- 1Section of Psychiatry, Department of Neuroscience, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health, University of Genoa, Genoa, Italy
- 2IRCCS Ospedale Policlinico San Martino, Genoa, Italy
- 3Department of Psychiatry and Psychotherapy, St. Rokus Clinical Center, Semmelweis University, Budapest, Hungary
- 4MTA-SE Neuropsychopharmacology Research Group, Hungarian Academy of Sciences and Semmelweis University, Budapest, Hungary
- 5NAP-2-SE New Antidepressant Target Research Group, Hungarian Brain Research Programme, Semmelweis University, Budapest, Hungary
- 6Department of Psychiatry and Addiction Medicine, AP-HP, Hopital Bichat-Claude Bernard, Paris, France
- 7NeuroDiderot, Inserm, Paris University, Paris, France
- 8Department of Neurosciences, Suicide Prevention Center, Sant’Andrea Hospital, University of Rome, Rome, Italy
Background: Stressful life events (SLE) may influence the illness course and outcome. This study aimed to characterize socio-demographic and clinical features of euthymic major depressive disorder (MDD) outpatients with SLE compared with those without.
Methods: The present sample included 628 (mean age=55.1 ± 16.1) currently euthymic MDD outpatients of whom 250 (39.8%) reported SLE and 378 (60.2%) did not.
Results: After univariate analyses, outpatients with SLE were most frequently widowed and lived predominantly with friends/others. Moreover, relative to outpatients without SLE, those with SLE were more likely to have a family history of suicidal behavior, manifested melancholic features, report a higher Coping Orientation to the Problems Experienced (COPE) positive reinterpretation/growth and less likely to have a comorbid panic disorder, residual interepisodic symptoms, use previous psychiatric medications, and currently use of antidepressants. Having a family history of suicide (OR=9.697; p=≤.05), history of psychotropic medications use (OR=2.888; p=≤.05), and reduced use of antidepressants (OR=.321; p=.001) were significantly associated with SLE after regression analyses. Mediation analyses showed that the association between current use of antidepressants and SLE was mediated by previous psychiatric medications.
Conclusion: Having a family history of suicide, history of psychotropic medications use, and reduced use of antidepressants is linked to a specific “at risk” profile characterized by the enhanced vulnerability to experience SLE.
Background
Stressful life events (SLE) may be defined as: “environmental events or chronic conditions that objectively threaten the physical and/or psychological health or well-being of individuals of a particular age in a particular society” (1). Life events may be described as social and environmental occurrences leading to psychophysiological modification in the general population during the time course (2). Life events are considered positive or negative according to the individual’s subjective experience. Negative life events, which may have a prominent role in the development and clinical course of psychiatric disorders may be identified in various social/environmental contexts (2) and may be commonly defined as: 1) maltreatment and violence; 2) loss events; 3) intrafamilial problems; 4) school and interpersonal problems (3, 4). These type of life events are usually associated with undesirable affective experiences exerting deleterious effects on the individual mental health and social/environmental adaption (4). Generally, SLE such as perceived loss, humiliation, entrapment, and perceived danger seem to provide interesting information about the course and outcome of psychiatric conditions (5). Notably, certain types of SLE such as involuntary occupation loss and marital separation may enhance suicide risk (6, 7), and influence the time to remission of major depressive disorder (MDD) (8) as well as substance use (9).
Based on stress vulnerability models, having experienced SLE is generally linked to poor mental health (10) with the development of major psychiatric conditions generally associated with the exposure to SLE (11). Having experienced more proximal life personal and situational factors may also enhance suicide risk (12) with the cumulative effect of multiple life events playing a more relevant effect than that of specific single life events (13).
While depression has a moderate heritability, environmental events account for approximately 60% of the variation in depression (14) on a general population level depending on the severity of the illness, with 80% of depressive episodes preceded by a major stress exposure (15) and etiologically relevant distal and proximal stressors occurring quite frequently, about at least once every 3–4 years.
SLE are able to strongly predict both the onset (16) and recurrence (17) of depressive episodes, including suicidal behavior. Evidence also suggested that negative life adversities are important risk factors particularly for depressed subjects with a negative cognitive style (18). This hypothesis postulated that exposure to SLE may determine sensitization or kindling and may enhance the individual vulnerability to manifest depressive episodes, although the patient is not directly experiencing a relevant psychosocial stressor. Socio-demographic and clinical variables such as gender potentially mediate the relation between SLE and depression. For instance, when compared to males, females seem to be more vulnerable to the adverse effects of psychosocial stressors (19). Studies (19, 20) stressed the link between the personality trait “neuroticism,” which increases the likelihood of maladaptive responses and coping in the face of negative life events and increased sensitivity to stress and severity of MDD. Importantly, Kendler and colleagues (20) found that, in a sample of more than 7500 twins, higher neuroticism enhanced the likelihood of depressive episodes in response to SLE.
The above indicates that SLE should be taken into consideration in affective disorder patients due to their impact on illness course and outcomes including suicide. Thus, the present study aimed to compare socio-demographic/clinical characteristics (including marital and living level, family history of psychiatric conditions and/or suicidal behavior, melancholic characteristics in the past, residual interepisodic symptoms, psychiatric medications in the past, current antidepressant medications use, and specific psychometric measures) of euthymic MDD outpatients experiencing significant SLE in the previous 6 months and those who did not, focusing on specific features that may explain the differential burden of disease directly linked to having or not experienced recent SLE. Our aim was also to test whether the effect of current antidepressants use on SLE was mediated by specific variables (i.e., previous psychiatric medications, family history of suicide). Here, we mainly hypothesize that previous psychiatric medications have a significant direct/indirect effect on SLE.
Methods
Sample
The present sample is composed of 628 currently euthymic MDD outpatients with age ranging from 18 to 85 years (mean age=55.1 ± 16.1). Clinically, euthymia was defined using a Montgomery–Asberg Depression Rating Scale (MADRS) (21) score of <10. Our sample included predominantly single MDD outpatients (52.9%) and, in a relatively smaller proportion, recurrent MDD outpatients (47.1%). Participants are all consecutive euthymic unipolar outpatients receiving only maintenance treatment at the time of evaluation. Overall, 488 subjects (77.7%) of our sample were treated with antidepressant medications and 140 individuals (22.3%) received only psychotherapy as maintenance. In particular, psychopharmacological treatments and psychopathological conditions were stable for at least 6 months before assessment. All euthymic MDD outpatients were recruited from our catchment area and have been followed/treated by our university outpatient service for at least 12 months. In addition, they were regularly followed by our local psychiatric services.
