
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 13 March 2020
Sec. Mood Disorders
Volume 11 - 2020 | https://doi.org/10.3389/fpsyt.2020.00129
This article is part of the Research Topic Toward Comprehensive Understanding of the Suicidal Phenomenon View all 21 articles
Background and Objective: Suicide is a leading cause of death in young people. Suicidal thoughts and behaviors can be triggered by life and study stresses; therefore, it is important to understand the role of coping strategies. The current study analyzed the link between different coping strategies and suicidality in university students in China.
Methods: A cross-sectional study of 2,074 undergraduate students from China used a stratified-clustered-random sampling method (response rate 94.4%). The Suicidal Behaviors Questionnaire–Revised Scale was used to identify suicidal risks, while the Brief COPE scale was used to measure different coping strategies. Univariate and multivariate logistic regression analyses were utilized to examine coping strategies and suicidality.
Results: A negative association of some coping skills (active coping and positive reframing) with suicidality and a positive association of some other coping skills (self-distraction, substance abuse, behavioral disengagement, venting, and self-blame) with suicidality were observed after adjusting for sociodemographic and mental health variables.
Conclusions: Training and supporting young people to identify and apply adaptive coping strategies to deal with life stress could help to reduce suicidal ideation and behavior.
Suicidal behavior in young people is a public health and social issue globally (1–3). Suicide is a leading cause of death in young people (4); furthermore, nonfatal suicidal behavior is more prevalent in younger age groups (5, 6). Similarly to other countries, China is reporting a high prevalence of suicidal behavior among young people, including college students (7–9). Transitioning from adolescence to young adults, university students are considered as the future elite; however, academic and career expectations from themselves and their parents, competitive environments, achieving less than hoped, and failing a grade may lead to interpersonal conflicts and a sense of isolation, and further to stress, low personal control, autistic traits, internet addiction, depression, anxiety, and suicidal thoughts and attempts (10–15).
There is currently limited knowledge about protective factors for suicidal behavior and ideation. Existing research has examined various coping strategies impacting suicidal behaviors (16) and has analyzed gender-specific coping strategies associated with suicidal ideation in university students (17). Nevertheless, there has been relatively limited research that has focused on protective and risk effects of specific coping styles (18–20).
The available literature is inconsistent in conceptualizing and categorizing different coping styles (21, 22). This might be partly attributable to a number of different scales used to investigate coping strategies in various social and cultural contexts, such as the COPE (23), the Brief COPE (24), and the Coping Styles Questionnaire (CSQ) (25). Nevertheless, one common view is that individuals would apply adaptive and/or maladaptive (dysfunctional) coping skills when they face stress and threats (23, 26, 27). A recent study using Brief COPE from China showed that having a meaning of life is a protective factor, while self-distraction and self-blame are risk factors for suicidality in collage students (28). In another cross-sectional study, Zhang et al. (9) used CSQ to evaluate suicidality of university students in China. They found that passive coping (especially fantasizing) was positively associated with suicidal ideation. The results of Horwitz et al. (29), based on a cross-sectional study using Brief COPE, showed that behavioral disengagement and self-blame increased suicidal vulnerability. Furthermore, in a prospective study in college students using COPE, Chou et al. (30) reported that ineffective coping skills together with persistence stress and negative emotions could generate higher risk of suicidality.
Research has also shown mixed results regarding the relationship between avoidant coping and suicidality. Some studies indicate that avoidance coping strategies heighten the risk of suicidality as individuals tend to resign themselves to the problem, and do not undertake further efforts to reduce stressors (31–33). Others suggest that avoidance coping with a good purpose (such as decreasing the negative feelings of life stressors and temporary shifting focus from the stressors to other important things in life) could prevent suicidal behavior in adolescents and young people (20, 34). Nevertheless, none of the studies above used Brief COPE in measuring avoidant coping. It is important to better understand the relationship between different coping strategies (particularly avoidance strategies) and suicidality in young people. Therefore, this paper aims to analyze the association between specific coping strategies and suicidality (suicidal ideation and behavior) in a sample of university students in China.
