- 1Department of Psychology, Humboldt University of Berlin, Berlin, Germany
- 2Department of General Psychiatry and Psychotherapy, KRH Psychiatry Wunstorf, Wunstorf, Germany
- 3Department of Economic and Social Psychology, Institute of Psychology, Georg-August-University Goettingen, Goettingen, Germany
- 4Faculty of Physics, Ludwig Maximilian University of Munich, Munich, Germany
- 5Psychiatric Outpatient Clinic, Asklepios Fachklinikum Göttingen, Göttingen, Germany
- 6NTFN e.V., Hannover, Germany
- 7Department of Psychiatry, Social Psychiatry and Psychotherapy, Hannover Medical School, Hannover, Germany
Introduction: Refugees have been shown to be a rather vulnerable population with increased psychiatric morbidity and lack of access to adequate mental health care. By expanding regional psychosocial and psychiatric-psychotherapeutic care structures and adapting psychiatric routine care to refugees’ needs, the state-funded project “refuKey” based in Lower Saxony, Germany, pursues to ease access to mental health care and increase service quality for refugees. A stepped-care treatment model along with intercultural opening of mental health care services is proposed.
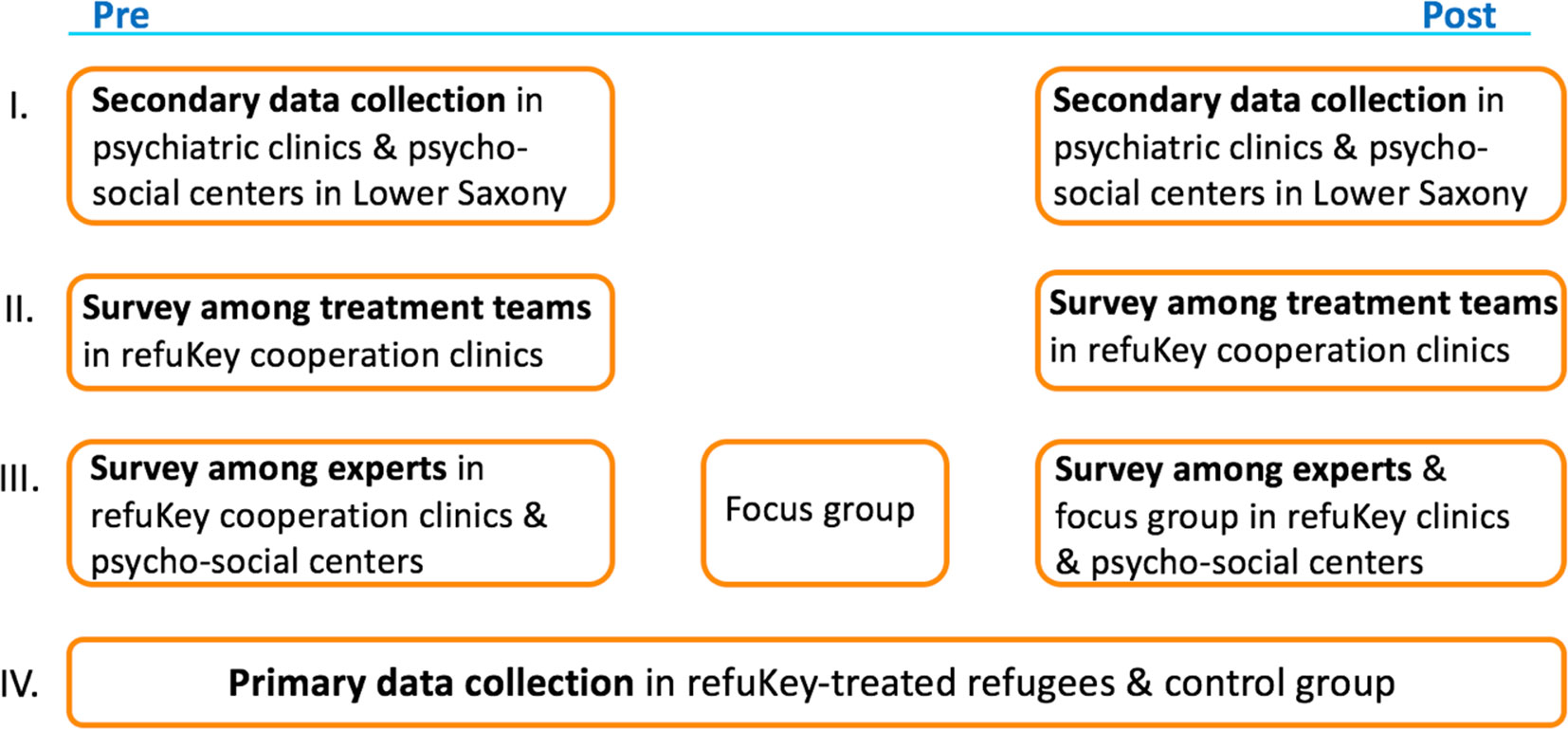
Methods: The project is subject to a four-part evaluation study. The first part investigates the state of psychiatric routine care for refugees in Lower Saxony by requesting data from all psychiatric clinics, participating and non-participating ones, regarding the numbers of refugee patients, their diagnoses, settings of treatment, etc. The second part explores experiences and work satisfaction of mental health care professionals treating refugees in refuKey cooperation clinics. The third part consists of interviews and focus group discussions with experts regarding challenges in mental health care of refugees and expectations for improvement through refuKey. The fourth part compares mental health parameters like depression, anxiety, traumatization, somatization, psychoticism, quality of life, as well as “pathways-to-care” of refuKey-treated refugees before and after treatment and, in a follow-up, to a non-refuKey-treated refugee control group.
Results: RefuKey-treated refugees reported many mental health problems and estimated their mental health burden as high. The symptoms decreased significantly over the course of treatment. Mental health in the refuKey sample was strongly linked to post-migration stressors.
Discussion: The state of mental health care for refugees is discussed. Implications for the improvement and the need for adaptation of routine mental health care services are drawn.
Introduction
Recent years have marked a stark increase in refugees1 leaving their home countries due to conflicts, poverty, and persecution. The numbers for forced displacement are highest on record with 28.5 million globally displaced people in 2018 (1). In 2015, roughly 890,000 asylum seekers arrived in Germany, of whom 441,900 officially applied for asylum, making Germany the most popular host country in the EU (2).
Several studies have shown an elevated risk for mental disorders in samples of refugees (3–5). A recent meta-analysis on refugee mental health reported increased prevalence rates for posttraumatic stress disorder (PTSD; 4.4–86%), depression (2.3–80%), and anxiety disorders (20.3–88%) (3). Compared to studies with small sample sizes, studies of higher methodological quality with large sample sizes generally report lower prevalence rates of mental disorders in refugees (3, 4). Even though prevalence rates should be interpreted with caution due to the heterogeneity of study designs and sample characteristics, there is evidence that refugees constitute a particularly vulnerable population with about 10 times increased risk of PTSD in comparison to the host countries’ native population [e.g., Refs. (3, 4)]. Furthermore, there is a growing body of evidence that the incidence of psychosis in migrant populations is elevated compared to non-migrant population (6). Recent studies further report that risk of developing psychotic disorders is higher for refugees than non-refugee migrants (7, 8).
In this context, research highlights the importance of post migratory factors showing that various stressors related to socioeconomic difficulties in host countries, social and interpersonal challenges, lengthy asylum-seeking process, and complicated immigration policies facilitate long-term mental health problems in refugees after resettlement (3, 9–11). For instance, Knipscheer et al. (12) reported negative effects of the asylum-seeking process on mental health, as they found an association between lack of refugee status and symptom severity of PTSD and depression. Generally, stressful life events that frequently moderate the onset of psychotic disorders might be particularly common among refugees (e.g., migration itself, physical and sexual abuse, perceived discrimination) (9, 13, 14).
Despite the fact that refugees, due to various risk factors, represent a population vulnerable to mental disorders, several structural and social barriers in host countries are preventing this population from receiving adequate mental health care (15). For one, refugees report difficulties in dealing with a foreign, complex health care system (16). Language deficiency represents one of the major access barriers to and a potential source of miscommunication within the health care system, leading to a risk of inadequate clinical assessment (15, 17). Further, the cultural background of an individual might affect symptom patterns, perception of mental disorders, as well as beliefs about mental health care and acceptability of certain treatments (15, 18). Therefore, lack of intercultural competence of mental health care providers, along with the inability to understand the effect of culture on different aspects of mental disorders, present an impediment for adequate health care (19,).
In many countries, including Germany, asylum seekers’ access to health care is limited directly by law. For the first 15 months after arrival in Germany, asylum seekers’ access to health care only covers measures deemed essential for life preservation [e.g., emergency medical care, treatment for acute and painful conditions, care during pregnancy and childbirth, vaccinations; AsylBLG2 sections 4 and 6 (21)]. During this period, regular treatment of mental disorders is not covered. Since 2016, asylum applications are steadily decreasing in Germany (2). However, the current situation still is a great challenge on how to address the needs of refugees for mental health care adequately. In that regard, stepped-care models may provide a promising framework, as they have proven their effectiveness for various disorders in different settings and regions of the world and are recommended for routine care practices (22). Within stepped care, treatment is distributed to several steps with different treatment thresholds, ranging from lower to higher intensities. This enables an optimized provision of mental health care, which takes into account limited clinical and therapeutic resources (22).
