
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 14 January 2021
Sec. Schizophrenia
Volume 11 - 2020 | https://doi.org/10.3389/fpsyt.2020.579484
Introduction: Patients who come to the emergency department because of acute psychiatric symptoms are often not admitted to the correct department timely. The purpose of this study is to identify the clinical characteristics of patients with acute psychiatric symptoms in order to achieve early and correct triage in the emergency room.
Methodology: We conducted a cross-analysis of inpatients who first came to the emergency department with acute psychiatric symptoms and then admitted to the department of neurology or psychiatry between years 2012 and 2018. Among them, 70 patients were rediagnosed and retransferred, with 38 patients to the department of neurology and 32 patients to the department of psychiatry. The clinical characteristics, laboratory examination, and Neuropsychiatric Inventory (NPI) were analyzed.
Results: Patients who were rediagnosed with neurological diseases were more prone to have somatic symptoms (headache, dizziness) (P < 0.05). Because of the atypical early clinical manifestations in the emergency room, fever and positive neurological signs do not necessarily represent the diagnosis of neurological diseases. On the other hand, the absence of these manifestations does not guarantee the diagnosis of psychiatric illness. According to NPI, abnormal behaviors, changes in appetite, and sleep disturbances were more obvious in patients with neurological diseases (P < 0.05), whereas patients with psychiatric disorders often showed prominent irritability (P < 0.05).
Conclusions: Acute psychiatric symptoms are usually complex and diverse. The triage and diagnosisshould be based on multiple factors. After triage, clinical symptoms should be dynamically observed.
The number of patients with mental disorders is increasing worldwide. According to a survey in the United States, one in eight emergency room visits involved acute psychiatric symptoms (1, 2). Conditions behind these psychiatric emergencies often include mental and substance use disorders (2), neurological (such as encephalitis, stroke, multiple sclerosis, etc.), endocrine, and metabolic diseases (3). Sometimes the situations can be life-threatening; as a result, it is critical to make judgments in a timely and accurate manner. Thus, the patients can be admitted to the proper department right away. However, identification of an underlying medical condition presenting as acute psychiatric symptoms can be very challenging sometimes, given the broad spectrum of diseases in the field of psychiatry and neurology. It was estimated that the average emergency room duration of stay for patients with psychiatric symptoms was three times longer than those presenting with physical illnesses and injuries (4).
There are several reasons for this. First, because of the complexity of brain structure and function, neurology and psychiatry have been intertwined since the establishment of the discipline. Many diseases even have overlaps in the pathogenesis, clinical manifestations, and treatment options (5). Second, the clinical manifestations of such patients are often atypical. Fever, seizures, and some focal neurological deficits may not present in the early stages of the disease. Besides, the course of illness is usually short. There is no previous mental stress and no family history of mental illness. Third, these patients with psychiatric symptoms often cooperate poorly in the history taking and neurological as well as physical examinations. Fourth, the triage system of the emergency room in China needs to be improved. The nurses, not the doctors, decide whether the psychiatrists or neurologists see the patient first. According to hospital regulations, if a neurologist was referred, the patient must be admitted immediately to the department of neurology, and vice versa. There is no acute medical unit to accommodate these patients. Logically, several important examinations, such as lumbar puncture, electroencephalography (EEG), and head magnetic resonance imaging (MRI) cannot be completed in the emergency room. Consequently, some patients failed to be admitted to the proper department timely.
In order to allow patients to be admitted to the correct department as soon as possible, at present, the best solution is to identify convenient and efficient clinical parameters, which help to improve the accuracy of triage. Most of the studies that can be retrieved are based on the diagnosis of mental illness. Some red flags were suggested to exclude mimics (3). These include abnormal vital signs, significant abnormalities on physical and neurological examination, impaired consciousness, visual hallucinations, and recent-onset incontinence (6–8). There was also some kind of literature discussing the classification and diagnosis of organic mental disorders (9). Only one literature analyzed 947 inpatients who requested a psychiatric consultation. It was found that 14.6% had a final diagnosis of mental disorder. Advanced age was significantly associated with an increased risk of misidentification of psychiatric symptoms (10). No literature, so far, cross-analyzed the characteristics of those inpatients who were misdiagnosed by both psychiatrists and neurologists. Our study was the first to sort out all inpatients with acute psychiatric symptoms in both departments of neurology and psychiatry. Efforts have been made to comprehensively analyze clinical characteristics, laboratory tests, and imaging results to better distinguish these patients promptly.
