- Department of Social Welfare, Faculty of Health Sciences, Aomori University of Health and Welfare, Aomori, Japan
Suicide prevention is an increasingly important issue, especially among older people. Recent work on improving its effectiveness has focused on developing a framework aligning interventions with key risk factors and stages of the suicide process. We have developed this further, by integrating psycho-behavioral components associated with suicide, existing guidelines for identifying critical points of intervention, and the previous preventive strategies framework. Our schematic diagram shows the relationship between the suicide process and prevention strategies, combined with initiatives for linking different types of strategies, from universal strategies at population level, through selective strategies focusing on groups at risk, to indicated strategies, aimed at specific high-risk individuals. We tested our framework using previous studies assessing the impact of suicide prevention interventions on suicide rates in older adults. It was possible to place all identified interventions within the framework. Examining effectiveness within the framework suggests that some interventions may be more successful in reducing suicide rates because they developed systematic linkages between universal, selective, and indicated prevention interventions. Other studies, however, show that interventions can be successful without these linkages, so other factors may also be important. The main weakness of our framework is a lack of evidence about critical intervention points within the suicide process, which may limit its practical application. However, the framework may help to improve the linkages between types of interventions, and support practitioners in developing a wide range of strategies across different areas and stages of the suicide process.
Introduction
Suicide is an important public health issue around the world, particularly among older people (those aged over 60) (1). Both suicide rates (2, 3) and the lethality of suicidal behavior (4, 5) are higher in this age group. Older people are more likely to have serious intent to commit suicide, with less warning, than younger people (6, 7).
Several risk factors are associated with suicide among older adults. At least one major psychiatric diagnosis is found in over 70% of suicides in this age group (8). Depression is particularly associated (8), and has a population-attributed risk of more than 40% for suicide, attempted suicide, and suicidal ideation (9–11). Several physical and psychosocial risk factors are also associated, including physical illness and functional impairment (12, 13), and age-related psychosocial stressors, such as lack of supportive social networks (14), loneliness (15), and loss of an important intimate relationship or social role (16).
There are several models of suicidal behavior (17–20). For example, the stress-diathesis theory (17) proposes that longitudinal factors predisposing individuals toward suicidal behavior are influenced by particular stressors. The psychological mechanisms underlying this model remain unclear, however, so it cannot distinguish those at imminent risk of suicidal behavior.
Suicide prevention work has used two basic approaches. The traditional approach is staged: primary, secondary, and tertiary prevention. Primary prevention aims to prevent onset of mental illness, secondary to detect and treat illness, and tertiary to reduce relapses and deterioration (21). The second approach focuses on effectiveness of interventions (2, 17, 22–24). A framework has been created to identify effective interventions, align them with suicidal risk factors, and classify them into three types of prevention strategies, universal, selective, and indicated (25, 26). Universal prevention strategies are applied across populations and individuals not necessarily identified as at particular risk of suicide (25). Selective prevention strategies are aimed at groups at risk of suicide, but not necessarily showing suicidal behavior. Indicated prevention strategies focus on high-risk individuals, such as those who have previously attempted suicide.
Suicide risk at individual level fluctuates over time (18), so efforts to reduce mortality from suicide among older adults in the community need to work with those at various levels of risk. The use of universal, selective and indicated strategies can both address stage of illness, and consider target populations (21), making it more suitable than the staged approach. Research suggests that the risk of suicidal acts could be reduced through a multilevel approach, linking different types of prevention strategies (27). However, no studies have explicitly examined the connections between levels or types of strategy. Another promising model (28) links the suicide process in older adults with the prevention framework (25, 26). It shows that indicated strategies are suitable for individuals with proximal risk factors for suicide (such as depression), selective strategies for those with distal risk factors (e.g., stress or illness), and universal strategies for the entire population, irrespective of risk status. The authors did not, however, show precisely how interventions addressed particular risk factors. This paper therefore aimed to further develop the framework to bring together the suicide process and prevention strategies at different levels.
It is important to ensure that individuals at higher risk of suicide participate in universal or selective interventions, so that they can be identified and supported appropriately. Making better, more systematic linkages between different types of prevention strategies may help with this. However, multilevel interventions and the linkages between them may have different effects (29). The effects may also vary in different age and population groups (30). This paper therefore draws on studies assessing the impact of suicide prevention interventions on suicide outcomes in older adults. It examines whether there were systematic linkages between universal, selective and indicated prevention interventions in studies evaluating the impact of interventions on suicide risk.
Methods
Hypothetical Schema of Suicide Progression With Universal, Selective, and Indicated Prevention Strategies
This study built on previous work to develop a framework for suicide prevention, including the steps of the suicide process and time points for specific interventions (31). We combined this with the universal, selective, and indicated preventive strategies framework (25, 26), and models of suicidal behavior (28, 32) to generate a schematic diagram of the suicide process and classify prevention activity by stage.
