
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 31 March 2020
Sec. Mood Disorders
Volume 11 - 2020 | https://doi.org/10.3389/fpsyt.2020.00188
 Mauro Giovanni Carta1*
Mauro Giovanni Carta1* Naomi Fineberg2,3
Naomi Fineberg2,3 Maria Francesca Moro4
Maria Francesca Moro4 Antonio Preti1
Antonio Preti1 Ferdinando Romano5
Ferdinando Romano5 Matteo Balestrieri6
Matteo Balestrieri6 Filippo Caraci7,8
Filippo Caraci7,8 Liliana Dell'Osso9
Liliana Dell'Osso9 Guido Disciascio10
Guido Disciascio10 Filippo Drago7
Filippo Drago7 Maria Carolina Hardoy11
Maria Carolina Hardoy11 Rita Roncone12
Rita Roncone12 Luigi Minerba1
Luigi Minerba1 Carlo Faravelli13
Carlo Faravelli13 Jules Angst14
Jules Angst14Background: The impact of the comorbidity between Obsessive-Compulsive Disorder (OCD) and Bipolar Disorder Spectrum (BDS) remains to be clarified. The objective of this study was to examine the lifetime prevalence of OCD, the strength of the association of OCD with comorbid BDS and the role of comorbidity of OCD with BDS in the impairment of health-related quality of life (HRQoL) in an Italian community survey.
Methods: The study is a community survey. The sample (N = 2,267; women: 55.3%) was randomly selected after stratification by sex and four age groups from the municipal records of the adult population of one urban, one suburban, and at least one rural area in six Italian regions. Physicians using a semi-structured interview (Advanced Tools and Neuropsychiatric Assessment Schedule, ANTAS-SCID) made Diagnostic and Statistical Manual of Mental Disorders – 4th revision (DSM-IV) diagnoses of OCD, Major Depressive Disorder (MDD) and Bipolar Disorder (BD). HR-QoL was measured by the Health Survey Short Form (SF-12). Lifetime Hypomania and subthreshold hypomania were screened by the Mood Disorder Questionnaire (MDQ). BDS was defined as the sum of people shown to be positive for hypomania by the MDQ—with or without a mood disorder diagnosis—plus people with a BD-DSMIV diagnosis even if negative for hypomania at the MDQ.
Results: Overall, 44 subjects were diagnosed with OCD, 6 with MDD and 1 with BD. The lifetime prevalence of OCD was 1.8% in men (n = 18) and 2.0% in women (n = 26). MDD with lifetime subthreshold hypomania (i.e., people screened positive at the MDQ, even without diagnosed mania or hypomania at the interview) was associated with OCD (OR = 18.15, CI 95% 2.45–103.67); MDD without subthreshold hypomania (and screened negative at the MDQ) was not (OR = 2.33, CI 95% 0.69–7.01). People with BDS were strongly associated with OCD (OR = 10.5, CI 95% 4.90–12.16,). People with OCD and BDS showed significantly poorer HR-QoL than people with OCD without BDS (F = 9.492; P < 0.003).
Discussion: The study found a strong association between BDS and OCD. BDS comorbid with OCD was associated with more severe impairment of HR-QoL than OCD without comorbid BDS. Identification of symptoms of hypomania, including subthreshold symptoms, may therefore be important in people with OCD as they might predict a course with poorer HR-QoL.
Obsessive-Compulsive Disorder (OCD) is a common, disabling neuropsychiatric disorder known to be highly comorbid with mood, anxiety, and other disorders classified in the “Obsessive-Compulsive And Related Disorders” group (1, 2). Comorbidity with other psychiatric disorders increases the levels of distress and disability, while the association with Bipolar Disorder (BD) is thought to be particularly harmful and difficult to treat (2).
Although there is a considerable body of recent research on OCD, most studies have focused on course, treatment, pathogenesis, and brain imaging, while methodological differences between published epidemiological studies leave many aspects of prevalence, and especially the comorbidity of OCD with mood disorders, in need of clarification (3, 4).
The estimated prevalence of OCD varies across surveys (2), perhaps as a consequence of different approaches in their design and methodology and of the diagnostic method adopted (1, 3, 5). However, the vast majority of studies, including the more recent ones adopting more structured interviews and lay interviewers (3–7) have found lifetime prevalence rates in a range of 2–3%. However, all of these results are far below the OCD findings from the recent WHO Health Survey, which reported a lifetime prevalence of DSM-IV OCD of 6.2%, ranging from 5.8% in low- and middle-income countries to 6.9% in high-income countries (8).