From January 2012 to December 2018, inpatients with acute psychiatric symptoms who first came to the emergency room of the First Affiliated Hospital of Chongqing Medical University and then admitted to the department of neurology or psychiatry were screened and cross-analyzed. Patients were enrolled if they were rediagnosed and retransferred. It should be noted that in the emergency room, as a routine, the emergency nurses will first record patients' vital signs and document the onset time, predisposing factors, medical history, family history, history of medication, and substance abuse, before they triage the patients to psychiatrists or neurologists. They also interview the accompanying family members and close friends, especially when the patients are unable to cooperate with the collection of medical history (11).
SPSS 26 software package was applied to process the statistic (IBM Corporation released in 2019, version 26.0, for Macintosh). For categorical variables (dichotomous variables), such as gender, clinical symptoms and signs, and laboratory test results, the χ2 test was used. There are some principles: (1) all theoretical numbers T ≥ 5 and total sample size n ≥ 40, tested by Pearson χ2; (2) if the theoretical number T < 5 but T ≥ 1, and n ≥ 40, the χ2 of the continuity test was used; (3) if there was a theoretical number T < 1 or n < 40, the Fisher test was used. Continuous variables, such as age, course of illness before admission, transfer time, length of stay in the hospital, and the number of consultations, were examined by the Shapiro–Wilk first. If the data were normally distributed, the Student t test was used; if not, the non-parametric Mann–Whitney U test was used. p < 0.05 was considered statistically significant.
A total of 168 patients with acute psychiatric symptoms who first came to the emergency room were sorted out. Ninety-eight patients were correctly triaged and diagnosed. However, after the initial triage, 70 patients had to be retransferred because of an incorrect diagnosis. Among them, 32 patients were transferred from the department of neurology to the department of psychiatry. The most commonly misdiagnosed disease was schizophrenia (17/32, 53.1%). Similarly, 38 patients were transferred from the department of psychiatry to the department of neurology. The most misdiagnosed diseases were anti–N-methyl-D-aspartate receptor (NMDAR) encephalitis (12/38, 31.6%) and viral encephalitis (12/38, 31.6%). Figure 1 shows the proportion of each disease.