Measures and Study Design
An investigator (GC) who was adequately trained to improve the interrater reliability administered to participants the following psychometric instruments: 1) Clinical Global Impression (CGI) (22); 2) Beck Hopelessness Scale (BHS) (23); 3) Hamilton Anxiety Rating Scale (HARS) (24); 4) Global Assessment of Functioning Scale (GAF) (American Psychiatric Association, 1987) (25); 5) Childhood Trauma Questionnaire (CTQ) (26); 6) Coping Orientation to the Problems Experienced (COPE) (27); 7) Toronto Alexithymia Scale (TAS-20) (28) to collect other relevant clinical information.
All clinical information were retraced, as specified, by using clinical files and lifetime computerized medical records. All outpatients accepted voluntarily to participate in the present study and provided their informed consent to participate. The local Ethical Review Board regularly approved the specified study design.
Ascertainment of Recent Stressful Life Events
Significant stressful/distressing life-events in the previous 6 months were collected based on self-report and described as follows: 1) maltreatment and violence (sexual/physical/emotional abuse, emotional/physical neglect, witnessing home/community aggression); 2) loss events (separations, death of a parent or close friend); 3) intrafamilial problems (parental divorce, family instability, social or economic problems); 4) school and interpersonal problems (failure of grade in school or in exam, breaking up with a close friend, and poor social relationships) (for more details, see 3 and 4).
Procedure and Data Collection
All MDD outpatients were recruited at the Department of Neuroscience (DINOGMI), University of Genoa, outpatient service, between July 2014 and February 2020. We used the following inclusion criteria: 1) a diagnosis of single/recurrent MDD; 2) euthymia; 3) a current age of >18 years. Depressive symptoms related to MDD were classified based on the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) (29). First, an investigator (GC) examined clinical records to retrace subjective histories and clinical variables; then, two senior authors (GS, MA) systematically and independently verified data by using the Mini International Neuropsychiatric Interview (MINI) (30) updated to map to DSM-5 (29). Direct interviews with patients/family members as well as investigation of existing medical records allow the detailed collection of clinical information regarding affective episodes prior the patients’ recruitment in our outpatient service. Specifically, we performed a comprehensive data collection using the following variables: 1) socio-demographic information; 2) individual data (e.g., personal autonomy, lifetime substance abuse/dependence, use of psychiatric medications and psychotherapy in the past); 3) positive history of clinical conditions/negative outcome in family (e.g., psychiatric disorders and suicidal behavior); 4) comorbid conditions (e.g., medical/psychiatric disorders); 5) illness course features (e.g., manifested melancholic features and/or current atypical depressive characteristics, seasonality, psychotic symptoms at first episode, single/recurrent episode, residual interepisodic symptoms, illness duration and untreated illness, current illness episode, number of previous affective episodes, age of illness onset, age at first treatment and first hospitalization, and lifetime suicide attempts).
Exclusion criteria were as follows: 1) all clinical conditions that may influence the ability to complete the evaluations including conditions such as Alzheimer’s disease, delirium, or severe neurological disorders like intellectual disability; 3) denial of informed consent, 4) a history of active abuse/dependence (throughout the previous 6 months). Lifetime substance use emerging during mental examination, was not considered a specific exclusion criterion. Intellectual disability was investigated using the Wechsler Adult Intelligence Scale (31).
Statistical Analyses
Subjects were categorized based on the presence/absence of SLE in the previous 6 months and divided into two groups similarly to existing published studies (32) outpatients with recent SLE and 2) outpatients without recent SLE. Data for categorical variables were analyzed using Student’s t-tests and Pearson chi-square/Fisher’s exact test in contingency tables (χ2). The Kolmogorov–Smirnov test was performed to confirm whether all the investigated variables in the sample followed the normal distribution. Significance was set at P ≤ 0.05 (two-tailed).
A binary logistic regression analysis considering specific socio-demographic characteristics (marital status that was dichotomized in married/unmarried status and living status that was dichotomized in living alone or not alone) together with other variables such as family history of suicidal behavior, comorbid panic disorder, previous psychiatric medications, manifested melancholic features in the past, interepisodic residual symptoms, current antidepressants use, and COPE positive reinterpretation and growth was carried out to investigate the contribution of these characteristics in predicting presence/absence of SLE.
Multicollinearity and extreme cases were excluded, and the normality of residuals (histograms and P–P plots) was appropriately checked.
To assess whether the effect of current antidepressants use on SLE was mediated by specific variables (i.e., previous psychiatric medications, family history of suicide), single-mediator models were tested according to the strategy recommended by Preacher and Hayes (33). In a single-mediator model, an independent variable (X = current antidepressants use) is hypothesized to act on the outcome variable (Y = SLE) in two ways: X change a mediator (e.g., Mi = previous psychiatric medications or family history of suicide; path Ai) that, in turn, changes an outcome variable (Y; path Bi), or X changes Y directly (path C′) (for more details, see Figure 1).
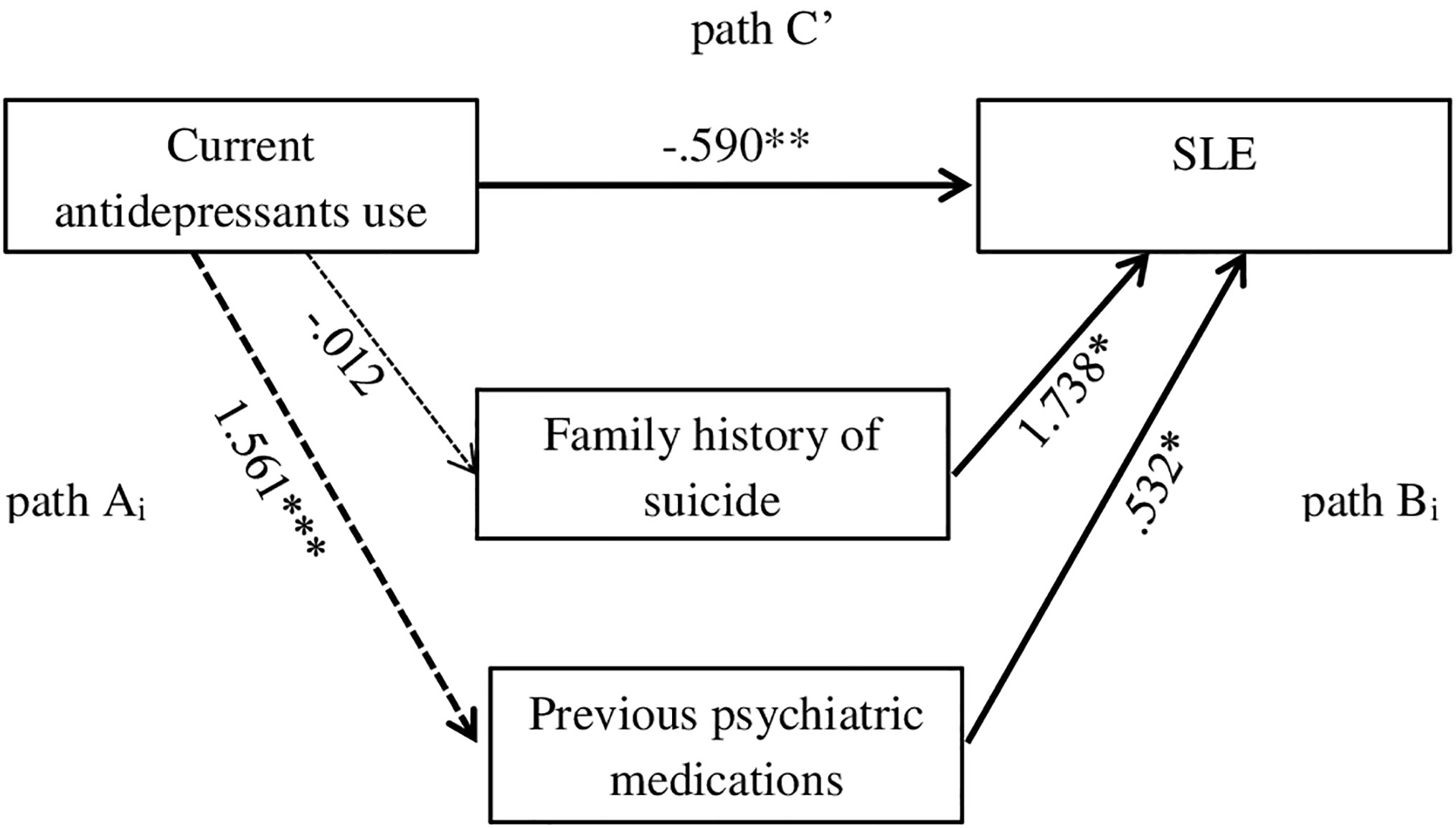
Figure 1 Mediation model with potential mediators (Paths Ai: Variable i→Mediator; Paths Bi: Mediator→Dependent Variable; Path C’: Independent Variable→Dependent Variable). *p = ≤ .05; **p = ≤ .01; ***p = ≤ .001.
