- Department of Operating Room, The First Affiliated Hospital of Sun Yat-sen University, Guangzhou, China
The present study aimed to evaluate the efficacy of psychological nursing of patients with stroke in China. The Embase, PubMed, Cochrane Library, CNKI, and Wanfang databases were searched from inception to February 1, 2020. Randomized controlled trials (RCTs) reporting the efficacy of psychological nursing of patients with stroke were included. Revman 5.3 and Stata 15.0 were used for data analysis. Twelve RCTs and 1,013 patients with stroke were included in this systematic review and meta-analysis. The results revealed a significant difference in the Hamilton depression score between the psychological nursing and usual care groups. The meta-analysis of three studies (n = 235) that used a depressive symptom control of ≥25% as the outcome measure showed a significant difference between the two groups. In addition, significant differences were detected in the National Institute of Health stroke scale score and activities of daily living score between the two groups. The present meta-analysis suggests that in China, compared to the usual care, psychological nursing is more effective for alleviating depressive symptoms, improving neurological rehabilitation, and recovering the ability of daily life.
Introduction
Social and psychological issues such as anxiety, depression, and cognitive impairment occur commonly after stroke in about 40% of the patients (1–3). Moreover, self-reported psychological conditions are prevalent, with ~60% of the patients with stroke feeling depressed and 67% feeling anxious (4). Psychological issues such as depression have a major impact on the quality of daily life (5) and are likely to occur over the first 26 weeks after stroke and predict poor functional outcomes at 52 weeks (6).
Nurses also face difficulty in coping with the fluctuating mood and uncooperative behavior of patients with stroke (7–9). Over half of the nurses and nearly half of the patients with stroke experience difficulties in interpersonal relationships (1). Thus, effective psychological care is necessary to improve nursing and to reduce the consumption and cost of healthcare (10).
Psychological nursing is the act of health professionals providing positive psychological interventions for patients after a medical event to help them acquire and maintain a good psychological state to ease rehabilitation and healthcare (11). Psychological nursing is of special importance for patients at high risk of illness-induced anxiety and depression (12). Psychological nursing is part of the shift of nursing toward the biological-psychological-social model (13). Psychological nursing does not only focus on the patient's illness but involves the entire nursing process (13). Its aim is to improve not only the patient's body comfort but also its psychological state, which is an important component of quality of life. Psychological nursing also affects the cognition of the patients through the behaviors and attitudes of the medical staff, improving their quality of life (14). It has been reported that psychological nursing can reduce perceived pain, anxiety, and depression in 82% of patients with advanced gastric cancer (15). The main difference between psychological interventions, such as cognitive-behavioral therapy and psychological nursing, is that cognitive-behavioral therapy is a definite treatment in time that requires a psychiatrist or psychologist while psychological nursing is an ongoing process (24 h/day, for the entire patient's hospitalization) that requires the active and continuous participation of all the nursing staff (11, 12). For now, psychological nursing is still in its infancy all over the world. Besides cultural and healthcare administrative differences among countries, the optimal psychological nursing interventions are still being pursued.
Presently, psychological nursing of patients with stroke is gaining increasing attention in China. Some studies compared psychological nursing to the usual care for patients with stroke (16–27), albeit the results were conflicting and no comprehensive analysis of these data are yet available. Therefore, systematic review and meta-analysis are essential to evaluate the efficacy of psychological nursing of patients with stroke in China.
Methods
Search Strategy
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) criteria (28). The Embase, PubMed, Cochrane Library, CNKI, and Wanfang databases were searched using the key words [“Psychological nursing” OR “Psychological care”] AND “Stroke” AND [“China” OR “Chinese”]. The databases were searched from their inception to February 1, 2020. We also screened the bibliographies of the retrieved studies and recent review articles to identify additional eligible trials. No language restrictions were applied.
Inclusion and Exclusion Criteria
The following selection criteria were applied according to the PICOS principles. Participants (P): patients with stroke in China; Intervention (I): psychological nursing; Comparison (C): usual care; Outcomes (O): efficacy, which was evaluated using the Hamilton depression (HAMD) score, the National Institute of Health stroke scale (NINSS) score, and activities of daily living (ADL) score; Study design (S): random controlled trials (RCTs). Studies were excluded if they were published as reviews, editorials, letters, case reports, cell and animal studies, or expert opinions. Bingye Liao and Minni Liang independently and systematically screened the literature by titles and abstracts, and then read the full texts to determine the eligibility of the articles. If more than one article was from the same dataset, only the one with the largest sample size was included. Any disagreement in the literature search was resolved by the third author (Yuejiao Su).
Data Extraction and Quality Assessment
All data from the selected studies were extracted independently by two reviewers (Qiuyi Ouyang and Xiaojun Chen), and any disagreement was resolved by the third reviewer (Hongqin Song). The extracted data, including the study year, number of samples, male, mean age (years) of the participants, and follow-up duration were summarized into simple standard forms. Each study was independently screened by two reviewers. The risk of bias assessment was evaluated according to the Cochrane Handbook for Systematic Reviews (29), which includes selective outcome, allocation concealment, blinding, incomplete outcome data, random generation, and other biases. Also, the quality of the included studies was assessed.
