-sectional study. BMJ Open. (2016) 6:e011999. doi: 10.1136/bmjopen-2016-011999
38. Bhatta N, Assanangkornchai S. Patterns of domestic violence against women during pregnancy and the postpartum period in Kathmandu, Nepal. Asia Pac Psychiatry. (2019) 11:e12342. doi: 10.1111/appy.12342
39. Carneiro JF, Valongueiro S, Ludermir AB, Araújo TVB. Physical violence by an intimate partner and the inappropriate use of prenatal care services among women in Northeastern Brazil. Rev Bras Epidemiol. (2016) 19:243–55. doi: 10.1590/1980-5497201600020003
40. Cervantes-Sánchez P, Delgado-Quiñones EG, Nuño-Donlucas MO, Sahagún-Cuevas MN, Hernández-Calderón J, Ramírez-Ramos JK. Prevalence of domestic violence in pregnant women from 20 to 35 years in a family medicine unit. Rev Méd Inst Mex Seguro Soc. (2016) 54:286–91. Available online at: https://www.medigraphic.com/pdfs/imss/im-2016/im163d.pdf (accessed August 10, 2020).
41. Charles P, Perreira KM. Intimate partner violence during pregnancy and 1-year post-partum. J Fam Violence. (2007) 22:609–19. doi: 10.1007/s10896-007-9112-0
42. Clark CJ, Hill A, Jabbar K, Silverman JG. Violence during pregnancy in Jordan: its prevalence and associated risk and protective factors. Violence Against Women. (2009) 15:720–35. doi: 10.1177/1077801209332191
43. Clarke S, Richmond R, Black E, Fry H, Obol JH, Worth H. Intimate partner violence in pregnancy: a cross-sectional study from post-conflict northern Uganda. BMJ Open. (2019) 9:e027541. doi: 10.1136/bmjopen-2018-027541
44. Das S, Bapat U, More NS, Alcock G, Joshi W, Pantvaidya S, et al. Intimate partner violence against women during and after pregnancy: a cross-sectional study in Mumbai slums. BMC Public Health. (2013) 13:817. doi: 10.1186/1471-2458-13-817
45. Moraes CL, Reichenheim ME, Gama SGN, Leal MC. Prevalence of physical intimate partner violence in the first six months after childbirth in the city of Rio de Janeiro, Brazil. Cad Saúde Pública. (2017) 33:e00141116. doi: 10.1590/0102-311x00141116
46. Epuitai J, Udho S, Auma AG, Nabirye RC. Intimate partner violence among pregnant women in Uganda. Afr J Midwifery Womens Health. (2019) 13:1–5. doi: 10.12968/AJMW.2018.0027
47. Ezeanochie MC, Olagbuji BN, Ande AB, Kubeyinje WE, Okonofua FE. Prevalence and correlates of intimate partner violence against HIV-seropositive pregnant women in a Nigerian population. Acta Obstet Gynecol Scand. (2011) 90:535–9. doi: 10.1111/j.1600-0412.2011.01083.x
48. Ezechi OC, Gab-Okafor C, Onwujekwe DI, Adu RA, Amadi E, Herbertson E. Intimate partner violence and correlates in pregnant HIV positive Nigerians. Arch Gynecol Obstet. (2009) 280:745–52. doi: 10.1007/s00404-009-0956-9
49. Farrokh-Eslamlou H, Oshnouei S, Haghighi N. Intimate partner violence during pregnancy in Urmia, Iran in 2012. J Forensic Leg Med. (2014) 24:28–32. doi: 10.1016/j.jflm.2014.03.007
50. Fawole OI, Abass LWA, Fawole AO. Prevalence of violence against pregnant women in Ibadan, Nigeria. Afr J Med Med Sci. (2010) 39:293. Available online at: https://www.researchgate.net/profile/Olufunmilayo_Fawole/publication/51473810_Prevalence_of_violence_against_pregnant_women_in_Ibadan_Nigeria/links/587a569108ae4445c0630535/Prevalence-of-violence-against-pregnant-women-in-Ibadan-Nigeria.pdf (accessed August 10, 2020).