The Statistical Package for Social Sciences (SPSS) for Windows 21.0 was used to carry out all the statistical analyses.
Results
Socio-Demographic and Clinical Variables of Outpatients With Significant Stressful Life Events in the Previous 6 Months Compared With Those Without
The sample includes 628 euthymic MDD outpatients who were consecutively and voluntarily recruited at the outpatient service of Department of Neuroscience (DINOGMI), University of Genoa from the catchment area. Socio-demographic and clinical features of outpatients are summarized in Table 1.
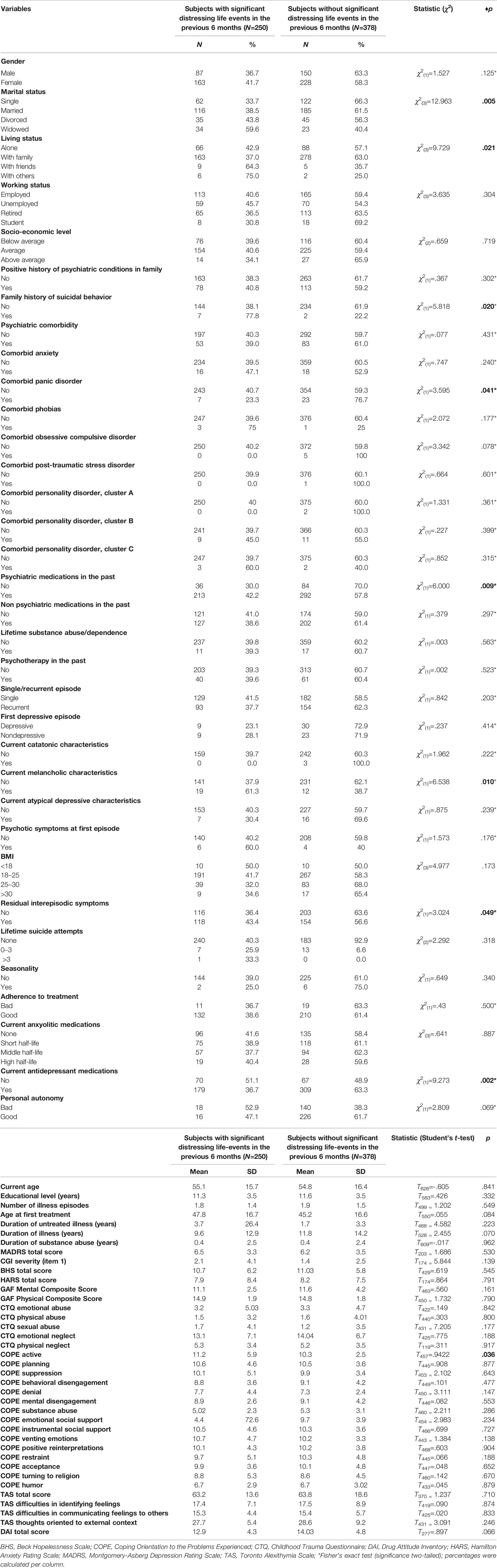
Table 1 Socio-demographic and clinical variables (categorical and quantitative) in patients with significant distressing life-events in the last 6 months (N=250) compared with those without (N=378).
Frequency of Recent Stressful Life Events and Associated Socio-Demographic and Clinical Characteristics
Among subjects who were recruited, 250 (39.8%) reported significant SLE in the previous 6 months and 378 (60.2%) did not.
Those reporting recent SLE [87 males (36.7%) and 163 females (41.7%)] differed from individuals who did not report recent SLE. Specifically, when compared with those who did not report recent SLE subjects with recent SLE differed in terms of both marital and living status (χ2(3)=12.963, p=.005; χ2(3)=9.729, p=≤.05), respectively.
Relative to outpatients without recent stressful life events, those who have experienced these events were more likely to have a family history of suicidal behavior (77.8 vs. 22.2%) (χ2(1)=5.818, p=≤.05), less likely to have a comorbid panic disorder (23.3 vs. 76.7%) (χ2(1)=3.595, p=≤.05) and less likely to have used psychiatric medications (42.2 vs. 57.8%) (χ2(1)=6.000, p=≤.01).
When compared to subjects without SLE in the previous 6 months, subjects with recent stressful events were also more likely to have exhibited melancholic characteristics in the past (61.3 vs. 38.7%) (χ2(1)=6.538, p=.01) and less likely to manifest residual interepisodic symptoms (43.4 vs. 56.6%) (χ2(1)=3.024, p=≤.05) and use current antidepressant medications (36.7 vs. 63.3%) (χ2(1)=9.273, p=≤.005).
The Kolmogorov–Smirnov test did not find any significant abnormality concerning the continuous data. Moreover, subjects with recent SLE were more likely to have a higher COPE positive reinterpretation and growth (11.2 ± 5.9 vs. 10.3 ± 2.5, t457 = 9.422, p ≤.05) when compared to those without SLE in the previous 6 months (for more details, see Tables 1 and 2).
