- 1University of Washington, Seattle, WA, United States
- 2Washington University, St. Louis, MO, United States
- 3Department of Health Metrics Sciences, University of Washington, Seattle, WA, United States
- 4VA Ann Arbor Healthcare System, Ann Arbor, MI, United States
- 5Department of Psychology, University of California Los Angeles Life Sciences, Los Angeles, CA, United States
- 6United Nations International Children's Emergency Fund (UNICEF), New York, NY, United States
- 7New York University, New York, NY, United States
- 8Harvard T.H Chan School of Public Health, Harvard University, Cambridge, MA, United States
- 9Uppsala University, Uppsala, Sweden
- 10University of Michigan, Ann Arbor, MI, United States
- 11University of Nairobi, Nairobi, Kenya
- 12Amref Health Africa, Nairobi, Kenya
- 13University of Botswana, Gaborone, Botswana
Background: COVID-19 prevention and mitigation efforts were abrupt and challenging for most countries with the protracted lockdown straining socioeconomic activities. Marginalized groups and individuals are particularly vulnerable to adverse effects of the pandemic such as human rights abuses and violations which can lead to psychological distress. In this review, we focus on mental distress and disturbances that have emanated due to human rights restrictions and violations amidst the pandemic. We underscore how mental health is both directly impacted by the force of pandemic and by prevention and mitigation structures put in place to combat the disease.
Methods: We conducted a review of relevant studies examining human rights violations in COVID-19 response, with a focus on vulnerable populations, and its association with mental health and psychological well-being. We searched PubMed and Embase databases for studies between December 2019 to July 2020. Three reviewers evaluated the eligibility criteria and extracted data.
Results: Twenty-four studies were included in the systematic inquiry reporting on distress due to human rights violations. Unanimously, the studies found vulnerable populations to be at a high risk for mental distress. Limited mobility rights disproportionately harmed psychiatric patients, low-income individuals, and minorities who were at higher risk for self-harm and worsening mental health. Healthcare workers suffered negative mental health consequences due to stigma and lack of personal protective equipment and stigma. Other vulnerable groups such as the elderly, children, and refugees also experienced negative consequences.
Conclusions: This review emphasizes the need to uphold human rights and address long term mental health needs of populations that have suffered disproportionately during the pandemic. Countries can embed a proactive psychosocial response to medical management as well as in existing prevention strategies. International human rights guidelines are useful in this direction but an emphasis should be placed on strengthening rights informed psychosocial response with specific strategies to enhance mental health in the long-term. We underscore that various fundamental human rights are interdependent and therefore undermining one leads to a poor impact on the others. We strongly recommend global efforts toward focusing both on minimizing fatalities, protecting human rights, and promoting long term mental well-being.
Introduction
On March 11, 2020, the World Health Organization (WHO) declared a public health emergency of international concern in response the global pandemic of the novel Coronavirus disease (SARS-COV-2). To reduce the spread of the virus, countries have implemented urgent emergency health measures. These measures include stay at home orders and the closure of schools which have led people to reorganize their lives and necessitated changes in livelihood and health services (1, 2).
In responding to public health emergencies, governmental authorities have to navigate the delicate balance between protecting the public's health and safeguarding their inherent human rights including education, freedom of movement, and access to health care. Measures to prevent the spread of infectious diseases are not zero-sum tradeoffs and can decrease fatalities but also increase suffering if human rights are not respected. As such, while being protected from clear public health threats, many people, especially vulnerable populations, may be deprived of their inherent human rights (3). We are in favor of using science to achieve globally shared objectives, but it is important to consider all sources of evidence in addition to the infectious diseases realm in the contexts of known tradeoffs—between lockdown and freedom to assert social and economic freedom. We recommend nations focus both on minimizing fatalities and protecting human rights. The United Nations (UN) defines human rights as: “…fundamental to all human beings, regardless of race, sex, nationality, ethnicity, language, religion, or any other status. These rights include the right to life and liberty, freedom from slavery and torture, freedom of opinion and expression, the right to work and education, and many more such as a safe & clean environment have become important to uphold. Everyone is entitled to these rights, without discrimination or threat of any kind” (4).
Within bioethics, the needs of different populations marked as vulnerable have even more urgent and impactful implications because applying the human rights lens focuses on highlighting and protecting the rights withing vulnerable populations. Vulnerable populations are defined as “groups and communities at a higher risk for poor health as a result of the barriers they experience to social, economic, political and environmental resources, as well as limitations due to illness or disability” (5). The principle of vulnerability is pertinent in the context of global disasters. It emphasizes ethical discourse on ameliorating the conditions that produce vulnerability, rather than on emergency actions focused on saving lives (6). Vulnerability is a global phenomenon but in the context of the pandemic it is exacerbated in many societies where inequality and access to basic freedoms is restricted. In lower- and middle-income countries (LMICs) such freedoms can easily be impacted due to existing system challenges and adverse social determinants of health. In High Income Countries (HICs), similar challenges surface during pandemic, and vulnerable groups have also been systematically marginalized.
Mental health is integral, closely related to, and dependent upon the realization of human rights (7). In the context of the coronavirus disease 2019 (COVID-19) pandemic, reports highlight gross undermining of mental health and violations of individual civil liberties and fundamental rights such as mobility rights, access to accurate information, access to proper protection for health workers, right to education, and discrimination against marginalized populations (8). Human rights protection and mental health needs are not always adequately integrated into emergency response policy and management. The evidence highlights that vulnerable populations, including those living in abusive families, individual with disabilities, children, elderly, domestic caregivers, health care workers (HCWs), and ethnic and marginalized communities, are especially at risk for mental health distress (9–11) with the psychological needs of these populations not likely to be fulfilled without meaningful legislation and intervention (9, 12). There have been long standing concerns within the field of mental health that the human rights of psychiatric populations and individuals and communities under psychosocial distress tend to be ignored. From mental health policy perspectives, how human right policies and practices is integrated in emergency response policy and management has not been focused. There are several aspects of vulnerability, disability, coerciveness of treatment and system level oppression that have been key concerns. In this review we focus on rights associated violations and grievances that would potentiate further mental distress and long-term harm to critical subsections of at-risk populations that will be negatively impacted.
Given the current evidence, we believe that it is important to broaden our understanding of what rights violations entail in the context of this global pandemic and learn critical lessons in mitigation and prevention of these abusive and unethical situations and mental distress emanating from these. As the first step to inform global human rights policy and guidelines, and practices for better managing a global pandemic, it is important to understand and summarize current knowledge and practices. The focus of this review therefore is to collate evidence on human rights abuses and violations and resultant mental and behavioral health outcomes of different populations, especially those known to be at high risk or have greater vulnerabilities warranting additional mitigation, prevention, and treatment approaches during COVID-19 (13). The two specific objectives are:
1) Scoping of prominent rights-based issues with a focus on basic human rights violations during the COVID-19 pandemic and its association with mental and behavioral health of populations. In this regard, people from different ages, regardless of their gender, ethnicity, status (i.e., orphans or refugees), profession, or religion, will be included.
2) Appraisal of binding agreements and global or national policies that enforce human rights during emergencies and developed for this pandemic that are designed to strengthen human rights and well-being of vulnerable populations.
Methods
A rapid literature review was conducted using published data sources on human rights violations and resulting psychological impact on vulnerable populations during COVID-19. For this review, we used the following working definition of rapid review “…a type of knowledge synthesis in which components of the systematic review process are simplified or omitted to produce information in a short period of time” (14, 15).
