- 1Department of Psychiatry, University of Cambridge, Cambridge, United Kingdom
- 2The Jockey Club School of Public Health and Primary Care, The Chinese University of Hong Kong, Hong Kong, China
- 3Department of Biostatistics and Epidemiology, Shenzhen University Health Science Center, Shenzhen, China
- 4Cambridgeshire and Peterborough NHS Foundation Trust, Cambridge, United Kingdom
- 5Department of Public Health and Primary Care, University of Cambridge, Cambridge, United Kingdom
- 6College of Public Administration, Central China Normal University, Wuhan, China
To date, there is a paucity of information regarding the effect of COVID-19 or lockdown on mental disorders. We aimed to quantify the medium-term impact of lockdown on referrals to secondary care mental health clinical services. We conducted a controlled interrupted time series study using data from Cambridgeshire and Peterborough NHS Foundation Trust (CPFT), UK (catchment population ~0.86 million). The UK lockdown resulted in an instantaneous drop in mental health referrals but then a longer-term acceleration in the referral rate (by 1.21 referrals per day per day, 95% confidence interval [CI] 0.41–2.02). This acceleration was primarily for urgent or emergency referrals (acceleration 0.96, CI 0.39–1.54), including referrals to liaison psychiatry (0.68, CI 0.35–1.02) and mental health crisis teams (0.61, CI 0.20–1.02). The acceleration was significant for females (0.56, CI 0.04–1.08), males (0.64, CI 0.05–1.22), working-age adults (0.93, CI 0.42–1.43), people of White ethnicity (0.98, CI 0.32–1.65), those living alone (1.26, CI 0.52–2.00), and those who had pre-existing depression (0.78, CI 0.19–1.38), severe mental illness (0.67, CI 0.19–1.15), hypertension/cardiovascular/cerebrovascular disease (0.56, CI 0.24–0.89), personality disorders (0.32, CI 0.12–0.51), asthma/chronic obstructive pulmonary disease (0.28, CI 0.08–0.49), dyslipidemia (0.26, CI 0.04–0.47), anxiety (0.21, CI 0.08–0.34), substance misuse (0.21, CI 0.08–0.34), or reactions to severe stress (0.17, CI 0.01–0.32). No significant post-lockdown acceleration was observed for children/adolescents, older adults, people of ethnic minorities, married/cohabiting people, and those who had previous/pre-existing dementia, diabetes, cancer, eating disorder, a history of self-harm, or intellectual disability. This evidence may help service planning and policy-making, including preparation for any future lockdown in response to outbreaks.
Introduction
The 2019 novel coronavirus disease (COVID-19) was declared a pandemic by the World Health Organization (WHO) on 11 March 2020 (1). To minimize transmission, “social distancing” or “lockdown” measures were adopted as public health measures globally, including in the United Kingdom (UK), which commenced social distancing from 16 May 2020 and lockdown rules from 23 March 2020.
It is already evident that COVID-19 and lockdown have the potential to lead to pervasive mental health problems. Li et al. (2) surveyed 5,033 individuals from the general population in China following the local onset of COVID-19 and found that 20.4% of people had anxiety or depression or both. Ni et al. (3) surveyed 1,577 adults in China and found that 23.8 and 19.2% of people reported probable anxiety and depression, respectively. Moghanibashi-Mansourieh (4) surveyed 10,754 individuals from the general population in Iran and found that 19.1% of people had severe symptoms of anxiety. A survey in the UK (5) involving 2,198 members of the general population also revealed widespread concerns about COVID-19 and mental health problems. A recent position paper (6) noted that besides the rise in adverse mental symptoms, there is also a risk of increasing numbers of people suffering clinically significant mental disorders. However, the effects of the COVID-19 pandemic and state-imposed lockdown on public mental health in a clinical setting have not been evaluated systematically, and current evidence is mainly based on online surveys. In addition, the evidence relating to long-term consequences of the COVID-19 lockdown upon mental health is sparse (6). Such evidence is urgently needed to inform interventions and for policy makers to formulate an appropriate response.
It has been suggested (7–12) that vulnerable groups such as children and adolescents, pregnant women, older adults, and people with pre-disposing physical and mental health conditions could suffer disproportionately from mental health problems resulting from the current COVID-19 lockdown. Relevant evidence is similarly sparse, and similarly required.
The present study investigated the impact of lockdown on referrals to secondary care mental health clinical services. In addition to examining the overall impact, we also performed a series of sub-group analyses paying special attention to vulnerable groups. As well as the short-term (instantaneous) effect of lockdown, we focused on the subsequent rate of change over time (the longer-term, or medium-term, effect).
Methods
Study Design and Participants
We conducted a controlled interrupted time series (CITS) study (13), testing the hypothesis of a causal effect of COVID-19 lockdown, using a historical control group (14). Data were derived from the electronic clinical records of Cambridgeshire and Peterborough NHS Foundation Trust (CPFT), UK. CPFT provides physical and mental health services to a population of approximately 0.86 million. Its records contains patient information recorded during routine treatment, such as age, gender, ethnicity, marital status, referral time, referral destination, diagnoses, and (in free text) some prescription data.
De-identified data were extracted via the CPFT Research Database (NHS Research Ethics 17/EE/0442). We included all records from 2020-01-01 to 2020-03-15 as the pre-lockdown period in 2020, and records from 2020-03-23 to 2020-05-19 as the post-lockdown period. Records from 16 March to 22 March were excluded because this was a transition period (from social distancing to lockdown). Records from 2019-01-01 to 2019-03-15, and from 2019-03-23 to 2019-05-19, were included as the corresponding control year. Weekends were excluded, and bank holidays were excluded from day-by-day analyses.
Variables
We examined daily referral numbers to mental health service teams. Subgroup CITSs were also conducted, by gender, age, ethnicity, marital status, referral urgency, referral destination (service referred to), and pre-existing diseases. Age was divided into three ranges: 0–19 years (children and adolescents), 20–64 years (working-age adults), and ≥65 years. Ethnicity was categorized into three groups: White, ethnic minorities, and unknown. Marital status was categorized into two groups: cohabiting/married, and single/divorced/widowed. Level of urgency was recorded by clinicians and was grouped into two levels: routine, and urgent/emergency. Referral destination was grouped into 13 team/service categories: crisis teams, liaison psychiatry, personality disorder services, perinatal mental health, autistic spectrum disorder services, eating disorder services, learning disability teams, substance misuse teams, memory or dementia services, psychological therapy services, forensic services, community mental health teams, and others.