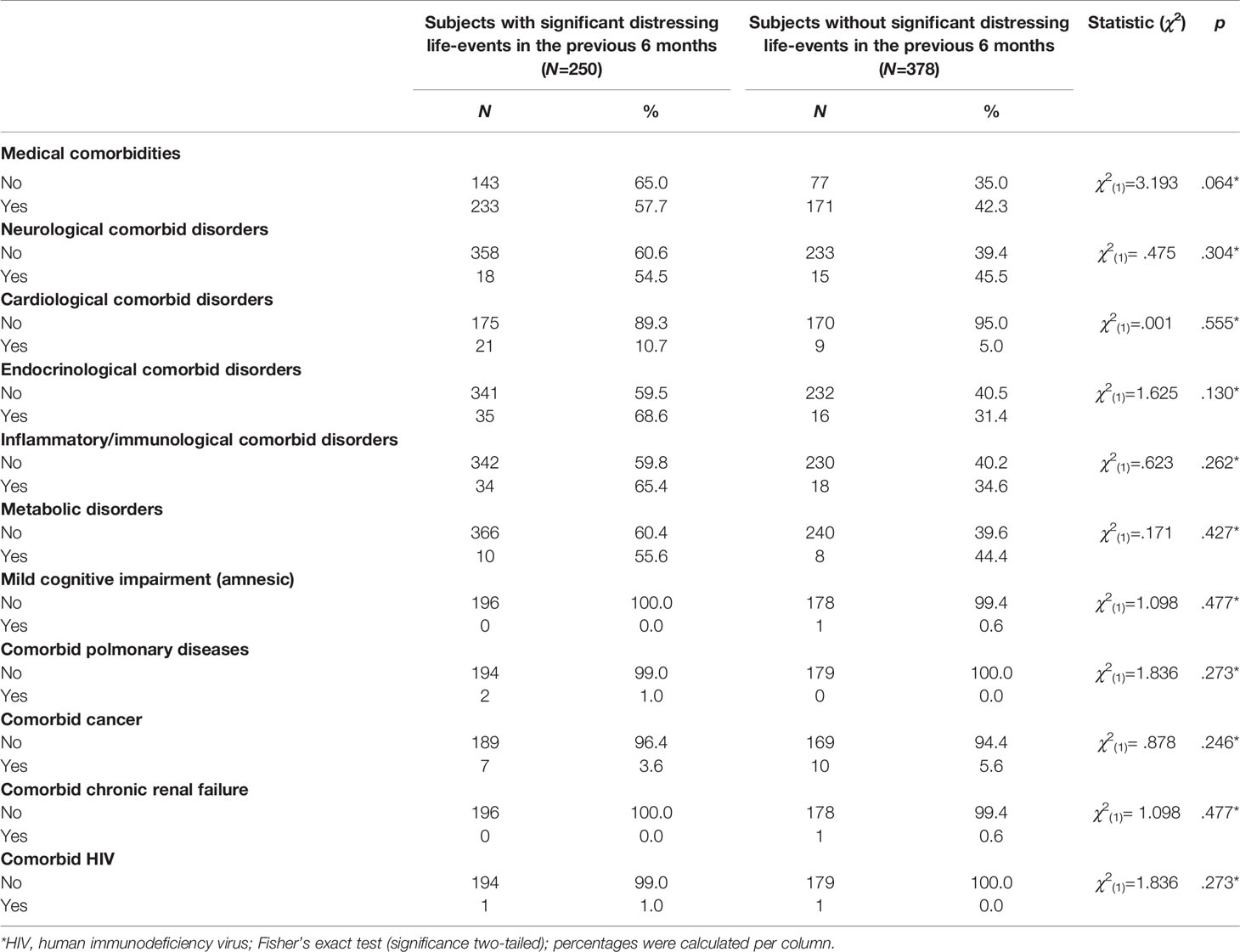
Table 2 Medical comorbidity in patients with significant distressing life-events in the previous 6 months (N=250) compared with those without (N=378).
Multivariate Regression Analyses Including Stressful Life Events as Dependent Variable in the Total Sample
All clinical variables which were significant at the univariate analyses were entered into a binary logistic regression analysis with SLE as dependent variable in order to identify independent factors which resulted associated with. Specific socio-demographic characteristics such as marital and living status as well as clinical variables (e.g., family history of suicidal behavior, comorbid panic disorder, previous psychiatric medications, manifested melancholic features in the past, interepisodic residual symptoms, current antidepressants use, and COPE positive reinterpretation and growth) were introduced into the regression model. The amount of variation in the first dependent variable (presence/absence of recent SLE) that was accounted for all predictors (R2-value) was 18.3% (p≤.001) (see Table 3).
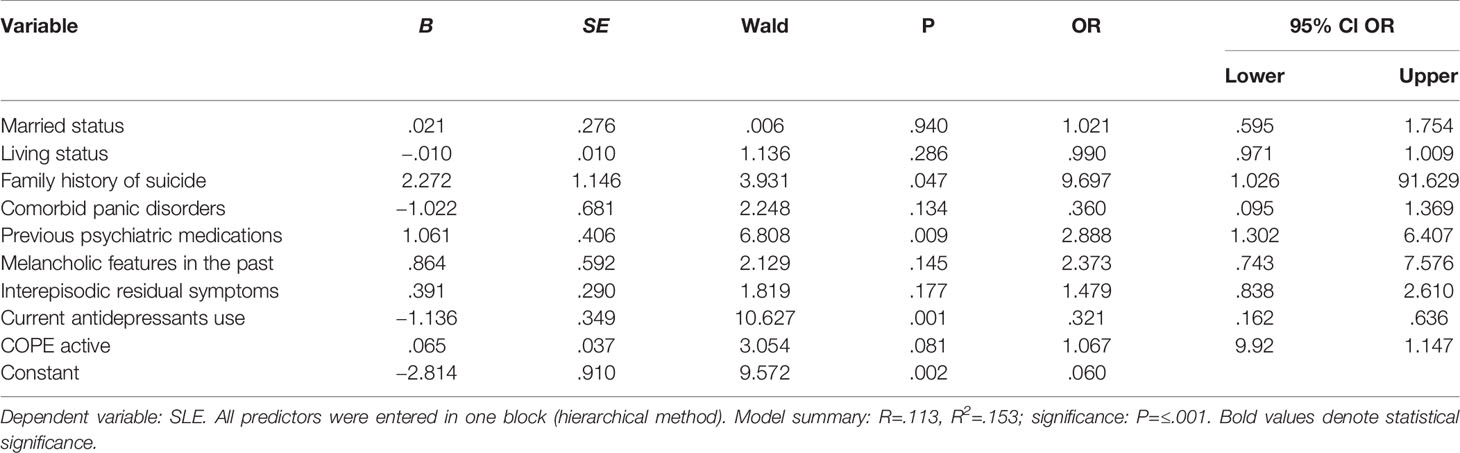
Table 3 Multiple regression model of significant distressing life-events in the previous 6 months in the total sample (N=628).