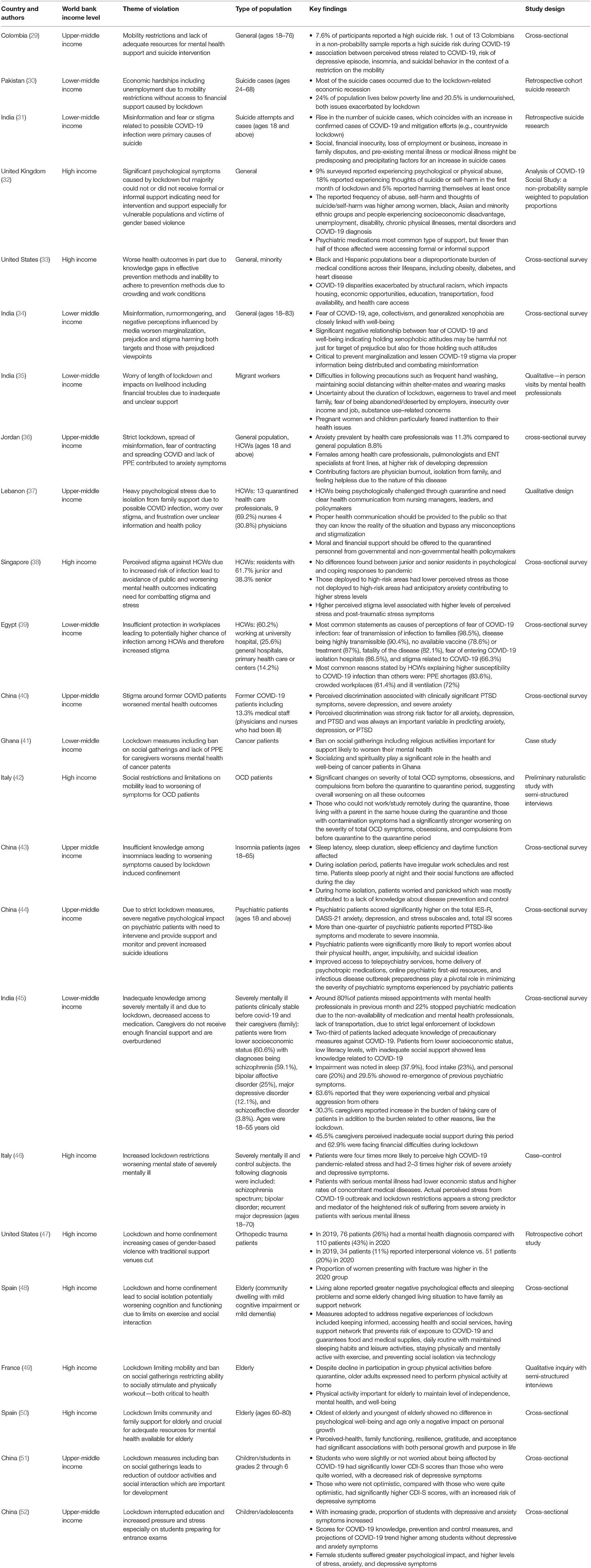
Literature that focused on human rights and related violations, health stigma and discrimination in the context of the pandemic was prioritized. For mental health, literature related to both generic factors such as quality of life, well-being and condition-specific aspects such as symptoms due to human rights abuses were included. The search strategy involved locating relevant concepts in PubMed and Embase databases. Relevant data was extracted and summarized into five main themes: (1) Mobility rights, quarantine, and lockdown, (2) Shortage of supplies and equipment for HCWs, (3) Child rights, (4) Elderly's rights, and (5) Disproportionate impacts on minority rights and psychiatric patients.
A search was conducted in July 2020 for studies published during December 2019 to July 2020 with assistance from a health science librarian. After eliminating duplicates, we screened titles and abstracts (MR and MK) and did a secondary screening of full-text articles using the inclusion/exclusion criteria and extracted data (MR, RA, and MK). A cursory search of Google Scholar was also conducted to identify any possible missed studies that meet the inclusion criteria. All authors read and commented on human rights and mental health related literature and their associations. We have reported findings following the PRISMA guidelines (16).
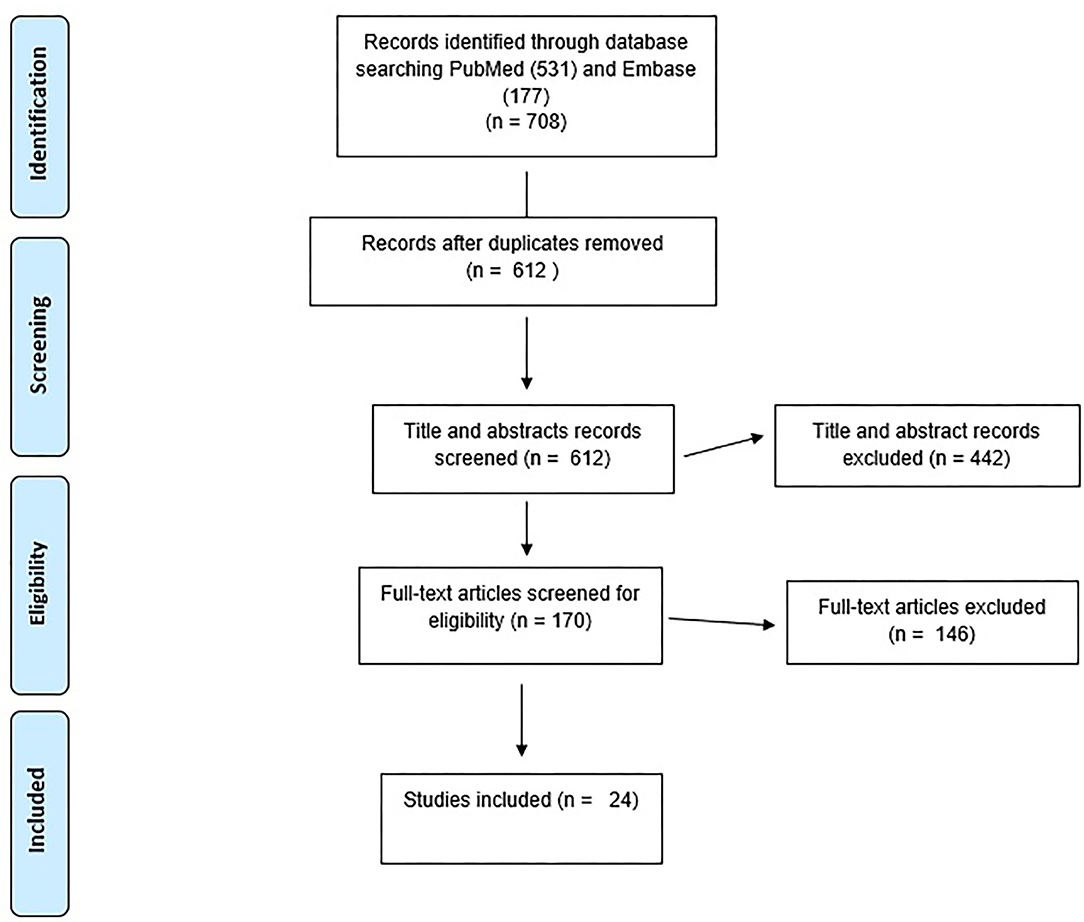
Studies were included if they described an empirically based (data-driven either qualitatively or quantitatively) assessment of human rights violations, social stigma and discriminatory behaviors against people of certain ethnic backgrounds, HCWs, and anyone perceived to have been in contact with the virus. It also included studies that reported mental, social, and behavioral health outcomes of the violations according to DSM/ICD classifications diagnostic categories or as ascertained using psychometric instruments. Furthermore, protocols and reports including guidelines by international agencies vetted by scientific and peer reviewers which address one of the primary outcomes were included. Studies were excluded if they tested one of the primary outcomes of interest without mentioning the association between them or the association between the constructs of interest or if those were not assessed in a data-driven approach. Systematic reviews, meta-analysis or scoping reviews were excluded if the analysis did not include one of the primary outcomes. Studies that are not peer-reviewed articles or not published in the English language were also excluded. Figure 1 shows the flowchart diagram of the selection of articles.
Results
A total of 24 studies were included in this review (see Figure 1). There was a wide variation in the included studies between methodology, the study design, and location. These studies represented findings from 14 countries (six from HICs and eight LMICs). Based on their methodological approach, 14 used a cross-sectional study design, three were observational studies, two were case studies and the rest had differing study designs such as two being case controls.
Of the empirically based studies, five studies examined impacts of limited mobility rights, due to quarantine and lockdown, on mental health; four studies examined impacts of lack of PPE or stigma on HCWs; and the rest examined impacts of COVID-19 such as violation of right to education, health care, and access, on special populations, including children, elderly, minorities, and psychiatric patients. The sections below highlighted key results in each area. Table 1 describes the characteristics for articles reviewed under each area (e.g., country, theme of violation, study population, design, and findings).
Mobility Rights, Quarantine, and Lockdown
According to the international human rights law, restrictions of mobility including lockdown or mandatory quarantine due to public health emergency must be carried out for a legitimate purpose, based on scientific evidence, of limited duration, and respectful of human dignity (53). Quarantines are successful at limiting the spread of infectious diseases, but they introduce the side effects of increasing people's risk for psychological impact including suicide and other behavioral symptoms.
In our review, three studies reported rise in suicide incidence in several countries due to mobility restriction and lockdown. In Colombia, a national-level lockdown increased the risk of suicide in vulnerable populations and among those with pre-existing predisposing factors such as emotional problems, financial troubles, and job loss (29). One out of 13 adult Colombians reported high suicide risk; people experiencing depressive episodes or poor sleep quality including insomnia, had a higher risk for suicidal behaviors than the general population. In Pakistan, most of the investigated suicide cases were carried out by individuals who were socially-economically impacted by economic turmoil and experiencing financial troubles caused by the lockdown (30). Similar findings were reported in India where suicide cases increased as COVID cases increased, especially among individuals with pre-existing mental illness and those in poor socio-economic conditions (31).
Mobility restrictions were also found to be correlated with poor mental and social well-being in developed countries. In Italy, lockdown restrictions mediated other mental and behavioral symptoms such as anxiety in patients with serious mental illness (46). In the United Kingdom, since the start of their national lockdown, 9% surveyed participants reported experiencing psychological or physical abuse during the lockdown (32). About, 18% reported experiencing thoughts of suicide or self-harm in the first month of lockdown and 5% reported harming themselves at least once since the start of the lockdown. Reported frequencies of abuse, self-harm, thoughts of suicide, and self-injurious behavior were higher among women, black, Asian and minority ethnic groups, people experiencing socioeconomic disadvantage, unemployment, disability, chronic physical illnesses, mental disorders and COVID-19 diagnosis. Furthermore, a study in the United States found an increased number of orthopedic trauma patients reporting a mental health diagnosis post-quarantine compared to pre-quarantine as well as an increased number of patients reporting interpersonal violence as the reason for their injury (47).