In November 2016, undergraduate university students from two universities in Jinan (the capital city of Shandong province), China, voluntary participated in a cross-sectional survey. In total 2,074 students responded, with a response rate of 94.4%. A stratified–clustered–random sampling method was applied to select from three or four classes of students for each grade. The study received ethics approval from the institutional review board of the Ethics Committee at the School of Public Health, Shandong University (No. 20161103). Each participant signed an informed consent form before undertaking the questionnaire. The survey contained a brief battery of self-report psychosocial instruments, as described below.
The Suicidal Behaviors Questionnaire Revised Scale (SBQR) (35), adapted from Osman et al. (36), contains four items that assess suicidal thoughts and behaviors from different perspectives: lifetime suicidal ideation and attempt(s), frequency of suicidal ideation over the past year, risk of suicide attempt, and likelihood of suicidal behavior in the future. The Chinese version of the SBQ-R was validated (35) and adapted for this study. The total score of the scale was calculated, and a cut-off value of 7 was applied as recommended by Osman et al. (36).
Depression, Anxiety & Stress Scale (DASS-21) (37) is a 21-item scale that measures three dimensions of mental health: depression (Cronbach's alpha = 0.84), anxiety (Cronbach's alpha = 0.79), and stress (Cronbach's alpha = 0.82). Responses for all items range from “0—Did not apply to me at all” to “3—Applied to me very much or most of the time.”
The Brief COPE Scale consists of 28 items to measure 14 different coping strategies (24). In this study, the Chinese version of the scale (38) was adapted. The scale presents good internal reliability, with Cronbach's alpha = 0.83. The 14 dimensions of coping strategies are comprised of self-distraction, active coping, denial, substance abuse, use of emotional support, use of instrumental support, behavioral disengagement, venting, positive reframing, planning, humor, acceptance, religion, and self-blame. Each dimension contains two items, with sum score as the total dimension score.
The questionnaire also included sociodemographic categories, such as gender, ethnicity, residency, being an only child (with no siblings), general physical health and mental health, academic performance, family economic status, parent education level, parental bonding, and religious affiliation.
Odds ratios (ORs) with 95% confidence intervals (CI) were calculated to explore differences between the suicidal and non-suicidal groups by the categorical sociodemographic variables. Independent sample t-tests were used to identify differences between the two groups by coping strategies, and effect size (Cohen's d) was calculated for each coping skill. The Cohen's d cut-off values were considered as small (≥0.2), medium (≥0.5), and large (≥0.8) (39). Further, each coping skill was entered as a predictor into a logistic regression with suicidality (suicidal vs. non-suicidal) as the dependent variable. The calculations were adjusted for confounding effect of other factors: (1) a coping skill + sociodemographic variables; (2) a coping skill + sociodemographic variables + Depression + Anxiety + Stress. A probability level of 0.05 was applied for all statistical tests. SPSS version 22.0 was used for data analysis (IBM SPSS, Inc. in Chicago, Illinois, USA).
Among the 2,074 students, 20.6% (n = 428) were identified to have an SBQ-R total score of 7 or above and were included in the suicidal group, and the remaining 79.4% (n = 1,646) were assigned to the non-suicidal group. Table 1 presents the sociodemographic backgrounds of participants in the suicidal and non-suicidal groups. Gender, being an only child, and religious affiliation did not differ significantly between the suicidal and non-suicidal groups. However, there were significant differences on residency, academic performance, and family economic status between the suicidal and non-suicidal groups. Students from urban areas, with poor academic performance, and from families with poorer socioeconomic background were more likely to be suicidal (see Table 1).
As shown in Table 2, there were significant differences between the suicidal and non-suicidal groups for all coping strategies except “Use of emotional support.” The effect size of the coping strategies were between a small and medium level. Table 3 presents ORs and 95% CIs after adjusting for the sociodemographic variables (gender, residency, being an only child, academic performance, family economic status, and religious affiliation). Self-distraction [Adj' OR = 1.09, 95%CI (1.01–1.18)], denial [Adj' OR = 1.23, 95% CI (1.14–1.33)], substance abuse [Adj' OR = 1.33, 95% CI (1.23–1.43)], behavioral disengagement [Adj' OR = 1.32, 95% CI (1.22–1.43)], venting [Adj' OR = 1.10, 95% CI (1.02–1.18)], humor [Adj' OR = 1.17, 95% CI (1.09–1.26)], religion [Adj' OR = 1.15, 95% CI (1.07–1.24)], and self-blame [Adj' OR = 1.28, 95% CI (1.18–1.38)] were significantly more likely to be used by students in the suicidal group. Active coping [Adj' OR = 0.77, 95% CI (0.71–0.83)], use of instrumental support [Adj' OR = 0.90, 95% CI (0.84–0.97)], positive reframing [Adj' OR = 0.82, 95% CI (0.76–0.89)], planning [Adj' OR = 0.84, 95% CI (0.77–0.91)], and acceptance [Adj' OR = 0.90, 95% CI (0.83–0.97)] were significantly less likely to be used by the suicidal group.