Pre-existing diseases were judged based on WHO International Classification of Diseases (ICD-10) codes and on prescription information. Clinician-recorded diagnoses were present in coded data. Medicine information was extracted from free text using GATE-based natural language processing (NLP) software (15). The diseases we focused on included dementia (recorded with ICD-10 codes F00-F03 and G30, or indicated by mentions of cholinesterase inhibitors or glutamate receptor antagonists), substance misuse (F10-F19), severe (serious) mental illness (F20-F29, F30, and F31, or taking antipsychotics), depression (F32 or F33, or taking antidepressants), anxiety (F41 or F42), reaction to severe stress/adjustment disorders (F43), eating disorders (F50), personality disorders (F60-F69), intellectual disability (F70-F79), intentional self-harm (X60-X84), diabetes mellitus (E10-E14, or taking hypoglycemic agents), hypertension or cardiovascular or cerebrovascular disease (I10-I13, I15, I21-I25, and I60-I69, or taking ACE inhibitors, angiotensin-II receptor antagonists, beta blockers, calcium channel antagonists, or diuretics), dyslipidemia (E78, or taking lipid-lowering medications), asthma or chronic obstructive pulmonary disease (COPD) (J44, J45, or taking oral or inhaled corticosteroids, bronchodilators, or anti-inflammatory drugs used for airways disease, accepting that oral corticosteroids may also indicate other inflammatory disorders), and cancer (C00-C97, or taking drugs specifically licensed for cancer). Identification of these diseases were based on CPFT records up to 1 year before a referral was made, except for lifelong diseases including dementia, severe mental illness and the aforementioned physical diseases (for which a record at any time was included). The medicines referred to were selected according to UK National Institute for Health and Care Excellence (NICE) guidelines and are listed in Supplementary Table 1.
Statistical Analysis
We report referral frequency as mean with standard deviation. For the CITS, data were fitted using the following equation:
where y is the daily number of referrals; Time is the time point of data (within a phase); Phase indicates “before/after lockdown or equivalent period” (0 before lockdown in 2020 or the equivalent period in 2019, and 1 after lockdown in 2020 or the equivalent period in 2019); Phase × Time was the time after lockdown in 2020 or the equivalent point in 2019; Year indicates 2020 (0 for control data from 2019, or 1 for 2020); Year × Time was time for 2020 and 0 for 2019; Year × Phase was 1 after lockdown, or 0 before lockdown and during the control year; Year × Phase × Time was the time after lockdown, or 0 before lockdown and during the control year.
The coefficients in equation 1 are described elsewhere (16) and in Table 2. Two are of particular importance with respect to lockdown. β6 reflects the short-term change (instantaneous effect) resulting from lockdown, over and above any equivalent change that may have occurred in 2019. β7 was the coefficient of primary interest in this study, and represents the longer-term effect of lockdown, namely the slope change in referral rate following lockdown (after any instantaneous effect and relative to the pre-lockdown slope), over and above any equivalent change in the control year (2019).