Having a family history of suicide with an OR of 9.697 (p=≤.05), history of psychotropic medications use with an OR of 2.888 (p=≤.01), and reduced use of antidepressant drugs with an OR of .321 (p=.001) were all significantly associated with recent SLE.
Mediation Analyses
In a regression model with current antidepressants use and family history of suicide as predictors and SLE as criterion, the regression models were both significant (R2 = .020, B = -.590, SE=.195, Wald = 9.145, p = .002, OR = .554) (R2 = .020, B = 1.738, SE=.809, Wald = 4.620, p = .032, OR = 5.687), respectively. When considering the effect of current antidepressants use on SLE in a single mediator model (considering first family history of suicide and later previous psychiatric medications as possible mediators), the results were as follows.
Family history of suicide had a significant direct effect on SLE (family history of suicide: omnibus test of direct effect of Mi on Y: R2 = .020, B = 1.738, SE=.809, Wald = 4.620, p = .032, OR = 5.687) but a nonsignificant indirect effect (family history of suicide: omnibus test of direct effect of X on Mi: R2 = .000, B = -.012, SE=.811, Wald = .000, p = .988, OR = .988). Previous psychiatric medications had a significant direct effect on SLE (previous psychiatric medications: omnibus test of direct effect of Mi on Y: R2 = .013, B = .532, SE=.219, Wald = 5.917, p = .015, OR = 1.702) and a significant indirect effect (previous psychiatric medications: omnibus test of direct effect of X on Mi: R2 = .121, B = 1.561, SE=.219, Wald = 50.777, p = <.001, OR = 4.765).
Discussion
Our study investigating the association of recent SLE in euthymic depressive patients indicated that the experience of recent stressful events was associated with several clinical, course, and sociodemographic characteristics, some of which may be clinically utilizable in understanding and managing the culminating effect of life stressors in influencing illness course and outcome.
Socio-Demographic Characteristics of Outpatients With Significant Stressful Life Events in the Previous 6 Months Compared With Those Without
Euthymic outpatients who experienced SLE differed from those who did not experience SLE in terms of both marital and living status.
Existing evidence suggested that being widowed is generally perceived as one of the most SLE (34) linked to relevant impairments in the general well-being of the bereaved spouse. According to previously published studies (35), widowers and widows should be considered at higher risk to experience lower subjective well-being even several years after the death of the spouse. In line with these findings, Carnelley and colleagues (36) found that widowers/widows experienced a significant distress and reduced subjective wellbeing even decades after the death. Similarly, we found a higher ratio of those widowed among those experiencing recent distressing events.
On the other hand, conversely to existing evidence suggesting that subjects who have more contact with friends and family are happier than those who have less contact (37), we found that outpatients who experienced SLE lived predominantly with friends or others. However, living with family rather than living with friends may be generally interpreted as a protective factor for MDD patients. This discrepancy could be related, in our opinion, to the fact that, although being recruited in stable psychopathological conditions, participants of the present study are predominantly affected by MDD (single episode) which is a condition for which many of them might have searched a significant social contact or asked support due to their illness.
Clinical Characteristics of Euthymic Outpatients Experiencing Significant Stressful Life Events in the Previous 6 Months Compared With Those Without
As for clinical variables, outpatients experiencing significant SLE were more likely to have a family history of suicidal behavior, manifested melancholic features in the past, report a higher COPE positive reinterpretation and growth, and less likely to have a comorbid panic disorder, residual interepisodic symptoms, past psychiatric medication use, and current antidepressant medication use.
In line with previous evidence (38) suggesting that the occurrence of SLE was higher and the associated perceived experience was more deleterious in suicidal patients, we found an association between SLE in the previous six months and family history of suicidal behavior. Specifically, this could be explained by the assumption that the interpersonal pattern linked to family history of suicide may consistently influence the ability to maintain stable and significant relations with others as supported by Rajalin and colleagues (39).
Moreover, we found that subjects with recent SLE were more likely to have manifested melancholic features in the past. Existing studies analyzed the association between depression subtypes and the likelihood to experience life adverisities. For instance, Kohn and colleagues (40) reported that, in a sample of 115 MDD patients, subjects with nonmelancholic depression or first depressive episode more frequently experienced ≥3 life adversities when compared to severe, melancholic, or recurrent depression. However, they investigated only a subset of MDD patients which is more prone to suffer from a cluster of negative life events. In addition, while the study of Kohn and colleagues (40) analyzed a sample of patients with mild-moderate depression, we investigated a larger (N=628) sample of MDD euthymic subjects. Thus, the main differences between our study and the study of Kohn and colleagues (40) may be related to the different study sample selection and different clinical characteristics.
Finally, we found that those who experienced SLE were more likely to report higher COPE positive reinterpretation and growth. This may be explained by the fact that the attitudes to cope with stress in our MDD patients, the psychopathological conditions of which were stable for at least 6 months before assessment, were more pronounced than those of other patient populations. Clinicians and health professionals should take appropriately into account these data in order to conduct psychotherapeutic interventions which are directed toward further coping with stress and create treatment strategies which may result especially useful in improving functional capacity in the identified stable phases of MDD.
Predictors of Stressful Life Events and Mediators of the Associations With Stressful Life Events
After binary regression analysis, MDD patients with recent SLE were more likely to have a family history of suicide (OR=9.68) and a history of psychotropic medications use (OR=2.89), but they were less likely to use currently antidepressants (OR=.32). In particular, outpatients who have experienced recent SLE were more likely to report a family history of suicide, more likely to have used previous psychiatric medications, and less likely to currently use antidepressants drugs that those without recent SLE in the previous 6 months.
Generally, having a family history of suicidal behavior is also associated with a greater propensity to SLE; thus, clinicians should be warned about carefully searching for suicidal thoughts in this patient subgroup as these individuals might exhibit a worse combination of biological, psychological, and environmental risk for suicide. In particular, in individuals with family history of suicidal behavior, the increased likelihood to experience stressful life events may enhance the perception of fewer reasons for living, thus elevating the risk of suicidal behavior, although in our study we did not observe significant differences in terms of suicide attempts between those with and without recent stressful life events. Consistent with this hypothesis, evidence documented that having a family history of suicide or attempted suicide is a significant risk factor for suicidal behavior and supposed the existence of a specific genetic component of suicidal behavior (41, 42). In line with these results, Rajalin and colleagues (39), recently found in a sample of 181 suicide attempters that having a family history of suicide was linked to factor 2 (nonassertive; exploitable; overly nurturant, and intrusive), in particular with Intrusive scale scores of the Inventory of Interpersonal Problems (IIP). Subjects with higher scores in the Intrusive subscale of the IIP are described to be excessively controlling, not careful to respect individual and other´s boundaries as well as more prone to take charge of other subjects’ problems (39). This may imply that these individuals pervasively experience disappointment and presumably reject in social contexts appearing unable to identify themselves in positive arguments with others. According to these findings, subjects who have experienced recent SLE and report a positive history of suicide among family members seem to exhibit specific deficits in interpersonal functioning. Moreover, evidence (43) clearly suggested that having a family history of suicide may be considered not only as a biological but also a psychological risk factor for familial transmission of suicide. Unfortunately, in our study we were not able to investigate the impact of interpersonal difficulties in subjects with family history of suicidal behavior who have also experienced recent SLE. In addition to the identified at risk profile, the participants of our study were also more likely to be widowed and have used psychiatric medications in the past.
