- 1Department of Mental Health and Pathological Addiction, Azienda Unità Sanitaria Locale-Istituto di Ricovero e Cura a carattere Scientifico (USL-IRCSS) di Reggio Emilia, Reggio Emilia, Italy
- 2Department of Primary Care, Azienda Unità Sanitaria Locale (USL) di Parma, Parma, Italy
- 3Anesthesia and Resuscitation Service, Azienda Ospedaliero-Universitaria di Parma, Parma, Italy
- 4Division of Psychiatry, Department of Medicine, University of Perugia, Perugia, Italy
- 5Center for Translational, Phenomenological and Developmental Psychopathology, Perugia University Hospital, Perugia, Italy
- 6Department of Mental Health and Pathological Addiction, Azienda Unità Sanitaria Locale (USL) di Parma, Parma, Italy
Aim: Ultrahigh-risk (UHR) individuals have an increased vulnerability to psychosis because of accumulating environmental and/or genetic risk factors. Although original research examined established risk factors for psychosis in the UHR state, these findings are scarce and often contradictory. The aims of this study were (a) to investigate the prevalence of severe mental illness (SMI) in family members of distinct subgroups of adolescents identified through the UHR criteria [i.e., non-UHR vs. UHR vs. first-episode psychosis (FEP)] and (b) to examine any relevant associations of family vulnerability and genetic risk and functioning deterioration (GRFD) syndrome with clinical and psychopathological characteristics in the UHR group.
Methods: Adolescents (n = 147) completed an ad hoc sociodemographic/clinical schedule and the Comprehensive Assessment of At-Risk Mental States to investigate the clinical status.
Results: More than 60% UHR patients had a family history of SMI, and approximately a third of them had at least a first-degree relative with psychosis or other SMI. A GRFD syndrome was detected in ~35% of UHR adolescents. GRFD adolescents showed baseline high levels of positive symptoms (especially non-bizarre ideas) and emotional disturbances (specifically, observed inappropriate affect).
Conclusions: Our results confirm the importance of genetic and/or within-family risk factors in UHR adolescents, suggesting the crucial need of their early detection, also within the network of general practitioners, general hospitals, and the other community agencies (e.g., social services and school).
Introduction
In the last three decades, the early intervention in psychosis (EIP) paradigm has achieved increased consideration attention in the scientific community, generating focused programs of care within the mental health care network of different countries (1). Indeed, leaving patients with early psychosis untreated may have severe consequences in terms of quality of life, functioning, and health (e.g., treatment dropout, inpatient care, symptom severity), as well as in socioeconomic costs related to unemployment, long-term intervention, and poor outcomes of illness (2–4). However, to date, psychosis remains one of the most puzzling mental disorders, and our understanding of its etiopathological mechanisms is still far from being conclusive (5).
Vulnerability to Psychosis and the “Ultrahigh-Risk” Paradigm
The most validated model to explain the etiology of psychosis is based on environmental and genetic risk factors and their interaction (in various modalities and at various levels), likely involving epigenetic mechanisms (6, 7). The evidence that many subjects who are at ultrahigh risk (UHR) of psychosis actually do not develop a full-blown psychotic episode seems to confirm this hypothesis, suggesting a complex interplay among genetic, neurodevelopmental, neuropsychological, sociocultural, and environmental factors in psychoses (6).
The detection of risk factors correlated with early psychosis is crucial to advance early identification of vulnerable subjects and to propose tailored interventions for young help-seeking individuals (8). Indeed, the delivery of specialized, evidence-based treatments as early as possible has become one of the current priorities for professionals involved in mental health care service network (9, 10).
Since its conceptualization, the UHR paradigm quickly became increasingly influential in the field of psychiatry (7). The UHR mental state is currently defined on the basis of three main inclusion criteria, which have been internationally validated: brief and limited intermittent psychotic symptoms (BLIPSs), attenuated psychotic symptoms (APSs), and genetic risk and functioning deterioration syndrome (GRFD) [for details, see (11)]. Specifically, APSs are subthreshold positive psychotic symptoms within the past 12 months. In the BLIPS group, criteria for psychosis are met for <7 days at a time and ceasing spontaneously (i.e., without antipsychotic medications). The GRFD syndrome is a state/trait risk condition in which the patient has a family history of psychosis (i.e., in first-degree relatives) or manifests a schizotypal personality disorder, along with low functioning sustained for at least 1 month. Accumulating findings have confirmed that young help-seekers meeting well-defined UHR psychometric criteria show an increased risk of developing psychosis (mostly schizophrenia spectrum disorders) within a relatively short period of time (12). Indeed, the psychosis conversion in people at UHR is most likely to occur within the first 24 months after the first contact to clinical services, with a risk of transition accumulating to 29% at 2 years (13). After this period, the speed of psychosis progression tends to plateau from the third year, reaching ~35% after 10 years (14). This risk is significantly greater than that reported in the general population: indeed, people at UHR have a 2-year relative risk of developing psychosis of 460, as compared to the general population (29%/0.063%) (7).
UHR subjects are likely to have an increased vulnerability to psychosis because of accumulating environmental and/or genetic risk factors (6). However, although several original research has explored the association of established risk factors for psychosis and the UHR state, the results are scarce and often contradictory, also with regard to the prevalence of severe mental illness (SMI) in family members of UHR individuals (15). As psychosocial dysfunction represents a common prodromal sign in UHR mental states, which exposes these young help-seeking individuals to social stigma and long-term interpersonal marginalization, reducing employment and economic opportunities (16), it is absolutely crucial to implement effective models of early detection of psychosis vulnerability as soon as possible within the mental health service network, especially because this “functional critical period” may be susceptible to change if effective interventions are provided (5).