Equation 1 was fitted by negative binomial regression, in view of overdispersion seen in the referral numbers. To control for seasonal trends, the day of week and month were also included in the regression. The Breusch–Godfrey and Breusch–Pagan tests were used to check for autocorrelation and heteroskedasticity of residuals, respectively. To interpret the fitted result, a linear approximation to the negative binomial was performed by estimating the marginal effects (ME) and 95% confidence intervals (CI) for the means.
Sensitivity analyses were conducted by examining weekly instead of daily referral numbers.
All statistical analysis were performed using R (version 3.5.0). Statistical significance was defined as P < 0.05, and all tests were two-tailed. Missing data were not imputed.
Patient and Public Involvement
Service user and carer representatives assessed this programme of work and approved it as members of the CPFT Research Database Oversight Committee, but were not involved in the development of this research question or the outcome measures, or in developing plans for the design and implementation of the study.
Results
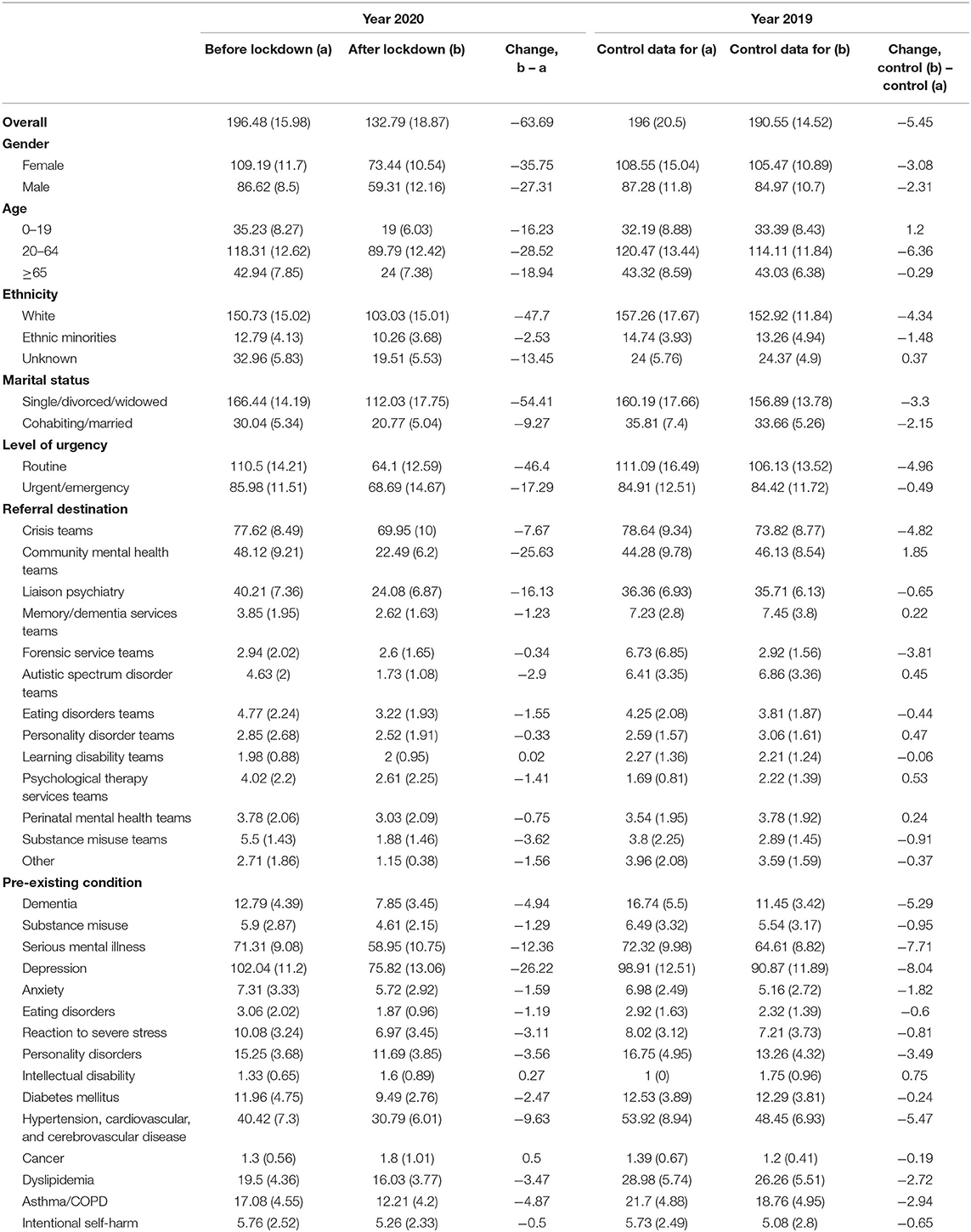
Table 1 shows the number of referrals before and after lockdown in 2020, and during the equivalent control periods. After lockdown, there was an immediate decrease in the number of referrals to mental health services. A decrease was also seen in the control period, but the decrease was much larger in 2020 than in 2019. Similar results were observed for subgroups. As shown in Figure 1, there was no difference in the trend between the pre-lockdown period in 2020 and the equivalent period in 2019. However, after lockdown, there was a substantial drop in the referral rate and then an acceleration of referrals compared to the control period.
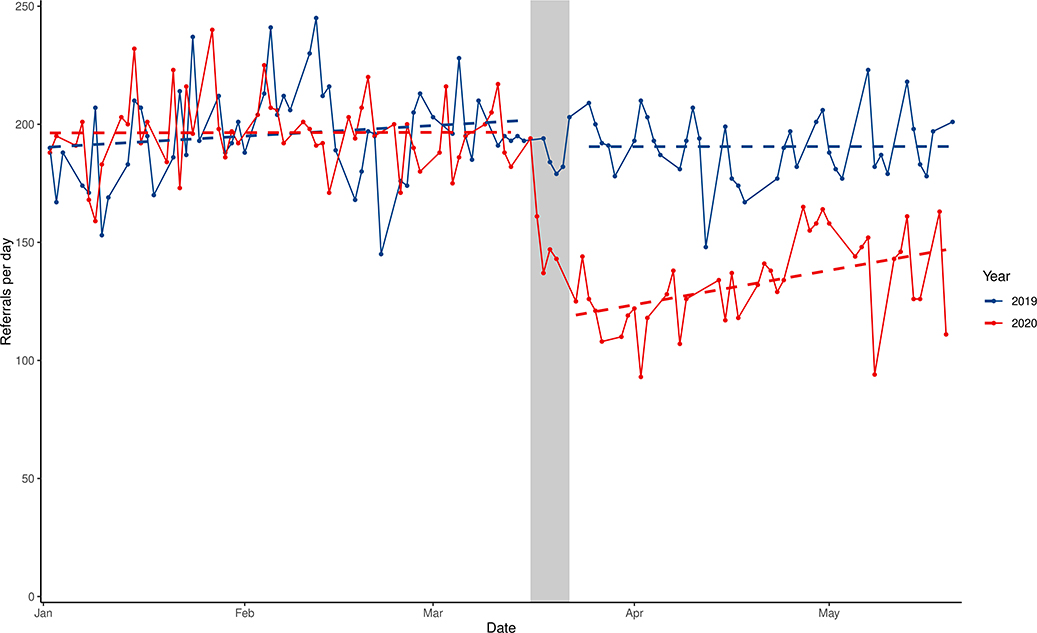
Figure 1. Interrupted time series analysis of referrals to secondary care mental health services in 2020 (red) and 2019 (blue). The dashed line is the model fit. The gray area indicates the transition period from social distancing (16 March 2020) to lockdown (23 March 2020).
Table 2 shows the overall regression results. After controlling for seasonal trends, neither the mean referral rate (β4, 6.06, 95% CI −6.41 to 18.53) nor the time trend in referral rate (β5, −0.21, CI −0.58 to 0.16) was significantly different between the pre-lockdown period in 2020 and its control period in 2019. This indicated that 2019 could be treated as a homogenous counterpart to 2020, before lockdown. Controlling for other temporal effects, lockdown resulted in an immediate decrease in the total number of referrals, by 72 referrals·day−1 (short-term effect, β6, CI −85.13 to −58.14), and a subsequent acceleration in referrals, of 1.21 referrals·day−2 (medium-term effect, β7, CI 0.41 to 2.02). There was no significant autocorrelation or heteroskedasticity in the fitted residuals (see Supplementary Table 2, Supplementary Figure 1).
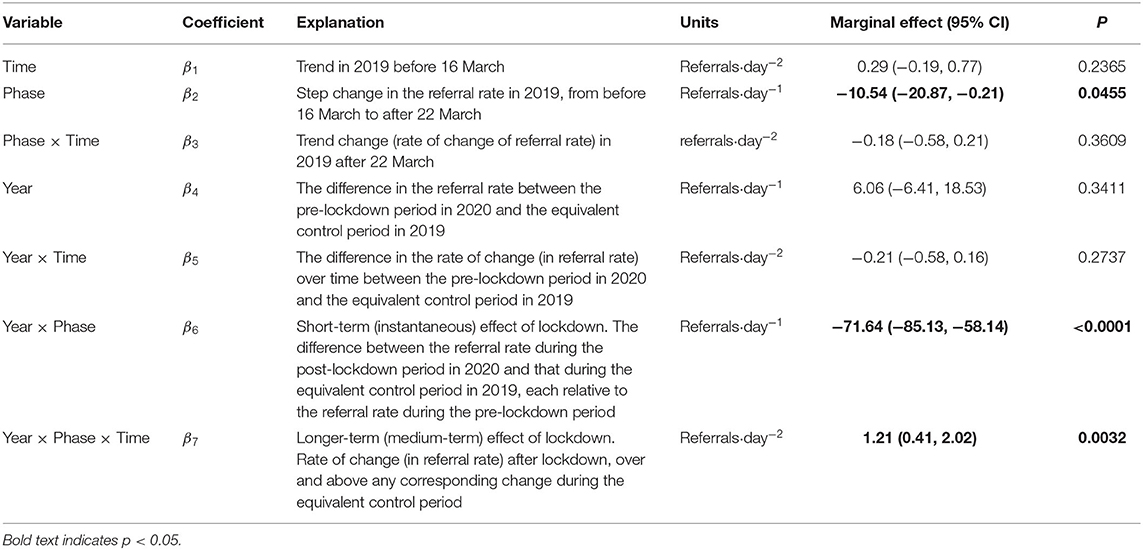
Table 2. Overall controlled interrupted time-series analysis: negative binomial regression adjusted for seasonal effects (month and day of week). The dependent variable is the referral rate (referrals·day−1).
