
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 10 February 2021
Sec. Public Mental Health
Volume 11 - 2020 | https://doi.org/10.3389/fpsyt.2020.613368
This article is part of the Research Topic Resilience and Health in the Chinese People during the COVID-19 Outbreak View all 22 articles
Background: Previous studies have found that disaster-related media exposure could predict acute stress responses. However, few studies have investigated the relationship between media exposure to COVID-19 and acute stress, and less is known about the mechanisms that translate media exposure to COVID-19 into acute stress. The current study explored the impact of media exposure to COVID-19 on acute stress, and examined the mediating role of intolerance of uncertainty (IU) and the moderating role of perceived social support (PSS).
Methods: A total of 1,483 Chinese participants (Mage = 27.93 years, SD = 8.45) completed anonymous online questionnaires regarding media exposure to COVID-19, IU, PSS, and acute stress during the COVID-19 outbreak in China.
Results: Media exposure to COVID-19 was positively related to acute stress, and IU partially mediated this relationship. The direct effect of media exposure to COVID-19 on acute stress, and the relationship between IU and acute stress, were both moderated by PSS. The impacts of both media exposure to COVID-19 and IU on acute stress were stronger for individuals with low PSS.
Limitations: This study collected data in a shorter timeframe, and no assessments occurred during the follow-up, which may prevent us from detecting the changes of the relationships between variables over time. Meanwhile, the self-report method limited the validity of the data due to subjective reporting bias.
Conclusions: These findings contribute to a better understanding of how and when pandemic-related media exposure affects acute stress, and provide new perspectives for the prevention to reduce psychological problems following traumatic events.
COVID-19, as a novel Coronavirus was first reported in Wuhan, China, and has rapidly spread into a global pandemic, causing huge numbers of hospitalizations and deaths (1, 2). The Chinese government executed preventative and control measures, including the lockdown of cities, travel bans, and home quarantine, to curb the spread of the virus (3, 4). During the COVID-19 outbreak, the public had a great need for the latest information about COVID-19 from the media to make clear of the situation and protect their health (5, 6). However, the over-reliance on media can cause long term and repeated exposure to the pandemic, which may put the public under psychological distress.
Previous empirical studies have found that media-based indirect exposure to disaster-related events was linked to poor psychological outcomes (7–10). Meanwhile, some studies also indicated that pandemic-related media exposure was positively associated with stress-related symptoms, such as anxiety, depression and worry (5, 6, 11, 12). One study even showed that media exposure was more closely correlated with acute stress than direct exposure (13). Therefore, media exposure to COVID-19 may be an important factor contributing to individuals' acute stress responses. However, less is known about the mechanisms that translate media exposure to COVID-19 into acute stress responses.
Some research suggested that media-related consumption was positively related to intolerance of uncertainty (IU) (14), and IU could lead to poor mental health (15–17). Thus, IU may mediate the relationship between media exposure to COVID-19 and acute stress. According to the stress-buffering model, perceived social support (PSS) may buffer individuals from the adverse effects of stressful events (18). Numerous empirical studies indeed revealed that PSS could moderate the relation between traumatic experiences or stress situations and their influences on people (19–21). Therefore, PSS may affect the relationship between media exposure to COVID-19 and acute stress. To this end, the present study attempted to investigate the relationship between media exposure to COVID-19 and acute stress, and to explore the mechanisms underlying the association by testing the mediating effect of IU and the moderating effect of PSS. The findings would advance our understanding of how and when media exposure to COVID-19 could impact acute stress.
According to the risk factor model of the post-traumatic stress response, disaster-related exposure is the primary factor affecting the physical and mental health after traumatic events (22–24). Being one of the disaster-related exposure, disaster-related media exposure can also lead to negative mental health outcomes (9, 25, 26). For instance, Yeung et al. (7) found that frequent exposure to distressing media information could predict PTSD symptoms several months after indirect exposure to the 2008 Wenchuan Earthquake. More importantly, a meta-analysis also demonstrated that media exposure to disasters or large-scale violence had far-reaching effects on poor psychological consequences (27).
Acute stress response refers to a series of physiological and psychological reactions, which is usually triggered by a stressful and life-threatening event (28). Previous empirical research has confirmed the relation between disaster-related media exposure and acute stress responses (10, 29, 30). For example, accumulated evidence indicated that frequently engaging with trauma-related media contents could extend acute stress experiences and increase stress-related symptoms following the Boston Marathon bombings (9, 10, 13). The COVID-19 pandemic, as a public health event, was featured by its rapid transmission, uncertainty about future, considerable mortality rate and serious impacts (31). Facing such an unpredictable and uncontrollable stressful event, the general public are under unprecedented pressure and are experiencing severe psychological distress, including COVID-19-related acute stress responses (32, 33). Correspondingly, some research has also found that the COVID-19 pandemic could induce acute stress responses among the public (33–35). The stressful experiences from either the outbreak itself or the subsequent government responses to the outbreak (e.g., lockdown, travel restrictions) occurred in a very short time period following the COVID-19 outbreak, which may lead to COVID-19-related acute stress responses (28). Besides, the ongoing perceived threats, inconsistent information and uncertainty about the future, accompanied by the pandemic may constitute a risk for mental health (36). When faced with the ambiguous situation and continued threats induced by COVID-19 pandemic, individuals tend to consume information form media to guide them (33). However, media coverage about COVID-19 may amplify the perception of risk, and lead to an exacerbation of stress-related symptoms (5, 6). Therefore, it can be inferred that pandemic-related media exposure could predict COVID-19-related acute stress responses.
Moreover, emotional contagion model indicates that negative emotions can be contagious to each other in crisis events (37, 38). Accordingly, widespread media coverage about disasters may extend the boundary of disaster itself and disseminate passive emotions among the population, thereby increasing psychological distress (39). In fact, the mere exposure of distressing media content is sufficient to provoke negative emotions (5, 6, 40, 41). During the COVID-19 outbreak, media coverage usually contained numerous stress-inducing contents, such as rumors, misrepresentation, and fear messages, especially media-based graphic images (e.g., diagnosed patients with ventilators), all of which would result in huge psychological stress on the public. Thus, it is reasonable that pandemic-related media exposure can promote the formation and development of COVID-19-related acute stress responses. Based on the theoretical and empirical grounds, we hypothesized that media exposure to COVID-19 would be positively correlated with acute stress (Hypothesis 1).
IU is defined as a relatively broad construct representing cognitive, emotional, and behavioral reactions to uncertainty in everyday life situations, which can be seen as a dispositional tendency (42, 43). According to uncertainty reduction theory, individuals with high IU tend to seek information about the potential threat to reduce anxiety and uncertainty after disasters (44). However, seeking information via the media may backfire when individuals are exposed to disaster-related media content, thereby exacerbating their distress and uncertainty (10, 14). Meanwhile, IU is in general sustained by the associated perception of uncertainty, and the uncertainty comes largely from uncertain situations and life events (43, 45). Given that many aspects of life were full of uncertainty due to the COVID-19 outbreak, pandemic-related media exposure can be seen as an important source of uncertainty. Thus, IU may also emerge in response to “uncertain” media exposure related to COVID-19. Indeed, a few studies have indicated that media-related consumption was positively associated with IU. For example, a meta-analysis showed that increased mobile phone penetration and Internet usage were positively correlated to the rising IU levels (46). Furthermore, broad evidence has showed that IU can be changed by a series of experimental manipulations, in which the uncertainty about the outcome of events was manipulated to induce high or low degrees of IU (47–49). Therefore, we inferred that media exposure to COVID-19 was positively related to IU.