The refuKey project aims to enhance regional psychosocial, psychiatric, and psychotherapeutic care services for refugees by means of stepped-care approaches optimizing regular mental health care in Lower Saxony, Germany (23). Within the scope of the refuKey project, psychosocial counseling centers (PCCs) have been founded close to refugee reception centres and joined forces with a psychiatric clinic nearby as cooperating competence centres. The project provides the clinics and PCCs with professional interpreters and academic refuKey staff to support treatment teams in coping with bureaucratic procedures as well as to help reduce diagnostic and therapeutic insecurities in dealing with refugee mental health and to ensure optimal regional networking. The refuKey staff is composed of clinical psychologists, psychiatrists, psychotherapists, and social workers who are trained and experienced in transcultural competence. By integrating low- and high-threshold programs, the refuKey project works to provide need-adapted mental health care for refugees and to promote intercultural opening of the mental health care system. The project started in May 2017 and is a cooperation between the Network for Traumatized Refugees in Lower Saxony (NTFN e.V.) and the German Association for Psychiatry, Psychotherapy, and Psychosomatics (DGPPN). The project is funded by the Ministry of Social Affairs, Health and Equality of Lower Saxony. RefuKey is meant to serve as a model/pilot project for further action. This paper aims to present the first naturalistic data of the refuKey project evaluation study.
Objectives
The study’s objective is to evaluate the efficacy of the project by answering the following three questions: First, do refugees have better access to mental health care as a result of the project? Better access is defined by an increase in the number of refugee patients treated in participating psychiatric clinics and PCCs as well as an increase in referrals between these institutions. Second, is there a decrease in re-hospitalization rates of refugees in participating psychiatric clinics, as well as a significant improvement of the mental state of refuKey-treated refugees as compared to non-refuKey-treated refugees? Third, is there a decrease of work-related strain in mental health care professionals working with refugees over the course of the project in participating psychiatric clinics?
Methods
Study Design
The study uses a complex naturalistic mixed-methods multi-centric design examining different aspects of treatment in four study parts (Figure 1). The first part investigates the state of psychiatric routine care for refugees in Lower Saxony at the start and end of the project. For this, secondary data from all psychiatric clinics in the state, both participating and not participating in refuKey, were requested via an online survey. The aim of the secondary data collection is to measure whether our project can facilitate access to standard psychiatric routine care comparing patient numbers, re-hospitalization rates, and referrals to follow-up treatment between refuKey participating and non-participating clinics. The second part explores the experiences and work-related strain of mental health care professionals involved in mental health care provision for refugees in psychiatric clinics participating in refuKey as well as in a non-participating clinic as a control group, is collected using standardized questionnaires provided at the start and end of the project. Challenges in providing mental health care to refugees and expectations for improvement through refuKey are assessed throughout the project in the third part with structured interviews and focus group discussions. The fourth and main part of the study measures mental health as well as “pathways-to-care” of refuKey-treated refugees before and after treatment using a standardized questionnaire to examine if refuKey treatment is effective. RefuKey treatment outcomes will be compared to a non-refuKey-treated refugee control group to check if refuKey treatment is superior to treatment as usual.
The study was approved by the Ethics Committees of Hannover Medical School and the Medical Association of Lower Saxony.
Sample
For the first study part, chief physicians of psychiatric clinics were recruited via a presentation of the project to the Committee3 of chief physicians of all psychiatric clinics in Lower Saxony and by sending a link to the survey through the committee’s mailing list. Seven clinics participated in the survey.
The sample of the ongoing second study part includes professionals who treat and care for refugee patients in psychiatric clinics participating in refuKey. We ask 10 representatives of a multi-professional team per psychiatric setting covering the professions of psychiatrists; psychologists; occupational, art, music, and body therapists; nurses; and social workers where applicable according to specific settings. A sample of 100 psychiatric clinic employees is planned. All participants are informed about the study by an information sheet and sign the form of consent prior to participation.
In this study part, an expert is defined as someone who works in refugee mental health provision at different levels of delivery within institutions participating in refuKey. The expert sample consists of members of the project steering group, directors of psycho-social centers, clinic directors, clinic personnel, as well as refuKey personnel and counts 14 participants at the start of the project.
Refugees receiving treatment and counseling in refuKey PCCs or psychiatric clinics are included in the sample of the fourth study part. Data collection for this part of the study will continue until the end of the project. Data are collected in four psychiatric clinics (Asklepios Clinic for Psychiatry and Psychotherapy in Goettingen, AWO Psychiatric Centre in Koenigsluther, Karl-Jaspers-Clinic in Oldenburg, Niels-Stensen-Clinics in Bramsche) and five PCCs (Brunswick, Goettingen, Lueneburg, Oldenburg, Osnabrueck) in Lower Saxony, Germany. Written informed consent is obtained from all participants. All participants are informed about the study by an information sheet and sign the form of consent prior to participation.
Refugees who make use of refuKey open counseling hours irregularly as well as refugees who are not capable of filling out a questionnaire due to insufficient educational background or acute mental health conditions (e.g., acute suicidality or acute psychotic symptoms) are excluded from the sample. So far, 171 refugees have participated in the study, while 283 refugees were excluded due to referral to a different mental health institution, transfer to another city, deportation, refusal to participate in the study, or meeting the exclusion criteria. A total of 133 pre-treatment as well as 28 post-treatment measurements including 28 paired pre- and post-treatment measurements were included in the analyses, while 29 participants were excluded due to missing data (Figure 2). Additional information about current symptoms and complaints as well as their severity was available for only 100 of the participants. Data from the control group will be collected as a double-blind study from all refugee patients treated in a psychiatric clinic in Lower Saxony, which does not participate in refuKey at a future point in time.
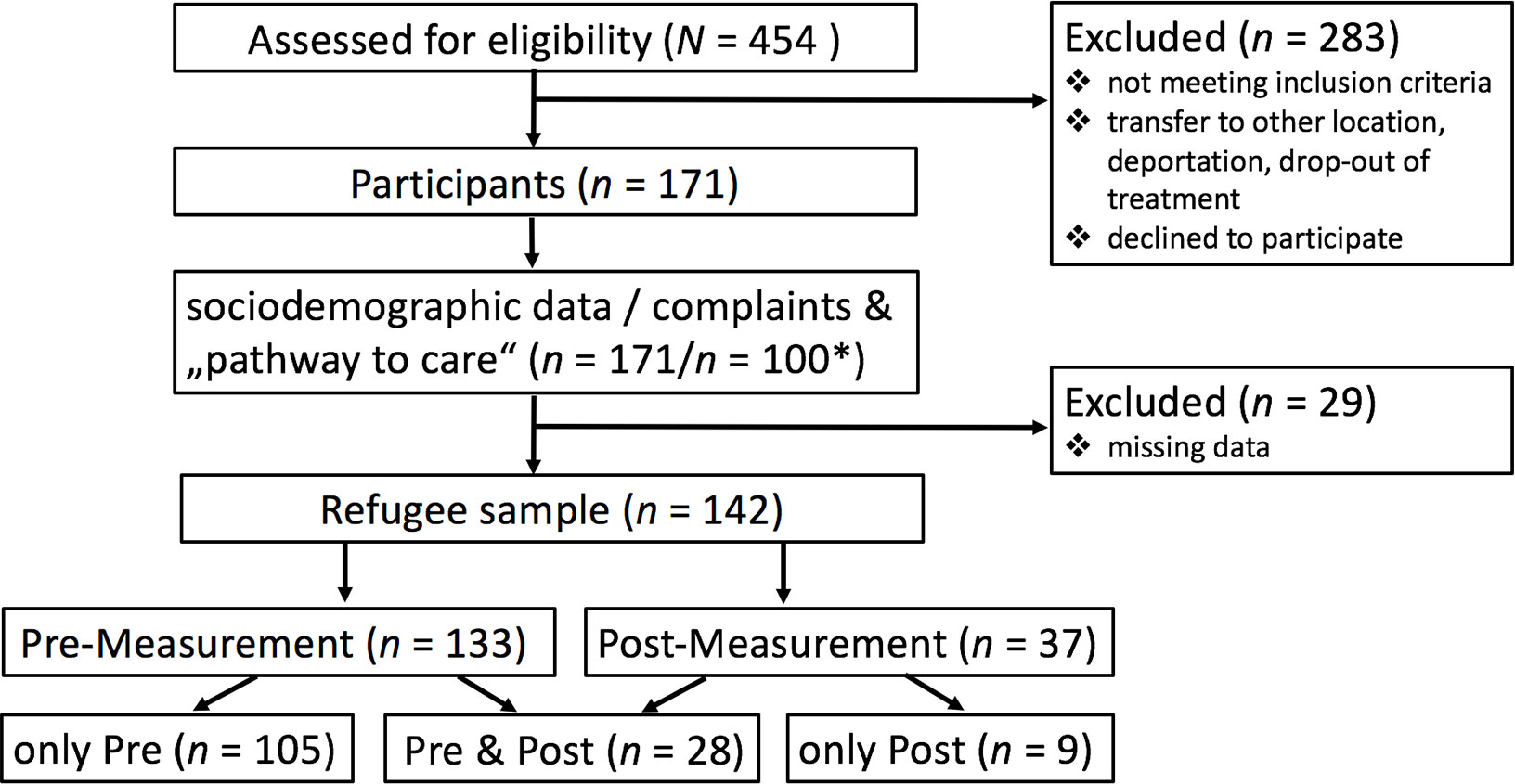
Figure 2 Refugee sample. *Due to the naturalistic design of the study and the hardships of data collection along the treatment process, the information about complaints and “pathway to care” is missing for 71 participants.
Measures
Secondary Data Collection
In the first part of the study, secondary data were collected in psychiatric clinics in Lower Saxony via a short online survey consisting of 11 questions. The survey asked for numbers of refugee patients treated, their diagnoses and reasons for admission, type of diagnostic assessment, settings, types and length of treatment, use of interpreters, re-hospitalization rate, referral to follow-up treatment in the first quarter of 2018, and for a rating of suggested impediments to the quality of mental health care for refugees.