Shortage of Supplies and Equipment for HCWs
As part of the right to health, the International Covenant on Economic, Social and Cultural Rights obliged the governmental and health agencies to plan and optimize the use of personal protective equipment (PPE) among HCWs during public health emergencies such as COVID-19 (54, 55). This also includes providing them with appropriate training, education, and informational material that can prevent physical and mental harm from health care-associated infections.
According to the UNICEF and WHO, it is estimated that the majority of HCWs provide services and work in environments that lack basic infrastructure to support water, sanitation, hygiene and basic health care-related waste management (56). Lack of PPE has found to have negative consequences on HCWs' mental health. In a study conducted in Egypt, HCWs reported that crowded and ill-equipped workplaces and widespread shortages of PPE during COVID-19 pandemic increased their fear of getting a serious infection (39). These situations add emotional and mental burden for HCWs in attempting to self-isolate themselves from their families and communities (36). A cross-sectional study in Lebanon reported that quarantined HCWs suffered adverse mental effects such as anxiety, stress, and depression that increase under self-isolation because suspected COVID-19 infection (37). A similar study in Jordan found depression and anxiety to be more prevalent among HCWs than the general population. Specifically, pulmonologists and ENT specialists, who are at the frontline of the pandemic, scored higher in depression and anxiety surveys compared to other specialists (36).
Studies reported that fear in communities about the exposure to infection through interaction with HCWs expose them to fear-driven shunning and outright discrimination and persecution (38, 57). In Singapore, a study conducted among different HCWs found a higher perceived stigma level that was associated with higher levels of stress and post-traumatic stress symptoms. The study highlighted how internalization of stigma can reinforce avoidant behavior and social isolation which would increase traumatic stress symptoms, triggered by negative reactions from the surrounding community (38). Another study from Egypt found two-thirds of surveyed HCWs feared stigmatization and discrimination related to COVID-19 (39). The authors suggested that in collective societies and faith-based communities in Egypt, social stigma associated with COVID-19 can be addressed through education, clear announcing of health care policies, and launching stigma reduction programs. A study from China on former COVID-19 patients, including 13.3% medical staff, found perceived discrimination was associated with clinically significant PTSD symptoms, severe depression, and severe anxiety (40).
Child Rights
According to the Declaration of the Rights of the Child (58), children's rights include protection, education, health care, shelter, and good nutrition. Numerous studies have found impacts of the pandemic on children's behavioral health, development and growth, physical health, and educational outcomes, with possible differential impacts by age and gender. In China, the national government imposed a reduction of outdoor activities and social interaction among the population, including children, out of fear of spreading the virus. This resulted in adverse outcomes in children's mental, social, and behavioral health. Specifically, it found that during home confinement, Chinese children, ages 7–11, who felt insecure and anxious, had a significantly higher risk of depressive and anxiety symptoms (51). Also, the closure of schools and educational institutions in China during lockdown disrupted the learning and educational process. It also deprived students of the sense of stability and normalcy that schooling provides. In a survey of 8,140 students in different educational stages, the proportion of students who reported depressive and anxiety symptoms was high, especially among those preparing for entrance exams which had been disrupted (52). The same study reported that female and male students differ in their perceptions of the psychological impact due to losing access to schools during COVID-19 with girls suffering from greater psychological impact, including stress, anxiety, and depressive symptoms (52). Also, specific facets of children's rights, such as health care, shelter, and nutrition, were also affected. Specifically, families that deal with lockdown and COVID-19 related financial stressors, struggle to provide basic needs and daily supplies, resulting in adverse mental health outcomes for family members such as stress, anxiety, and depression (59).
Rights of Elderly Individuals
In recent years, there have been significant advocacy efforts supporting human rights of older persons including full respect for their needs, privacy, and health care (60). During COVID-19, elderly individuals were found to have less access to free movement including in open and public spaces which restricted their ability to exercise and engage in leisurely or other essential activities—deteriorating their mental health and well-being (49). In our review, we identified two studies in developed countries, and no studies related to elderly populations in developing countries. A study in Spain of community-dwelling older adults with mild cognitive impairment or dementia found that enforced lockdowns, curfews, and social isolation had more significant adverse psychological effects and exacerbated sleeping problems for elderly living alone (48). In contrast, another study found that the COVID stress-related factors, except for the loss of a loved one, were not statistically linked with the deterioration of psychological health among the elderly during stay-at-home orders; the participants showed resilience in managing COVID-related stress challenges due to sufficient personal resources (50).
Disproportionate Impacts on Minorities and Psychiatric Patients
In accordance with the UN Pact on civil and political rights, national, ethnic, religious, or linguistic minorities (61) are meant to freely receive health services without any discrimination (62). In the United States, which has the highest number of confirmed COVID-19 cases as of August 2020 (Johns Hopkins University, 2020) (63), the populations that have been impacted the most disproportionately are racial and ethnic minorities. Prevalence for COVID-19 infection was reported higher in ethnic minorities than whites given inequality in health, welfare service access, and other existing social structural issues such as structural racism and discrimination, and this inequality and right violations may have led to higher mental health problems in racial and ethnic minorities. A cross-sectional study investigating differences between awareness about COVID-19 by race and ethnicity found African-Americans and Hispanics were less likely to be informed about the pandemic and effective prevention methods (33). These findings align with another study in India where patients with mental illness from disadvantaged backgrounds had less access to information via the internet, media, online health information (45). Unequal access to information along with lack of proper health care during lockdown jeopardize their physical and mental health.
Spreading of infectious diseases often fuels racism and xenophobic tendencies, especially against racial and ethnic minorities (64, 65). This results in a detrimental impact on the health well-being of disadvantaged minority populations and indirectly denies them access to medical care (66). A cross-sectional study linked xenophobia with mental well-being among ethnic/religious minorities: a survey of the non-Muslim Indian population found that fear, generalized xenophobia, and specific xenophobia, and collectivism negatively impacted their feelings and functional aspects of mental well-being (34). In another study, researchers screened the physical and mental health of minority migrants' workers in 140 areas across India, which included construction sites, relief camps, government hostels, and shelter homes during the COVID-19 pandemic. Their findings underscored that the economic, social, and environmental disadvantages were bothersome to the migrants and were worsening their mental health, undermining their resilience, and upsetting their quality of daily living (35). The impact was prominent among pregnant women as the interviewees who were feeling overwhelmed and concerned about their lack of access to health services because of the pandemic.
Similarly, unintended consequences of the strict legal enforcement of lockdown during the COVID-19, including lack of access to medications and mental health professionals and coupled with lack of transportation, negatively impacted treatment compliance among psychiatric patients. Specifically, in India, a study of severely mentally ill patients during lockdown found 80% of patients missed their appointments and failed to contact their mental health professionals, 30% showed features of relapse of symptoms during the lockdown, and 22% stopped their psychiatric medication with patients from lower socioeconomic status, low literacy levels, and with inadequate social support showing less knowledge related to COVID-19 (45). A similar pattern was observed among patients with Obsessive-compulsive disorder (OCD) in Italy. In a group of patients with OCD who had completed an evidence-based therapeutic path for OCD before the quarantine, there was significant worsening of OCD symptoms compared to the pre-quarantine period. The author hypothesized that the lockdown and limited access to mental health centers may have discouraged patients in from seeking help and delayed the needed interventions (42).
Psychiatric patients in China were found to show higher rates of anxiety, depression, and stress symptoms compared to the general population (44). Another study from China found insomnia patients had worse sleep latency, sleep duration, and sleep efficiency due to home isolation and insufficient knowledge (43). Due to limitation on mobility, cancer patients in Ghana were unable to engage in activities involving social gatherings, worsening their mental health (41). Even though psychiatric patients often experience high levels of social discrimination (67), in this review, a study in China reported that patients with mental illnesses had not been experiencing additional discrimination during the COVID-19 epidemic (44). Though, in India, self-isolation and stay-at-home orders forced many psychiatric patients to live in unsafe homes and increase their exposure to domestic violence. In India, ~63.6% of psychiatric patients reported that they were experiencing verbal and physical aggression from others and 30.3% of their caregivers expressed a feeling of the excessive burden of taking care of patients in addition to the burden related to other reasons, like financial issues related to the lockdown (45).