Moreover, IU plays a significant role in the development and maintenance of distress (16, 50). There is increasing evidence to support that IU is closely associated with mental health problems. For instance, ample empirical evidence has shown that IU was a risk factor for affective disorders, such as generalized anxiety disorder (51), obsessive-compulsive disorder (52), major depressive disorder (53). Similarly, some studies have also demonstrated that IU was highly linked with anxiety, depression and worry (17, 54, 55). Furthermore, previous research has also found that IU was related to elevated post-traumatic stress symptoms (PTSS) (56–58). Individuals with high IU are prone to respond negatively to uncertain or ambiguous situations, which may lead to negative psychological responses over time (58, 59). Hence, it is reasonable to infer that IU could affect acute stress. Taken together, we speculated that IU may act as a mediating role between media exposure to COVID-19 and acute stress (Hypothesis 2).
Although disaster-related media exposure may increase the risk of acute stress through IU, it seems impossible that all individuals would experience an equivalent level of acute stress. PSS may moderate the effect of pandemic-related media exposure on acute stress.
PSS refers to an individual's confidence that sufficient support can be available during times of need (60). It can help individuals manage stressful life events by providing a sense of feeling valued and accepted and by prompting appropriate coping responses (18). Several studies suggested that social support was negatively associated with passive emotions, such as anxiety, depression and stress (61–63). According to the stress-buffering model, PSS can buffer individuals from the passive impacts of stressful events (18, 64). As such, individuals with high levels of PSS may present better psychological adjustment (65). Numerous empirical studies have supported this model. For instance, some studies found social support had a potential moderating effect in the relationship between trauma exposure and psychological health outcomes, such as depression and PTSD (66, 67). The risk-buffering hypothesis also holds that one protective factor can mitigate the association between environmental risk factors and negative outcomes (68). Therefore, we inferred that PSS may moderate the relationships between media exposure to COVID-19 and IU, as well as between media exposure to COVID-19 and acute stress.
Moreover, PSS may buffer the negative effects of psychological distress (18, 68). Some research has found that social support could attenuate the relationships between personal risk factors and health outcomes and behaviors (69–71). For example, it was found that PSS moderated the relation between depression and adolescent problematic smartphone use (72), and the relation between psychological insecurity and depression (73). IU is, understandably, a personal risk factor that may cause negative psychological outcomes (e.g., anxiety, depression) (54, 55). Therefore, PSS may act as a moderator in the relationship between IU and acute stress. To some extent, PSS can be seen as a protective factor for stress-related outcomes (74–76), and may contribute to enhancing individuals' internal mental resources (77). As a result, individuals perceiving more social support would be less likely to have psychological problems in response to stressful events or other psychological distress (78, 79). Based on the theoretical views and empirical evidence, we deduced that PSS would moderate the direct and indirect relations between media exposure to COVID-19 and acute stress (Hypothesis 3).
The present study aimed to examine the impact of media exposure to COVID-19 on acute stress and its underlying mechanisms. First, we examined whether media exposure to COVID-19 would directly affect acute stress. Second, we tested the mediating role of IU in the relation between media exposure to COVID-19 and acute stress. Third, we tested whether the direct and indirect relations between media exposure to COVID-19 and acute stress through IU would be moderated by PSS. Therefore, we proposed a moderated mediation model (see Figure 1).
This survey was conducted from February 7 to February 28, 2020, during the COVID-19 outbreak in China. Participants were required to finish Internet-based questionnaires via social media (WeChat, Tencent). A total of 1,626 participants from 32 provinces or political areas participated in our research. The final sample consisted of 1,483 participants after removing participants who gave uniform answers to all items in the questionnaire and those who were directly exposed to COVID-19 (e.g., close contacts, confirmed cases). Among the participants, 466 (31.42%) were males and 1,017 (68.58%) were females, with a mean age of 27.93 years (SD = 8.45; range: 18–87 years), and 932 (62.85%) were single. Nearly half of respondents lived in city (46.66%), and more than half of participants were undergraduate (55.02%). Detailed demographic characteristics are presented in Table 1. All participants signed an electronic informed consent prior to their participation, and they could withdraw at any time if they wished. All procedures performed in this study involving human participants were in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Media Exposure Questionnaire (MEQ) was developed to test media exposure to COVID-19 following previous research (13, 14). Nine items were used to assess the media exposure to COVID-19 by asking participants how many hours per day (0–24 h) they spent engaged with information about COVID-19 from the nine most common media sources separately (e.g., television, online news, social media). An example item is “How many hours per day did you spend watching TV to know about COVID-19 in the latest week.” Total media exposure scores were calculated based on the accumulated continuous number of hours across types of media, with higher scores indicating higher levels of media exposure to COVID-19. The Cronbach's α in this study was 0.82.
Intolerance of Uncertainty Scale-12 (IUS-12) is a 12-item self-report scale that assesses reactions and desired control over ambiguous or uncertain situations (80). The measure uses a 5-point scale scored from 1 (strongly disagree) to 5 (strongly agree). The total scores can range from 12 to 60, with higher scores indicating more serious IU. The Cronbach's α in current study was 0.88.
Perceived social support was tested by Perceived Social Support Scale (PSSS) (81). The PSSS is a 12-item self-report scale, and each item uses a 7-point scale (1 = strongly disagree; 7 = strongly agree). The total scores can range from 12 to 84, with higher scores indicating better social support the participants perceived. In this study, the Cronbach's α was 0.94.
Stanford Acute Stress Reaction Questionnaire (SASRQ) is usually used to measure acute stress and acute stress disorders (ASD) (82). The Chinese version of SASRQ was revised by Jia and Hou (83) through standard translation and back-translation procedure. Many empirical results have showed that the Chinese version of SASRQ has a good reliability and validity (84–86). In present study, some items were modified to ensure that the scale could be suitable to assess COVID-19-related acute stress responses by reference to previous research (9, 10, 13). An example item is “The COVID-19 pandemic made it difficult for me to perform work or other things I needed to do.” The SASRQ is a self-report questionnaire with 30 items including dissociation (10 items), reexperiencing of trauma (six items), avoidance (six items), anxiety and hyperarousal (six items), and impairment in functioning (two items). The measure uses a 6-point scale scored from 0 (not experienced) to 5 (very often experienced). The total scores can range from 0 to 150, with higher scores indicating higher levels of acute stress. The Cronbach's α in current study was 0.95.
In this study, all statistical analyses were performed using SPSS 25.0. First, a factor analysis was used to test common method biases. Second, descriptive statistics and Pearson correlations were calculated among the study variables. Third, independent t-test and one-way ANOVA were used to compare the differences of study variables in gender, age and marital status. Next, we used Model 4 of the PROCESS macro for SPSS to examine the mediating effect of IU (87). Finally, Model 59 of the PROCESS macro was used to test the moderating effects of PSS in the direct and indirect relationships between media exposure to COVID-19 and acute stress (87). The bootstrapping method (5,000 bootstrapping samples) with 95% confidence intervals (CIs) was conducted to detect the significance of the effects (87). All study variables, except gender and marital status, were standardized in Model 4 and Model 59 before data analyses. Since previous studies reported that gender, age and marital status could influence psychological health following traumatic events (29, 88, 89), we added gender, age and marital status as control variables in the models.
Given that the data were obtained by self-report questionnaires, we conducted a Harman's single factor test to examine the common method biases (90). The results indicated that 10 factors with eigenvalues > 1 were extracted, which explained 62.28% of the total variance. The first principal factor explained 24.75% of the variance. These results showed that no common method bias existed in current study.