Starting from this background, the first aim of the current study was to investigate the prevalence of SMI in family members of UHR adolescents compared to similar age group of help-seeking peers with first-episode psychosis (FEP) or not meeting both UHR and FEP criteria (11). Moreover, for better specifying the clinical profile of UHR adolescents with family prevalence of SMI (especially psychosis), we also examined any relevant associations of the presence of family members with SMI (and psychosis) with functioning and psychopathology in our UHR subgroup. Finally, for the same reasons, we also investigated any significant relationship of the presence of a GRFD syndrome (i.e., a specific clinical index of family history of psychosis in first-degree relatives of UHR subjects) with functioning, sociodemographic, clinical, and psychopathological characteristics in our UHR subsample. To the best of our knowledge, this is the first Italian study specifically developed to examine the prevalence of SMI in family members of UHR adolescent help-seekers recruiting within a specific EIP program, as well as the presence of a GRSD syndrome in adolescents with early psychosis.
Materials and Methods
Subjects
Participants were help-seeking adolescents who entered the “Reggio Emilia at Risk Mental States” (ReARMS) program [for details, see also (1)] between September 2012 and December 2018. All participants (n = 147) and their parents gave an informed consent prior to their inclusion in the research. Relevant local ethical approvals were sought for the study. This research has been also performed according to the Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments including humans. The data that support the findings of this study are available on request from the authors. The data are not publicly available because of privacy or ethical restrictions.
Inclusion criteria of the present research were (a) age 13–18 years, (b) specialist help-seeking, (c) UHR criteria defined by the CAARMS (the “Comprehensive Assessment of At-Risk Mental States”) (i.e., BLIPSs, APSs, and GRFD) [for details, see (11)], or (d) a duration of untreated psychosis (DUP: defined as the time interval between the beginning of psychotic features and the first antipsychotic treatment) (17) <2 years if a CAARMS-defined FEP is identified at the initial assessment (11). According to the EIP paradigm (4), a DUP <2 years is a crucial limit to begin an EIP intervention, being a shorter DUP correlated with better FEP outcomes (18, 19). In the ReARMS program, early detection of UHR/FEP help-seeking adolescents was a 2-step procedure (1, 20). The first was a screening step using the “Screening Schedule” for Psychosis (21), administered by general service staff members. The second step consisted of the CAARMS interview (to explore the presence of an UHR mental state, a first-episode psychosis or neither), within a baseline multidimensional assessment process also including an ad hoc clinical/sociodemographic schedule [for details, see also (1)]. UHR– individuals were excluded from the ReARMS protocol, but received specific information for an appropriate treatment (2).
Exclusion criteria were (a) previous Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revised (DSM-IV-TR) affective and non-affective psychoses (22); (b) past exposure to antipsychotics; (c) known intellectual disability (IQ <70); (d) neurological disease or any other medical illness with psychiatric features; and (e) current substance dependence, according to DSM-IV-TR criteria (22). Specifically, we considered past exposure to antipsychotics (i.e., before the ReARMS recruitment) as an equivalent of a previous psychotic episode, in accordance with CAARMS-defined FEP criteria, suggesting that the FEP threshold essentially corresponds to that at which antipsychotics would supposedly be started in the common clinical practice (11).
Instruments and Measures
In the present research, the following instruments were used:
• An “ad hoc schedule” collecting specific clinical and sociodemographic information: i.e., gender, age, level of education, ethic group, mother tongue, employment status, prevalence of SMI in family members, DSM-IV-TR diagnosis, duration of untreated illness (DUI, defined as the time interval between the beginning of a marked psychopathological symptom and the first psychological/pharmacological intervention) (23), past hospitalization, previous specialist contact, previous suicide attempts [defined as a potentially injurious, self-inflicted behavior without a fatal outcome for which there was (implicit or explicit) evidence of intent to die] (24, 25), current substance abuse at the ReARMS enrollment, 1-year “dropout” rate, 1-year “psychosis transition” rate, 1-year CAARMS-defined psychometric criteria, and the specific ReARMS interventions provided to the users.
• CAARMS: a semistructured interview exploring several characteristics of the attenuated and full-blown psychotic psychopathology (i.e., positive symptoms, negative symptoms, disorganization, cognitive change, emotional disturbances, and general psychopathology), as well as the socio-occupational functioning [using the SOFAS (“Social and Occupational Functioning Assessment Scale”) module] [see (11), for details]. The CAARMS was administered by trained clinical psychologists and neuropsychiatrists [for details, see also (26)]. In the present research, we used the approved Italian version of the CAARMS (CAARMS-ITA) (27), which showed an excellent interrater reliability in Italian clinical samples of adolescents and young adults (26, 28).
In accordance with the DSM-IV-TR criteria (20), Axis I diagnoses were made using the Structured Clinical Interview for DSM-IV-TR Axis I Disorders (29). CAARMS UHR/FEP criteria (11) were used to separate the participants into the following three subsamples: (a) FEP sample; (b) UHR+ sample (i.e., BLIPSs, APSs, and GRFD), and (c) UHR– sample (i.e., those subjects who were below the CAARMS inclusion criteria). Finally, for better specifying the clinical profile of UHR adolescents with family history of SMI (especially psychosis), UHR+ participants were further dichotomized using the following criteria: (a) family history of SMI (i.e., considering all the degrees of family relationships), (b) presence of at least one first-degree relative with psychosis or other SMI, and (c) presence of a GRFD syndrome (i.e., alone or in comorbidity with APS or BLIPS condition). As suggested by Fulone et al. (30), for SMI, we expressly intended schizophrenia spectrum disorders or other related psychosis, bipolar disorder, and major depression.
