- 1Department of Psychiatry, Faculty of Medicine and Health Sciences, University of Stellenbosch, Cape Town, South Africa
- 2School of Public Health, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
- 3Mental Health Project, MRC/UVRI Uganda Research Unit on AIDS/Senior Wellcome Trust Fellowship, Entebbe, Uganda
- 4Department of Psychiatry, Stony Brook University, New York, NY, United States
- 5Department of Global Health and Social Medicine, Harvard Medical School, Massachusetts, MA, United States
- 6Departments of Epidemiology, Infectious Diseases and Microbiology, University of Pittsburgh Graduate School of Public Health, Pittsburgh, PA, United States
- 7Departments of Epidemiology and International Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, United States
- 8Department of Medicine and Centre for Infectious Diseases, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
- 9Department of Psychiatry, Makerere College of Health Sciences, Kampala, Uganda
- 10Department of Population Health, London School of Hygiene and Tropical Medicine, London, United Kingdom
Background: HIV-infected children and adolescents (CA-HIV) face significant mental health challenges related to a broad range of biological and psychosocial factors. Data are scarce on the agreement and discrepancy between caregivers and CA-HIV regarding emotional and behavioral problems (EBPs) in CA-HIV.
Objectives: We determined agreement between self- versus caregiver- reported EBPs and describe factors associated with informant discrepancy among caregiver–youth dyads who participated in the “Mental health among HIV-infected CHildren and Adolescents in KAmpala and Masaka, Uganda” (CHAKA) study.
Methods: In a cross-sectional sample, caregiver-reported EBPs were assessed with the Child and Adolescent Symptom Inventory-5 (CASI-5), and self-reported problems were evaluated with the Youth Inventory-4 (YI-4) in 469 adolescents aged 12–17 years and the Child Inventory-4 (CI-4) in 493 children aged 8–11 years. Adolescents were questioned about experiences of HIV stigma. Caregiver psychological distress was assessed with the Self-Reporting Questionnaire (SRQ-20). Linear regression models were applied to identify variables associated with discrepancy scores.
Results: Self-reported emotional problems (EPs) were present in 28.8% of adolescents and 36.9% of children, and 14.5% of adolescents self-reported behavioral problems (BPs). There was only a modest correlation (r ≤ 0.29) between caregiver- and CA-HIV-reported EBPs, with caregivers reporting more EPs whereas adolescents reported more BPs. Informant discrepancy between adolescents and caregivers for BPs was associated with adolescent age and caregiver’s employment and HIV status. Among adolescents, EP discrepancy scores were associated with adolescent’s WHO HIV clinical stage, caregiver level of education, and caregivers caring for other children. Among children, EP discrepancy scores were associated with child and caregiver age, caregiver level of education, and caregiver self-rated health status. HIV stigma and caregiver psychological distress were also associated with discrepancy, such that adolescents who experienced HIV stigma rated their EPs as more severe than their caregivers did and caregivers with increased psychological distress rated EBPs as more severe than CA-HIV self-rated.
Conclusions: EBPs are frequently endorsed by CA-HIV, and agreement between informants is modest. Informant discrepancy is related to unique psychosocial and HIV-related factors. Multi-informant reports enhance the evaluation of CA-HIV and informant discrepancies can provide additional insights into the mental health of CA-HIV.
Introduction
Of the 36.7 million people living with HIV in 2016, 52.9% (19.4 million) were residing in Eastern and Southern Africa (1). In Uganda in 2016, there were 1.4 million people living with HIV, of which 130,000 were under the age of 15 years (2). Despite the high health care burden of HIV in Sub-Saharan Africa, the majority of studies evaluating the mental health of HIV-infected children and adolescents (CA-HIV) have been conducted in developed regions (3). Generally, studies show that CA-HIV have high rates of medical and psychiatric morbidity (3–7). An earlier review of psychiatric disorders in CA-HIV based on the Diagnostic and Statistical Manual of Mental Disorders (DSM) nosology reported an average prevalence across studies of 28.6% for attention deficit hyperactivity disorder (ADHD), 24.3% for anxiety disorders, and 25.0% for depression (8). When rates of mental health problems are compared to other high-risk groups, such as HIV-exposed but uninfected youth or youth from HIV-affected households (e.g., AIDS orphans or HIV-infected caregivers), results tend to be more mixed (3, 6, 7, 9–12). Studies from African countries with a high prevalence of HIV have also found clinically significant rates of mental health problems. For example, in a Kenyan study, 48.8% of CA-HIV received a DSM-IV-based diagnosis (13), and an earlier cross-sectional Ugandan study in antiretroviral (ARV) naive adolescents found that over half (51.2%) self-reported significant psychological distress, and anxiety (45.6%) and depression (40.8%) were the most common International Classification of Diseases (ICD) psychiatric disorders (14).
CA-HIV from both high-income and resource-limited settings face increased mental health challenges that are related to a broad range of biopsychosocial factors (3, 15), such as overall health status, cognitive functioning, caregiver general health and mental health status, stressful life events, neighborhood stressors, and a lack of social support (3). HIV clinical disease factors, such as CD4 cell count and viral load, have not consistently been linked to poorer mental health outcomes; some studies have reported relations between indicators of HIV progression and mental health problems (16–19), whereas others have found no clear links (5, 10, 20, 21). Further, the presence of psychiatric disorders in CA-HIV has been associated with increased risk behaviors, including substance abuse, treatment non-adherence, and early-onset sexual intercourse (22–25). Stigma, related to being HIV positive, is another factor impacting the well-being of CA-HIV. Meta-analyses have demonstrated that HIV-related stigma is associated with various negative outcomes, including adverse mental health outcomes, such as increased depression, anxiety, and psychological distress (26). Similarly, studies in Africa have demonstrated an association between HIV stigma and increased mental health problems in both adult and adolescent samples (23, 27–29).
There is general consensus that a thorough assessment of child and adolescent mental health problems requires integrating information from various sources, including caregivers, educators, health care providers, and youth self-report (30, 31). Children and adolescents can provide information that may not be known to caregivers such as internal experiences (e.g., thought content, affect) or symptoms and behaviors that occur in contexts where caregivers are not present, such as school or peer interactions (32, 33). Certain problems may be underreported by caregivers, such as abuse and neglect by caregivers, and youth may keep some behaviors hidden from caregivers such as substance use or antisocial behaviors (33). Furthermore, youth self-report can assist in improving accuracy of certain diagnoses, in treatment planning, and in determining the reliability of caregiver information (33). Youth self-report can also provide unique insights into CA-HIV. For instance, in one study, CA-HIV reported elevated depression scores compared to HIV-negative youth, whereas there were no differences by youth HIV status for internalizing or externalizing problems according to caregiver reports (34). Furthermore, a multisite study in CA-HIV and HIV-affected youth found that having received prior mental health interventions was associated with caregiver-reported emotional and behavioral problems (EBPs), but not with youth self-reported EBPs, suggesting that youth self-report may be overlooked in routine practice (35).
Overall, agreement between caregiver-reported and youth self-reported problems is modest at best (32, 36, 37). Studies in CA-HIV have similarly reported low agreement between caregiver and youth self-report (5, 7). The agreement between reports from different informants, while providing information regarding different perspectives and contexts, does not reflect inter-rater reliability (30, 31, 36). For example, research has shown that the correlation between informants does not change much over time, whereas the correlation within informants does change substantially over time (36).
Research has consistently demonstrated discrepancies between different informants about child EBPs (38). As each informant provides a unique contribution to the assessment of EBPs, disagreements that may arise from informant reports can provide more information than when informants agree (36). Discrepancies between caregiver and youth report may provide additional information above each report alone, such as contextual variations in symptoms and treatment response, the individual characteristics of the informants, and features of the caregiver–child relationship (39). For instance, discrepancies in parent- and child self-reported social functioning among youth with autism spectrum disorder provided additional information about parental self-efficacy, youth psychopathology, and treatment response and predicted outcomes better than parent or youth self-report alone (39). Furthermore, another study demonstrated that teacher–adolescent pretreatment discrepancy about prosocial behaviors predicted post-treatment caregiver-rated improvements, whereas the actual ratings of the teachers and adolescents individually did not. Adolescents showed greater improvements according to caregiver report if teachers rated their prosocial behaviors as better than adolescents did themselves, again demonstrating the value of multi-informant report (40).
Discrepancies between caregiver and youth self-reports have been associated with the development of child psychopathology, caregiver stress, and problems in the caregiver–child relationship, although there is no clear patterning between informant characteristics and discrepancies (38). Caregiver psychopathology, and in particular depression, has been one of the most consistent factors associated with informant discrepancy of EBPs (38). Caregivers who are depressed or anxious rate their children’s EBPs as more severe than other informants, such as teachers and youth themselves (38). Furthermore, a meta-analysis revealed that the association between maternal depression and child EBPs was significantly greater if maternal report was used as compared to child self-report, a combination of mother and child self-report, or reports from teachers or others (41). Inconsistencies in the association between caregiver psychological distress and informant discrepancy pertain mainly to specifics, such as whether anxiety or depression is the primary factor contributing to discrepancy or how the child’s age and gender influence the outcomes (38).
EBPs are associated with adverse outcomes among CA-HIV, yet the source of information used to establish their presence is often not taken into consideration. Discrepancy between informants can provide more information than informant reports alone (36, 39). Moreover, informant discrepancies have also been associated with poorer treatment outcomes (42–44). Yet, informant discrepancy of EBPs have not been evaluated among CA-HIV, a group facing additional challenges, such as parental illness, orphanhood, HIV stigma, and HIV disease and treatment-related factors (3, 15, 26). Caregivers of HIV-infected children also face increased challenges, such as financial strain, food insecurity, parenting stress, anxiety, depression, and difficulties pertaining to accessing health care services and treatment adherence (45–49). Studies have also demonstrated discrepancies between caregiver and youth-reported barriers to ART adherence, thus further demonstrating the value of assessing informant discrepancy among CA-HIV (50). Evaluating informant discrepancy of EBPs in CA-HIV can provide further insights into the factors affecting mental health outcomes in CA-HIV and thus help inform treatment strategies.
The primary objective of this study was to better understand the clinical correlates of informant discrepancy between caregiver-reported and CA-HIV self-reported DSM-5-referenced EBPs. To the best of our knowledge, this is the first study to examine the clinical implications of informant discrepancy among CA-HIV. The study sample comprised youth who were participating in the Mental health among HIV-infected CHildren and Adolescents in KAmpala and Masaka, Uganda (CHAKA) study. Specifically, we describe relations between informant discrepancy and a range of sociodemographic and HIV-related factors for the symptoms of a number of common child and adolescent EBPs. Additionally, we investigate the association of HIV stigma and caregiver psychological distress with informant discrepancy. We also report on the prevalence of self-rated EBPs as compared to caregiver-rated EBPs and assessed the level of agreement. Based on existing research (36, 51), we hypothesized that CA-HIV would self-rate a greater number and severity of EBPs than caregivers.
Materials and Methods
Study Design
The CHAKA study assessed the prevalence of, and factors associated with, psychiatric disorders among CA-HIV. Participants were recruited between January 2014 and June 2015. Published manuscripts addressing other research questions emanating from this study can be reviewed for further details (52–55). The study was conducted in accordance with the Declaration of Helsinki and ethical approval was obtained from the Uganda Virus Research Institute’s Research and Ethics Committee, the Ethics Committee of the London School of Hygiene and Tropical Medicine, and the Uganda National Council of Science and Technology.
Setting
A sample of 1,339 child/adolescent–caregiver dyads was recruited from five HIV clinics in central and southwestern Uganda, three in the rural Masaka district (the AIDS Support Organisation clinic, Kitovu Mobile AIDS organisation, and the Uganda Cares clinic) and two in the urban Kampala City Council (Joint Clinical Research Centre and Nsambya Homecare Department). Eligible participants were recruited from each study site consecutively until the required sample size was attained. An equal number of 268 dyads was planned for recruitment at each site. Interviews were conducted in partitioned tents that were erected at each of the study sites to ensure privacy and limit distraction.
Participants
CA-HIV between 5 and 17 years of age with caregivers older than 17 years of age were included. Additionally, participants were included if both caregivers and CA-HIV could speak English or Luganda (the local language spoken in the study areas), and they remained in the study’s geographical area for the subsequent 12 months. Participants were excluded if they were concurrently enrolled in another study, if they were unwell and in need of immediate medical attention, and if they did not understand the study instruments for any reason. Furthermore, to be able to address the objectives of this study, we only included CA-HIV who had completed the self-report measures for EBPs. Eligible study participants provided written informed consent (caregiver) and assent (CA-HIV) after explanation of the study objectives and procedures. No CA-HIV were enrolled without their assent, and all participants were informed that they could withdraw without prejudice at any time. In the majority of cases, the parents provided informed consent for participation of the CA-HIV, but in cases where the primary caregivers were not parents, the guardians of the CA-HIV provided the informed consent. Approximately 2% of participants assessed for eligibility were not included due to factors such as caregiver refusal, CA-HIV refusal, inability to contact the caregiver to obtain consent, and ongoing participation in another study.
