- 1Chair of Psychiatry, Department of Systems Medicine, University of Rome Tor Vergata, Rome, Italy
- 2Department of Biotechnological and Applied Clinical Sciences, University of L’Aquila, L’Aquila, Italy
- 3Department of Anesthesiology, Intensive Care and Emergency Medicine, Fondazione Policlinico Universitario A. Gemelli IRCCS, Rome, Italy
- 4Psychiatry and Clinical Psychology Unit, Fondazione Policlinico Tor Vergata, Rome, Italy
- 5Department of Information Engineering, Computer Science and Mathematics, University of L’Aquila, L’Aquila, Italy
- 6IRCCS Fondazione Santa Lucia, Rome, Italy
Background: The psychological impact of the COronaVIrus Disease 2019 (COVID-19) outbreak and lockdown measures on the Italian population are unknown. The current study assesses rates of mental health outcomes in the Italian general population three to 4 weeks into lockdown measures and explores the impact of COVID-19 related potential risk factors.
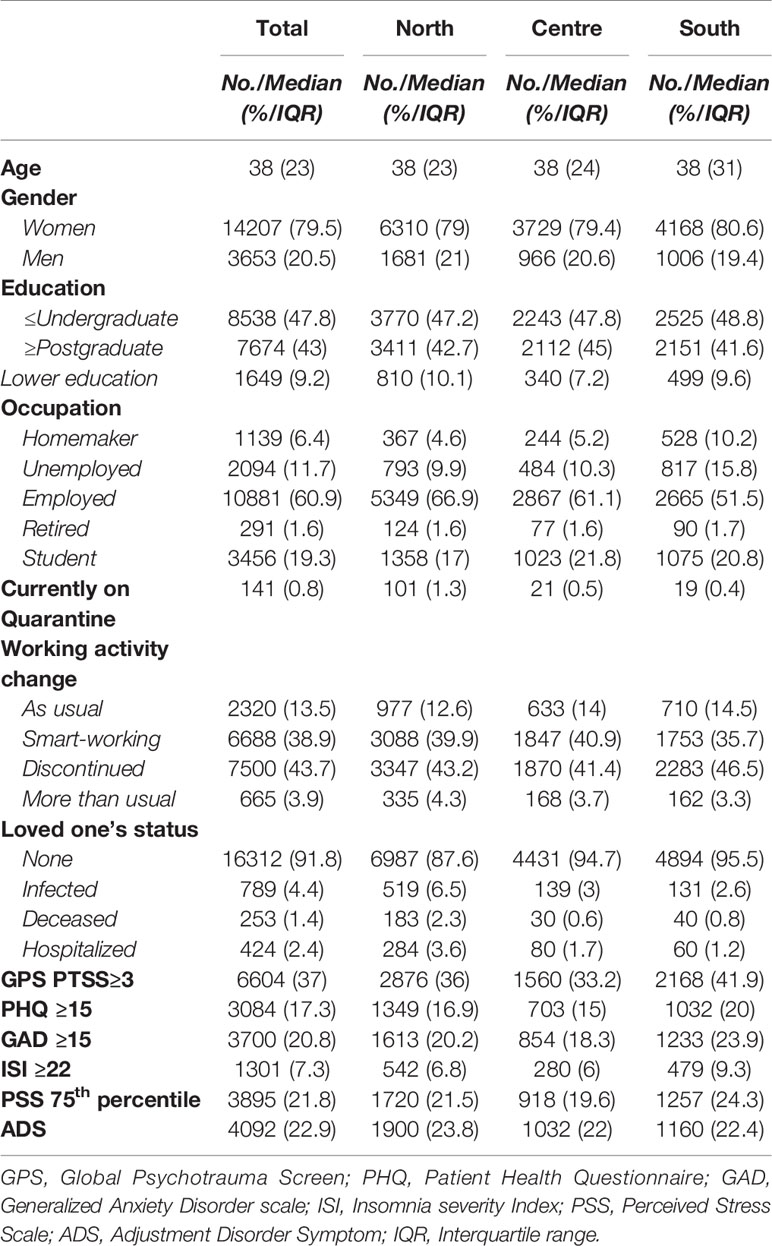
Methods: A web-based survey spread throughout the internet between March 27th and April 6th 2020. Eighteen thousand one hundred forty-seven individuals completed the questionnaire, 79.6% women. Selected outcomes were post-traumatic stress symptoms (PTSS), depression, anxiety, insomnia, perceived stress, and adjustment disorder symptoms (ADS). Seemingly unrelated logistic regression analysis was performed to identify COVID-19 related risk factors.