Lifetime OCD occurring in people with lifetime diagnosis of BD range from 11 to 21% in population-based surveys (9, 10). Lower values were found in hospital-based studies, ranging from 3 to 16% (11, 12). It is not known whether this could be due to the lower diagnostic threshold (of one or both of the disorders) in the community surveys combined with higher co-morbidity in sub-threshold cases, or if it is due to higher accuracy of the diagnoses with co-morbidity produced by the use of standardized tools in community surveys. Conversely, there is a wide variance in the reported lifetime prevalence of Bipolar Disorder Spectrum (BDS) in people with OCD, ranging from 6 to 55% depending on the method of investigation and the definition of the bipolar spectrum adopted (12). A recent meta-analysis estimated the lifetime prevalence of OCD in patients with BD to be 10.9% (95% CI: 7.8–14.4%) (13). This estimated lifetime prevalence was several times higher than the prevalence of OCD estimated in the general population (2.5%; 1.9–3.1%) (13).
There are authors who include in their definitions of the bipolar spectrum those patients in which episodes of subthreshold mania occur concomitantly with lifetime depressive episodes, anxiety disorders, obsessive compulsive disorders, and substance abuse disorder but without previous episodes of mania or hypomania (14). However, according to some authors the spectrum also includes the hyperthymic temperament, even without episodes of impaired mood (15). Yet some other authors define the bipolar spectrum as including those symptoms that have been seen to be associated with or to precede the onset of bipolar disorder: sleep disturbances, subthreshold anxiety and depression, behavioral dyscontrol, and irritability (16).
People with both OCD and BD have been found to show greater disability, poorer HR-QoL, and poorer treatment response compared to those with only one of the two disorders (12). However, a similarly negative outcome was also found in patients having OCD in association with conditions of the BDS, i.e., with subthreshold hypomania but without a DSM diagnosis of BD (12).
It should further be noted that in epidemiological studies the approach based on lay interviewers and structured interviews has been of little help in explaining the role of BD, since this method of information gathering hinders the identification of the disorder, particularly BD II (alternating episodes of Major Depressive Disorder [MDD] and of hypomania). The frequent lack of subjective insight regarding episodes of hypomania means that a correct diagnosis requires sources other than self-reporting (i.e., how these patients appear to others, and what relatives and friends say about the patient) (14). Such information is systematically gathered in clinical practice but is not collected by structured interviews conducted by lay interviewers in epidemiological surveys. This approach has led to the frequent mis-identification of episodes of the depressive phase of the BD as a part of a MDD (14).
This issue is particularly relevant for the study of the comorbidity of OCD with mood disorders. Data from the Zurich study (17) have underlined a closer association between OCD and BD (but also with the subthreshold bipolar syndromes) than between OCD and MDD. The Zurich study was the only epidemiological survey repeated over time (which is an additional source for identifying lifetime mania) and also the only one, in recent years, in which clinicians made the diagnoses. That study further indicated that comorbidity with BD (and with subthreshold bipolar syndromes) is a powerful factor in determining impairment in people suffering from OCD (2).
The objectives of this paper are therefore to extend the investigation of the association between OCD and bipolar spectrum by (a) identifying the lifetime prevalence of OCD in a community study in six Italian regions, using semi-structured interviews conducted by physicians with experience in mental health; (b) determining the comorbidity of OCD with mood disorders, both MDD and BD, including subthreshold manic episodes (BDS broadly defined); and (c) clarifying how far OCD in association with MDD, BD, and subthreshold manic episodes impairs HR-QoL.
The sample was randomly drawn from the municipal records of one urban, one suburban, and at least one rural area in six Italian regions, which were chosen because they are representative, in terms of geography and socio-cultural characteristics, of the entire national territory. Randomization for those registers was performed after stratification by sex and four age groups (18–24; 25–44; 45–64; >64). Participants were contacted by phone and mail. The interviews were carried out by physicians, face to face in the subjects' homes. The survey methodology was published earlier (18). The main objective of that study was to measure the relationship between the use of drugs and psychiatric disorders in the community.
1) The Advanced Tools and Neuropsychiatric Assessment Schedule -Structured Clinical Interview for DSM-IV (ANTAS—SCID-IV) (18), a semi-structured, clinician administered, computerized interview derived from the SCID (19); ANTAS–SCID-IV allows diagnosis of Mood, Anxiety and Eating disorders according to DSM—IV-TR (20) high reliable with SCID (18).
2) The Italian version (21) of the Mood Disorder Questionnaire (MDQ) (22) was adopted to assess lifetime hypomanic symptoms and subthreshold hypomanic episodes. Although this tool shows low accuracy as a screener for DSM—defined BD (23), the research has shown that it is acceptable for identifying subthreshold cases (15).
3) The cut-off score for screening positive for BDS was established on the basis of the standardization study (21) and involved scoring “Yes” to ≥8 items on a list of the 13 best known symptoms of mania / hypomania and “yes” to a question “have several of these ever happened during the same period of time?”