Surprisingly, after multivariate analysis, subjects with significant SLE were less likely to currently use antidepressant drugs compared to those without recent stressful life events. This finding may be presumably explained by the fact that the majority of our study participants suffer predominantly from reactive and situational depression, but it is also possible that individuals who experienced recent SLE in our study may rely on more resilient social groups in which they received social support even in the context of negative interpersonal events or may have benefited from a psychotherapeutic approach. Such support may have helped them to better cope with SLE, thus reducing the current use of antidepressant medications. However, most patients do not frequently consult psychiatrists or mental health professionals due to stigma and discrimination as well as fear of disability and chronicity related to psychiatric conditions. This may, at least partially, justify the reduced or absent psychiatric services attendance in the past.
Finally, according to mediation analyses the association between the reduced use of antidepressant drugs and SLE was mediated by the history of psychotropic medications use. Thus, with this result we confirm the initial hypothesis based on which previous psychiatric medications had a significant direct/indirect effect on SLE. Specifically, subjects with a reduced use of antidepressants may be more vulnerable to experience SLE, in particular whether they have been treated in the past with psychiatric medications (that may have been prematurely discontinued by patients). This result is in line with the questioned long-term partial benefits of psychiatric medications (44) and may reflect, in our opinion, the limited potential of these compounds, which are detrimentally interrupted by patients on their own initiative (45, 46), on protecting against long-term exposure to stressors.
Unfortunately, whether the use of pharmacological medications is not combined with other available treatment strategies (e.g., psychotherapy), depressed individuals who have been treated only with psychoactive agents may be insufficiently protected in the long-term period towards potential illness recurrences (47, 48) neither they seem to have developed specific coping strategies to successfully cope with psychosocial distress in daily life. To further confirm our findings, it has been reported that the current use of antidepressants may help subjects to face intense emotional stimuli and stressful cues (49), presumably by attenuating the brain expression and/or actions of pro-inflammatory mediators. Here, we add that having undergone a psychiatric treatment (that may have been prematurely discontinued) is associated with the more frequent occurrence of SLE, if MDD patients are not adequately treated with antidepressant medications.
Limitations of the Study
The present study should be considered in the light of the following limitations/shortcomings. First, SLE were not measured using specific psychometric instruments such as the Social Readjustment Rating Scale (SRRS) which assesses the frequency of 43 common stressful life events occurring over the previous 12 months (34), that would allow us to rate the impact of specific stressful life experiences on a specific severity scale. In addition, we were also unable to use specific psychometric tools like the Karolinska Self Harm History Interview (50), including specific questions regarding family history of suicidal behavior in order to investigate the family history of completed suicide in a more detailed manner. In addition, the cross-sectional nature of the present study potentially leading to type I errors needs to be considered as an additional caveat. Moreover, we were not able to collect information regarding positive life events in the present study and thus we mainly explored the impact of negative ones. Additionally, by setting a P value of ≤.05, some significant differences in our univariate analyses may lead to false-positive findings due to multiple comparisons. Unfortunately, we were not able to apply an adjustment for multiple comparisons (e.g., Bonferroni’s adjustment)
Furthermore, we mainly analyzed a specific list of SLE: maltreatment and violence; loss events; intrafamilial problems; school and interpersonal problems based on our clinical experience as well as according to previously published studies (3, 4) without considering other types of SLE such as specific interpersonal stressors that may influence the onset/maintenance of depression in specific sociocultural environments (39).
Additionally, we did not take into account the possible link between the time from the occurrence of these events and recent SLE. For instance, one can inquire that having experienced the loss of a loved one by suicide even in the past may have influenced the likelihood to experience recent SLE. Although we did not find in our sample any recent loss event directly related to the loss of a loved one by suicide, the association between family history of suicide in the past and SLE may be affected by this caveat. Furthermore, we were not able in this study to investigate the effect of previous SLE, such as childhood traumatic experiences. Moreover, psychological factors which may further enhance the risk of negative outcome such as neuroticism, that were comprehensively examined in existing studies (19), were not considered in our study. Also, the role of potential protective factors like social support (51) or coping skills (52) were not taken specifically into account. Finally, while previous studies (53) supported a significant dose-response effect of the number of life events on illness course and outcome, here we were not able to identify the exact number of SLE.
However, despite the mentioned shortcomings, the recruitment of a large homogeneous sample of outpatients with MDD who were clearly euthymic together with the investigation of the effects of a comprehensive set of potential socio-demographic and clinical variables on the outcome need to be considered as major strengths of this study.
Conclusion
Having a family history of suicide and history of psychotropic medications use but even the reduced use of antidepressant drugs, of which some (e.g., duloxetine) act as inhibitors of both norepinephrine and serotonin transporters (54) and others (e.g., agomelatine) are of particular interest due to their ability to enhance neuroplasticity mechanisms (55), may reflect a specific “at risk” clinical profile characterized by the enhanced vulnerability to experience SLE. This finding is in line with the expression of a complement of genes that correlates with the degree of adversity, based on the assumption that early adversities may predispose selective molecular systems and related gene expression profiles associated with impaired stress response and/or differences in the sensitivity of specific genes involved in the response to stress signals (56, 57). Further additional studies are needed in order to test these exploratory findings.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material; further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Local Ethical Review Board of the University of Genoa, Liguria, Italy. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
GS designed the study and wrote the manuscript. GC managed the literature searches and analyses. XG and PG contributed to write the first draft of the manuscript. MA provided the intellectual impetuous and MP supervised the study design and search strategy. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This work was developed within the framework of the DINOGMI Department of Excellence of MIUR 2018-2022 (law 232/2016). Xenia Gonda was supported by the Janos Bolyai Research Fellowship of the Hungarian Academy of Sciences.
