
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 15 April 2021
Sec. Mood Disorders
Volume 12 - 2021 | https://doi.org/10.3389/fpsyt.2021.585537
This article is part of the Research Topic Impact of the Coronavirus Pandemic (COVID-19) on Mood Disorders and Suicide View all 41 articles
 Wentao Chen1,2†
Wentao Chen1,2† Yumeng Ju1,2†
Yumeng Ju1,2† Bangshan Liu1,2
Bangshan Liu1,2 Mei Huang1,2
Mei Huang1,2 Aiping Yang3
Aiping Yang3 Yun Zhou4
Yun Zhou4 Mi Wang1,2
Mi Wang1,2 Mei Liao1,2
Mei Liao1,2 Kongliang Shu5*
Kongliang Shu5* Jiyang Liu6*
Jiyang Liu6* Yan Zhang1,2*
Yan Zhang1,2*Objective: Little is known about the factors affecting the recovery of mental health in COVID-19 patients. The purpose of this study is to look into the change of psychological distress and to explore the role of negative appraisals in the improvement of psychological distress in COVID-19 patients after they recovered from the infection.
Methods: We conducted a longitudinal survey on patients with COVID-19 infection in Changsha. The 9-item Patient Health scale, the 7-item Generalized Anxiety Disorder scale, and a newly developed measure, the COVID-19 Impact Scale (CIS) were applied to assess patients' depression, anxiety, and negative appraisal toward COVID-19 infection during their hospitalization and 1 month post-discharge.
Results: Seventy-two patients were included in the analysis. A significant decrease in anxiety and depression levels was observed after patients were discharged from hospital. Two meaningful factors of the CIS were extracted based on factor analysis, namely “health impact,” and “social impact.” The change of social impact explained the 12.7 and 10.5% variance in the depression and anxiety symptom improvement, respectively.
Conclusions: Change in negative appraisals, especially the appraisals related to COVID-19 social impact may play a vital role in the relief of psychological distress of infected patients. Therefore, a cognitive and social care perspective might be considered when promoting the mental health recovery and readjustment to society among COVID-19 patients.
Since the end of 2019, coronavirus disease 2019 (COVID-19) has emerged from China and spread rapidly to other countries. As of February 2021, the virus has been transmitted to 213 countries, had more than 100 million confirmed cases, and a death toll of 2.2 million has been reached (1). The highly contagious disease has had significant negative impacts on people's health, both physically and mentally.
Previous studies on viral infectious diseases, such as Severe Acute Respiratory Syndrome (SARS) and Ebola virus disease (EVD), have shown that emerging infectious disease can cause serious psychological distress (i.e., depression and anxiety) in patients during the acute phase of the disease (2–4). Studies also showed that the infection may have long-term effects on the mental health of the survivors (5–7). One study pointed out that 1 year after the outbreak of SARS, a large portion of survivors were still at a high level of stress, with more than 64% of patients developing mental disorders (8). One study investigated neurological and neuropsychiatric complications in patients with COVID-19 and found that 23 of 123 patients showed altered mental health status that fulfilled psychiatric diagnosis (9). Another qualitative study provided evidence that patients with COVID-19 experienced mental distress including anxiety and fear during the early stages of the disease (10). Moreover, a rapid review indicated that COVID-19 infection adversely affects the mental health status in patients (11). These findings suggest that we need to pay attention not only to the physical recovery of the infected patients, but also to the mental recovery of patients in the current COVID-19 epidemic.
Several factors were suggested to play an important role in the mental health status of the infected patients, including the disease condition (12) or being isolated or quarantined during hospitalization (13). However, these short-term influencing factors do not sufficiently explain the continued mental distress in patients after they have recovered from the infection. There are other factors that influence the long-term mental health condition of patients.
Negative appraisals were found to play an important role in the course of mental distress and its prognosis (14–17). A study of collegiate students in China showed that COVID-19-related negative appraisals was positively correlated with their emotional distress (18). A previous SARS study on medical staff reported a high level of post-traumatic symptoms among those who had perceived discrimination or felt rejected (19). In addition, another SARS study revealed a significant correlation between negative appraisals of the disease and symptoms of depression and anxiety (20). These lead us to the hypothesis that negative appraisals of the COVID-19 infection may exert influence on the mental recovery of patients.