Procedure
The assessment battery comprised structured, standardized, and locally translated instruments. Measures not previously used in Uganda were forward and back translated and locally adapted and piloted before use (52, 55). Assessments were administered by trained psychiatric nurses and psychiatric clinical officers and supervised by a psychiatrist and a clinical psychologist. All measures used were read to participants to accommodate for variation in reading level. Participants diagnosed with putative psychiatric disorders were provided with psychoeducation and referred to local mental health care services. A demographic questionnaire was designed to obtain sociodemographic information of caregivers and CA-HIV [e.g., age, gender, employment status, highest level of education (HLOE), caregiver relationship to child] and a medical questionnaire to obtain data regarding caregiver and child health status (e.g., nadir CD4, current CD4, ART status, caregiver HIV status).
Measures
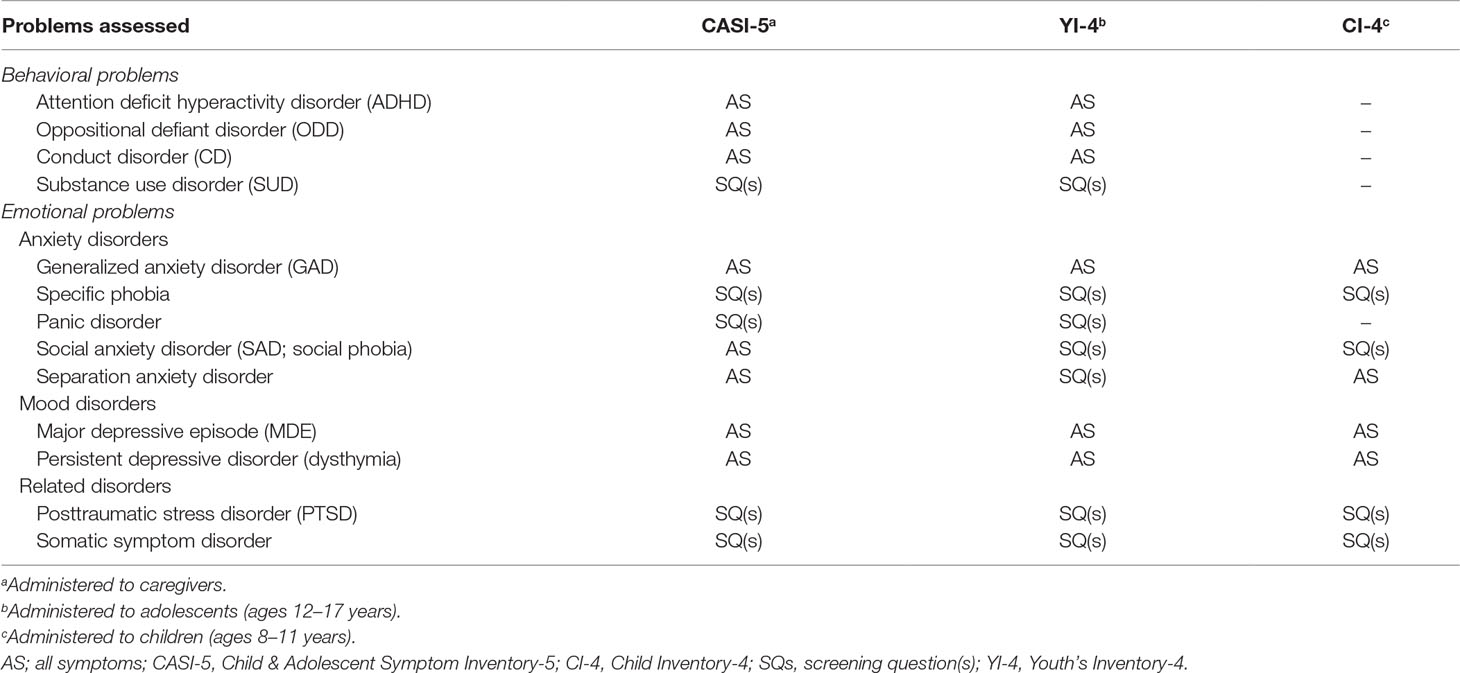
Emotional and Behavioral Problems
Caregivers completed the parent version of the Child & Adolescent Symptom Inventory-5 (CASI-5) (56), which includes the symptoms of DSM-5 psychiatric disorders among youth aged between 5 and 18 years old. Symptoms are rated on a four-point Likert scale (0—never, 1—sometimes, 2—often, 3—very often) with an impairment rating (rated on the same Likert scale as symptoms) for each disorder. The CASI-5 can be utilized to obtain a symptom cutoff score (number of symptoms required for a DSM-5 diagnosis rated “2” or higher), an impairment cutoff score (impairment rated “2” or higher, regardless of number of symptoms), a clinical cutoff score (has to fulfill both symptoms cutoff and impairment cutoff scores), and a symptom severity score (dimensional model). The symptom severity scores are calculated by adding the individual ratings of each of the symptoms for each disorder. We evaluated for the presence of EBPs utilizing the symptom cutoff score (see Table 1) and used the severity scores to calculate discrepancy on EBPs. The CASI has been used in hundreds of studies (57), including in HIV-positive youth (7), and has demonstrated satisfactory psychometric properties, including internal consistency (Cronbach’s α between 0.45 and 0.92), test–retest reliability (r > 0.65), and convergent, divergent, and discriminant validity in various settings (58–61). The CASI-5 was adapted for use in the local Ugandan setting (52) and internal consistency was satisfactory (Cronbach’s α between 0.70 and 0.85) (55).
Adolescents between 12 and 18 years old completed the Youth’s Inventory-4 (YI-4) (62), which is a self-report measure of DSM-referenced symptoms. The YI-4 comprises 120 items that correspond to items in the CASI-5 and is rated and scored in a similar way to the CASI-5. The YI-4 has demonstrated satisfactory internal consistency (Cronbach’s α between 0.66 and 0.87) and test–retest reliability (r between 0.54 and 0.92) and aligns well with other self-report measures and clinical diagnoses (33). Internal consistency in this study was also fair (Cronbach’s α between 0.49 and 0.88) (55).
The Child Self-Report Inventory-4 (CI-4) (63) is a parallel self-report measure for use with children aged between 8 and 11 years and includes 34 items that are phrased and rated similarly to the YI-4 and CASI-5, but does not include an impairment rating. The CI-4 rates only for EPs (Table 1), and thus, for the child sample, results are limited to EPs. Formal validation studies have not yet been published regarding the CI-4, although it has been used in other studies of HIV-positive children (61, 64). In this sample, the internal consistency of disorders assessed (Cronbach’s α between 0.62 and 0.79) as well as the full scale (Cronbach’s α = 0.89) was satisfactory.
Caregiver Psychological Distress
The Self-Reporting Questionnaire (SRQ-20) (65) is a brief measure developed by the WHO to screen for common mental problems, such as depression and anxiety, in developing countries. Respondents indicate the presence or absence of 20 symptoms in the prior month by answering yes (scored 1) or no (scored 0) to each item. Items are summed to provide a total score (range 0–20), with higher scores indicating greater symptomatology. The SRQ-20 has been translated and validated for use in Uganda and demonstrated good internal consistency (Cronbach’s α = 0.84) and moderate test–retest reliability (κ = 0.48), and a cutoff score of ≥6 identified current depression with a sensitivity of 84% and specificity of 93% (66). The SRQ-20 was administered to caregivers to assess psychological distress and demonstrated good internal consistency (Cronbach’s α = 0.83).
HIV Stigma
To assess for HIV-related stigma, adolescents were asked five questions (yes/no) pertaining to stigma experienced in the prior year. The questions asked about i) being teased at home because of HIV status, ii) being teased at school/work because of HIV status, iii) being discriminated at home because of HIV status, iv) being discriminated at school/work because of HIV status, and v) having lost friends because of HIV status. Adolescents responding “yes” to any of the questions were regarded as having experienced HIV stigma in the prior year (yes/no).
Clinical Correlates
Child/adolescent characteristics: Gender (male/female), age (continuous in years), and whether the child missed any days of school in the last term (yes/no).
Household characteristics: Study site (rural/urban), who the child lives with (two parents, single parent, grandparents, other), food security (based on whether the household had enough food to eat in the prior month, yes/no), and socioeconomic index based on common household items (0–2, 3–4, 5–6, 7–9 items) constructed for use in Uganda (67) (including the following items: electricity, a car, a motorcycle, a bicycle, a radio, a telephone, a refrigerator, a cupboard, and a flask).
HIV characteristics: Whether the child was born with HIV (yes/no), nadir CD4 cell count (<200, 200–349, 350–499, 500+ cells/mm3), current CD4 cell count (< 200, 200–349, 350–499, 500+ cells/mm3), reported WHO HIV clinical stage (stage 1, stage 2, stage 3, stage 4), currently on antiretroviral treatment (ART, yes/no), possible virological treatment failure (current viral load > 1,000 copies/ml, yes/no), whether the adolescent missed any ARV doses in the past 3 days (yes/no), and whether HIV status has been disclosed to the child (yes/no).
Caregiver characteristics: Gender (male/female), age (continuous in years), caregiver status (mother, father, grandparent, other), employment (yes/no), HLOE (no formal education, primary education, secondary education, tertiary education), marital status (cohabiting, widowed, separated, single), caregiver also caring for other children (yes/no), caregiver HIV positive (yes/no), and caregiver health status (poor or average, good or very good).
EBPs: Rates of individual EBPs (as listed in Table 1) based on symptom cutoff scores on diagnostic measures are reported. Emotional problems (EPs) were considered present if the child or adolescent fulfilled symptom criteria for at least one EP. Behavioral problems (BPs) were considered present if the adolescent fulfilled symptom criteria for at least one BP. Similar to other studies that have used diagnostic tools (68, 69), we calculated total severity scores for EPs and BPs by adding the severity scores for the individual disorders (as presented in Table 1). With this approach, each symptom assessed would contribute equally to overall severity; however, total severity scores could be more heavily influenced by disorders with a greater number of symptoms. We, therefore, also calculated averaged total severity scores by dividing the severity score for each disorder by the number of symptoms assessed, which we used to conduct sensitivity analysis. By using averaged severity scores, each disorder would contribute equally to overall severity; however, disorders that were assessed with limited screening questions would be weighted equivalently to disorders that had been assessed in full.
Statistical Analysis
The sample size of 1339 was based on an estimated prevalence of at least one psychiatric disorder of 25% with a precision of around 2.5%. Analyses were conducted separately for the child and adolescent samples as they completed different self-report questionnaires; “adolescents” aged 12–17 years completed the YI-4 and “children” aged 8–11 years completed the CI-4. Descriptive data include rates (%) of self-rated and caregiver-rated EBPs and sociodemographic and clinical variables (as specified above). We compared the rates reported by the caregivers and CA-HIV by conducting chi-square or Fisher’s exact tests as indicated.
Agreement between caregiver- and youth self-rated disorders was evaluated with the kappa statistic based on symptom cutoff scores (i.e., categorical) and Pearson correlation coefficients for severity scores (i.e., dimensional). To measure the discrepancy between caregivers and CA-HIV, we used a recommended approach by calculating standardized difference scores (69). We transformed each informant’s total EP and total BP severity scores into z scores. We subtracted the z score obtained for the CA-HIV from the z score obtained for the caregivers to obtain the standardized difference (discrepancy) score for EPs and BPs. Positive scores indicate caregivers rating problems as more severe and negative scores indicate CA-HIV rating problems as more severe. We repeated the same process using averaged severity scores to compute the discrepancy scores, which were used in sensitivity analyses.
To identify clinical and sociodemographic factors that were associated with discrepancy between caregivers and CA-HIV on EPs or BPs, t tests and analyses of variance (ANOVAs) were conducted for categorical variables and Pearson correlation coefficients for continuous variables. Variables with a p value of less than 0.1 were entered into multiple linear regression models to assess factors that each best predicted the discrepancy between caregivers and CA-HIV of EPs and BPs. CA-HIV age and gender were included in each of the models, even if their p values were not significant on univariate analyses. To assess for the effects of HIV stigma and caregiver psychological distress on discrepancy scores, we added the variables “experienced HIV stigma” and “SRQ-20 total score” as an additional step to the final model. We conducted sensitivity analyses by repeating the regression models, but with discrepancy scores based on averaged severity scores as the dependent variables. We did not correct for multiple comparisons due to the exploratory nature of the analyses. Analyses were conducted using SPSS version 25 software package (SPSS Inc., Chicago, IL), and all tests were two-tailed with the alpha (α) set at 0.05.