4) The Health Survey Short Form (SF−12) (24) was used to assess perceived HR-QoL as a measure of the impact of OCD and its comorbid conditions. The SF-12 covers physical functioning, physical health, emotional state, physical pain, general health, vitality, social activity, and mental health. The HR-QoL is considered a relevant construct for measuring outcome in chronic diseases that require long-term treatments and greatly impair and impact daily life (25).
OCD, MDD, and BD were defined according to DSM-IV criteria.
The BDS group was defined as including either all those with DSM-IV BD (i.e., diagnosed with Bipolar Disorder on the ANTAS-SCID) and all those screening positive on the MDQ. This group thus includes those diagnosed (on the ANTAS-SCID) with BD or with MDD and lifetime hypomanic symptoms (i.e., MDQ positives), and those with lifetime subthreshold hypomania (i.e., MDQ positives) but having no diagnosis of MDD or BD according ANTAS-SCID.
The MDD group was thus sub-divided into those with and without subthreshold lifetime hypomania (i.e., respectively, screening positive or negative on the MDQ) and included in or excluded from the BDS group.
The odds ratio (univariate analysis) for DSM-IV OCD diagnosis and age, gender, and comorbidity with DSM-IV MDD, DSM-IV BD, and BDS (i.e., any case diagnosed with BD according to DSM-IV or screened positive on the MDQ) was calculated using one of the groups in each table as a “pivot.” Statistical significance was calculated using the χ2 test. Odds, ratios and 95% confidence intervals were calculated using Miettinen's simplified method (26). The comparisons between the scores on the SF-12 in the different groups were calculated by one-way ANOVA.
The burden in the worsening of HR-QoL attributable to OCD was calculated as the difference between the HR-QoL (mean score on the SF-12) in a sample from the same community survey database of people without OCD and the SF-12 mean score of those with OCD. The randomization was conducted after standardization by blocks. For each person with OCD two people, matched by age and sex, were selected by randomization from the cell of all without OCD.
A similar method was adopted for measuring the burden in the deterioration of HR-QoL attributable to OCD with BDS. Thus, the attributable burden of OCD with BDS was the difference between the HR-QoL (mean score on the SF-12) in a sample from the community survey database of people without OCD and the SF-12 mean score of those with OCD plus BDS as above defined (BD + all positives on MDQ). The proportion of the sample drawn for comparison (without OCD) was 2/1 for OCD without BDS and 4/1 for OCD with BDS.
Overall, 44 subjects were diagnosed with OCD at the ANTAS-SCID, 6 were diagnosed with MDD and just 1 was diagnosed with BD.
Table 1 illustrates the lifetime prevalence for OCD by age and gender in the epidemiological sample (2,267 subjects, 1,253 women [55.3%]). The prevalence of OCD was 1.8% in men (n = 18) and 2.0% in women (n = 26); with no difference by gender (OR = 1.15, CI 95% 0.61–2.19). The prevalence rate among young women aged 18–24 (n = 7 [5.1%]), was higher than in all other age groups.
Table 2 shows the associations between mood disorders and OCD. MDD was associated with OCD in 13.6% of all cases of OCD (OR = 3.69, CI 95% 1.36–9.41). When the set of MDD was subdivided into those cases with and without subthreshold episodes of hypomania (MDQ positive and MDQ negative), only the subgroup of MDD with lifetime subthreshold hypomania, constituting 4.5% of the whole OCD sample, showed a strong association with OCD (OR = 18.15, CI 95% 2.45–103.67). In contrast, the MDD subgroup without subthreshold hypomania, constituting 9% of the whole OCD sample, showed no association with OCD (OR = 2.33, CI 95% 0.69–7.01). The BDS group (as defined above) was also strongly associated with OCD (OR = 10.5, CI 95% 4.90–12.16). The one participant who was recognized positive for BD at the ANTAS-SCID also had OCD (2.8%; OR = 26.6, CI 95% 0.93–384.3).
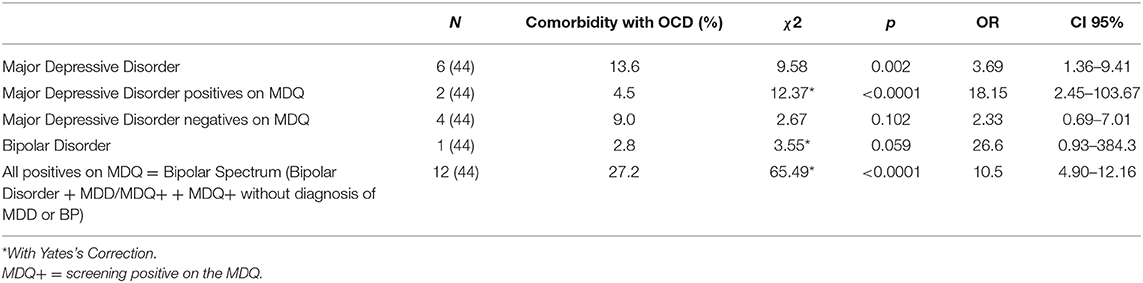
Table 2. Comorbidity between Obsessive Compulsive Disorders and Major Depressive Disorders (MDD) with further subdivision between MDD screening positive on the MDQ and MDD screening negative on the MDQ; Bipolar Disorders and Bipolar Spectrum Disorders (including BD, MDD positives on the MDQ, and positives on the MDQ without a diagnosis of BP or MDD).