Data Synthesis and Statistical Analysis
The continuous variable data were expressed as mean differences (MD) with 95% confidence intervals (CI). Odds ratio (ORs) and the 95% CI were calculated to combine the categorical variable data. Next, the missing standard deviations (SD) such as P-values or 95% CI were estimated if needed (29, 30). Among the combined study results, Cochran's Q test and the degree of inconsistency (I2) were used to assess heterogeneity (29). A fixed-effects model was used if I2 was <50%. Otherwise, the data were pooled using the random-effects method. All statistical analyses were performed in an intent-to-treat principle and using the RevMan 5.3 and Stata® Statistical Software Package, version 15.0 (StataCorp LP, College Station, TX, USA). The publication bias was estimated using the Egger's test. P < 0.05 indicated statistical significance.
Results
Search Results
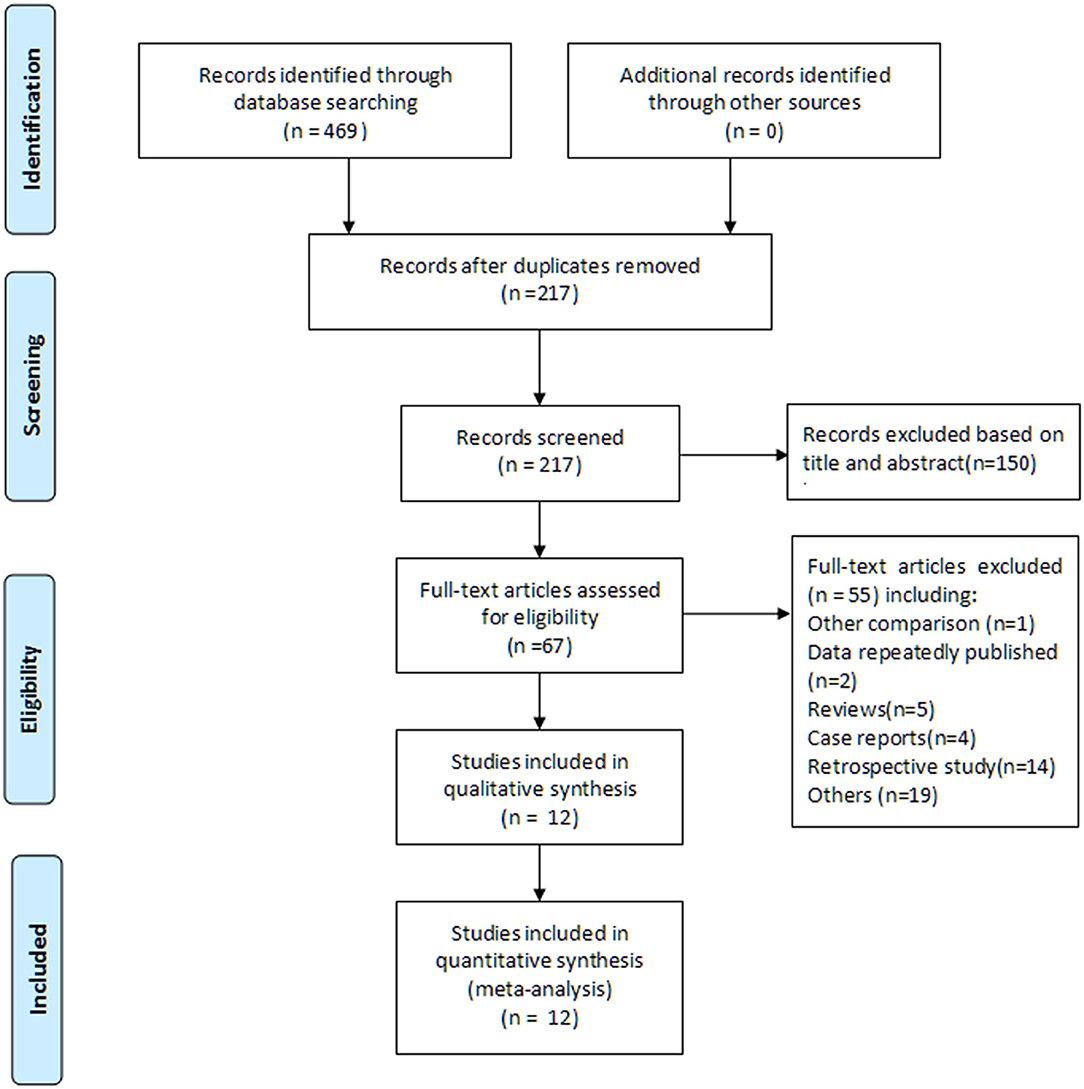
A total of 469 articles were screened after a combined search of Embase, PubMed, Cochrane Library, CNKI, and Wanfang for articles published until February 1, 2020. Subsequently, 217 potential articles were selected after removing the duplicates. Of these, 150 articles were excluded based on title and abstract review, and the full-text of the remaining 67 articles was reviewed. An additional 55 articles were excluded according to the inclusion and exclusion criteria. Finally, 12 studies (1,013 patients; psychological nursing group: 509 patients; usual care group: 504 patients), published from 2004 to 2019, were included in this meta-analysis (16–27). The study selection process is illustrated in Figure 1.