Procedures and Statistical Analysis
In the present research all participants underwent ReARMS program, a baseline multidimensional assessment process including the ad hoc clinical/sociodemographic schedule and the CAARMS interview (to explore the presence of an UHR mental state, a first-episode psychosis or neither) [for details, see also (1)]. UHR– individuals were excluded from the ReARMS protocol, but received specific advises for an appropriate treatment (2).
Depending on the severity of their symptoms and functioning decline, UHR and FEP adolescents were provided with a 5-year intervention package composed by pharmacological therapy and a multielement psychosocial treatment [including individual cognitive-behavioral therapy (CBT), psychoeducational sessions for family members, and a case management for an early rehabilitation], in accordance with the modern guidelines (31–33). Specifically, antipsychotics were avoided unless the UHR+ participants (a) were rapidly deteriorating in daily functioning, (b) were overwhelmed by psychotic symptoms, and (c) had an imminent risk of suicide or serious violence (2, 19). Atypical antipsychotics in low dose were typically used. Benzodiazepines and selective serotonin reuptake inhibitors were also administered to treat anxiety, insomnia, and depressive symptoms.
Collected data were analyzed using the 15.0 version of the Statistical Package for Social Science for Windows (34). Significance threshold was fixed at p = 0.05 for all two-tailed tests. Descriptive variables were represented using mean values ± standard deviation (if continuous parameters) or frequencies and percentages (if categorical parameters). As all explorations were not normally distributed (Kolmogorov–Smirnov-test with Lilliefors correction: p < 0.05) (34), non-parametric statistics were used. Specifically, intergroup comparisons on characteristics involving continuous variables were analyzed with the Kruskal–Wallis-test and the Mann–Whitney U-test (as appropriate). The χ2-test or the Fisher exact test (i.e., when 20% of expected frequency was ≤ 5 or any expected frequency was <1) was performed for categorical parameters. The Mann–Whitney U-test was also used as post-hoc procedure in comparisons of continuous variables within more than two subgroups. Finally, the Holm-Bonferroni correction method (35) was performed to counteract the problem of multiple comparisons. Specifically, sociodemographic, clinical, and psychopathological features were compared in UHR+ participants subsequently dichotomized using the following categories: (a) family history of SMI (i.e., considering all the degrees of family relationships), (b) presence of at least one first-degree relative with psychosis or other SMI, (c) presence of GRFD syndrome (i.e., alone or in comorbidity with APS or BLIPS condition).
Results
A total of 147 adolescents [80 females (54.4%); 127 white adolescents (86.4%); mean age = 15.84 ± 1.67 years] consecutively entered the ReARM protocol from September 2012 to December 2018; of them, 96 (65.3%) youths were treated in the ReARMS program. As previously described [for details on characterization of young people with early psychosis who entered the ReARMS protocol, see also (2)], 11 adolescents were excluded because of exclusion criteria.
In the UHR+ subgroup [n = 51 (34.7% of the total sample)], 48 adolescents (94.1%) met the APS criteria, 2 (3.9%) met the BLIPS criteria, and only 1 met the GRFD criteria alone. Among the APS and BLIPS participants, 17 (34%) also met the GRFD criteria. At baseline, the most common diagnoses were represented by major depression (n = 23; 45.1%), anxiety disorders (n = 9; 17.6%), schizotypal personality disorder (n = 9; 17.6%), and obsessive–compulsive disorder (n = 4; 7.8%).
The FEP subgroup [n = 45 (30.6% of the total sample)] was composed of patients with DSM-IV-TR schizophrenia (n = 22; 48.9%), psychotic disorder not otherwise specified (n = 10; 22.2%), affective (major depressive or bipolar) psychosis (n = 9; 20.0%), and schizophreniform disorder (n = 4; 8.9%).
The remaining 51 adolescents (34.7% of the total sample) were under the CAARMS-defined UHR/FEP threshold and composed the UHR– subgroup. The most common diagnoses were represented by DSM-IV-TR depressive disorders (n = 22; 43.1%), non-schizotypal personality disorder (n = 18; 35.3%) (i.e., borderline, narcissistic, and avoidance personality disorder), and anxiety disorders (n = 11; 21.6%).
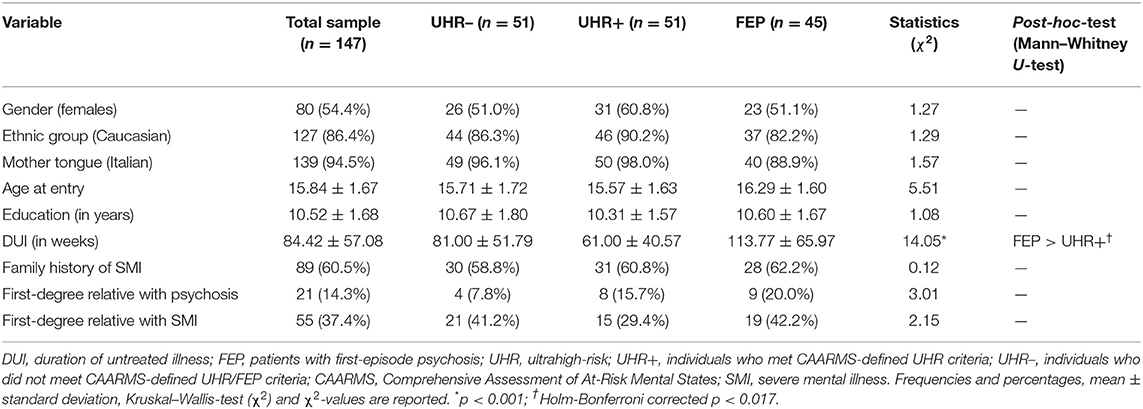
No intergroup differences in terms of gender, age, ethnic group, mother tongue, and years of education were observed (Table 1). Compared to UHR+, FEP adolescents showed a longer DUI. No intergroup differences were also found in terms of family history of SMI, as well as in first-degree relatives with psychosis or other SMI.