Subgroup analyses are shown in Figure 2 (short-term effect) and Figure 3 (longer-term effect). The immediate decrease in referral rate to mental health services (β6) remained statistically significant for both genders; all age groups; those of White ethnicity; both levels of marital status; both levels of urgency; referrals to community mental health teams, liaison psychiatry, crisis teams, autistic spectrum disorder teams, memory/dementia services, and personality disorder services; and for those who had pre-existing depression, hypertension/cardiovascular/cerebrovascular disease, and reaction to severe stress. After these immediate effects of lockdown, there was an acceleration (β7) in urgent/emergency referrals (0.96 referrals·day−2, CI 0.39 to 1.54), and in referrals to liaison psychiatry (0.68, CI 0.35 to 1.02) and mental health crisis teams (0.61, CI 0.20 to 1.02). The acceleration remained significant for both genders (females 0.56, CI 0.04 to 1.08, males 0.64, CI 0.05 to 1.22); working-age adults (0.92, CI 0.42 to 1.43); those of White ethnicity (0.98, CI 0.32 to 1.65), those living alone (1.26, CI 0.52 to 2.00); and those who had previous or pre-existing depression (0.78, CI 0.19 to 1.34), severe mental illness (0.67, CI 0.19 to 1.15), hypertension/cardiovascular/cerebrovascular disease (0.56, CI 0.24 to 0.89), personality disorders (0.32, CI 0.12 to 0.51), asthma/COPD (0.28, CI 0.08 to 0.49), dyslipidemia (0.26, CI 0.04 to 0.47), anxiety (0.21, CI 0.08 to 0.34), substance misuse (0.20, CI 0.06 to 0.34), or reactions to severe stress (0.17, CI 0.01 to 0.32). No significant longer-term rate changes were observed for children and adolescents, older adults, people of ethnic minorities, married/cohabiting people, or those who had pre-existing dementia, diabetes, cancer, eating disorder, a history of intentional self-harm, or intellectual disability.
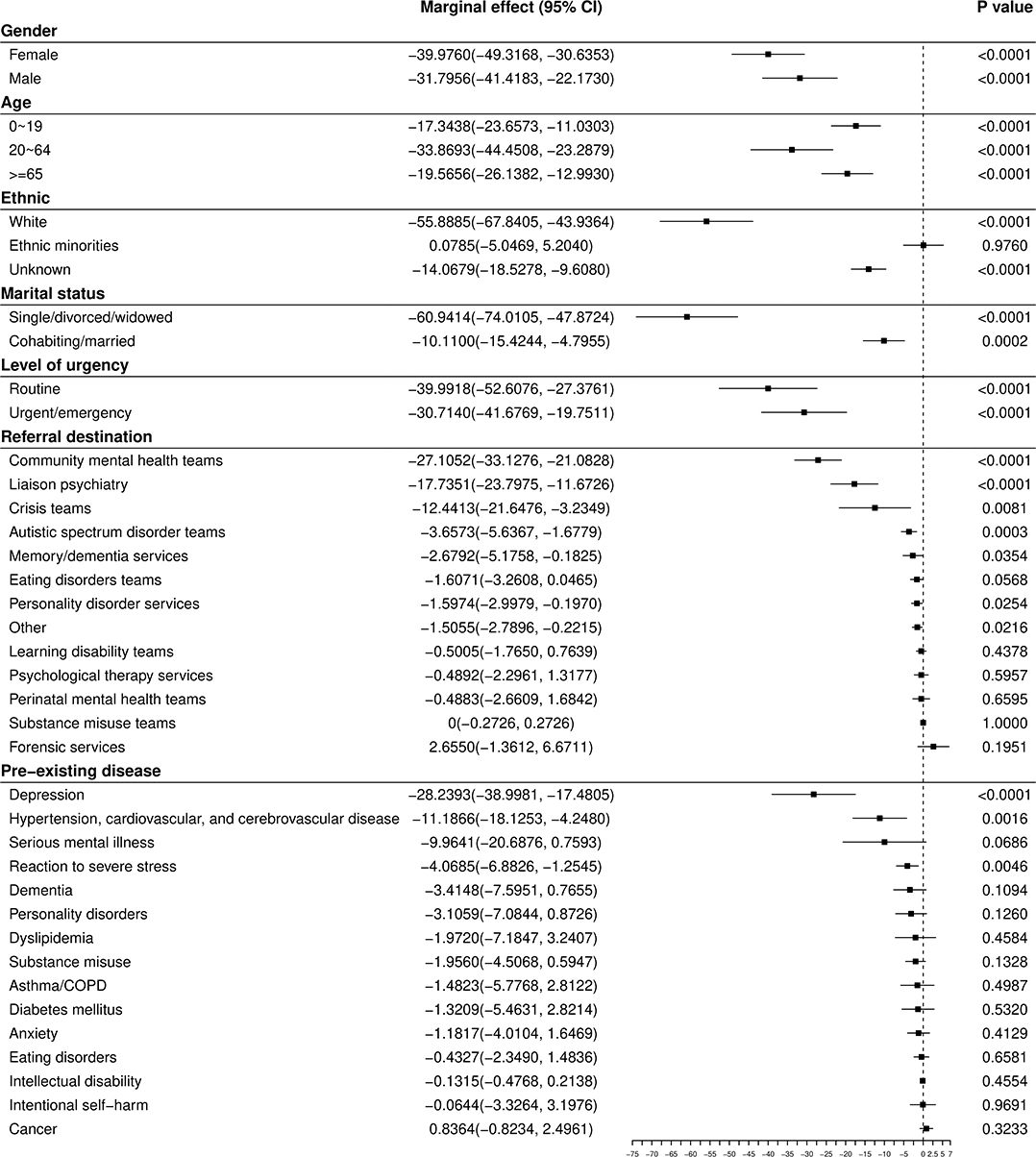
Figure 2. Short-term (β6) effects of COVID-19 lockdown on the daily number of referrals to mental health services for subgroups. Units are referrals·day−1.