In light of the above, we conducted a longitudinal study involving patients with COVID-19 in Changsha. The purpose of this study is as follows: first, to track the change in depression and anxiety levels in patients before and after they have recovered from the COVID-19 infection. Second, to explore the role of negative appraisals in depression and anxiety symptom improvement in patients after COVID-19 recovery.
This study was approved by the ethics review boards of The First Hospital of Changsha. The target population comprised all the COVID-19 patients admitted to The First Hospital of Changsha (Changsha, Hunan, China), which is the only designated hospital in Changsha city to receive patients with COVID-19 for treatment.
We conducted a longitudinal questionnaire survey on all hospitalized patients with COVID-19 from February to April 2020. COVID-19 was diagnosed according to the diagnosis and treatment plan for COVID-2019 released by the National Health Commission (21). Patients who consented to participate and were able to complete the online survey were included in the study. Patients who were below the age of 18, were unable to provide informed consent for any reason, or could not use mobile devices to complete all the questionnaires on their own were excluded from the study.
A baseline survey was conducted during patients' hospitalization. The nurse in the isolation ward informed the eligible patients that the online survey was set up to investigate the prevalence and related factors of mental distress in the COVID-19 pandemic. After acquiring the verbal consent of the participants, the nurse provided the patients with the website to fill out the questionnaire. The patients signed the electronic informed consent on the homepage of the website before the survey. At the end of the questionnaire, participants were asked about their needs for mental health services.
A follow-up survey was conducted 1 month after the patients were discharged from the hospital. The researchers contacted the patients by phone to learn about their current physical and mental health status. After obtaining verbal consent, the researchers sent patients a website link of the follow-up survey. Participants were asked to sign the electronic informed consent before they completed the questionnaire. Furthermore, mental health services were provided according to their self-reported mental health service needs after the follow-up survey, and patients who met the cut-off points (10 points) for PHQ-9 or GAD-7 were suggested for further individual evaluation and psychological counseling.
The patients who agreed to participate in the study were asked to fill out a questionnaire recording their demographic information, clinical characteristics, and psychological variables. The demographics included age, gender, marital status, and years of education. The clinical characteristics comprised past medical history, duration of hospitalization, and the severity of COVID-19. The Chinese version of the 9-item Patient Health Questionnaire (PHQ-9; range, 0–27) and the 7-item Generalized Anxiety Disorder scale (GAD-7; range, 0–21) were used to assess the severity of the patients' depression and anxiety symptoms. The Chinese version of PHQ-9 and GAD-7 showed good reliability and validity in general hospital inpatients (22, 23). The COVID-19 disease-related questionnaire was used to reflect the degree of the patients' negative attitudes toward the infection. This 9-item scale was referred to the self-compiled questionnaire of the SARS Impact Scale (20). These nine items assessed the most common negative appraisals during and after the acute phase of coronavirus infection. A Likert scale was used to compile the scale and each question had five options with a score of 1–5 (1 = “not worried at all” and 5 = “extremely worried”). We named the revised self-rating scale COVID-19 Impact Scale (CIS). Moreover, we calculated the change scores of PHQ-9 /GAD-7/CIS by subtracting the baseline scores from the follow-up scores to indicate the improvement of mental distress or the change of negative appraisals. Other variables included patients' isolation sites during the first 2 weeks after getting discharged (categorized as at home or at the designated hotel) and mental health service utilization throughout the follow-up period (categorized as received or not received online or telephone supportive counseling).
All analyses were conducted in SPSS Version 25.0. The significance evaluation was set at P < 0.05 (two-tailed). For continuous variables, a Kolmogorov-Smirnov test was carried out to test for normality of the distribution. Data with normal distribution were presented as mean and standard deviation, and an independent sample t-test was used to compare the differences between the patients included and excluded. Data that were non-normally distributed were presented as median and quartile distance, and a Mann–Whitney U test was used for comparison of the two groups. Categorical variables were presented as frequency and percentages in each category, and a Pearson's chi-squared test was used to detect differences between the included and excluded patients as well.