Family History of SMI and UHR+ Individuals: Clinical Profile
Among 31 UHR+ adolescents with family history of SMI [i.e., UHR+/F+ (60.8% of the UHR+ total group)], 30 met the APS criteria, and 1 met the BLIPS criteria at the baseline assessment; of them, 11 (35.5% of the UHR+/F+ total subgroup) also met the GRFD criteria.
Compared to UHR+ individuals without a family history of SMI (i.e., UHR+/F–), UHR+/F+ subjects showed a significantly lower CAARMS “Alogia” item subscore (Table 2). No other between-group difference in terms of baseline functioning, sociodemographic, clinical, and psychopathological characteristics was found. Similarly, no intergroup differences were observed in terms of frequency of specific ReARMS interventions provided to the UHR+ participants (i.e., antipsychotic medication, CBT, psychoeducational sessions for family members and case management oriented to an early recovery and rehabilitation).
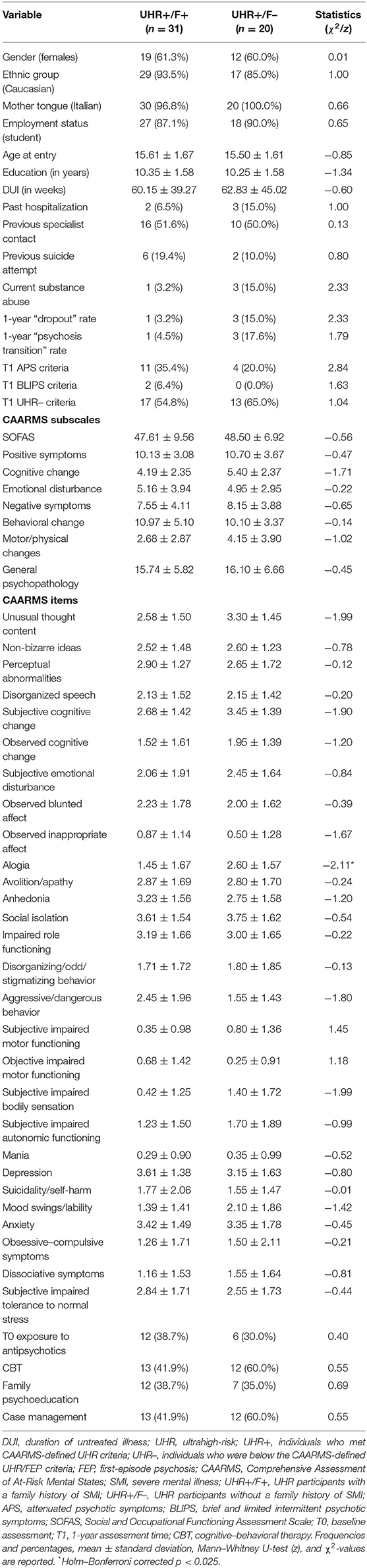
Table 2. Sociodemographic, psychopathological, and clinical characteristics between UHR+ participants with and without family history of SMI.
Among 15 UHR+ adolescents with at least a first-degree relative with psychosis or other SMI [i.e., UHR+/FDR+ (29.4% of the UHR+ total group)], 14 met the APS criteria and 1 met the BLIPS criteria at the baseline assessment; of them, 7 (46.7% of the UHR+/FDR+ total subgroup) also met the GRFD criteria.
Compared to UHR+ individuals without a first-degree relative with psychosis or other SMI (i.e., UHR+/FDR–), UHR+/FDR+ subjects showed a significantly lower CAARMS “alogia” and “suicidality/self-harm” item subscores (Table 3). No other intergroup differences in terms of baseline functioning and sociodemographic, clinical, and psychopathological features were found. Similarly, no between-group difference was reported in terms of frequency of specific ReARMS interventions provided to the UHR+ adolescents.
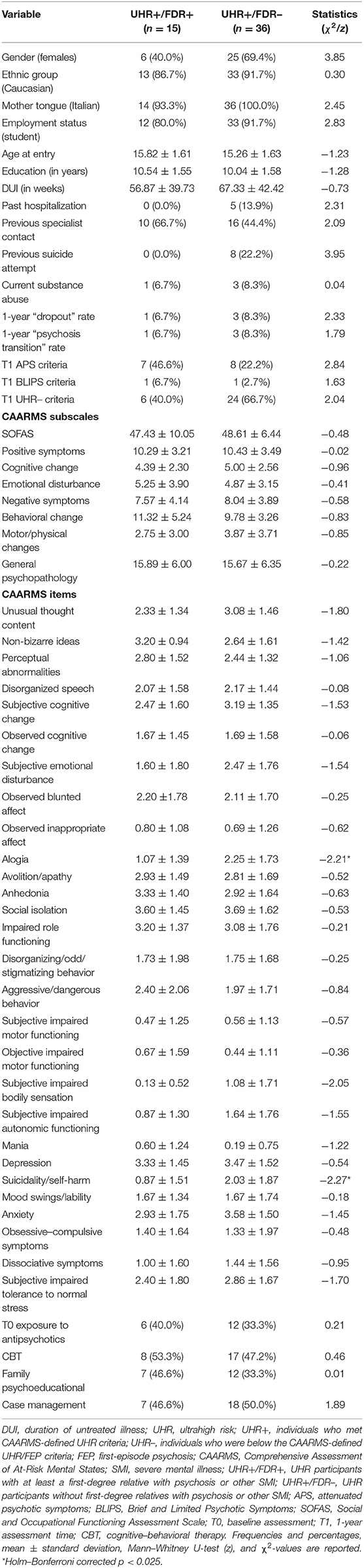
Table 3. Sociodemographic, psychopathological, and clinical characteristics between UHR+ participants with and without first-degree relatives with psychosis or other SMI.