Discussion
Overview
The review identified human rights violations that are associated with adverse mental health outcomes such as mobility restrictions including quarantines and lockdowns, shortages of supplies and equipment, stigma, xenophobia, and discrimination, losing access to schools and proper education, lack of access to information, and inequalities around access to quality mental health services. In addition, the findings of this review underscore several points in advancing our understanding and knowledge of human rights restrictions and violations and their association with mental health well-being during the COVID pandemic. Given these findings, we would like to make a case that human rights of individuals and vulnerable populations must be protected during this pandemic and given that mental health is one of the fundamental rights, it needs prioritization at the public policy level (8). Human rights and mental health are such delicate entities that at times public health and public policy actions might compromise larger interests of the most afflicted or vulnerable populations. Evidence-based policies may not always be representative of all members of the community. Therefore, ethical and rights-based approaches to ensure no added harm or disenfranchisement of individuals/groups is a sentiment that needs to be acted upon post-pandemic.
Summary Findings Around Vulnerable Groups
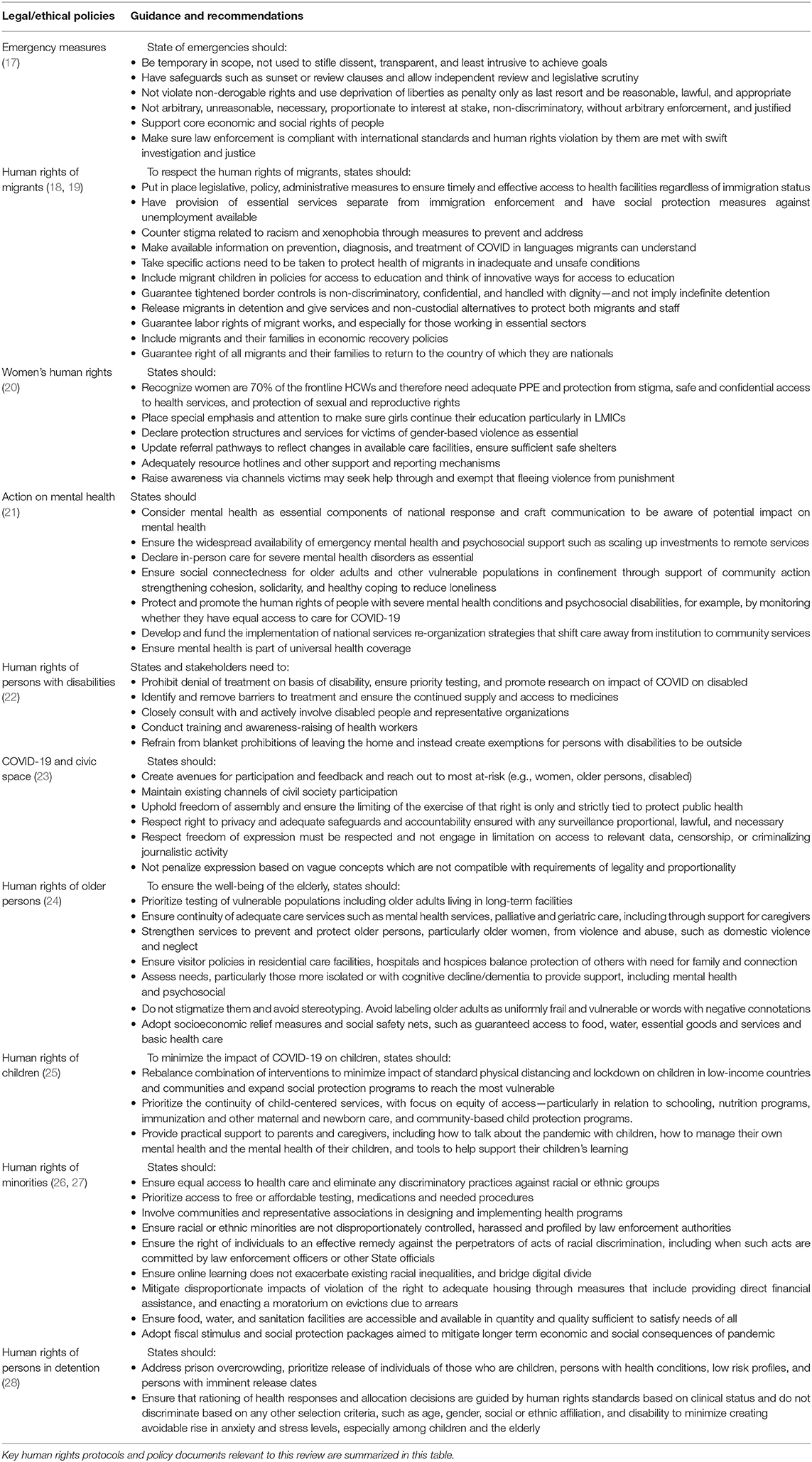
From the articles reviewed, 24 identified studies were published between April and July 2020. This is consistent with the fact that the health emergency measures in response to COVID-19 were declared worldwide in March 2020 and therefore most relevant studies for this review would take place in the following months. Many of the identified studies were conducted in developed countries and there may be variation in the understanding of human rights and legislations across countries. See Table 2 that enlists Key UN human rights protocols and policy documents for diverse populations. The definition, understanding and agreement on vulnerable populations might also vary from one country context to the other. The understanding, development and functioning of public mental health systems might also vary in different geopolitical contexts. Previous studies found that many developing countries lack the basic legal framework to protect patients suffering with mental illness as well as a recognition that there is an absence of specific human rights policy during health emergencies to guide mitigation and protection measures (13). Both observations lend evidence to disproportionate impact on vulnerable key populations. The intersectional nature of multiple minoritized identities coalescing together such as being a migrant, disabled, and an adolescent girl—their complexity, need for comprehensive policy action—cannot be under-emphasized here.
In our review, a strong association between the adverse mental health outcomes and human rights restrictions such as quarantine has been well-documented, a clear finding in our review with anxiety and mood disorders being the most common conditions impacting populations (68). Additionally, countries with higher-than-average rates of stress-related symptoms pre-COVID may continue to experience increases if effective measures are not implemented which necessitates a collective plan of action.
Findings of adverse mental health outcomes following human rights violations were reported among vulnerable subgroups such as children, girls, elderly, and racial/ethnic minorities. The two studies that examined the mental health-related adverse outcomes associated with human rights violations found significant deterioration in children's mental, social, and behavioral health due to restriction in daily activities and movement (51, 52). It is important to note that the lockdown and social distancing could cause children—and especially children with mental disorders including developmental disabilities or physical or psychological comorbidities—to be prevented from fulfilling their psychological needs and developmental milestones leading to underdevelopment (69). Furthermore, home confinement can increase child abuse as pre-pandemic the vast majority of abuse was reported by staff working at institutions which were temporarily closed raising concerns that child abuse will go unnoticed, leading to higher child morbidity and mortality and long-term negative developmental consequences (70). The United Nations Population Fund (UNFPA) estimates, due to the COVID-19 pandemic, 42–66 million more children potentially falling into poverty, and 13 million child marriages by 2030 that could otherwise have been averted, and 2 million more cases of female genital mutation by 2030 that could have been avoided (71, 72). Child marriages, child labor and such practices can flourish unchecked during this protracted pandemic. This is also an example of practices and cultural traditions that would yield in harmful short and long term mental health outcomes for the vulnerable children.
In this review, we found that girls suffered varied mental health outcomes due to violations of their human rights via losing access to school (52). These are consistent with what is reported by WHO (73), as existing gender inequalities are exacerbated by COVID-19 which affect both genders differently (74). The realization of girls' human rights and their well-being, especially during emergencies, have not always been accorded priority attention (75). Furthermore, females' access to sexual and reproductive health services is likely to be affected (76). In our review, difficulties were reported by pregnant women in accessing basic prenatal services during the pandemic due to closure and movement restrictions (35) and a previous report found that stay-at-home orders may contribute to women's vulnerability and considered a risk factor for gender based violence (74). Mobility restrictions can increase domestic violence and in our review a study from the United States found an increase in orthopedic trauma patients reporting interpersonal violence post-lockdown compared with pre-lockdown with an increase in fractures in female patients indicating an increase in gender based violence (47). Additionally, a UN human rights report alluded to rise in gender based and domestic violence due to economic and psychosocial challenges (76). We do strongly recommend national level action on mitigating the harms caused by violence on women and girls as domestic violence is both a cause and consequence of mental ill-health (77). A gender responsive training for health care workers, police, law enforcement officers and social protection workers would be critical in reducing the disproportionate burden of mental ill-health that will fall on young girls and women exposed to abusive environments.
Our review found HCWs suffered negative consequences as a result of shortage of supplies and equipment as well as stigma (39). Other reports have also found mistreatment because of stigma toward HCWs such as the denial of public transport, eviction from homes, and assaults when carrying out duties negatively impacted their mental health (75). To mitigate stigma, proper health education is needed to target the public to prevent social harassments of HCWs and COVID-19 survivors.
Regarding elderly's rights, two studies examined the association of human rights violations and mental health outcomes among elderly people in developed countries (48, 50). Common characteristics across the studies that were indicative of human rights violations were: enforced lockdown, curfews, and restricted the ability to exercise and engage in essential activities. No identified study examined old age discrimination or factors that directly contributed to autonomy of elderly individuals. However, other reports have noted that well-intentioned but ageist public messages can cause the elderly to be marginalized and to mitigate this, countries can use inclusive language and avoid negative emphasis on risk (78). Furthermore, to lessen potential adverse mental health impacts on the elderly—especially those with mental disorders or predisposed to feelings of loneliness—due to home confinement and curtailing of mobility rights, countries can engage in promoting social connection in public health messaging, mobilizing resources from family members, and giving help via community-based networks (79, 80). One of the moral imperatives we have as a global community is to strengthen mental health via reduction of increasing social isolation in the face of this protracted pandemic.