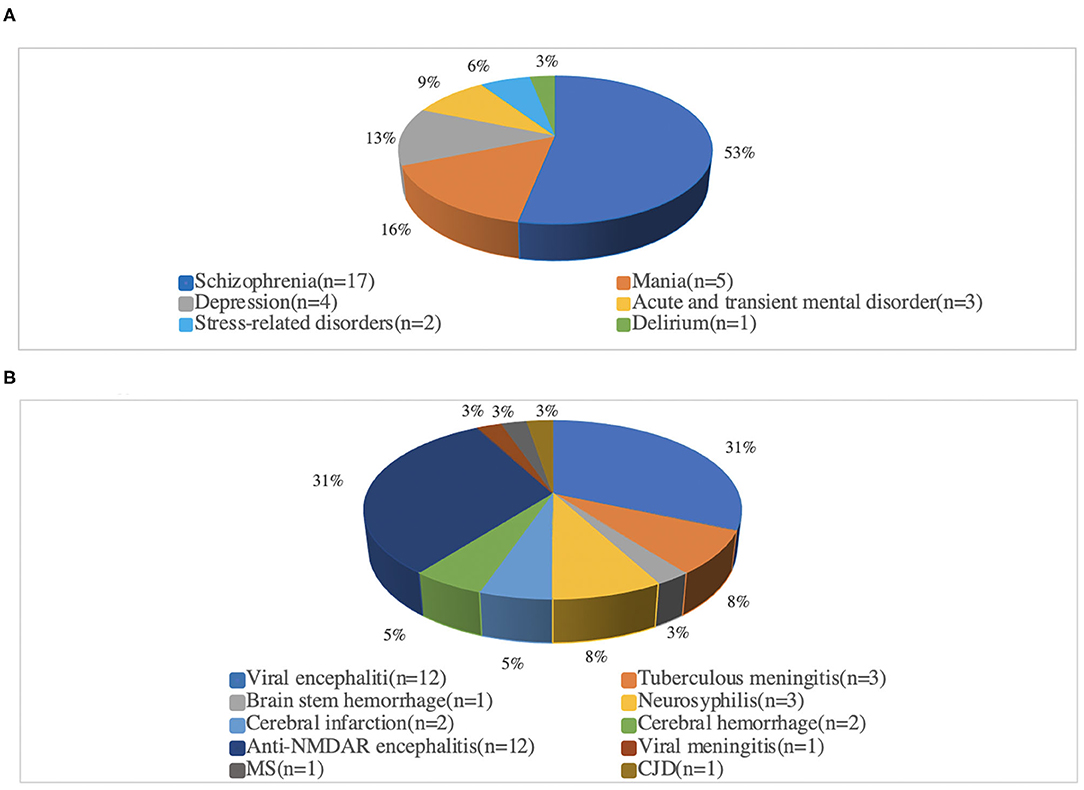
Figure 1. Proportionof each disease after re-diagnosis. (A) Admitted to the Department of Neurology, and finally diagnosed with psychiatric related disease. (B) Admitted to the Department of psychiatric, and finally diagnosed as neurology related disease. Anti-NMDAR encephalitis, Anti-N-methyl-D-aspartate receptor encephalitis; MS, Multiple sclerosis; CJD, Creutzfeldt-Jakob disease.
Thirty-seven (52.9%) of the 70 patients were female. The mean age was 34 ± 16.2 years with a range from 12 to 67 years. The clinical characteristics of 70 patients are shown in Table 1. In general, there was no difference in age and gender between the two groups. The somatic symptoms were more commonly seen in neurological diseases (P < 0.05). Compared with psychiatric diseases, the duration of neurological diseases and the number of consultations before admission were longer and more frequent (P < 0.05). Interestingly, patients with psychiatric disorders had more fever and positive meningeal irritations (P < 0.05). In addition, predisposing factors (such as psychological stress, flu history), family history of mental illness, history of physical illness and mental illness, and even Babinski sign were of no significance in distinguishing the diseases (P > 0.05).
The patients initially admitted to the department of neurology or psychiatry had significant statistical differences in the following aspects (P < 0.05) (Table 2): (1) blood tests: percentage of neutrophils, and procalcitonin; (2) cerebrospinal fluid examinations: cell count, protein level, virus antibodies, and autoimmune encephalitis–related antibodies; (3) EEG; (4) head MRI.
Overall, the most common neuropsychiatric symptoms among the 70 patients included abnormal behavior (85.7%), delusions (58.6%), hallucinations (52.8%), sleep disturbances (45.7%), and agitation/aggression (44.3%). Specifically, abnormal behavior (97.4%), sleep disturbance (68.4%), delusions (68.4%), hallucinations (60.5%), appetite change (50.0%), and agitation/aggression (42.1%) were most frequently in patients with neurological diseases, whereas for the patients with psychiatric disorders, abnormal behavior (71.9%), irritability (46.9%), delusions (46.8%), agitation/aggression (46.8%), and hallucinations (43.7%) were the most common. There were statistical differences between the two groups, in irritability, abnormal behavior, changes in appetite, and sleep disturbances (P < 0.05) (Table 3).