Results
Participants and Descriptive Data
The overall sample of 1,339 included 351 children under the age of 8 years who did not qualify for inclusion in this study, as they were too young to complete the CI-4. We excluded one adolescent aged 18 years and three CA-HIV for whom age data were missing. We excluded a further 18 children who had not completed the CI-4 and four adolescents who had not completed the YI-4. Our final sample included 493 children who had completed the CI-4 and 469 adolescents who had completed the YI-4. CASI-5 data were missing for 28 (5.9%) adolescents, and five (1.0%) children were excluded from the analysis as the caregivers who completed the CASI-5 were not above the age of 17 years. Factors associated with adolescents who were excluded (n = 33, 7.0%) were older age [t(472) = 3.1, p = 0.002], urban study site [χ²(1) = 25.9, p < 0.001], a higher socioeconomic index [χ²(3) = 8.0, p = 0.047], caregivers interviewed not the parents or grandparents [χ²(3) = 24.7, p < 0.001], and caregivers being employed [χ²(1) = 5.3, p = 0.021]. Factors associated with children who were excluded (n = 23, 4.5%) were urban study site [χ²(1) = 10.7, p = 0.001], WHO clinical stage 1 or 2 [χ²(3) = 8.0, p = 0.046], caregiver younger [t(472) = −2.5, p = 0.012], and caregiver not HIV positive [χ²(1) = 4.1, p = 0.042].
The mean age of CA-HIV was 11.9 (SD = 2.6) years, and 52.9% of CA-HIV were female. The majority of CA-HIV (94.2%) were perinatally infected and were receiving ART (95.4%). Eighty-seven (19.7%) of the adolescents reported experiencing HIV-related stigma in the prior year, with 31 (7.0%) answering “yes” to two or more questions. Of the caregivers assessed, 177 (19.1%) scored ≥6 on the SRQ-20 (the threshold indicating possible depression in the Ugandan validation study), and the median score on the SRQ-20 was 4.0 (IQR 0.0; 4.0). For detailed descriptive data, see Tables 3 and 4.
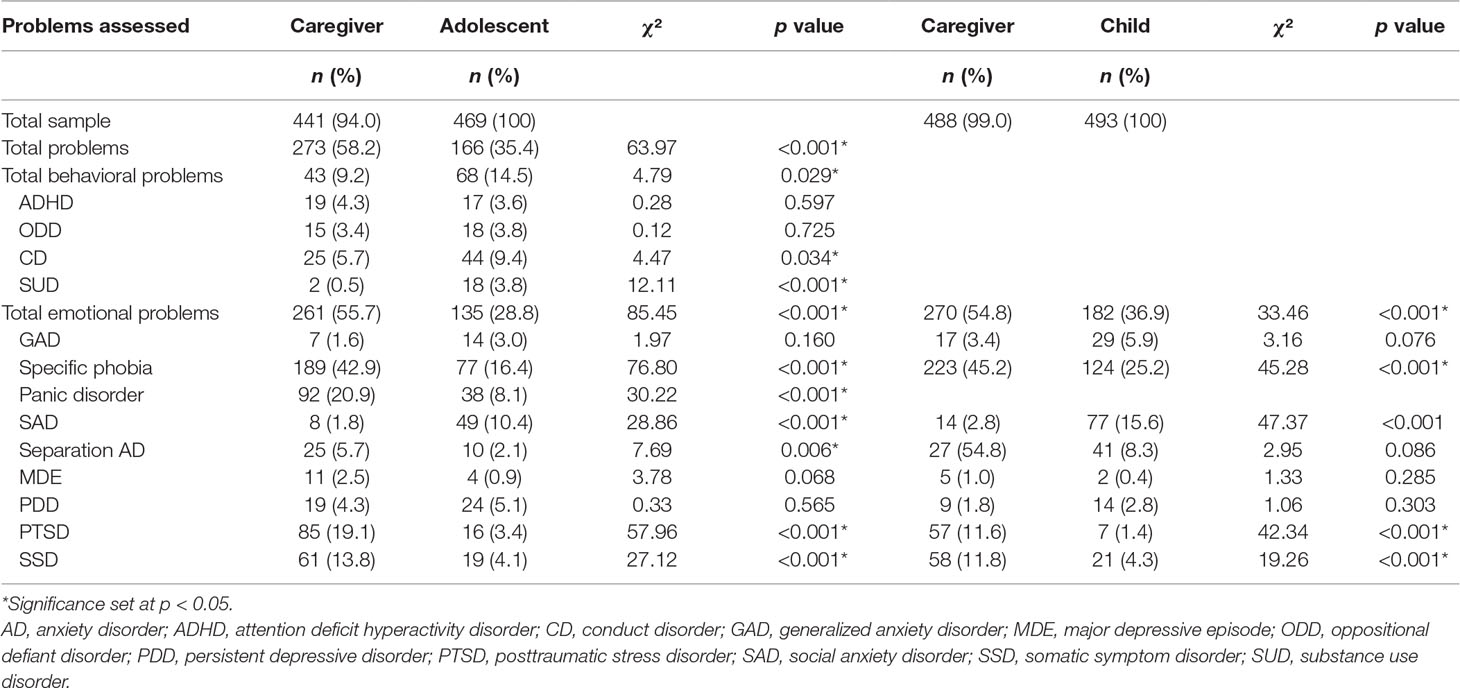
Rates of EBPs (Table 2)
Rates of Behavioral Problems
Adolescents
Based on symptom count cutoff scores, caregiver- and self- reported BPs were present among 9.2% and 14.5% of adolescents, respectively. Adolescents self-reported a mean number of 0.21 (SD = 0.58) BPs, and of those reporting BPs, 30.9% reported having at least two BPs. Adolescents self-reported more BPs than their caregivers [χ²(1) = 4.8, p = 0.029], particularly conduct disorder [χ²(1) = 4.5, p = 0.034] and substance use problems [χ²(1) = 12.1, p < 0.001].
Rates of Emotional Problems
Adolescents
Caregivers reported that 55.7% of adolescents met symptom count criteria for an EP compared with 28.8% according to adolescent self-report. The mean number of self-reported EPs was 0.54 (SD = 1.12), and of those adolescents reporting EPs, 43.7% met criteria for at least two, and 21.5% met criteria for at least three EPs. Caregivers reported more EPs than adolescents [χ²(1) = 85.5, p < 0.001], specifically higher rates of specific phobia [χ²(1) = 76.8, p < 0.001], panic attacks [χ²(1) = 30.2, p < 0.001], posttraumatic stress disorder (PTSD) [χ²(1) = 58.0, p < 0.001], somatic symptoms [χ²(1) = 27.1, p < 0.001], and separation anxiety disorder [χ²(1) = 7.7, p = 0.006]. Adolescents self-reported higher rates of social anxiety disorder [SAD, χ²(1) = 28.9, p < 0.001].
Children
Caregivers indicated that 54.8% of the children met criteria for an EP whereas 36.9% of the children self-reported EPs. The mean number of self-reported EPs was 0.64 (1.07), and of the children self-reporting EPs, 42.9% reported at least two EPs and 18.1% reported three or more. Caregivers reported more EPs than children [χ²(1) = 33.5, p < 0.001], specifically specific phobia [χ²(1) = 45.3, p < 0.001], PTSD [χ²(1) = 42.3, p < 0.001], and somatic symptoms [χ²(1) = 19.3, p < 0.001]. Children self-reported higher rates of SAD [χ²(1) = 47.4, p < 0.001].
Co-Occurrence
Comorbidity of EPs and BPs was also noted, with 41 (8.7%) adolescents and 31 (7.0%) caregivers reporting both EPs and BPs. The number of EPs reported was significantly correlated with the number of BPs reported by both caregivers (r s = 0.14, p = 0.004) and adolescents (r s = 0.29, p < 0.001).
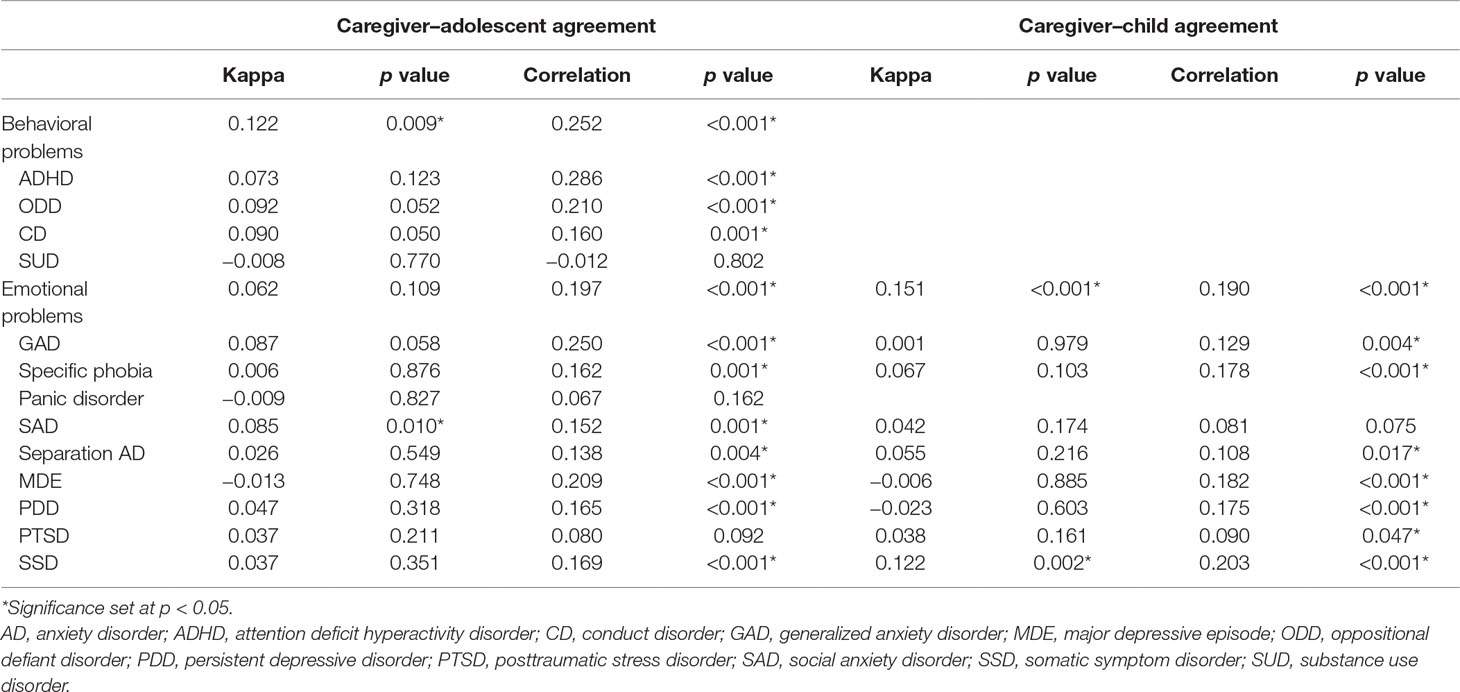
Caregiver and Self-Report Agreement (Table 3)
Informant agreement was poor (κ between −0.023 and 0.122), with a maximum kappa of 0.122 (p = 0.002) for somatic symptom presence. There was also only modest agreement based on severity scores (r between −0.012 and 0.286).
Factors Associated With Caregiver and CA-HIV Discrepancy
Discrepancy scores were all positive, indicating that overall caregivers rated increased severity of EBPs than CA-HIV. The discrepancy scores between EPs and BPs in adolescents were also significantly correlated (r = 0.66, p < 0.001). The association between caregiver and CA-HIV discrepancy and sociodemographic and clinical factors based on univariate analyses are reported in Tables 4 and 5 for adolescents and children, respectively.