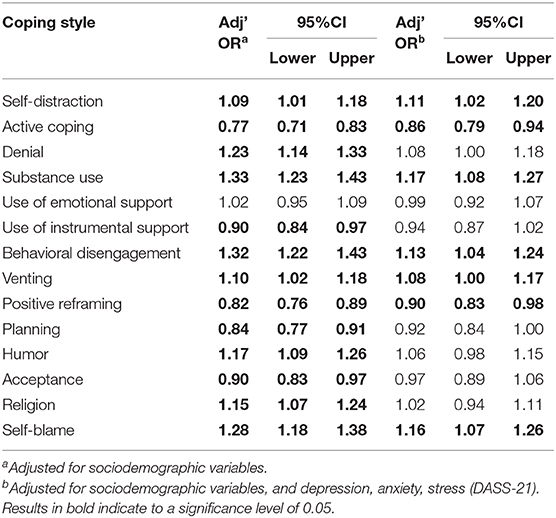
Table 3. Multivariate logistic regression analyses of the association between copying skills and suicidality (suicidal vs. non-suicidal) adjusted for sociodemographic factors and mental health.
Further adjustment for the sociodemographic variables and three dimensions of the DASS-21 (depression, stress, anxiety) showed that self-distraction [Adj' OR = 1.11, 95% CI (1.02–1.20)], substance abuse [Adj' OR = 1.17, 95% CI (1.08–1.27)], behavioral disengagement [Adj' OR = 1.13, 95% CI (1.04–1.24)], venting [Adj' OR = 1.08, 95% CI (1.00–1.17)], and self-blame [Adj' OR = 1.16, 95% CI (1.07–1.26)] remained significantly associated in a positive direction with suicidality. Active coping [Adj' OR = 0.86, 95% CI (0.79–0.94)] and positive reframing [Adj' OR = 0.90, 95% CI (0.83–0.98)] remained negatively associated with suicidality (Table 3).
The present study aimed to better understand the association between specific coping strategies and suicidality using the Brief COPE scale and measures of suicidality in a sample of Chinese university students. A significant association was found. More specifically, after controlling for sociodemographic circumstances, stress, depression, and anxiety, the strategies of active coping and positive reframing were less likely to be used by the suicidal group compared to the non-suicidal group. Self-distraction, substance abuse, behavioral disengagement, venting, and self-blame were more likely to be used by the suicidal group.
Active coping has been found to buffer suicidality (9, 40), and a similar effect has also been shown for positive reframing (19, 41). These are both adaptive coping skills, with active coping referring to actively removing or reducing the stressors, and positive reframing to cognitively constructing a stressful transaction in a positive way (23). The findings of this study suggest that the application of these two coping skills could be beneficial to students in reducing their suicidality. Furthermore, the use of instrumental support, planning, and acceptance were also negatively associated with suicidality after controlling for sociodemographic circumstances, indicating that these coping strategies may also be helpful in reducing suicidality in young people (42).
Several coping strategies related to avoidance, such as behavioral disengagement, self-distraction, venting, and humor, were more likely to be used by suicidal students in the current study; however, previous research has not clearly specified the adaptive or maladaptive effect of these strategies in dealing with stress (23, 43) or suicidality (20). Behavioral disengagement was positively associated with suicidality in our study, echoing results from some earlier studies in late adolescence (29) and in university students (44). Nevertheless, some scholars argue that behavioral disengagement could help reduce the risk of suicidality by temporarily shifting focus away from the stressors, to release negative emotions, and finally to turn back to problem-solving (20, 34).