51. Fekadu E, Yigzaw G, Gelaye KA, Ayele TA, Minwuye T, Geneta T, et al. Prevalence of domestic violence and associated factors among pregnant women attending antenatal care service at University of Gondar Referral Hospital, Northwest Ethiopia. BMC Womens Health. (2018) 18:138. doi: 10.1186/s12905-018-0632-y
52. Field S, Onah M, van Heyningen T, Honikman S. Domestic and intimate partner violence among pregnant women in a low resource setting in South Africa: a facility-based, mixed methods study. BMC Womens Health. (2018) 18:119. doi: 10.1186/s12905-018-0612-2
53. Finnbogadóttir H, Dykes AK, Wann-Hansson C. Prevalence of domestic violence during pregnancy and related risk factors: a cross-sectional study in southern Sweden. BMC Womens Health. (2014) 14:63. doi: 10.1186/1472-6874-14-63
54. Finnbogadóttir H, Dykes AK, Wann-Hansson C. Prevalence and incidence of domestic violence during pregnancy and associated risk factors: a longitudinal cohort study in the south of Sweden. BMC Pregnancy Childbirth. (2016) 16:228. doi: 10.1186/s12884-016-1017-6
55. Fiorotti KF, Amorim MHC, Lima EFA, Primo CC, Moura MAV, Leite FMC. Prevalence and factors associated with domestic violence: study in a high-risk maternity hospital. Texto Contexto Enfermagem. (2018) 27:e0810017. doi: 10.1590/0104-07072018000810017
56. Fisher M, Yassour-Borochowitz D, Neter E. Domestic abuse in pregnancy: results from a phone survey in northern Israel. IMAJ RAMAT GAN. (2003) 5:35–9. Available online at: https://www.researchgate.net/profile/Menachem_Fisher/publication/10894738_Domestic_abuse_in_pregnancy_Results_from_a_phone_survey_in_Northern_Israel/links/0fcfd509179e957cb7000000.pdf (accessed August 10, 2020).
57. Flanagan JC., Véronique J, Gordon KC, Moore TM, Stuart GL. Examining the prevalence, bidirectionality, and co-occurrence of sexual intimate partner violence among women during pregnancy and postpartum. Partner Abuse. (2014) 5:407–19. doi: 10.1891/1946-6560.5.4.407
58. Garg S, Singh MM, Rustagi R, Engtipi K, Bala I. Magnitude of domestic violence and its socio-demographic correlates among pregnant women in Delhi. J Family Med Prim Care. (2019) 8:3634–9. doi: 10.4103/jfmpc.jfmpc_597_19
59. Gartland D, Hemphill SA, Hegarty K, Brown SJ. Intimate partner violence during pregnancy and the first year postpartum in an Australian pregnancy cohort study. Matern Child Health J. (2011) 15:570–8. doi: 10.1007/s10995-010-0638-z
60. Groves AK, Moodley D, McNaughton-Reyes L, Martin SL, Foshee V, Maman S. Prevalence, rates and correlates of intimate partner violence among South African women during pregnancy and the postpartum period. Matern Child Health J. (2015) 19:487–95. doi: 10.1007/s10995-014-1528-6
61. Gyuse AN, Ushie AP, Etukidem A. Prevalence of domestic violence among antenatal women attending a Nigerian hospital. Niger J Med. (2009) 18:375–9. doi: 10.4314/njm.v18i4.51246
62. Habib S, Abbasi N, Khan B, Danish N, Nazir Q. Domestic violence among pregnant women. J Ayub Med Coll Abbottabad. (2018) 30:237–40. Available online at: https://pesquisa.bvsalud.org/portal/resource/%20es/mdl-29938426 (accessed August 10, 2020).