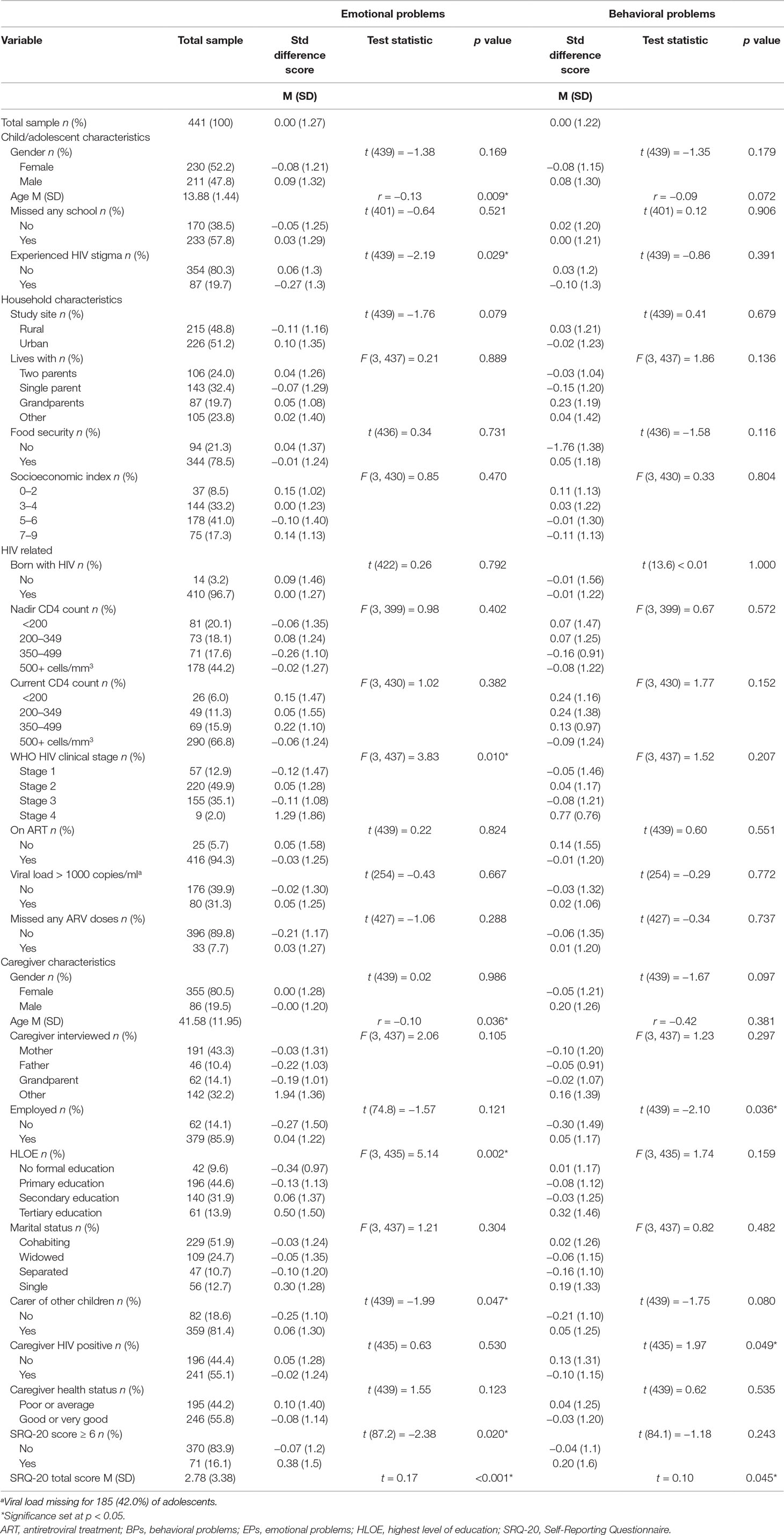
Table 4 Association of demographic and clinical variables to the standardized difference score for emotional and behavioral problems between caregivers and adolescents.
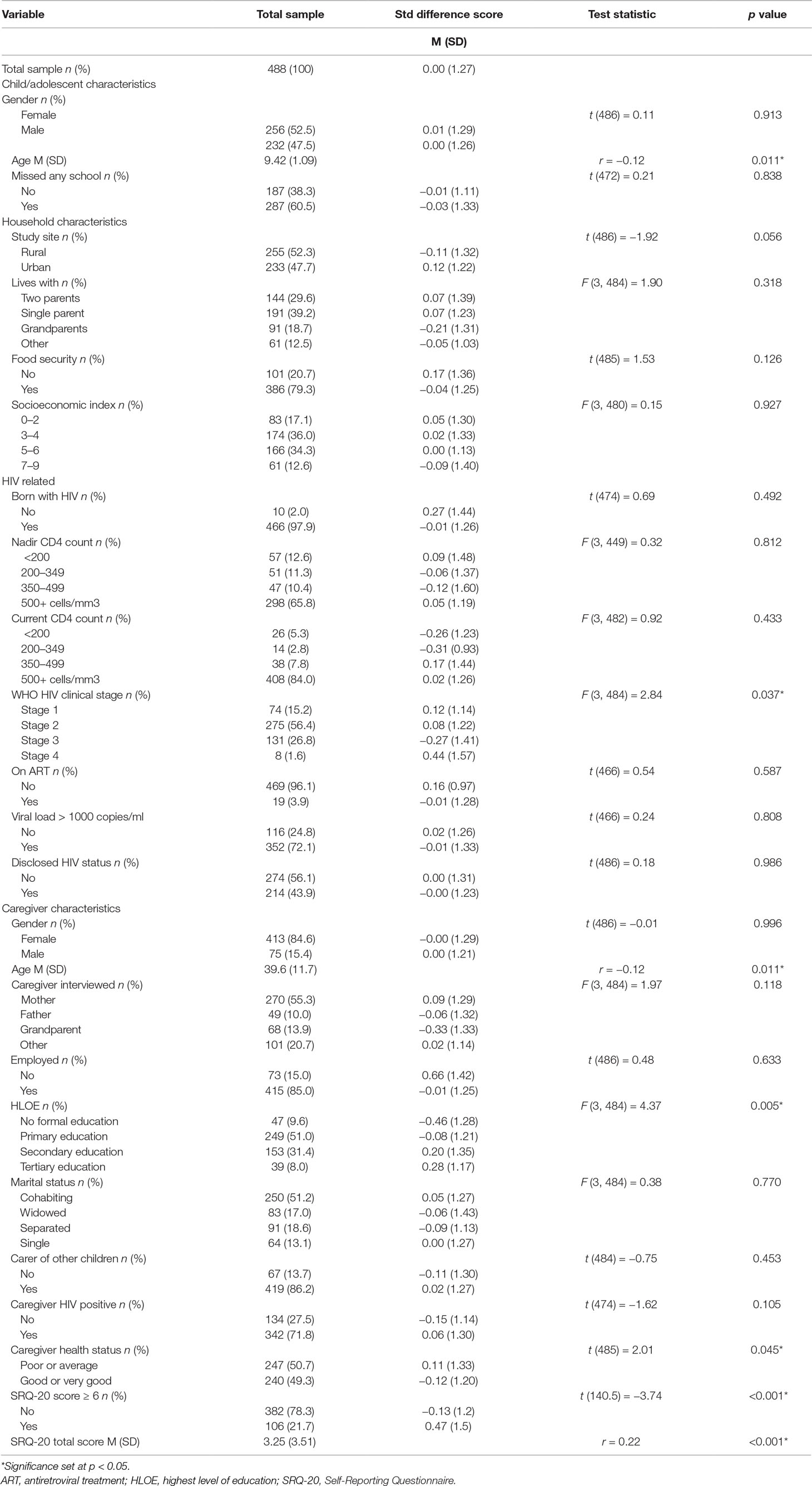
Table 5 Association of demographic and clinical variables to the standardized difference score for emotional problems between caregivers and children.
Adolescent Behavior Problems
Discrepancy scores for BPs were significantly different by caregiver employment status [t(439) = −2.10, p = 0.036] and caregiver HIV status [t(435) = 1.97, p = 0.049]. These variables were added to the linear regression model along with caregiver caring for other children [t(439) = −1.75, p = 0.080], caregiver gender [t(439) = −1.67, p = 0.097], adolescent gender [t(439) = −1.35, p = 0.179], and adolescent age (r = −0.09, p = 0.072) (Table 6). Discrepancy on BP scores were associated with adolescent age (B = −0.09, 95% CI −0.17; −0.01, p = 0.037), caregiver employment status (B = 0.33, 95% CI 0.00; 0.67, p = 0.049), and caregiver HIV status (B = −0.26, 95% CI −0.50; −0.02, p = 0.037). Discrepancy scores decreased with advancing adolescent age and caregivers rated BPs as less severe than adolescents if caregivers were HIV positive and unemployed.
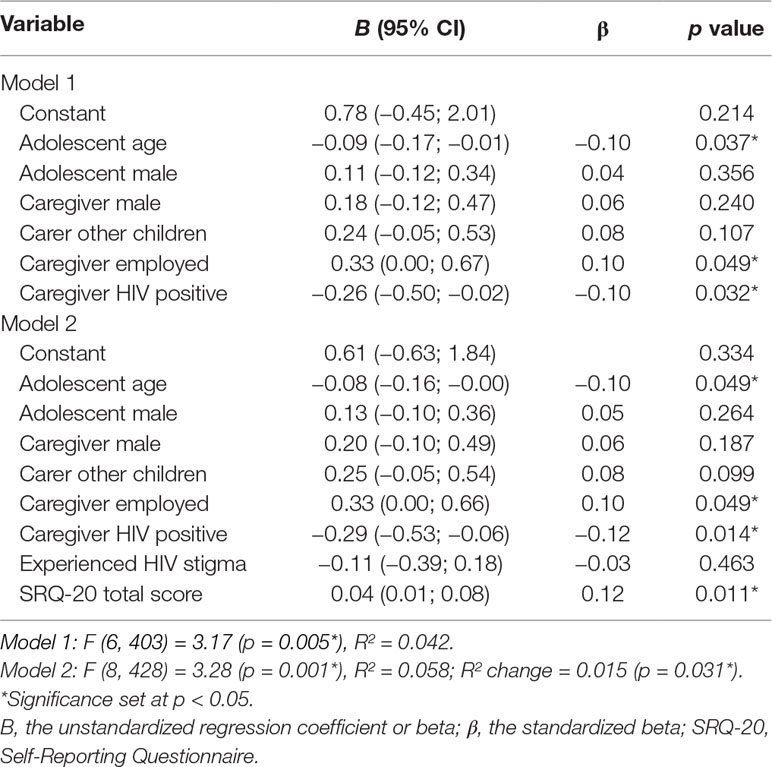
Table 6 Linear regression of factors associated with discrepancy in the presence of behavioral problems between caregivers and adolescents.
Discrepancy scores were significantly associated with caregiver SRQ-20 scores (r = 0.10, p = 0.045), but not with HIV stigma experienced by adolescents [t(439) = −0.86, p = 0.391]. When these variables were added to the model, the model was significantly improved (R² change = 0.015, p = 0.031) and discrepancy scores were significantly associated with caregiver SRQ-20 scores (B = 0.04, 95% CI 0.01; 0.08, p = 0.011), such that caregivers with higher levels of psychological distress rated BPs as being more severe than adolescents self-rated.
Adolescent Emotional Problems
Discrepancy scores for EPs were significantly associated with adolescent age (r = −0.13, p = 0.009), CA-HIV WHO HIV clinical stage [F(3, 437) = 3.83, p = 0.010], caregiver age (r = −0.10, p = 0.036), caregiver HLOE [F(3, 435) = 5.14, p = 0.002], and caregiver caring for other children [t(439) = −1.99, p = 0.047]. These variables were added to the linear regression model along with adolescent gender [t(439) = −1.38, p = 0.169] and study site [t(439) = −1.76, p = 0.079] (Table 7). Discrepancy in EPs was significantly associated with WHO HIV stage 4 (B = 1.47, 95% CI 0.59; 2.34, p = 0.001), caregivers caring for other children (B = 0.32, 95% CI 0.02; 0.62, p = 0.038), and a tertiary HLOE in caregivers (B = 0.77, 95% CI 0.26; 1.27, p = 0.003). Caregivers rated EPs as being more severe than adolescents if the adolescents had WHO HIV stage 4 compared to stage 1, if the caregiver had a tertiary HLOE as compared to no formal education, and if the caregiver was also caring for other children.
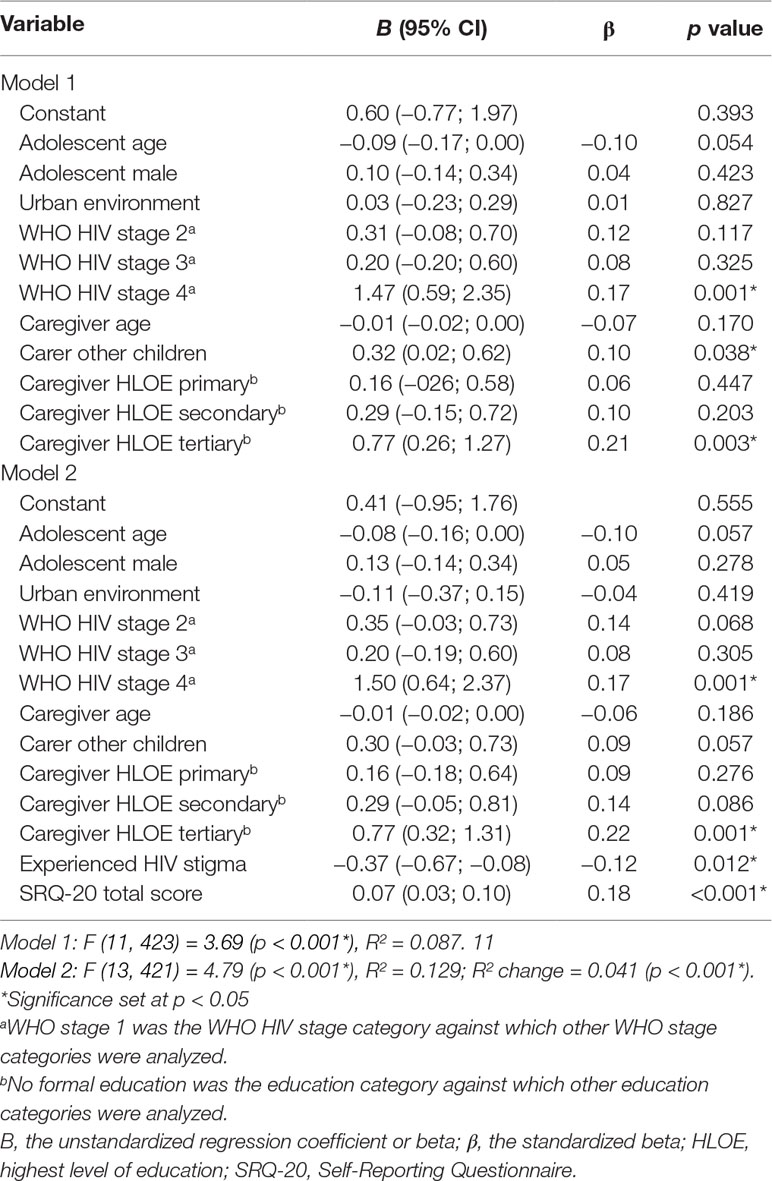
Table 7 Linear regression of factors associated with discrepancy in the presence of emotional problems between caregivers and adolescents.