Studies have noted with concern adverse mental health outcomes due to human rights violations including lack of access to accurate and up-to-date information among racial and ethical minorities (33). Our review also found xenophobic viewpoints were correlated with negative well-being for both holding those viewpoints and those targeted which have co-incited with underreporting and biased media coverage as well as misinformation targeting religious minorities (34). In our review, a study has revealed an additional model of ecology of health and sickness based on social determinants of health among migrant workers which are one of most marginalized and stigmatized population in LMICs (35). It has also been noted that refugees and immigrants in detention centers face an increased likelihood of developing post-traumatic stress disorder as many refugees associate economic hardship, food and medicine shortages with a threat to life alongside viewing military presence to enforce restrictions as a threat and not a protection (81). There has been little-to-no scholarly work on this subject though police brutality has been on the rise in context of enforcing stay-at-home and mask-guidelines (82). Concerns have been raised over the disproportionate impact of over policing in enforcing lockdown measures toward minority communities (83). There have also been reports of physical beatings or killings over breakings of curfew laws (84) which is a violation of human rights (85). The mental stress and trauma associated with such events would become subject of further inquiry as time moves on but sensitivity training and ethical psychosocial response needs to be embedded within judicial and armed services assisting emergency response. Racial, ethnic and religious discrimination remains an area with very limited evidence around how mental health field can be leveraged to promote equity and social justice focused messages but also ways of providing care to aggrieved populations.
Human rights restrictions and violations have significant impacts on treatment outcomes, but higher impacts on patients with mental disorders given pre-existing mental health condition and social ostracization due to stigma. Research suggests that patients with mental illness are suffering from worsening of their pre-existing condition and difficulty in maintaining medication adherence because of restriction of mobility and lack of access to medications (42, 45). This was coupled with increased experiences of verbal and physical violence at hands caregivers. It is important to limit the abuses of human rights of those with mental health conditions especially by curtailing marginalization and stigmatization and increasing resources toward providing services (86). Article 11 of the Convention on the rights of individuals with disabilities (CRPD) stipulating that all necessary measures to ensure protection and safety of persons with disabilities in situations of risk should be pursued (87). Furthermore, it is vital to ensure the well-being of caregivers of vulnerable individuals. This is especially pertinent in a disability setting as the caregiver's well-being is also important for the well-being of their charge or family member. A side effect of the lockdown in Europe on people with disabilities has been a massive harmful impact with reductions, early discharge, and the stoppings of admissions to rehabilitation expected to lead to an increased rehabilitation demand after the emergency subsides (88). Despite the boom in digital health during the COVID-19, no reported studies examined the role of engagement of technology with available services in mitigating the structural barriers to getting mental health care during the COVID pandemic. For example, concerns have been expressed that digital health services may not assist in decreasing inequity due to factors such as limited access of digital health services for those in poverty (89). This is an area in need of serious research and policy level attention. Resource allocation in providing quality digital and telehealth services, online learning or improving access to services for high risk groups also needs urgent prioritization.
Upholding Global Rights Conventions and Further Recommendations
UN committees that monitor nation states human rights actions include UN International Covenant on Civil and Political rights (ICCPR) (90), Committee on Economic, Social and Cultural rights (CESCR) (55), Committee on Elimination of Racial Discrimination (CERD) (91), Committee on All forms of discrimination against women (CEDAW) (92), Committee against Torture (CAT) (93), Convention on the rights of the child (CRC) (94), and CRPD (95). In the context of emergencies, these committees advocate for right to health, human rights in health systems as well as upholding of human rights through health (96). There are a number of guidelines in place as seen from Table 1 on key recommendations mostly from the Office of the High Commissioner around COVID-19 and vulnerable populations. The UN recommendations and guidance around COVID stipulates a public health approach to managing the pandemic impact based on equal rights, opportunity, and valuing freedoms especially of the most-at risk populations. Many share similar recommendations such as advising for more investment into these vulnerable populations to ensure the negative impacts of the lockdown—including quarantine, social distancing, economic fallout—are lessened and disproportionate limitations around access to services and rights due to structural inequities are addressed. It is important to consider these as they provide valuable insight in how to minimize the consequences of the COVID-19 pandemic response and its response which embeds human rights informed care and risk mitigation pathway. However, there needs to be more emphasis on strategies that would address lockdown, public health action associated impacts and their mental health outcomes, and the need to prioritize mental health and well-being holistically. Given that the pandemic is going to take us through several waves of infection spread and containment, it is critical for this rights based approach to embrace short and long term mental health consequences and mitigation strategies.
If we are to achieve a shared vision of protecting the population from adverse mental effects due to the pandemic and necessary pandemic responses, policy makers would benefit from an increased focus on strengthening leadership and governance, finance mechanisms, and developing programs and policies that include vulnerable populations (97). For LMICs, it is critical for the service provision be focused on accessible and equitable evidence-based community care models corresponding with the existing mental health capacity to deliver care, train existing primary care staff to cater to increased mental health needs, implement prevention and promotion programs tailored to local needs, and support civil societies and employers to address the increased burden of mental illness.
Furthermore, mental health can be supported in the form of investment in the development of virtual platforms and telehealth to provide psychoeducation, self-guided low intensity interventions, alongside peer, and specialist-supported e-therapies. These can be embedded within integrated electronic health records and service platforms (98). Task shifting to provide psychosocial and peer-based support will also be useful such as using lay volunteers trained to provide human connectedness to address physical distancing and resultant isolation- a strategy well-adopted in LMICs. These approaches will also be beneficial in HICs in that effective management of the mental health consequences of the pandemic in historically marginalized communities requires a multilevel, community-wide approach led by culturally sensitive mental health professionals (99).
Improving Care for All
Regarding vulnerable and at-risk populations, there is a specific need to pay attention to their mental health as many of the inequities, access and service issues have longstanding history prior to COVID-19, and the pandemic has only further exacerbated them. Human rights violations in the mental health context remain significant throughout the world and cannot be explained by a lack of resources alone (100). WHO QualityRights initiative aims to reform human rights within mental health field and has developed policies and sensitization strategies to carry out system level strengthening of a holistic response to mental illness keeping our right to dignity, freedom and health at center (101). This thinking has been part of the WHO mental health treatment gap action program (mhGAP) framework to champion human rights informed thinking and rally for mental health as a core human right. Various fundamental human rights are interdependent therefore undermining one leads to a poor impact on others (102). This means that all human rights should be addressed together, including mental health.
To help strengthen mental health systems researchers should focus on developing robust information systems able to be enhanced by linking with other data sources to run predictive models using robust informatics methodology. A focus can also be placed on community-based interventions to address the COVID-19 mental health issues in integrated approach alongside innovative digital solutions (97). There is an urgent need for research to address how mental health consequences for vulnerable groups can be mitigated under pandemic conditions, and on the impact of repeated media consumption and health messaging around COVID-19 (103).
Addressing human rights can be a helpful way to mitigate the impact of mental illness on populations especially during public health emergency. Policy and frameworks to address different aspects of human rights can complement the various form of health services to enhance the mental health well-being during pandemics. However, effective implementation of the medico-legal and ethical aspect of the human rights will rely on the extent to which the research proved a direct association between violations and adverse mental health outcomes and how the implementation will be applied through public policy. Going forward this understanding may help to minimize the mental health risk associated with violations of human rights during health emergencies and provide the policy makers useful directions on how to address discrimination and human right violations in guidance, policies, and practices (104). This review we hope has provided findings that set the foundation on how to integrate human rights as an integral part of public health response keeping mental health as a core thematic. In addition, the review provides pointers to ethical guidance when dealing with vulnerable populations especially during public heath crises (see Table 3 for further recommendations and overview of prominent findings). To target concerns about human rights violations during pandemics, policy makers should work with mental healthcare providers and target populations to ensure that suitable emergency health measures are provided through human rights lenses. This collaborative approach can pave the road to continue engaging or increasing engagement of different stakeholders in different sectors during stressful periods.
Although this review provides evidence that is valuable for addressing human rights perspectives while providing mental health services to different population, future research should (1) consider that some countries are still not signatories of the UN universal declaration of human rights and countries may have a different interpretation of what counts as a human rights violation; (2) countries also have different legal systems to define and enforce human rights measures; (3) there is need to arrive at a consensus on defining of human rights restrictions and violations in mental health and how it should be identified and quantified; and going forward through different UN human rights conventions as instruments to make that change; (4) adequate reporting of human rights restrictions and violations especially among vulnerable populations should be better etched out and this should include adverse mental health outcomes.