Figure 1 shows the schema for suicide prevention (29). The left shows the four sequential steps of the suicide process: a non-suicidal state, suicidal ideation, suicidal plans, and suicidal acts. The right shows preventive strategies classified by suicide process stage and type of intervention (2, 23).
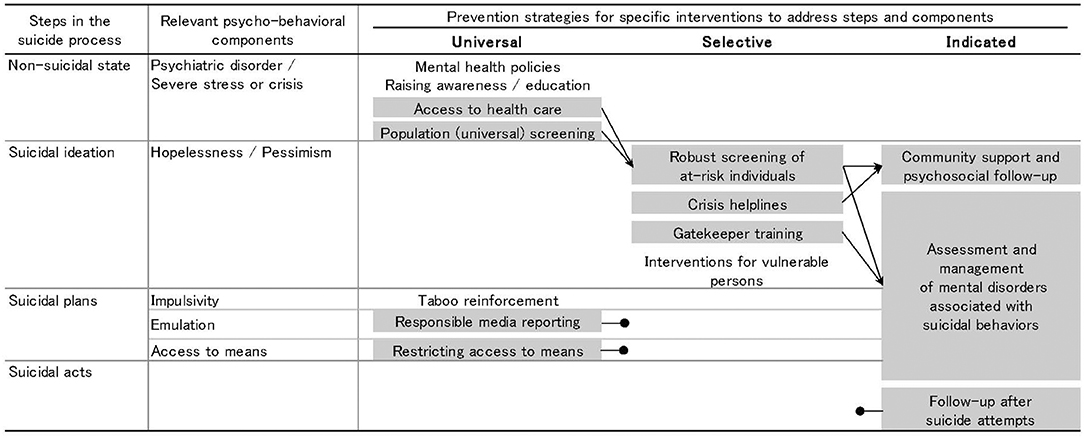
Figure 1. Schematic diagram of suicide process and prevention strategies (29). Interventions highlighted in gray are supported by evidence of their efficacy in reducing suicide risk. A black arrow indicates a clear link to another intervention. A black circle indicates no known link to other interventions. The interventions at each point in the suicide process are expected to involve people at stages closer to suicide.
The second column integrates the stress-diathesis model for suicidal behavior (32). This model identifies particular psycho-behavioral components that may lead to progression to the next step. For example, depression, hopelessness, suicidal ideation, and impulsivity are suicide risk factors for all age groups, although acute deterioration and acute psychosocial crises are the most important predictors of suicidal ideation. Similarly, hopelessness and pessimism can lead to suicidal thoughts and plans. Emulation and access to means are also important factors in suicide (33, 34). Certain interventions may act on particular psycho-behavioral components, so can minimize progression to the next stage (31). Conwell et al.'s (28) risk factors overlap significantly with the stress-diathesis model. It is therefore helpful to link the elements of the stress-diathesis model to universal, selective, and indicated prevention strategies.
Testing the Framework Against Evidence on Suicide Prevention Programs
We wanted to know whether the schematic diagram explained findings about suicide prevention interventions. We used a literature search to identify systematic reviews and reports of systematic reviews as reliable sources of articles on intervention types and linkages (see Appendix 1). We included studies assessing the impact of suicide prevention interventions on suicide rates in older adults, particularly initiatives linking different types of prevention strategies.
We examined all the interventions against the diagram. We used previous studies (2, 17, 24) to categorize interventions within universal, selected and indicated strategies.
Results
Identifying Studies to Test the Diagram
We identified 53 review articles, and excluded 46 because they did not meet the criteria (Appendix 1). One article (23) was added following cross-referencing. One report (2) was substituted for an overview (35). We found four systematic reviews (24, 36–38), two overviews (29, 39) and two reports of systematic reviews (2, 23), and their reference lists gave 17 suitable studies to test the hypothetical schema and six to examine the effect of linkages between levels of intervention on suicide rate at the population level.
Universal Prevention Strategies
Universal prevention strategies included mental health policies, awareness-raising and education, improving access to health care, and population or universal screening.
Mental Health Policies, Raising Awareness, and Education
Combining these interventions may prevent individuals from developing suicidal ideation (31). However, several systematic reviews have indicated that these interventions alone do not reduce suicidal activities among adults (40, 41). They may facilitate other preventive interventions that address acute deteriorations and psychosocial crises (42, 43), but there is no evidence that they are usually designed to be integrated directly with these strategies.