The results showed that self-blame and use of alcohol and drugs to cope with problems and escape from stress (“substance use” by the Brief COPE scale) were significantly more likely to be used by suicidal students and also showed the highest adjusted OR after controlling for the confounding effects of sociodemographic circumstances, stress, depression, and anxiety. Several studies have demonstrated an association between alcohol and substance use in suicidality (45, 46). Drink to cope could associate with poor problem-solving skills, avoidance coping, and negative urgency in young people who have suicidal risk (47). In addition, a rapid increase in alcohol use in China and alcohol consumption becoming more normalized in recent decades call for further public health actions (48).
Although having a religious affiliation was not significantly different in suicidal and non-suicidal groups, contrary to our expectations, we found “religion” as a coping strategy to be significantly more frequent in the suicidal group. Nevertheless, after controlling for sociodemographic factors, stress, anxiety, and depression, this association became non-significant. It is also important to note that in the Brief COPE scale, the items under “religion” also include spirituality. Cook (49) indicates that there have been mixed results on this topic and argues that those who are spiritual but not religious may not experience buffering or protection against depression or suicidal behavior. Furthermore, remarkable differences in the relationship between religion and suicidality between countries have been reported (50).
It is important to note some of the limitations of this study. Despite a large sample size, a relatively small number of students were identified as having experienced suicidal ideation and attempted suicide. Therefore, we were unable to separately analyze the differences between those who experienced suicidal ideation and those who (also) attempted suicide. The Brief COPE scale helped articulate the coping strategies that the students preferred/applied; however, it is not necessarily comparable with other studies that used different coping scales. Furthermore, the cross-sectional nature of the study limits the analyses to the association between coping styles and suicidality, and does not allow us to determine causality, and we cannot present the effectiveness of each coping strategy (51). It is also important to note that we merged suicidality as measured by SBQ-R, and therefore it may not be applicable specifically to the risk of suicide attempts or suicides. Lastly, the research participants were university students, and therefore the results are not generalizable to all young people in China.
Nevertheless, these results may present some important implications. Using active coping skills to solve problems and developing a positive self-appraisal (52) have been shown to be important for young people facing stressful events and may help to reduce their suicide risks. It is also important to encourage help-seeking from families, peers, and other professionals while having suicidal thoughts (6). In addition, we could help young people to identify the negative impacts of maladaptive coping strategies (such as using drugs or alcohol to manage stress) and replace them with more adaptive coping strategies to reduce the risks of suicide. Programs and services, such as cognitive behavioral therapy (2), mindfulness training to manage stress (53), and routine counseling screening to identify the individuals who rely heavily on avoidance coping (33), could be put in place for young people suicide prevention. The student-friendly university mental health services could also be helpful in connecting students with broader public health resources, and in educating them to cope effectively with academic and life stress (54).
This study provides new insights on the relationship between coping strategies and suicidality in young people. After controlling for the possible confounding effects of sociodemographic circumstances, stress, depression, and anxiety, active coping and positive reframing were negatively associated with suicidality, whereas self-distraction, substance abuse, behavioral disengagement, venting, and self-blame were positively associated with suicidality. There is a need to support young people to develop adaptive and effective coping strategies in order to reduce suicide ideation and attempts.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
The studies involving human participants were reviewed and approved by the institutional review board of the Ethics Committee at the School of Public Health, Shandong University (No. 20161103). The patients/participants provided their written informed consent to participate in this study.
BL, CJ, and KK designed the study. CJ, LY, and BL organized data collection. JL and KK analyzed and interpreted the data. JL and KK were major contributors in writing the manuscript. All authors read and approved the final manuscript.
This work was supported by the Shandong University International Cooperation Fund, under Grant No: 21320005281601, and was partially funded by AsiaCrux Limited (charity organization). Both funding bodies did not engage in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
WHO, World Health Organization; SBQ-R, The Suicidal Behaviors Questionnaire–Revised Scale; DASS-21, Depression, Anxiety & Stress Scale; OR, odds ratio; CI, confidence intervals.