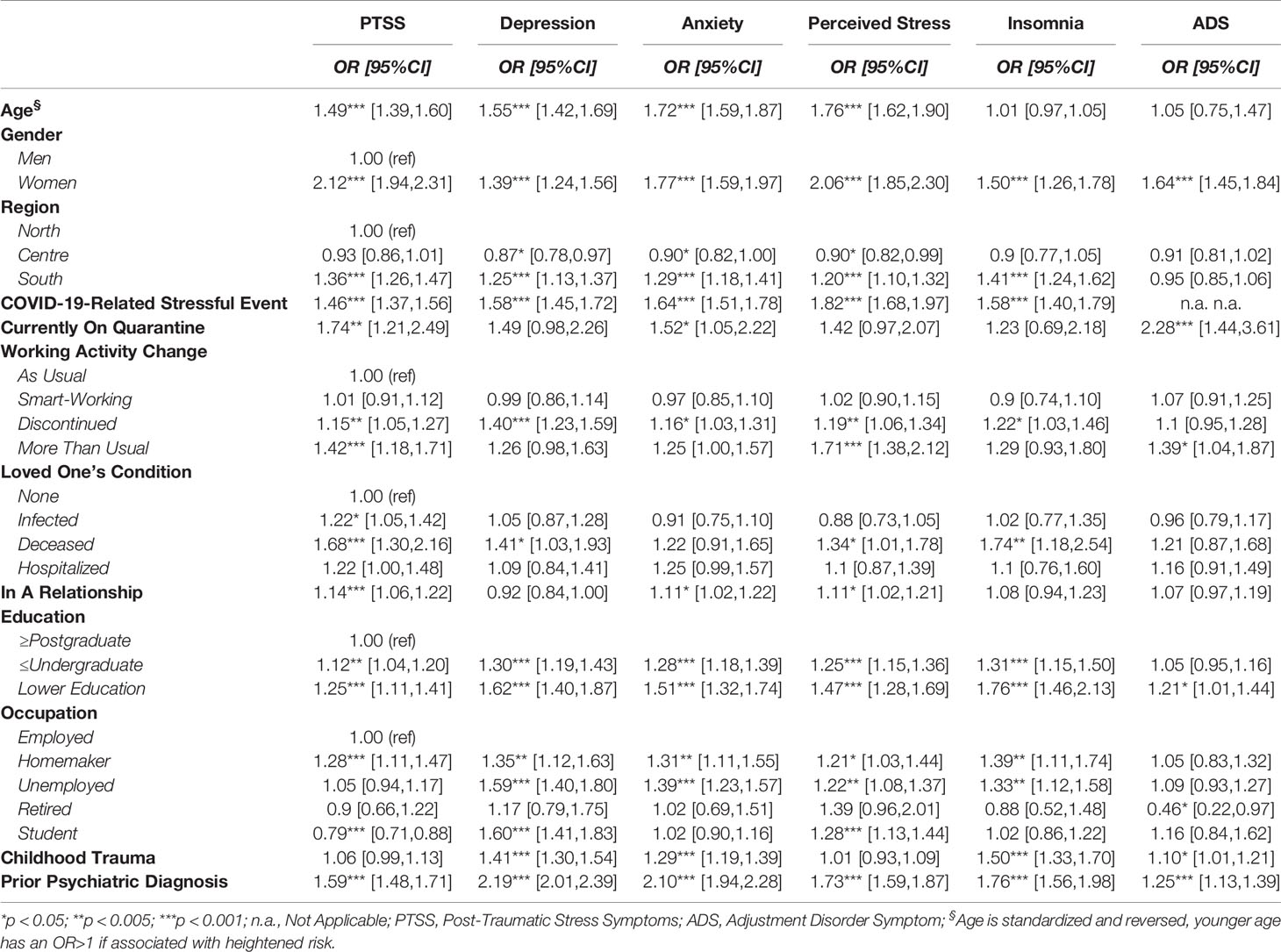
Results: Endorsement rates for PTSS were 6,604 (37%), 3,084 (17.3%) for depression, 3,700 (20.8%) for anxiety, 1,301 (7.3%) for insomnia, 3,895 (21.8%) for high perceived stress and 4,092 (22.9%) for adjustment disorder. Being woman and younger age were associated with all of the selected outcomes. Quarantine was associated with PTSS, anxiety and ADS. Any recent COVID-related stressful life event was associated with all the selected outcomes. Discontinued working activity due to the COVID-19 was associated with all the selected outcomes, except for ADS; working more than usual was associated with PTSS, Perceived stress and ADS. Having a loved one deceased by COVID-19 was associated with PTSS, depression, perceived stress, and insomnia.