Discrepancy scores were significantly associated with caregiver SRQ-20 scores (r = 0.17, p < 0.001) and with HIV stigma experienced by adolescent [t(439) = −2.19, p = 0.029]. The model was significantly improved (R² change = 0.041, p < 0.001) when these variables were added and discrepancy scores were significantly associated with HIV stigma experienced by adolescents (B = −0.37, 95% CI −0.67; −0.08, p = 0.012) and with caregiver SRQ-20 scores (B = 0.07, 95% CI 0.03; 0.10, p = 0.011). Caring for other children was no longer significantly associated with discrepancy scores (B = 0.30, 95% CI −0.03; 0.73, p = 0.057). Adolescents who had experienced stigma in the prior year rated EPs as more severe than caregivers and caregivers with increased psychological distress rated EPs more severe than adolescents self-rated.
To assess for possible effects related to the context in which adolescents had experienced HIV-related stigma, we performed post hoc testing by repeating the final model, but dividing HIV stigma according to those who endorsed stigma at home only, outside the home only, or in both settings. Adolescents who experienced stigma at home only (B = −0.70, 95% CI −1.20; −0.20, p = 0.007), but not outside the home only (B = −0.31, 95% CI −0.68; 0.06, p = 0.097) or in both settings (B = 0.03, 95% CI −0.67; 0.74, p = 0.926), self-rated their EPs as significantly more severe than their caregivers rated, compared with adolescents who did not endorse experiencing HIV-related stigma.
Child Emotional Problems
Discrepancy scores for EPs were associated with child age (r = 0.10, p = 0.011), CA-HIV WHO HIV clinical stage [F(3, 484) = 2.84, p = 0.037], caregiver age (r = −0.12, p = 0.011), caregiver HLOE [F(3, 484) = 4.37, p = 0.005], and caregiver health status [t(485) = 2.01, p = 0.045]. These factors were added to the linear regression model along with study site [t(486) = −1.92, p = 0.056] and child gender [t(486) = 0.11, p = 0.913] (Table 8). Discrepancy in reporting EPs was significantly associated with child age (B = −0.16, 95% CI −0.26; −0.06, p = 0.003), caregiver age (B = −0.01, 95% CI −0.02; −0.00, p = 0.030), caregiver health status (B = −0.31, 95% CI −0.54; −0.08, p = 0.007), and caregivers having a primary (B = 0.43, 95% CI 0.04; 0.82, p = 0.031), secondary (B = 0.62, 95% CI 0.21; 1.04, p = 0.004), and tertiary HLOE (B = 0.80, 95% CI 0.25; 1.34, p = 0.004). Discrepancy scores decreased with advancing child and caregiver age. Caregivers rated EPs as more severe than children rated EPs if caregivers rated their own health status as “average” or “poor” as compared to “good” or “very good” or if caregivers had any level of education as compared to no formal education.
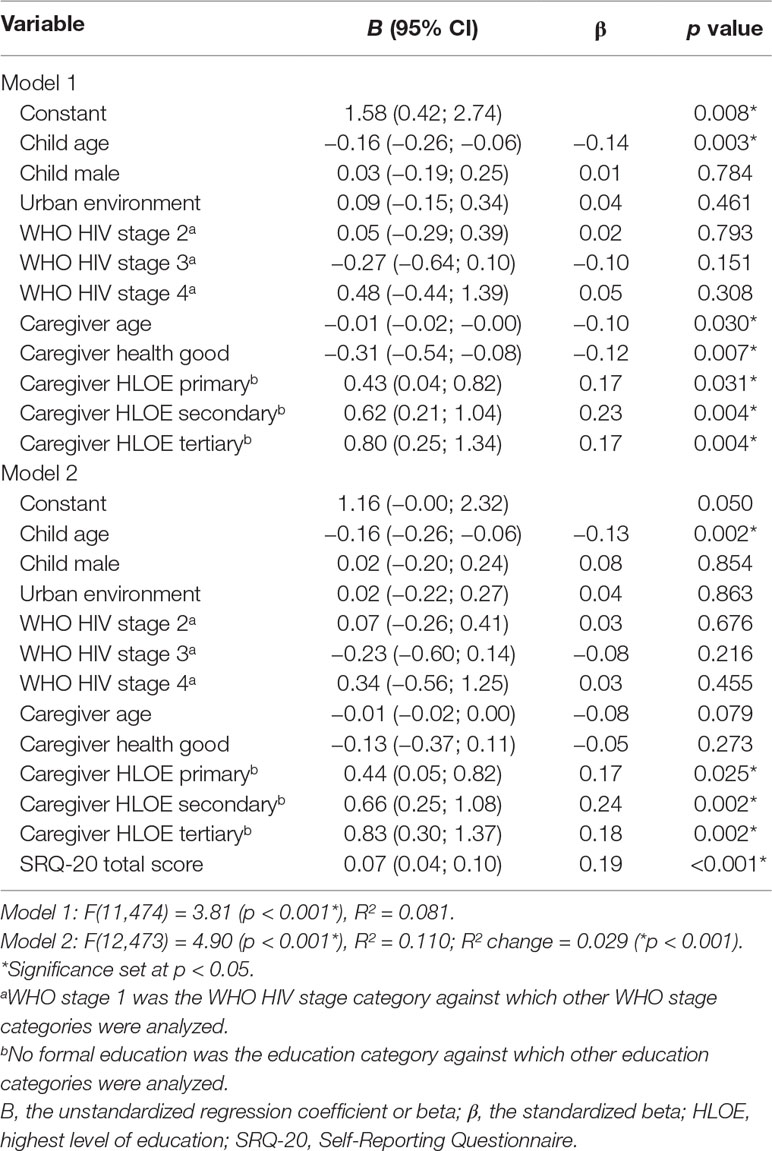
Table 8 Linear regression of factors associated with discrepancy on the presence of emotional problems between caregivers and children.
Discrepancy scores were significantly associated with caregiver SRQ-20 scores (r = 0.22, p < 0.001), and the model was significantly improved when SRQ-20 scores were added to the model (R² change = 0.029, p < 0.001). Discrepancy scores were significantly associated with caregiver SRQ-20 scores (B = 0.07, 95% CI 0.04; 0.10, p = 0.011). Caregiver age (B = −0.01, 95% CI −0.02; 0.00, p = 0.079) and caregiver health status (B = −0.13, 95% CI −0.37; 0.11, p = 0.273) were no longer significantly associated with discrepancy scores, with a pronounced change for caregiver health status. Similar to adolescents, caregivers with increased psychological distress rated EPs as more severe than children self-rated.
Sensitivity Analysis With Discrepancy Scores Based on Averaged Severity Scores
Only results that are different (in terms of a change in statistical significance) from the main results are reported.
Adolescent BPs
Discrepancy scores based on averaged total severity scores were significantly correlated with discrepancy scores using total severity scores (r = 0.986, p < 0.001). Adolescent age (B = −0.70, 95% CI = −0.15; −0.01, p = 0.098) was only trend significantly associated with discrepancy scores.
Adolescent EPs
Discrepancy scores based on averaged total severity scores were significantly correlated with discrepancy scores using total severity scores (r = 0.937, p < 0.001). Discrepancy scores for EPs were significantly associated with adolescent age (B = −0.11, 95% CI = −0.20; −0.03, p = 0.009) and WHO stage 2 (B = 0.44, 95% CI = 0.05; 0.83, p = 0.026), such that discrepancy in reporting EPs decreased with advancing adolescent age and caregivers rated EPs as more severe than adolescents if adolescents were in WHO HIV stage 2 as compared to stage 1.
Child EPs
Discrepancy scores based on averaged total severity scores were significantly correlated with discrepancy scores using total severity scores (r = 0.915, p < 0.001). Child age (B = −0.10, 95% CI = −0.20; 0.01, p = 0.063) and caregivers having a primary (B = 0.40, 95% CI = −0.03; 0.75, p = 0.071) level of education were only trend significantly associated with discrepancy scores.
Discussion
To the best of our knowledge, this is the first study to examine the clinical correlates of informant discrepancy for EBPs among CA-HIV. Older adolescents rated their BPs more severely than their caregivers, whereas caregivers who were employed and HIV negative rated BPs as being more severe than adolescents self-rated. Caregivers rated EPs as more severe than adolescents if the adolescents had WHO HIV stage 4 as compared to stage 1, if the caregiver was also caring for other children, and if the caregiver had a tertiary level of education as compared to no formal education. In the child sample, younger children and older caregivers rated EPs as more severe than their counter informants did. Caregivers rated EPs as more severe than children self-rated if the caregiver’s self-reported health status was poor, and if they had any level of education as compared to no formal education. Informant discrepancy of EBPs was also associated with HIV stigma experienced by adolescents and caregiver psychological distress. Adolescents who reported experiencing HIV-related stigma in the prior year rated their EPs, but not BPs, as more severe than their caregivers rated. Caregivers with greater psychological distress rated all EBPs as more severe than CA-HIV, especially EPs. In summary, caregiver and CA-HIV discrepancy was associated with sociodemographic features of the CA-HIV and their caregivers, HIV disease-related factors, HIV stigma, and caregiver psychological distress and associations varied between EPs and BPs.
Similar to other settings, CA-HIV in this study frequently endorsed experiencing EBPs, with 14.5% of adolescents self-reporting BPs, 28.8% self-reporting EPs, and 36.9% of the children self-reporting EPs. These rates are comparable to what has been found in other studies globally (9, 10, 16, 23, 70). An earlier Ugandan study among HIV-positive adolescents documented higher rates of self-reported psychological distress (51.2%) and substance use (6.1%) (14); however, the adolescents had more advanced HIV and were not receiving ART. Also, in that study, adolescents aged between 13 and 18 years were more likely to be psychologically distressed than those between 10 and 12 years, whereas in our study, rates of self-reported EPs were higher in children than in adolescents. Among CA-HIV, similar to other settings, comorbidity of mental health problems is common (13, 71). In our sample, comorbidity was also frequently reported with 44.0% of adolescents and 42.9% of children with EBPs, endorsing two or more conditions.
Based on previous research with child and adolescent samples, we expected that caregiver and youth agreement would be modest (5, 32, 36, 37). We found generally low agreement between caregivers and CA-HIV, based on symptom severity and symptom count cutoff scores. Although caregiver–adolescent agreement was lower than demonstrated in the YI-4 validation study, it was similar to caregiver–youth agreement in another sample of CA-HIV (7, 33). Agreement between caregivers and children was also of a similar magnitude to the aforementioned study that employed the CI-4 (7). We thus demonstrated similarly low agreement between caregivers and CA-HIV to what has been found in other settings. Meta-analyses have revealed that generally there is greater caregiver–child agreement for externalizing than for internalizing symptoms (32, 37). Similarly, we found that agreement between caregivers and adolescents about the presence of EBPs was significant for BPs, but not EPs. Agreement between caregivers and children regarding the presence of EPs was also significant, suggesting greater agreement between caregivers and children, than between caregivers and adolescents. An earlier meta-analysis also revealed greater agreement between caregivers and younger children, than between caregivers and adolescents, although this association was not demonstrated in a more recent meta-analysis (32, 37). A longitudinal study that evaluated multi-informant reports from childhood into adulthood also found that the agreement between caregiver and youth self-report for internalizing problems decreased as individuals became older, whereas agreement regarding externalizing problems increased with age (36).
It is interesting to note that, in our sample, contrary to our hypothesis, caregivers reported higher rates of EPs than CA-HIV and adolescents self-reported higher rates of BPs than their caregivers. Across various societies, adolescents tend to rate more, and more severe, problems, both internalizing and externalizing, than their caregivers do (36, 51). Other studies of HIV-affected youth have found that caregivers reported more BPs than self-reported by youth (72, 73), and youth reported higher rates of EPs than caregivers (16, 73). Although caregivers reported higher rates of EPs, CA-HIV reported significantly higher rates of SAD, which could be related to context, with SAD occurring in situations where caregivers are often not present; in addition, the internal experience of certain anxiety symptoms may not be evident to caregivers. Generally, agreement has been demonstrated to be higher for observable symptoms than for unobservable symptoms (38). Adolescents also reported higher rates of substance use and conduct problems, which again could reflect the context in which these behaviors occur, as well as adolescents hiding certain unfavorable behaviors from their caregivers. The setting in which discrepancy is being evaluated can also influence the association; for instance, one study found that among clinical samples, both parent- and youth-reported EPs were associated with clinician diagnoses of EPs, but among community samples, only youth self-reported EPs were associated with clinician diagnoses, whereas only parent-reported BPs were associated with clinician diagnoses of BPs among both community and clinic samples (74).