As schizophrenia and anti-NMDAR encephalitis were the most common diseases in the two groups, their clinical features were compared. It was found that the clinical manifestations assessed by Neuropsychiatric Inventory (NPI), laboratory test, and imaging results (Table 4) had statistically significant differences (P < 0.05). These differences mainly refer to the number of consultations, history of previous physical diseases, abnormal behavior, sleep disturbances, Babinski sign, cerebrospinal fluid virus antibody, autoimmune encephalitis–related antibody, EEG, and head MRI.
The most prominent feature of our study was that we were the first to cross-analyze the clinical characteristics of inpatients from the department of neurology or psychiatry with acute psychiatric symptoms. These patients were first triaged by the emergency nurse and initially misdiagnosed by psychiatrists or neurologists. They had a transfer after rediagnosis. We hope to identify the characteristics of patients with acute psychiatric symptoms in order to achieve early and correct triage in the emergency room.
Our study found that patients diagnosed with neurological diseases are more likely to have somatic symptoms such as dizziness and headaches. On the one hand, this may be caused by the central nervous system disease itself, such as intracranial hypertension, brain stem disease, and prefrontal and temporal Lobe injuries. On the other hand, neurological diseases are often accompanied by somatic symptoms. Research involving 300 patients showed that headaches accounted for the largest proportion of outpatient neurology visits. One hundred forty of them met the diagnostic criteria for mood disorders (Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition). Further, the somatic symptoms of patients with mood disorders are more serious than those of patients without mood disorders, which may also be the cause of misdiagnosis (12).
It is worth mentioning that previous studies have suggested abnormal vital signs (e.g., fever) and focal neurological signs (i.e., meningeal irritation and Babinski sign) as red flags of organic diseases (6–8). However, our study found this was not always the case, in the setting of the emergency room. Fever and meningeal irritation may be more indicative of psychiatric disorders, and the Babinski sign was not statistically associated. In our study, 13 patients (40.6%) with fever were mistakenly admitted to the department of neurology. It turned out that the fever was not associated with any neurological diseases, rather, with mental stress, concomitant flu, or infections in other parts of the body. More interestingly, 30 patients (78.9%) who were admitted to the psychiatric department by mistake had a fever within a few days of admission (P < 0.05), although their temperature was normal at the time of admission. The same situation applied to the focal nervous system signs, meningeal irritation signs, and Babinski signs. In summary, in the emergency room, all vital signs and focal neurological signs should be recorded immediately, because of the atypical early clinical manifestations. Fever does not necessarily represent the diagnosis of neurological diseases. On the contrary, the absence of fever does not mean they are psychiatric illness. Doctors must be very vigilant to screen carefully.
According to the analysis of the NPI scale, many psychiatric symptoms in these two categories of diseases were overlapping and often atypical. The literature showed that the early clinical manifestations of anti-NMDAR encephalitis and schizophrenia had lots of similarities. Approximately 95% of patients with anti-NMDAR encephalitis have psychiatric abnormal behavior in the early stage, and approximately 75% of them are first treated by a psychiatrist (13–16). Our study revealed that prominent irritability indicated psychiatric diseases (P < 0.05), whereas obvious abnormal behaviors, changes in appetite, and sleep disturbances were more suggestive of neurological diseases (P < 0.05). When separately analyzing the psychiatric symptoms of patients with anti-NMDAR encephalitis and schizophrenia, we found that 11 of the 12 patients with anti-NMDAR encephalitis (91.7%) had sleep disturbances, whereas there was only one case (5.8%) with schizophrenia (P < 0.05). Therefore, sleep disturbance may be an important early symptom of encephalitis, which can provide an important clue for correct and rapid diagnosis, especially in the setting of an emergency room. Previous studies have shown that visual hallucination is a red flag for organic diseases (3). In our study, unfortunately, hallucination had no obvious role in distinguishing these two diseases. When collecting medical history in the future, it may be helpful to further subdivide hallucinations into visual, auditory, and olfactory hallucinations.