Population Screening for Mental Illness
Access to healthcare (2) and universal screening (29) have both been linked to selective preventive strategies, often because they involve the same systems and staff. One study found that community-based interventions, involving universal, in-depth screening and general care for all older people in a region with a high suicide rate, resulted in a lower suicide rate (44). These community-based interventions used a self-report instrument to assess the risk of depression among older people, and therefore identify those who may otherwise not seek help. This first stage was linked to a selective intervention involving in-depth screening of those identified as at risk, for example, because they were depressed, which is a known suicide risk factor (9–11). This provided a systematic link from universal to selective prevention. Improving education and awareness, and incorporating interventions locally, might improve uptake of screening.
Responsible Media Reporting and Restricting Access to Means of Suicide
Other universal prevention strategies include taboo reinforcement to minimize impulsivity, responsible media reporting to minimize emulation, and restricting access to means of suicide. There is evidence that some of these interventions can reduce suicide rates (2, 23, 24, 36), but no proof for others, notably taboo reinforcement. Responsible media reporting and restricting access to means are both supported by evidence, in one case of short-term benefits and in the other of benefits limited to the specific means of suicide (17). These interventions may reduce the frequency of progression toward suicidal acts (31), but are hard to integrate with selective or indicated strategies because they do not allow selection or identification of individuals to target further intervention.
Selective Prevention Strategies
Selective prevention interventions included gatekeeper training for physicians, robust screening, and counseling of at-risk individuals, the availability of crisis helplines, and interventions for vulnerable people (e.g., those experiencing severe stress).
Identifying and Referring At-Risk Individuals
Studies have found that gatekeeper training for physicians to enable them to detect and treat depression can reduce suicide rates (45, 46), probably because depression is such a common risk factor for suicide in this age group (9–11). This, like robust screening and counseling, integrates universal, and selective strategies. Previous community-based interventions using this combination resulted in lower suicide rates. These interventions involved universal, in-depth screening of older people in a region with a high suicide rate. Those who were depressed or suffering from depressive episodes were referred for semi-structured clinical interviews (44). These interventions may help to minimize hopelessness and pessimism, and therefore stop progression toward suicidal plans and acts (29, 31). The model suggests that interventions at particular time points might reasonably target people at stages closer to suicide.
Crisis Helplines and Telephone Counseling
Crisis helplines and emergency response services also reduce suicide. One study (47) provided regular telephone support for at-risk individuals and an emergency response when required. This resulted in a lower suicide rate among older women. A community agency that provided telephone counseling with emotional support, crisis intervention, referral services, and home visits reduced hopelessness, but not depressive symptoms (48). Crisis helplines, even without subsequent support, can reduce suicide risk among callers during the call itself and over subsequent weeks (49).
These selective strategies are usually closely linked to indicated strategies, often follow-up with specific individuals, but few rigorous studies have evaluated the efficacy of interventions targeted at specific vulnerable groups.
Indicated Prevention Strategies
These interventions included assessment and management of mental disorders associated with suicidal behaviors, community support, and psychosocial follow-up.
Management of Mental Disorders Associated With Suicidal Outcomes
The appropriate management of mental illness can minimize hopelessness, pessimism, and impulsivity, reducing the likelihood of individuals developing suicidal thoughts or taking action (31, 32). Antidepressants (50, 51) and collaborative care (52, 53) of older people with depression have been associated with reduced risk of suicidal ideation in institutional settings. A secondary analysis (50) of data from three studies on late-life major depression found that antidepressants and interpersonal psychotherapy reduced suicidal ideation. Other studies investigated the effect of antidepressants on suicidal ideation and behavior in patients with late-life major depression (51) and the 2-year effect of collaborative primary care interventions on suicidal ideation and depressive symptoms among older people (52). Interventions included antidepressant treatment, patient education, interpersonal psychotherapy, and care management. Both studies (51, 52) found reduced suicidal ideation among the target group. Collaborative depression care can also reduce suicidal ideation among older people (53). The sample size of treatment studies in institutional settings is usually too small to detect changes in suicide rates, but the link to risk factors such as depression (9–11) suggests that these interventions may be clinically useful to reduce suicidal acts.
These studies suggest that appropriate management of mental illness is an important part of suicide prevention, and can reduce the risk of progression toward suicide ideation, planning, and attempts. However, it may be possible to make a more direct link. One previous study in northern Japan detected individuals with depression via screening interventions (44) and successfully treated them for depression via psychiatric or primary care. This linked the management of mental illness directly with selective preventive strategies, and fits with our model's suggestion that these interventions may become more effective by linking different levels.
Community Support and Psychosocial Follow-Up
Follow-up care after attempted suicide is associated with positive outcomes, such as reduced risk of re-attempting (54–56). Follow-up care among recently discharged patients was effective in reducing suicide attempts and deaths in all age groups (54), especially those discharged from emergency departments (35, 55). This intervention may work by reducing the risk of re-attempting (56) and therefore of death by suicide, but the small numbers mean that population suicide rates are not affected. This care is also not usually designed to be integrated with other prevention strategies (37, 54), which might limit its benefits.