Discrepancy in EP severity ratings decreased with increased child and caregiver age and decreased with increased adolescent age for BPs. Similar to our results, other studies have also found that discrepancies in child BPs decreased with advancing child age (68). The effect of child age on agreement between caregiver and child have, however, been inconsistent and may be related to differences in approach (38). We found that when averaged severity scores were used, associations between discrepancy and child age for EPs, and adolescent age for BPs were no longer significant, whereas adolescent age was significantly associated with discrepancy for EPs. Thus, overall, older CA-HIV rated their EBPs as more severe than caregivers rated them, but this association was of a small magnitude.
Caregivers rated BPs as less severe than adolescents if they themselves were HIV positive or were unemployed. Caregivers rating BPs as less severe than adolescents may reflect caregivers being unaware of adolescent behaviors occurring in contexts outside of the home environment. Parents who are unemployed and HIV positive may be dealing with their own stressors and thus may be less aware of other difficulties faced by adolescents. A systematic review evaluating the effects of HIV-infected caregivers on children in Sub-Saharan Africa reported on a number of studies that noted an association between caregiver HIV and increased EBPs (75). Of note, an earlier Ugandan study found that increased CA-HIV psychological distress was associated with the caretaker being HIV negative (14). Thus, the effect of caregiver HIV status may vary according to the youth’s own status.
Educational attainment of caregivers was associated with increased discrepancy in severity ratings for EPs in both the child and adolescent samples. Caregivers with primary, secondary, or tertiary HLOE rated child EPs as more severe than caregivers with no formal education. In the adolescent sample, this association was demonstrated only for those who had attained a tertiary HLOE as compared to no formal education. In line with these results, a study of CA-HIV found that family characteristics (including caregiver HLOE), largely, were associated with caregiver-rated EBPs, but not with youth self-rated EBPs (7). In contrast, a study of an adolescent forensic sample found that caregiver education had no effect on discrepancy of EBPs (76). An opposite association was demonstrated in a Taiwanese study, where investigators used parental level of education as a proxy of socioeconomic status (SES), and found that parents rated EBPs as less severe than youths if the father had completed tertiary education as compared to not completing secondary education (40). Beyond SES, educational attainment of caregivers may reflect caregiver health/mental health literacy and thus their awareness of EPs.
Adolescents who had attained a WHO HIV stage 4, as compared to stage 1, rated their EPs as less severe than their caregivers did, and when averaged severity scores were used, this was also demonstrated for WHO HIV stage 2. Caregivers of adolescents who had attained a more advanced clinical HIV status may be more concerned about the adolescent’s health status overall due to previous significant health problems. Some studies have demonstrated that more advanced HIV disease may be linked to EBPs in CA-HIV. One study in 81 adolescents found that having a past Centers for Disease Control and Prevention (CDC) class C diagnosis was associated with having at least one prior psychiatric disorder diagnosis and having received prior mental health treatment (18). Another US study of 274 clinically stable CA-HIV found that those with CD4 counts in the lower 50% (<660 cells/mm3) were more likely to have caregiver-reported conduct problems (17). In a Malawian study of 562 adolescents, self-rated depression severity was also associated with more severe immunosuppression (based on CD4 count) (19).
Similar to our research, other studies have also found that discrepancies were not related to who the caregiver was (42, 77), although most studies evaluating informant discrepancies have included the mother as caregiver (38). In our sample, caregivers who were also caring for other children rated adolescent EPs as more severe than the adolescents themselves, and caregivers who rated their own general health status lower rated child EPs as more severe than children themselves. Caregivers caring for multiple children may have a higher burden of care, and caregivers with poorer overall health status may also face increased stressors that influence their ratings of CA-HIV mental health status. A study from New York in CA-HIV, aged between 7 and 16 years, utilizing structural equation modeling (SEM), found that caregiver–child stress (including factors such as parent–child relationship problems, caregiver mental health problems, and stressful or negative life events) was associated with both CA-HIV self-reported and caregiver-reported EBPs (78). Other studies have also demonstrated that parents reporting increased caregiving stress rated EBPs as more severe than their children self-reported (42, 76). When caregiver psychological distress was controlled for, however, neither caring for other children nor self-rated health status remained significantly associated with informant discrepancy.
Adolescents who reported experiencing HIV-related stigma in the prior year rated EPs, but not BPs, as more severe than their caregivers did. Of note, when the setting where stigma had been experienced was evaluated, this association was significant for stigma occurring only within the home environment. Other studies in Ugandan adolescents have also demonstrated that HIV-related stigma was associated with increased self-rated mental health problems (27, 29). Adolescents experiencing HIV stigma may develop more EPs; alternatively, adolescents with EPs may interpret events as stigmatizing. Studies have suggested that the pathway between HIV stigma experienced in the community and mental health and adherence outcomes is mediated through internalized stigma (e.g., negative self-views related to HIV) (79). The fact that discrepancy between caregivers and adolescents on EPs was demonstrated largely for stigma experienced in the home environment suggests that familial relational problems may be playing a role in discrepancy, with caregivers not aware of how adolescents are experiencing the home environment as well as the EPs they contend with.
Increased severity of caregiver psychological distress was associated with caregivers rating EPs and BPs as more severe than adolescents self-rated. The association was stronger for EPs than BPs and psychological distress ratings suggestive of possible depression in caregivers was also associated with increased discrepancy of EPs, but not BPs, on bivariate analysis. Our findings are consistent with the majority of the literature (38, 40, 41), although some studies have found that caregiver self-reported mood symptoms were not associated with discrepancy (42). Studies have also demonstrated that maternal anxiety, but not depression, was significantly associated with discrepancy, such that anxious mothers rated their child’s anxiety as more severe than children themselves (80). The SRQ-20 includes symptoms of both anxiety and depression, and we assessed for discrepancy in the severity of CA-HIV EPs combined and thus cannot comment on possible differential associations for anxiety and depression. Increased reporting of EBPs in their children by mothers with depression have been postulated to be due to possible distortion, with depressed mothers over-reporting EBPs, or to reflect accuracy, such that children of depressed mothers have more EBPs and mothers are accurately reporting on those (81). One study found that parental psychological distress was associated with increased parental report of BPs and EPs as well as increased EPs according to parental and child report combined, thus suggesting that parental psychopathology is associated with both increased child EPs and with possible over-reporting of EBPs by parents (82). Regardless of whether discrepancy is due to distortion or an accurate reflection of CA-HIV EBPs, the discrepancy demonstrated still highlights the need for multi-informant reports (41).
Strengths and Limitations
One of the strengths of the study is the relatively large sample of CA-HIV from a region with a high HIV prevalence. It also includes youth self-report, which is often not assessed in CA-HIV studies, providing unique information on context and how CA-HIV view their own EBPs. This study also considered a broader range of sociodemographic variables than has typically been evaluated in studies examining discrepancy. The assessment instruments adopted for this study were previously used in a large-scale study of CA-HIV from the US (7), thus facilitating cross-cultural comparisons. These measures are also well suited to assess informant agreement as they were designed to have corresponding items and are scored in a similar fashion. Meta-analyses indicate that informant agreement is best evaluated by measures that share the same content, item labeling and scaling (32).
This study also has some notable limitations. We utilized a cross-sectional research design and as such could not determine cause-and-effect relationships. The EBPs reported by caregivers and CA-HIV were not confirmed with a clinical interview, and thus we cannot comment on specificity and sensitivity in this sample. The sample included differed from the sample excluded, and this may have influenced results. Adolescents who were older, living in urban areas, who had a higher socioeconomic index, with caregivers interviewed who were employed and who were not their parents or grandparents were more likely to be excluded. The main reasons these participants were excluded was that caregivers did not complete the CASI-5, and within this context, the differences could be explained by caregivers who were likely unable to complete the assessment as they were working, and that older adolescents were more likely to attend appointments unaccompanied. Children who were residing in urban areas, had a WHO clinical stage 1 or 2, with caregivers interviewed who were younger and HIV negative were more likely to be excluded. The age discrepancy with caregivers is likely due to excluding caregivers who were not older than 17 years; the reasons for the other differences are less apparent. We grouped EBPs together into broad constructs when assessing discrepancy and thus cannot comment on factors associated with discrepancy for individual disorders. The approach we used to determine overall severity of BP and EPs may also have implications. We used total severity scores obtained for disorders to compute discrepancy scores, which may have weighted total severity towards disorders with more symptoms. However, sensitivity analysis with discrepancy scores determined with averaged severity scores mostly provided the same results, with some differences noted. The differences were of a small magnitude, such that significant associations became trend significant and vice versa. The strength of association for the factors that differed according to approach used to determine severity scores was thus likely small. Future studies can perform more in-depth analysis evaluating agreement and discrepancy for individual disorders as it is beyond the scope of this manuscript. Although we noted receipt of ART, data were not collected on specific ARV regimens. Lastly, we did not correct for multiple comparisons (and type I error) and thus our results should be considered exploratory.
Conclusions
Similar to other studies, we demonstrate that CA-HIV commonly experience EBPs, whether based on caregiver or youth self-report. Furthermore, CA-HIV may be prone to develop more severe psychopathology as reflected by higher rates of psychiatric hospitalizations and increased rates of prior psychotropic and behavioral treatments (35, 83). Mental health problems can have serious detrimental consequences in individuals with HIV; for instance, higher mortality rates were reported for HIV-infected individuals with comorbid psychiatric and substance use disorders than those without (84). In the aforementioned study, the mortality risk was lower in those who had received treatment for EBPs, highlighting the importance of screening and timely intervention. Although mental health outcomes have not always been linked to adherence problems in individual studies, a systematic review identified mental health as a factor influencing adherence, particularly when other risk factors are also present (85). Despite the burden of mental health problems in CA-HIV, there is a dearth of appropriate mental health services, especially in resource-limited settings (15).
To our knowledge, this is the first study to evaluate informant discrepancy of EBPs in CA-HIV. Discrepancy between caregivers and CA-HIV was greater if caregivers were unemployed and had no formal education. These results suggest that socioeconomic status may influence the discordance between caregivers and CA-HIV regarding the presence of EBPs. Although many studies have not found an association between socioeconomic status and informant discrepancies, a meta-analysis demonstrated that agreement between mothers and fathers on internalizing and externalizing problems was lower for children of low socioeconomic status (38, 86). Of note, some HIV-related variables were associated with discrepancy (i.e., caregivers rating more severe BPs than adolescents if they were HIV negative and more severe EPs if the child had a history of more advanced clinical HIV). These findings suggest that HIV disease-related factors may influence caregiver CA-HIV discrepancy regarding EBPs. HIV stigma was associated with discrepancy, yet again highlighting the negative impact of HIV stigma as well as the importance of the context in which it is experienced. In addition to HIV-related stigma, mental-health-related stigma can be another barrier to CA-HIV receiving mental health care (15). We assessed only for adolescent perceived interpersonal HIV stigma, and future investigations utilizing broader constructs related to stigma, such as internalized HIV stigma, HIV disclosure stigma, stigma in health care services, mental health stigma, and stigma experienced by caregivers, are warranted. Consistent with prior research (38, 40, 41), we also demonstrated that caregivers with increased psychological distress rate the EBPs of CA-HIV as more severe than youths self-rated.
Informant discrepancies have been linked to poorer youth outcomes (42, 43). Fewer discrepancies between caregivers and youths predict improved treatment engagement and outcomes (44, 87, 88). Informant discrepancy can, therefore, be considered in treatment planning and may contribute to improved treatment outcomes, further highlighting the value of evaluating informant discrepancy in CA-HIV (42, 89). Our study supports the general consensus that mental health screening and assessments, including CA-HIV self-report, should be integrated into routine care and multilevel psychosocial and family-based interventions are needed to support CA-HIV and their caregivers (9).
Ethics Statement
The study was conducted in accordance with the Declaration of Helsinki and ethical approval was obtained from the Uganda Virus Research Institute’s Research and Ethics Committee, the Ethics Committee of the London School of Hygiene and Tropical Medicine, and the Uganda National Council of Science and Technology. Eligible study participants provided written informed consent (caregiver) and assent (CA-HIV) after explanation of the study objectives and procedures. No CA-HIV were enrolled without their assent and all participants were informed that they could withdraw without prejudice at any time. In the majority of cases, the parents provided informed consent for participation of the CA-HIV, but in cases where the primary caregivers were not parents, the guardians of the CA-HIV provided the informed consent.
Author Contributions
EK, JL, KG, and VP contributed to the concept and design of the study. Data collection was done by EK, JL, and RM. LH performed statistical data analysis and wrote the paper. All authors contributed to revising the manuscript and have read and approved the submitted version.