Conclusion: We found high rates of negative mental health outcomes in the Italian general population 3 weeks into the COVID-19 lockdown measures and different COVID-19 related risk factors. These findings warrant further monitoring on the Italian population’s mental health.
Background
The psychological impact of the COronaVIrus Disease 2019 (COVID-19) outbreak and related lockdown measures among the Italian population are unknown. The COVID-19 pandemic is a global health emergency that could potentially have a serious impact on public health, including mental health (1, 2). Since clusters of atypical pneumonia of unknown aetiology were discovered in the city of Wuhan, Hubei province, in late December 2019, the viral disease has continued to exponentially spread throughout China and worldwide. Italy has been the first European country that had to face the pandemic. On March 9th 2020, lockdown measures were enforced by the government on entire national territory. Lockdown measures included travel restrictions, the mandatory closure of schools, nonessential commercial activities and industries. People were asked to stay at home and socially isolate themselves to prevent being infected.
As previously reported, health emergencies such as epidemics can lead to detrimental and long-lasting psychosocial consequences, due to disease related fear and anxiety, large-scale social isolation, and the overabundance of (mis)information on social media and elsewhere (3). At the individual level, epidemics are associated with a wide range of psychiatric comorbidities including anxiety, panic, depression, and trauma-related disorders (4). The psychosocial impact of health emergences seems to be even higher during quarantine measures (5). Quarantine has been associated with high stress levels (6), depression (7), irritability and insomnia (8). Furthermore, being quarantined is associated with acute stress (9) and trauma-related (10) disorders, particularly in specific at-risk populations such as health workers (11).
Concerning the COVID-19 pandemic, a study on 1210 respondents in China found rates of 30% of anxiety and 17% of depression (12). Further, in a nationwide survey including more than 50,000 Chinese respondents, almost 35% of the participants reported trauma-related distress symptoms, with women and young adults showing significantly higher psychological distress (13).
Together, these findings strongly suggest the need to accurately and timely assess the magnitude of mental health outcomes in the general population exposed to COVID-19 pandemic, with particular regard to the implementation of preventive and early interventions strategies for those at higher risk. However, no study to date has investigated mental health outcomes and associated risk factors in the Italian population. This could be of additional relevance considering the implementation of the strict lockdown and social distancing measures imposed on the entire national territory.
The aim of the current study was to assess rates of mental health outcomes in the Italian general population three to 4 weeks into lockdown measures and to explore the impact of COVID-19 related potential risk factors. This study aims at providing evidence that could potentially inform subsequent research strategies and mental health delivery in Italy and Europe. Our hypothesis is that specific COVID-19 related risk factors could show a relevant association with mental health in the general population.
Methods
Study Design
A cross-sectional web-based survey design was adopted. Approval for this study was obtained from the local IRB at University of L’Aquila. On-line consent was obtained from the participants. Participants were allowed to terminate the survey at any time they desired. The survey was anonymous, and confidentiality of information was assured.
Data on mental health were collected between March 27th and April 6th 2020 using an on-line questionnaire spread throughout the internet, using sponsored social network advertisement together with a snowball recruiting technique. Questionnaires were evenly distributed across the national territory. The investigated timeframe corresponds to the contagion peak in Italy, according to epidemiological data confirmed by the World Health Organization (1). The survey was developed using the free software Google Forms®.
Participants
All Italian citizens ≥ 18 years were eligible. A total of 18,147 individuals completed the questionnaire, of which 14,447 (79.6%) women, median age was 38 (IQR=23). Because of the web-based design, no response rate could be estimated as it was not possible to estimate how many persons were reached by social network advertisement.
