
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Psychiatry , 05 February 2019
Sec. Public Mental Health
Volume 10 - 2019 | https://doi.org/10.3389/fpsyt.2019.00032
Background: Many sex workers suffer from mental health problems, but do not seek help.
Aim: To examine stigma-related and non stigma-related barriers to care and perceived need for treatment among female sex workers in Switzerland.
Methods: Mental health service use, barriers to care, perceived need and presence of illness, symptoms, and psychiatric diagnoses were assessed among 60 female sex workers in Zürich, Switzerland.
Outcomes: Mental health service use was defined as use of psychiatric medication, psychotherapy, or substance use services for at least 1 month during the past 6 months.
Results: Adjusting for symptom levels, mental health service use was predicted by lower stigma-related, not by structural, barriers as well as by more perceived need for treatment and higher age.
Clinical Implications: Sex workers with mental health problems would benefit from non-stigmatizing mental health care as well as from interventions to reduce public and self-stigma associated with mental illness and sex work.
Strengths and Limitations: Limitations are the cross-sectional data, limited sample size, and recruitment from an information center for sex workers.
Conclusion: Interventions that aim to increase mental health service use among sex workers should take stigma variables into account.
Mental health problems are common among sex workers (1, 2). In a previous Swiss study one half of female sex workers reported at least one mental disorder in the past year (3), which is higher than the 12-month prevalence of about one third for any mental disorder in the general population (4). In the Swiss general population only about 7% of all women receive mental health care (5). Rates of mental health service use among female sex workers in Switzerland are unknown, but international data suggest that unmet health care needs are higher among sex workers than in the general population (6).
Many sex workers have a double stigmatized identity due to their work and common mental health problems (7). Despite high rates of unmet mental healthcare needs (6) specific interventions for sex workers with mental health problems are lacking. Previous research with sex workers suggested that instrumental barriers, e.g., lack of time or money, as well as stigma-related variables (fear of being labeled or shame) were a barrier to mental health service use (6, 7). Studies among people with mental illness outside the sex industry highlighted perceived need for treatment as a determinant of help-seeking (8).
Previous research on predictors of mental health service use among sex workers is inconclusive so far, and this especially applies to Europe. We therefore conducted a study among female sex workers in Switzerland to examine predictors of mental health service use. We expected that higher perceived need for treatment and lower stigma-related as well as non stigma-related barriers to care would predict help-seeking, adjusted for symptom levels.
Sixty female sex workers were recruited in a church-funded information center for sex workers in the inner-city red light district of Zürich, Switzerland. The center offers advice on health and prevention, legal issues, as well as assistance in dealing with paperwork and government agencies. German language courses and free lunch are also provided. There is no system of regular referrals of clients to mental health services. The study was approved by the local ethics committee (Kantonale Ethikkomission Zürich). All participants provided written informed consent and were reimbursed for their time during assessments. Participants were female and 18 years or above (M = 38.4 years, SD = 11.7). Most participants (n = 46, 78%) came from Hungary, Nigeria or Latin America. Work settings varied, including streets, bars and brothels.
All questionnaire data were collected during one-to-one interviews. Barriers to care were assessed using the 30-item Barriers to Access to Care Evaluation scale [BACE 9], rating barriers to professional care in the past 6 months from 0/not at all to 3/a lot. The BACE contains a 12-item stigma-related (M = 1.1; SD = 0.9; Cronbach's alpha 0.92; e.g., “feeling embarrassed or ashamed”) and an 18-item non-stigma-related subscale (structural and attitudinal barriers, M = 1.1, SD = 0.4; Cronbach's alpha 0.65; e.g., “thinking appointments take too much time or are inconvenient”). Perceived need for treatment and perceived presence of illness were measured with the 6-item Perceived Need for Treatment subscale and the 4-item Presence of Illness subscale of the Self-Appraisal of Illness Questionnaire (10), with higher mean scores from 1 to 4 indicating more perceived need (M = 2.4, SD = 0.8; alpha 0.87) or a perceived stronger presence of illness, respectively (M = 2.0, SD = 0.8; alpha 0.96).