Funding
This work was supported by an MRC/DFID African Leadership Award to Eugene Kinyanda, Number MR/L004623/1. Leigh van den Heuvel was supported in this work by a NIH-Fogarty Project Titled: “Pittsburgh-Stellenbosch University AIDS-comorbidities Training Research Programme (Pitt-SU AICoTRP; Award to Jean B. Nachega and Soraya Seedat)” and her work reported herein was made possible through funding by the South African Medical Research Council through its Division of Research Capacity Development under the SAMRC CLINICIAN RESEARCHER (M.D PHD) SCHOLARSHIP PROGRAMME from funding received from the South African National Treasury. The content hereof is the sole responsibility of the authors and do not necessarily represent the official views of the SAMRC or the funders. Soraya Seedat is supported by the South African Research Chairs Initiative in PTSD funded by the Department of Science and Technology and the National Research Foundation.
Funders have played no role in the study design, data collection, analysis, and interpretation and in writing the manuscript.
Conflict of Interest Statement
KG is a shareholder in Checkmate Plus and publisher of the CASI-5, YI-4, and CI-4.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer JA declared a shared affiliation, with no collaboration, with one of the authors JN to the handling editor.
Acknowledgments
We would like to acknowledge the work and support provided by the staff of the Mental Health Project at the MRC/UVRI Uganda Research Unit. We would also like to acknowledge the support and cooperation of children/adolescents, caregivers, and management of The AIDS Support Organisation (TASO) clinic (Masaka), Kitovu Mobile AIDS organisation (Masaka), The Uganda Cares clinic (Masaka), Joint Clinical Research Centre clinic (Kampala), and Nsambya Home Care Department (Kampala).
References
2. UNAIDS. Country factsheets Uganda | 2016 HIV and AIDS Estimates Adults and children living with Country factsheets Uganda | 2016 HIV testing and treatment cascade. People living with HIV Coverage of adults and children. (2016)1–6. Available at: http://www.unaids.org/en/regionscountries/countries/pakistan.
3. Mellins CA, Malee KM. Understanding the mental health of youth living with perinatal HIV infection: lessons learned and current challenges. J Int AIDS Soc (2013) 16, 18593. doi: 10.7448/IAS.16.1.18593
4. Vreeman RC, Scanlon ML, McHenry MS, Nyandiko WM. The physical and psychological effects of HIV infection and its treatment on perinatally HIV-infected children. J Int AIDS Soc (2015) 18:1–15. doi: 10.7448/IAS.18.7.20258
5. Mellins CA, Brackis-Cott E, Leu C, Elkington KS, Dolezal C, Wiznia A, et al. Rates and types of psychiatric disorders in perinatally HIV-infected youth and seroconverters. J Child Psychol Psychiatry (2009) 50:1131–8. doi: 10.1111/j.1469-7610.2009.02069.x
6. Scorza P, Kanyanganzi F, Smith MC, Sezibera V, Cyamatare F, Beardslee W, et al. HIV and child mental health: a case–control study in Rwanda. Pediatrics (2014) 134(2):e464–e472. doi: 10.1542/peds.2013-2734
7. Gadow KD, Chernoff M, Williams PL, Brouwers P, Morse E, Heston J, et al. Co-occuring psychiatric symptoms in children perinatally infected with HIV and peer comparison sample. J Dev Behav Pediatr (2010) 31:116–28. doi: 10.1097/DBP.0b013e3181cdaa20
8. Scharko A. DSM psychiatric disorders in the context of pediatric HIV/AIDS. AIDS Care (2006) 18:441–5. doi: 10.1080/09540120500213487
9. Mellins CA, Tassiopoulos K, Malee K, Moscicki A-B, Patton D, Smith R, et al. Behavioral health risks in perinatally HIV-exposed youth: co-occurrence of sexual and drug use behavior, mental health problems, and nonadherence to antiretroviral treatment. AIDS Patient Care STDS (2011) 25:413–22. doi: 10.1089/apc.2011.0025
10. Malee KM, Tassiopoulos K, Huo Y, Siberry G, Williams PL, Hazra R, et al. Mental health functioning among children and adolescents with perinatal HIV infection and perinatal HIV exposure. AIDS Care (2012) 23:1533–44. doi: 10.1080/09540121.2011.575120.Mental
11. Menon A, Glazebrook C, Ngoma MS. Mental health of HIV positive adolescents in Zambia. Med J Zambia (2009) 36:151–6. https://www.ajol.info/index.php/mjz/article/view/76371
12. Mutumba M, Bauermeister JA, Elkington KS, Bucek A, Dolezal C, Leu C-S, et al. A prospective longitudinal study of mental health symptoms among perinatally HIV-infected and HIV-exposed but uninfected urban youths. J Adolesc Health (2016) 58:460–6. doi: 10.1016/j.jadohealth.2015.12.014
13. Kamau JW, Kuria W, Mathai M, Atwoli L, Kangethe R. Psychiatric morbidity among HIV-infected children and adolescents in a resource-poor Kenyan urban community. AIDS Care (2012) 24:836–42. doi: 10.1080/09540121.2011.644234
14. Musisi S, Kinyanda E. Emotional and behavioural disorders in HIV seropositive adolescents in urban uganda. East Afr Med J (2009) 86:16–24. doi: 10.4314/eamj.v86i1.46923
15. Vreeman RC, McCoy BM, Lee S. Mental health challenges among adolescents living with HIV. J Int AIDS Soc (2017) 20:100–9. doi: 10.7448/IAS.20.4.21497
16. Nachman S, Chernoff M, Williams P, Hodge J, Heston J, Gadow KD. Human immunodeficiency virus disease severity, psychiatric symptoms, and functional outcomes in perinatally infected youth. Arch Pediatr Adolesc Med (2012) 166:528–35. doi: 10.1001/archpediatrics.2011.1785
17. Nozyce ML. A behavioral and cognitive profile of clinically stable HIV-infected children. Pediatrics (2006) 117:763–70. doi: 10.1542/peds.2005-0451
18. Wood SM, Shah SS, Steenhoff AP, Rutstein RM. The impact of AIDS diagnoses on long-term neurocognitive and psychiatric outcomes of surviving adolescents with perinatally acquired HIV. Aids (2009) 23:1859–65. doi: 10.1097/QAD.0b013e32832d924f
19. Kim MH, Mazenga AC, Yu X, Devandra A, Nguyen C, Ahmed S, et al. Factors associated with depression among adolescents living with HIV in Malawi. BMC Psychiatry (2015) 15:1–12. doi: 10.1186/s12888-015-0649-9
20. Zeegers I, Rabie H, Swanevelder S, Edson C, Cotton M, van Toorn R. Attention deficit hyperactivity and oppositional defiance disorder in HIV-infected South African children. J Trop Pediatr (2009) 56:97–102. doi: 10.1093/tropej/fmp072
21. Mellins CA, Elkington KS, Leu CS, Santamaria EK, Dolezal C, Wiznia A, et al. Prevalence and change in psychiatric disorders among perinatally HIV-infected and HIV-exposed youth. AIDS Care (2012) 24:953–62. doi: 10.1080/09540121.2012.668174
22. Kapetanovic S, Wiegand RE, Dominguez K, Blumberg D, Bohannon B, Wheeling JR, the LEGACY Consortium R. Associations of medically documented psychiatric diagnoses and risky health behaviors in highly active antiretroviral therapy-experienced perinatally HIV-infected youth. AIDS Patient Care STDS (2011) 25:493–501. doi: 10.1089/apc.2011.0107
23. Dow DE, Turner EL, Shayo AM, Mmbaga B, Cunningham CK, O’Donnell K. Evaluating mental health difficulties and associated outcomes among HIV-positive adolescents in Tanzania. AIDS Care (2016) 28:825–33. doi: 10.1080/09540121.2016.1139043
24. Malee K, Williams P, Montepiedra G, McCabe M, Nichols S, Sirois PA, et al. Medication adherence in children and adolescents with HIV infection: associations with behavioral impairment. AIDS Patient Care STDS (2011) 25:191–200. doi: 10.1089/apc.2010.0181
25. Alperen J, Brummel S, Tassiopoulos K, Mellins CA, Kacanek D, Smith R, et al. Prevalence of and risk factors for substance use among perinatally human immunodeficiency virus–infected and perinatally exposed but uninfected youth. J Adolesc Health (2015) 54:341–9. doi: 10.1016/j.jadohealth.2013.09.003
26. Rueda S, Mitra S, Chen S, Gogolishvili D, Globerman J, Chambers L, et al. Examining the associations between HIV-related stigma and health outcomes in people living with HIV/AIDS: a series of meta-analyses. BMJ Open (2016) 6:e011453. 10.1136/bmjopen-2016-011453
27. Mutumba M, Bauermeister JA, Harper GW, Musiime V, Lepkowski J, Resnicow K, et al. Psychological distress among Ugandan adolescents living with HIV: examining stressors and the buffering role of general and religious coping strategies. Glob Public Health (2017) 12:1479–91. doi: 10.1080/17441692.2016.1170871
28. Akena D, Musisi S, Joska J, Stein DJ. The association between aids related stigma and major depressive disorder among HIV-positive individuals in Uganda. PLoS One (2012) 7:7–12. doi: 10.1371/journal.pone.0048671
29. Ashaba S, Cooper-Vince C, Vořechovská D, Maling S, Rukundo GZ, Akena D, et al. Development and validation of a 20-item screening scale to detect major depressive disorder among adolescents with HIV in rural Uganda: a mixed-methods study. SSM Popul Health (2018) 7:100332. doi: 10.1016/j.ssmph.2018.100332
30. Achenbach TM. As others see us correlations for psychopathology. Curr Dir Psychol Sci (2006) 15:94–8. doi: 10.1111/j.0963-7214.2006.00414.x
31. Achenbach TM, Krukowski RA, Dumenci L, Ivanova MY. Assessment of adult psychopathology: meta-analyses and implications of cross-informant correlations. Psychol Bull (2005) 131:361–82. doi: 10.1037/0033-2909.131.3.361
32. De Los Reyes A, Augenstein TM, Wang M, Thomas SA, Drabick DA, Burgers DE RJ. The validity of the multi-informant approach to assessing child and adolescent mental health. Psychol Bull (2015) 141:858. doi: 10.1039/C5RA11250H.Thermal
33. Gadow KD, Sprafkin J, Carlson GA, Schneider J, Nolan EE, Mattison RE, et al. A DSM-IV–referenced, adolescent self-report rating scale. J Am Acad Child Adolesc Psychiatry (2002) 41:671–9. doi: 10.1097/00004583-200206000-00006
34. Elkington KS, Robbins RN, Bauermeister JA, Abrams EJ, McKay M, Mellins CA. Mental health in youth infected with and affected by HIV: the role of caregiver HIV. J Pediatr Psychol (2011) 36:360–73. doi: 10.1093/jpepsy/jsq094
35. Chernoff M, Nachman S, Williams P, Brouwers P, Heston J, Hodge J, et al. Mental health treatment patterns in perinatally HIV-infected youth and controls. Pediatrics (2009) 124:627–36. doi: 10.1542/peds.2008-2441
36. Van der Ende J, Verhulst FC, Tiemeier H. Agreement of informants on emotional and behavioral problems from childhood to adulthood. Psychol Assess (2012) 24:293–300. doi: 10.1037/a0025500
37. Achenbach TM, McConaughy SH, Howell CT. Child/adolescent behavioral and emotional problems: implications of cross-informant correlations for situational specificity. Psychol Bull (1987) 101:213–32. doi: 10.1037/0033-2909.101.2.213
38. De Los Reyes A, Kazdin AE. Informant discrepancies in the assessment of childhood psychopathology: a critical review, theoretical framework, and recommendations for further study. Psychol Bull (2005) 131:483–509. doi: 10.1037/0033-2909.131.4.483
39. Lerner MD, Calhoun CD, Mikami AY, De Los Reyes A. Understanding parent–child social informant discrepancy in youth with high functioning autism spectrum disorders. J Autism Dev Disord (2012) 42:2680–92. doi: 10.1007/s10803-012-1525-9
40. Chen YY, Ho SY, Lee PC, Wu CK, Gau SSF. Parent–child discrepancies in the report of adolescent emotional and behavioral problems in Taiwan. PLoS One (2017) 12:1–12. doi: 10.1371/journal.pone.0178863
41. Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: a meta-analytic review. Clin Child Fam Psychol Rev (2011) 14:1–27. doi: 10.1007/s10567-010-0080-1
42. De Los Reyes A, Youngstrom EA, Pabón SC, Youngstrom JK, Feeny NC, Findling RL. Internal consistency and associated characteristics of informant discrepancies in clinic referred youths age 11 to 17 years. J Clin Child Adolesc Psychol (2011) 40:36–53. doi: 10.1080/15374416.2011.533402
43. Ferdinand RF, van der Ende J, Verhulst FC. Parent–adolescent disagreement regarding psychopathology in adolescents from the general population as a risk factor for adverse outcome. J Abnorm Psychol (2004) 113:198–206. doi: 10.1037/0021-843X.113.2.198
44. Jensen-Doss A, Weisz JR. Diagnostic agreement predicts treatment process and outcomes in youth mental health clinics. J Consult Clin Psychol (2008) 76:711–22. doi: 10.1037/0022-006X.76.5.711
45. Osafo J, Knizek BL, Mugisha J, Kinyanda E. The experiences of caregivers of children living with HIV and AIDS in Uganda: a qualitative study. Glob Health (2017) 13:1–13. doi: 10.1186/s12992-017-0294-9
46. Lentoor AG. Psychosocial challenges associated with caregiving in the context of pediatric HIV in rural Eastern Cape. Front Public Health (2017) 5:127. doi: 10.3389/fpubh.2017.00127
47. Mafune RV, Lebese RT, Nemathaga LH. Challenges faced by caregivers of children on antiretroviral therapy at Mutale Municipality selected healthcare facilities, Vhembe District, Limpopo Province. Curationis (2017) 40:1–9. doi: 10.4102/curationis.v40i1.1541
48. Pinquart M. Parenting stress in caregivers of children with chronic physical condition—a meta-analysis. Stress Health (2018) 34:197–207. doi: 10.1002/smi.2780
49. Pinquart M. Meta-analysis of anxiety in parents of young people with chronic health conditions. J Pediatr Psychol (2019) jsz024. doi: 10.1093/jpepsy/jsz024
50. Buchanan AL, Montepiedra G, Sirois PA, Kammerer B, Garvie PA, Storm DS, et al. Barriers to medication adherence in HIV-infected children and youth based on self- and caregiver report. Pediatrics (2012) 129:e1244–e1251. doi: 10.1542/peds.2011-1740
51. Rescorla LA, Ginzburg S, Achenbach TM, Ivanova MY, Almqvist F, Begovac I, et al. Cross-informant agreement between parent-reported and adolescent self-reported problems in 25 societies. J Clin Child Adolesc Psychol (2013) 42:262–73. doi: 10.1080/15374416.2012.717870
52. Mpango RS, Kinyanda E, Rukundo GZ, Gadow KD, Patel V. Cross-cultural adaptation of the Child and Adolescent Symptom Inventory-5 (CASI-5) for use in central and south-western Uganda: the CHAKA project. Trop Doct (2017) 47:347–54. doi: 10.1177/0049475517724688
53. Mpango RS, Kinyanda E, Rukundo GZ, Osafo J, Gadow KD, Mpango RS. Exploration of the understanding and etiology of ADHD in HIV/AIDS as observed by adolescents with HIV/AIDS, caregivers and health workers—using case vignettes. Afr Health Sci (2018) 18(3):488–95. doi: 10.4314/ahs.v18i3.4
54. Mpango RS, Kinyanda E, Rukundo GZ, Levin J, Gadow KD, Patel V. Prevalence and correlates for ADHD and relation with social and academic functioning among children and adolescents with HIV/AIDS in Uganda. BMC Psychiatry (2017) 17:1–8. doi: 10.1186/s12888-017-1488-7
55. Kinyanda E, Salisbury TT, Levin J, Nakasujja N, Mpango RS, Abbo C, et al. Rates, types and co-occurrence of emotional and behavioural disorders among perinatally HIV-infected youth in Uganda: the CHAKA study. Soc Psychiatry Psychiatr Epidemiol (2019) 54:415–25. doi: 10.1007/s00127-019-01675-0
56. Gadow KD, Sprafkin J. Child and Adolescent Symptom Inventory-5 (CASI-5). Stonybrooke, New York: Checkmate Plus (2013). Available at: https://www.checkmateplus.com/product/casi5.htm.