Mental Health Outcomes
Post-Traumatic Stress Symptoms (PTSS), depression symptoms, anxiety symptoms, insomnia, perceived stress and adjustment disorder symptoms (ADS) were assessed using the Italian versions of the following instruments and cut-offs or scoring:
● The Global Psychotrauma Screen, post-traumatic stress symptoms subscale (GPS-PTSS) (14): PTSS were considered of clinical relevance if more than three out of five symptoms were reported as present. In our sample, internal consistency was α=0.54.
● the 9-item Patient Health Questionnaire (PHQ-9) (15), using the cut-off for severe depression symptoms at ≥15. In our sample, internal consistency was α=0.87
● the 7-item Generalized Anxiety Disorder scale (GAD-7) (16), using the cut-off for severe anxiety symptoms at ≥15. In our sample, internal consistency was α=0.91
● the 7-item Insomnia Severity Index (ISI) (17), using the cut-off at ≥22 for severe insomnia. In our sample, internal consistency was α=0.90
● the 10-item Perceived Stress Scale (PSS) (18), using a quartile split to separate the higher quartile from the remaining participants. In our sample, internal consistency was α=0.87
● the International Adjustment Disorder Questionnaire (IADQ) (19), using the standard scoring system. IADQ comprises a brief checklist of potentially stressful events, such as financial, work, health or housing problems. The IADQ checklist was modified in order to ascertain if the reported problem was due to COVID-19. ADS were rated as present if a stressful life event correlated to COVID-19 was present, together with preoccupation and failure to adapt symptoms and a relevant impact on global functioning. In our sample, internal consistency was α=0.90
Independent Variables
Standardized age, gender, and region of residence (Northern Italy: Aosta Valley, Piedmont, Liguria, Lombardy, Trentino-Alto Adige, Veneto, Friuli-Venezia Giulia, Emilia-Romagna; Central Italy: Tuscany, Umbria, Marche, Lazio; Southern Italy: Abruzzo, Molise, Apulia, Campania, Basilicata, Calabria, Sicily, and Sardinia) were inserted as independent variables. Region of residence was inserted in order to account for the different incidence of COVID-19 among Italian regions. COVID-19 related independent variables were:
● being under quarantine either because infected or in close proximity to infected people;
● any changes in working activity compared to “working as usual” (e.g., smart-working, working activity discontinued due to lockdown measures, higher workload due to COVID-19);
● having a loved one infected, hospitalized or deceased due to COVID-19;
● any stressful events comprised in the IDAQ checklist, purposely modified in order to capture only stressful events due to COVID-19. The IADQ checklist comprises eight questions about any potential stressful life event occurred in the recent past, with a yes/no response, including financial, working, educational, housing, relationship, own or loved one’s health and caregiving problems. In order to separate COVID-19 related stressful life events from non-COVID-19 related events, responses to the checklist were modified as follows: “no”; “yes”; “yes, due to COVID-19”. Responses were collapsed in a binary variable where 1=“any stressful life evet only if due to COVID-19” and 0=“no stressful life events or presence of a stressful life event not due to COVID-19”.
Confounders
A history of childhood trauma and any previous mental illness, as assessed by the dedicated GPS module; education level, occupation (employed, unemployed, student, retired) and being in a relationship.
Statistical Analysis
Frequency analysis were performed in order to ascertain the prevalence of each outcome, separately for Northern, Central, and Southern Italy.
A seemingly-unrelated multivariate logistic regression model was fitted in order to explore the impact of the proposed covariates and confounders on the selected outcomes. Seemingly unrelated regression models are systems of equations that allow to jointly model several outcomes, assuming correlation among their errors. Because of the very low missing data rates (<3%), missing data were treated with listwise deletion in regression analysis.
Data analysis was performed using Stata v. 16® (StataCorp). Seemingly unrelated logistic regression was performed using the -suest- postestimation command after running a panel of logistic regressions.