Means, standard deviations and correlations between main variables are provided in Table 2. Media exposure to COVID-19 was positively correlated with IU (r = 0.17, p < 0.001) and acute stress (r = 0.26, p < 0.001), and the Hypothesis 1 was supported. IU was positively correlated with acute stress (r = 0.35, p < 0.001). However, PSS was negatively correlated with IU (r = −0.10, p < 0.001) and acute stress (r = −0.24, p < 0.001).
As shown in Table 3, t-tests showed that there were significant gender differences in PSS (t = −4.30, p < 0.001) and acute stress (t = −2.02, p < 0.05). Females reported higher levels of both PSS and acute stress than males. One-way ANOVAs indicated that age and marital status had significant effects on PSS (both p < 0.01). Individuals aged 26–44 and married people had higher levels of PSS.
In Hypothesis 2, we deduced that IU would mediate the relationship between media exposure to COVID-19 and acute stress. The hypothesis was examined with Model 4 of the PROCESS macro after controlling for gender, age and marital status (87). As Table 4 shows, media exposure to COVID-19 was positively associated with IU [β = 0.17, t = 6.60, p < 0.001, 95% CI = (0.12, 0.22)], and IU was positively associated with acute stress [β = 0.32, t = 13.13, p < 0.001, 95% CI = (0.27, 0.36)]. Moreover, when the mediator (IU) was included in the model, media exposure to COVID-19 was also positively associated with acute stress [β = 0.20, t = 8.43, p < 0.001, 95% CI = (0.16, 0.25)]. This indicated that IU partially mediated the relationship between media exposure to COVID-19 and acute stress. The bootstrapping results also indicated that the conditional indirect effect of media exposure to COVID-19 on acute stress through IU was significant [indirect effect = 0.05, Boot SE = 0.009, Boot 95% CI = (0.036, 0.073)]. The mediation effect accounted for 21.38% of the total effect.
To test moderated mediation (Hypothesis 3), we adopted Model 59 of the PROCESS macro for SPSS after controlling for gender, age and marital status (87). As presented in Table 5, the interaction between media exposure to COVID-19 and PSS had a significant predictive effect on acute stress [β = −0.08, t = −3.32, p < 0.001, 95% CI = (−0.12, −0.03)], but not on IU [β = −0.02, t = −0.83, p > 0.05, 95% CI = (−0.07, 0.03)]. The interaction between IU and PSS had a significant predictive effect on acute stress [β = −0.07, t = −3.40, p < 0.001, 95% CI = (−0.10, −0.03)]. The results suggested that PSS moderated the relationships between media exposure to COVID-19 and acute stress, and between IU and acute stress.
To better interpret the moderating effects of PSS, we examined the simple effects of both media exposure to COVID-19 on acute stress and IU on acute stress, at different levels of PSS (1 SD below the mean and 1 SD above the mean). Simple slope tests showed that the association between media exposure to COVID-19 and acute stress was stronger for individuals with low PSS (βsimple = 0.27, t = 8.59, p < 0.001) than for individuals with high PSS (βsimple = 0.12, t = 3.57, p < 0.001) (see Figure 2). Similarly, the association between IU and acute stress was stronger for individuals with low PSS (βsimple = 0.36, t = 12.20, p < 0.001) than for individuals with high PSS (βsimple = 0.22, t = 7.04, p < 0.001) (see Figure 3).
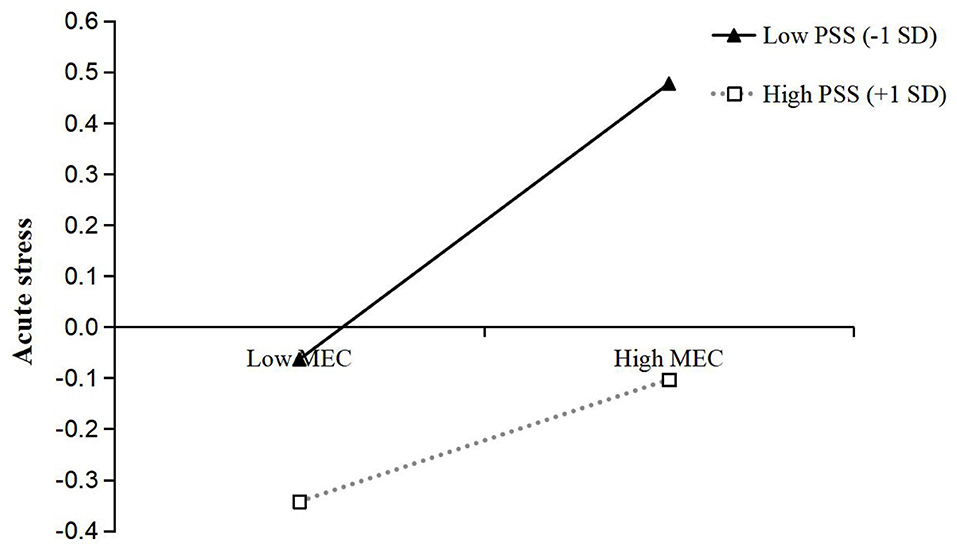
Figure 2. The interaction between media exposure to COVID-19 and perceived social support on acute stress. MEC, Media exposure to COVID-19; PSS, Perceived social support.
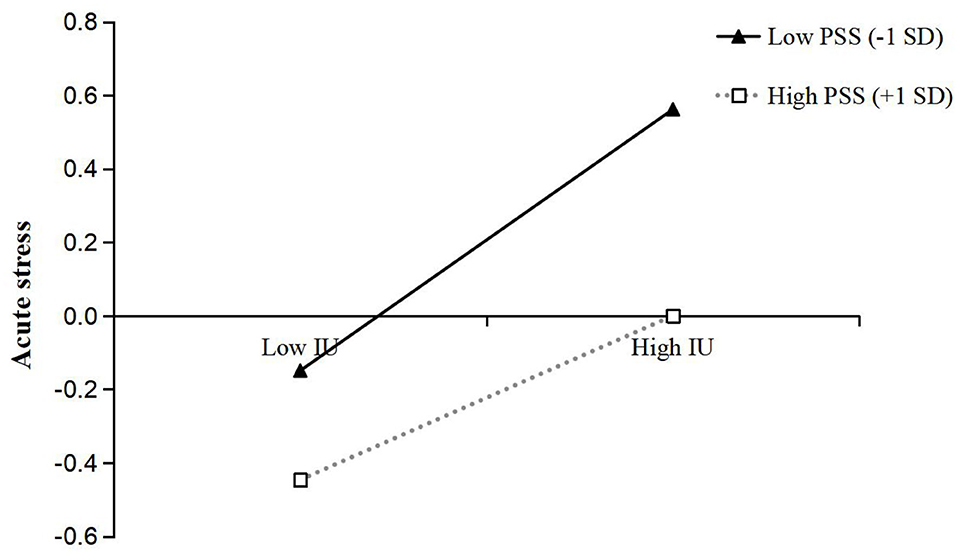
Figure 3. The interaction between intolerance of uncertainty and perceived social support on acute stress. IU, Intolerance of uncertainty; PSS, Perceived social support.