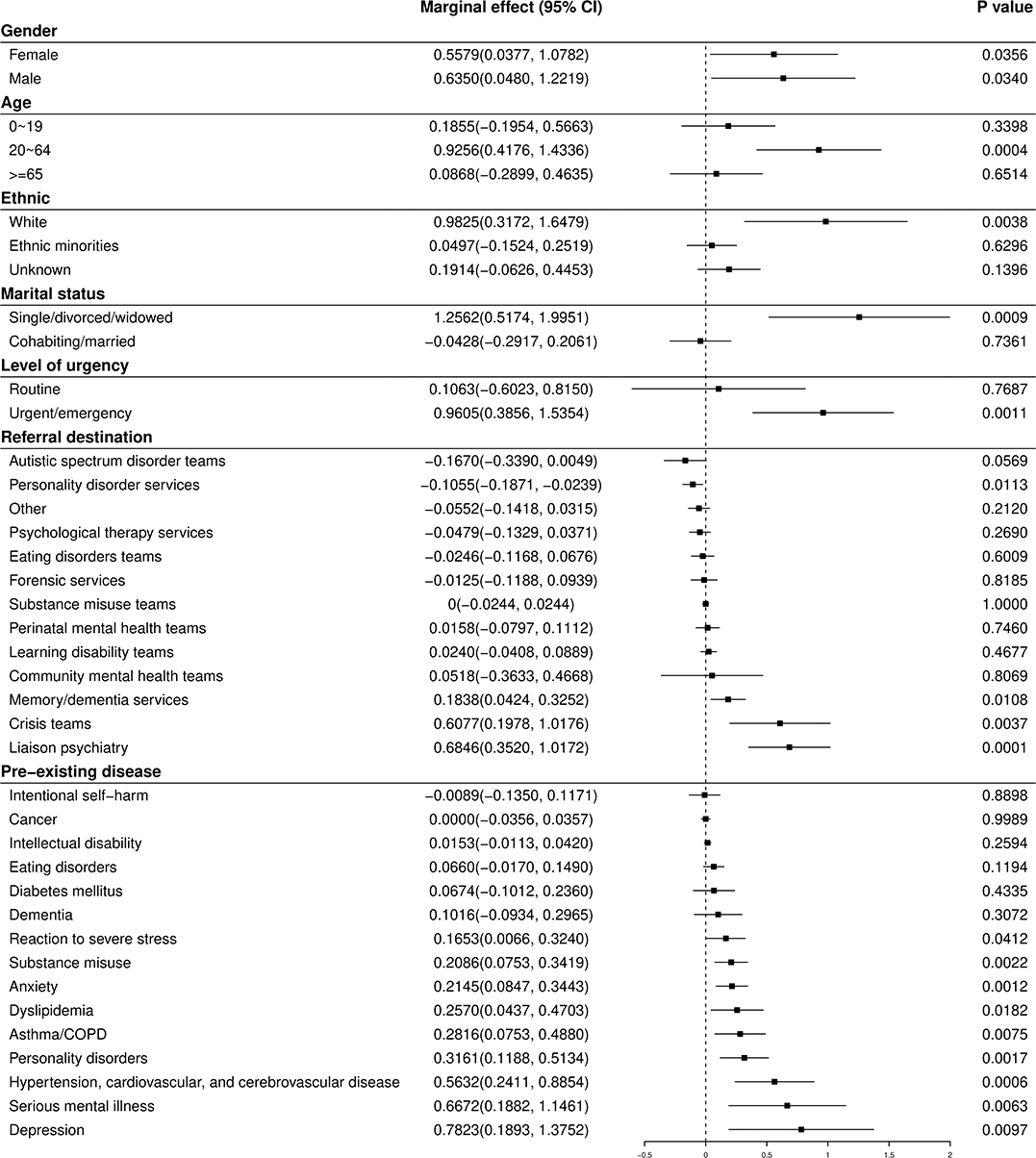
Figure 3. Medium-term (β7) effects of COVID-19 lockdown on the time trend in referrals to mental health services for subgroups. Units are referrals·day−2.
Sensitivity analyses confirmed this pattern of results (Supplementary Figures 2, 3).
Discussion
To our knowledge, this is the first study to evaluate systematically the longer-term effects of COVID-19 lockdown on a population's mental health in a clinical setting via a detailed examination of the trajectory of referral numbers. With a rigorous study design to detect causal effects in time series data, we found that after an initial decrease (17), lockdown led in the medium term to an acceleration in the rate of referrals. The significant longer-term effects revealed in our study are generally consistent with the mental health concerns associated with COVID-19 raised by others. However, the finding was to some extent inconsistent with a study conducted by Wang et al. (18). They conducted two online cross-sectional studies in China, 4 weeks apart, and found no significant changes in scores of depression, anxiety, and stress. This might be partially attributed to the variations in methodology and characteristics of study participants (e.g., the online design, the relatively small sample size of Wang's study, and the measurement of self-reported mental health problems). Given that our study was conducted in a clinical setting, had a longer duration, and used a more rigorous design for causal inference, we suggest our findings are more representative of clinical practice compared with previous cross-sectional or online surveys that used screening scales for mental disorders.