References
1. Grant KE, Compas BE, Stuhlmacher AF, Thurm AE, McMahon SD, Halpert JA. Stressors and child and adolescent psychopathology: Moving from markers to mechanisms of risk. Psychol Bull (2003) 129:447–66. doi: 10.1037/0033-2909.129.3.447
2. Monroe SM, Harkness KL. Life stress, the `kindling’ hypothesis, and the recurrence of depression: Considerations from a life stress perspective. Psychol Rev (2005) 112:417–45. doi: 10.1037/0033-295X.112.2.417
3. Serafini G, Muzio C, Piccinini G, Flouri E, Ferrigno G, Pompili M, et al. Life adversities and suicidal behavior in young individuals: a systematic review. Eur Child Adolesc Psychiatry (2015) 24:1423–46. doi: 10.1007/s00787-015-0760-y
4. Zhou L, Chen J. Life events and hopelessness depression: The influence of affective experience. PloS One (2017) 12:e0187898. doi: 10.1371/journal.pone.0187898
5. Kendler KS, Hettema JM, Butera F, Gardner CO, Prescott CA. Life event dimensions of loss, humiliation, entrapment, and danger in the prediction of onsets of major depression and generalized anxiety. Arch Gen Psychiatry (2003) 60:789–96. doi: 10.1001/archpsyc.60.8.789
6. Pompili M, Innamorati M, Lamis DA, Erbuto D, Venturini P, Ricci F, et al. The associations among childhood maltreatment, “male depression” and suicide risk in psychiatric patients. Psychiatry Res (2014) 220:571–8. doi: 10.1016/j.psychres.2014.07.056
7. Kõlves K, Ide N, De Leo D. Fluctuations of suicidality in the aftermath of a marital separation: 6-month follow-up observations. J Affect Disord (2012) 142:256–63. doi: 10.1016/j.jad.2012.04.036
8. Spinhoven P, Elzinga BM, Hovens JG, Roelofs K, van Oppen P, Zitman FG, et al. Positive and negative life events and personality traits in predicting course of depression and anxiety. Acta Psychiatr Scand (2011) 124:462–73. doi: 10.1111/j.1600-0447.2011.01753.x
9. Gallo WT, Bradley EH, Siegel M, Kasl SV. Health effects of involuntary job loss among older workers: Findings from the health and retirement survey. J Gerontol B Psychol Sci Soc Sci (2000) 55B:S131–40. doi: 10.1093/geronb/55.3.s131
10. Turner RJ, Lloyd DA. Lifetime traumas and mental health: the significance of cumulative adversity. J Health Soc Behav (1995) 36:360–76. doi: 10.2307/2137325
11. Mayo D, Corey S, Kelly LH, Yohannes S, Youngquist AL, Stuart BK, et al. The role of trauma and stressful life events among individuals at clinical high risk for psychosis: A review. Front Psychiatry (2017) 20:55. doi: 10.3389/fpsyt.2017.00055
12. Oquendo MA, Perez-Rodriguez MM, Poh E, Sullivan G, Burke AK, Sublette ME, et al. Life events: a complex role in the timing of suicidal behavior among depressed patients. Mol Psychiatry (2014) 19:902–9. doi: 10.1038/mp.2013.128
13. Furniss T, Beyer T, Müller JM. Impact of life events on child mental health before school entry at age six. Eur Child Adolesc Psychiatry (2009) 18:717–24. doi: 10.1007/s00787-009-0013-z
14. Rutter M, Silberg J. Gene-environment interplay in relation to emotional and behavioral disturbance. Annu Rev Psychol (2002) 53:463–90. doi: 10.1146/annurev.psych.53.100901.135223
15. Maciejewski PK, Mazure CM. Stressful life events and depression. Am J Psychiatry (2000) 157:1344–5. doi: 10.1176/appi.ajp.157.8.1344-a
16. Kendler KS, Karkowski LM, Prescott CA. Stressful life events and major depression: risk period, longterm contextual threat, and diagnostic specificity. J Nerv Ment Dis (1988) 186:661–9. doi: 10.1097/00005053-199811000-00001
17. Bos EH, Bouhuys AL, Geerts E, van Os TW, Ormel J. Stressful life events as a link between problems in nonverbal communication and recurrence of depression. J Affect Disord (2007) 97:161–9. doi: 10.1016/j.jad.2006.06.011
18. Post RM. Transduction of psychosocial stress into the neurobiology of recurrent affective disorder. Am J Psychiatry (1992) 149:999–1010. doi: 10.1176/ajp.149.8.999
19. Kendler KS, Kuhn J, Prescott CA. The interrelationship of neuroticism, sex, and stressful life events in the prediction of episodes of major depression. Am J Psychiatry (2004) 161:631–6. doi: 10.1176/appi.ajp.161.4.631
20. Kendler KS, Gardner CO. A longitudinal etiologic model for symptoms of anxiety and depression in women. Psychol Med (2011) 41:2035–45. doi: 10.1017/S0033291711000225
21. Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry (1979) 134:382–9. doi: 10.1192/bjp.134.4.382
22. Guy W. ECDEU Assessment Manual for Psychopharmacology. Rockville, MD (US): Department of Health, Education, and Welfare (1976).
24. Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol (1959) 32:50–5. doi: 10.1111/j.2044-8341.1959.tb00467.x
25. American Psychiatric Association. Diagnactic and Statical Manual of Mental Disorders. 3rd edn, revised. DSM-III-R: Washington, DC (1987).
26. Bernstein DP, Ahluvalia T, Pogge D, Handelsman L. Validity of the Childhood Trauma Questionnaire in an adolescent psychiatric population. J Am Acad Child Adolesc Psychiatry (1997) 36:340–8. doi: 10.1097/00004583-199703000-00012
27. Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: A theoretically based approach. J Pers Soc Psychol (1989) 56:267. doi: 10.1037//0022-3514.56.2.267
28. Bagby RM, Parker JD, Taylor GJ. The twenty-item Toronto Alexithymia Scale–I. Item selection and cross-validation of the factor structure. J Psychosom Res (1994) 38:23–32. doi: 10.1016/0022-3999(94)90005-1
29. American Psychiatric Association. DSM-5 Task Force. In: Diagnostic and statistical manual of mental disorders: DSM-5™, 5th ed. Arlington, VA: American Psychiatric Publishing (2013).
30. Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry (1998) 59(Suppl 20):22–33; quiz 34-57.
31. Wechsler D. WISC-IV Wechsler Intelligence Scale for Children: Technical and interpretative manual. Psychological Corporation: San Antonio (TX) (2003).
32. Mazure CM, Maciejewski PK, Jacobs SC, Bruce ML. Stressful life events interacting with cognitive/personality styles to predict late-onset major depression. Am J Geriatr Psychiatry (2002) 10:297–304. doi: 10.1097/00019442-200205000-00009
33. Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods (2008) 40:879–91. doi: 10.3758/brm.40.3.879
34. Holmes TH, Rahe RH. The social readjustment rating scale. J Psychosom Res (1967) 11:213–8. doi: 10.1016/0022-3999(67)90010-4
35. Yap SCY, Anusic I, Lucas RE. Does personality moderate reaction and adaptation to major life events? Evidence from the British Household Panel Study. J Res Pers (2012) 46:477–88. doi: 10.1016/j.jrp.2012.05.005
36. Carnelley KB, Wortman CB, Bolger N, Burke CT. The time course of grief reactions to spousal loss: Evidence from a national probability sample. J Pers Soc Psychol (2006) 91:476–92. doi: 10.1037/0022-3514.91.3.476
37. Lucas RE, Dyrenforth PS. Does the Existence of Social Relationships Matter for Subjective Well-being. In: Vohs KD, Finkel EJ, editors. Self and relationships: Connecting intrapersonal and interpersonal processes. New York: Guilford Press (2006).