63. Haron K, Shaffie Z, Ghazi HF, Isa ZM. Women's attitude and its influence on violence during pregnancy in northern state of Peninsular Malaysia: cross-sectional study. J Interpers Violence. (2018). doi: 10.1177/0886260518759059
64. Harrykissoon SD, Rickert VI, Wiemann CM. Prevalence and patterns of intimate partner violence among adolescent mothers during the postpartum period. Arch Pediatr Adolesc Med. (2002) 156:325–30. doi: 10.1001/archpedi.156.4.325
65. Hellmuth JC, Gordon KP, Stuart GL, Moore TM. Women's intimate partner violence perpetration during pregnancy and postpartum. Matern Child Health J. (2013) 17:1405–13. doi: 10.1007/s10995-012-1141-5
66. Islam MJ, Broidy L, Mazerolle P, Baird K, Mazumder N. Exploring intimate partner violence before, during, and after pregnancy in Bangladesh. J Interpers Violence. (2018). doi: 10.1177/0886260518775753
67. Islam MJ, Broidy L, Baird K, Mazerolle P. Exploring the associations between intimate partner violence victimization during pregnancy and delayed entry into prenatal care: evidence from a population-based study in Bangladesh. Midwifery. (2017) 47:43–52. doi: 10.1016/j.midw.2017.02.002
68. Jahanfar S, Malekzadegan Z. The prevalence of domestic violence among pregnant women who were attended in Iran University of Medical Science Hospitals. J Fam Violence. (2007) 22:643. doi: 10.1007/s10896-007-9084-0
69. Jain S, Varshney K, Vaid NB, Guleria K, Vaid K, Sharma N. A hospital-based study of intimate partner violence during pregnancy. Int J Gynecol Obstet. (2017) 137:8–13. doi: 10.1002/ijgo.12086
70. Jamshidimanesh M, Soleymani M, Ebrahimi E, Hosseini F. Domestic violence against pregnant women in Iran. J Fam Reprod Health. (2013) 7:7–10. Available online at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4064743/pdf/JFRH-7-007.pdf (accessed August 10, 2020).
71. Jeremiah IGBK, Oriji VK. Domestic violence in pregnancy among antenatal attendees at the University of Port Harcourt Teaching Hospital, Port Harcourt. Niger J Med. (2011) 3: 355-59. Available online at: https://www.researchgate.net/profile/Israel_Jeremiah/publication/51692762_Domestic_violence_in_pregnancy_among_antenatal_attendees_at_the_University_of_Port_Harcourt_Teaching_Hospital_Port_Harcourt/links/5dbd84bc92851c8180258ab9/Domestic-violence-in-pregnancy-among-antenatal-attendees-at-the-University-of-Port-Harcourt-Teaching-Hospital-Port-Harcourt.pdf (accessed August 10, 2020).
72. Johnson JK, Haider F, Ellis K, Hay DM, Lindow SW. The prevalence of domestic violence in pregnant women. BJOG. (2003) 110:272–5. doi: 10.1046/j.1471-0528.2003.02216.x
73. Karaoglu L, Celbis O, Ercan C, Ilgar M, Pehlivan E, Gunes G, et al. Physical, emotional and sexual violence during pregnancy in Malatya, Turkey. Eur J Public Health. (2006) 16:149–56. doi: 10.1093/eurpub/cki161
74. Karmaliani R, Irfan F, Bann CM, Mcclure EM, Moss N, Pasha O, et al. Domestic violence prior to and during pregnancy among Pakistani women. Acta Obstet Gynecol Scand. (2008) 87:1194–201. doi: 10.1080/00016340802460263
75. Kaye D, Mirembe F, Bantebya G. Risk factors, nature and severity of domestic violence among women attending antenatal clinic in Mulago Hospital, Kampala, Uganda. Cent Afr J Med. (2002) 48:64–8.