Characteristics of the Studies
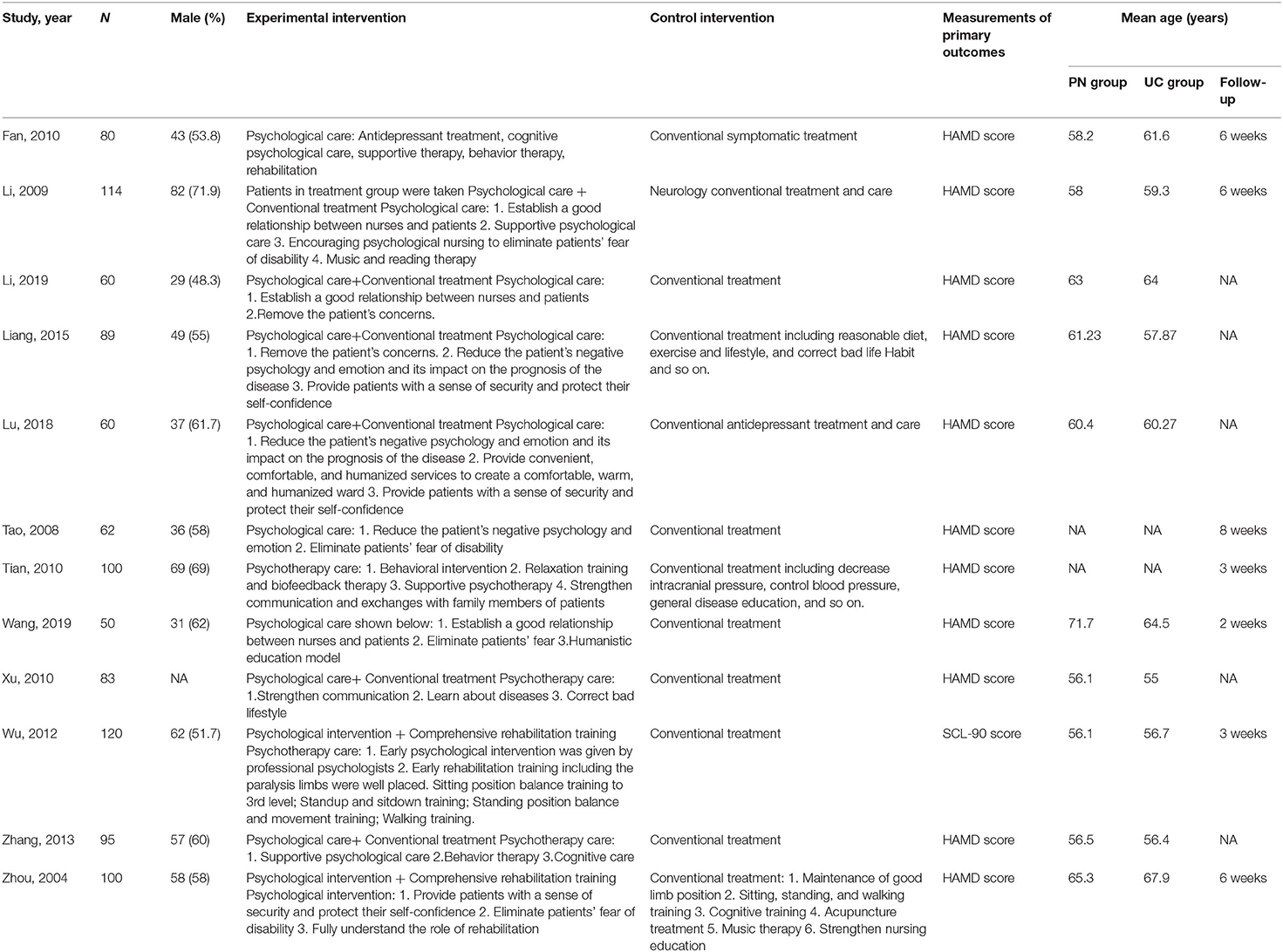
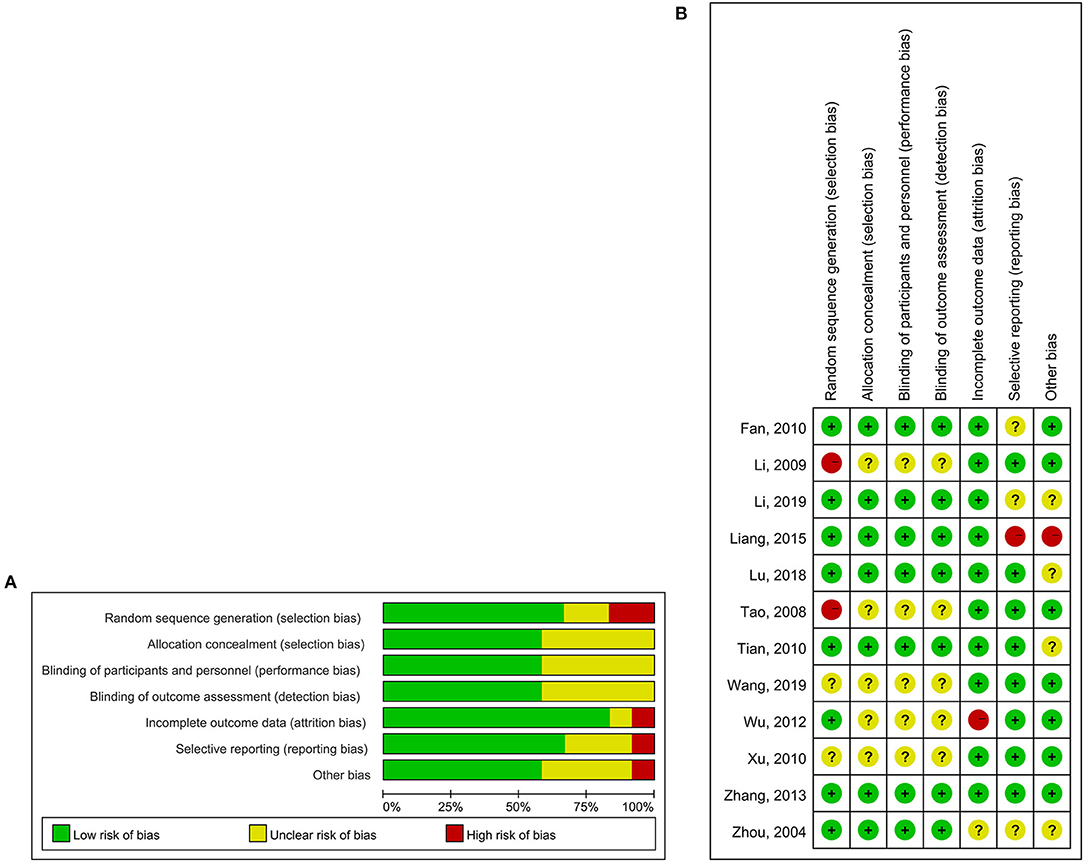
The sample size of the included studies was 50–114 cases, and the duration of follow-up was 2–8 weeks. The baseline characteristics of the 12 studies are summarized in Table 1. Three studies used an adequate method of random sequence generation by randomized code table (17, 19, 26). The quality of the included studies is summarized in Figures 2A,B.
Psychological Nursing of Patients With Stroke
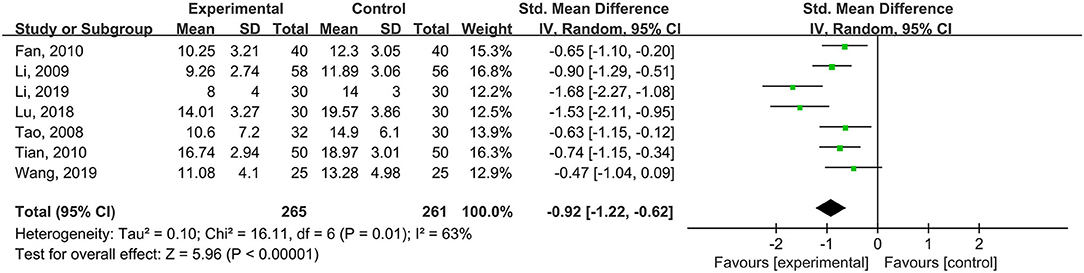
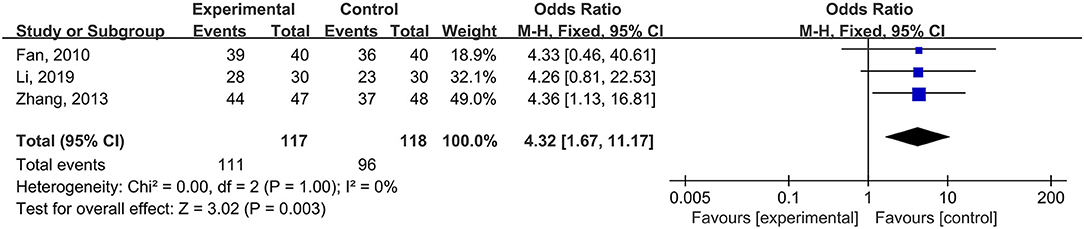
Seven studies (n = 526 patients) used the total HAMD scale as the outcome measurement, and the results of the meta-analysis showed a significant difference in the HAMD score between the psychological nursing and the usual care groups (standardized mean difference (SMD) = −0.92, 95% CI: −1.22 to −0.62, I2 = 63%, Pheterogeneity = 0.01) (Figure 3). Meta-regression analyses revealed that the publication year (P = 0.642), sample size (P = 0.633), and mean age (P = 0.175) of the intervention group did not have moderating effects. The meta-analysis of three studies (n = 235) that used a depressive symptom control of ≥25% as the outcome revealed a significant difference between the two groups (OR = 4.32, 95% CI: 1.67–11.17, I2 = 0%, Pheterogeneity > 0.999) (Figure 4).