Moreover, we further examined whether the moderated direct and indirect effects of media exposure to COVID-19 on acute stress were statistically significant. First, the moderated direct effect showed that the association between media exposure to COVID-19 and acute stress was stronger for individuals with low PSS [β = 0.27, t = 8.59, p < 0.001, 95% CI = (0.21, 0.33)] than for individuals with high PSS [β = 0.12, t = 3.57, p < 0.001, 95% CI = (0.05, 0.19)]. Second, the bootstrapping results indicated that the indirect effect of media exposure to COVID-19 on acute stress via IU was moderated by PSS [the index of moderated mediation = −0.01, Boot SE = 0.004, Boot 95% CI = (−0.020, −0.004)]. The indirect effect of media exposure to COVID-19 on acute stress via IU was stronger for individuals with low PSS [indirect effect = 0.06, Boot SE = 0.011, Boot 95% CI = (0.040, 0.084)] than for individuals with high PSS [indirect effect = 0.04, Boot SE = 0.008, Boot 95% CI = (0.023, 0.055)]. In addition, the pairwise contrasts between conditional indirect effects (Effect1 minus Effect2) were all significant: Contrasts effect 1 (0.05–0.06) = −0.01, Boot SE = 0.004, Boot 95% CI = (−0.020, −0.004); Contrasts effect 2 (0.04–0.06) = −0.02, Boot SE = 0.008, Boot 95% CI = (−0.040, −0.008); Contrasts effect 3 (0.04–0.05) = −0.01, Boot SE = 0.004, Boot 95% CI = (−0.020, −0.004). In sum, these results indicated that PSS moderated the relationship between media exposure to COVID-19 and acute stress via IU.
In current study, we investigated the influence of media exposure to COVID-19 on acute stress during the COVID-19 outbreak in China, and built a moderated mediation model with IU as a mediating variable and PSS as a moderating variable. Results showed that media exposure to COVID-19 could directly affected acute stress, which supported previous studies that pandemic-related media exposure could lead to stress-related responses (5, 6, 11, 12). Moreover, this study further extended previous research by confirming that media exposure to COVID-19 could affect acute stress indirectly through the mediator of IU, and PSS moderated the relationships between media exposure to COVID-19 and acute stress, as well as between IU and acute stress.
The demographic variable tests on PSS showed that there were significant differences in gender, age and marital status. In particular, the females, the age group of 26–44 years and being married had higher levels of PSS than other groups. Actually, the differences of PSS in the demographic variables of gender, age, marital status are controversial in previous studies against the background of COVID-19 outbreak. For example, Zmete and Pak (91) found the differences of PSS only in marital status but not in gender and age. Contrarily, another study suggested that there were significant differences of PSS in gender and age (36). Therefore, further research is warranted to explore the differences of PSS in the demographic variables. Moreover, we found that females had higher levels of acute stress than males during the COVID-19 outbreak, which supported the most previous studies demonstrating that females generally have more serious psychological symptoms than males following disaster-related events (88, 92). One possible explanation is that as a special group with delicate perception and emotional vulnerability, females are more susceptible to negative outcomes following disasters, thus experiencing higher acute stress. Furthermore, females are vulnerable to multiple stresses in that they are often more sensitive to the guarantee of family stability in China, which may render females more prone to psychological problems during the pandemic.
The present study discovered that media exposure to COVID-19 was positively correlated with acute stress, even after controlling for demographics. That is, individuals engaging in more pandemic-related information were more likely to show higher acute stress. Our results supported the risk factor model of the post-traumatic stress response (23, 24), suggesting that pandemic-related media exposure was a potential risk factor for mental health. Meanwhile, this further indicated that trauma-related media exposure could predict negative psychological outcomes in different traumatic events (e.g., natural disasters, man-made accidents, public health emergencies). In addition, our results were in line with emotional contagion model (37, 38). This may suggest that emotional contagion is an interactive process between individuals, and the negative emotions induced by COVID-19 pandemic could be contagious to each other. As a result, individuals with more media exposure to COVID-19 were more vulnerable to acute stress.
Furthermore, our findings echoed the previous empirical studies, which stated that disaster-related media exposure was predictably related to acute stress (9, 10, 13). Besides, the present study further supported recent research suggesting that media exposure to COVID-19 could result in stress-related symptoms (5, 6, 11). In the period of COVID-19 outbreak in China, the rapid spread of pandemic caused social isolation of an entire nation, and people also had a great craving for information to figure out the situation and to reduce potential risks and uncertainties. In this situation, media became the main source of pandemic-related information for the majority of people in China. However, prolonged and uncontrolled media exposure could reinforce rumination and intrusive thoughts, activate fear circuitry (13, 93), and enhance autonomic activation and affecting physiologic systems (94–96), thus leading to the increase of acute stress.
As predicted, IU partially mediated the relationship between media exposure to COVID-19 and acute stress. Therefore, IU may be not only an outcome of media exposure to COVID-19, but also a predictor of acute stress. To our knowledge, this is the first study that tests the mediating effect of IU in the relation between media exposure and acute stress following stressful events.
For the first path of the mediation process, we found that media exposure was positively linked to IU, which coincided with one prior study (14). Media coverage usually contains ambiguous, exaggerated and even dramatic information, which may lead to more information-seeking behaviors aimed at reducing uncertainty and relieving discomfort. However, these information-seeking behaviors could provide new entries to exposure to more pandemic-related information by all kinds of media, in turn causing people to experience more uncertainty. That is, pandemic-related media exposure could provide necessary psychological basis for the generation of IU. Besides, given that COVID-19 is a highly contagious virus without effective treatment and adequate protective materials (2), people with frequent media exposure to COVID-19 are more likely to hold a negative expectation for the future and thus cannot tolerate uncertainty. The findings also supported prior studies revealing that IU could be subject to change in response to uncertainty information or scenes (47–49). Moreover, given that individuals high in IU are more likely to seek information from media to reduce uncertainty, future research is needed to explore the influence of IU on media exposure related to stressful events.
For the second path of the mediation process, this study indicated that IU was positively related to acute stress, which supported the previous research showing that IU could lead to negative psychological outcomes (54, 97, 98). There are two possible explanations for this finding. First, individuals with higher levels of IU may display an exaggerated perception of threat and engage in increased avoidance following a traumatic event due to the uncertainty (57, 80, 99). They usually evidence a greater likelihood to interpret uncertain information as unacceptable and threatening (100, 101). Thus, those high in IU may display increased acute stress. Second, IU, as a tendency to response negatively to uncertain situations and events, essentially reflects the worry about the uncertainty in the future (59). And repeated experiencing such feeling may also contribute to other stress-related psychological symptoms, such as anxiety, depression and PTSD (17, 55, 56). Therefore, it is not difficult to explain that IU can affect acute stress.
Our study further found that PSS weakened the associations between media exposure to COVID-19 and acute stress, as well as between IU and acute stress. This means that the influences of both media exposure to COVID-19 and IU on acute stress got weaker when individuals had higher levels of PSS.
First, we found that PSS could moderate the relation between media exposure to COVID-19 and acute stress. As the stress-buffering model (18) suggests, PSS could buffer individuals from the impact of negative situations. Thus, people with high levels of PSS tend to perceive warmth, and get love and help from their family and friends when they encounter stressful life events (89, 102). These supports can contribute to enhancing positive mental resources and self-efficacy to cope with adversity effectively (77). Accordingly, they are less likely to experience acute stress compared with people with low levels of PSS, when indirectly exposing to stressful events. Consistent with previous studies (74, 76, 77), our findings indicated that PSS could be regarded as a protective factor to promote the positive development of mental health, and to help individuals flexibly adapt to adversity. As the media exposure to COVID-19 prolonged, people could suffer continuously increasing acute stress. In this situation, social support is an important protective resource to produce beneficial psychosocial changes and attenuate the detrimental effects of pandemic-related media exposure on acute stress.