After admission, the lumbar puncture, MRI of the head, and EEG will be performed for further diagnosis. If the early clinical symptoms are atypical, or some patients have severe agitation/aggressive behaviors, those examinations usually cannot be completed. However, the abnormality of these examinations is of great significance for the diagnosis of neurological and psychiatric diseases, for example, anti-NMDAR encephalitis and schizophrenia. These abnormalities include detection of cerebrospinal fluid virus antibody, autoimmune encephalitis–related antibody, lesions on head MRI, and characteristic EEG findings. Sometimes, doctors will use antipsychotics to control symptoms or perform diagnostic treatments, but studies have shown that long-term or high-dose use of antipsychotics may induce abnormal EEG and even seizures, which further interferes with the diagnosis (17–19).
There are some shortcomings in this study. (1) The sample size is relatively small. But we have screened all the inpatients with acute psychiatric symptoms from the emergency room for 7 years and cross-analyzed them. Hopefully, in future research, we will combine data from other hospitals to expand the sample size. (2) Only NPI was used to assess the psychiatric symptoms in our study. The symptoms may be better classified and refined if other positive and negative symptoms scales were added. (3) The cognitive functions were not evaluated.
Acute psychiatric symptoms in the emergency room are usually complex and diverse. Diagnosis can be very challenging. By cross-analyzing inpatient information that misdiagnosed, rediagnosed, and retransferred, clinical characteristics were identified to aid in rapid differential diagnosis promptly.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
This study was a retrospective chart review study, ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the patients was not required to participate in this study in accordance with the national legislation and the institutional requirements.
FL, JC, and JM performed material preparation, data collection and analysis. FL wrote the first draft of the manuscript. All authors contributed to the study conception and design, commented on previous versions of the manuscript, and read and approved the final manuscript.
This article was funded by National Natural Science Foundation of China (Grant No. 81371310), Science and Technology Committee of Chongqing (Grant No. cstc2018jcyjAX0130) and Chongqing Health Commission (Grant No. 2020MSXM038).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors wish to acknowledge the data collection assistance provided by Dr. Zheng Peng at the Department of Neurology, The First Affiliated Hospital of Chongqing Medical University.
NPI, Neuropsychiatric Inventory; EEG, Electroencephalography; ECG, Electrocardiogram; Anti-NMDAR encephalitis, Anti–N-methyl-D-aspartate receptor encephalitis; MS, Multiple sclerosis; CJD, Creutzfeldt-Jakob disease; PCT, Procalcitonin; WBC, White blood cell count; DP, Department of Neurology; DN, Department of Psychiatry.
1. Weiss AJ, Barrett ML, Heslin KC, Stocks C. Trends in Emergency Department Visits Involving. Mental and Substance Use Disorders, 2006–2013: Statistical Brief #216. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs Statistical Briefs. (2016). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK409512/ (accessed December, 2016).
2. Owens PL, Mutter R, Stocks C. Mental Health and Substance Abuse-Related Emergency. Department Visits among Adults, 2007: Statistical Brief #92. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. (2010). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK52659/ (accessed July, 2010).
3. McKee J, Brahm N. Medical mimics: differential diagnostic considerations for psychiatric symptoms. Ment Health Clin. (2016) 6:289–96. doi: 10.9740/mhc.2016.11.289
4. Zeller SL. Treatment of psychiatric patients in emergency settings. Prim Psychiatry. (2010) 17:35–41. Available online at: https://www.researchgate.net/publication/283157460_Treatment_of_psychiatric_patients_in_emergency_settings
5. Reynolds E. The historical evolution and future of neurology and psychiatry. J Neurol Neurosurg Psychiatry. (2015) 86:1386–8. doi: 10.1136/jnnp-2014-310113
6. Freudenreich O. Differential diagnosis of psychotic symptoms: medical mimics. Psychiatric Times. (2010) 27:56–61. Available online at: https://www.psychiatrictimes.com/view/differential-diagnosis-psychotic-symptoms-medical-mimics
7. Reeves RR, Parker JD, Loveless P, Burke RS, Hart RH. Unrecognized physical illness prompting. psychiatric admission. Ann Clin Psychiatry. (2010) 22:180–5.