In terms of the impairment of HR-QoL attributable to OCD alone, OCD with BDS and OCD without BDS, the results revealed that OCD alone is a significant factor in compromising HR-QoL, with mean SF-12 scores of 35.4 ± 6.9 and an attributable impairment of HR-QoL of 2.9 ± 6.0 in 44 cases as against 88 controls. We isolated the 12 cases of OCD with BDS (of these 12 cases, one also had a diagnosis of BD, 6 had a diagnosis of Panic Disorder, 2 of MDD [1 of which had comorbid Panic Disorder], 1 of Post Traumatic Stress Disorder). These cases were found to have a significantly higher level of impairment of HR-QoL than the other OCD cases, even though the latter group included those with MDD screening negative on the MDQ. The mean SF-12 scores were 33.6 ± 6.7 in those with OCD and BDS, and it 36.1 ± 7.1 in those with OCD without comorbid BDS, with an attributable impairment of HR-QoL of, respectively, 6.1 ± 5.9 (12 cases vs. 48 controls) and 2.1 ± 7.4 (32 cases vs. 64 controls): F[1;110;111] = 9.49; P < 0.003.
The study, which was based on semi-structured clinical interviews administered by physicians with experience in mental health, found lower prevalence rates of OCD than the recent WHO epidemiological survey (8). Our results were closer to other studies conducted since the 1980s, including those relying on lay interviewers and structured interviews (3, 5, 27–31), although caution is needed when comparing these surveys on account of methodological differences.
Our study showed a higher frequency among younger age groups, which suggests a youthful onset or a cohort effect (8).
The frequency of the association between Bipolar Disorder and OCD in our sample (2.8%) is lower than the frequency found in previous epidemiological studies (10, 11) but in the range [2–3%] reported in the aforementioned clinical studies (11, 12), and in studies looking for comorbidity with BD in patients with OCD (32); this is probably due to methodological differences. The diagnosis of BD (and OCD) in our study was detected with a semi-structured interview conducted by clinicians, as opposed to the community surveys in which the diagnoses are made by structured interviews conducted by lay interviewers. It is known that the frequencies of psychiatric disorders identified with the SCID interview are tendentially low (14). Studies form the same data-base of the present found lower frequencies of both MDD (18) and BD (33) compared to other studies conducted by means of structured interviews.
The notable finding of the present study is the close association between OCD and BDS including DSM-IV Bipolar Disorder, DSM-IV Major Depressive Disorder showing hypomanic subthreshold episodes, and people showing hypomanic subthreshold episodes without a mood diagnosis. The association of OCD with the BDS is well-documented in clinical settings (12, 34).
Our study also found that in a random sample of the general population the comorbidity between OCD and BDS is associated with a seriously impaired HR-QoL. That impairment is considerably less marked in people with OCD who did not display bipolar spectrum symptoms. The impairment of HR-QoL attributable to the comorbidity of OCD with the BDS is substantial, and the measurable burden is equal or very similar to that of other psychiatric (MDD, Panic Disorder, Eating Disorders) conditions, as measured in case-control studies that used the same methodology applied in the present study (35–38). It should be noted that some of the cases included in the BDS subgroup also were comorbid with other disorders, such as Panic Disorder, and this might have influenced the extent of the impairment of HR-QoL attributable to the comorbidity of OCD. However, BD is highly comorbid with anxiety disorders such as Panic Disorder (39), and therefore it might be difficult to disentangle the impact of the associated hypomania and of comorbid anxiety disorders when investigating samples that are distinguished on the basis of their comorbidity with BD.