Results
Socio-demographic characteristics of the sample, along with rates of mental health outcomes, are reported in Table 1. Of the 18,147 respondents, 6,666 (37.14%) reported ≥3/5 PTSS, with a median total GPS symptom score of 7 (IQR=6, range 0‑17); 3,099 respondents (17.3%) reported severe depressive symptoms, with a PHQ total median score of 8 (IQR=6, range 0‑17); 3,732 (20.8%) respondents reported severe anxiety symptoms, with GAD median score of 8 (range 0‑21, IQR=10); 1,306 (7.3%) respondents reported severe insomnia symptoms, with ISI median total score of 10 (range 0‑28, IQR=12); PSS total score median was 25 (range 4‑44, IQR=13), 75th percentile was 31, with 3,933 (21.9%) respondents scoring above this threshold; 4,129 (23.0%) respondents reported a IADQ scoring compatible with the suspect of a presence of an adjustment disorder.
Seemingly unrelated logistic regression analyses are reported in Table 2. Being a woman was associated with all of the selected outcomes. Younger age was associated with PTSS, depression symptoms, anxiety symptoms, and perceived stress. Compared to Northern Italy, participants from Southern Italy showed higher odds of all of the selected outcomes, except for ADS. Being under quarantine because infected or in close proximity to infected people was associated with PTSS, Anxiety and ADS. Having experienced a stressful life event due to COVID-19, as assessed by the modified IADQ checklist, was associated with all of the selected outcomes. OR of IADQ-Checklist on ADS was not estimated due to the perfect prediction, because having an IADQ checklist event is a prerequisite for having a suspected Adjustment Disorder. Working activity discontinued due to COVID-19 was associated with all of the selected outcomes except for ADS, while working more than usual due to the COVID-19 was associated with PTSS, perceived stress and ADS. Having a loved one deceased by COVID-19 was associated with PTSS, while having a loved one diagnosed with COVID-19 was associated with PTSS.
Discussion
In this study, we report for the first time on the mental health outcomes related to COVID-19 outbreak and related lockdown measures on the general population in Italy. To the best of our knowledge, this is the first study to report on mental health outcomes related to the COVID-19 outbreak in Europe on such a large sample size. This study shows relatively high rates of PTSS, Depression symptoms, Anxiety symptoms, Insomnia, Perceived stress and ADS, with young women having higher odds of endorsing a mental health outcome. These outcomes were associated with a number of COVID-19-related risk factors, including being under quarantine, having a loved one deceased by COVID-19, working activity discontinued due to lockdown measures, or experiencing other stressful events (i.e. working, financial, relationship, or housing problems) due to the pandemic or lockdown measures. These findings were adjusted for previous psychiatric illness and a history of childhood trauma, suggesting that the COVID-19 pandemic is exerting an independent effect on the population mental health.
Previous Literature
Compared to previous reports on common mental disorders in the Italian population, our data suggest in increase in rates of common mental disorders such as depression symptoms and anxiety symptoms (20). However, this comparison should be taken with caution, because of the inherently different assessment methods used (interview vs. self-report) and sampling strategy. Furthermore, our study uses screening tools that may only suggest the presence of a mental disorders. To the best of our knowledge, no large epidemiological study has ever been conducted in Italy on stress-related disorders, so no comparison with pre-covid evidence can be proposed.
Compared to an early report on the mental health outcomes related to COVID-19 in China on 1210 respondents (12), we found lower rates of anxiety, similar rates of depression and higher levels of perceived stress, notwithstanding differences in assessment tools. The negative association with age and the positive association with female gender were confirmed, suggesting that young women may be at heightened risk for mental disorders. Compared to another large web-based survey from China on 52,730 respondents that evaluated peritraumatic stress-related symptoms, we found similar rates of PTSS (13). Another study on 285 participants from hardest-hit Hubei province found substantially lower rates of PTSS, around 7% (21). Such disparities could be due to different assessment tools used and differences in sample size. A study on 7,143 medical students in China (22) found severe anxiety rates, assessed as GAD≥15, to be 0.9%, compared to our 20.9%. This inconsistence could be due to the particular population investigated, having a high education level. Indeed, higher education was associated with better outcomes in our study. Furthermore, cultural, social, and health care system differences between China and Italy could explain differences in reported mental health outcomes.
Coherently with previous reports from China, female gender (12, 13, 21) and younger age (12, 13) were consistently associated with higher risk for different mental health outcomes. If confirmed in other populations worldwide, these findings could be of great importance for subsequent intervention strategy for global mental health related to COVID-19.