76. Khaironisak H, Zaridah S, Hasanain FG, Zaleha MI. Prevalence, risk factors, and complications of violence against pregnant women in a hospital in Peninsular Malaysia. Women Health. (2017) 57:919–41. doi: 10.1080/03630242.2016.1222329
77. Kita S, Yaeko K, Porter SE. Prevalence and risk factors of intimate partner violence among pregnant women in Japan. Health Care Women Int. (2014) 35:442–57. doi: 10.1080/07399332.2013.857320
78. Koenig LJ, Whitaker DJ, Royce RA, Wilson TE, Callahan MR, Fernandez MI. Violence during pregnancy among women with or at risk for HIV infection. Am J Public Health. (2002) 92:367–70. doi: 10.2105/AJPH.92.3.367
79. Kothari R, Easter A, Lewis R, Howard LM, Micali N. Intimate partner violence among women with eating disorders during the perinatal period. Int J Eat Disord. (2015) 48:727–35. doi: 10.1002/eat.22429
80. Lukasse M, Schroll AM, Ryding EL, Campbell J, Karro H, Kristjansdottir H, et al. Prevalence of emotional, physical and sexual abuse among pregnant women in six European countries. Acta Obstet Gynecol Scand. (2014) 93:669–77. doi: 10.1111/aogs.12392
81. Lutgendorf MA, Busch JM, Doherty DA, Conza LA, Moone SO, Magann EF. Prevalence of domestic violence in a pregnant military population. Obstet Gynecol. (2009) 113:866–72. doi: 10.1097/AOG.0b013e31819bdc93
82. Mahenge B, Stöckl H, Abubakari A, Mbwambo J, Jahn A. Physical, sexual, emotional and economic intimate partner violence and controlling behaviors during pregnancy and postpartum among women in Dar es Salaam, Tanzania. PLoS ONE. (2016) 11:e0164376. doi: 10.1371/journal.pone.0164376
83. Makayoto LA, Omolo J, Kamweya AM, Harder VS, Mutai J. Prevalence and associated factors of intimate partner violence among pregnant women attending Kisumu District Hospital, Kenya. Matern Child Health J. (2013) 17:441–7. doi: 10.1007/s10995-012-1015-x
84. Malan M, Spedding MF, Sorsdahl K. The prevalence and predictors of intimate partner violence among pregnant women attending a midwife and obstetrics unit in the Western Cape. Glob Ment Health. (2018) 5:e18. doi: 10.1017/gmh.2018.9
85. Marcacine KO, Abuchaim ESV, Abrahão AR, Michelone CSL, Abrão ACFV. Prevalence of intimate partner violence reported by puerperal women. Acta Paul Enferm. (2013) 26:395–400. doi: 10.1590/S0103-21002013000400015
86. Massumi Okada M, Hoga LAK, Borges ALV, Albuquerque RS, Belli MA. Domestic violence against pregnant women. Acta Paulista de Enfermagem. (2015) 28:270–4. doi: 10.1590/1982-0194201500045
87. Modiba LM, Baliki O, Mmalasa R, Reineke P, Nsiki C. Pilot survey of domestic abuse amongst pregnant women attending an antenatal clinic in a public hospital in Gauteng Province in South Africa. Midwifery. (2011) 27:872–9. doi: 10.1016/j.midw.2010.09.008
88. Mohammad-Alizadeh-Charandabi S, Bahrami-Vazir E, Kamalifard M, Mirghafourvand M. Intimate partner violence during the first pregnancy: a comparison between adolescents and adults in an urban area of Iran. J Forensic Leg Med. (2016) 43:53–60. doi: 10.1016/j.jflm.2016.07.002
89. Mohammadhosseini E, Sahraean L, Bahrami T. Domestic abuse before, during and after pregnancy in Jahrom, Islamic Republic of Iran. East Mediterr Health J. (2010) 16:752–8. doi: 10.26719/2010.16.7.752
90. Muzrif MM, Perera D, Wijewardena K, Schei B, Swahnberg K. Domestic violence: a cross-sectional study among pregnant women in different regions of Sri Lanka. BMJ Open. (2018) 8:e017745. doi: 10.1136/bmjopen-2017-017745