Exploratory factor analysis using principal component analysis (PCA) and Varimax rotation was conducted to explore the underlying structure of CIS as well as summarize the variables of CIS. The appropriateness of factor analysis was assessed with the Bartlett's test of sphericity and the Kaiser-Meyer-Olkin (KMO) measure. The minimum factor loading cut-off point was set at 0.4 and factors with eigenvalues > 1 were selected. The internal consistency of each factor was assessed by Cronbach's α. Items were combined if Cronbach's α reached 0.80.
Repeated measure of the General Linear Model (GLM) was used to examine the effect of time on depression and anxiety as well as on patients' negative attitudes toward the infection. Demographics (age, gender, education, marriage), clinical characteristics (past medical history, severity of COVID-19, and duration of hospitalization), and supportive counseling during isolation (received or not) were included in the GLM as covariates, but were finally removed from the model as none of them showed significant effect.
Pearson correlation analysis was applied to explore the variables (i.e., demographic variable, clinical variable, and negative appraisals) that were associated with depression and anxiety symptom improvement (baseline scores—follow-up scores). Linear regression analyses were used to examine variables that explained the variance of patients' depression and anxiety symptom improvement. Variables significantly correlated with depression and anxiety symptom improvement were used as independent variables in the linear regression analysis, and depression and anxiety symptom improvement served as dependent variables, respectively.
A total of 251 patients with COVID-19 were admitted to the hospital during the peak stage of COVID-19 in China. By February 9, 39 patients had recovered and been discharged from hospital. Besides, six subjects under 14 years old were excluded from our study. Questionnaires were sent to 206 patients in hospitalization and 163 patients gave their consent to take part in the study at baseline. The overall response rate at baseline was 79.13%. During follow-up, 18 patients dropped out because of incorrect phone numbers or missed calls. Among 145 potential participants who answered the calls, 39 subjects did not consent to participate in the follow-up survey at the time of informed consent. The remaining 114 replies represented a response rate of 78.6%.
There were 42 patients who had not fully completed the Coronavirus Impact Scale (CIS) during baseline or the follow-up time point. Eventually, 72 patients who filled in the CIS in both time points were included in the analysis. Table 1 shows the demographic and clinical characteristics of the patients. The median age was 38 years (IQR, 29–47) among the included patients. Gender was closely balanced between men and women with 37 male patients (57.1%). Twenty-three patients (31.9%) had a history of physical disease and three patients (4.2%) had a history of mental disorder. The average length of stay was 17.7 days. There were no significant differences between included and excluded (the participants dropped out or with incomplete data) patients in the demographics, clinical characteristics, and psychological dimension.
Depression and anxiety scores during baseline and follow-up are shown in Table 2. The median scores of PHQ-9 and GAD-7 at baseline were 4 (IQR, 2–7), and 5 (IQR, 0–7), respectively. A total of 42.3% of the patients reported at least mild depression and 50.7% of patients reported anxiety symptoms. One month after discharge, the scores of both scales decreased (PHQ: 3, IQR 0–7; GAD: 3, IQR 0–7). GLM analysis revealed a significant effect of time on depression levels (F = 5.593, P = 0.021; Figure 1) and anxiety levels (F = 6.387, P = 0.014; Figure 1).
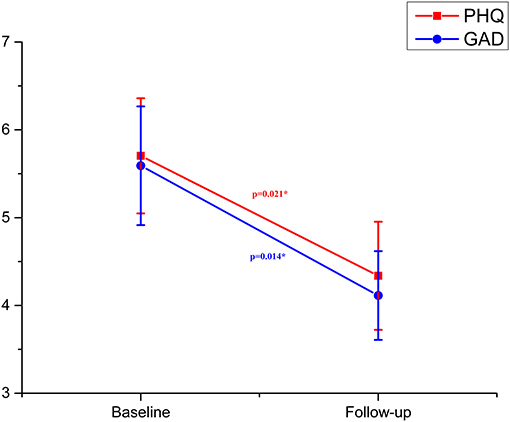
Figure 1. Depression and anxiety in patients with coronavirus infection at baseline and follow-up (error bars indicate standard errors of the variables). *P < 0.05.