Using a previously validated self-report measure of mental health service use (11), participants indicated whether or not, and for how long, they had used mental health care in the past 6 months in terms of psychiatric medication, psychotherapy/counseling, or substance use services. There was a bimodal distribution, i.e., most participants had used the respective service continuously over 6 months or not at all. For a logistic regression, we therefore created one dependent binary variable (using one or more of these three services not at all/only once, vs. continuously for 1–6 months). Psychopathology was assessed using a 9-item version of the Symptom Check List–Revised (12), and axis-I mental disorders with the Mini International Neuropsychiatric Interview (13).
Among all 60 participants, 20 (33%) had used mental health care continuously for at least 1 month during the past 6 months, while 40 (67%) had not. Out of those 45 with at least one psychiatric diagnosis, 20 (44% of 45) had used mental health care and 25 (56% of 45) had not. Forty-five (75%) participants had at least one mental disorder, most commonly affective or anxiety disorders. The most common diagnoses were major depression (n = 34, 54%), dysthymia (n = 25, 42%), and panic disorder (n = 22, 37%).
In a multiple logistic regression and adjusted for symptoms, mental health service use was predicted by a lower level of stigma-related, not of non-stigma related, barriers to care, by more perceived need for treatment, higher perceived presence of illness, and by higher age (Table 1; Nagelkerke's R2 = 0.73). The non-significant Hosmer-Lemeshow-Test (χ2 = 2.85, p = 0.94) indicates adequate model fit. The regression model correctly predicted 87% of those who did not, and 85% of those who did, use mental health services. When repeating the regression among only those 45 participants with at least one mental disorder, results remained largely unchanged (stigma-related barriers, p = 0.03; perceived need for treatment, p = 0.009; presence of illness, p = 0.07; symptoms, p = 0.09; age, p = 0.02).
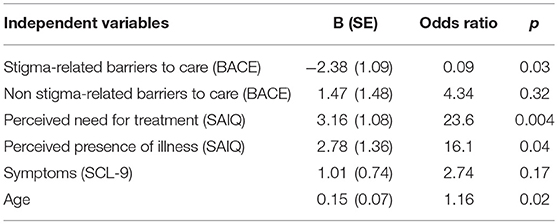
Table 1. Logistic regression on mental health service use (i.e., use of psychopharmacotherapy or psychotherapy or substance use services in the past 6 months, for at least 1 month; N = 60).
The prevalence of common mental disorders among female sex workers in our study was high, confirming a previous Swiss study (3), and elevated compared to the general population. The majority of participants, even of those with a manifest mental disorder, had not sought mental health care in the past 6 months. This can also be said about the Swiss general population (5), but it highlights the sizeable treatment gap in this particularly vulnerable population.
Our findings underline the role of stigma-related barriers to care while previous research focused on structural barriers, such as lack of time or financial resources (6); the latter were not associated with service use in our study. Interventions to increase mental health service use of female sex workers could therefore address stigma as a barrier to treatment. This could involve setting up non-stigmatizing mental health care environments as well as interventions to reduce self-stigma and shame. These interventions could also try to increase mental health literacy as a means to increase perceived need for treatment and knowledge about the benefits of available treatments (14).
Several limitations of our study need to be considered. Recruitment among sex workers, a fluctuating and hard-to-reach population, is notoriously difficult; due to recruitment from an information center our sample is unlikely to be representative and thus findings cannot be generalized. The cross-sectional data preclude conclusions on causality. Barriers to care were assessed by a generic measure, and information for barriers to care specific for sex workers was not collected. Finally, due to our limited sample size odds ratios in the regression model may be overestimated.
Despite these limitations, our study suggests that stigma and the subjective appraisal of illness are relevant barriers to care seeking. Interventions that aim to increase mental health service use among the vulnerable population of sex workers with mental health problems should target these variables.
Study participants provided written informed consent on the condition that their data would be available only to our research group. Therefore, data cannot be made publicly available.
MZ, JM, WR, and NR contributed to study design. MZ led recruitment and data collection, supported by JM and NR. MZ and NR analyzed the data. NR wrote the first draft of the manuscript. All authors contributed to the manuscript's content and read and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We are grateful to all participants.