Just as PSS could buffer the negative effects of pandemic-related media exposure on acute stress, PSS also moderated the relation between IU and acute stress. The result supported the stress-buffering model and the risk-buffering hypothesis (18, 68), and further indicated that PSS was a critical protective factor in mitigating the passive effects of personal risk factors on mental health. Similarly, this finding was in line with previous research, suggesting that PSS could buffer the negative effects of personal risk factors (70, 71). Therefore, PSS could to some extent protect the public from a series of adverse impacts caused by IU during the COVID-19 outbreak. This means that although IU could produce negative influences on mental health, the individuals who perceived more social support from their families and friends would be less affected by IU during the COVID-19 pandemic. Additionally, individuals with high levels of social support could take full use of coping strategies to deal with psychological distress (78, 79, 103), thus contributing to reducing their vulnerability to acute stress. Therefore, PSS acted as a stress-buffering factor in the second link of the mediation chain.
Contrary to our hypothesis, PSS did not moderate the link between media exposure to COVID-19 and IU. One possible explanation is that the influence of pandemic-related media exposure on IU is direct, fast and stable, and this process is less susceptible to external factors. Hence, more media exposure to COVID-19 was associated with more serious IU regardless of the level of PSS. Meanwhile, this result also revealed that PSS may not always act as a protective factor to reduce IU in uncertain conditions. Some prior studies supported this view of point as well (104, 105). Therefore, further studies are needed to better clarify the role of PSS in the relation between media exposure and IU following stressful events.
There are several limitations that should be noted. First, the self-report method limited the validity of the data due to subjective reporting bias. Thus, future research could take various measures to obtain more objective and comprehensive information. Second, we collected data in a shorter timeframe, and no assessments occurred during the follow-up, which may prevent us from detecting the changes of the relationships between variables over time. In future research, we could collect data at different stages of the pandemic to examine the temporal stability of these relationships. Third, we only examined the impacts of overall media exposure to pandemic on acute stress, and did not distinguish different media contents or types. Future studies should further explore the associations between different media contents or types and acute stress responses. Fourth, the present study focused on the passive impacts of pandemic-related media exposure on mental health, but neglected its positive effects. Future research could explore the positive implications of media exposure following public health events. Last, given that the COVID-19 pandemic is not a typical traumatic event, the application of the SASRQ in current study may be limited. Thus, further studies are needed to explore the applicability of the SASRQ in the pandemic-related events.
Despite these limitations, the current study has some theoretical and practical implications. First, this study further extends previous research by confirming the mediating role of IU and the moderating role of PSS. This could contribute to a better understanding of how and when pandemic-related media exposure can influence acute stress. Second, our findings revealed that PSS could help protect individuals from the development of acute stress related to IU. This indicates that it is critical to empower social support networks and minimize uncertain situations for the public, thereby reducing their acute stress responses. Third, our study confirmed the negative impacts of media exposure to pandemic, which could remind the public that appropriate use of media is necessary to maintain psychological health during the pandemic. Similarly, governments and relevant agencies should consider implementing the effective prevention and intervention to reduce negative psychological effects following traumatic events.
In summary, this study found that increased media exposure to COVID-19 was associated with higher acute stress during the COVID-19 outbreak in China. This association was partially mediated by IU. In particular, increased media exposure to COVID-19 was associated with higher IU, which in turned was associated with higher acute stress. Moreover, PSS can buffer the relationships between media exposure to COVID-19 and acute stress, as well as between IU and acute stress. Specifically, the effect of media exposure to COVID-19 on acute stress was stronger for individuals with low levels of PSS. Similarly, the effect of IU on acute stress was stronger for individuals with low levels of PSS.
The original contributions presented in the study are included in the article/Supplementary Files, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by the Ethical Committee of Guizhou Normal University. All participants provided electronic informed consent prior to their participation.
XH designed the research and wrote up the manuscript. YZ analyzed data and wrote up the original draft. MC performed the research. JZ designed the structure and performed the calculations. WZ reviewed literature and revised manuscript. YL reviewed manuscript and supervised the project. All authors contributed to the article and approved the submitted version.
This work was supported by the Sichuan Research Center of Applied Psychology Chengdu Medical College (CSXL-202A17), the Primary Health Development Research Center of Sichuan Province (SWFZ20-C-063) and the School Fund of Chengdu Medical College (CYS19-05).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2020.613368/full#supplementary-material
1. Chan JF, Yuan S, Kok K-H, To KK, Chu H, Yang J, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. (2020) 395:514–23. doi: 10.1016/S0140-6736(20)30154-9
2. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. Int J Env Res Pub Health. (2020) 17:1729. doi: 10.3390/ijerph17051729
3. Tang F, Liang J, Zhang H, Kelifa MM, He Q, Wang P. COVID-19 related depression and anxiety among quarantined respondents. Psychol Health. (2020) 35:1782410. doi: 10.1080/08870446.2020.1782410
4. Cheng VCC, Wong SC, Chuan VWM, So SYC, Chen JHK, et al. The role of community-wide wearing of face mask for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. J Infect. (2020) 81:107–14. doi: 10.1016/j.jinf.2020.04.024
5. Chao M, Xue D, Liu T, Yang H, Hall BJ. Media use and acute psychological outcomes during COVID-19 outbreak in China. J Anxiety Disord. (2020) 74:102248. doi: 10.1016/j.janxdis.2020.102248
6. Garfin DR, Silver RC, Holman EA. The novel coronavirus (COVID-2019) outbreak: amplification of public health consequences by media exposure. Health Psychol. (2020) 39:355–7. doi: 10.1037/hea0000875
7. Yeung NCY, Lau JTF, Yu NX, Zhang J, Xu Z, Choi KC. Media exposure related to the 2008 Sichuan Earthquake predicted probable PTSD among Chinese adolescents in Kunming, China: A longitudinal study. Psychol Trauma US. (2016) 10:253–62. doi: 10.1037/tra0000121
8. Bernstein KT, Ahern J, Tracy M, Boscarino JA, Vlahov D, Galea S. Television watching and the risk of incident probable posttraumatic stress disorder: a prospective evaluation. J Nerv Ment Dis. (2007) 195:41–7. doi: 10.1097/01.nmd.0000244784.36745.a5
9. Holman EA, Garfin DR, Lubens P, Silver RC. Media exposure to collective trauma, mental health, and functioning: does it matter what you see?. Clin Psychol Sci. (2019) 8:216770261985830. doi: 10.1177/2167702619858300
10. Thompson RR, Jones NM, Holman EA, Silver RC. Media exposure to mass violence events can fuel a cycle of distress. Sci Adv. (2019) 5:eaav3502. doi: 10.1126/sciadv.aav3502
11. Elhai JD, Yang H, Mckay D, Asmundson GJG. COVID-19 anxiety symptoms associated with problematic smartphone use severity in Chinese adults. J Anxiety Disord. (2020) 274:567–82. doi: 10.1016/j.jad.2020.05.080
12. Thompson RR, Garfin DR, Holman EA, Silver RC. Distress, worry, and functioning following a global health crisis: a national study of Americans' responses to Ebola. Clin Psychol Sci. (2017) 5:513–21. doi: 10.1177/2167702617692030
13. Holman EA, Garfin DR, Silver RC. Media's role in broadcasting acute stress following the Boston Marathon bombings. PNAS. (2014) 111:93–8. doi: 10.1073/pnas.1316265110
14. Hal BJ, Xiong YX, Yip PSY, Lao CK, Shi W, Sou EKL, et al. The association between disaster exposure and media use on post-traumatic stress disorder following typhoon Hato in Macao, China. Eur J Psychotraumato. (2019) 10:1–12. doi: 10.1080/20008198.2018.1558709
15. Boelen PA, Reijntjes A, Carleton RN. Intolerance of uncertainty and adult separation anxiety. Cogn Behav Therapy. (2014) 43:133–44. doi: 10.1080/16506073.2014.888755
16. Carleton RN, Mulvogue MK, Thibodeau MA, McCabe RE, Antony MM, Asmundson GJ. Increasingly certain about uncertainty: intolerance of uncertainty across anxiety and depression. J Anxiety Disord. (2012) 26:468–79. doi: 10.1016/j.janxdis.2012.01.011
17. Liao YH, Wei M. Intolerance of uncertainty, depression, and anxiety: the moderating and mediating roles of rumination. J Clin Psychol. (2011) 67:1220–39. doi: 10.1002/jclp.20846
18. Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. (1985) 98:310–57. doi: 10.1037/0033-2909.98.2.310
19. Bokszczanin A. Social support provided by adolescents following a disaster and perceived social support, sense of community at school, and proactive coping. Anxiety Stress Coping. (2012) 25:575–92. doi: 10.1080/10615806.2011.622374
20. Neria Y, Besser A, Kiper D, Westphal M. A longitudinal study of posttraumatic stress disorder, depression, and generalized anxiety disorder in Israeli civilians exposed to war trauma. J Trauma Stress. (2010) 23:322–30. doi: 10.1002/jts.20522
21. Simşir Z, Dilmaç B. Predictive relationship between war posttraumatic growth, values, and perceived social support. Illness Crisis Loss. (2018) 26:1–17. doi: 10.1177/1054137318788655
22. Calhoun LG, Tedeschi RG. The foundations of posttraumatic growth: an expanded framework. In: Calhoun LG, Tedeschi RG, editors. Handbook of Posttraumatic Growth. Mahwah, NJ: Lawrence Erlbaum Associates (2006). p. 1–23.