This finding is consistent with the clinical observation that cases of OCD in association with BD (including subthreshold manifestations) are the most severe and have a worse course (40, 41). The prospective epidemiological Zurich Study, which analyzed two groups of probands from age 20 to 40, one having OCD with BD, the other without, showed more chronic episodes, residual symptoms and previous recurrence of depressive episodes in the comorbid group. In the comorbid group higher rates of anxiety disorders, impulse control disorders, eating disorders, and tic disorders were also found (17). The follow-up analysis to age 50 also confirmed that the co-occurrence of OCD and bipolar spectrum (including subthreshold bipolar disorder) was associated with significantly higher levels of treatment-seeking, impairment, distress, suicidality, and an increased risk of alcohol abuse/dependence compared with “pure” OCD (2), although this is not an universal finding (42). A poorer quality of life was also indicated as a specific feature of bipolar-OCD comorbidity (41). In agreement with these results, our study found that the association of OCD with BDS produced more substantial impairment than those with comorbid MDD but without bipolar spectrum symptomatology. Given that a diagnosis of MDD is known to be a major determinant of reduced HR-QoL when comorbid with other psychiatric conditions (18), this finding emphasizes the damaging effect of BDS on HRQoL, with or without diagnosis of a mood disorder, when combined with OCD.
Criticism has been leveled against the use of screening questionnaires to detect cases of BD. It is argued that only a small percentage of “positives” on such screening tools would be recognized as having BD if they were to undergo a structured interview using DSM as the diagnostic gold standard (23, 43, 44). However, our research has provided clear evidence that the wide spectrum of “false positives” that emerge when screening for BDS (i.e., being positive at screening but below the diagnostic threshold according to the gold standard international descriptive criteria) show demographic characteristics, a comorbidity profile, a type of social impairment, drug and health care use, and have brain imaging profiles that indicate that they belong to clearly defined subthreshold bipolar spectrum group (14, 18). It is also interesting to note that in the previously mentioned clinical studies on OCD, many of the characteristics identified as defining OCD comorbid with bipolar subthreshold, namely anxiety disorders, substance abuse, personality disorders, and the risk of suicide, are also to be found among the so-called “false positives” identified by screening tools such as MDQ, i.e., people positive at the screening but who did not fulfill the DSM-IV criteria for BD (14).
The results suggest that screening people with OCD for symptoms of hypomania is crucial, as the comorbidity represents an important marker of severity and risk of impairment. The fact that longitudinal clinical studies have also found that the presence of hypomanic symptoms (including subthreshold symptoms) is a predictor of treatment response (45–47) adds strength to the argument.
This study has both strengths and limitations. The main strengths are the use of structured, standardized instruments for measurement, and the investigation in a reasonably large, community-based sample randomly drawn from the municipal records of geographical areas expected to be representative of the socio-cultural characteristics of the entire national territory.
The most important limitation is that, although the research is a community survey with a large sample, the focus of this research was not the main objective of the project. The sample was built on the basis of the expected frequencies of subthreshold mania (focus of main objective of the whole project), which was estimated at 4% (18), while the lifetime prevalence of OCD (focus on this secondary objective) was found in this study to be <2%. Thus, the hypotheses that can arise from the reading of these data have a heuristic and stimulating value rather than a conclusive one. The results must therefore be confirmed by future studies with larger samples and specifically focused on this topic.
Another important limitation is that we used ratings on the MDQ to identify a diagnostic group (“subthreshold bipolar disorders”) that is hard to pin down and is particularly controversial. Additional limitations include the lack of details on some correlates of BDS comorbidity among OCD participants, which could be of interest on a clinical ground (e.g., OCD course and severity, symptom dimensions, suicidality, other comorbidities); lack of statistical power for some analysis due to the small size of some subsamples; lack of information on some unexplored comorbidities, such as impulse control disorder or personality disorders, which could have a differential impact on HR-QoL in the two study groups.
These results from a random sample of the general population have found a strong association between mood disorders including bipolar and subthreshold bipolar symptomatology and the diagnosis of OCD. These findings confirm that cases of BDS comorbid with OCD are associated with more severe impairment of quality of life. The identification of symptoms of hypomania, including subthreshold symptoms, may therefore be crucial in people with OCD. The results must be confirmed by future studies.
The datasets for this article are not publicly available because: the agreement shared with the partners in the planning of the study, in the presentation for the assignment of the original grant and in the request for authorization to the ethics committee was that the database (with anonymous records) would be available under the review of the project leader as guarantor. Requests to access the datasets should be directed to Mauro Giovanni Carta.
The ethics committee of the Italian National Health Institute, Rome (Istituto Superiore della Sanità) approved the study. All procedures performed in the studies were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments. Each participant was provided with full information on the aims and methodology of the study and signed an informed consent form. Participants were also made aware of data protection and privacy laws and that they could terminate the interview at any time. It was explained that the data would be used as an anonymous database, in order to maintain confidentiality in accordance with data protection laws. In addition, all studies that are carried out by our Center at the University of Cagliari are reviewed by the Comitato Etico Indipendente Azienda Ospedaliera Universitaria di Cagliari. Written informed consent was collected from all participants.