Linkages Between Types of Intervention
Table 1 shows the main characteristics of recent studies evaluating multilevel programs to reduce suicide rate among older adults, and shows specific linkages between types of intervention. For example, two studies linked selective and indicated interventions by emergency calls for help (47) and treatment and referrals (46). They found lower suicide rates among older women in the intervention group (47) and in the population of the intervention area (46). One study evaluated systematic linkages across types of interventions, such as recommendations to move from universal to selective interventions (44), and found reduced suicide rates in both older men and women.
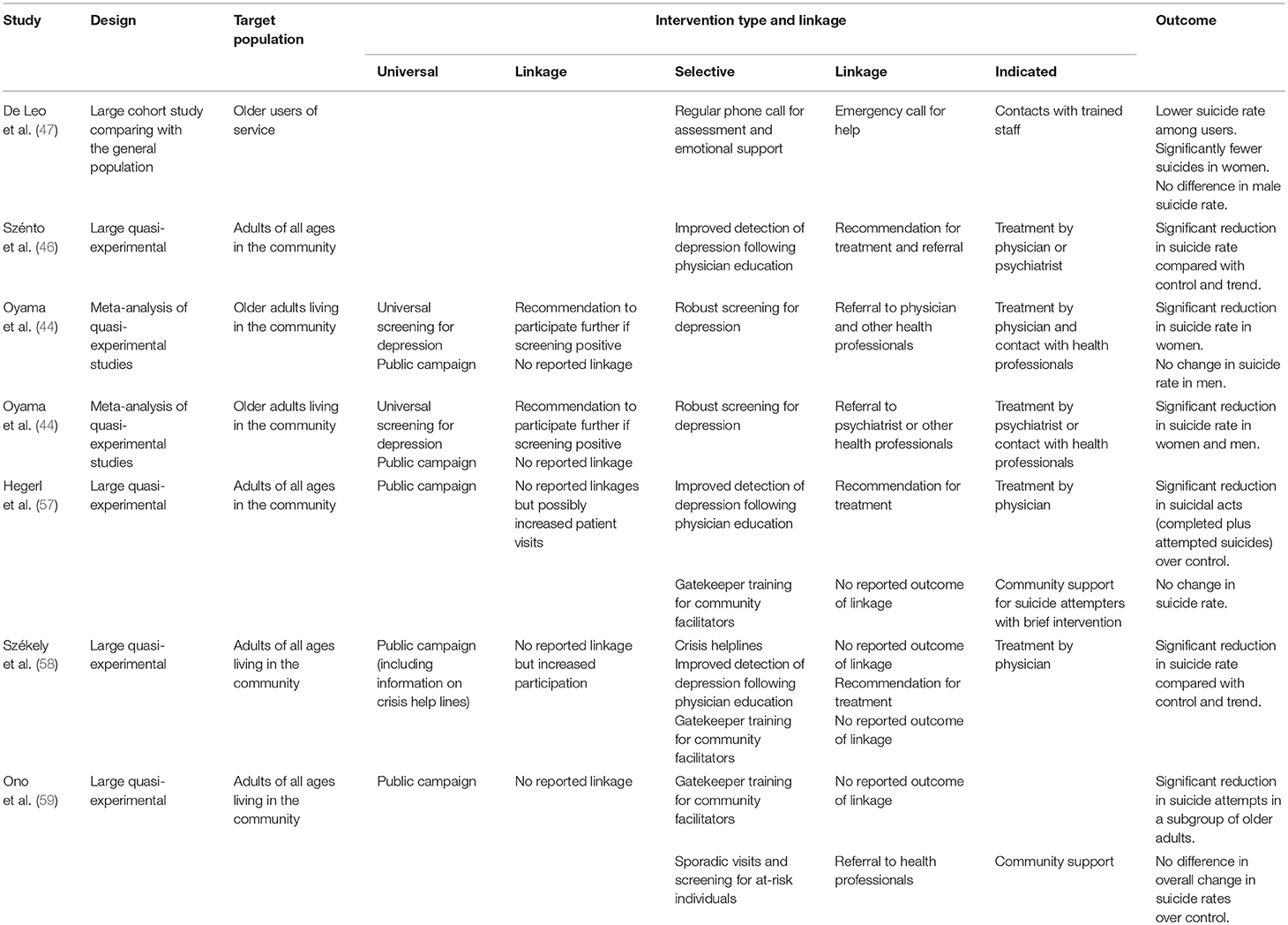
Table 1. The main characteristics of recent studies evaluating multilevel programs to reduce suicide rate among older adults.