The significant medium-term effects of COVID-19 lockdown on referrals to mental health services were observed in multiple subgroups, supporting the validity of the findings. For instance, after lockdown, referrals accelerated again across genders. Unexpectedly, no such acceleration was observed among those aged ≤19 or ≥65, who have been suspected to be especially vulnerable to mental health problems resulting from social distancing or lockdown (10, 12, 19–21), even though all age groups exhibited the significant instantaneous drop in referrals at lockdown. The lack of acceleration in referrals for older adults after lockdown was also to some extent inconsistent with a study (22) conducted in Hong Kong at the time of the severe acute respiratory syndrome (SARS) epidemic in 2003, which found SARS to be associated with a 30% increase in suicide in those aged ≥65. A possible reason why referrals did not accelerate again for this group may have been that some older people who lived alone and without close support may have lost their capability to access services as usual (19). Fear of contracting COVID-19 infection in a healthcare setting might also have deterred people from seeking help for their mental health, especially for the elderly (for whom a UK public campaign emphasized their additional vulnerability).
Similarly, we did not observe a significant post-lockdown acceleration in referrals for those from ethnic minorities, though this acceleration was significant for those of White ethnicity (indeed, the acceleration for the ethnic minority group was significantly less). Although the immediate lockdown-associated change in referrals for those of ethnic minorities was also not significant, this observation, coupled with the fact that ethnic minority groups are already at elevated risk of dying from COVID-19 in the UK (23), raises the concern that they may not be obtaining mental health support proportionally following lockdown. Together with the lack of acceleration observed in children/adolescents and elderly people, these findings should prompt consideration as to whether these represent disadvantaged groups requiring active mental health intervention.
A significant contribution of this study is that we explored the post-lockdown trends in referral by service referred to, which indirectly suggests the type and degree of mental disorders to which the lockdown may lead. The post-lockdown acceleration in referrals to liaison psychiatry and crisis teams is in keeping with the fact that the acceleration was for urgent/emergency rather than routine referrals (which may also reflect a reduction in routine services). It has been hypothesized (6) and suggested by two cross-sectional studies that COVID-19 might lead to an increase in depressive symptoms and anxiety amongst pregnant women (24, 25). In contrast, our study found neither an initial change nor a subsequent rate of change in the referral rate to perinatal mental health teams. This may reflect service supply as well as patient demand factors, but this inconsistency clearly shows that the increase of mental symptoms assessed by screening scales may not necessarily predict clinical referrals for mental disorders.
This study also provides evidence about the longer-term effect of lockdown on referrals for patients with pre-existing diseases, suggesting indirectly which groups of patients suffer more mental ill health during the lockdown, and providing implications for resource planning and clinical management. Our results give support to concerns that those with severe mental illness (11, 26, 27) would be particularly vulnerable to the long-term effects of lockdown. Our results also indicate that patients with previous/pre-existing depression, personality disorders, anxiety, substance misuse, and reactions to severe stress also required accelerating rates of referral after lockdown, and may need early intervention to prevent the relapse or aggravation of pre-existing mental disorders or the emergence of new problems. Previous cross-sectional studies (28–31) indicated that people with poorer self-reported health status, or comorbid chronic diseases, were more likely to report mental health problems. Our study found that patients who had hypertension, cardiovascular, cerebrovascular disease, asthma, COPD, or dyslipidemia showed accelerating rates of mental health referrals after COVID-19 lockdown. [Hypertension and dyslipidemia are perhaps notable as largely asymptomatic disorders; the association here may reflect an indirect relationship via other conditions, be they physical, such as other cardiometabolic diseases, or psychiatric, such as depression (32).] Special attention may need to be paid to the mental health of patients with chronic cardiovascular or respiratory diseases.
Notably, referral types that showed the greatest initial drop (Figure 2) tended to show the largest subsequent rate increase (Figure 3). Referral numbers reflect the actions of professionals, and the instantaneous drop reflected, in part, attempts by health services to minimize the probability of patients entering high-risk areas for infection unnecessarily (17), and to release resources for the management of patients with COVID-19. However, it is less clear that this explains the subsequent increase in referral rates. Therefore, although it is possible that the longer-term effects identified in this study may not result solely from the social consequences of COVID-19 lockdown but also from adaptation and “rebound” of the health system from the initial sharp decline resulting from lockdown, the prior probability that the changes observed were caused by the pandemic is extremely high and this may have been direct or via a range of indirect mechanisms. For example, these effects may reflect both changes in supply (reduced provision of health services, and the prioritization of urgent over routine referrals with discouragement of routine referral) as well as changes in patient-led demand (17). Regression to the mean (“what went down most, came up most”) cannot explain our data fully. Routine referrals, for example, decreased substantially but then did not increase accordingly. This may have reflected service-driven pressures to reduce non-urgent activity. Referrals for people who were married/cohabiting dropped at lockdown, but then did not increase subsequently, perhaps reflecting less mental health need in this group compared with people who live alone. Referrals for people with pre-existing asthma/COPD did not decrease significantly at lockdown but still increased subsequently. This is in keeping with the suggestion that COVID-19 imposes particular additional mental stress on patients with pre-existing respiratory disease (33, 34).
Our findings are, of course, correlational and do not prove causality. However, a number of potential mitigating strategies may be applicable to “lockdown.” First, mental health services must to be able to deliver services to all in need, by operating a flexible mix of in-person and remote (e.g., videoconferencing) consultations to balance clinical and infection control requirements; there is not a “one size fits all” approach (35). Secondly, referrers should be encouraged to have a low threshold for potentially vulnerable populations (including children, the elderly, those of ethnic minorities, those who are socially isolated, and those with pre-existing mental disorders and physical comorbidities). Thirdly, evidence-based measures to support population mental health (36)—including the promotion of community cohesion (37)—are likely to be helpful, and to require government support (36). Such interventions may be constrained additionally by the economic effects of the pandemic, and governments must balance economic and health considerations. However, it is notable that personal economic loss during lockdown is associated with worsening of mental health, particularly an increase in depressive symptoms (38), and that explicit consideration of the trade-offs between infective and economic/wellbeing considerations may be required for maximum public benefit (39).
Our study had several limitations. First, we used clinical data up to ~2 months after UK lockdown; this may not be long enough for some effects of lockdown to have become evident. Second, the referral data used in this study could only reflect problems severe enough to require referral to secondary care mental health services. Thus, this study may underestimate longer-term effects, as some individuals may have been suffering mental health problems resulting from COVID-19/lockdown but used primary care services only, or did not seek mental health services at all. The present findings thus highlight mental health needs and a disease burden that should be prioritized for attention and treatment. Third, classifying by diagnosis instead of referral service would be more helpful to establish disease patterns, but frequent missing coded data on diagnosis following urgent or emergency referrals impeded our analysis. Fourth, some types of referral, for example for people with diabetes or cancer, were relatively rare in the dataset, posing a challenge (via low power) to identifying the effects of lockdown upon them. We addressed this by performing sensitivity analyses examining weekly instead of daily referral numbers; this confirmatory analysis supported our primary results. Finally, our findings may not generalize to other areas, such as with very different COVID-19 infection rates, or health service organization. However, measures such as social distancing and lockdown are being adopted in similar ways internationally, so the results of the present study may be useful for other regions and countries.