Strengths and Limitations
This review followed the guidelines for a rapid review. The review highlights human rights violations influencing the mental well-being in impacted population. We summarize the agreements and global or national policies that enforce human rights during emergencies as a reminder of what we ought to be looking out for and values countries need to hold themselves accountable to. Our findings contribute to a broader understanding of the impact of COVID pandemic on population health. This review does have some limitations, however. The research team tried to identify and include as many published papers as possible; however, because of the novelty of the topic, the defined articles were limited and the rapidly evolving nature of the pandemic and associated scholarly literature could have caused some relevant articles to be missed. There is difficulty in creating a comprehensive list of human rights constructs as they are different based on factors such as target population and country of interest (105). Also, articles that were not data-driven were not included in our analysis, which may have impacted results of this review. Nevertheless, this approach was applied to ensure peer-reviewed articles were included which strengthens our results. Moreover, the study team attempted to group the results based on the themes that reported in the WHO report (84). We only included articles that addressed the research questions of focus of the review and therefore, generalizing the results on different setting and population should be done with caution.
Conclusions
Finally, this review also acknowledges the implications for guideline and policies on different populations and therefore, (1) efforts to improve engagement of policy makers may be beneficial to address mental health outcomes during public health emergency and (2) civil society and human rights champions (including lived experience representatives), health care providers, and policy makers should work together to identify the policy, services, and interventions that enforce human rights which have a lasting impact on mental health of key populations during emergencies. We will be better served to understand the tradeoffs and the reciprocating relationships among physical health, mental health, human rights, and individual rights, that there could be better statements in global reports of values-driven, shared objectives in light of these tradeoffs and relationships, and a more thorough consideration of many relevant areas of science (including but not limited to, infectious disease) to establish a policy that strikes the most acceptable balance.
Author Contributions
MR and MK developed the study protocol. RA helped edit the protocol. MR, RA, and MK extracted the data and compiled the initial list of studies. MR and RA along with MK wrote the manuscript. All authors read, edited, and approved the final version of the paper.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2020.603875/full#supplementary-material
References
1. World Bank. How the World Bank Is Mitigating the Impacts of COVID-19 in the Health Sector (2020). Available online at: www.worldbank.org/en/news/feature/2020/06/16/how-the-world-bank-is-mitigating-the-impacts-of-covid-19-in-the-health-sector
2. World Health Organization. Coronavirus Disease (COVID-19) - Events as They Happen (2020). Available online at: www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen
3. United Nations. We are all in this Together: Human Rights and COVID-19 Response and Recovery (2020). Available online at: www.un.org/en/un-coronavirus-communications-team/we-are-all-together-human-rights-and-covid-19-response-and
4. United Nations. Human rights (2016). Available online at: https://www.un.org/en/sections/issues-depth/human-rights/
5. National Collaborating Centre for Determinants of Health. Vulnerable Populations. Available online at: https://nccdh.ca/glossary/entry/vulnerable-populations#:~:text=Vulnerable%20populations%20are%20groups%20and,due%20to%20illness%20or%20disability.
6. ten Have H. Disasters, vulnerability and human rights. In: O'Mathúna D, Dranseika V, Gordijn B, editors. Disasters: Core Concepts and Ethical Theories. Advancing Global Bioethics. Vol 11:1–10. Cham: Springer (2018).
7. American Psychological Association. Mental Health is a Human Right (2020). Available online at: https://www.apa.org/international/pi/2018/12/mental-health-rights
8. Office of the High Commissioner for Human Rights. COVID-19 and Its Human Rights Dimensions: Guidance (2020). http://digitallibrary.un.org/record/3860124/files/COVID19Guidance.PDF
9. Dubey S, Biswas P, Ghosh R, Chatterjee S, Dubey MJ, Chatterjee S, et al. Psychosocial impact of COVID-19. Diabetes Metab Syndr Clin Res Rev. (2020) 14:779–88. doi: 10.1016/j.dsx.2020.05.035
10. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
11. Moitra M., Rahman M., Collins P., Gohar F., Weaver M., Kinuthia J., et al. Mental Health Consequences of Health care Workers in the context of COVID-19: a scoping review to draw lessons for LMICs and fragile settings. Front Psychiatry. (2020).
12. Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med. (2020) 383:510–2. doi: 10.1056/NEJMp2008017
13. United Nations. COVID-19 and Human Rights (2020). Available online at: https://www.un.org/victimsofterrorism/sites/www.un.org.victimsofterrorism/files/un_-_human_rights_and_covid_april_2020.pdf
14. Tricco AC, Antony J, Zarin W, Strifler L, Ghassemi M, Ivory J, et al. A scoping review of rapid review methods. BMC Med. (2015) 13:224. doi: 10.1186/s12916-015-0465-6
15. Khangura S, Konnyu K, Cushman R, Grimshaw J, Moher D. Evidence summaries: the evolution of a rapid review approach. System Rev. (2012) 1:10. doi: 10.1186/2046-4053-1-10
16. McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. (2016) 75:40–6. doi: 10.1016/j.jclinepi.2016.01.021
17. Office of the High Commissioner for Human Rights. Emergency Measures and COVID-19 : Guidance (2020). Available online at: http://digitallibrary.un.org/record/3861152/files/EmergencyMeasuresCOVID19.PDF
18. Office of the High Commissioner for Human Rights. COVID-19 and the Human Rights of Migrants: Guidance (2020). Available online at: digitallibrary.un.org/record/3861155/files/OHCHRGuidanceCOVID19Migrants.PDF
19. United Nations. Joint Guidance Note on the Impacts of the COVID-19 Pandemic on the Human Rights of Migrants (2020). Available online at: https://www.ohchr.org/Documents/Issues/Migration/CMWSPMJointGuidanceNoteCOVID-19Migrants.pdf
20. Office of the High Commissioner for Human Rights. COVID-19 and women's human rights : guidance. (2020) Available online at: http://digitallibrary.un.org/record/3861157/files/COVID-19ndWomensHumanRights.PDF
21. Office of the High Commissioner for Human Rights. COVID-19 and the need for action on mental health: policy brief (2020). Available online at: http://digitallibrary.un.org/record/3866300/files/mentalhealth.PDF
22. Office of the High Commissioner for Human Rights. COVID-19 and the rights of persons with disabilities : guidance (2020). Available online at: http://digitallibrary.un.org/record/3861159/files/COVID-19the_RightsPersonsDisabilities.PDF
23. United Nations. Civic space and COVID-19: guidance (2020). Available online at: http://digitallibrary.un.org/record/3861153/files/CivicSpaceandCovid.PDF
24. United Nations. Policy Brief: The Impact of COVID-19 on older persons (2020). Available online at: www.un.org/sites/un2.un.org/files/un_policy_brief_on_covid-19_and_older_persons_1_may_2020.pdf
25. United Nations. Policy Brief: The Impact of COVID-19 on children (2020). Available online at: www.un.org/sites/un2.un.org/files/policy_brief_on_covid_impact_on_children_16_april_2020.pdf
26. Office of the High Commissioner for Human Rights. Racial Discrimination in the Context of the COVID-19 Crisis (2020). Available online at: https://www.ohchr.org/Documents/Issues/Racism/COVID-19_and_Racial_Discrimination.pdf
27. Office of the High Commissioner for Human Rights. COVID19 and Minority Rights: Overview And Promising Practices (2020). Available online at: ohchr.org/Documents/Issues/Minorities/OHCHRGuidance_COVID19_MinoritiesRights.pdf
28. Inter-Agency Standing Committee. COVID-19: Focus On Persons Deprived of Their Liberty (2020). Available online at: https://interagencystandingcommittee.org/system/files/2020-03/IASC%20Interim%20Guidance%20on%20COVID-19%20-%20Focus%20on%20Persons%20Deprived%20of%20Their%20Liberty.pdf
29. Carmen C, Caballero-Domínguez CC, Jiménez-Villamizar MP, Campo-Arias A. Suicide risk during the lockdown due to coronavirus disease (COVID-19) in Colombia. Death Stud. (2020) 1–6. doi: 10.1080/07481187.2020.1784312
30. Mamun MA, Ullah I. COVID-19 suicides in Pakistan, dying off not COVID-19 fear but poverty?–The forthcoming economic challenges for a developing country. Brain Behav Immunity. (2020) 87:163–6. doi: 10.1016/j.bbi.2020.05.028