Survey Among Treatment Teams
In the second part, we applied the Maslach Burnout Inventory— Human Services Survey (MBI) by Maslach and Jackson (24) to measure the work-related strain in the care for refugee patients. The MBI consists of 21 items rated from 1 to 6 (1 = “never” to 6 = “very often”). Internal consistency was reported to lie between Cronbach’s α of .71 and .82 (24).
We used the Current Mood Scale (Aktuelle Stimmungsskala, ASTS) by Dalbert (25) to assess personnel’s mood while providing mental health care for refugee and non-refugee patients. The ASTS assesses mood in the categories of sadness, hopelessness, tiredness, anger and positive mood with 19 items on a seven-point Likert scale (1 = “extremely” to 7 = “not at all”). The internal consistency is relatively high (Cronbach’s α = .83–.94) (25).
Additionally, sociodemographic data, such as age, sex, migration background, and occupation, as well as workplace-related data, such as work setting, income, and whether or not refugees are treated, are collected.
Survey Among Experts
The experts in the third part of the study were interviewed using a structured questionnaire composed of open questions asking about challenges in the mental health care of refugees. In particular, they were asked about financial constraints, networks and cooperation, difficulties for treatment teams, and barriers to mental health care access faced by refugees. Expectations about improvements through refuKey were asked about as well.
Primary Data Collection
A standardized questionnaire consisting of validated scales widely used in international refugee research is applied in the fourth part of the study (Health TA Center: Assessment for Trauma and Mental Health in Refugees, www.refugeehealthta.org). The questionnaire is available in eight languages: German, English, Arabic, Farsi, Dari, French, Serbian, and Russian. It contains, if available, validated adaptations of the scales in those languages and, if not, translations into them and back. The questionnaire was tested in a test run.
Mental Health
We assessed the following mental health parameters: general mental well-being with the Warwick Edinburgh Mental Well-Being Scale by Tennant et al. (26), depression and anxiety with the Hopkins Symptom Checklist 25 by Derogatis et al. (27), somatization and psychoticism with the Symptom Checklist 90 by Derogatis (28), traumatization with the Harvard Trauma Questionnaire by Mollica et al. (29), as well as quality of life with the WHO Quality of Life Questionnaire (30).
The Warwick Edinburgh Mental Well-Being Scale (WEMWBS) measures general mental well-being as a sum score of 14 positively worded items rated on a five-point Likert scale. The questionnaire shows high internal consistency (α = .91) (26).
The Hopkins Symptom Checklist 25 (HSCL-25) is a well-known and widely used clinical screening instrument. It assesses anxiety experienced in the last 7 days by means of 10 items and depression by means of 15 items with four categories of response (1 = “not at all,” 2 = “a little,” 3 = “quite a bit,” 4 = “extremely”). Internal consistency is high (α = .89) (31). The scale has been adapted to many languages and has been used with a number of refugee groups.
The Symptom Checklist 90-R (SCL-90) evaluates a broad range of psychological symptoms experienced in the last 7 days rated on a five-point Likert scale. Internal consistency was shown to be at α = .77 for the somatization subscale and α = .73 for the psychoticism subscale (32).
The Harvard Trauma Questionnaire (HTQ) is a cross-cultural screening instrument assessing trauma exposure and its subjective description as well as head trauma and trauma-related symptoms in refugees. In this study, only the last part composed of 30 items regarding posttraumatic symptoms experienced in the last week was administered. The first 16 items reflect the DSM-IV criteria for PTBS and the other 14 items describe trauma-related symptoms. Items are rated on a 1 (“not at all”) to 4 (“extremely”) Likert scale. Internal consistency of the scale is high (α = .96) (29).
The WHO Quality of Life Questionnaire (WHOQoL)—BREF is a short version of the WHO Quality of Life scale, which is cross-culturally applicable. It has 26 items and a response scale ranging from 1 to 5. The questionnaire assesses physical and psychological quality of life, social relationships, and environment. Psychometric properties were tested internationally and have been reported as high (α = .78, α = .89, α = .70, and α = .80, respectively) (33).
Other Factors
Furthermore, we measured current migrant life stressors with the Post-Migration Living Difficulties Checklist (PMLDC) by Silove et al. (34). The 17-item version that we selected is rated on a scale from 1 (“no problem at all”) to 5 (“a very serious problem”) and showed good internal consistency of α = .72 (35). Additionally, the three-item scale for perceived discrimination by Finch et al. (36) was used and adapted to the refugee context (internal consistency: α = .76). The sociodemographic and flight-specific data as well as data about current complaints and help-seeking behavior are assessed with the National Migration Questionnaire by the German Association for Psychiatry, Psychotherapy, and Psychosomatics.
Statistical Analysis
Statistical analyses of the data collected so far were conducted using IBM SPSS Statistics 24 (IBM-Deutschland GmbH, Munich, Germany). Descriptive statistics are given in terms of means and standard deviations for continuous variables, and counts and percentages for categorical variables. Prevalence rates were calculated on the basis of cutoff scores, where applicable. Comparability of the participant and non-participant sample was assessed with analyses of variance (ANOVAs) regarding continuous variables, and with chi-square-analysis (χ2) regarding discrete variables. Descriptive analyses were followed by multivariate analyses of variance (MANOVAs), after having performed power analysis4, comparing the mental state of refugees treated in psychiatric clinics vs. PCC, and by a paired samples t test for a comparison of the refugees’ mental state before and after treatment. Analyses were conducted at a significance level of p = .05. Assumption of normal distribution was tested in the paired sample using the Shapiro–Wilk Test. The data were normally distributed except for psychoticism, somatization, and trauma symptomatic in the post-treatment measurement. In these cases, the Wilcoxon Signed Rank Test was applied in addition to the paired samples t test. Finally, Pearson’s correlation analysis was carried out for the link between post-migration living difficulties and mental health indices.
Results
Secondary Data Collection
The rate of return in this part of the study was relatively low. Of the 32 psychiatric clinics that were approached in the state of Lower Saxony, only 7 completed the survey. Lack of available data about refugee patients in the hospital documentation systems was the major reason for non-participation.
The clinics that did complete the survey reported varying numbers of refugee patients across settings, ranging from 1 to 180 patients in the first quarter of 2018 (see Figure 3).
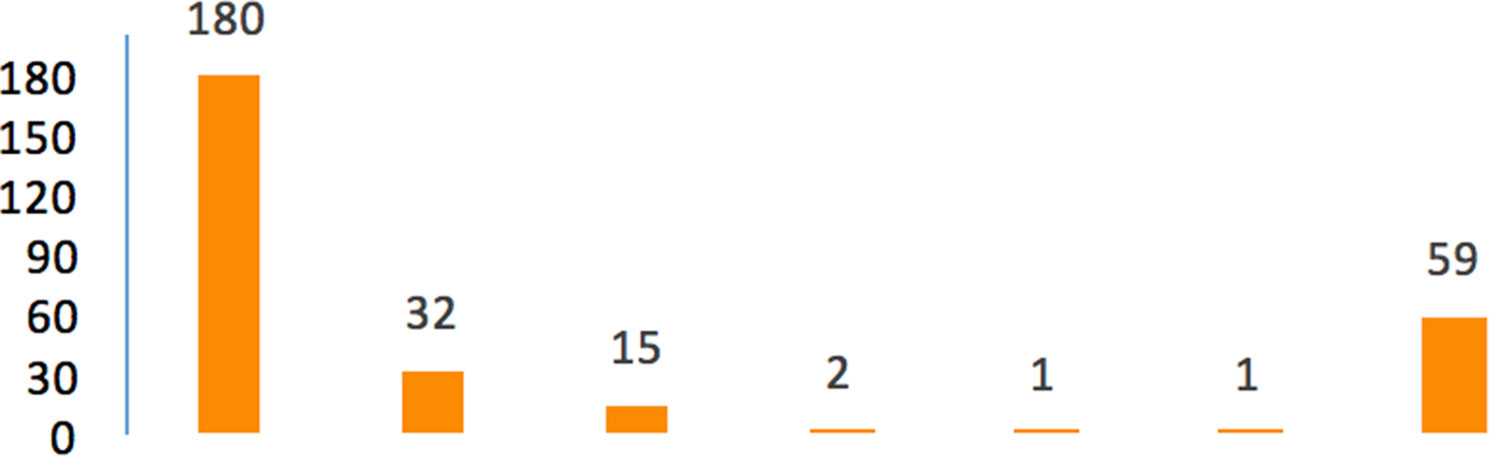
Figure 3 Numbers of refugee patients in seven psychiatric clinics in Lower Saxony in the first quarter of 2018 (N = 7 psychiatric clinics).
The chief physicians of these clinics (N = 5) also rated a given variety of impediments to high-quality mental health care for refugees, i.e., differences in gender roles, institutional racism, time consumption, lack of compliance, lack of trust by the patient, different systems of values, different presentation of symptoms, different understanding of disease, diagnostic uncertainty, and linguistic difficulties. Most notably, out of these, language barriers and lack of sufficient time were reported by all clinics as significant impeding factors. The answers to the other questions in this survey are omitted in this report because of the low return rate.
Survey Among Experts
The impediments to high-quality mental health care for refugees reported by the expert sample match to some extent with those reported by the clinics (see Figure 4). In particular, language barriers and limited personnel resources were among the four most widely reported factors together with the insecure legal status of refugees and bureaucratic workload, which was the most-reported factor of all. The other results of the expert survey fall outside the scope of this article.