Three other recent multilevel approaches (57–59) had partial linkages of primary care features (for instance, improved management of depression by physicians) between selective and indicated prevention elements, but no reported linkages between universal and selective elements. These studies reported clear reductions in attempted suicide and death by suicide, but the changes in suicide rate with large sample sizes were less clear.
This suggests that selective and indicated interventions, and close linkages between the two, are more likely to affect suicide among older people. It also suggests that multilevel approaches with systematic linkages between levels of intervention are more likely to affect the suicide rate at the population level than those with partial or subtle linkages between universal and selective interventions, in particular.
Discussion
Our schematic diagram/framework integrates the stress-diathesis model (32), existing guidelines for identifying the critical time for interventions (31), and Gordon's preventive strategies framework (25). It therefore shows the relationship between the suicide process and suitable prevention strategies (29). Our model builds on that of Conwell et al. (28) by illustrating types of intervention strategy (2), possible linkages between interventions, and interventions related to risk factors from the stress-diathesis model (32). These risk factors are similar to those identified by Conwell et al. but focus on specific interventions rather than precise level of risk.
Practical Application of the Diagram
We hope that the diagram provides a framework to help practitioners and policy-makers to combine elements of intervention programs at different levels and produce more opportunities for effective intervention. This may, in particular, improve the detection of at-risk individuals, altering their progress through the suicide process, and resulting in fewer suicides.
Linking Interventions Across Preventive Levels
The model suggests that one reason why particular interventions may affect suicide rates may be whether the intervention is linked to others at different preventive levels. Linking interventions and levels may mean that preventive action can follow individual trajectories toward suicide more closely than separate interventions, and therefore alter these trajectories more effectively (29). For example, population-based studies of depression screening strategies and intervention among older individuals made a systematic link between universal, selective, and indicated prevention strategies (44). Rigorous community-based studies of interventions promoting regular telephone support and emergency response services among older clients (47), and encouraging physicians to attend gatekeeper training (46), linked selective and indicated strategies. These studies suggest that interventions involving assessment and management of mental illnesses associated with suicidal behaviors may be more effective if integrated with selective strategies targeting at-risk groups.
Other Effective Interventions
A number of studies, however, have identified effective interventions that were not linked to other types of prevention strategy. For example, meticulous population-based studies of universal interventions to encourage responsible media reporting and restricting access to suicidal means (17, 24) show that these interventions were not designed to be integrated with other strategies. Hospital-based studies of indicated prevention interventions, including follow-up care after suicide attempts (37, 54), suggest these interventions were also not integrated with other prevention strategies. Both these interventions were apparently effective, however, suggesting that other factors are also important in preventing suicide, such as individual risk factors.
Limitations and Suggestions for Future Research
The diagram's main weakness is the lack of evidence for the precise critical points in the suicide process. Interventions are probably more effective when targeted at particular risk factors in the stress-diathesis model (32), minimizing progression between stages. However, our model does not identify these precise risk factors, which may limit its practical use. Other weaknesses include the small number of studies used in testing. Using literature reviews to identify studies was convenient, and ensured that only validated studies were examined, but may have limited the number of studies available. Future researchers may wish to use a wider search strategy and include more studies.
Conclusions
Studies suggest that community interventions are important in reducing suicide in older adults, and that integrating universal, selective, and indicated prevention strategies may be crucial in this process. The most important relationship is probably between selective and indicated prevention interventions. These interventions are tailored to individual risk profiles, targeting those most at risk—for example, because they show signs of depression (9–11). They therefore make best use of scarce resources. Our diagram visualizes the relationships, and can help to ensure that strategies and resources are appropriately targeted and interlinked. We hope that the framework may help to improve the linkages between types of interventions, and support practitioners in developing a wide range of strategies across different areas and stages of the suicide process. It may also help policy-makers to take a more strategic approach to suicide prevention at a population level.
Author Contributions
TS and HO contributed equally to the literature review and manuscript preparation, including discussion.
Funding
This study was funded by the Ministry of Education, Culture, Sports, Science and Technology of Japan (Grants-in-Aid for Scientific Research No. 17K04208).
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer DH and handling editor declared their shared affiliation.