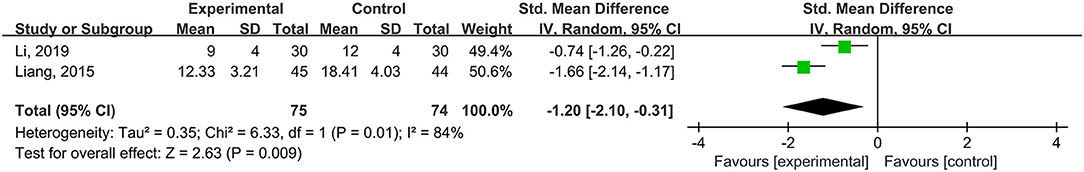
Efficacy for Improving Neurological Rehabilitation by the NIHSS Scale
Two studies (n = 149 patients) used the NIHSS scale as the outcome. The results of the meta-analysis showed a significant difference in the NIHSS score between the psychological nursing and the usual care groups (SMD = −1.20, 95% CI: −2.10 to −0.31, I2 = 84%, Pheterogeneity = 0.01) (Figure 5). The meta-regression analyses revealed that the publication year (P = 0.46), sample size (P = 0.24), and mean age of the intervention group (P = 0.68) did not have moderating effects on the efficacy for improving neurological rehabilitation by the NIHSS scale.
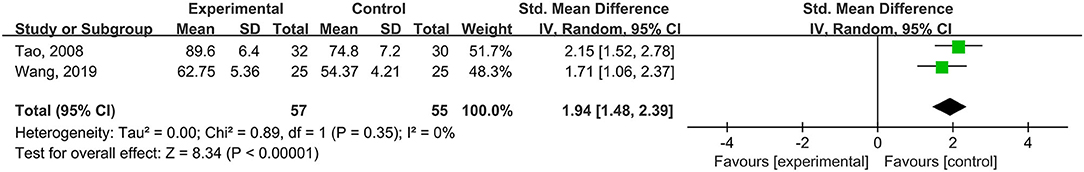
Efficacy for Recovering ADL
Two studies (n = 817 patients) used the ADL scale as the outcome. The meta-analysis showed a significant difference in the ADL score between the psychological nursing and the usual care groups (SMD = 1.94, 95% CI (1.48–2.39), I2 = 0%, Pheterogeneity = 0.35) (Figure 6).
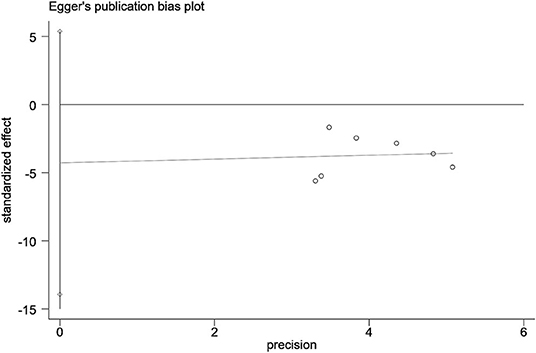
Publication Bias
Funnel plots and Egger's test did not show any publication bias across studies with respect to data on alleviating depressive symptoms, as assessed by the HAMD scale (t = −1.14, 95% CI: −13.9 to 5.36, P = 0.305) (Figure 7).
Discussion
This systematic review and meta-analysis identified 12 studies investigating the psychological nursing of patients with stroke in China. The analysis found that compared to the usual care, psychological nursing is more effective for alleviating depressive symptoms, improving neurological rehabilitation, and recovering the ADL.
In the present meta-analysis, the HAMD, NIHSS, and ADL scores favored the psychological nursing group as compared to the usual care group. Nevertheless, all three scores examine different aspects. HAMD is a well-known and widely used questionnaire for depression and recovery (31). It examines mood, guilt, suicide ideation, insomnia, agitation or retardation, anxiety, weight loss, and somatic symptoms. NIHSS is a tool that allows the objective quantification of the impairments caused by stroke; also, it is applied to determine the severity of a stroke and examine recovery (32). ADL is used to determine the extent to which a patient is able to care for him/herself and determine the extent of the disabilities after stroke (33). Despite that these scales do not measure the same outcomes, all three are inter-related in patients with stroke (34–36). Patients with more severe stroke are more likely to have impairments in daily life activities and to have depression, patients with higher impairments are more likely to be depressed and present a lower score of NIHSS, and depressed patients putatively score low in the NIHSS and have low willingness to perform daily activities.
Several recent RCTs assessed the effects of psychological nursing of patients with stroke in China. These trials assessed the effects of psychological nursing on depressive symptoms, neurological rehabilitation, and the ADL. Li et al. (19) concluded that the HAMD and NIHSS scores of the psychological nursing group were significantly lower than those of the usual care group, and the total effective rate of the nursing intervention was 93% (28/30), which was significantly higher than the 77% (23/30) of the usual care group. Tian et al. (22) demonstrated that the HAMA and HAMD scores in the psychological nursing group were significantly lower than those in the usual care group after 3 weeks of intervention. Wu et al. (25) showed that psychological nursing significantly improved the mental health, limb movement function, stress ability, and the activity of daily living in patients with acute stroke. In the current meta-analysis, we observed a significant difference in the HAMD score, NIHSS score, and ADL scale between the psychological nursing and the usual care groups. The results demonstrated that psychological nursing is more effective than the usual care for alleviating depressive symptoms, improving neurological rehabilitation, and recovering ADL.