The Bartlett's test of spherical (χ2 = 371.98, df =36, P < 0.001) and KMO measure (KMO = 0.845) showed that the CIS was suitable for factor analysis. The internal consistency of the total score was 0.932. PCA analysis yielded two factors, explaining 69.84% of the variance of CIS data. The two factors were named as health impact and social impact, respectively (Table 3). Both factors showed good internal consistency; Cronbach's alpha reached 0.896 for health impact and 0.885 for social impact. Therefore, the subsequent analysis will use the total scores of the two dimensions.
No significant effect of time was detected by the GLM analysis on the total scores of the CIS (F = 3.75, P = 0.057; Figure 2). However, a significant effect of time on the health impact scores was observed (F = 11.94, P < 0.001; Figure 2). Particularly, the health impact scores decreased over time. Besides, there was no significant effect of time on the social impact scores (F = 1.29, P = 0.259; Figure 2).
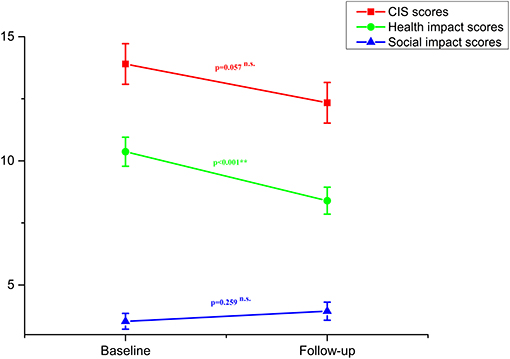
Figure 2. Total COVID-19 Impact Scale (CIS) scores, scores of health impact and scores of social impact in patients with coronavirus infection at baseline and follow-up (error bars indicate standard errors of the variables). n.s, non-significant; **P < 0.01.
To explore the variables associated with the depression and anxiety symptom improvement, correlation analyses were conducted. Pearson correlation analysis showed that the patients' demographic data, clinical characteristics, or negative appraisals (total score or factor score) had no significant correlation with the improvement in PHQ-9 scores and GAD-7 scores. However, the change of social impact was significantly correlated with the improvement in PHQ-9 scores and GAD-7 scores (PHQ: t = 0.440, P < 0.001; GAD: t = 0.251, P = 0.038). The change of health impact was significantly correlated with the improvement in PHQ-9 scores (t = 0.29, P = 0.017), but not with the improvement in GAD-7 scores (Table 4).
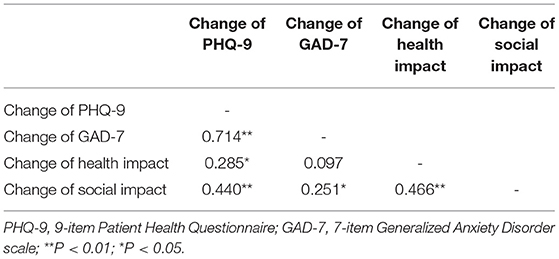
Table 4. Association between the change of negative appraisals and patients' depression and anxiety symptom improvement.
Based on the above results, we included variables that were significantly associated with the improvement of depression and anxiety scores in the linear regression analysis. Results showed that the change of social impact could explain the 12.7% variance of the PHQ-9 improvement and the 10.5% variance of the GAD-7 improvement (PHQ-9: R2 = 0.127, t = 2.691, P = 0.009; GAD-7: R2 = 0.105, t = 2.547, P = 0.013). Health impact could not explain the variance of improvement in PHQ-9 or GAD-7 (Table 5).
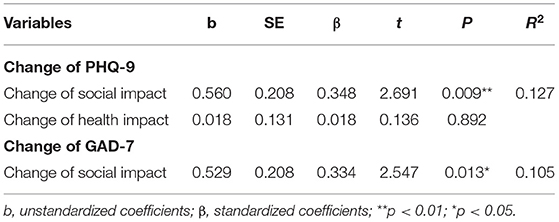
Table 5. Results of linear regression analyses on patients' depression and anxiety symptom improvement.