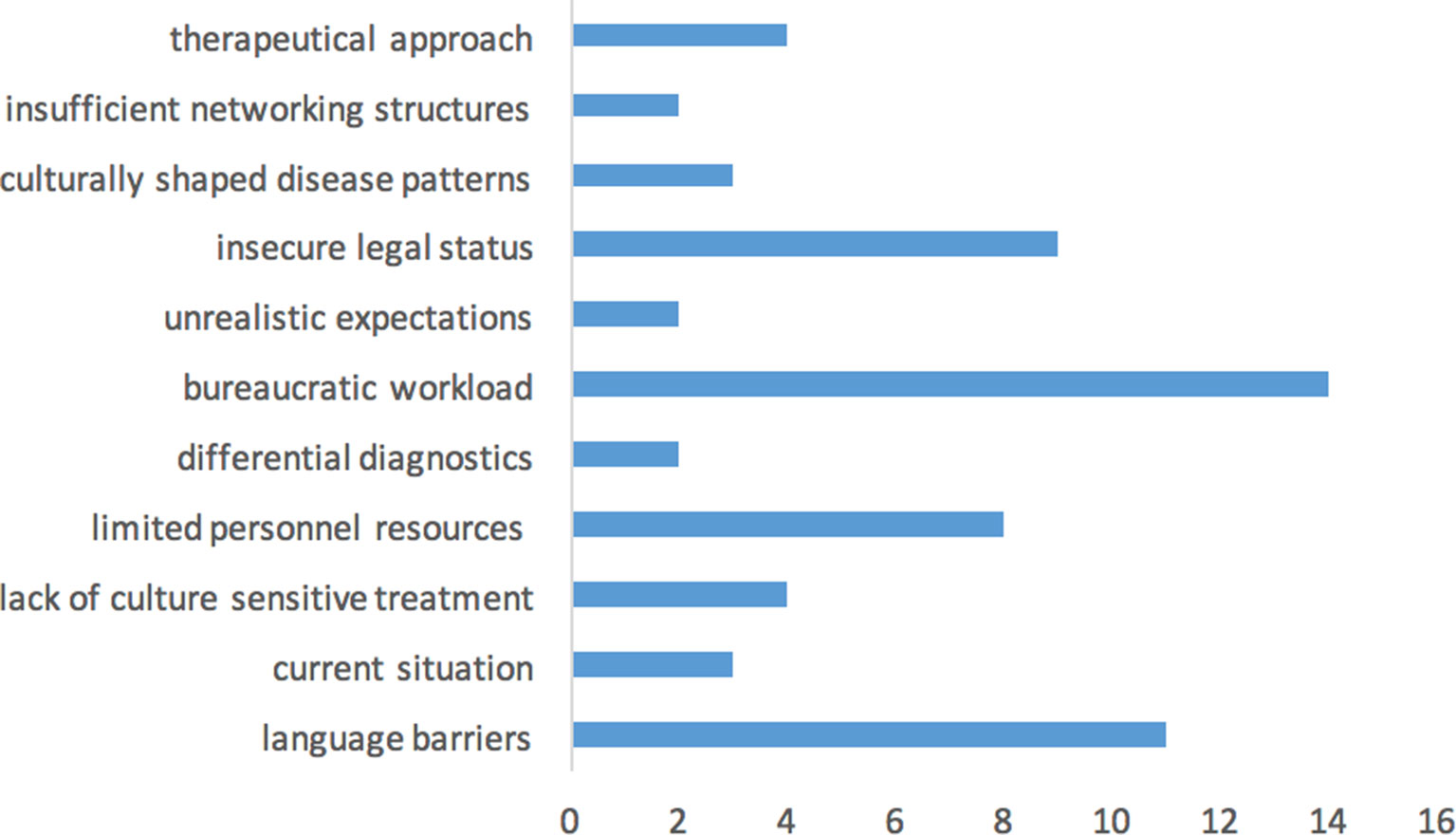
Figure 4 Impediments to high quality of mental health care for refugees and the number of namings (N = 14 experts).
Primary Data Collection
Sociodemographic and flight-specific data reported by the refugees treated or counseled within refuKey-participating institutions are presented in Table 1. The participant sample in this study so far consisted of 54% males and 46% females, with a mean age of 31.07 years. Participants came from 30 different countries of origin, with Afghanistan (15.4%), Iran (14.2%), Syria (8.0%), and Iraq (6.8%) ranking at the top, followed by Kosovo, Lebanon, Turkey, and Sudan (3.1% each). Notably, over 60% of the participants had an insecure residency status (ranging from threat of deportation to having a residence acceptance), while almost one third of participants did not or could not report any information on residence status.
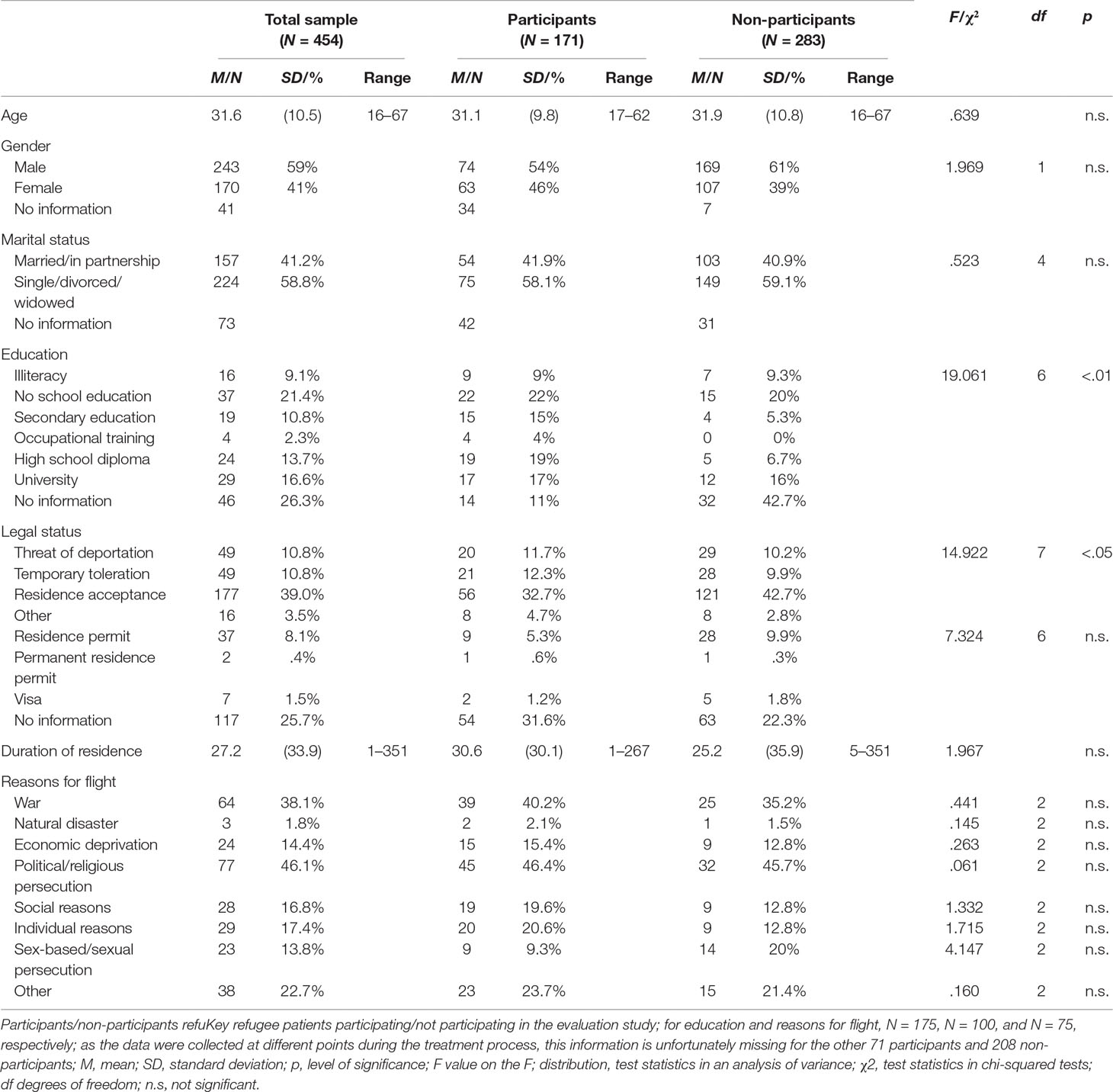
Table 1 Sociodemographic and flight-specific characteristics for participating and non-participating refugee patients (ANOVA and chi-squared analysis).
The refugee patients participating in this study are comparable to those not participating or excluded from the study, in terms of age, gender, and marital status as well as duration of residence and reasons for flight. However, we found significant differences in levels of education [χ2(6) = 19.061, p < .01] as study participants were more educated than non-participants. In terms of legal status, fewer study participants had a residence permit and more are under threat of deportation or are only temporarily tolerated in comparison to non-participants [χ2(7) = 14.922, p < .05].