GRFD Syndrome in UHR+ Individuals: Clinical Profile
Among 51 UHR+ participants, 18 (35.2% of the UHR+ total group) met the CAARMS-defined GRFD criteria (i.e., UHR+/GRFD+); of them, 17 individuals (94.4% of the total GRFD subgroup) showed a co-occurrence of GRFD syndrome with APS or BLIPS criteria.
Compared to UHR+ subjects not meeting the GRFD criteria (i.e., UHR+/GRFD–), UHR+/GRFD+ individuals showed a significantly higher CAARMS “positive symptoms” and “emotional disturbance” subscale scores, as well as higher “non-bizarre ideas” and “observed inappropriate affect” item subscores (Table 4). No other intergroup differences in terms of baseline functioning and sociodemographic, clinical, and psychopathological characteristics were observed. Similarly, no between-group differences were found in terms of frequency of specific ReARMS interventions provided to the UHR+ participants.
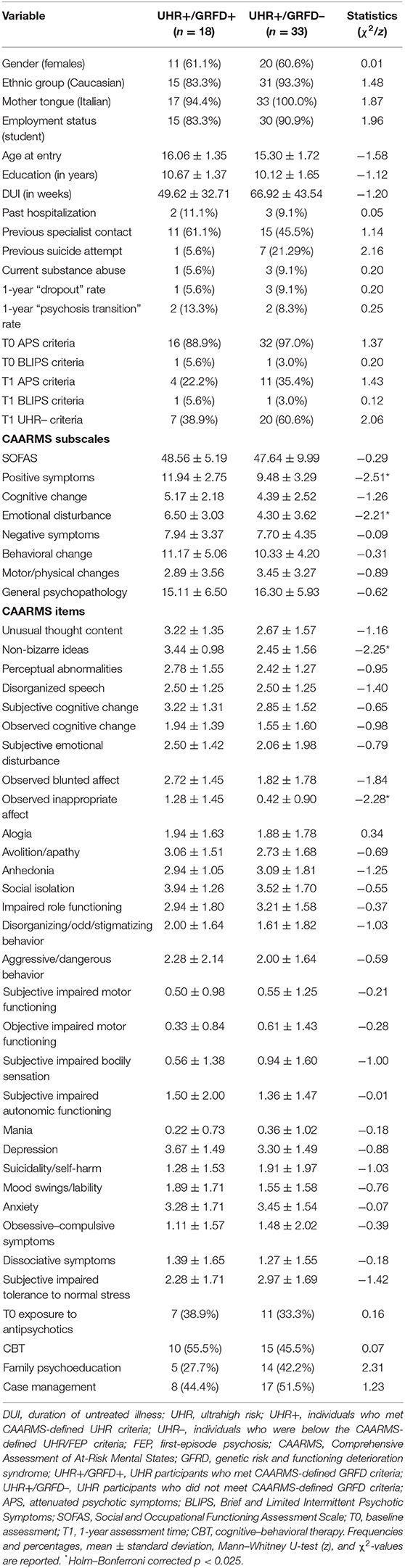
Table 4. Sociodemographic, psychopathological, and clinical characteristics between UHR+ participants meeting or not meeting CAARMS-defined GRFD criteria.
Discussion
The first aim of the present research was to examine the prevalence of SMI in family members of distinct help-seeking subsamples of adolescents identified through the UHR criteria (i.e., UHR+ vs. FEP vs. UHR–). Although no statistically significant intergroup-differences were found in terms of family load for SMI, more than 60% of our UHR+ and FEP adolescents showed a general family history of SMI, and approximately a third of them (with percentages ranging from 29.4% in UHR+ subjects to 42.2% in FEP patients) had at least a first-degree relative with psychosis or other SMI. As expected, these findings confirm the epidemiological burden of a family history of SMI in the prodromal phase of psychosis and at the onset of illness, already in adolescence, consistently with the very few results reported in the current literature (15, 36–38).
However, our UHR+ adolescents with a family history of SMI (specifically those with a first-degree relative with psychosis or other SMI) showed lower levels of alogia, self-harm, and suicidality (i.e., suicidal thoughts and behaviors). These results seem to suggest that the experience of a family psychiatric suffering and the custom of living with people with an SMI could increase the personal ability to find words to express a request for specialist help and to describe their symptoms, as well as to support their hope and future projects. Moreover, this also confirms the absolute need for clinical attention for children and adolescents with family members with SMI (39) and the crucial importance of psychotherapeutic and psychoeducational interventions to support their coping skills, their resilience, and their quality of life (40).