This study explored the mental health recovery and its relationship with negative appraisals in patients who had recovered from COVID-19. We found that 1 month after discharge, patients' depression and anxiety symptoms were significantly improved. The change of the negative appraisals of COVID-19 social impact, rather than the health impact, could explain the depression and anxiety symptom improvement.
Previous studies have shown that patients infected with a novel virus also suffered from mental health problems (24–26). Recently, many studies also revealed that people associated with COVID-19 have suffered varying degrees of psychological distress (9–11, 27–30). However, most of these were cross-sectionally designed and failed to explore the changing process and influencing factors of patients' mental health status. In our study, we found that nearly half of patients with COVID-19 exhibited depression and anxiety symptoms. Although a significant decrease in both depression and anxiety levels was observed, about a third of patients who had recovered from COVID-19 still had obvious psychological distress 1 month after discharge. The improvement in depression and anxiety symptoms was related to the change in the negative appraisals of COVID-19 social impact. The social impact items in the CIS questionnaire (i.e., financial stress, stigma, and concerns about family) did not diminish with the recovery of the disease, yet it explained the change in depression and anxiety levels. Previous studies have shown that greater negative attitudes will lead to a more protracted depressive episode (31, 32). Persistent negative appraisals might lead to long-term depression, while negative emotions may enhance patients' negative appraisals, which is a negative thinking cycle (33). Besides, social support was a main protective factor of maintaining mental wellbeing. However, negative appraisal including fear of infection, feeling of uncertainty, and stigmatization were risk factors for self-isolation which often leads to deprivation of social support (34). Therefore, the negative appraisals, especially those related to COVID-19 social impact, may be one of the sources that perpetuates psychological stress in patients after physical recovery.
It is interesting that the change of negative appraisals related to COVID-19 social impact was more related to symptom improvement in depression and anxiety than the change in negative appraisals of COVID-19 health impact. Several factors might contribute to this phenomenon. On the one hand, COVID-19 had a much lower case fatality rate than that of SARS or Ebola, and most of the patients with COVID-19 presented with mild symptoms. Therefore, the negative appraisals related to COVID-19 health impact might have a limited contribution to depression and anxiety. And the decrease in negative appraisals of COVID-19 health impact was not very closely related to depression and anxiety symptom improvement. On the other hand, COVID-19 is a highly contagious infectious disease and triggers an unprecedented level of panic among the public (35). Patients who recovered from COVID-19 are facing substantial stigma and discrimination when they come back home (36). Although patients have recovered from the infection and finished quarantine for medical observation, they are suffering from social isolation and economic problems or unemployment because of the diagnosis (37). Consistently, a recent study also reported that COVID-19-related financial and social difficulties or concerns were a major risk factor for psychological distress in subjects (38). Therefore, disturbing social problems may be more strongly linked to psychological distress in patients. And the change of negative appraisals related to COVID-19 social impact might contribute to the variation in depression and anxiety. In order to alleviate the depression and anxiety in recovered patients, we could address COVID-19-related social issues. For example, during patients' hospitalization, mental health professionals should be integrated into the medical treatment team to provide targeted psychological interventions. In addition, continued mental health interventions should be prepared for those affected patients after they have been discharged from the designated hospital. These approaches could help to reduce patients' maladaptive beliefs and help to minimize their psychological distress. Except for specific interventions aimed at patients, some effort could be done among the general public and government. For example, health education for the general public could help to reduce the stigma attached to COVID-19. Broadcasting precise and authoritative information such as the fact that recovered patients do not pass the virus to others will help to decrease the discrimination among society (39). In addition, the government could provide unemployment insurance to mitigate the economic impact of COVID-19.