Those effects of psychological nursing on scales of anxiety, depression, and stroke-related impairments are consistent with the core aim of psychological nursing, i.e., improving the quality of life of the patients by decreasing anxiety and depression through a continuous and ongoing psychological care process, which is opposite to classical psychological interventions such as cognitive-behavioral therapy, which requires the participation of the patients and specialized healthcare professionals (11, 12). Decreased anxiety and depression are conducive to improved quality of life, which in turn is conducive to better functional outcomes and decreased health-related anxiety (34–36). Psychological nursing involves all the minute details in the nurse-patient relationship and that are related to the biological-psychological-social model paradigm of modern nursing care (13).
Nevertheless, the current study has some limitations. First, because of the differences between the healthcare systems in China and Western countries, a decision was made to include studies conducted only in China. Although this limits the generalizability, it improves the applicability of the results nationwide. Second, although all included studies were RCTs, the main limitation was the significant risk of reporting bias and selection, as well as the risk of bias evaluation. Third, the gray literature was not included. Fourth, the efficacy in long-term follow-up lacked evidence. Fifth, the majority of the included studies were from a single site using a small sample size, and hence, larger sample size and multicenter studies should be conducted. Finally, high heterogeneity was detected across some outcomes. This could be attributed to the articles with meta-analysis that investigated psychological nursing after stroke; however, the exact content of this psychological nursing varied across centers.
In conclusion, this systematic review and meta-analysis demonstrated that psychological nursing might be more effective for alleviating depressive symptoms, improving neurological rehabilitation, and recovering the ADL than the usual care group in China. Thus, well-designed and larger studies are essential to characterize the efficacy of psychological nursing for patients with stroke. Nevertheless, the present meta-analysis suggested that psychological nursing improves the psychological outcomes of patients after stroke and that such programs should be implemented in centers caring for patients with stroke. This should be conducive to reduce the burden on the healthcare system.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Materials, further inquiries can be directed to the corresponding authors.
Author Contributions
BL and ML conceived and supervised the study. QO and XC analyzed the data. BL, ML, and HS wrote the manuscript. YS and QO made manuscript revisions. All authors reviewed the results and approved the final version of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2020.569426/full#supplementary-material
References
1. The Stroke Association. Feeling Overwhelmed: The Emotional Impact of Stroke. London: The Stroke Association (2013).
2. Murray J, Young J, Forster A, Ashworth R. Developing a primary care-based stroke model: the prevalence of longer-term problems experienced by patients and carers. Br J Gen Pract. (2003) 53:803–7.
3. McKevitt C. The Stroke Association UK Stroke Survivor Needs Survey. London: The Stroke Association (2010).
4. Murray J, Ashworth R, Forster A, Young J. Developing a primary care-based stroke service: a review of the qualitative literature. Br J Gen Pract. (2003) 53:137–42.
5. Lincoln C, Kneebone I, MacNiven J, Morris R. The Psychological Management of Stroke. Chichester: Wiley International (2012). doi: 10.1002/9781119961307
6. West R, Hill K, Hewison J, Knapp P, House A. Psychological disorders after stroke are an important influence on functional outcomes: a prospective cohort study. Stroke. (2010) 41:1723–7. doi: 10.1161/STROKEAHA.110.583351
7. Low JT, Payne S, Roderick P. The impact of stroke on informal carers: a literature review. Soc Sci Med. (1999) 49:711–25. doi: 10.1016/S0277-9536(99)00194-X
8. Simon C, Kumar S. Stroke patients' carers' views of formal community support. Br J Community Nurs. (2002) 7:158–63. doi: 10.12968/bjcn.2002.7.3.10216
9. Mackenzie A, Perry L, Lockhart E, Cottee M, Cloud G, Mann H. Family carers of stroke survivors: needs, knowledge, satisfaction and competence in caring. Disabil Rehabil. (2007) 29:111–21. doi: 10.1080/09638280600731599
10. Gilham S, Carpenter M, Leathley M. Psychological Care After Stroke: Economic Modelling of a Clinical Psychology Led Team Approach. Leicester: NHS Improvement (2012).