In the present research, a GRFD syndrome was detected in ~35% of UHR+ adolescents, mostly (i.e., almost in 95% of cases) in co-occurrence with APS or BLIPS criteria. This result is slightly higher than that reported in the current literature (6, 41) and confirms the very low incidence of a GRFD syndrome alone in adolescent help-seeking populations attending specialist mental health services offering dedicated EIP programs (2, 7). Hence, there is a specific need to diffusely spread the early identification of psychosis in all the community services (e.g., school and social agencies, general practitioners, general hospital, emergency room), going beyond the boundaries of mental health centers and emphasizing the crucial attention to be paid to children and adolescent with a family history of SMI (40, 41) or with schizotypal personality traits (42, 43), together with a socio-occupational functioning decline. From a psychopathological point of view, in the present study, GRFD adolescents showed baseline high levels of positive symptoms (especially, non-bizarre ideas) and emotional disturbances (specifically, observed inappropriate affect). These specific clinical features may be useful for an early characterization of adolescents with a genetic risk of psychosis and an incipient functioning deterioration, also in developing specific screening test.
Limitations
A first methodological limitation of the current research is the relatively small sample size. Therefore, further studies on larger populations of both UHR and FEP adolescents are needed.
Second, our sample was recruited within a specific EIP program. Thus, our results cannot be generalized outside UHR/FEP-enriched populations.
Third, future studies to better specify and deepen the clinical profile of UHR adolescents (e.g., non-bizarre ideas or emotional disturbances) meeting GRFD criteria are also recommended.
Conclusions
This is the first Italian study specifically developed to investigate the prevalence of SMI and in family members of adolescent help-seekers recruited within a specific EIP program, as well as the presence of a GRFD syndrome in Italian youths with early psychosis. Our results confirm the importance of family load and genetic risk factors in young people at UHR of psychosis (as well as in FEP adolescents), suggesting the need of their early detection, already within the network of general practitioners, general hospitals, and the other community agencies (e.g., social services and school). Moreover, this clinical attention becomes even more crucial because adolescents receiving treatment in CAMHS are at elevated risk of falling through the child-adult service gap as they cross the transition boundary between services (i.e., from child–adolescent mental health services to adult mental health services) (1). Bridging this gap might be achievable through a framework shift that incorporates the full continuum of service response within a prevention and promotion framework for youth mental health (44).
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by AVEN (Area Vasta Emilia Nord) Ethics Committee (protocol 36102/2019). Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
LP and AR designed the study and conducted the main data analysis. SA, FP, SG, IS, and LC collected data. LP and SP managed the literature. MP, LP, and AR drafted the manuscript. All authors read and approved the final version of the manuscript.
Funding
ReARMS program is partly financed through a special, treatment-oriented, regional fund: Progetto Esordi Psicotici della Regione Emilia Romagna.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The ReARMS technical-scientific multi-professional steering committee was established in 2012 and included in alphabetical order: SA (psychologist), Cioncolini Leonardo (head nurse), LC (psychologist), Fabiani Michela (child-adolescent psychiatrist), Favazzo Rosanna (psychiatrist), Fontana Francesca (psychiatrist), SG (psychologist), FP (psychologist), LP (psychiatrist), Pensieri Luana (child-adolescent psychologist), AR (psychiatrist), IS (psychologist), and Semrov Enrico (senior psychiatrist). We wish to thank all the patients and family members who actively participated to the ReARMS program. We also gratefully acknowledge the facilitating support of Dr. Enrico Semrov and all the other colleagues of the Reggio Emilia Department of Mental Health and Pathological Addiction for their technical and administrative support. Further to that, we wish to thank Dr. Eva Gebhardt who acted as external advisor insuring wide-spread educational training and clinical-supervision support.
References
1. Pelizza L, Azzali S, Paterlini F, Garlassi S, Scazza I, Chiri LR, et al. The “Reggio Emilia At-Risk Mental States” program: a diffused liquid model of early intervention in psychosis implemented in an Italian Department of Mental Health. Early Interv Psychiatry. (2019) 13:1513–24. doi: 10.1111/eip.12851
2. Pelizza L, Azzali S, Paterlini F, Garlassi S, Scazza I, Chiri LR, et al. Characterization of young people with first episode psychosis or at ultra-high risk: the Reggio Emilia at-risk mental states (ReARMS) program. Riv Psichiatr. (2019) 54:254–63. doi: 10.1708/3281.32544
3. McGorry PD, Mei C. Early intervention in youth mental health: progress and future directions. Evid Based Ment Health. (2018) 21:182–4. doi: 10.1136/ebmental-2018-300060
4. McGorry PD, Mei C. Ultra-high-risk paradigm: lessons learnt and new directions. Evid Based Ment Health. (2018) 21:131–3. doi: 10.1136/ebmental-2018-300061
5. Fiorillo A. The complexity of vulnerability to psychosis. Epidemiol Psychiatr Sci. (2019) 28:138–9. doi: 10.1017/S2045796018000690