Our study has the following strengths: first, we longitudinally investigated the change in mental distress of patients infected with COVID-19. In addition, we found that the social dimensions played an important role in the mental health of patients during the pandemic. Furthermore, we suggested that more attention should be given to the negative impact of the social dimension on patients' mental health. There are nevertheless several limitations in this study. Firstly, the small sample size and single-site study design limits the ability to generalize the results of the current study. Secondly, online self-reporting was used in the survey, which may bring selection bias since those who cannot use mobile devices were excluded from our study. Thirdly, we recruited 163 participants in the baseline but only 72 participants had complete data at both time points, the response rate was unsatisfactory. However, this may not bring significant bias to the results since we did not detect significant difference in baseline characteristics between the patients with complete data and those excluded. Furthermore, a causal relationship between the change of negative appraisal in COVID-19 social impact and depression or anxiety symptom improvement cannot be drawn from the current study. Long-term change in patients' mental status should be monitored and how the change in negative appraisals influence the future psychological distress should be explored. Finally, using only negative appraisals as a risk factor for the psychological distress in patients was inadequate. Future studies could investigate other influencing factors for patients' mental health during the pandemic.
Patients who had recovered from COVID-19 showed significant improvement in depression and anxiety symptoms. The change of negative appraisals in the COVID-19 social impact might play a major role in reducing their depression and anxiety. Strategies targeting the reduction of COVID-19-related social issues might be helpful to improve the mental health of recovered patients during the COVID-19 crisis.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the ethics review boards of The First Hospital of Changsha. The patients/participants provided their electronic informed consent to participate in this study.
All authors had full access to all the data in the study and had full responsibility for the content of the manuscript for publication. KS, JL, and YZha was responsibility for the final review and had final responsibility for the decision to submit for publication.
This work was supported by the Project of Hunan Provincial Department of Science and Technology (2020SK3014 to JL), the Defense Innovative Special Region Program (17-163-12-ZT-001-041-01 to YZha), the National Natural Science Foundation of China (81671353 to YZha), the National Key Research and Development Program of China (2019YFA0706200 to YZha), and Changsha Science and Technology Bureau (KQ2001005 to KS). The authors gratefully acknowledge financial support from the above affiliations.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors would like to thank all the health care workers and patients who fighting against the COVID-19. YJ was supported by postdoctoral programme in Central South University.
1. World Health Organization (2020). WHO Coronavirus Disease (COVID-19) Dashboard. World Health Organization. Available online at: https://covid19.who.int/ (accessed March 31, 2020).
2. Wu KK, Chan SK, Ma TM. Posttraumatic stress, anxiety, and depression in survivors of severe acute respiratory syndrome (SARS). J Trauma Stress. (2005) 18:39–42. doi: 10.1002/jts.20004
3. Mak IW, Chu CM, Pan PC, Yiu MG, Chan VL. Long-term psychiatric morbidities among SARS survivors. Gen Hosp Psychiatry. (2009) 31:318–26. doi: 10.1016/j.genhosppsych.2009.03.001
4. Blakey SM, Abramowitz JS. Psychological predictors of health anxiety in response to the Zika virus. J Clin Psychol Med Settings. (2017) 24:270–8. doi: 10.1007/s10880-017-9514-y
5. Lettinga KD, Verbon A, Nieuwkerk PT, Jonkers RE, Gersons BP, Prins JM, et al. Health-related quality of life and posttraumatic stress disorder among survivors of an outbreak of Legionnaires disease. Clin Infect Dis. (2002) 35:11–7. doi: 10.1086/340738
6. Kapfhammer HP, Rothenhausler HB, Krauseneck T, Stoll C, Schelling G. Posttraumatic stress disorder and health-related quality of life in long-term survivors of acute respiratory distress syndrome. Am J Psychiatry. (2004) 161:45–52. doi: 10.1176/appi.ajp.161.1.45
7. Ji D, Ji YJ, Duan XZ, Li WG, Sun ZQ, Song XA, et al. Prevalence of psychological symptoms among Ebola survivors and healthcare workers during the 2014-2015 Ebola outbreak in Sierra Leone: a cross-sectional study. Oncotarget. (2017) 8:12784–91. doi: 10.18632/oncotarget.14498
8. Lee AM, Wong JG, McAlonan GM, Cheung V, Cheung C, Sham PC, et al. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can J Psychiatry. (2007) 52:233–40. doi: 10.1177/070674370705200405
9. Varatharaj A, Thomas N, Ellul MA, Davies NWS, Pollak TA, Tenorio EL, et al. Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study. Lancet Psychiatry. (2020) 7:875–82. doi: 10.1016/S2215-0366(20)30287-X
10. Sun N, Wei L, Wang H, Wang X, Gao M, Hu X, et al. Qualitative study of the psychological experience of COVID-19 patients during hospitalization. J Affect Disord. (2021) 278:15–22. doi: 10.1016/j.jad.2020.08.040
11. Leung TYM, Chan AYL, Chan EW, Chan VKY, Chui CSL, Cowling BJ, et al. Short- and potential long-term adverse health outcomes of COVID-19: a rapid review. Emerg Microbes Infect. (2020) 9:2190–9. doi: 10.1080/22221751.2020.1825914
12. Liu LS, Li XW, Hua Q, Yang X, Wu H, et al. Psychological health status in 500 patients with SARS. J Capital Medical University. (2003) 4:427–74.