12. Peyrovi H, Raiesdana N, Mehrdad N. Living with a heart transplant: a phenomenological study. Prog Transplant. (2014) 24:234–41. doi: 10.7182/pit2014966
13. Han SF, Zhu RF, Zhao J. A study of clinical psychological nursing research hotspots in China and variation trends based on word frequency analysis and visualization analysis. Chin Nursing Res. (2017) 4:186–91. doi: 10.1016/j.cnre.2017.06.005
14. Liu XY, Zhao X, Gan CB, Shao LL, Wang X. Effect of psychological nursing based on relaxation training for the psychological state in patients with impacted third molar removal surgery. Zhonghua Kou Qiang Yi Xue Za Zhi. (2018) 53:324–7. doi: 10.3760/cma.j.issn.1002-0098.2018.05.007
15. Liu Q, Zhao R, Wu Q, Zhuang GH. Meta-analysis on influence of psychological nursing on quality of life of AIDS patients. Zhonghua Liu Xing Bing Xue Za Zhi. (2017) 38:972–6. doi: 10.3760/cma.j.issn.0254-6450.2017.07.025
16. Liang S, Wu Z. Effect of psychological nursing intervention on mental health and quality of life for stroke patients with depression and anxiety. Chin J Nod Nurs. (2015) 16:1912–4. Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CJFD&dbname=CJFDZHYX&filename=HLJH201516019&uid=WEEvREcwSlJHSldSdmVqeVpQWEhjK1FkWlowOExsMjZ5amd5ZnhRdVJwYz0=$9A4hF_YAuvQ5obgVAqNKPCYcEjKensW4ggI8Fm4gTkoUKaID8j8gFw!!&v=MTA5NjNVUjdxZVp1UnRGeXptVjdyS0xTSEJackc0SDlUTnFZOUViWVI4ZVgxTHV4WVM3RGgxVDNxVHJXTTFGckM=
17. Yanfang L, Yang W. Effect of early psychological nursing intervention on neuropsychological improvement of patients with poststroke depression. Shanxi Med J. (2019) 48:2101–3. Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CJFQ&dbname=CJFDLAST2019&filename=SXYY201917005&uid=WEEvREcwSlJHSldSdmVqeVpQWEhjK1FkWlowOExsMjZ5amd5ZnhRdVJwYz0=$9A4hF_YAuvQ5obgVAqNKPCYcEjKensW4ggI8Fm4gTkoUKaID8j8gFw!!&v=MTExMTQ5RllZUjhlWDFMdXhZUzdEaDFUM3FUcldNMUZyQ1VSN3FlWnVSdEZ5em5VcjdMTmpYU2Q3RzRIOWpOcUk=
18. Fan J, He H. Effect of psychological nursing on rehabilitation of patients with post-stroke depression. J Clin Exp Med. (2010) 1335–8. Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CJFD&dbname=CJFDZHYX&filename=GWHL201009021&uid=WEEvREcwSlJHSldSdmVqeVpQWEhjK1FkWlowOExsMjZ5amd5ZnhRdVJwYz0=$9A4hF_YAuvQ5obgVAqNKPCYcEjKensW4ggI8Fm4gTkoUKaID8j8gFw!!&v=MDcxNDNEWXJHNEg5SE1wbzlIWllSOGVYMUx1eFlTN0RoMVQzcVRyV00xRnJDVVI3cWVadVJ0Rnl6blVMek5JanI=
19. Li X, Lai Z. Psychological care of patients with post-stroke depression. J Clin Exp Med. (2009) 8:4–5. Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CJFQ&dbname=CJFD2009&filename=SYLC200906003&uid=WEEvREcwSlJHSldSdmVqeVpQWEhjK1FkWlowOExsMjZ5amd5ZnhRdVJwYz0=$9A4hF_YAuvQ5obgVAqNKPCYcEjKensW4ggI8Fm4gTkoUKaID8j8gFw!!&v=MTQ2NTZaNFI4ZVgxTHV4WVM3RGgxVDNxVHJXTTFGckNVUjdxZVp1UnRGeXpuVkx2UE5qVEhiYkc0SHRqTXFZOUY=
20. Lu X, Li M, Zhao Y. Clinical observation on the application of psychological intervention and humanistic care nursing in patients with post-stroke depression. J Qiqihar Univ Med. (2018) 39:2066–7. Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CJFQ&dbname=CJFDLAST2019&filename=QQHB201817036&uid=WEEvREcwSlJHSldSdmVqeVpQWEhjK1FkWlowOExsMjZ5amd5ZnhRdVJwYz0=$9A4hF_YAuvQ5obgVAqNKPCYcEjKensW4ggI8Fm4gTkoUKaID8j8gFw!!&v=MjE4MDFYMUx1eNEg5bk5xSTlHWW9SOGU=
21. Tao M, Yang X. Effect of psychological nursing on depressive symptoms and functional recovery of patients with stroke depression. Chin J Pract Nerv Dis. (2008) 11:154. Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CJFQ&dbname=CJFD2008&filename=HNSJ200808119&uid=WEEvREcwSlJHSldSdmVqeVpQWEhjK1FkWlowOExsMjZ5amd5ZnhRdVJwYz0=$9A4hF_YAuvQ5obgVAqNKPCYcEjKensW4ggI8Fm4gTkoUKaID8j8gFw!!&v=MTM5NjZxZVp1UnRGeXpuVzc3QkxTUFlaTEc0SHRuTXA0NUViWVI4ZVgxTHV4WVM3RGgxVDNxVHJXTTFGckNVUjc=
22. Tian Y, Ren A. Observation on the effect of psychological care on the patients anxiety and depression disorders after stroke. J Qilu Nurs. (2010) 16:6–7. Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CJFQ&dbname=CJFD2010&filename=QLHL201016003&uid=WEEvREcwSlJHSldSdmVqeVpQWEhjK1FkWlowOExsMjZ5amd5ZnhRdVJwYz0=$9A4hF_YAuvQ5obgVAqNKPCYcEjKensW4ggI8Fm4gTkoUKaID8j8gFw!!&v=MjgwMDFyQ1VSN3FlWnVSdEZ5emdVcnJPTkNIRFlyRzRIOUhOcVk5Rlo0UjhlWDFMdXhZUzdEaDFUM3FUcldNMUY=