91. Nguyen TH, Ngo TV, Nguyen VD, Nguyen HD, Nguyen HTT, Gammeltoft T, et al. Intimate partner violence during pregnancy in Vietnam: prevalence, risk factors and the role of social support. Glob Health Action. (2018) 11:69–76. doi: 10.1080/16549716.2019.1638052
92. Okour AM, Badarneh R. Spousal violence against pregnant women from a Bedouin community in Jordan. J Womens Health. (2011) 20:1853–9. doi: 10.1089/jwh.2010.2588
93. Olagbuji B, Ezeanochie M, Ande A, Ekaete E. Trends and determinants of pregnancy-related domestic violence in a referral center in southern Nigeria. Int J Gynecol Obstet. (2010) 108:101–3. doi: 10.1016/j.ijgo.2009.09.024
94. Onoh RC, Umeora OUJ, Ezeonu PO, Onyebuchi AK, Lawani OL, Agwu UM. Prevalence, pattern and consequences of intimate partner violence during pregnancy at Abakaliki Southeast Nigeria. Ann Med Health Sci Res. (2013) 3:484–91. doi: 10.4103/2141-9248.122048
95. Owaka IO, Nyanchoka MK, Atieli HE. Intimate partner violence in pregnancy among antenatal attendees at health facilities in West Pokot county, Kenya. Pan Afr Med J. (2017) 28:229. doi: 10.11604/pamj.2017.28.229.8840
96. Oweis A, Gharaibeh M, Alhourani R. Prevalence of violence during pregnancy: findings from a Jordanian survey. Matern Child Health J. (2010) 14:437–45. doi: 10.1007/s10995-009-0465-2
97. Peedicayil A, Sadowski LS, Jeyaseelan L, Shankar V, Jain D, Suresh S, et al. Spousal physical violence against women during pregnancy. BJOG. (2004) 111:682–7. doi: 10.1111/j.1471-0528.2004.00151.x
98. Pitter CP, Dunn L. Profiling pregnant women at risk for domestic violence in Jamaica: a pilot study. Int J Childbirth. (2018) 7:170–80. doi: 10.1891/2156-5287.7.4.170
99. Romero-Gutiérrez G, Cruz-Arvizu VH, Regalado-Cedillo CA, León ALPP. Prevalence of violence against pregnant women and associated maternal and neonatal complications in Leon, Mexico. Midwifery. (2011) 27:750–3. doi: 10.1016/j.midw.2010.06.015
100. Rubertsson C, Hildingsson I, Rådestad I. Disclosure and police reporting of intimate partner violence postpartum: a pilot study. Midwifery. (2010) 26:e1–5. doi: 10.1016/j.midw.2008.01.003
101. Salari Z, Nakhaee N. Identifying types of domestic violence and its associated risk factors in a pregnant population in Kerman hospitals, Iran Republic. Asia Pac J Public Health. (2008) 20:49–55. doi: 10.1177/1010539507308386
102. Shamu S, Abrahams N, Zarowsky C, Shefer T, Temmerman M. Intimate partner violence during pregnancy in Zimbabwe: A cross-sectional study of prevalence, predictors and associations with HIV. Trop Med Int Health. (2013) 18:696–711. doi: 10.1111/tmi.12078
103. Shrestha SD, Pradhan R, Tran TD, Gualano RC, Fisher JRW. Reliability and validity of the Edinburgh Postnatal Depression Scale (EPDS) for detecting perinatal common mental disorders (PCMDs) among women in low-and lower-middle-income countries: a systematic review. BMC Pregnancy Childbirth. (2016) 16:72. doi: 10.1186/s12884-016-0859-2
104. Silverman JG, Balaiah D, Decker MR, Boyce SC, Ritter J, Naik DD, et al. Family violence and maltreatment of women during the perinatal period: associations with infant morbidity in Indian slum communities. Matern Child Health J. (2016) 20:149–57. doi: 10.1007/s10995-015-1814-y
105. Sohail S, Qadir E. The frequency of domestic violence in pregnancy and its demographic characteristics. Med Forum Mon. (2009) 20:25–8. Available online at: https://www.researchgate.net/publication/289162266_The_frequency_of_domestic_violence_in_pregnancy_and_its_demographic_characteristics (accessed August 10, 2020).