Conclusions
The present study, using clinical records and the optimal causal inference study design for time series analysis, is compatible with the hypothesized negative long-term impact of lockdown on mental health. After an initial drop in referrals, we observed a post-lockdown acceleration in urgent and emergency mental health referrals. This acceleration was significant for adults of working age, people who live alone, and those with a broad range of pre-existing mental disorders and a subset of physical comorbidities. No such acceleration was observed for children/adolescents, older adults, and those from ethnic minorities; one possibility is that they may be facing insufficient access to mental health services. The timely evidence in this study could help the response of mental health systems and policy to support population mental health, as well as in preparation for any future lockdown in response to further outbreaks.
Data Availability Statement
The data analyzed in this study is subject to the following licenses/restrictions: Patient-level data is not publicly available, under NHS Research Ethics terms. Source code and summary data are available on request. Requests to access these datasets should be directed to Rudolf N. Cardinal, cm5jMTAwMSYjeDAwMDQwO2NhbS5hYy51aw==.
Ethics Statement
The studies involving human participants were reviewed and approved by the NHS Health Research Authority Cambridge Central Research Ethics Committee (reference 17/EE/0442) and CPFT Research Database Oversight Committee. Written informed consent from the participants' legal guardian/next of kin was not required to participate in this study in accordance with national legislation and institutional requirements.
Author Contributions
SC and RC contributed to the study design and wrote the first draft. SC and JL processed the data. SC conducted the statistical analyses. All authors edited and approved the final manuscript.
Funding
SC's, JN's, and RC's research was supported by the Medical Research Council (grant MC_PC_17213 to RC). This research was supported in part by the UK National Institute for Health Research (NIHR) Cambridge Biomedical Research Centre.
Disclaimer
The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health and Social Care.
Conflict of Interest
RC consults for Campden Instruments Ltd and receives royalties from Cambridge University Press, Cambridge Enterprise, and Routledge.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank Phil Alsop, Chris Carling, Golam Khandaker, Linda Jones, Rachel Kyd, Iliana Rokkou, Ginny Russell, and Mary-Beth Sherwood for providing oversight. We thank our referees for helpful comments.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2020.585915/full#supplementary-material
References
1. World Health Organization. Timeline of WHO's Response to COVID-19. (2020). Available online at: https://www.who.int/news-room/detail/29-06-2020-covidtimeline (accessed July 7, 2020).
2. Li J, Yang Z, Qiu H, Wang Y, Jian L, Ji J, et al. Anxiety and depression among general population in China at the peak of the COVID-19 epidemic. World Psychiatry. (2020) 19:249–50. doi: 10.1002/wps.20758
3. Ni MY, Yang L, Leung CMC, Li N, Yao XI, Wang Y, et al. Mental health, risk factors, and social media use during the COVID-19 epidemic and cordon sanitaire among the community and health professionals in Wuhan, China: cross-sectional survey. JMIR Ment Health. (2020) 7:e19009. doi: 10.2196/19009
4. Moghanibashi-Mansourieh A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J Psychiatr. (2020) 51:102076. doi: 10.1016/j.ajp.2020.102076
5. Academy of Medical Royal Colleges, MQ. Survey Results: Understanding People's Concerns About the Mental Health Impacts of the COVID-19 Pandemic. (2020). Available online at: https://acmedsci.ac.uk/file-download/99436893 (accessed May 22, 2020).
6. Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. (2020) 7:547–60. doi: 10.1016/S2215-0366(20)30168-1
7. Zeng L-N, Chen L-G, Yang C-M, Zeng L-P, Zhang L-Y, Peng T-M. Mental health care for pregnant women in the COVID-19 outbreak is urgently needed. Women Birth. (2020) doi: 10.1016/j.wombi.2020.03.009
8. Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med. (2020) 383:510–12. doi: 10.1056/NEJMp2008017
9. Yang Y, Li W, Zhang Q, Zhang L, Cheung T, Xiang Y-T. Mental health services for older adults in China during the COVID-19 outbreak. Lancet Psychiatry. (2020) 7:e19. doi: 10.1016/S2215-0366(20)30079-1
10. Lee J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc Health. (2020) 4:421. doi: 10.1016/S2352-4642(20)30109-7
11. Druss BG. Addressing the COVID-19 pandemic in populations with serious mental illness. JAMA Psychiatry. (2020) 77:891–2. doi: 10.1001/jamapsychiatry.2020.0894
12. Golberstein E, Wen H, Miller BF. Coronavirus disease 2019. (COVID-19) and mental health for children and adolescents. JAMA Pediatr. (2020) 174:819–20. doi: 10.1001/jamapediatrics.2020.1456
13. Hawton K, Bergen H, Simkin S, Dodd S, Pocock P, Bernal W, et al. Long term effect of reduced pack sizes of paracetamol on poisoning deaths and liver transplant activity in England and Wales: interrupted time series analyses. BMJ. (2013) 346:f403. doi: 10.1136/bmj.f403
14. Lopez Bernal JA, Lu CY, Gasparrini A, Cummins S, Wharam JF, Soumerai SB. Association between the 2012 Health and Social Care Act and specialist visits and hospitalisations in England: a controlled interrupted time series analysis. PLoS Med. (2017) 14:e1002427. doi: 10.1371/journal.pmed.1002427
15. Cardinal RN. Clinical records anonymisation and text extraction. (CRATE): an open-source software system. BMC Med Inform Decis Mak. (2017) 17:50. doi: 10.1186/s12911-017-0437-1
16. Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. (2017) 46:348–55. doi: 10.1093/ije/dyw098
17. Chen S, Jones PB, Underwood BR, Moore A, Bullmore ET, Banerjee S, et al. The early impact of COVID-19 on mental health and community physical health services and their patients' mortality in Cambridgeshire and Peterborough, UK. J Psychiatr Res. (2020) 131:244–54. doi: 10.1016/j.jpsychires.2020.09.020
18. Wang C, Pan R, Wan X, Tan Y, Xu L, McIntyre RS, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. (2020) 87:40–48. doi: 10.1016/j.bbi.2020.04.028
19. Wang H, Li T, Gauthier S, Yu E, Tang Y, Barbarino P, et al. Coronavirus epidemic and geriatric mental healthcare in China: how a coordinated response by professional organizations helped older adults during an unprecedented crisis. Int Psychogeriatr. (2020) 32:1117–1120. doi: 10.1017/S1041610220000551
20. Webb L. COVID-19 lockdown: a perfect storm for older people's mental health. J Psychiatr Ment Health Nurs. (2020) doi: 10.1111/jpm.12644
21. Banerjee D. The impact of Covid-19 pandemic on elderly mental health. Int J Geriatr Psychiatry. (2020) doi: 10.1002/gps.5320
22. Yip PSF, Cheung YT, Chau PH, Law YW. The impact of epidemic outbreak: the case of severe acute respiratory syndrome. (SARS) and suicide among older adults in Hong Kong. Crisis. (2010) 31:86–92. doi: 10.1027/0227-5910/a000015
23. Office for National Statistics. Coronavirus. (COVID-19) Related Deaths by Ethnic Group, England and Wales: 2 March 2020 to 15 May 2020. (2020). Available online at: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/coronaviruscovid19relateddeathsbyethnicgroupenglandandwales/2march2020to15may2020 (accessed June 19, 2020).