1. Kolves K, de Leo D. Adolescent suicide rates in 1990-2009: analysis of age group 15 to 19 years worldwide. J Adolesc Health. (2016) 58:69–77. doi: 10.1016/j.jadohealth.2015.09.014
2. Robinson J, Hetrick SE, Martin C. Preventing suicide in young people: systematic review. Aust NZ J Psychiatry. (2011) 45:3–26. doi: 10.3109/00048674.2010.511147
3. World Health Organization (WHO). Suicide Data. (2019). Available online at: http://www.who.int/mental_health/prevention/suicide/suicideprevent/en/ (accessed April 25, 2019).
4. World Health Organization (WHO). Preventing Suicide: A Global Imperative. World Health Organization, Geneva (2014). Available online at: http://www.who.int/mental_health/suicide-prevention/world_report_2014/en/ (accessed April 25, 2019).
5. Bertolote JM, Fleischmann A, Butchart A, Besbelli N. Suicide, suicide attempts and pesticides: a major hidden public health problem. Bull World HealthOrgan. (2006) 84:257–336. doi: 10.2471/BLT.06.030668
6. Michelmore L, Hindley P. Help-seeking for suicidal thoughts and self-harm in young people: a systematic review. Suicide Life Threat Behav. (2012) 42:507–24. doi: 10.1111/j.1943-278X.2012.00108.x
7. Chen R, An J, Ou J. Suicidal behaviour among children and adolescents in China. Lancet Child Adolesc Health. (2018) 2:551–3. doi: 10.1016/S2352-4642(18)30170-6
8. Yang LS, Zhang ZH, Sun L, Sun YH, Ye DQ. Prevalence of suicide attempts among college students in China: a meta-analysis. PLoS ONE. (2015) 10:e0116303. doi: 10.1371/journal.pone.0116303
9. Zhang X, Wang H, Xia Y, Liu X, Jung E. Stress, coping and suicide ideation in Chinese college students. J Adolesc. (2012) 35:683–90. doi: 10.1016/j.adolescence.2011.10.003
10. Chang EC, Lucas AG, Chang OD, Duan T, Zhou Z, Yang JZ, et al. Presence of trauma and suicide risk: personal control as a moderator. Death Stud. (2018) 42:529–33. doi: 10.1080/07481187.2017.1411991
11. Dell'Osso L, Bertelloni CA, Di Paolo M, Avella MT, Carpita B, Gori F, et al. Problematic internet use in university students attending three superior graduate schools in Italy: is autism spectrum related to suicide risk? Int J Environ Res Public Health. (2019) 16:1098. doi: 10.3390/ijerph16071098
12. Eskin M, Sun JM, Abuidhail J, Yoshimasu K, Kujan O, Janghorbani M, et al. Suicidal behavior and psychological distress in university students: a 12-nation study. Arch Suicide Res. (2016) 20:369–88. doi: 10.1080/13811118.2015.1054055
13. Hunt J, Eisenberg D. Mental health problems and help-seeking behavior among college students. J Adolesc Health. (2010) 46:3–10. doi: 10.1016/j.jadohealth.2009.08.008
14. Lamis DA, Ballard ED, May AM, Dvorak RD. Depressive symptoms and suicidal ideation in college students: the mediating and moderating roles of hopelessness, alcohol problems, and social support. J Clin Psychol. (2016) 72:919–32. doi: 10.1002/jclp.22295
15. Mortier P, Demyttenaere K, Auerbach RP, Cuijpers P, Green JG, Kiekens G, et al. First onset of suicidal thoughts and behaviours in college. J Affect Disord. (2017) 207:291–9. doi: 10.1016/j.jad.2016.09.033
16. Tang F, Qin P. Influence of personal social network and coping skills on risk for suicidal ideation in Chinese university students. PLoS ONE. (2015) 10:e0121023. doi: 10.1371/journal.pone.0121023
17. Kim SM, Han DH, Trksak GH, Lee YS. Gender differences in adolescent coping behaviors and suicidal ideation: findings from a sample of 73,238 adolescents. Anxiety Stress Coping. (2014) 27:439–54. doi: 10.1080/10615806.2013.876010
18. Endler NS, Parker JD. Assessment of multidimensional coping: task, emotion, and avoidance strategies. Psychol Assess. (1994) 6:50. doi: 10.1037/1040-3590.6.1.50