Relevance
Monitoring populations’ mental health is critical during a pandemic, as generalized fear and fear-induced over-reactive behaviour among the public could impede infection control (3). Further, the current strict lockdown measures and the home confinement of unknown duration represent an unprecedented stressful event potentially leading to significant long-term health costs. Epidemiological monitoring and targeted intervention should be therefore timely implemented to prevent further mental health problems. Indeed, once the outbreak will be over, its negative socio-economic consequences may have a detrimental effect on the population’s mental health, as suggested by our finding of an heightened risk of mental health issues due to COVID-19 related working difficulties and by earlier studies related to the last economic crisis (23).
Limitations and Future Directions
This study has some important limitations due to the sampling technique. Relying on social networks voluntary recruitment and re-sharing could have introduced an important selection bias, firstly excluding people not on social networks, and secondly introducing a self-selection bias, as suggested by the highly unbalanced gender ratio observed. This latter bias could have affected also two other large web-based surveys in China, that reported on samples with a 64.7% and 67.3% proportion of woman (12, 13). For these reasons, rates of mental health outcomes should be interpreted with caution. Secondly, this survey was based on self-report instruments that could introduce a systematic bias and return different rates compared to interview-based measures.
This study has also several strengths, including a very large sample size and the sampling timeframe that corresponded to the pandemic peak in Italy.
Future studies will need to monitor the trajectory of mental health outcomes, in order to define mental health interventions at a population level.
Moreover, these results suggests that appropriate mental health care delivery should be at the centre of future re-organization healthcare management, anticipating the needs, planning, and delivering much needed mental health protection of the whole community as well as in special populations (i.e. healthcare workers, adolescents, older age).
Conclusions
We found high rates of negative mental health outcomes in the Italian general population three to 4 weeks into the COVID-19 pandemic and lockdown measures. COVID-19 related factors were associated with these outcomes independently from previous mental illness or childhood trauma. These findings warrant further monitoring on the Italian population’s mental health and could serve to inform structured interventions in order to mitigate the impact on mental health of the outbreak.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Internal review board, University of L’Aquila. The patients/participants provided their written informed consent to participate in this study.
Authors Contribution
Conceptualization: RR, VS, FP, GL. Methodology: RR. Formal Analysis: RR. Data Curation: RR, SM, GL. Writing—Original Draft: RR, VS. Writing—Review and Editing: RR, VS, DT, AM, FP, SM, CN, AR, AS, GL.
Conflict of Interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This work is supported by Territori Aperti, a project founded by “Fondo Territori Lavoro e Conoscenza CGIL CISL UIL”.
References
1. World Health Organization. Mental Health and Psychosocial Considerations During COVID-19 Outbreak. (2020).
2. Xiang Y-T, Yang Y, Li W, Zhang L, Zhang Q, Cheung T, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry (2020) 7(3):228–9. doi: 10.1016/S2215-0366(20)30046-8
3. Dong L, Bouey J. Public Mental Health Crisis during COVID-19 Pandemic, China. Emerg Infect Dis (2020) 26(7):1616–8. doi: 10.3201/eid2607.202407
4. Tucci V, Moukaddam N, Meadows J, Shah S, Galwankar SC, Bobby Kapur G. The forgotten plague: Psychiatric manifestations of ebola, zika, and emerging infectious diseases. J Global Infect Dis (2017) 9:151–6. doi: 10.4103/jgid.jgid_66_17
5. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet (2020) 395(10227):912–20. doi: 10.1016/S0140-6736(20)30460-8