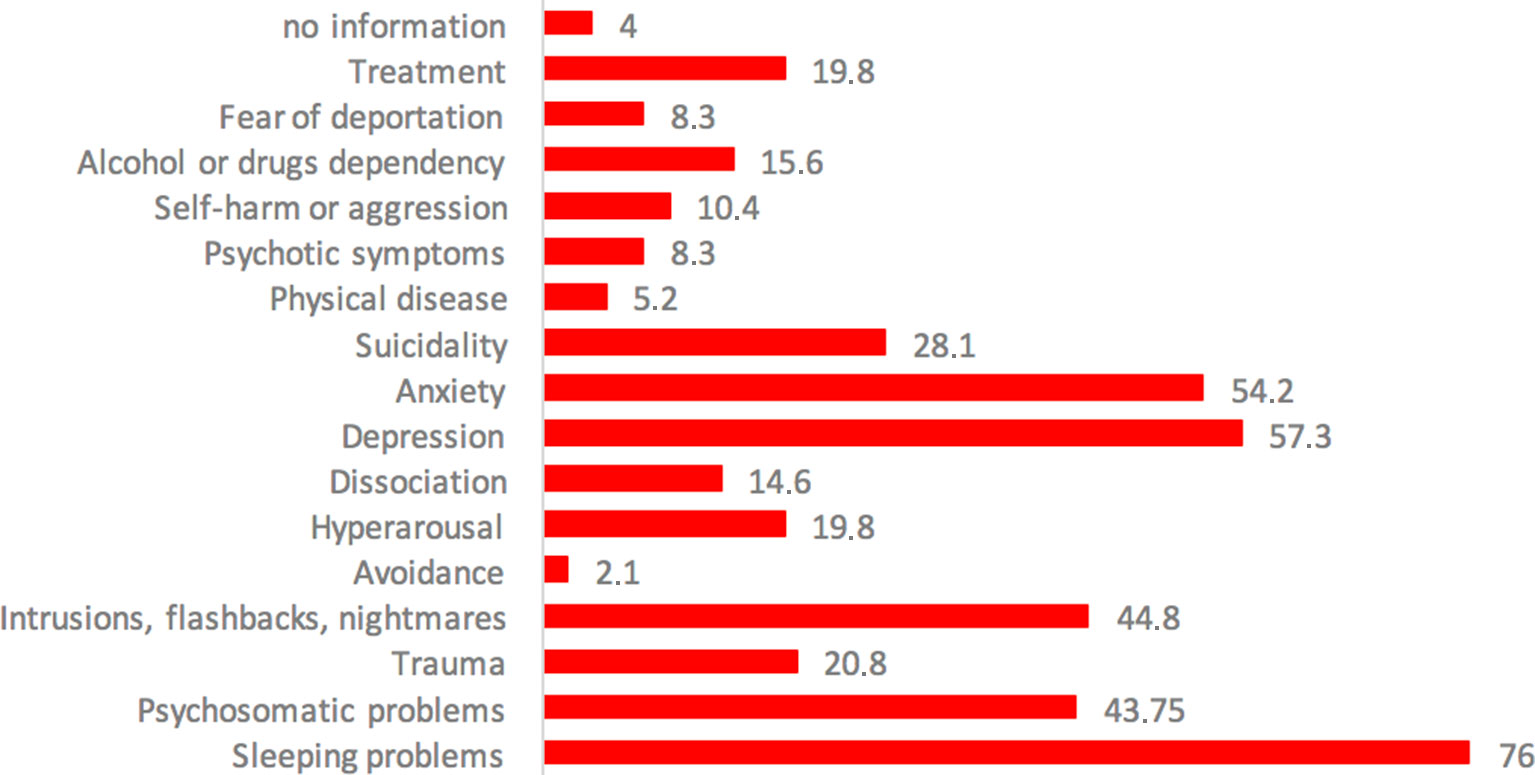
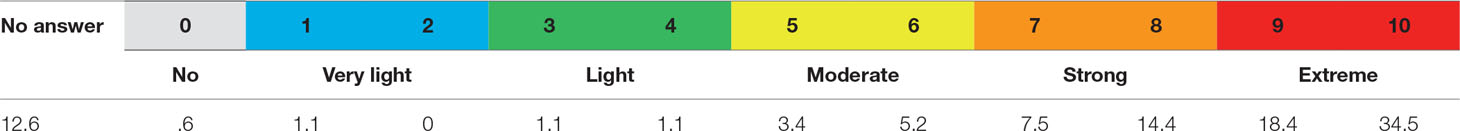
Complaints and symptoms reported by the participants as reason for seeking help in refuKey are given in Figure 5. By far, the most commonly encountered symptom was that of sleeping problems, with three quarters of participants (76%) suffering from it. Furthermore, approximately half of the participants reported symptoms of depression (57.3%), anxiety (54.2%), psychosomatic problems (43.7%), as well as posttraumatic symptoms (44.8%). The mental health burden of refugees in our sample was very high, reflected by participants’ symptom severity estimation shown in Table 2. Three quarters (74.8%) reported strong to extreme symptom severity.
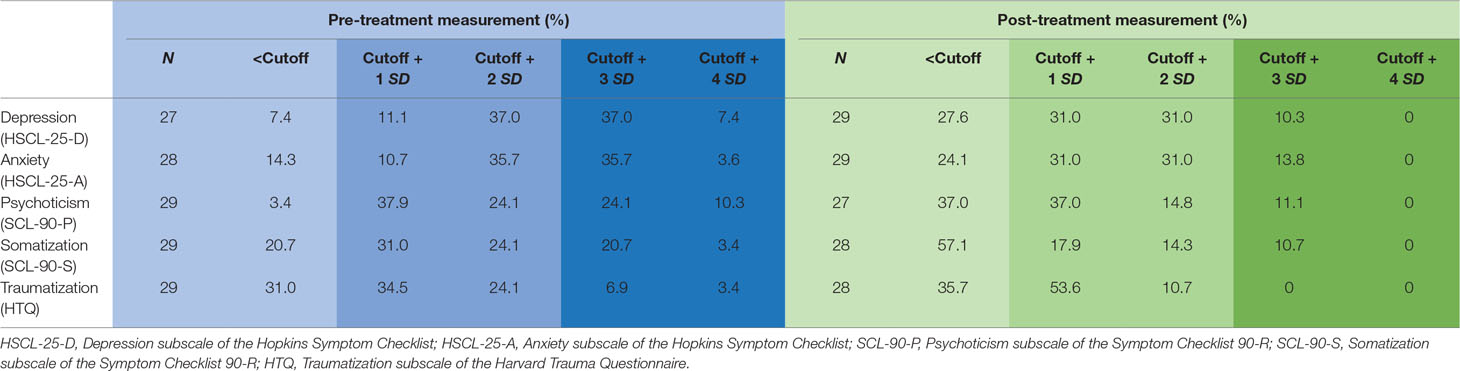
The prevalence of clinically relevant symptoms and their severity decreased in the course of treatment as demonstrated in Table 3. Prevalence rates decreased from 92.6% to 72.4% for depressive symptoms, from 85.7% to 75.9% for anxiety, from 96.6% to 63% for psychoticism, from 79.3% to 42.9% for somatization, and from 69% to 64.3% for traumatization. Prevalence of very severe symptoms went down to zero after treatment.
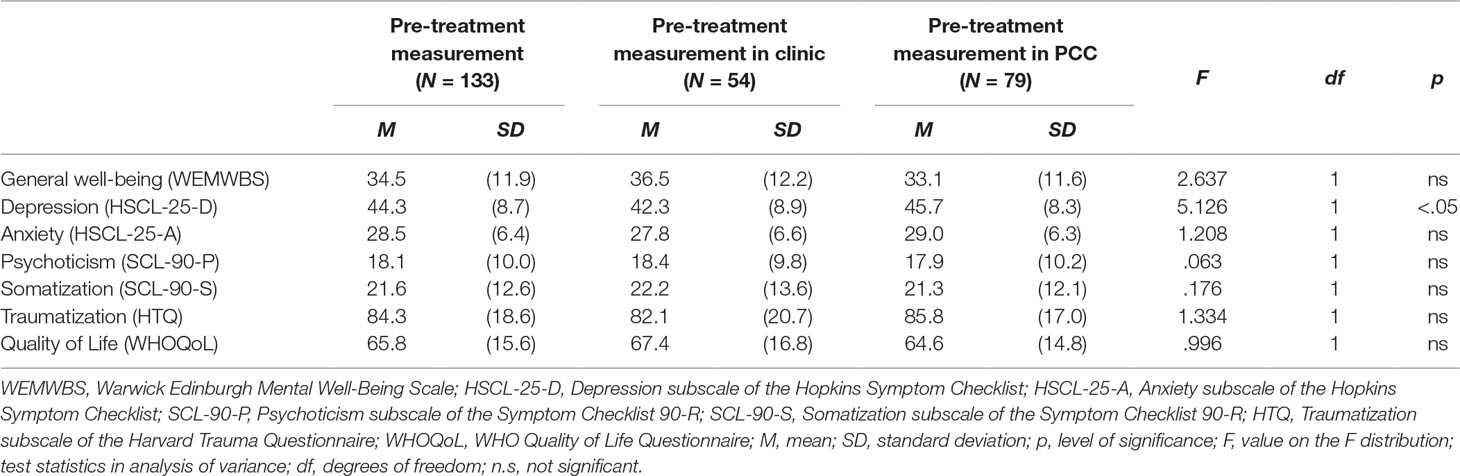
Table 4 compares mental health parameters of participants treated in a clinic and participants treated in a PCC. Pre-treatment values did not differ significantly between clinic and PCC, except for pre-treatment depression values being higher in the PCC sample than the clinic sample (F = 5.126, p < .05).