MC had the first idea of the epidemiological study that was planned and carried out jointly with MB, FC, LD, GD, FD, MH, RR, and CF (these researchers are also responsible for the database). The present study was proposed by the MC, JA, and MM to the coordination group. The processing group was also involved, due to their specific skills, NF, FR, AP, and LM. The study and data processing was planned and conducted with the participation of the entire group. MC with MM wrote the first draft that was revised by each of the participants who approved the reworked paper based on the suggestions.
The study was based on a databank of a project funded by AIFA, Agenzia Italiana del Farmaco that was closed in 2012, the project planned these secondary analyses. No additional resources were found for the present analyses.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Arlington, VA: American Psychiatric Publishing (2013).
2. Fineberg NA, Hengartner MP, Bergbaum C, Gale T, Rössler W, Angst J. Lifetime comorbidity of obsessive-compulsive disorder and sub-threshold obsessive-compulsive symptomatology in the community: impact, prevalence, socio-demographic and clinical characteristics. Int J Psychiatry Clin Pract. (2013) 17:188–96. doi: 10.3109/13651501.2013.777745
3. Ruscio AR, Stein DJ, Chiu WT, and Kessler RC. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Mol Psychiatry. (2010) 15:53–63. doi: 10.1038/mp.2008.94
4. Fontenelle LF, Mendlowicz MV, Versiani M. The descriptive epidemiology of obsessive-compulsive disorder. Prog Neuropsychopharmacol Biol Psychiatry. (2006) 30:327–37. doi: 10.1016/j.pnpbp.2005.11.001
5. Torres AR, Prince MJ, Bebbington PE, Bhugra D, Brugha TS, Farrell M, et al. Obsessive-compulsive disorder: prevalence, comorbidity, impact, and help-seeking in the British National Psychiatric Morbidity Survey of 2000. Am J Psychiatry. (2006) 163:1978–85. doi: 10.1176/ajp.2006.163.11.1978
6. Weissman MM, Bland RC, Canino GJ, Greenwald S, Hwu HG, Lee CK, et al. The cross national epidemiology of obsessive compulsive disorder. J Clin Psychiatry. (1994) (Suppl. 55):5–10.
7. Karno M, Golding JM, Sorenson SB, Burnam MA. The epidemiology of obsessive-compulsive disorder in five US communities. Arch Gen Psychiatry. (1988) 45:1094–9. doi: 10.1001/archpsyc.1988.01800360042006
8. Kessler RC, Ormel J, Petukhova M, McLaughlin KA, Green JG, Russo LJ, et al. Development of lifetime comorbidity in the World Health Organization world mental health surveys. Arch Gen Psychiatry. (2011) 68:90–100. doi: 10.1001/archgenpsychiatry.2010.180
9. Chen YW, Dilsaver SC. Comorbidity for obsessive-compulsive disorder in bipolar and unipolar disorders. Psychiatry Res. (1995) 59:57–64. doi: 10.1016/0165-1781(95)02752-1
10. Marikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RM, Petukhova M, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Arch Gen Psychiatry. (2007) 64:543–52. doi: 10.1001/archpsyc.64.5.543
11. Shashidhara M, Sushma BR, Viswanath B, Math SB, Janardhan Reddy YC. Comorbid obsessive compulsive disorder in patients with bipolar-I disorder. J Affect Disord. (2015) 174:367–71 doi: 10.1016/j.jad.2014.12.019
12. Amerio A, Odone A, Liapis CC, Ghaemi SN. Diagnostic validity of comorbid bipolar disorder and obsessive-compulsive disorder: a systematic review. Acta Psychiatr Scand. (2014) 129:343–58. doi: 10.1111/acps.12250
13. Ferentinos P, Preti A, Veroniki AA, Pitsalidis KG, Theofilidis AT, Antoniou A, et al. Comorbidity of obsessive-compulsive disorder in bipolar spectrum disorders: systematic review and meta-analysis of its prevalence. J Affect Disord. (2020) 263:193–208. doi: 10.1016/j.jad.2019.11.136
14. Carta MG, Angst J. Screening for bipolar disorders: a public health issue. J Affect Disord. (2016) 205:139–43. doi: 10.1016/j.jad.2016.03.072
15. Karam EG, Salamoun MM, Yeretzian JS, Mneimneh ZN, Karam AN, Fayyad J, et al. The role of anxious and hyperthymic temperaments in mental disorders: a national epidemiologic study. World Psychiatry. (2010) 9:103–10. doi: 10.1002/j.2051-5545.2010.tb00287.x
16. Hafeman DM, Merranko J, Axelson D, Goldstein BI, Goldstein T, Monk K, et al. Toward the definition of a bipolar prodrome: dimensional predictors of bipolar spectrum disorders in at-risk youths. Am J Psychiatry. (2016) 173:695–704. doi: 10.1176/appi.ajp.2015.15040414
17. Angst J, Gamma A, Endrass J, Hantouche E, Goodwin R, Ajdacic V, et al. Obsessive-compulsive syndromes and disorders: significance of comorbidity with bipolar and anxiety syndromes. Eur Arch Psychiatry Clin Neurosci. (2005) 255:65–71. doi: 10.1007/s00406-005-0576-8
18. Carta MG, Aguglia E, Bocchetta A, Balestrieri M, Caraci F, Casacchia M, et al., The use of antidepressant drugs and the lifetime prevalence of major depressive disorders in Italy. Clin Pract Epidemiol Ment Health. (2010) 6:94–100. doi: 10.2174/1745017901006010094
19. First M, Spitzer R, Gibbon M, Williams J. Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version, Non-Patient Edition (SCID-I/NP). New York, NY: Biometrics Research, New York State Psychiatric Institute (1997).
20. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Text Revision. Washington, DC: APA Press (2000).
21. Hardoy MC, Cadeddu M, Murru A, dell Osso B, Carpiniello B, Morosini PL, et al. Validation of the Italian version of the mood disorder questionnaire for the screening of bipolar disorders. Clin Pract Epidemiol Ment Health. (2005) 1:8. doi: 10.1186/1745-0179-1-8
22. Hirschfeld RM, Calabrese JR, Weissman MM, Reed M, Davies MA, Frye MA, et al. Screening for bipolar disorder in the community. J Clin Psychiatry. (2003) 64:53–9. doi: 10.4088/JCP.v64n0111
23. Zimmerman M, Galione, JN, ChelminskiI I, Young D, Dalrymple K. Psychiatric diagnoses in patients who screen positive on the mood disorder questionnaire: implications for using the scale as a case-finding instrument for bipolar disorder. Psychiatry Res. (2011) 185:444–9. doi: 10.1016/j.psychres.2010.06.025
24. Ware J Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. (1996) 34:220–33. doi: 10.1097/00005650-199603000-00003
25. Mantovani G, Astara G, Lampis B, Bianchi A, Curreli L, Orrù W, et al. Evaluation by multidimensional instruments of health-related quality of life of elderly cancer patients undergoing three different “psychosocial” treatment approaches. a randomized clinical trial. Support Care Cancer. (1996) 4:129–40. doi: 10.1007/BF01845762
26. Miettinen O, Nurminen M. Comparative analysis of two rates. Stat Med. (1985) 4:213–26. doi: 10.1002/sim.4780040211
27. Bebbington PE. Epidemiology of obsessive-compulsive disorder. Br J Psychiatry Suppl. (1998) 2–6.
28. Osland S, Arnold PD, Pringsheim T. The prevalence of diagnosed obsessive compulsive disorder and associated comorbidities: a population-based Canadian study. Psychiatry Res. (2018) 268:137–42. doi: 10.1016/j.psychres.2018.07.018
29. Mohammadi MR, Ghanizadeh A, Rahgozar M, Noorbala AA, Davidian H, Afzali HM, et al. Prevalence of obsessive-compulsive disorder in Iran. BMC Psychiatry. (2004) 4:2. doi: 10.1186/1471-244X-4-2
30. Subramaniam M, Abdin E, Vaingankar JA, Chong SA. Obsessive – compulsive disorder: prevalence, correlates, help-seeking and quality of life in a multiracial Asian population. Soc Psychiatry Psychiatr Epidemiol. (2012) 47:2035–43. doi: 10.1007/s00127-012-0507-8
31. Subramaniam M, Abdin E, Vaingankar JA, Shafie S, Chua BY, Sambasivam R, et al. Tracking the mental health of a nation: prevalence and correlates of mental disorders in the second Singapore mental health study. Epidemiol Psychiatri Sci. (2019) 29:e29. doi: 10.1017/S2045796019000179
32. Saraf G, Paul I, Viswanath B, Narayanaswamy JC, Math SB, Reddy YC. Bipolar disorder comorbidity in patients with a primary diagnosis of OCD. Int J Psychiatry Clin Pract. (2017) 21:70–4. doi: 10.1080/13651501.2016.1233344
33. Carta MG, Sorbello O, Moro MF, Bhat KM, Demelia E, Serra A, et al. Bipolar disorders and Wilson's disease. BMC Psychiatry. (2012) 12:52. doi: 10.1186/1471-244X-12-52
34. Perugi G, Toni C, Frare F, Travierso MC, Hantouche E, Akiskal HS. Obsessive-compulsive-bipolar comorbidity: a systematic explorationof clinical features and treatment outcome. J Clin Psychiatry. (2002) 63:1129–34. doi: 10.4088/JCP.v63n1207
35. Carta MG, Lecca ME, Saba L, Sanfilippo R, Pintus E, Cadoni M, et al. Patients with carotid atherosclerosis who underwent or did not undergo carotid endarterectomy: outcome on mood, cognition and quality of life. BMC Psychiatry. (2015) 15:277. doi: 10.1186/s12888-015-0663-y