6. Fusar-Poli P, Tantardini M, De Simone S, Ramella-Cravaro V, Oliver D, Kingdon J, et al. Deconstructing vulnerability for psychosis: meta-analysis of environmental risk factors for psychosis in subjects at ultra-high risk. Eur Psychiatry. (2017) 40:65–75. doi: 10.1016/j.eurpsy.2016.09.003
7. Radua J, Ramella-Cravaro V, Ioannidis JP, Reichenberg A, Phiphopthatsanee N, Amir T, et al. What causes psychosis? An umbrella review of risk and protective factors. World Psychiatry. (2018) 17:49–66. doi: 10.1002/wps.20490
8. Pelizza L, Raballo A, Semrov E, Chiri LR, Azzali S, Scazza I, et al. Validation of the “early detection Primary Care Checklist” in an Italian community help-seeking sample: the “checklist per la Valutazione dell'Esordio Psicotico”. Early Interv Psychiatry. (2019) 13:86–94. doi: 10.1111/eip.12455
9. Malla A, Shah J, Lal S. Advances and challenges in early intervention in psychosis. World Psychiatry. (2017) 16:274–5. doi: 10.1002/wps.20453
10. Pelizza L, Azzali S, Paterlini F, Scazza I, Garlassi S, Chiri LR, et al. The Italian version of the brief 21-item Prodromal Questionnaire: field test, psychometric properties and age-sensitive cut-offs. Psychopathology. (2018) 51:234–44. doi: 10.1159/000490708
11. Yung AR, Yuen HP, McGorry PD, Phillips LJ, Kelly D, Dell'Olio M, et al. Mapping the onset of psychosis: the comprehensive assessment of at-risk mental states. Aust N Z J Psychiatry. (2005) 39:964–71. doi: 10.1080/j.1440-1614.2005.01714.x
12. Yuen HP, Mackinnon A, Hartmann J, Amminger GP, Markulev C, Lavoie S, et al. Dynamic prediction of transition to psychosis using joint modelling. Schizophr Res. (2018) 202:333–40. doi: 10.1016/j.schres.2018.07.002
13. Kotlicka-Antczak M, Karbownik MS, Stawiski K, Pawełczyk A, Zurner N, Pawelczyk T, et al. Short clinically-based prediction model to forecast transition to psychosis in individuals at clinical high risk state. Eur Psychiatry. (2019) 58:72–9. doi: 10.1016/j.eurpsy.2019.02.007
14. Malda A, Boonstra N, Barf H, de Jong S, Aleman A, Addington J, et al. Individualized prediction of transition to psychosis in 1,676 individuals at clinical high risk: development and validation of a multivariable prediction model based on individual patient data meta-analysis. Front Psychiatry. (2019) 10:345. doi: 10.3389/fpsyt.2019.00345
15. Madsen HK, Nordholm D, Krakauer K, Randers L, Nordentoft M. Psychopathology and social functioning of 42 subjects from a Danish ultra-high risk cohort. Early Interv Psychiatry. (2018) 12:1181–7. doi: 10.1111/eip.12438
16. Pelizza L, Ficarelli ML, Vignali E, Artoni S, Franzini MC, Montanaro S, et al. Individual placement and support in Italian young adults with mental disorder: findings from the Reggio Emilia experience. Early Interv Psychiatry. (2019) 14:577–86. doi: 10.1111/eip.12883
17. Ran MS, Xiao Y, Chui CHK, Hu XZ, Yu YH, Peng MM, et al. Duration of untreated psychosis (DUP) and outcome of people with schizophrenia in rural China: 14-year follow-up study. Psychiatry Res. (2018) 267:340–5. doi: 10.1016/j.psychres.2018.06.043
18. Penttila M, Jaaskelainen E, Hirvonen N, Isohanni M, Miettunen J. Duration of untreated psychosis as predictor of long-term outcome in schizophrenia: systematic review and meta-analysis. Br J Psychiatry. (2014) 205:88–94. doi: 10.1192/bjp.bp.113.127753
19. Pelizza L, Azzali S, Garlassi S, Paterlini F, Scazza I, Chiri LR, et al. Adolescents at ultra-high risk of psychosis in Italian neuropsychiatry services: prevalence, psychopathology and transition rate. Eur Child Adolesc Psychiatry. (2018) 27:725–37. doi: 10.1007/s00787-017-1070-3
20. Raballo A, Chiri LR, Pelizza L, Fontana F, Favazzo R, Pensieri L, et al. Field-testing the early intervention paradigm in Emilia-Romagna: the Reggio Emilia at risk mental state (ReARMS) project. Early Interv Psychiatry. (2014) 8:88.
21. Jablensky A, Sartorius N, Ernberg G, Anker M, Korten A, Cooper JE, et al. Schizophrenia: manifestations, incidence and course in different cultures, a World Health Organization ten-country study. Psychol Med Monogr Suppl. (1992) 20:1–97. doi: 10.1017/S0264180100000904
22. American Psychiatric Association (APA). Diagnostic and Statistical Manual of Mental Disorders, IV Edition, Text Revised (DSM-IV-TR). Washington, DC: American Psychiatric Association Publishing (2000).
23. Rapp C, Canela C, Studerus E, Walter A, Aston J, Borgwardt S, et al. Duration of untreated psychosis/illness and brain volume changes in early psychosis. Psychiatry Res. (2017) 255:332–7. doi: 10.1016/j.psychres.2017.06.004
24. Silverman MM, Berman AL, Sanddal ND, O'Carroll PW, Joiner TE. Rebuilding the Tower of Babel: a revised nomenclature for the study of suicide and suicidal behaviors—Part 2: suicide-related ideations, communications, and behaviors. Suicide LifeThreat Behav. (2007) 37:264–77. doi: 10.1521/suli.2007.37.3.264
25. Pelizza L, Poletti M, Azzali S, Paterlini F, Garlassi S, Scazza I, et al. Suicidal thinking and behavior in adolescents at Ultra-high-risk of psychosis: a two-year longitudinal study. Suicide Life-Threat Behav. (2019) 49:1637–52. doi: 10.1111/sltb.12549
26. Pelizza L, Paterlini F, Azzali S, Garlassi S, Scazza I, Pupo S, et al. The approved Italian version of the comprehensive assessment of at-risk mental states (CAARMS-ITA): field test and psychometric features. Early Interv Psychiatry. (2019) 13:810–7. doi: 10.1111/eip.12669
27. Raballo A, Semrov E, Bonner Y, Simmons M. Traduzione e adattamento italiano della CAARMS (the Comprehensive Assessment of At-Risk Mental States). Bologna: Centro Stampa della Regione Emilia-Romagna (2013).