When comparing post-treatment values to pre-treatment values using a paired t test, we found statistically significant improvements in mental health of refugee patients within refuKey in the aggregated sample (clinic and PCC; see Table 5). Significantly reduced mental health burden with moderate to high effect sizes (Cohen’s d between .5 and 1) was found for the majority of the measured indices including general well-being (t = −2.644, p < .05, Cohen’s d = .499), depression (t = 3.902, p < .001, Cohen’s d = .613), anxiety (t = 3.345, p < .01, Cohen’s d = .751), psychoticism (t = 4.945, p < .001, Cohen’s d = .952), somatization (t = 4.807, p < .001, Cohen’s d = .908), and traumatization (t = 2.529, p < .05, Cohen’s d = .487) but not for quality of life (t = −1.816, n.s.) or post-migration stressors (t = .919, n.s.). Since post-treatment psychoticism, somatization, and traumatization were not normally distributed and our sample size was slightly smaller than 30 (the minimum sample size for which this violation could be ignored), the Wilcoxon Signed Rank Test was applied additionally, showing the same result (p < .001, p < .001, p < .05, respectively). After Bonferroni correction for multiple testing, the improvements were still significant for depression, anxiety, somatization, and psychoticism.
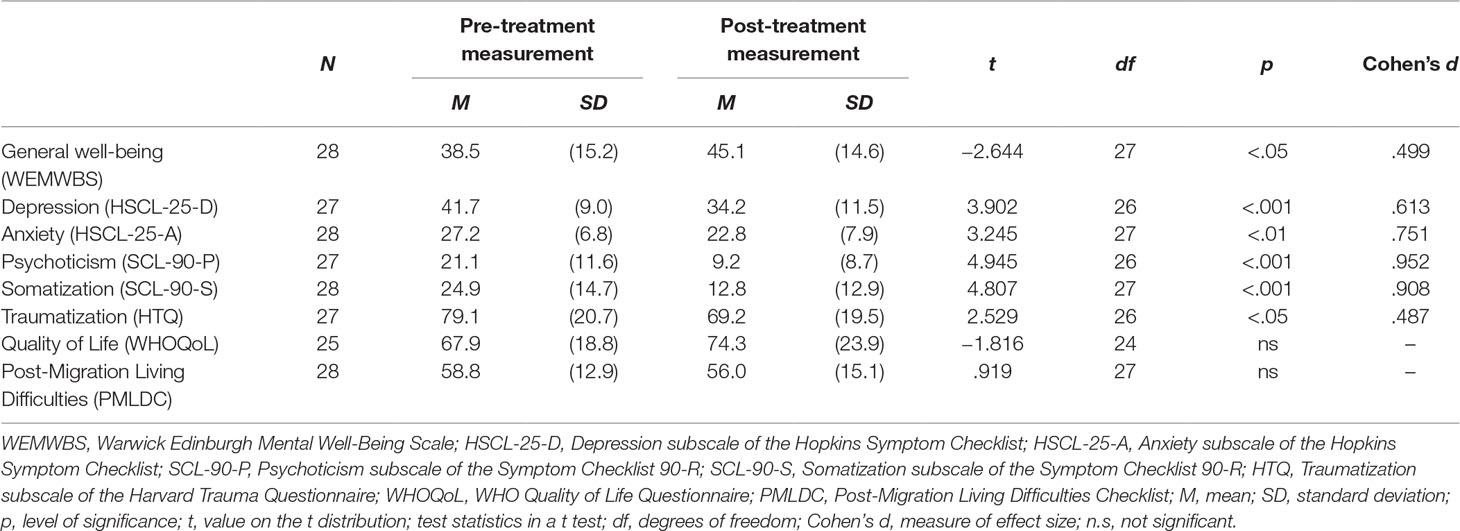
Table 5 Mental health scores of refugee patients before and after treatment within refuKey (paired t test).
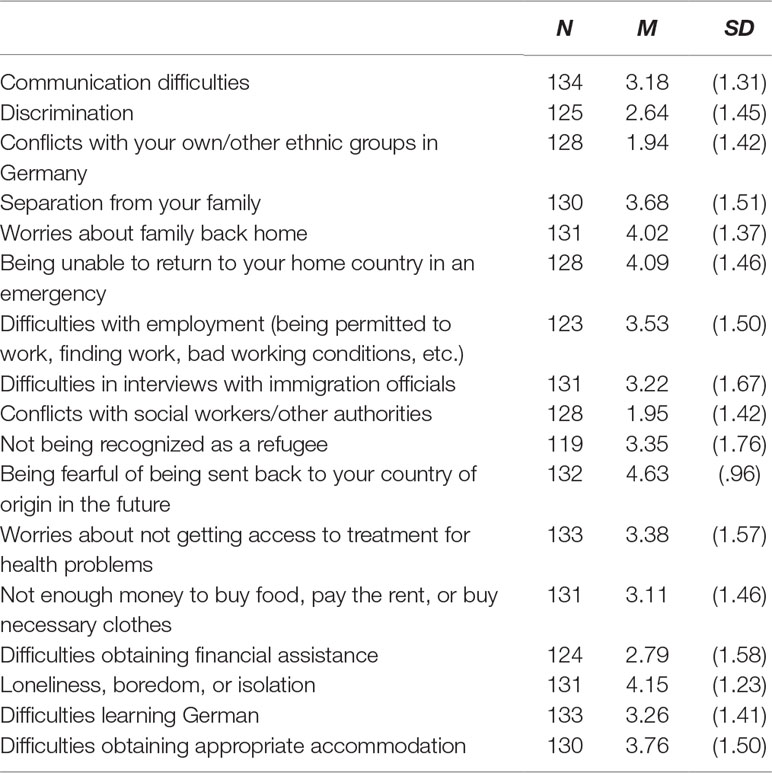
Post-migration living difficulties reported by participants are shown in Table 6. Family issues (separation from family, worries about family back home, inability to return to home country in case of emergency, loneliness), asylum procedure (fear of being sent back to country of origin), and socioeconomic living conditions (difficulties with employment, difficulties obtaining appropriate accommodation) represented major problems for the participants.
Finally, Table 7 presents correlations of the Post-Migration Living Difficulties index with the measured mental health indices. Each of these correlations is both highly significant as well as moderate in strength ranging from r = −.250 for general well-being to r = −.537 for quality of life.
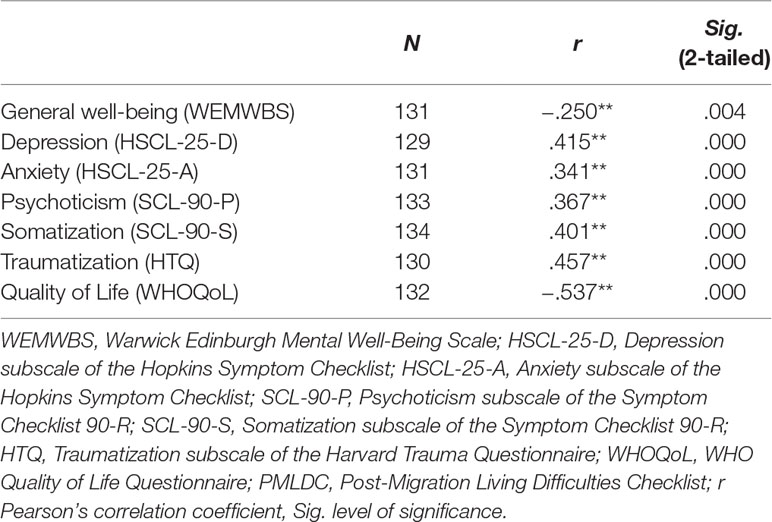
Table 7 Correlation between mental health indices and Post-Migration Living Difficulties Scale (PMLDC, Pearson’s correlation analysis).
Discussion
The present paper describes the implementation and scientific evaluation of the refuKey project in Lower Saxony, Germany. RefuKey aims to reduce cultural and structural barriers to mental health care faced by refugees by using a need-adapted stepped-care approach and to promote intercultural opening in psychiatric routine care by using a multi-centric approach. The refuKey project offers a differentiated support and care model that includes psychiatric and psychotherapeutic treatments as well as psychosocial counseling with the involvement of interpreters, giving refugees low-threshold access to mental health care services. Furthermore, it provides qualified training in transcultural competence, interpreter-assisted psychotherapy, bureaucratic and legal issues, etc. for mental health care professionals and interpreters. With this approach, refuKey incorporates into its mental health care model all the aspects subsequently recommended in a position paper by the National Academy of Science in Germany (37).
Evidence on refugee mental health care in psychiatric settings in Germany is generally quite scarce. Our secondary data survey provides first insight into the current situation of psychiatric-psychotherapeutic routine care for refugees in Lower Saxony, Germany. The survey shows large differences in the numbers of treated refugees between the psychiatrics clinics as reported by chief physicians, suggesting different levels of transcultural opening in these mental health institutions. Another important finding is the lack of systematic documentation of refugees in psychiatric clinics, explaining the low rate of return in our survey. Records about the authority covering the costs of treatment are often the only indication of refugee status of a patient. Furthermore, the authorities responsible for refugees’ health care differ between federal states and change depending on the duration of stay5. Due to these differences, some of the refugees cannot be identified as such in the documentation systems of clinics, which makes it difficult to make inferences about the mental health care of this vulnerable group in Germany. An attempt to standardize the documentation processes in medical institutions in Germany is therefore indispensable for improving intercultural opening and finding new strategies for refugee mental health care.
Additionally, in the secondary data collection, chief physicians of psychiatric clinics reported various barriers with a negative impact on the quality of mental health care of refugees. The most commonly reported barriers were 1) communication problems due to lack of language proficiency and 2) the resulting additional time required for psychiatric assessment. Experts also pointed out several difficulties concerning their work with refugees. These included health care barriers (e.g., insecure residence status, bureaucratic burden, linguistic problems) as well as difficulties associated with characteristics of the refugee population itself (e.g., lack of culturally sensitive treatment options, culturally shaped disease patterns, refugees’ living conditions). These findings are in line with various structural and social barriers faced by refugees in the health care system that are reported in the literature (15). They also highlight the need for an intercultural opening of the health care system that would, for example, include culturally adapted interventions, cultural competence training for mental health care professionals as well as availability of professional interpreters to overcome language barriers, as implemented by the refuKey project.