13. Hawryluck L, Gold WL, Robinson S, Pogorski S, Galea S, Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis. (2004) 10:1206–12. doi: 10.3201/eid1007.030703
14. Hulbert-Williams N, Neal R, Morrison V, Hood K, Wilkinson C. Anxiety, depression and quality of life after cancer diagnosis: what psychosocial variables best predict how patients adjust? Psychooncology. (2012) 21:857–67. doi: 10.1002/pon.1980
15. Spinhoven P, Penninx BW, Krempeniou A, van Hemert AM, Elzinga B. Trait rumination predicts onset of post-traumatic stress disorder through trauma-related cognitive appraisals: a 4-year longitudinal study. Behav Res Ther. (2015) 71:101–9. doi: 10.1016/j.brat.2015.06.004
16. Uchida Y, Takahashi T, Katayama S, Masuya J, Ichiki M, Tanabe H, et al. Influence of trait anxiety, child maltreatment, and adulthood life events on depressive symptoms. Neuropsychiatr Dis Treat. (2018) 14:3279–87. doi: 10.2147/NDT.S182783
17. Yoon H, Chatters L, Kao TA, Saint-Arnault D, Northouse L. Predictors of quality of life and depression among Korean-American cancer patients and their family caregivers. Psychooncology. (2018) 27:2717–24. doi: 10.1002/pon.4864
18. Xin M, Luo S, She R, Yu Y, Li L, Wang S, et al. Negative cognitive and psychological correlates of mandatory quarantine during the initial COVID-19 outbreak in China. Am Psychol. (2020) 75:607–17. doi: 10.1037/amp0000692
19. Reynolds DL, Garay JR, Deamond SL, Moran MK, Gold W, Styra R. Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiol Infect. (2008) 136:997–1007. doi: 10.1017/S0950268807009156
20. Cheng SK, Wong CW, Tsang J, Wong KC. Psychological distress and negative appraisals in survivors of severe acute respiratory syndrome (SARS). Psychol Med. (2004) 34:1187–95. doi: 10.1017/s0033291704002272
21. The National Health Commission. (2020). Diagnosis and Treatment Plan of COVID-2019 (7th edition). Joint Prevention and Control Mechanism of the State Council. Available online at: http://wwwnhcgovcn/yzygj/s7653p/202003/46c9294a7dfe4cef80dc7f5912eb1989shtml (accessed March 31, 2020).