106. Spangenberg K, Wobil P, Betts CL, Wiesner TF, Gold KJ. Intimate partner violence among mothers of sick newborns in Ghana. Health Care Women Int. (2016) 37:583–94. doi: 10.1080/07399332.2015.1037444
107. Stöckl H, Watts C, Mbwambo JKK. Physical violence by a partner during pregnancy in Tanzania: prevalence and risk factors. Reprod Health Matters. (2010) 18:171–80. doi: 10.1016/S0968-8080(10)36525-6
108. Umoh AV, Abah GM, Ugege WE, Inyangetoh EC. Prevalence and attitude of women to spousal physical abuse in pregnancy in a Niger delta community of Nigeria. TAF Prev Med Bull. (2012) 11:731–6. doi: 10.5455/pmb.1-1329127812
109. Valladares E, Pena R, Persson LA, Högberg U. Violence against pregnant women: prevalence and characteristics. A population-based study in Nicaragua. BJOG. (2005) 112:1243–8. doi: 10.1111/j.1471-0528.2005.00621.x
110. Van Parys AS, Deschepper E, Michielsen K, Temmerman M, Verstraelen H. Prevalence and evolution of intimate partner violence before and during pregnancy: a cross-sectional study. BMC Pregnancy Childbirth. (2014) 14:294. doi: 10.1186/1471-2393-14-294
111. Yang M-S, Yang M-J, Chou F-H, Yang H-M, Wei S-L, Lin J-R. Physical abuse against pregnant aborigines in Taiwan: prevalence and risk factors. Int J Nurs Stud. (2006) 34:21–7. doi: 10.1016/j.ijnurstu.2004.12.005
112. Yohannes K, Abebe L, Kisi T, Demeke W, Yimer S, Feyiso M, et al. The prevalence and predictors of domestic violence among pregnant women in Southeast Oromia, Ethiopia. Reprod Health. (2019) 16:37. doi: 10.1186/s12978-019-0694-9
113. Gazmararian JA, Lazorick S, Spitz AM, Ballard TJ, Saltzman LE, Marks S. Prevalence of violence against pregnant women. JAMA. (1996) 275:1915–20. doi: 10.1001/jama.275.24.1915
114. Audi CAF, Segall-Corrêa AM, Santiago SM, Andrade MGG, Pèrez-Escamila R. Violence against pregnant women: prevalence and associated factors. Revista de saude publica. (2008) 42:877–85. doi: 10.1590/S0034-89102008005000041
115. Ghaffari M. Spiritual well-being and dyadic adjustment: Mediator effects for family strengths. Iran J Psychiatry Behav Sci. (2016) 10:e1699. doi: 10.17795/ijpbs-1699
116. Jasinski JL. Pregnancy and domestic violence: a review of the literature. Trauma Violence Abuse. (2004) 5:47–64. doi: 10.1177/1524838003259322
117. Stylianou AM. Economic abuse within intimate partner violence: a review of the literature. Violence Vict. (2018) 33:3–22. doi: 10.1891/0886-6708.VV-D-16-00112
118. Ruiz-Pérez I, Plazaola-Castaño J, Vives-Cases C. Methodological issues in the study of violence against women. J Epidemiol Community Health. (2007) 61:ii26–31. doi: 10.1136/jech.2007.059907
119. Straus MA, Gelles RJ, Smith C. Physical Violence in American Families: Risk Factors and Adaptations to Violence in 8,145 Families. 1st ed. New York: Routledge (1990). doi: 10.1891/0886-6708.5.4.297
120. Kimmel MS. “Gender symmetry” in domestic violence: a substantive and methodological research review. Violence Against Women. (2002) 8:1332–63. doi: 10.1177/107780102237407
121. Dobash RP, Dobash RE, Wilson M, Daly M. The myth of sexual symmetry in marital violence. Soc Probl. (1992) 39:71–91. doi: 10.1525/sp.1992.39.1.03x0064l
122. Ellsberg M, Heise L, World Health Organization. Researching Violence Against Women: A Practical Guide for Researchers and Activists. (2005). Available online at: http://dspace.ceid.org.tr/xmlui/bitstream/handle/1/941/9241546476_eng.pdf?sequence=1&isAllowed=y (accessed August 12, 2020).