23. Ben-Ezra M, Palgi Y, Essar N, Sofer H, Haber Y. Acute stress symptoms, dissociation, and depression among rescue personnel 24 hours after the bet-yehoshua train crash: the effects of exposure to dead bodies. Prehosp Disaster Med. (2008) 23:461–5. doi: 10.1017/S1049023X00006208
24. Freedy JR, Resnick HS, Kilpatrick DG. Conceptual framework for evaluating disaster impact: implications for clinical intervention In: Austin LS, editor. Responding to Disaster: A Guide for Mental Health Professionals. Washington, DC: American Psychiatric Press (1992). p. 6–14.
25. Silver RC, Garfin DR. Coping with disasters. In: Norcross JC, VandenBos GR, Freedheim DK, Pole N, editors. APA Handbook of Clinical Psychology: Psychopathology and Health. Washington, DC: American Psychological Association (2016). p. 597–611.
26. van der Meer TGLA, Verhoeven P. Public framing organizational crisis situations: social media versus news media. Public Relat Rev. (2013) 39:229–31. doi: 10.1016/j.pubrev.2012.12.001
27. Hopwood T, Schutte N. Psychological outcomes in reaction to media exposure to disasters and largescale violence: a meta-analysis. Psychol Violence. (2017) 7:316–27. doi: 10.1037/vio0000056
28. Pappas G, Kiriaze IJ, Giannakis P, Falagas ME. Psychosocial consequences of infectious diseases. Clin Microbiol Infect. (2009) 15:743–7. doi: 10.1111/j.1469-0691.2009.02947.x
29. Silver RC, Holman EA, Andersen JP, Poulin M, McIntosh DN, Gil-Rivas V. Mental- and physical-health effects of acute exposure to media images of the September 11, 2001, attacks and the Iraq War. Psychol Sci. (2013) 24:1623–34. doi: 10.1177/0956797612460406
30. Goodwin R, Palgi Y, Lavenda O, Hamama-Raz Y, Ben-Ezra M. Association between media use, acute stress disorder and psychological distress. Psychother Psychosom. (2015) 84:253–4. doi: 10.1159/000377706
31. Ye Z, Yang X, Zeng C, Wang Y, Shen Z, Li X, et al. Resilience, social support, and coping as mediators between COVID-19-related stressful experiences and acute stress disorder among college students in China. Appl Psychol Health Well Being. (2020) 12:12211. doi: 10.1111/aphw.12211
32. Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. (2020) 395:e37–8. doi: 10.1016/S0140-6736(20)30309-3
33. Holman EA, Thompson RR, Garfin DR, Silver RC. The unfolding COVID-19 pandemic: a probability-based, nationally representative study of mental health in the U.S. Sci Adv. (2020) 6:eabd5390. doi: 10.1126/sciadv.abd5390
34. Zhou X, Yao B. Social support and acute stress symptoms (ASSs) during the COVID-19 outbreak: deciphering the roles of psychological needs and sense of control. Eur J Psychotraumato. (2020) 11:1779494. doi: 10.1080/20008198.2020.1779494
35. Shi L, Lu Z, Que J, Huang X, Liu L, Ran M, et al. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw Open. (2020) 3:e2014053. doi: 10.1001/jamanetworkopen.2020.14053
36. Zysberg L, Zisberg A. Days of worry: emotional intelligence and social support mediate worry in the COVID-19 pandemic. J Health Psychol. (2020) 25:1–10. doi: 10.1177/1359105320949935
37. Ferrara E, Yang Z. Measuring emotional contagion in social media. PLoS ONE. (2015) 10:e0142390. doi: 10.1371/journal.pone.0142390
38. Du J, Fan X, Feng T. Multiple emotional contagions in service encounters. J Acad Market Sci. (2011) 39:449–66. doi: 10.1007/s11747-010-0210-9
39. Vasterman P, Yzermans CJ, Dirkzwager AJE. The role of the media and media hypes in the aftermath of disasters. Epidemiol Rev. (2005) 27:107–14. doi: 10.1093/epirev/mxi002
40. Zakout YM, Alreshidi FS, Elsaid RM, Ahmed HG. The magnitude of COVID-19 related stress, anxiety and depression associated with intense mass media coverage in Saudi Arabi. AIMS Public Health. (2020) 7:664–78. doi: 10.3934/publichealth.2020052
41. Yao H. The more exposure to media information about COVID-19, the more distressed you will feel. Brain Behav Immun. (2020) 87:167–9. doi: 10.1016/j.bbi.2020.05.031
42. Morriss J, McSorley E. Intolerance of uncertainty is associated with reduced attentional inhibition in the absence of direct threat. Behav Res Ther. (2019) 118:1–6. doi: 10.1016/j.brat.2019.03.011
43. Freeston M, Rhéaume J, Letarte H, Dugas MJ, Ladouceur R. Why do people worry? Pers Indiv Differ. (1994) 17:791–802. doi: 10.1016/0191-8869(94)90048-5
44. Boyle MP, Schmierbach M, Armstrong CL, McLeod DM, Shah DV, Pan Z. Information seeking and emotional reactions to the September 11 terrorist attacks. J Mass Commun Q. (2004) 81:155–67. doi: 10.1177/107769900408100111
45. Carleton RN. Into the unknown: a review and synthesis of contemporary models involving uncertainty. J Anxiety Disord. (2016) 39:30–43. doi: 10.1016/j.janxdis.2016.02.007
46. Carleton RN, Desgagné G, Krakauer R, Hong RY. Increasing intolerance of uncertainty over time: the potential influence of increasing connectivity. Cogn Behav Therapy. (2019) 48:121–36. doi: 10.1080/16506073.2018.1476580
47. Rosen NO, Knäuper B. A little uncertainty goes a long way: state and trait differences in uncertainty interact to increase information seeking but also increase worry. Health Commun. (2009) 24:228–38. doi: 10.1080/10410230902804125
48. Mosca O, Lauriola M, Carleton RN. Intolerance of uncertainty: a temporary experimental induction procedure. PLoS ONE. (2016) 11:e0155130. doi: 10.1371/journal.pone.0155130
49. Ladouceur R, Gosselin P, Dugas MJ. Experimental manipulation of intolerance of uncertainty: a study of a theoretical model of worry. Behav Res Ther. (2000) 38:933–41. doi: 10.1016/S0005-7967(99)00133-3
50. Rosen NO, Knäuper B, Sammut J. Do individual differences in intolerance of uncertainty affect health monitoring?. Psychol Health. (2007) 22:413–30. doi: 10.1080/14768320600941038
51. Dugas MJ, Savard P, Gaudet A, Turcotte J, Laugesen N, Robichaud M, et al. Can the components of a cognitive model predict the severity of generalized anxiety disorder? Behav Ther. (2007) 38:169–78. doi: 10.1016/j.beth.2006.07.002
52. Lind C, Boschen MJ. Intolerance of uncertainty mediates the relationship between responsibility beliefs and compulsive checking. J Anxiety Disord. (2009) 23:1047–52. doi: 10.1016/j.janxdis.2009.07.005
53. Yook K, Kim K-H, Suh SY, Lee KS. Intolerance of uncertainty, worry, and rumination in major depressive disorder and generalized anxiety disorder. J Anxiety Disord. (2010) 24:623–8. doi: 10.1016/j.janxdis.2010.04.003
54. Dar KA, Iqbal N, Mushtaq A. Intolerance of uncertainty, depression, and anxiety: examining the indirect and moderating effects of worry. Asian J Psychiatr. (2017) 29:129–33. doi: 10.1016/j.ajp.2017.04.017