19. Folkman S, Moskowitz JT. Positive affect and the other side of coping. Am Psychol. (2000) 55:647–54. doi: 10.1037/0003-066X.55.6.647
20. Wang MC, Lightsey OR, Pietruszka T, Uruk AC, Wells AG. Purpose in life and reasons for living as mediators of the relationship between stress, coping, and suicidal behavior. J Posit Psychol. (2007) 2:195–204. doi: 10.1080/17439760701228920
21. Compas BE, Connor-Smith JK, Saltzman H, Thomsen AH, Wadsworth ME. Coping with stress during childhood and adolescence: problems, progress, and potential in theory and research. Psychol Bull. (2001) 127:87–127. doi: 10.1037/0033-2909.127.1.87
22. Skinner EA, Edge K, Altman J, Sherwood H. Searching for the structure of coping: a review and critique of category systems for classifying ways of coping. Psychol Bull. (2003) 129:216–69. doi: 10.1037/0033-2909.129.2.216
23. Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol. (1989) 56:267–83. doi: 10.1037/0022-3514.56.2.267
24. Carver CS. You want to measure coping but your protocol's too long: consider the brief cope. Int J Behav Med. (1997) 4:92–100. doi: 10.1207/s15327558ijbm0401_6
25. Roger D, Jarvis G, Najarian B. Detachment and coping: the construction and validation of a new scale for measuring coping strategies. Pers Individ Differ. (1993) 15:619–26. doi: 10.1016/0191-8869(93)90003-L
26. Ben-Zur H. Coping styles and affect. Int J Stress Manag. (2009) 16:87–101. doi: 10.1037/a0015731
27. Folkman S. Stress: appraisal and coping. In: Gellman MD, Turner JR, editors. Encyclopedia of Behavioral Medicine. New York, NY: Springer (2013). p. 1913–15.
28. Lew B, Huen J, Yu P, Yuan L, Wang DF, Ping F, et al. Associations between depression, anxiety, stress, hopelessness, subjective well-being, coping styles and suicide in Chinese university students. PLoS ONE. (2019) 14:e0217372. doi: 10.1371/journal.pone.0217372
29. Horwitz AG, Hill RM, King CA. Specific coping behaviors in relation to adolescent depression and suicidal ideation. J Adolesc. (2011) 34:1077–85. doi: 10.1016/j.adolescence.2010.10.004
30. Chou WP, Yen CF, Liu TL. Predicting effects of psychological inflexibility/experiential avoidance and stress coping strategies for internet addiction, significant depression, and suicidality in college students: a prospective study. Int J Environ Res Public Health. (2018) 15:788. doi: 10.3390/ijerph15040788
31. Blankstein KR, Lumley CH, Crawford A. Perfectionism, hopelessness, and suicide ideation: revisions to diathesis-stress and specific vulnerability models. JRE CBT. (2007) 25:279–319. doi: 10.1007/s10942-007-0053-6
32. Labelle R, Breton JJ, Pouliot L, Dufresne MJ, Berthiaume C. Cognitive correlates of serious suicidal ideation in a community sample of adolescents. J Affect Disord. (2013) 145:370–7. doi: 10.1016/j.jad.2012.08.027
33. Woodhead EL, Cronkite RC, Moos RH, Timko C. Coping strategies predictive of adverse outcomes among community adults. J Clin Psychol. (2014) 70:1183–95. doi: 10.1002/jclp.21924
34. Miotto P, Preti A. Suicide ideation and social desirability among school-aged young people. J Adolesc. (2008) 31:519–33. doi: 10.1016/j.adolescence.2007.08.004
35. Zhao JB. Influencing of Life Meaning and Cognitive Factors on Suicidal Ideation Among Medical College Students. Guangzhou: Southern Medical University (2006).
36. Osman A, Bagge CL, Gutierrez PM, Konick LC, Kopper BA, Barrios FX. The Suicidal Behaviors Questionnaire-Revised (SBQ-R): validation with clinical and nonclinical samples. Assessment. (2001) 8:443–54. doi: 10.1177/107319110100800409
37. Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales, 2nd ed. Sydney: Psychology Foundation (1995).