23. Wang Z, Cai X, Xin H. Effect of psychological counseling nursing on training mentality and quality of life of patients with post-stroke depression. Mod Diagn Treat. (2019) 30:2528–30. Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CJFQ&dbname=CJFDLAST2019&filename=XDZD201914086&uid=WEEvREcwSlJHSldSdmVqeVpQWEhjK1FkWlowOExsMjZ5amd5ZnhRdVJwYz0=$9A4hF_YAuvQ5obgVAqNKPCYcEjKensW4ggI8Fm4gTkoUKaID8j8gFw!!&v=MDQ2MzJxNDlOWW9SOGVYMUx1eFlTN0RoMVQzcVRyV00xRnJDVVI3cWVadVJ0Rnl6Z1U3dklQU25SYXJHNEg5ak4=
24. Xu H, Cao N, Xu D. Effect of cognitive behavioral psychological nursing on rehabilitation of post-stroke depression. Chin J Pract Nerv Dis. (2010) 13:13–4. Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CJFQ&dbname=CJFD2010&filename=HNSJ201020008&uid=WEEvREcwSlJHSldSdmVqeVpQWEhjK1FkWlowOExsMjZ5amd5ZnhRdVJwYz0=$9A4hF_YAuvQ5obgVAqNKPCYcEjKensW4ggI8Fm4gTkoUKaID8j8gFw!!&v=MTE1NjRSN3FlWnVSdEZ5emdVYi9QTFNQWVpMRzRIOUhPcjQ5RmJJUjhlWDFMdXhZUzdEaDFUM3FUcldNMUZyQ1U=
25. Wu DY, Guo M, Gao YS, Kang YH, Guo JC, Jiang XL, et al. Clinical effects of comprehensive therapy of early psychological intervention and rehabilitation training on neurological rehabilitation of patients with acute stroke. Asian Pac J Trop Med. (2012) 5:914–6. doi: 10.1016/S1995-7645(12)60171-0
26. Zhou CX, Su XL, Yang XZ, Xiao XC. Effect of psychological nursing on the rehabilitation of post-stroke depression. Chin J Clin Rehab. (2004) 8:3008–9. Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CJFQ&dbname=CJFD2004&filename=XDKF200416004&uid=WEEvREcwSlJHSldSdmVqeVpQWEhjK1FkWlowOExsMjZ5amd5ZnhRdVJwYz0=$9A4hF_YAuvQ5obgVAqNKPCYcEjKensW4ggI8Fm4gTkoUKaID8j8gFw!!&v=MjMzMDNMdXhZUzdEaDFUM3FUcldNMUZyQ1VSN3FlWnVSdEZ5emdWcnpBUFNuQWFMRzRIdFhOcVk5RllJUjhlWDE=
27. Zhang Q. Effect of psychological nursing on neurological impairment and depression degree in patients with post-stroke depression. Chin J Pract Nerv Dis. (2013) 16:83–4. Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CJFQ&dbname=CJFD2013&filename=HNSJ201310052&uid=WEEvREcwSlJHSldSdmVqeVpQWEhjK1FkWlowOExsMjZ5amd5ZnhRdVJwYz0=$9A4hF_YAuvQ5obgVAqNKPCYcEjKensW4ggI8Fm4gTkoUKaID8j8gFw!!&v=MDM4MDR1eFlTN0RoMVQzcVRyV00xRnJDVVI3cWVadVJ0Rnl6Z1ZML1BMU1BZWkxHNEg5TE5yNDlBWm9SOGVYMUw=
28. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
29. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
30. Higgins JG. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. London: The Cochrane Collaboration (2011).
31. Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. (1960) 23:56–62. doi: 10.1136/jnnp.23.1.56
33. Edemekong PF, Bomgaars DL, Sukumaran S, Levy SB. Activities of Daily Living (ADLs). Treasure Island, FL: StatPearls (2020).
34. Hiraga A, Yamaoka T, Sakai Y, Osakabe Y, Suzuki A, Hirose N. Relationship between outcome in acute stroke patients and multiple stroke related scores obtained after onset of stroke. J Phys Ther Sci. (2018) 30:1310–4. doi: 10.1589/jpts.30.1310
35. Delavaran H, Aked J, Sjunnesson H, Lindvall O, Norrving B, Kokaia Z, et al. Spontaneous recovery of upper extremity motor impairment after ischemic stroke: implications for stem cell-based therapeutic approaches. Transl Stroke Res. (2017) 8:351–61. doi: 10.1007/s12975-017-0523-9
Keywords: psychological nursing, usual care, stroke, depressive symptoms, meta-analysis
Citation: Liao B, Liang M, Ouyang Q, Song H, Chen X and Su Y (2020) Psychological Nursing of Patients With Stroke in China: A Systematic Review and Meta-Analysis. Front. Psychiatry 11:569426. doi: 10.3389/fpsyt.2020.569426
Received: 04 June 2020; Accepted: 04 November 2020;
Published: 11 December 2020.
Edited by:
Preethi Premkumar, London South Bank University, United KingdomReviewed by:
Zhen Yuan, University of Macau, ChinaReiji Yoshimura, University of Occupational and Environmental Health Japan, Japan
Copyright © 2020 Liao, Liang, Ouyang, Song, Chen and Su. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuejiao Su, c3V5dWVqaWFvMDJAMTYzLmNvbQ==; Xiaojun Chen, Y2hlbnhqODhAbWFpbC5zeXN1LmVkdS5jbg==
†These authors have contributed equally to this work
 Bingye Liao†
Bingye Liao† Yuejiao Su
Yuejiao Su