28. Paterlini F, Pelizza L, Galli G, Azzali S, Scazza I, Garlassi S, et al. Interrater reliability of the authorized Italian version of the comprehensive assessment of at-risk mental states (CAARMS-ITA). J Psychopathol. (2019) 25:24–8. Available online at: https://www.jpsychopathol.it/article/interrater-reliability-of-the-authorized-italian-version-of-the-comprehensive-assessment-of-at-risk-mental-states-caarms-ita/
29. First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders (SCID-I). New York, NY: New York State Psychiatric Institute (2002).
30. Fulone I, Barreto JOM, Barberato-Filho S, de Carvalho MH, Lopes LC. Knowledge translation for improving the care of deinstitutionalized people with severe mental illness in health policy. Front Pharmacol. (2020) 10:1470. doi: 10.3389/fphar.2019.01470
31. National Institute for Health and Care Excellence (NICE). Psychosis and Schizophrenia in Children and Young People: Recognition and Management. Leicester: British Psychological Society (2013).
32. Schmidt SJ, Schultze-Lutter F, Schimmelmann BG, Maric NP, Salokangas RK, Riecher-Rössler A, et al. EPA guidance on the early intervention in clinical high risk states of psychoses. Eur Psychiatry. (2015) 30:388–404. doi: 10.1016/j.eurpsy.2015.01.013
33. Regione Emilia Romagna (RER). Raccomandazioni regionali per la promozione della salute e del benessere in persone all'esordio psicotico. Bologna: Centro stampa della Regione Emilia Romagna (2016).
34. SPSS Inc. Statistical Package for Social Science (SPSS) for Windows, version 15.0. Chicago, IL: SPSS Inc. Press (2010).
36. Cocchi A, Balbi A, Corlito G, Ditta G, Di Munzio W, Nicotera M, et al. Early intervention in psychosis: a feasibility study financed by the Italian Center on Control of Maladies. Early Interv Psychiatry. (2015) 9:163–71. doi: 10.1111/eip.12135
37. Pakyurek M, Yarnal R, Carter C. Treatment of psychosis in children and adolescents: a review. Adolesc Med State Art Rev. (2013) 24:420–32.
38. Yung AR, Phillips LJ, Yuen HP, McGorry PD. Risk factors for psychosis in an ultra-high risk group: psychopathology and clinical features. Schizophr Res. (2004) 67:131–42. doi: 10.1016/S0920-9964(03)00192-0
39. Thorup AAE, Laursen TM, Munk-Olsen T, Ranning A, Mortensen PB, Plessen KJ, et al. Incidence of child and adolescent mental disorders in children aged 0-17 with familial high risk for severe mental illness: a Danish register study. Schizophr Res. (2018) 197:298–304. doi: 10.1016/j.schres.2017.11.009
40. Müller AD, Gjøde ICT, Eigil MS, Busck H, Bonne M, Nordentoft M, et al. VIA Family: a family-based early intervention versus treatment as usual for familial high-risk children: a study protocol for a randomized clinical trial. Trials. (2019) 20:112. doi: 10.1186/s13063-019-3191-0
41. Cannon TD, Cadenhead K, Cornblatt B, Woods SW, Addington J, Walker E, et al. Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Arch Gen Psychiatry. (2008) 65:28–37. doi: 10.1001/archgenpsychiatry.2007.3
42. Poletti M, Pelizza L, Azzali S, Paterlini F, Garlassi S, Scazza I, et al. Clinical high risk for psychosis in childhood and adolescence: findings from the 2-year follow-up of the ReARMS project. Eur Child Adolesc Psychiatry. (2019) 28:957–71. doi: 10.1007/s00787-018-1262-5
43. Pelizza L, Poletti M, Azzali S, Paterlini F, Garlassi S, Scazza I, et al. Anhedonia in adolescents at ultra-high risk (UHR) of psychosis: findings from a 1-year longitudinal study. Eur Arch Psychiatry Clin Neurosci. (2020) 270:337–50. doi: 10.1080/08039488.2020.1799430
Keywords: vulnerability, familiarity, early psychosis, early intervention, early detection, ultra-high risk (UHR) of psychosis, clinical high risk (CHR), adolescence
Citation: Poletti M, Azzali S, Paterlini F, Garlassi S, Scazza I, Chiri LR, Pupo S, Raballo A and Pelizza L (2021) Familiarity for Serious Mental Illness in Help-Seeking Adolescents at Clinical High Risk of Psychosis. Front. Psychiatry 11:552282. doi: 10.3389/fpsyt.2020.552282
Received: 15 April 2020; Accepted: 27 November 2020;
Published: 08 January 2021.
Edited by:
Maude Schneider, Université de Genève, SwitzerlandReviewed by:
Sebastien Urben, Centre Hospitalier Universitaire Vaudois (CHUV), SwitzerlandMaria Pontillo, Bambino Gesù Children Hospital (IRCCS), Italy
Copyright © 2021 Poletti, Azzali, Paterlini, Garlassi, Scazza, Chiri, Pupo, Raballo and Pelizza. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Michele Poletti, bWljaGVsZXBvbGV0dGkyQGF1c2wucmUuaXQ=
 Michele Poletti
Michele Poletti Silvia Azzali1
Silvia Azzali1 Andrea Raballo
Andrea Raballo Lorenzo Pelizza
Lorenzo Pelizza