55. Song Y, Li B. Locus of control and trait anxiety in aged adults: the mediating effect of intolerance of uncertainty. Int J Ment Health Addict. (2017) 17:1–9. doi: 10.1007/s11469-017-9860-x
56. Bardeen JR, Fergus TA, Wu KD. The interactive effect of worry and intolerance of uncertainty on posttraumatic stress symptoms. Cognitive Ther Res. (2013) 37:742–51. doi: 10.1007/s10608-012-9512-1
57. Fetzner MG, Horswill SC, Boelen PA, Carleton RN. Intolerance of uncertainty and PTSD symptoms: exploring the construct relationship in a community sample with a heterogeneous trauma history. Cognitive Ther Res. (2013) 37:725–34. doi: 10.1007/s10608-013-9531-6
58. Oglesby ME, Boffa JW, Short NA, Raines AM, Schmidt NB. Intolerance of uncertainty as a predictor of post-traumatic stress symptoms following a traumatic event. J Anxiety Disord. (2016) 41:82–7. doi: 10.1016/j.janxdis.2016.01.005
59. Dugas MJ, Schwartz A, Francis K. Intolerance of uncertainty, worry and depression. Cognitive Ther Res. (2004) 28:835–42. doi: 10.1007/s10608-004-0669-0
60. Barrera M. Distinctions between social support concepts, measures, and models. Am J Commun Psychol. (1986) 14:413–45. doi: 10.1007/BF00922627
61. Abbas J, Aqeel M, Abbas J, Shaher B, A J, Sundas J, et al. The moderating role of social support for marital adjustment, depression, anxiety, and stress: evidence from Pakistani working and nonworking women. J Anxiety Disord. (2019) 244:231–8. doi: 10.1016/j.jad.2018.07.071
62. Falgares G, Gioco AL, Verrocchio MC, Marchetti D. Anxiety and depression among adult amputees: the role of attachment insecurity, coping strategies and social support. Psychol Health Med. (2018) 24:281–93. doi: 10.1080/13548506.2018.1529324
63. Roohafza HR, Afshar H, Keshteli AH, Mohammadi N, Feizi A, Taslimi M, et al. What's the role of perceived social support and coping styles in depression and anxiety? J Res Med Sci. (2014) 19:944–9.
64. Rueger SY, Malecki CK, Pyun Y, Aycock C, Coyle S. A meta-analytic review of the association between perceived social support and depression in childhood and adolescence. Psychol Bull. (2016) 142:1017–67. doi: 10.1037/bul0000058
65. Rueger SY, Malecki CK, Demaray MK. Relationship between multiple sources of perceived social support and psychological and academic adjustment in early adolescence: comparisons across gender. J Youth Adolescence. (2010) 39:47–61. doi: 10.1007/s10964-008-9368-6
66. Dar KA, Iqbal N, Prakash A, Paul MA. PTSD and depression in adult survivors of flood fury in Kashmir: the payoffs of social support. Psychiat Res. (2018) 261:449–55. doi: 10.1016/j.psychres.2018.01.023
67. McGuire AP, Gauthier JM, Anderson LM, Hollingsworth DW, Tracy M, Galea S, et al. Social support moderates effects of natural disaster exposure on depression and posttraumatic stress disorder symptoms: effects for displaced and nondisplaced residents. J Trauma Stress. (2018) 31:223–33. doi: 10.1002/jts.22270
68. Hollister-Wagner GH, Foshee VA, Jackson C. Adolescent aggression: models of resiliency. J Appl Soc Psychol. (2001) 31:445–66. doi: 10.1111/j.1559-1816.2001.tb02050.x
69. Xia Z, Dan Z, Menglian W, Yang Y, Hui X, Yuqin L, et al. Loneliness and depression symptoms among the elderly in nursing homes: a moderated mediation model of resilience and social support. Psychiat Res. (2018) 268:143–51. doi: 10.1016/j.psychres.2018.07.011
70. Chan DW. Stress, self-efficacy, social support, and psychological distress among prospective Chinese teachers in Hong Kong. Educ Psychol. (2002) 22:557–69. doi: 10.1080/0144341022000023635
71. Xu J, Wei Y, Chen H. Social support as a moderator of the relationship between anxiety and depression: an empirical study with adult survivors of Wenchuan Earthquake. PLoS ONE. (2013) 8:e79045. doi: 10.1371/journal.pone.0079045
72. Fu L, Wang P, Zhao M, Xie X, Chen Y, Nie J, et al. Can emotion regulation difficulty lead to adolescent problematic smartphone use? A moderated mediation model of depression and perceived social support. Child Youth Serv Rev. (2019) 108:104660. doi: 10.1016/j.childyouth.2019.104660
73. Li Y, Li D, Li X, Zhou Y, Sun W, Wang Y, et al. Cyber victimization and adolescent depression: the mediating role of psychological insecurity and the moderating role of perceived social support. Child Youth Serv Rev. (2018) 94:10–9. doi: 10.1016/j.childyouth.2018.09.027
74. Han KM, Park JY, Park HE, An SR, Lee EH, Yoon HK, et al. Social support moderates association between posttraumatic growth and trauma-related psychopathologies among victims of the Sewol Ferry Disaster. Psychiat Res. (2019) 272:507–14. doi: 10.1016/j.psychres.2018.12.168
75. Ouyang C, Li D, Li X, Xiao J, Wang Y. Cyber victimization and tobacco and alcohol use among adolescents: a moderated mediation model. Child Youth Serv Rev. (2020) 114:105041. doi: 10.1016/j.childyouth.2020.105041
76. Schubert CF, Schmidt U, Rosner R. Posttraumatic growth in populations with posttraumatic stress disorder: a systematic review on growth-related psychological constructs and biological variables. Clin Psychol Psychother. (2016) 23:469–86. doi: 10.1002/cpp.1985
77. Ren Y, Li M. Influence of physical exercise on social anxiety of left-behind children in rural areas in China: the mediator and moderator role of perceived social support. J Affect Disorders. (2020) 266:2232–29. doi: 10.1016/j.jad.2020.01.152
78. Holt MK, Espelage DL. Perceived social support among bullies, victims, and bully-victims. J Youth Adolescence. (2007) 36:984–94. doi: 10.1007/s10964-006-9153-3
79. Cavanaugh AM, Buehler C. Adolescent loneliness and social anxiety: the role of multiple sources of support. J Soc Pers Relat. (2016) 33:149–70. doi: 10.1177/0265407514567837
80. Carleton RN, Norton PJ, Asmundson GJG. Fearing the unknown: a short version of the intolerance of uncertainty scale. J Anxiety Disord. (2007) 21:105–17. doi: 10.1016/j.janxdis.2006.03.014
81. Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. J Pers Assess. (1988) 52:30–41. doi: 10.1207/s15327752jpa5201_2
82. Cardeña E, Koopman C, Classen C, Waelde LC, Spiegel D. Psychometric properties of the stanford acute stress reaction questionnaire (SASRQ): a valid and reliable measure of acute stress. J Trauma Stress. (2000) 13:719–34. doi: 10.1023/A:1007822603186
83. Jia FJ, Hou CL. Assessment Manual of Psychological Stress and Trauma. Beijing: People's Medical Publishing House (2009).