36. Carta MG, Preti A, Moro MF, Aguglia E, Balestrieri M, Caraci F, et al. Eating disorders as a public health issue: prevalence and attributable impairment of quality of life in an Italian community sample. Int Rev Psychiatry. (2014) 26:486–92. doi: 10.3109/09540261.2014.927753
37. Carta MG, Moro MF, Aguglia E, Balestrieri M, Caraci F, dell'osso L, et al. The attributable burden of panic disorder in the impairment of quality of life in a national survey in Italy. Int J Soc Psychiatry. (2015) 61:693–9. doi: 10.1177/0020764015573848
38. Sancassiani F, Romano F, Balestrieri M, Caraci F, di Sciascio G, Drago F, et al. The prevalence of specific phobia by age in an Italian Nationwide Survey: how much does it affect the quality of life? Clin Pract Epidemiol Ment Health. (2019) 15:30–7. doi: 10.2174/1745017901915010030
39. Preti A, Vrublevska J, Veroniki AA, Huedo-Medina TB, Kyriazis O, Fountoulakis KN. Prevalence and treatment of panic disorder in bipolar disorder: systematic review and meta-analysis. Evid Based Ment Health. (2018) 21:53–60. doi: 10.1136/eb-2017-102858
40. Timpano KR, Rubenstein LM, Murphy DL. Phenomenological features and clinical impact of affective disorders in OCD: a focus on the bipolar disorder and OCD connection. Depress Anxiety. (2012) 29:226–33. doi: 10.1002/da.20908
41. Issler CK, Monkul ES, de Mello Siqueira Amaral JA, Tamada RS, Shavitt RG, Miguel EC, et al. Bipolar disorder and comorbid obsessive-compulsive disorder is associated with higher rates of anxiety and impulse control disorders. Acta Neuropsychiatr. (2010) 22:81–6. doi: 10.1111/j.1601-5215.2010.00457.x
42. Maina G, Albert U, Pessina E, Bogetto F. Bipolar obsessive-compulsive disorder and personality disorders. Bipolar Disord. (2007) 9:722–9. doi: 10.1111/j.1399-5618.2007.00508.x
43. Zimmerman M, Galione JN, Ruggero CJ, Chelminski I, Young D, Dalrymple K, et al. Screening for bipolar disorder and finding borderline personality disorder. J Clin Psychiatry. (2010) 71:1212–7. doi: 10.4088/JCP.09m05161yel
44. Zimmerman M, Galione JN, Ruggero CJ, Chelminski I, Dalrymple K, Young D. Are screening scales for bipolar disorder good enough to be used in clinical practice? Compr Psychiatry. (2011) 52:600–6. doi: 10.1016/j.comppsych.2011.01.004
45. Tukel R, Oflaz SB, Ozyildirim I, Aslantaş B, Ertekin E, Sözen A, et al. Comparison of clinical characteristics in episodic and chronic obsessive-compulsive disorder. Depress Anxiety. (2007) 24:251–5. doi: 10.1002/da.20234
46. Pallanti S, Grassi G, Sarrecchia ED, Cantisani A, Pellegrini M. Obsessive-compulsive disorder comorbidity: clinical assessment and therapeutic implications. Front Psychiatry. (2011) 2:70. doi: 10.3389/fpsyt.2011.00070
Keywords: obsessive compulsive disorders, bipolar disorder, epidemiology, community survey, bipolar spectrum, quality of life
Citation: Carta MG, Fineberg N, Moro MF, Preti A, Romano F, Balestrieri M, Caraci F, Dell'Osso L, Disciascio G, Drago F, Hardoy MC, Roncone R, Minerba L, Faravelli C and Angst J (2020) The Burden of Comorbidity Between Bipolar Spectrum and Obsessive-Compulsive Disorder in an Italian Community Survey. Front. Psychiatry 11:188. doi: 10.3389/fpsyt.2020.00188
Received: 08 September 2019; Accepted: 26 February 2020;
Published: 31 March 2020.
Edited by:
Xenia Gonda, Semmelweis University, HungaryReviewed by:
Albina Rodrigues Torres, São Paulo State University, BrazilCopyright © 2020 Carta, Fineberg, Moro, Preti, Romano, Balestrieri, Caraci, Dell'Osso, Disciascio, Drago, Hardoy, Roncone, Minerba, Faravelli and Angst. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mauro Giovanni Carta, bWdjYXJ0YUB0aXNjYWxpLml0
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.