24. Wu Y, Zhang C, Liu H, Duan C, Li C, Fan J, et al. Perinatal depressive and anxiety symptoms of pregnant women during the coronavirus disease 2019 outbreak in China. Am J Obstet Gynecol. (2020) 223:240.e1-9. doi: 10.1016/j.ajog.2020.05.009
25. Durankuş F, Aksu E. Effects of the COVID-19 pandemic on anxiety and depressive symptoms in pregnant women: a preliminary study. J Matern Fetal Neonatal Med. (2020) doi: 10.1080/14767058.2020.1763946
26. Torous J, Keshavan M. COVID-19, mobile health and serious mental illness. Schizophr Res. (2020) 218:36–7. doi: 10.1016/j.schres.2020.04.013
27. Shinn AK, Viron M. Perspectives on the COVID-19 pandemic and individuals with serious mental illness. J Clin Psychiatry. (2020) 81:20com13412. doi: 10.4088/JCP.20com13412
28. Lei L, Huang X, Zhang S, Yang J, Yang L, Xu M. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 epidemic in Southwestern China. Med Sci Monit. (2020) 26:e924609. doi: 10.12659/MSM.924609
29. Tan W, Hao F, McIntyre RS, Jiang L, Jiang X, Zhang L, et al. Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain Behav Immun. (2020) 87:84–92. doi: 10.1016/j.bbi.2020.04.055
30. Gao J, Zheng P, Jia Y, Chen H, Mao Y, Chen S, et al. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE. (2020) 15:e0231924. doi: 10.1371/journal.pone.0231924
31. Özdin S, Bayrak Özdin S. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: the importance of gender. Int J Soc Psychiatry. (2020) 66:504–11. doi: 10.1177/0020764020927051
32. Baune BT, Stuart M, Gilmour A, Wersching H, Arolt V, Berger K. Moderators of the relationship between depression and cardiovascular disorders: a systematic review. Gen Hosp Psychiatry. (2012) 34:478–92. doi: 10.1016/j.genhosppsych.2012.05.013
33. Yohannes AM. COPD patients in a COVID-19 society: depression and anxiety. Expert Rev Respir Med. (2020) doi: 10.1080/17476348.2020.1787835
34. Boyer J. COVID-19, medication-assisted treatment, and increased risk for further respiratory depression. Am J Psychiatry. (2020) 177:636. doi: 10.1176/appi.ajp.2020.20030348
35. Cardinal RN, Meiser-Stedman CE, Christmas DM, Price AC, Denman C, Underwood BR, et al. Simulating a community mental health service during the COVID-19 pandemic: effects of clinician–clinician encounters, clinician–patient–family encounters, symptom-triggered protective behaviour, and household clustering. medRxiv [Preprint]. (2020) doi: 10.1101/2020.04.27.20081505
36. Belkin G, McCray C. ThriveNYC: delivering on mental health. Am J Public Health. (2019) 109:S156–63. doi: 10.2105/AJPH.2019.305040
37. Pridmore S, Ahmadi J, Pridmore W. Suicide of Australians during the Vietnam War. Australas Psychiatry. (2018) 26:149–51. doi: 10.1177/1039856217734740
38. Hertz-Palmor N, Moore TM, Gothelf D, DiDomenico GE, Dekel I, Greenberg DM, et al. Association among income loss, financial strain and depressive symptoms during COVID-19: evidence from two longitudinal studies. medRxiv [Preprint]. (2020) doi: 10.1101/2020.09.15.20195339
Keywords: COVID-19/SARS-CoV-2 coronavirus pandemic, lockdown, secondary care mental health services, controlled interrupted time series analysis, comorbidity
Citation: Chen S, She R, Qin P, Kershenbaum A, Fernandez-Egea E, Nelder JR, Ma C, Lewis J, Wang C and Cardinal RN (2020) The Medium-Term Impact of COVID-19 Lockdown on Referrals to Secondary Care Mental Health Services: A Controlled Interrupted Time Series Study. Front. Psychiatry 11:585915. doi: 10.3389/fpsyt.2020.585915
Received: 21 July 2020; Accepted: 28 October 2020;
Published: 26 November 2020.
Edited by:
Wulf Rössler, Charité – Universitätsmedizin Berlin, GermanyReviewed by:
Elizabeta Blagoja Mukaetova-Ladinska, University of Leicester, United KingdomMichaela Pascoe, Victoria University, Australia, Australia
Copyright © 2020 Chen, She, Qin, Kershenbaum, Fernandez-Egea, Nelder, Ma, Lewis, Wang and Cardinal. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rudolf N. Cardinal, cm5jMTAwMSYjeDAwMDQwO2NhbS5hYy51aw==
 Shanquan Chen
Shanquan Chen Rui She
Rui She Pei Qin3
Pei Qin3 Emilio Fernandez-Egea
Emilio Fernandez-Egea Chuoxin Ma
Chuoxin Ma Rudolf N. Cardinal
Rudolf N. Cardinal