First preliminary findings on the treatment of refugees within refuKey showed significant improvements (both statistically and in terms of effect sizes) on most general and symptom-specific outcome measures. RefuKey patients displayed increased general well-being and lower depression, anxiety, psychoticism, somatization, and traumatization values at the end of treatment, while perceived quality of life did not increase significantly, which could be ascribed to insufficient statistical power due to small sample size. As the post-migration stressors did not change over the course of the treatment and despite the fact of possible confounders, the improvement in refuKey patients’ mental health might be attributable to the treatment itself. However, a control group is needed to evaluate the specific effectiveness of treatment within refuKey as compared to treatment as usual.
Another important point to emphasize is that refugees admitted to psychosocial counseling centers showed psychiatric symptom severity levels similar to those admitted to psychiatric clinics. In this context, it is especially important to distinguish between the refugees who could be treated solely by psychosocial interventions in the PCCs and those who display more severe symptoms, in order to provide sufficient care for the latter group through cooperation and networking between PCCs and psychiatric clinics. This finding speaks in favor of a need-adapted stepped-care model with cooperating competence centers as implemented in the refuKey project to overcome structural and social barriers. In this sense, experience that will be gained in the course of the refuKey project regarding the close collaboration between PCCs and psychiatric clinics will deepen our understanding of how to implement stepped-care approaches, especially concerning the extent of the needed support and the question of how to overcome access barriers.
Additionally, we examined the relationship between post-migratory living difficulties and indicators of mental health in refugees treated within refuKey and found an association between the two. Specifically, a higher load of post-migration stressors was strongly associated with lower quality of life and moderately associated with lower general well-being. A moderate association of post-migratory living difficulties with more severe syndrome-specific outcomes such as symptoms of depression, anxiety, psychoticism, somatization, and traumatization was similarly observed. Exposure to multiple post-migration stressors combined with psychological resource constraints faced by refugees may lead to poorer mental health and thus explain this association(38). In this study, the main stressors reported by refugee participants were fear of deportation, concerns about family members back home, inability to return home in case of emergency as well as loneliness, boredom, and isolation. Similarly, studies examining the nature of post-migration stressors in samples of asylum seekers reported fear of deportation and concerns about family members back home, but also delays in processing asylum applications, and not having a work permit as main stressors (39, 40). Furthermore, the link between psychoticism and post-migration stressors has been addressed by research showing elevated risk of psychosis not only in first- but also in second-generation migrants (6). Selten and Cantor-Graae, (41) suggest that social defeat, defined as the long-term experience of an outsider status or a subordinate position, might be the mechanism underlying the enhanced risk of psychosis in the respective population.
Interestingly, we found no increase in quality of life after treatment but observed a strong negative association between quality of life and post-migration stressors. This finding might suggest that in contrast to the other mental health measures, quality of life depends more on factors such as post-migration stressors, which are not solely influenced by a psychotherapeutic or psychiatric treatment. Even though our analysis of the former relationship does not allow causal inferences, it seems likely that attempts to reduce post-migration stressors could improve quality of life in refugees. This hypothesis is supported by longitudinal evidence examining distress in refugees in relation to the state of their asylum-seeking process, which revealed a decrease in mental health burden only for those refugees who obtained a positive legal status outcome within the measurement data points (40). Moreover, Laban, Gernaat, Komproe, Schreuders, and De Jong (42) compared recently arrived (<6 months) with long-term (>2 years) asylum seekers and found increased prevalence of psychiatric disorders in the long-term group, which implies an influence of post-migration factors on mental health. Thus, it would be beneficial to the mental health of refugees to reduce post-migration stressors through appropriate administrative changes to the asylum procedure and social policies. Providing culturally adapted and timely mental health care for refugees including support for social integration has also positive socio-political consequences. Integration of refugees to the host country is a manifold and multifaceted process, including adaptation into the educational, labor, health, and community systems and affected by various factors such as pre- and post-migratory experiences and openness of the host society towards cultural diversity (43). Moreover, it has been shown that the psychiatric impairment goes along with poor integration measures in refugees (35). Therefore, early recognition and mitigation of the psychiatric symptoms via culture-sensitive and need-adapted approaches are crucial to promote social integration and psycho-social functioning of the refugees who have to contend not only with their previous traumatic experiences but also with the post-migratory stress factors.
With our primary dataset, we provide a naturalistic overview of various demographic and clinical variables in a help-seeking refugee population. Therefore, our results should not be generalized to refugees outside psychiatric and psychosocial settings. Furthermore, no causal conclusions regarding post-migration factors can be drawn from our data, since it is cross-sectional. Additionally, since this is an ongoing study, the statistical power is still low. Therefore, we could not yet control for covariates within our analysis and cannot exclude that the results are influenced by a third variable (e.g., country of origin, changes in asylum status), so that the results should be interpreted with caution. Self-reports were provided in the patients’ native language to overcome a possible source of bias, which can be regarded as one of the key strengths of our study. It is also important to emphasize that it is challenging to assess the effectiveness of these complex interventions in a way that allows for drawing robust conclusions. For that reason, further evaluation strategies such as prospective comparative methods will be combined with the ongoing evaluation process.
To conclude, this study provides the first scientific naturalistic preliminary dataset from the implementation of an innovative need-adapted stepped-care model project (refuKey) in Lower Saxony, Germany. The existence of structural and social barriers regarding the access of refugees to adequate and high-quality mental health care was discussed. Our data also support findings concerning the impact of the post-migratory living difficulties on mental health and quality of life of refugees. In addition, the need for stepped-care approaches and firm networking between psychosocial centers and psychiatric clinics was underlined. First results suggest a positive impact of the project on the mental health care situation of asylum seekers who seek help from refuKey mental health care services and indicate that the mental health care model implemented by the project might serve as a good adaptation to the needs of refugees.
Data Availability
The datasets generated for this study are available on request to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics committee of the Hanover Medical School. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
BT, LE, IO, and IG-C contributed conception and design of the study. BT, LE, KL, and GP contributed to the acquisition of data. LE organized the database. BT performed the statistical analysis. BT, UA, and JW wrote sections of the manuscript. All authors contributed to manuscript revision, read and approved the submitted version.
Funding
The project and the research for this paper were financially supported by the Ministry of Social Affairs, Health and Equality of Lower Saxony (grant number: 4 SL 1.6.-41583/2017-8).
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank the Network for Traumatized Refugees Lower Saxony (NTFN e.V.) and the German Association for Psychiatry, Psychotherapy, and Psychosomatics (DGPPN) for their support and engagement in the project.
We gratefully acknowledge their support and generosity, without which the project and the present study would not have been possible. We also thank Andreas Pahler for his valuable linguistic contribution to the manuscript.
Footnotes
- ^ In this article, we prefer to use the term “refugees” as an umbrella term, which denotes all asylum seekers regardless of the recognition of their claim.
- ^ Asylum Seekers Benefits Act.
- ^ Psychiatry conference Lower Saxony (Niedersächsische Psychiatrie Konferenz).
- ^ GPower analysis indicated a 93% chance of detecting a large effect size and a 49% chance of detecting a medium effect size (G*Power uses f2 as the effect size parameter (.12 = .01 is small, .252 = .0625 is medium, and .402 = .16 is large) between the two groups as significant at the 5% level (two tailed).
- ^ Within the first 15 months, the authorities determined by federal law are responsible for the provision of health care services for refugees (§4&6 AsylbLG). Afterwards, refugees receive the benefits of health insurance (§2 AsylbLG, §264 SGB V) that are covered by the social welfare office.