22. Chen R, Wang Y, Yu JY, Zhang L. Evaluation of the reliability and validity of PHQ. SiChuan Mental Health. (2017) 30:149–53. doi: 10.11886/j.issn.1007-3256.2017.02.013
23. Wang Y, Chen R, Zhang L. Evaluation of the reliability and validity of the generalized anxiety disorder 7-item scale among inpatients in general hospital. J Clin Psychiatry. (2018) 28:168–71. doi: 10.3969/j.issn.1005-3220.2018.03.007
24. Chua SE, Cheung V, McAlonan GM, Cheung C, Wong JW, Cheung EP, et al. Stress and psychological impact on SARS patients during the outbreak. Can J Psychiatry. (2004) 49:385–90. doi: 10.1177/070674370404900607
25. Lee DT, Wing YK, Leung HC, Sung JJ, Ng YK, Yiu GC, et al. Factors associated with psychosis among patients with severe acute respiratory syndrome: a case-control study. Clin Infect Dis. (2004) 39:1247–9. doi: 10.1086/424016
26. Wu KK, Chan SK, Ma TM. Posttraumatic stress after SARS. Emerg Infect Dis. (2005) 11:1297–300. doi: 10.3201/eid1108.041083
27. Kang L, Ma S, Chen M, Yang J, Wang Y, Li R, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun. (2020). doi: 10.1016/j.bbi.2020.03.028
28. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
29. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. (2020) 17:1729. doi: 10.3390/ijerph17051729
30. Epstein D, Andrawis W, Lipsky AM, Ziad HA, Matan M. Anxiety and suicidality in a hospitalized patient with COVID-19 infection. Eur J Case Rep Intern Med. (2020) 7:001651. doi: 10.12890/2020_001651
31. Kavanagh DJ, Wilson PH. Prediction of outcome with group cognitive therapy for depression. Behav Res Ther. (1989) 27:333–43. doi: 10.1016/0005-7967(89)90003-x
32. Beevers CG, Wells TT, Miller IW. Predicting response to depression treatment: the role of negative cognition. J Consult Clin Psychol. (2007) 75:422–31. doi: 10.1037/0022-006X.75.3.422
33. Takano K, Van Grieken J, Raes F. Difficulty in updating positive beliefs about negative cognition is associated with increased depressed mood. J Behav Ther Exp Psychiatry. (2019) 64:22–30. doi: 10.1016/j.jbtep.2019.02.001
34. World Health Organization (2020). Mental health and psychosocial considerations during the COVID-19 outbreak. Available online at: https://apps.who.int/iris/handle/10665/331490 (accesssed March 18, 2020).
35. Sotgiu G, Carta G, Suelzu L, Carta D, Migliori GB. How to demystify COVID-19 and reduce social stigma. Int J Tuberc Lung Dis. (2020) 24:640–2. doi: 10.5588/ijtld.20.0233
36. Bagcchi S. Stigma during the COVID-19 pandemic. Lancet Infect Dis. (2020) 20:782. doi: 10.1016/S1473-3099(20)30498-9
37. Singh R, Subedi M. COVID-19 and stigma: social discrimination towards frontline healthcare providers and COVID-19 recovered patients in Nepal. Asian J Psychiatr. (2020) 53:102222. doi: 10.1016/j.ajp.2020.102222
38. Carmassi C, Bertelloni CA, Dell'Oste V, Barberi FM, Maglio A, Buccianelli B, et al. Tele-psychiatry assessment of post-traumatic stress symptoms in 100 patients with bipolar disorder during the COVID-19 pandemic social-distancing measures in Italy. Front Psychiatry. (2020) 11:580736. doi: 10.3389/fpsyt.2020.580736
39. World Health Organization (2020). WHO Says Positive Tests for Recovered Virus Patients are Not Reinfections. Available online at: http://www.naharnet.com/stories/en/271638-who-says-positive-tests-for-recovered-virus-patients-are-not-reinfections (accessed May 6, 2020).
Keywords: coronavirus disease 2019, patients, mental health, psychology, depression, anxiety, negative appraisals
Citation: Chen W, Ju Y, Liu B, Huang M, Yang A, Zhou Y, Wang M, Liao M, Shu K, Liu J and Zhang Y (2021) Negative Appraisals of the COVID-19 Social Impact Associated With the Improvement of Depression and Anxiety in Patients After COVID-19 Recovery. Front. Psychiatry 12:585537. doi: 10.3389/fpsyt.2021.585537
Received: 20 July 2020; Accepted: 01 March 2021;
Published: 15 April 2021.
Edited by:
Carlo Lai, Sapienza University of Rome, ItalyReviewed by:
Alessia Renzi, Sapienza University of Rome, ItalyCopyright © 2021 Chen, Ju, Liu, Huang, Yang, Zhou, Wang, Liao, Shu, Liu and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kongliang Shu, c2tsMTk3NzA0MTBAMTYzLmNvbQ==; Jiyang Liu, Y3NwaHFAMTYzLmNvbQ==; Yan Zhang, enlkZDc4NzdAY3N1LmVkYy5jbg==
†These authors have contributed equally to this work and share the first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.