6. DiGiovanni C, Conley J, Chiu D, Zaborski J. Factors influencing compliance with quarantine in Toronto during the 2003 SARS outbreak. Biosecur Bioterror (2004) 2(4):265–72. doi: 10.1089/bsp.2004.2.265
7. Hawryluck L, Gold WL, Robinson S, Pogorski S, Galea S, Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis (2004) 10(7):1206–12. doi: 10.3201/eid1007.030703
8. Lee S, Chan LYY, Chau AMY, Kwok KPS, Kleinman A. The experience of SARS-related stigma at Amoy Gardens. Soc Sci Med (2005) 61(9):2038–46. doi: 10.1016/j.socscimed.2005.04.010
9. Bai YM, Lin CC, Lin CY, Chen JY, Chue CM, Chou P. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr Serv (2004) 55:1055–7. doi: 10.1176/appi.ps.55.9.1055
10. Wu P, Fang Y, Guan Z, Fan B, Kong J, Yao Z, et al. The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry (2009) 54(5):302–11. doi: 10.1177/070674370905400504
11. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw Open (2020) 3(3):e203976. doi: 10.1001/jamanetworkopen.2020.3976
12. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int J Env Res Public Heal (2020) 17(5):1729. doi: 10.3390/ijerph17051729
13. Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen Psychiatry (2020) 33(2):19–21. doi: 10.1136/gpsych-2020-100213
14. Olff M, Bakker A, Frewen P, Aakvaag H, Ajdukovic D, Brewer D, et al. Screening for consequences of trauma – an update on the global collaboration on traumatic stress. Eur J Psychotraumatol (2020) 11(1):1752504. doi: 10.1080/20008198.2020.1752504
15. Spitzer RL, Kroken K, Williams JB. Validation and Utility of a Self-Report Version of PRIME-MD: The PHQ Primary Care Study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA (1999) 282(18):1737. doi: 10.1001/jama.282.18.1737
16. Spitzer RL, Kroenke K, Williams JBW, Löwe B. A Brief Measure for Assessing Generalized Anxiety Disorder. Arch Intern Med (2006) 166(10):1092. doi: 10.1001/archinte.166.10.1092
17. Morin CM, Belleville G, Bélanger L, Ivers H. The Insomnia Severity Index: Psychometric Indicators to Detect Insomnia Cases and Evaluate Treatment Response. Sleep (2011) 34(5):601–8. doi: 10.1093/sleep/34.5.601
18. Cohen S, Hoberman HM. Positive Events and Social Supports as Buffers of Life Change Stress1. J Appl Soc Psychol (1983) 13(2):99–125. doi: 10.1111/j.1559-1816.1983.tb02325.x
19. Shevlin M, Hyland P, Ben-Ezra M, Karatzias T, Cloitre M, Vallières F, et al. Measuring ICD-11 adjustment disorder: the development and initial validation of the International Adjustment Disorder Questionnaire. Acta Psychiatr Scand (2020) 141(3):265–74. doi: 10.1111/acps.13126
20. Girolamo G, Polidori G, Morosini P, Scarpino V, Reda V, Serra G, et al. Prevalence of common mental disorders in Italy. Soc Psychiatry Psychiatr Epidemiol (2006) 41(11):853–61. doi: 10.1007/s00127-006-0097-4
21. Liu N, Zhang F, Wei C, Jia Y, Shang Z, Sun L, et al. Prevalence and predictors of PTSS during COVID-19 Outbreak in China Hardest-hit Areas: Gender differences matter. Psychiatry Res (2020) 287:112921. doi: 10.1016/j.psychres.2020.112921
22. Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res (2020) 287:112934. doi: 10.1016/j.psychres.2020.112934
Keywords: covid-19, mental health, trauma, depression, anxiety, stress
Citation: Rossi R, Socci V, Talevi D, Mensi S, Niolu C, Pacitti F, Di Marco A, Rossi A, Siracusano A and Di Lorenzo G (2020) COVID-19 Pandemic and Lockdown Measures Impact on Mental Health Among the General Population in Italy. Front. Psychiatry 11:790. doi: 10.3389/fpsyt.2020.00790
Received: 09 April 2020; Accepted: 23 July 2020;
Published: 07 August 2020.
Edited by:
Dinesh Kumar Bhugra, King’s College London, United KingdomReviewed by:
Andres Ricardo Schneeberger, Albert Einstein College of Medicine, United StatesMichaela Pascoe, Victoria University, Australia
Copyright © 2020 Rossi, Socci, Talevi, Mensi, Niolu, Pacitti, Di Marco, Rossi, Siracusano and Di Lorenzo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Valentina Socci, dmFsZW50aW5hc29jY2lAZ21haWwuY29t
 Rodolfo Rossi
Rodolfo Rossi Valentina Socci
Valentina Socci Dalila Talevi
Dalila Talevi Sonia Mensi
Sonia Mensi Cinzia Niolu
Cinzia Niolu Francesca Pacitti
Francesca Pacitti Antinisca Di Marco5
Antinisca Di Marco5 Alessandro Rossi
Alessandro Rossi Giorgio Di Lorenzo
Giorgio Di Lorenzo