References
2. Federal Ministry of the Interior. (2019). Migration Report of the Federal Office for Migration and Refugees by order of the Federal Government - Migration Report 2015. Retrieved from http://www.bamf.de/SharedDocs/Anlagen/DE/Publikationen/Migrationsberichte/migrationsbericht-2016-2017.pdf?__blob=publicationFile
3. Bogic M, Njoku A, Priebe S. Long-term mental health of war-refugees: a systematic literature review. BMC Int Health Hum Rights (2015) 15(1):29. doi: 10.1186/s12914-015-0064-9
4. Fazel M, Wheeler J, Danesh J. Prevalence of serious mental disorder in 7000 refugees resettled in western countries: a systematic review. The Lancet (2005) 365(9467):1309–14. doi: 10.1016/S0140-6736(05)61027-6
5. Steel Z, Chey T, Silove D, Marnane C, Bryant RA, Van Ommeren M. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: a systematic review and meta-analysis. JAMA (2009) 302(5):537–49. doi: 10.1001/jama.2009.1132
6. Bourque F, van der Ven E, Malla A. A meta-analysis of the risk for psychotic disorders among first-and second-generation immigrants. Psychol Med (2011) 41(5):897–910. doi: 10.1017/S0033291710001406
7. Dapunt J, Kluge U, Heinz A. Risk of psychosis in refugees: a literature review. Transl Psychiatry (2017) 7(6):e1149. doi: 10.1038/tp.2017.119
8. Hollander AC, Dal H, Lewis G, Magnusson C, Kirkbride JB, Dalman C. Refugee migration and risk of schizophrenia and other non-affective psychoses: cohort study of 1.3 million people in Sweden. BMJ (2016) 352:i1030. doi: 10.1136/bmj.i1030
9. Li SS, Liddell BJ, Nickerson A. The relationship between post-migration stress and psychological disorders in refugees and asylum seekers. Curr Psychiatry Rep (2016) 18(9):82. doi: 10.1007/s11920-016-0723-0
10. Georgiadou E, Zbidat A, Schmitt GM, Erim Y. Prevalence of mental distress among Syrian refugees with residence permission in Germany: a registry-based study. Front Psychiatry (2018) 9:393. doi: 10.3389/fpsyt.2018.00393
11. Giacco D, Laxhman N, Priebe S. Prevalence of and risk factors for mental disorders in refugees. Semin Cell Dev Biol (2018) 77(5):144–152. doi: 10.1016/j.semcdb.2017.11.030
12. Knipscheer JW, Sleijpen M, Mooren T, Heide FJJ, van der Aa N. Trauma exposure and refugee status as predictors of mental health outcomes in treatment-seeking refugees. BJPsych Bull (2015) 39(4):178–82. doi: 10.1192/pb.bp.114.047951
13. Stepniak B, Papiol S, Hammer C, Ramin A, Everts S, Hennig L, et al. Accumulated environmental risk determining age at schizophrenia onset: a deep phenotyping-based study. The Lancet Psychiatry (2014) 1(6):444–53. doi: 10.1016/S2215-0366(14)70379-7
14. Veling W, Selten JP, Susser E, Laan W, Mackenbach JP, Hoek HW. Discrimination and the incidence of psychotic disorders among ethnic minorities in The Netherlands. Int J Epidemiol (2007) 36(4):761–8. doi: 10.1093/ije/dym085
15. Morris MD, Popper ST, Rodwell TC, Brodine SK, Brouwer KC. Healthcare barriers of refugees post-resettlement. J Community Health (2009) 34(6):529. doi: 10.1007/s10900-009-9175-3
16. Asgary R, Segar N. Barriers to health care access among refugee asylum seekers. J Health Care Poor Underserved (2011) 22(2):506–22. doi: 10.1353/hpu.2011.0047
17. Bauer AM, Alegría M. Impact of patient language proficiency and interpreter service use on the quality of psychiatric care: a systematic review. Psychiatr Serv (2010) 61(8):765–73. doi: 10.1176/ps.2010.61.8.765
18. Kohlenberger J, Buber-Ennser I, Rengs B, Leitner S, Landesmann M. Barriers to health care access and service utilization of refugees in Austria: evidence from a cross-sectional survey. Health Policy (2019) doi: 10.1016/j.healthpol.2019.01.014
19. Betancourt JR, Green AR, Carrillo JE, Park ER. Cultural competence and health care disparities: key perspectives and trends. Health Affairs (2005) 24(2):499–505. doi: 10.1377/hlthaff.24.2.499
20. Schouler-Ocak M, Graef-Calliess IT, Tarricone I, Qureshi A, Kastrup MC, Bhugra D. EPA guidance on cultural competence training. Eur Psychiatry (2015) 30(3):431–40. doi: 10.1016/j.eurpsy.2015.01.012
21. Asylbewerberleistungsgesetz. (n.d.). Retrieved from http://www.gesetze-im-internet.de/asylblg/index.html#BJNR107410993BJNE000109116
22. National Institute for Health Care and Excellence [NICE], 2011. Common mental health problems: identification and pathways to care. Clin Guidel. Retrieved from: https://www.nice.org.uk/guidance/cg123/resources/common-mental-health-problems-identification-and-pathways-to-care-pdf-35109448223173
23. Trilesnik B, Eckhoff L, Özkan K, Loos G, Penteker I, Graef-Calliess IT. Evaluation des Pilotprojektes “refuKey” zur Optimierung der psychiatrisch-psychotherapeutischen Versorgung von traumatisierten Geflüchteten in Niedersachen. DGPPN Kongress, Berlin (2018).
24. Maslach C, Jackson SE, Leiter MP, Schaufeli WB, Schwab RL. Maslach burnout inventory Vol. 21. Palo Alto, CA: Consulting Psychologists Press (1986) p. 3463–4. z
25. Dalbert C. Subjektives wohlbefinden junger erwachsener: theoretische und empirische analysen der struktur und stabilität. Z Differentielle Diagnostische Psychol (1992) 13(4): 207–220
26. Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The Warwick-Edinburgh mental well-being scale (WEMWBS): development and UK validation. Health Qual Life Outcomes (2007) 5(1):63. doi: 10.1186/1477-7525-5-63
27. Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): a self-report symptom inventory. Behav Sci (1974) 19(1):1–15. doi: 10.1002/bs.3830190102
28. Derogatis LR. Symptom Checklist-90-R: administration, scoring & procedure manual for the revised version of the SCL-90. Minneapolis, MN: National Computer Systems (1994).
29. Mollica RF, Caspi-Yavin Y, Bollini P, Truong T, Tor S, Lavelle J. The Harvard Trauma Questionnaire: validating a cross-cultural instrument for measuring torture, trauma, and posttraumatic stress disorder in Indochinese refugees. J Nerv Mental Dis (1992). 180(2): 111–6. doi: 10.1037/t07469-000
30. Whoqol Group. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med (1998) 28(3):551–8. doi: 10.1017/S0033291798006667
31. Thapa SB, Hauff E. Psychological distress among displaced persons during an armed conflict in Nepal. Soc Psychiatry Psychiatr Epidemiol (2005) 40(8):672–9. doi: 10.1007/s00127-005-0943-9
32. Franke GH. Symptom-Checkliste von LR Derogatis: SCL-90-R; deutsche Version. Göttingen: Beltz Test (2002).
33. Bandar NFA, Jani R, Karim MA. Psychometric properties of the WHOQOL-BREF questionnaire among disabled students in Malaysian higher learning institutions. Appl Res Qual Life (2014) 9(3):469–78. doi: 10.1007/s11482-013-9244-8
34. Silove D, Sinnerbrink I, Field A, Manicavasagar V, Steel Z. Anxiety, depression and PTSD in asylum-seekers: associations with pre-migration trauma and post-migration stressors. Br J Psychiatry (1997) 170(4):351–7. doi: 10.1192/bjp.170.4.351
35. Schick M, Zumwald A, Knöpfli B, Nickerson A, Bryant RA, Schnyder U, et al. Challenging future, challenging past: the relationship of social integration and psychological impairment in traumatized refugees. Eur J Psychotraumatol (2016) 7(1):28057. doi: 10.3402/ejpt.v7.28057
36. Finch BK, Hummer RA, Kol B, Vega WA. The role of discrimination and acculturative stress in the physical health of Mexican-origin adults. Hisp J Behav Sci (2001) 23(4):399–429. doi: 10.1177/0739986301234004
37. Leopoldina (Nationale Akademie der Wissenschaften). Traumatisierte Flüchtlinge – schnelle Hilfe ist jetzt nötig. Halle, Germany: Saale. (2018)
38. Ryan DA, Benson CA, Dooley BA. Psychological distress and the asylum process: a longitudinal study of forced migrants in Ireland. J Nerv Mental Dis (2008) 196(1):37–45. doi: 10.1097/NMD.0b013e31815fa51c
39. Begley M, Garavan KC, Condon M, Kelly I, Holland K, Staines A. Asylum in Ireland—a public health perspective. In: Project Report. Department of Public Health Medicine and Epidemiology, University College Dublin, and the Congregation of the Holy Ghost, Dublin (1999).
40. Ryan D, Dooley B, Benson C. Theoretical perspectives on post-migration adaptation and psychological well-being among refugees: towards a resource-based model. J Refugee Stud (2008) 21(1):1–18. doi: 10.1093/jrs/fem047
41. Selten J. Cantor-Graae E. Social defeat: risk factor for schizophrenia? Br J Psychiatry (2005) 187(2):101–102. doi:10.1192/bjp.187.2.101
42. Laban CJ, Gernaat HB, Komproe IH, Schreuders BA, De Jong JT. Impact of a long asylum procedure on the prevalence of psychiatric disorders in Iraqi asylum seekers in The Netherlands. J Nerv Mental Dis (2004) 192(12):843–51. doi: 10.1097/01.nmd.0000146739.26187.15
43. Robila M (2018). Refugees and social integration in Europe, presented at United Nations Expert Group Meeting of the United Nations Department of Economic and Social Affairs (UNDESA) Division for Social Policy and Development, New York, 2018. Retrieved from: https://www.un.org/development/desa/family/wp-content/uploads/sites/23/2018/05/Robila_EGM_2018.pdf
Keywords: mental health, post-migration living difficulties, refugees, stepped-care model, intercultural opening
Citation: Trilesnik B, Altunoz U, Wesolowski J, Eckhoff L, Ozkan I, Loos K, Penteker G and Graef-Calliess IT (2019) Implementing a Need-Adapted Stepped-Care Model for Mental Health of Refugees: Preliminary Data of the State-Funded Project “RefuKey”. Front. Psychiatry 10:688. doi: 10.3389/fpsyt.2019.00688
Received: 20 May 2019; Accepted: 27 August 2019;
Published: 27 September 2019.
Edited by:
Thomas Wenzel, Medizinische Universität Wien, AustriaReviewed by:
Andreas Hoell, Central Institute for Mental Health, GermanyMohammed T. Abou-Saleh, University of London, United Kingdom
Siroos Mirzaei, Wilhelminen Hospital, Austria
Copyright © 2019 Trilesnik, Altunoz, Wesolowski, Eckhoff, Ozkan, Loos, Penteker and Graef-Calliess. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Beata Trilesnik, YnRyaWxlc25pa0BnbWFpbC5jb20=
†These authors have contributed equally to this work and share first authorship
 Beata Trilesnik
Beata Trilesnik Umut Altunoz
Umut Altunoz Janina Wesolowski
Janina Wesolowski Leonard Eckhoff4
Leonard Eckhoff4 Ibrahim Ozkan
Ibrahim Ozkan Iris Tatjana Graef-Calliess
Iris Tatjana Graef-Calliess