38. Tang KN, Chan CS, Ng J, Yip CH. Action type-based factorial structure of Brief COPE among Hong Kong Chinese. J Psychopathol Behav Assess. (2016) 38:631–44. doi: 10.1007/s10862-016-9551-0
39. Cohen J. Statistical Power Analysis for the Behavioral Sciences. New York, NY: Academic Press (1977).
40. Kwok SYC, and Shek DTL. Social problems solving, family functioning, and suicidal ideation among Chinese adolescents in Hong Kong. Adolescence. (2009) 44:391–406.
41. Hirsch JK, Wolford K, LaLonde SM, Brunk L, Parker-Morris A. Optimistic explanatory style as a moderator of the association between negative life events and suicide ideation. Crisis. (2009) 30:48–53. doi: 10.1027/0227-5910.30.1.48
42. Gould MS, Velting D, Kleinman M, Lucas C, Thomas JG, Chung M. Teenagers' attitudes about coping strategies and help-seeking behavior for suicidality. J Am Acad Child Adolesc Psychiatry. (2004) 43:1124–33. doi: 10.1097/01.chi.0000132811.06547.31
43. Lazarus RS. Coping theory and research: past, present, and future. Psychosom Med. (1993) 55:234–47. doi: 10.1097/00006842-199305000-00002
44. Brown SA, Williams K, Collins A. Past and recent deliberate self-harm: emotion and coping strategy differences. J Clin Psychol. (2007) 63:791–803. doi: 10.1002/jclp.20380
45. Gonzalez VM. Association of solitary binge drinking and suicidal behavior among emerging adult college students. Psychol Addict Behav. (2012) 26:609. doi: 10.1037/a0026916
46. Schneider B. Substance use disorders and risk for completed suicide. Arch Suicide Res. (2009) 13:303–16. doi: 10.1080/13811110903263191
47. Gonzalez VM. Factors linking suicidal ideation with drinking to cope and alcohol problems in emerging adult college drinkers. Exp Clin Psychopharmacol. (2019) 27:166. doi: 10.1037/pha0000242
48. Li Q, Babor TF, Zeigler D, Xuan Z, Morisky D, Hovell MF, et al. Health promotion interventions and policies addressing excessive alcohol use: a systematic review of national and global evidence as a guide to health-care reform in China. Addiction. (2015) 110:68–78. doi: 10.1111/add.12784
49. Cook CCH. Suicide and religion. Br J Psychiatry. (2014) 2004:254–5. doi: 10.1192/bjp.bp.113.136069
50. Sisask M, Värnik A, Kolves K, Bertolote JM, Bolhari J, Botega NJ, et al. Is religiosity a protective factor against attempted suicide: a cross-cultural case-control study. Arch Suicide Res. (2010) 14:44–55. doi: 10.1080/13811110903479052
51. Cramer RJ, Braitman A, Bryson CN, Long MM, La Guardia AC. The Brief COPE: factor structure and associations with self-and other-directed aggression among emerging adults. Eval Health Prof. (2019). doi: 10.1177/0163278719873698. [Epub ahead of print].
52. Johnson J, Gooding PA, Wood AM, Tarrier N. Resilience as positive coping appraisals: testing the schematic appraisals model of suicide (SAMS). Behav Res Ther. (2010) 48:179–86. doi: 10.1016/j.brat.2009.10.007
53. Weinstein N, Brown KW, Ryan RM. A multi-method examination of the effects of mindfulness on stress attribution, coping, and emotional well-being. J Res Pers. (2009) 43:374–85. doi: 10.1016/j.jrp.2008.12.008
Keywords: China, coping skills, suicidal behavior, mental health, students
Citation: Liang J, Kõlves K, Lew B, de Leo D, Yuan L, Abu Talib M and Jia C-x (2020) Coping Strategies and Suicidality: A Cross-Sectional Study From China. Front. Psychiatry 11:129. doi: 10.3389/fpsyt.2020.00129
Received: 26 November 2019; Accepted: 13 February 2020;
Published: 13 March 2020.
Edited by:
Maurizio Pompili, Sapienza University of Rome, ItalyReviewed by:
Liliana Dell'Osso, University of Pisa, ItalyCopyright © 2020 Liang, Kõlves, Lew, de Leo, Yuan, Abu Talib and Jia. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cun-xian Jia, amlhY3VueGlhbkBzZHUuZWR1LmNu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.