57. Gadow KD. The symptom inventories: An annotated bibliography. Stonybrooke, New York: Checkmate Plus (2015). Available at: https://www.checkmateplus.com/research/research_univ.htm [Accessed December 13, 2018].
58. Sprafkin J, Gadow KD, Salisbury H, Schneider J, Loney J. Further evidence of reliability and validity of the Child Symptom Inventory-4: parent checklist in clinically referred boys. J Clin Child Adolesc Psychol (2002) 31:513–24. doi: 10.1207/S15374424JCCP3104_10
59. Salcedo S, Chen YL, Youngstrom EA, Fristad MA, Gadow KD, Horwitz SM, et al. Diagnostic efficiency of the Child and Adolescent Symptom Inventory (CASI-4R) depression subscale for identifying youth mood disorders. J Clin Child Adolesc Psychol (2017) 00:1–15. doi: 10.1080/15374416.2017.1280807
60. Gadow KD, Sprafkin J. Child symptom inventory 4: Screening and norms manual. Stony Brook, NY: Checkmate Plus (2002).
61. Chernoff M, Angelidou K, Williams PL, Brouwers P, Warshaw M, Nachman S. Assessing psychiatric symptoms in youth affected by HIV: comparing a brief self-administered rating scale with a structured diagnostic interview. J Clin Psychol Med Settings (2018) 25:420–8. doi: 10.1007/s10880-018-9550-2
62. Gadow KD, Sprafkin J, (1999). Youth’s inventory-4 (YI-4) manual. Stony Brook, NY: Checkmate Plus.
64. Salcedo S, Chen Y, Youngstrom EA, Fristad MA, Gadow KD, Horwitz SM, et al. Co-occuring psychiatric symptoms in children perinatally infected with HIV and peer comparison sample. J Am Acad Child Adolesc Psychiatry (2010) 31:671–9. doi: 10.1097/DBP.0b013e3181cdaa20
65. Beusenberg M, Orley J, (1994). World Health Organization. A user’s guide to the self reporting questionnaire (SRQ/compiled by M. Beusenberg, and J. Orley. World Health Organization).
66. Nakimuli-Mpungu E, Mojtabai R, Alexandre PK, Katabira E, Musisi S, Nachega JB, et al. Cross-cultural adaptation and validation of the self-reporting questionnaire among HIV+ individuals in a rural ART program in southern Uganda. HIV AIDS (Auckl) (2012) 4:51–60. doi: 10.2147/HIV.S29818
67. Kinyanda E, Waswa L, Baisley K, Maher D. Prevalence of severe mental distress and its correlates in a population-based study in rural south-west Uganda. BMC Psychiatry (2011) 11:97. doi: 10.1186/1471-244X-11-97
68. De Los Reyes A, Kazdin AE. Informant discrepancies in assessing child dysfunction relate to dysfunction within mother–child interactions. J Child Fam Stud (2006) 15:643–61. doi: 10.1007/s10826-006-9031-3
69. De Los Reyes A, Kazdin AE. Measuring informant discrepancies in clinical child research. Psychol Assess (2004) 16:330–4. doi: 10.1037/1040-3590.16.3.330
70. Orban LA, Stein R, Koenig LJ, Conner LC, Rexhouse EL, Lewis JV, et al. Coping strategies of adolescents living with HIV: disease-specific stressors and responses. AIDS Care (2010) 22:420–30. doi: 10.1080/09540120903193724
71. Williams P, Leister E, Chernoff M, Nachman S, Morse E, Di Poalo V, et al. Substance use and its association with psychiatric symptoms in perinatally HIV-infected and HIV-affected adolescents. AIDS Behav (2010) 14:1072–82. doi: 10.1007/s10461-010-9782-0
72. Li M, Betancourt T, Eustache E, Oswald C, Louis E, Mukherjee J, et al. Risk and protective factors for internalizing and externalizing outcomes among HIV-affected youth in Haiti. AIDS Care (2015) 27:995–9. doi: 10.1080/09540121.2015.1020751
73. Doku PN, Minnis H. Multi-informant perspective on psychological distress among Ghanaian orphans and vulnerable children within the context of HIV/AIDS. Psychol Med (2016) 46:2329–36. doi: 10.1017/S0033291716000829
74. Aebi M, Kuhn C, Banaschewski T, Grimmer Y, Poustka L, Steinhausen HC, et al. The contribution of parent and youth information to identify mental health disorders or problems in adolescents. Child Adolesc Psychiatry Ment Health (2017) 11:1–12. doi: 10.1186/s13034-017-0160-9
75. Goldberg RE, Short SE. What do we know about children living with HIV-infected or AIDS-ill adults in Sub-Saharan Africa? A systematic review of the literature. AIDS Care (2016) 28(Suppl 2):130–41. doi: 10.1080/09540121.2016.1176684
76. Penney SR, Skilling TA. Moderators of informant agreement in the assessment of adolescent psychopathology: extension to a forensic sample. Psychol Assess (2012) 24:386–401. doi: 10.1037/a0025693
77. De Los Reyes A, Goodman KL, Kliewer W, Reid-Quiñones K. Whose depression relates to discrepancies? Testing relations between informant characteristics and informant discrepancies from both informants’ perspectives. Psychol Assess (2008) 2:139–49. doi: 10.1037/1040-3590.20.2.139
78. Hermetet-Lindsay KD, Correia KF, Williams PL, Smith R, Malee KM, Mellins CA, et al. Contributions of disease severity, psychosocial factors, and cognition to behavioral functioning in US youth perinatally exposed to HIV. AIDS Behav (2017) 21:2703–15. doi: 10.1007/s10461-016-1508-5
79. Turan B, Budhwani H, Fazeli PL, Browning WR, Raper JL, Mugavero MJ, et al. How does stigma affect people living with HIV? The mediating roles of internalized and anticipated HIV stigma in the effects of perceived community stigma on health and psychosocial outcomes. AIDS Behav (2017) 21:283–91. doi: 10.1007/s10461-016-1451-5
80. Pereira AI, Muris P, Barros L, Goes R, Marques T, Russo V. Agreement and discrepancy between mother and child in the evaluation of children’s anxiety symptoms and anxiety life interference. Eur Child Adolesc Psychiatry (2015) 24:327–37. doi: 10.1007/s00787-014-0583-2
81. Ordway MR. Depressed mothers as informants on child behavior: methodological issues. Res Nurs Health (2011) 34:520–32. doi: 10.1002/nur.20463
82. Bajeux E, Klemanski DH, Husky M, Leray E, Chan Chee C, Shojaei T, et al. Factors associated with parent–child discrepancies in reports of mental health disorders in young children. Child Psychiatry Hum Dev (2018) 49:1003–10. doi: 10.1007/s10578-018-0815-7
83. Gaughan D, Hughes M, Oleske J, Malee K, Gore CA, Nachman S. Pediatric AIDS Clinical Trials Group 219C Team. Pediatrics (2004) 133:e544–e551. doi: 10.1542/peds.113.6.e544
84. DeLorenze GN, Satre DD, Quesenberry CP, Tsai A-L, Weisner CM. Mortality after diagnosis of psychiatric disorders and co-occurring substance use disorders among HIV-infected patients. AIDS Patient Care STDS (2010) 24:705–12. doi: 10.1089/apc.2010.0139
85. Lall P, Lim SH, Khairuddin N, Kamarulzaman A. Review: an urgent need for research on factors impacting adherence to and retention in care among HIV-positive youth and adolescents from key populations. J Int AIDS Soc (2015) 18:41–53. doi: 10.7448/IAS.18.2.19393
86. Duhig AM, Renk K, Epstein MK, Phares V. Interparental agreement on internalizing, externalizing, and total behavior problems: a meta-analysis. Clin Psychol Sci Pract (2000) 7:435–53. doi: 10.1093/clipsy.7.4.435
87. Brookman-Frazee L, Haine RA, Gabayan EN, Garland AF. Predicting frequency of treatment visits in community-based youth psychotherapy. Psychol Serv (2008) 5:126–38. doi: 10.1037/1541-1559.5.2.126
88. Ferdinand RF, van der Ende J, Verhulst FC. Prognostic value of parent–adolescent disagreement in a referred sample. Eur Child Adolesc Psychiatry (2006) 15:156–62. doi: 10.1007/s00787-005-0518-z
Keywords: children, adolescents, HIV, emotional problems, behavioral problems, caregiver report, self-report, discrepancy
Citation: van den Heuvel LL, Levin J, Mpango RS, Gadow KD, Patel V, Nachega JB, Seedat S and Kinyanda E (2019) Agreement and Discrepancy on Emotional and Behavioral Problems Between Caregivers and HIV-Infected Children and Adolescents From Uganda. Front. Psychiatry 10:460. doi: 10.3389/fpsyt.2019.00460
Received: 20 December 2018; Accepted: 11 June 2019;
Published: 11 July 2019.
Edited by:
Amritha Bhat, University of Washington, United StatesReviewed by:
Krishnamachari Srinivasan, St. John’s Research Institute, IndiaJura Augustinavicius, Johns Hopkins University, United States
Copyright © 2019 van den Heuvel, Levin, Mpango, Gadow, Patel, Nachega, Seedat and Kinyanda. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Leigh L. van den Heuvel, bGx2ZGhAc3VuLmFjLnph; bHVlbGxhekBnbWFpbC5jb20=
 Leigh L. van den Heuvel
Leigh L. van den Heuvel Jonathan Levin2
Jonathan Levin2 Soraya Seedat
Soraya Seedat