31. Shoib S, Nagendrappa S, Grigo O, Rehman S, Ransing R. Factors associated with COVID-19 outbreak-related suicides in India. Asian J Psychiatry. (2020) 53:e102223. doi: 10.1016/j.ajp.2020.102223
32. Iob E, Steptoe A, Fancourt D. Abuse, self-harm and suicidal ideation in the UK during the COVID-19 pandemic. Br J Psychiatry (2020) 217:543–6. doi: 10.1192/bjp.2020.130
33. Jones J, Sullivan PS, Sanchez TH, Guest JL, Hall EW, Luisi N, et al. Similarities and differences in COVID-19 awareness, concern, and symptoms by race and ethnicity in the United States: cross-sectional survey. J Med Internet Res. (2020) 22:e20001. doi: 10.2196/20001
34. Ahuja KK, Banerjee D, Chaudhary K, Gidwani C. Fear, xenophobia and collectivism as predictors of well-being during Coronavirus disease 2019: an empirical study from India. Int J Soc Psychiatry (2020). doi: 10.1177/0020764020936323
35. Chander R, Murugesan M, Ritish D, Damodharan D, Arunachalam V, Parthasarathy R, et al. Addressing the mental health concerns of migrant workers during the COVID-19 pandemic: an experiential account. Int J Soc Psychiatry (2020). doi: 10.1177/0020764020937736
36. Naser AY, Dahmash EZ, Al-Rousan R, Alwafi H, Alrawashdeh HM, Ghoul I, et al. Mental health status of the general population, health care professionals, and university students during 2019 coronavirus disease outbreak in Jordan: a cross-sectional study. Brain Behav. (2020) 10:e01730. doi: 10.1002/brb3.1730
37. Fawaz M, Samaha A. The psychosocial effects of being quarantined following exposure to COVID-19: a qualitative study of Lebanese health care workers. Int J Soc Psychiatry. (2020) 66:560–5. doi: 10.1177/0020764020932202
38. Chew QH, Chia FL, Ng WK, Lee W, Tan P, Wong CS, et al. Psychological and coping responses to COVID-19 amongst residents in training across ACGME-I accredited specialties in Singapore. Psychiatry Res. (2020) 290:113146. doi: 10.1016/j.psychres.2020.113146
39. Wahed WYA, Hefzy EM, Ahmed MI, Hamed NS. Assessment of knowledge, attitudes, and perception of health care workers regarding COVID-19, a cross-sectional study from Egypt. J Community Health. (2020) 45:1242–51. doi: 10.1007/s10900-020-00882-0
40. Liu D, Baumeister RF, Veilleux JC, Chen C, Liu W, Yue Y, et al. Risk factors associated with mental illness in hospital discharged patients infected with COVID-19 in Wuhan, China. Psychiatry Res. (2020) 292:113297. doi: 10.1016/j.psychres.2020.113297
41. Kugbey N, Ohene-Oti N, Vanderpuye V. COVID-19 and its ramifications for cancer patients in low-resource settings: Ghana as a case study. Ecancermed Sci. (2020) 14:ed99. doi: 10.3332/ecancer.2020.ed99
42. Davide P, Andrea P, Martina O, Andrea E, Davide D, Mario A. The impact of the COVID-19 pandemic on patients with OCD: effects of contamination symptoms and remission state before the quarantine in a preliminary naturalistic study. Psychiatry Res. (2020) 291:113213. doi: 10.1016/j.psychres.2020.113213
43. Yang L, Yu Z, Xu Y, Liu W, Liu L, Mao H. Mental status of patients with chronic insomnia in China during COVID-19 epidemic. Int J Soc Psychiatry. (2020) 66:821–6. doi: 10.1177/0020764020937716
44. Hao F, Tan W, Jiang L, Zhang L, Zhao X, Zou Y, et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav Immunity. (2020) 87:100–6. doi: 10.1016/j.bbi.2020.04.069
45. Muruganandam P, Neelamegam S, Menon V, Alexander J, Chaturvedi SK. COVID-19 and severe mental illness: impact on patients and its relation with their awareness about COVID-19. Psychiatry Res. (2020) 291:113265. doi: 10.1016/j.psychres.2020.113265
46. Iasevoli F, Fornaro M, D'Urso G, Galletta D, Casella C, Paternoster M. Psychological distress in serious mental illness patients during the COVID-19 outbreak and one-month mass quarantine in Italy. Psychol Med. (2020) 1–3. doi: 10.1017/S0033291720001841
47. Ohliger E, Umpierrez E, Buehler L, Ohliger AW, Magister S, Vallier H, et al. Mental health of orthopaedic trauma patients during the 2020 COVID-19 pandemic. Int Orthopaedics. (2020) 44:1921–5. doi: 10.1007/s00264-020-04711-w
48. Goodman-Casanova JM, Dura-Perez E, Guzman-Parra J, Cuesta-Vargas A, Mayoral-Cleries F. Telehealth home support during COVID-19 confinement for community-dwelling older adults with mild cognitive impairment or mild dementia: survey study. J Med Internet Res. (2020) 22:e19434. doi: 10.2196/19434
49. Goethals L, Barth N, Guyot J, Hupin D, Celarier T, Bongue B. Impact of home quarantine on physical activity among older adults living at home during the COVID-19 pandemic: qualitative interview study. JMIR Aging (2020) 3:e19007. doi: 10.2196/19007
50. Lopez J, Perez-Rojo G, Noriega C, Carretero I, Velasco C, Martinez-Huertas JA, et al. Psychological well-being among older adults during the covid-19 outbreak: a comparative study of the young-old and the old-old adults. Int Psychogeriatrics. (2020) 1–6. doi: 10.1017/S1041610220000964
51. Xie X, Xue Q, Zhou Y, Zhu K, Liu Q, Zhang J, et al. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatr. (2020) 174:898–900. doi: 10.1001/jamapediatrics.2020.1619
52. Zhou SJ, Zhang LG, Wang LL, Guo ZC, Wang JQ, Chen JC, et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur Child Adolesc Psychiatry. (2020) 29:749–58. doi: 10.1007/s00787-020-01541-4
53. ILGA Europe. Obligations of States in the Field of Human Rights in the Context of COVID-19 (2020). Available online at: ilga-europe.org/sites/default/files/covid19%20%20states%20obligations%20in%20the%20field%20of%20lgbti%20human%20rights.pdf
54. World Health Organization. International Covenant on Economic, Social Cultural Rights. Health Human Rights. United Nations Human Rights, Office of the High Commissioner (2013). Available from: http://www.ohchr.org/EN/ProfessionalInterest/Pages/CESCR.aspx
55. UN General Assembly. International Covenant on Economic, Social and Cultural Rights, United Nations, Treaty Series. Vol. 993 (1966). p. 3. Available online at: https://www.refworld.org/docid/3ae6b36c0.html
57. Rana W, Mukhtar S, Mukhtar S. Mental health of medical workers in Pakistan during the pandemic COVID-19 outbreak. Asian J Psychiatry. (2020) 51:102080. doi: 10.1016/j.ajp.2020.102080
58. Assembly UG. Convention on the Rights of the Child. United Nations, Treaty Series, 1577. (1989).
59. Rehman U, Shahnawaz MG, Khan NH, Kharshiing KD, Khursheed M, Gupta K, et al. Depression, anxiety and stress among indians in times of covid-19 lockdown. Community Mental Health J. (2020) 1–7. doi: 10.1007/s10597-020-00664-x
60. United Nations. Human Rights of Older Persons. (2011). Available online at: www.ohchr.org/en/issues/olderpersons/pages/olderpersonsindex.aspx
61. Office of the United Nations High Commissioner for Human Rights. Minorities Under International Law (2020). Available online at: ohchr.org/en/issues/minorities/pages/internationallaw.aspx
62. Panel on Race E, Bulatao RA, Anderson NB, National Research Council. National Research Council (US) Panel on Race, Ethnicity, and Health in Later Life. In: Bulatao RA, Anderson NB, editors. Understanding Racial and Ethnic Differences in Health in Late Life: A Research Agenda. Washington, DC: National Academies Press (2004).
63. Johns Hopkins University of Medicine. “COVID-19 Map.” Johns Hopkins Coronavirus Resource Center. (2020). Available online at: coronavirus.jhu.edu/map.html
64. Kurzban R, Leary MR. Evolutionary origins of stigmatization: the functions of social exclusion. Psychol Bull. (2001) 127:187–208. doi: 10.1037/0033-2909.127.2.187
65. Park JH, Faulkner J, Schaller M. Evolved disease-avoidance processes and contemporary anti-social behavior: prejudicial attitudes and avoidance of people with physical disabilities. J Nonverb Behav. (2003) 27:65–87. doi: 10.1023/A:1023910408854
66. Williams DR, Rucker TD. Understanding and addressing racial disparities in health care. Health Care Financing Rev. (2000) 21:75–90.
67. Zhang Z, Sun K, Jatchavala C, Koh J, Chia Y, Bose J, et al. Overview of stigma against psychiatric illnesses and advancements of anti-stigma activities in Six Asian Societies. Int J Environ Res Public Health. (2019) 17:280. doi: 10.3390/ijerph17010280
68. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
69. Ye J. Pediatric mental and behavioral health in the period of quarantine and social distancing with COVID-19. JMIR Pediatr Parent. (2020) 3:e19867. doi: 10.2196/19867
70. Martinkevich P, Larsen LL, Græsholt-Knudsen T, Hesthaven G, Hellfritzsch MB, Petersen KK, et al. Physical child abuse demands increased awareness during health and socioeconomic crises like COVID-19: a review and education material. Acta Orthop. (2020) 1–7. doi: 10.1080/17453674.2020.1782012
71. UNFPA. “Impact of the COVID-19 Pandemic on Family Planning Ending Gender-based Violence, Female Genital Mutilation Child Marriage” Interim Technical Note. (2020). Available online at: https://www.unfpa.org/sites/default/files/resource-pdf/COVID-19_impact_brief_for_UNFPA_24_April_2020_1.pdf
72. Gentilini U, Almenfi M, Orton I, Dale P. Social Protection and Jobs Responses to COVID-19: A Real-Time Review of Country Measures. Washington, DC: World Bank (2020).