Acknowledgments
We thank Melissa Leffler, MBA, for editing a draft of this manuscript.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2019.00161/full#supplementary-material
References
1. Snowdon J, Phillips J, Zhong B, Yamauchi T, Chiu HF, Conwell Y. Changes in age patterns of suicide in Australia, the United States, Japan and Hong Kong. J Affect Disord. (2017) 211:12–9. doi: 10.1016/j.jad.2017.01.007
2. World Health Organization. Preventing Suicide: A Global Imperative. Geneva: World Health Organization (2014).
3. Hawton K, van Heeringen K. Suicide. Lancet. (2009) 373:1372–81. doi: 10.1016/S0140-6736(09)60372-X
4. Dombrovski AY, Szanto K, Duberstein P, Conner KR, Houck PR, Conwell Y. Sex differences in correlates of suicide attempt lethality in late life. Am J Geriatr Psychiatry. (2008) 16:905–13. doi: 10.1097/JGP.0b013e3181860034
5. Harwood DM, Hawton K, Hope T, Jacoby R. Suicide in older people: mode of death, demographic factors, and medical contact before death. Int J Geriatr Psychiatry. (2000) 15:736–43. doi: 10.1002/1099-1166(200008)15:8<736::AID-GPS214>3.0.CO;2-K
6. Salib E, Rahim S, El-Nimr G, Habeeb B. Elderly suicide: an analysis of coroner's inquests into two hundred cases in Cheshire 1989–2001. Med Sci Law. (2005) 45:71–80.
7. Conwell Y, Duberstein PR, Cox C, Herrmann J, Forbes N, Caine ED. Age differences in behaviors leading to completed suicide. Am J Geriatr Psychiatry. (1998) 6:122–6. doi: 10.1097/00019442-199805000-00005
8. Conwell Y, Thompson C. Suicidal behavior in elders. Psychiatr Clin North Am. (2008) 31:333–56. doi: 10.1016/j.psc.2008.01.004
9. Conwell Y. Suicide later in life: challenges and priorities for prevention. Am J Prev Med. (2014) 47:S244-50. doi: 10.1016/j.amepre.2014.05.040
10. Goldney RD, Dal Grande E, Fisher LJ, Wilson D. Population attributable risk of major depression for suicidal ideation in a random and representative community sample. J Affect Disord. (2003) 74:267–72. doi: 10.1016/S0165-0327(02)00017-4
11. Beautrais AL. A case control study of suicide and attempted suicide in older adults. Suicide Life Threat Behav. (2002) 32:1–9. doi: 10.1521/suli.32.1.1.22184
12. Kaplan MS, McFarland BH, Huguet N, Newsom JT. Physical illness, functional limitations, and suicide risk: a population-based study. Am J Orthopsychiatry. (2007) 77:56–60. doi: 10.1037/0002-9432.77.1.56
13. Waern M, Rubenowitz E, Runeson B, Skoog I, Wilhelmson K, Allebeck P. Burden of illness and suicide in elderly people: case-control study. Brit Med J. (2002) 324:1355. doi: 10.1136/bmj.324.7350.1355
14. Turvey CL, Conwell Y, Jones MP, Phillips C, Simonsick E, Pearson JL, Wallace R. Risk factors for late-life suicide: a prospective, community-based study. Am J Geriatr Psychiatry. (2002) 10:398–406. doi: 10.1097/00019442-200207000-00006
15. Rubenowitz E, Waern M, Wilhelmson K, Allebeck P. Life events and psychosocial factors in elderly suicides–a case-control study. Psychol Med. (2001) 31:1193–202. doi: 10.1017/S0033291701004457
16. Erlangsen A, Jeune B, Bille-Brahe U, Vaupel JW. Loss of partner and suicide risks among oldest old: a population-based register study. Age Ageing. (2004) 33:378–83. doi: 10.1093/ageing/afh128
17. Mann JJ, Apter A, Bertolote J, Beautrais A, Currier D, Haas A, et al. Suicide prevention strategies: a systematic review. JAMA. (2005) 294:2064–74. doi: 10.1001/jama.294.16.2064
19. Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE Jr. The interpersonal theory of suicide. Psychol Rev. (2010) 117:575–600. doi: 10.1037/a0018697
20. O'Conner R. Towards an integrated motivational-volitional model of suicidal behavior. In: O'Conner R, Platt S, Gordon J, editors, International Handbook of Suicide Prevention: Research, Policy and Practice. Chichester: John Wiley & Sons Ltd. (2011). p. 181–98.
21. Dwight EL, Foa EB, Gur RE, Hendin H, O'Brein CP, Seligman MEP, et al. Prevention of schizophrenia. In: Dwight EL, Foa EB, Gur RE, Hendin H, O'Brein CP, Romer D, Seligman MEP, Walsh BT, editors, Treating and Preventing Adolescent Mental Health Disorders. What We Know and What We Don't Know. A Research Agenda for Improving the Mental Health for our Youth. New York, NY: Oxford University Press USA (2005). p. 133–56.