84. Li Y, Chen C. Application of stanford acute stress reaction questionnaire in trauma. CHS J Rehabil Theory Pract. (2015) 11:717–22. doi: 10.3969/j.issn.1006-9771
85. Hu X, Du Q, Luo J, Song L, Tian F, Zeng R, et al. Acute stress response among rescued miners in Wangjialing coal mine disaster. CHS Ment Health J. (2011) 25:814–8.
86. Liu P, Zhou J, Li A, Li Y, Zhang J, Chen J. Acute stress reaction and its influencing factors in patients with brain injury. CHS J Gerontology. (2019) 39:3069–72. doi: 10.3969/j.issn.1005-9202.2019.12.074
87. Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York, NY: Guilford Publications (2017).
88. Baschnagel JS, Gudmundsdottir B, Hawk LW, Beck JG. Post-trauma symptoms following indirect exposure to the September 11th terrorist attacks: the predictive role of dispositional coping. J Anxiety Disord. (2009) 23:915–22. doi: 10.1016/j.janxdis.2009.05.005
89. Ford JD, Adams ML, Dailey WF. Psychological and health problems in a geographically proximate population time-sampled continuously for three months after the September 11th, 2001 terrorist incidents. Anxiety Stress Coping. (2007) 20:129–46. doi: 10.1080/10615800701303215
90. Zhou H, Long L. Statistical remedies for common method biases. Adv Psychol Sci. (2004) 12:942–50. doi: 10.3969/j.issn.1671-3710.2004.06.018
91. Zmete E, Pak M. The relationship between anxiety levels and perceived social support during the pandemic of COVID-19 in Turkey. Soc Work Public Health. (2020) 35:603–16. doi: 10.1080/19371918.2020.1808144
92. Xiao X, Zhu X, Fu S, Hu Y, Li X, Xiao J. Psychological impact of healthcare workers in China during COVID-19 pneumonia epidemic: a multi-center cross-sectional survey investigation. J Affect Disord. (2020) 274:405–10. doi: 10.1016/j.jad.2020.05.081
93. Bourne C, Mackay CE, Holmes EA. The neural basis of flashback formation: the impact of viewing trauma. Psychol Med. (2013) 43:1521–32. doi: 10.1017/S0033291712002358
94. Watkins ER. Constructive and unconstructive repetitive thought. Psychol Bull. (2008) 134:163–206. doi: 10.1037/0033-2909.134.2.163
95. Brosschot JF. Markers of chronic stress: prolonged physiological activation and (un)conscious perseverative cognition. Neurosci Biobehav Rev. (2010) 35:46–50. doi: 10.1016/j.neubiorev.2010.01.004
96. Gerin W, Zawadzki MJ, Brosschot JF, Thayer JF, Christenfeld NJ, Campbell TS, et al. Rumination as a mediator of chronic stress effects on hypertension: a causal model. Int J Hypertens. (2012) 2012:453–65. doi: 10.1155/2012/453465
97. Reuther ET, Davis TE, Rudy BM, Jenkins WS, Whiting SE, May AC. Intolerance of uncertainty as a mediator of the relationship between perfectionism and obsessive-compulsive symptom severity. Depress Anxiety. (2013) 30:773–7. doi: 10.1002/da.22100
98. Carleton RN. The intolerance of uncertainty construct in the context of anxiety disorders: theoretical and practical perspectives. Expert Rev Neurother. (2012) 12:937–47. doi: 10.1586/ern.12.82
99. Oglesby ME, Gibby BA, Mathes BM, Short NA, Schmidt NB. Intolerance of uncertainty and post-traumatic stress symptoms: an investigation within a treatment seeking trauma-exposed sample. Compr Psychiat. (2017) 72:34–40. doi: 10.1016/j.comppsych.2016.08.011
100. Dugas MJ, Hedayati M, Karavidas A, Buhr K, Francis K, Phillips NA. Intolerance of uncertainty and information processing: evidence of biased recall and interpretations. Cognitive Ther Res. (2005) 29:57–70. doi: 10.1007/s10608-005-1648-9
101. Chen JT-H, Lovibond PF. Intolerance of uncertainty is associated with increased threat appraisal and negative affect under ambiguity but not uncertainty. Behav Ther. (2016) 47:42–53. doi: 10.1016/j.beth.2015.09.004
102. Wang P, Xie X, Wang X, Wang X, Zhao F, Chu X, et al. The need to belong and adolescent authentic self-presentation on SNSs: a moderated mediation model involving FoMO and perceived social support. Pers Indiv Differ. (2018) 128:133–8. doi: 10.1016/j.paid.2018.02.035
103. Prati G, Pietrantoni L. Optimism, social support, and coping strategies as factors contributing to posttraumatic growth: a meta-analysis. J Loss Trauma. (2009) 14:364–88. doi: 10.1080/15325020902724271
104. Li Q, Chi P, Hall BJ, Wu Q, Du H. Job stress and depressive symptoms among migrant workers in macau: a moderated mediation model of self-esteem and perceived social support. PsyCh J. (2019) 8:298. doi: 10.1002/pchj.298
Keywords: COVID-19, media exposure, acute stress, intolerance of uncertainty, perceived social support
Citation: He X, Zhang Y, Chen M, Zhang J, Zou W and Luo Y (2021) Media Exposure to COVID-19 Predicted Acute Stress: A Moderated Mediation Model of Intolerance of Uncertainty and Perceived Social Support. Front. Psychiatry 11:613368. doi: 10.3389/fpsyt.2020.613368
Received: 02 October 2020; Accepted: 09 December 2020;
Published: 10 February 2021.
Edited by:
Nancy Xiaonan Yu, City University of Hong Kong, Hong KongReviewed by:
Wei Wang, Norwegian University of Science and Technology, NorwayCopyright © 2021 He, Zhang, Chen, Zhang, Zou and Luo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yu Luo, eXVsdW9AZ3pudS5lZHUuY24=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.