73. World Health Organization. Addressing human rights as key to the COVID-19: response. 21 April 2020). (No. WHO/2019-nCoV/SRH/Rights/2020.1). World Health Organization (2020).
74. United Nations. In Focus: Gender Equality Matters in COVID-19 Response (2020). Available online at: www.unwomen.org/en/news/in-focus/in-focus-gender-equality-in-covid-19-response
75. Bagcchi S. Stigma during the COVID-19 pandemic. Lancet Infect Dis. (2020) 20:782. doi: 10.1016/S1473-3099(20)30498-9
76. United Nations Fund for Population Activities. COVID-19: A Gender Lens (2020). Available online at: www.unfpa.org/resources/covid-19-gender-lens
77. World Health Organization. COVID-19 and Violence Against Women (2020). Available online at: www.who.int/reproductivehealth/publications/vaw-covid-19/en/
78. Webb L. Covid-19 lockdown: a perfect storm for older people's mental health. J Psychiatric Mental Health Nurs (2020). doi: 10.1111/jpm.12644
79. Brown EE, Kumar S, Rajji TK, Pollock BG, Mulsant BH. Anticipating and mitigating the impact of COVID-19 pandemic on Alzheimer's disease and related dementias. Am J Geriatric Psychiatry. (2020) 28:712–21. doi: 10.1016/j.jagp.2020.04.010
80. Wu B. Social isolation and loneliness among older adults in the context of COVID-19: a global challenge. Global Health Res Policy. (2020) 5:1–3. doi: 10.1186/s41256-020-00154-3
81. Rees S, Fisher J. COVID-19 and the mental health of people from refugee backgrounds. Int J Health Serv. (2020) 50:415–7. doi: 10.1177/0020731420942475
82. Rani J. Tamil Nadu: Blanket of Silence over Caste-Based Atrocities During COVID-19 Lockdown (2020). Available online at: https://thewire.in/caste/tamil-nadu-dalit-tribal-violence-atrocities-covid-19-lockdown-silence
83. Amnesty International. Policing the Pandemic: Human Rights Violations in the Enforcement of COVID-19 Measures in Europe. Available online at: https://www.amnesty.org/download/Documents/EUR0125112020ENGLISH.PDF
84. Mark Heywood. Human Rights, the Rule of Law, and COVID-19 in South Africa (2020). Available online at: https://blog.petrieflom.law.harvard.edu/2020/06/04/south-africa-global-responses-covid19/
85. Office of the High Commissioner for Human Rights. COVID-19 exacerbates the risk of ill-treatment and torture worldwide – UN experts (2020). Available online at: https://www.ohchr.org/EN/NewsEvents/Pages/int-day-torture.aspx
86. Mfoafo-M'Carthy M, Huls S. Human rights violations and mental illness: Implications for engagement and adherence. Sage Open. (2014) 4:2158244014526209. doi: 10.1177/2158244014526209
87. Wilson K. The COVID-19 pandemic and the human rights of persons with mental and cognitive impairments subject to coercive powers in Australia. Int J Law Psychiatry. (2020) 72:101605. doi: 10.1016/j.ijlp.2020.101605
88. Negrini S, Grabljevec K, Boldrini P, Kiekens C, Moslavac S, Zampolini M, et al. Up to 2.2 million people experiencing disability suffer collateral damage each day of COVID-19 lockdown in Europe. Eur J Phys Rehabil Med. (2020) 56:361–5. doi: 10.23736/S1973-9087.20.06361-3
89. Crawford A, Serhal E. Digital health equity and COVID-19: the innovation curve cannot reinforce the social gradient of health. J Med Internet Res. (2020) 22:e19361. doi: 10.2196/19361
90. UN General Assembly. International Covenant on Civil and Political Rights. United Nations, Treaty Series, Vol. 999. (1966). p. 171. Available online at: https://www.refworld.org/docid/3ae6b3aa0.html
91. UN General Assembly. International Convention on the Elimination of All Forms of Racial Discrimination. United Nations, Treaty Series, vol. 660. (1965). p. 195. Available online at: https://www.refworld.org/docid/3ae6b3940.html (accessed September 7, 2020)
92. UN General Assembly. Convention on the Elimination of All Forms of Discrimination Against Women. United Nations, Treaty Series, vol. 1249. (1979). p. 13. Available online at: https://www.refworld.org/docid/3ae6b3970.html
93. Office of the High Commissioner for Human Rights. Committee Against Torture. Available online at: https://www.ohchr.org/en/hrbodies/cat/pages/catindex.aspx
95. United Nations. Convention on the Rights of Persons with Disabilities. Treaty Series, 2515.3 (2006).
97. Maulik PK, Thornicroft G, Saxena S. Roadmap to strengthen global mental health systems to tackle the impact of the COVID-19 pandemic. Int J Mental Health Syst. Stockholm (2020) 14:1–13. doi: 10.1186/s13033-020-00393-4. Available online at: https://www.sida.se/contentassets/64753a5f4dee4a04af103e1cec12f247/20022-a-health-and-human-rights.-issue-paper_638.pdf
98. Vigo D, Patten S, Pajer K, Krausz M, Taylor S, Rush B, Yatham LN. Mental Health of Communities during the COVID-19 Pandemic. Can J Phychiatry (2020) 65:681–7. doi: 10.1177/0706743720926676
99. Sneed RS, Key K, Bailey S, Johnson-Lawrence V. Social and psychological consequences of the COVID-19 pandemic in African-American communities: Lessons from Michigan. Psychol Trauma. (2020) 12:446–8. doi: 10.1037/tra0000881
100. Puras D, Gooding P. Mental health and human rights in the 21st century. World Psychiatry. (2019) 18:42–3. doi: 10.1002/wps.20599
101. World Health Organization. Ethical Considerations in Developing a Public Health Response to Pandemic Influenza (2007). Available online at: https://apps.who.int/iris/bitstream/handle/10665/70006/WHO_CDS_EPR_GIP_2007.2_eng.pdf;jsessionid=C4EF6DC7DD0A26339AA681A7F6051A82?sequence=1
102. Institute of Medicine (US) Forum on Microbial Threats. Ethical and Legal Considerations in Mitigating Pandemic Disease: Workshop Summary (2007). Available online at: www.ncbi.nlm.nih.gov/books/NBK54169/
103. Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. (2020) 7:547–60. doi: 10.1016/S2215-0366(20)30168-1
104. World Health Organization. Addressing Human Rights as Key to the COVID-19 Response (2020). Available online at: www.who.int/publications/i/item/addressing-human-rights-as-key-to-the-covid-19-response
105. United Nations. Human Rights (2020). Available online at: www.un.org/en/sections/issues-depth/human-rights/
Keywords: mental and behavioral health, human rights, lockdown, health care worker [non-MESH], stigma and discrimination, vulnerable populations, LMICs (low and middle income countries)
Citation: Rahman M, Ahmed R, Moitra M, Damschroder L, Brownson R, Chorpita B, Idele P, Gohar F, Huang KY, Saxena S, Lai J, Peterson SS, Harper G, McKay M, Amugune B, Esho T, Ronen K, Othieno C and Kumar M (2021) Mental Distress and Human Rights Violations During COVID-19: A Rapid Review of the Evidence Informing Rights, Mental Health Needs, and Public Policy Around Vulnerable Populations. Front. Psychiatry 11:603875. doi: 10.3389/fpsyt.2020.603875
Received: 08 September 2020; Accepted: 23 November 2020;
Published: 08 January 2021.
Edited by:
Wulf Rössler, Charité – Universitätsmedizin Berlin, GermanyReviewed by:
Samia Tasnim, Texas A&M University, United StatesFred Were, University of Nairobi, Kenya
Andy Shih, Autism Speaks, United States
Copyright © 2021 Rahman, Ahmed, Moitra, Damschroder, Brownson, Chorpita, Idele, Gohar, Huang, Saxena, Lai, Peterson, Harper, McKay, Amugune, Esho, Ronen, Othieno and Kumar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Manasi Kumar, bWFubmlfM2luQGhvdG1haWwuY29t
 Muhammad Rahman
Muhammad Rahman Rabab Ahmed
Rabab Ahmed Modhurima Moitra
Modhurima Moitra Laura Damschroder
Laura Damschroder Ross Brownson
Ross Brownson Bruce Chorpita5
Bruce Chorpita5 Priscilla Idele
Priscilla Idele Fatima Gohar
Fatima Gohar Shekhar Saxena
Shekhar Saxena Joanna Lai
Joanna Lai Stefan Swartling Peterson
Stefan Swartling Peterson Gary Harper
Gary Harper Beatrice Amugune
Beatrice Amugune Keshet Ronen
Keshet Ronen Caleb Othieno
Caleb Othieno Manasi Kumar
Manasi Kumar