1. Coetzee J, Buckley J, Otwombe K, Milovanovic M, Gray GE, Jewkes R. Depression and posttraumatic stress amongst female sex workers in Soweto, South Africa: a cross sectional, respondent driven sample. PLoS ONE (2018) 13:e0196759. doi: 10.1371/journal.pone.0196759
2. Carlson CE, Witte SS, Pala AN, Tsai LC, Wainberg M, Aira T. The impact of violence, perceived stigma, and other work-related stressors on depressive symptoms among women engaged in sex work. Global Soc Welfare (2017) 4:51–7. doi: 10.1007/s40609-017-0085-5
3. Rössler W, Koch U, Lauber C, Hass AK, Altwegg M, Ajdacic-Gross V, et al. The mental health of female sex workers. Acta Psychiatr Scand. (2010) 122:143–52. doi: 10.1111/j.1600-0447.2009.01533.x
4. Wittchen HU, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jönsson B, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacol. (2011) 21:655–79. doi: 10.1016/j.euroneuro.2011.07.018
5. Schuler D, Tuch A, Buscher N, Camenzind P. Psychische Gesundheit in der Schweiz, Monitoring 2016 (Obsan Bericht 72). Neuchâtel: Schweizerisches Gesundheitsobservatorium (2016).
6. Benoit C, Ouellet N, Jansson M. Unmet health care needs among sex workers in five census metropolitan areas of Canada. Can J Public Health (2016) 107:e266–e271. doi: 10.17269/cjph.107.5178
7. Benoit C, Jansson SM, Smith M, Flagg J. Prostitution stigma and its effect on the working conditions, personal lives, and health of sex workers. J Sex Res. (2018) 55:457–71. doi: 10.1080/00224499.2017.1393652
8. Bonabi H, Müller M, Ajdacic-Gross V, Eisele J, Rodgers S, Seifritz E, et al. Mental health literacy, attitudes to help-seeking and perceived need as predictors of mental health service use: a longitudinal study. J Nerv Mental Dis. (2016) 204:321–4. doi: 10.1097/NMD.0000000000000488
9. Clement S, Brohan E, Jeffery D, Henderson C, Hatch SL, Thornicroft G. Development and psychometric properties the Barriers to Access to Care Evaluation scale (BACE) related to people with mental ill health. BMC Psychiatry (2012) 12:36. doi: 10.1186/1471-244X-12-36
10. Marks KA, Fastenau PS, Lysaker PH, Bond GR. Self-Appraisal of Illness Questionnaire (SAIQ): relationship to researcher-rated insight and neuropsychological function in schizophrenia. Schizophrenia Res. (2000) 45:203–11. doi: 10.1016/S0920-9964(99)00208-X
11. Rüsch N, Corrigan PW, Wassel A, Michaels P, Larson JE, Olschewski M, et al. Self-stigma, group identification, perceived legitimacy of discrimination and mental health service use. Br J Psychiatry (2009) 195:551–2. doi: 10.1192/bjp.bp.109.067157
12. Klaghofer R, Brähler E. Konstruktion und teststatistische Prüfung einer Kurzform der SCL-90-R [Construction and statistical evaluation of a short version of the SCL-90-R]. Z Klin Psychol Psychiatr Psychother. (2001) 49:115–24.
13. Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry (1998) 59(Suppl. 20):22–33.
Keywords: sex work, prostitution, stigma, barriers to care, service use, mental health, perceived need for treatment
Citation: Zehnder M, Mutschler J, Rössler W, Rufer M and Rüsch N (2019) Stigma as a Barrier to Mental Health Service Use Among Female Sex Workers in Switzerland. Front. Psychiatry 10:32. doi: 10.3389/fpsyt.2019.00032
Received: 23 October 2018; Accepted: 18 January 2019;
Published: 05 February 2019.
Edited by:
Adriana Mihai, University of Medicine and Pharmacy of Târgu Mureş, RomaniaReviewed by:
Charles Bonsack, Lausanne University Hospital (CHUV), SwitzerlandCopyright © 2019 Zehnder, Mutschler, Rössler, Rufer and Rüsch. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nicolas Rüsch, bmljb2xhcy5ydWVzY2hAdW5pLXVsbS5kZQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.