123. Swan SC, Gambone LG, Caldwell JE, Sullivan TP, Snow DL. A review of research on women's use of violence with male intimate partners. Violence Vict. (2008) 23:301–14. doi: 10.1891/0886-6708.23.3.301
124. Jewkes R, Levin J, Penn-Kekana L. Risk factors for domestic violence: findings from a South African cross-sectional study. Soc Sci Med. (2002) 55:1603–17. doi: 10.1016/S0277-9536(01)00294-5
125. Alhusen JL, Ray L, Sharps P, Bullock L. Intimate partner violence during pregnancy: maternal and neonatal outcomes. J Womens Health. (2015) 24:100–6. doi: 10.1089/jwh.2014.4872
126. Naghavi A, Amani S, Bagheri M, De Mol J. A critical analysis of intimate partner sexual violence in Iran. Front Psychol. (2019) 10:2729. doi: 10.3389/fpsyg.2019.02729
127. Ellsberg M, Peña R, Herrera A, Liljestrand J, Winkvist A. Candies in hell: women's experiences of violence in Nicaragua. Soc Sci Med. (2000) 51:1595–610. doi: 10.1016/S0277-9536(00)00056-3
128. Collins PH. Black Feminist Thought: Knowledge, Consciousness, and the Politics of Empowerment. 2nd ed. New York: Routledge (2002). Available online at: https://homologacao-reciis.icict.fiocruz.br/index.php/reciis/article/download/854/1496 (accessed August 12, 2020).
129. Reeves RV. Hoarding the dream, still. In: Dream Hoarders. Washington: Brookings Institution (2018). Available online at: https://www.brookings.edu/wp-content/uploads/2018/03/9780815734482_ch1.pdf (accessed August 12, 2020).
130. Sowell RL, Seals BF, Phillips KD, Julious CH. Disclosure of HIV infection: how do women decide to tell? Health Educ Res. (2003) 18:32–44. doi: 10.1093/her/18.1.32
Keywords: intimate partner violence, bidirectional IPV, perinatal period, prevalence, associated factors, narrative review
Citation: Mojahed A, Alaidarous N, Kopp M, Pogarell A, Thiel F and Garthus-Niegel S (2021) Prevalence of Intimate Partner Violence Among Intimate Partners During the Perinatal Period: A Narrative Literature Review. Front. Psychiatry 12:601236. doi: 10.3389/fpsyt.2021.601236
Received: 06 October 2020; Accepted: 12 January 2021;
Published: 09 February 2021.
Edited by:
Xavier Noel, Université libre de Bruxelles, BelgiumReviewed by:
Georgios Demetrios Kotzalidis, Sapienza University of Rome, ItalyCopyright © 2021 Mojahed, Alaidarous, Kopp, Pogarell, Thiel and Garthus-Niegel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Amera Mojahed, YW1lcmEubW9qYWhlZEB1bmlrbGluaWt1bS1kcmVzZGVuLmRl
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.