22. Wasserman D, Wasserman C. Oxford Textbook of Suicidology and Suicide Prevention: A Global Perspective. New York, NY: Oxford University Press (2009). doi: 10.1093/med/9780198570059.001.0001
23. Pompili M, Tatarelli R. Evidence-Based Practice in Suicidology: A Source Book. Göttingen: Hogrefe Publishing (2011).
24. Zalsman G, Hawton K, Wasserman D, van Heeringen K, Arensman E, Sarchiapone M, et al. Suicide prevention strategies revisited: 10-year systematic review. Lancet Psychiatry. (2016) 3:646–59. doi: 10.1016/S2215-0366(16)30030-X
25. Gordon RS Jr. An operational classification of disease prevention. Public Health Rep. (1983) 98:107–9.
26. Mrazek PJ, Haggerty RJ. Reducing Risks from Mental Disorders: Frontiers for Preventive Intervention Research. Washington, DC: National Academy Press (1994).
27. Hegerl U, Rummel-Kluge C, Värnik A, Arensman E, Koburger N. Alliances against depression–a community based approach to target depression and to prevent suicidal behaviour. Neurosci Biobehav Rev. (2013) 37:2404–9. doi: 10.1016/j.neubiorev.2013.02.009
28. Conwell Y, Van Orden K, Caine ED. Suicide in older adults. Psychiatr Clin North Am. (2011) 34:451–68. doi: 10.1016/j.psc.2011.02.002
29. Sakashita T, Oyama H. Overview of community-based studies of depression screening interventions among the elderly population in Japan. Aging Ment Health. (2016) 20:231–9. doi: 10.1080/13607863.2015.1068740
30. Van Orden K, Deming C. Late-life suicide prevention strategies: current status and future directions. Curr Opin Psychol. (2017) 22:79–83. doi: 10.1016/j.copsyc.2017.08.033
31. Jenkins S, Singh B. General population strategies of suicide prevention. In Hawton K, van Heeringen K, editors. The International Handbook of Suicide and Attempted Suicide. New York, NY: Wiley. (2000). p 579–615.
32. Mann JJ. Neurobiology of suicidal behaviour. Nat Rev Neurosci. (2003) 4:819–28. doi: 10.1038/nrn1220
33. Sudak HS, Sudak DM. The media and suicide. Acad Psychiatry. (2005) 29:495–9. doi: 10.1176/appi.ap.29.5.495
34. Yip PS, Caine E, Yousuf S, Chang SS, Wu KC, Chen YY. Means restriction for suicide prevention. Lancet. (2012) 379:2393–9. doi: 10.1016/S0140-6736(12)60521-2
35. Fleischmann A, Arensman E, Berman A, Carli V, De Leo D, Hadlaczky G, et al. Overview evidence on interventions for population suicide with an eye to identifying best-supported strategies for LMICs. Glob Ment Health. (2016) 3:e5. doi: 10.1017/gmh.2015.27
36. Pirkis J, Too LS, Spittal MJ, Krysinska K, Robinson J, Cheung YT. Interventions to reduce suicides at suicide hotspots: a systematic review and meta-analysis. Lancet Psychiatry. (2015) 2:994–1001. doi: 10.1016/S2215-0366(15)00266-7
37. Milner AJ, Carter G, Pirkis J, Robinson J, Spittal MJ. Letters, green cards, telephone calls and postcards: systematic and meta-analytic review of brief contact interventions for reducing self-harm, suicide attempts and suicide. Br J Psychiatry. (2015) 206:184–90. doi: 10.1192/bjp.bp.114.147819
38. Lapierre S, Erlangsen A, Waern M, De Leo D, Oyama H, Scocco P, et al. A systematic review of elderly suicide prevention programs. Crisis. (2011) 32:88–98. doi: 10.1027/0227-5910/a000076
39. Chen YY, Wu KC, Yousuf S, Yip PS. Suicide in Asia: opportunities and challenges. Epidemiol Rev. (2012) 34:129–44. doi: 10.1093/epirev/mxr025
40. Dumesnil H, Verger P. Public awareness campaigns about depression and suicide: A review. Psychiatr Serv. (2009) 60:1203–13. doi: 10.1176/ps.2009.60.9.1203
41. Fountoulakis KN, Gonda X, Rihmer Z. Suicide prevention programs through community intervention. J Affect Disord. (2011) 130:10–6. doi: 10.1016/j.jad.2010.06.009
42. Matsubayashi T, Ueda M, Sawada Y. The effect of public awareness campaigns on suicides: evidence from Nagoya, Japan. J Affect Disord. (2014) 152-154:526–9. doi: 10.1016/j.jad.2013.09.007
43. Reynders A, Kerkhof AJ, Molenberghs G, Van Audenhove C. Attitudes and stigma in relation to help-seeking intentions for psychological problems in low and high suicide rate regions. Soc Psychiatry Psychiatr Epidemiol. (2014) 49:231–9. doi: 10.1007/s00127-013-0745-4