38. Fennig S, Horesh N, Aloni D, Apter A, Weizman A, Fennig S. Life events and suicidality in adolescents with schizophrenia. Eur Child Adolesc Psychiatry (2005) 14:454–60. doi: 10.1007/s00787-005-0498-z
39. Rajalin M, Hirvikoski T, Salander Renberg E, Åsberg M, Jokinen J. Family history of suicide and interpersonal functioning in suicide attempters. Psychiatry Res (2017) 247:310–4. doi: 10.1016/j.psychres.2016.11.029
40. Kohn Y, Zislin J, Agid O, Hanin B, Troudart T, Shapira B, et al. Increased prevalence of negative life events in subtypes of major depressive disorder. Compr Psychiatry (2001) 42:57–63. doi: 10.1053/comp.2001.19753
41. Pompili M, Gibiino S, Innamorati M, Serafini G, Del Casale A, De Risio L, et al. Prolactin and thyroid hormone levels are associated with suicide attempts in psychiatric patients. Psychiatry Res (2012) 200:389–94. doi: 10.1016/j.psychres.2012.05.010
42. Roy A, Segal NL, Centerwall BS, Robinette CD. Suicide in twins. Arch Gen Psychiatry (1991) 48:29–33. doi: 10.1001/archpsyc.1991.01810250031003
43. Tidemalm D, Runeson B, Waern M, Frisell T, Carlström E, Lichtenstein P, et al. Familial clustering of suicide risk: a total population study of 11.4 million individuals. Psychol Med (2011) 41:2527–34. doi: 10.1017/S0033291711000833
44. Gøtzsche PC, Young AH, Crace J. Does long term use of psychiatric drugs cause more harm than good? BMJ (2015) 350:h2435. doi: 10.1136/bmj.h2435
45. McCann DJ, Petry NM, Bresell A, Isacsson E, Wilson E, Alexander RC. Medication Nonadherence, “Professional Subjects,” and Apparent Placebo Responders: Overlapping Challenges for Medications Development. J Clin Psychopharmacol (2015) 35:566–73. doi: 10.1097/JCP.0000000000000372
46. Lanouette NM, Folsom DP, Sciolla A, Jeste DV. Psychotropic medication nonadherence among United States Latinos: a comprehensive literature review. Psychiatr Serv (2009) 60:157–74. doi: 10.1176/appi.ps.60.2.157
47. Jawad I, Watson S, Haddad PM, Talbot PS, McAllister-Williams RH. Medication nonadherence in bipolar disorder: a narrative review. Ther Adv Psychopharmacol (2018) 8:349–63. doi: 10.1177/2045125318804364
48. Swann AC. Approaches to preventing relapse in bipolar disorder: addressing nonadherence and prodromal symptoms. J Clin Psychiatry (2010) 71:e35. doi: 10.4088/JCP.9075tx4c
49. Castanon N, Leonard BE, Neveu PJ, Yirmiya R. Effects of antidepressants on cytokine production and actions. Brain Behav Immun (2002) 16:569–74. doi: 10.1016/s0889-1591(02)00008-9
50. Jokinen J, Forslund K, Ahnemark E, Gustavsson JP, Nordström P, Asberg M. Karolinska Interpersonal Violence Scale predicts suicide in suicide attempters. J Clin Psychiatry (2010) 71:1025–32. doi: 10.4088/JCP.09m05944blu
51. Dalgard OS, Dowrick C, Lehtinen V, Vazquez-Barquero JL, Casey P, Wilkinson G, et al. Negative life events, social support and gender difference in depression: A multinational community survey with data from the ODIN study. Soc Psychiatry Psychiatr Epidemiol (2006) 41:444–51. doi: 10.1007/s00127-006-0051-5
52. Wilhelm K, Parker G, Dewhurst J. Examining sex differences in the impact of anticipated and actual life events. J Affect Disord (1998) 48:37–45. doi: 10.1016/s0165-0327(97)00138-9
53. Liu X, Tein JY. Life events, psychopathology, and suicidal behavior in Chinese adolescents. J Affect Disord (2005) 86:195–203. doi: 10.1016/j.jad.2005.01.016
54. Girardi P, Pompili M, Innamorati M, Mancini M, Serafini G, Mazzarini L, et al. Duloxetine in acute major depression: review of comparisons to placebo and standard antidepressants using dissimilar methods. Hum Psychopharmacol (2009) 24:177–90. doi: 10.1002/hup.1005
55. Pompili M, Serafini G, Innamorati M, Venturini P, Fusar-Poli P, Sher L, et al. P. Agomelatine, a novel intriguing antidepressant option enhancing neuroplasticity: a critical review. World J Biol Psychiatry (2013) 14:412–31. doi: 10.3109/15622975.2013.765593
56. Miller GE, Chen E, Parker KJ. Psychological stress in childhood and susceptibility to the chronic diseases of aging: moving towards a model of behavioral and biological mechanisms. Psychol Bull (2011) 137:959–97. doi: 10.1037/a0024768
Keywords: negative distressing/stressful life events, family history of suicide, major depressive disorder, previous psychiatric medications, antidepressant medications
Citation: Serafini G, Gonda X, Canepa G, Geoffroy PA, Pompili M and Amore M (2020) Recent Stressful Life Events in Euthymic Major Depressive Disorder Patients: Sociodemographic and Clinical Characteristics. Front. Psychiatry 11:566017. doi: 10.3389/fpsyt.2020.566017
Received: 26 May 2020; Accepted: 17 August 2020;
Published: 11 September 2020.
Edited by:
Manit Srisurapanont, Chiang Mai University, ThailandReviewed by:
George P. Chrousos, National and Kapodistrian University of Athens, GreeceLiliana Dell’Osso, University of Pisa, Italy
Copyright © 2020 Serafini, Gonda, Canepa, Geoffroy, Pompili and Amore. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gianluca Serafini, Z2lhbmx1Y2Euc2VyYWZpbmlAdW5pZ2UuaXQ=
 Gianluca Serafini
Gianluca Serafini Xenia Gonda
Xenia Gonda Giovanna Canepa
Giovanna Canepa Pierre A. Geoffroy
Pierre A. Geoffroy Maurizio Pompili
Maurizio Pompili Mario Amore1,2
Mario Amore1,2