8. Bishop KM, Robinson LM, VanLare S. Healthy aging for older adults withintellectual and. development disabilities. J Psychosoc Nurs Ment Health Serv. (2013) 51:15–8. doi: 10.3928/02793695-20121218-02
9. Allen MH, Fauman MA, Morin SF. Emergency psychiatric evaluation of “organic” mental disorders. New Dir Ment Health Serv. (1995) 67:45–55.
10. Otani VHO, Otani TZDS, Freirias A, Calfat ELdB, Aoki PS, Cordeiro QJ, et al. Misidentification. of mental health symptoms inpresence of organic diseases and delirium during psychiatric liaison. consulting. Int J Psychiatry Clin Pract. (2017) 21:215–20. doi: 10.1080/13651501.2017.1301483
11. Cummings J. The neuropsychiatric inventory: assessing psychopathology in dementia patients. Neurology. (1997) 48:S10–6. doi: 10.1212/WNL.48.5_Suppl_6.10S
12. Carson A, Ringbauer B, MacKenzie L, Warlow C, Sharpe M. Neurological disease, emotional disorder, and disability: they are related: a study of 300 consecutive new referrals to a neurology outpatient department. J Neurol Neurosurg Psychiatry. (2000) 68:202–6. doi: 10.1136/jnnp.68.2.202
13. Dalmau J, Tüzün E, Wu HY, Masjuan J, Rossi JE, Voloschin A, et al. Paraneoplastic Anti-NMDAR encephalitis associated with ovarian teratoma. Ann Neurol. (2007) 61:25–36. doi: 10.1002/ana.21050
14. Jorgensen A, Hansen BS, Stanislaus S, During S, Jorgensen MB, Pinborg LH, et al. Anti-NMDAR. encephalitis is an important differential diagnosis in acute psychiatric disease. Acta Psychiatr Scand. (2015) 131:69–70. doi: 10.1111/acps.12351
15. Kayser MS, Titulaer MJ, Gresa-Arribas N, Dalmau J. Frequency and characteristics of isolated psychiatric episodes in Anti-NMDAR encephalitis. JAMA Neurol. (2013) 70:133–9. doi: 10.1001/jamaneurol.2013.3216
16. Fleischhacker WW, Arango C, Arteel P, Barnes TR, Carpenter W, Duckworth K, et al. Schizophrenia–time to commit to policy change. Schizophr Bull. (2014) 40(Suppl. 3):165–94. doi: 10.1093/schbul/sbu006
17. Dalmau J, Lancaster E, Martinez-Hernandez E, Rosenfeld MR, Balice-Gordon R. Clinical experience and laboratory investigations in patients with anti-NMDAR encephalitis. Lancet Neurol. (2011) 10:63–74. doi: 10.1016/S1474-4422(10)70253-2
18. Irani SR, Bera K, Waters P, Zuliani L, Maxwell S, Zandi MS, et al. N-methyl-D-aspartate antibody encephalitis: temporal progression of clinical and paraclinical observations in a predominantly non-paraneoplastic disorder of both sexes. Brain. (2010)133:1655–67. doi: 10.1093/brain/awq113
Keywords: acute psychiatric symptoms, misidentification, differential diagnosis, clinical characteristics, emergency room
Citation: Liu F, Chen J, Du Y, Jiang W, Gong L and Mu J (2021) Misidentification of Acute Psychiatric Symptoms in the Emergency Room: Clinical Experience in China. Front. Psychiatry 11:579484. doi: 10.3389/fpsyt.2020.579484
Received: 04 August 2020; Accepted: 04 December 2020;
Published: 14 January 2021.
Edited by:
Felice Iasevoli, University of Naples Federico II, ItalyReviewed by:
Massimo Tusconi, University of Cagliari, ItalyCopyright © 2021 Liu, Chen, Du, Jiang, Gong and Mu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jun Mu, am11QGhvc3BpdGFsLmNxbXUuZWR1LmNu
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.