44. Oyama H, Sakashita T, Ono Y, Goto M, Fujita M, Koida J. Effect of community-based intervention using depression screening on elderly suicide risk: a meta-analysis of the evidence from Japan. Community Ment Health J. (2008) 44:311–20. doi: 10.1007/s10597-008-9132-0
45. Rutz W, von Knorring L, Walinder J. Long-term effects of an educational program for general practitioners given by the Swedish committee for the prevention and treatment of depression. Acta Psychiatr Scand. (1992) 85:83–8. doi: 10.1111/j.1600-0447.1992.tb01448.x
46. Szanto K, Kalmar S, Hendin H, Rihmer Z, Mann JJ. A suicide prevention program in a region with a very high suicide rate. Arch Gen Psychiatry. (2007) 64:914–20. doi: 10.1001/archpsyc.64.8.914
47. De Leo D, Dello Buono M, Dwyer J. Suicide among the elderly: the long-term impact of a telephone support and assessment intervention in northern Italy. Br J Psychiatry. (2002) 181:226–9. doi: 10.1192/bjp.181.3.226
48. Fiske A, Arbore P. Future directions in late life suicide prevention. Omega-J Death Dying. (2000) 42:37–53. doi: 10.2190/3T4G-T5U2-Q724-E0K8
49. Gould MS, Kalafat J, Harrismunfakh JL, Kleinman M. An evaluation of crisis hotline outcomes. Part 2: suicidal callers. Suicide Life Threat Behav. (2007) 37:338–52. doi: 10.1521/suli.2007.37.3.338
50. Szanto K, Mulsant BH, Houck P, Dew MA, Reynolds CF 3rd. Occurrence and course of suicidality during short-term treatment of late-life depression. Arch Gen Psychiatry. (2003) 60:610–7. doi: 10.1001/archpsyc.60.6.610
51. Nelson JC, Delucchi K, Schneider L. Suicidal thinking and behavior during treatment with sertraline in late-life depression. Am J Geriatr Psychiatry. (2007) 15:573–80. doi: 10.1097/JGP.0b013e318050c9c2
52. Bruce ML, Ten Have TR, Reynolds CF III, Katz II, Schulberg HC, Mulsant BH, et al. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: a randomized controlled trial. JAMA. (2004) 291:1081–91. doi: 10.1001/jama.291.9.1081
53. Unützer J, Tang L, Oishi S, Katon W, Williams JW Jr, Hunkeler E, et al. Reducing suicidal ideation in depressed older primary care patients. J Am Geriatr Soc. (2006) 54:1550–6. doi: 10.1111/j.1532-5415.2006.00882.x
54. Luxton DD, June JD, Comtois KA. Can postdischarge follow-up contacts prevent suicide and suicidal behavior? A review of the evidence. Crisis. (2013) 34:32–41. doi: 10.1027/0227-5910/a000158
55. Kawanishi C, Aruga T, Ishizuka N, Yonemoto N, Otsuka K, Kamijo Y, et al. Assertive case management versus enhanced usual care for people with mental health problems who had attempted suicide and were admitted to hospital emergency departments in Japan. (ACTION-J): a multicentre, randomised controlled trial. Lancet Psychiatry. (2014) 1:193–201. doi: 10.1016/S2215-0366(14)70259-7
56. Hepp U, Wittmann L, Schnyder U, Michel K. Psychological and psychosocial interventions after attempted suicide: an overview of treatment studies. Crisis. (2004) 25:108–17. doi: 10.1027/0227-5910.25.3.108
57. Hegerl U, Althaus D, Schmidtke A, Niklewski G. The alliance against depression: 2-year evaluation of a community-based intervention to reduce suicidality. Psychol Med. (2006) 36:1225–33. doi: 10.1017/S003329170600780X
58. Székely A, Konkolý Thege B, Mergl R, Birkás E, Rózsa S, et al. How to decrease suicide rates in both genders? An effectiveness study of a community-based intervention. (EAAD). PLoS ONE. (2013) 8:e75081. doi: 10.1371/journal.pone.0075081
Keywords: suicide, suicide prevention, suicide rate, older adults, Japan, hypothetical model
Citation: Sakashita T and Oyama H (2019) Developing a Hypothetical Model for Suicide Progression in Older Adults With Universal, Selective, and Indicated Prevention Strategies. Front. Psychiatry 10:161. doi: 10.3389/fpsyt.2019.00161
Received: 25 April 2018; Accepted: 05 March 2019;
Published: 26 March 2019.
Edited by:
Yari Gvion, Bar-Ilan University, IsraelCopyright © 2019 Sakashita and Oyama. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hirofumi Oyama, aF9veWFtYUBhdWh3LmFjLmpw
 Tomoe Sakashita
Tomoe Sakashita Hirofumi Oyama
Hirofumi Oyama