
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 04 December 2018
Sec. Psychological Therapy and Psychosomatics
Volume 9 - 2018 | https://doi.org/10.3389/fpsyt.2018.00660
Objective: Outcome predictors and determinants for treatment outcome of inpatient psychotherapy will be assessed in a follow-up-study. Sociodemographic factors and the level of depressiveness at admission, the perceived psychotherapist's empathy rated by patients and the therapy motivation as possible moderators of treatment outcome (reduction of depressive symptoms) are analyzed.
Methods: In a cohort study, the outcome of inpatient multimodal psychotherapy was examined with Beck-Depression-Inventory (BDI) at admission (T1), discharge (T2) and at follow-up (1–3 years after treatment) (T3). Inclusion criteria were: Inpatient psychotherapy between 2007 and 2010 with a duration of at least 1 week and complete data set. The influence on therapy success of (1) sociodemographic factors, (2) the perceived psychotherapist's empathy rated by patients using the Consultation and Relational Empathy Measure (CARE), and (3) the therapy motivation of the patients rated by therapists are examined by means of correlation analysis, distribution comparisons and subsequently logistic regression.
Results: Ninety-two (64 females, average age 39 yrs.) of 182 eligible patients participated in the follow-up survey. Duration of inpatient psychotherapy lasted 8.7 weeks ± 3.6 [min. 1, max. 33 weeks]. The perceived psychotherapist's empathy, therapy motivation, education level and depression at baseline had a significant impact on therapy success. Gender, age, and partnership were not significant. The length between discharge and follow-up had no influence on the results. Based on these variables a multiple logistic regression explained 42% of the variation (goodness-of-fit).
Conclusion: Due to the shown relevance of the psychotherapist's empathy perceived by patients and the therapy motivation of patients for therapy success, both factors should be considered already at the beginning of the therapy. Consequently, they should be recognized in the context of postgraduate training and education.
The effectiveness of inpatient psychotherapy which in most cases is short-term psychotherapy has already been demonstrated in various studies in psychosomatic-psychotherapeutic acute and rehabilitation clinics with different outcomes (1–6).
Furthermore, numerous follow-up studies (catamnesis studies) showed positive long-term effects of inpatient psychotherapy (5, 7–10).
In recent years, predictors have also been identified in various studies for the treatment success of psychotherapy. Sociodemographic as well as disease and therapy-related factors could be identified as possible moderators of the therapy success. However, some controversial results were found or recognized.
Lambert and Barley (11) summarized the research on therapeutic relationship and psychotherapy outcome. In their research factors as empathy and the therapeutic relationship correlated more highly with outcome than specialized treatment interventions.
Previous studies in inpatient psychotherapy with a mixed patient sample showed no relationship between gender and therapy success (2, 5, 6, 12, 13). The relationship between age of the patient and therapy success is just as inconsistent as the relationship between partnership and therapy success (2, 5–7). Thus, Beutel et al. (5) could show in a comparative study design between inpatient short- and long-term therapy, that the lack of a stable partner is a negative predictor of therapy success in a long-term setting whereas the presence of a stable partnership has no significant effect on the success of inpatient psychotherapy (6, 12).
Riedel (14) showed that patients with a lower education level had a significantly lower therapy success. Hiller et al. (15) reported, that patients with lower education level showed more improvements in their symptoms during inpatient therapy for somatoform disorders than patients with a higher education level. In other studies the level of education had no influence on the therapy success (6, 16).
More obvious is the relationship between patients' therapy motivation and its therapy success. Previous studies have consistently concluded that therapy motivation is a major predictor of therapy success (6, 14, 17–20).
A number of studies have shown that patients who are depressed are significantly more likely to benefit from inpatient psychotherapy (2, 10, 21, 22). Patients with depressive disorder showed better therapy success than patients with other non-somatic diseases (6).
Bassler (7) showed that a lower level of depression at the beginning of therapy proved to be prognostically beneficial for therapy success. In contrast to this, a strong somatic comorbidity has an unfavorable effect on the therapy success (12). To sum it up the present findings on depression are inconsistent.
Patients with positive treatment outcome assessed the relationship with their therapists as good, while patients with worsened outcome also judged the therapeutic relationship more critically (23). The therapeutic relationship in an individual therapy has therefore been described by Sammet et al. (23) as a “relevant treatment component.” Bassler (24) also showed that the relationship between patient and therapist is a relevant criterion for the success of inpatient psychotherapy. In a study of Konzag et al. (25), the patient's evaluation of the therapeutic relationship was also an important prognostic factor for the outcome of inpatient psychotherapy.
The relationship between patient and therapist plays a decisive role for the success of the treatment, regardless of the therapeutic orientation or the school of therapy (26, 27).
Especially, Norcross and Wampold (28) focused on evidence-based therapy relationships. In a research based on meta-analyses, Norcross and Wampold reported several effective relationship elements, e.g., empathy and alliance in psychotherapy.
A positive therapeutic relationship is characterized by “empathic understanding” (29).
Berger (30) showed that the empathy of the therapist in the sense of “empathic compassion” as well as respect is of great importance for a successful psychotherapy. Similarly, Malin and Pos (31) and Watson et al. (32) showed the impact of empathy for the psychotherapeutic success.
Some studies on empathy perceived by the patient that is reflected in psychophysiological synchronization, e.g., Messina et al. (33), showed that shared psychophysiology can indeed represent an unbiased measure of empathy in terms of synchronization between patient and therapist. In particular, the study of Messina et al. (33) took into account the training of psychologists, showing that the more trained is the psychologist, the higher is the synchronization in clinical dyad.
Palmieri et al. (34) showed that psychophysiological synchronization [already proven to be a correlation of the patient's perceived empathy by the therapist as demonstrated by Messina et al.(33)] increases in the clinical dyad when the psychotherapist receives an induction to a mental state related to secure attachment. This means that, in addition to training, also other strategies related to positive mental states can increase the empathy perceived from patient by the therapist.
In a study of Barnicot (35) clinicians' empathy was significantly associated with lower depression severity during treatment.
However, the present findings on empathy as a predictor of therapy success are contradictory and depend among other factors on the measures used (36–38). The results of two meta-analyses (36, 39) regarding the relationship between empathy and psychotherapeutic outcome showed that empathy perceived by patients could significantly better predict therapy success than empathy assessed by therapist or observer. Empathy as a predictor of therapy success and as a determinant of quality was described not only especially for psychotherapeutic settings (40, 41), but also described for medical care generally (42).
Abbas et al. (43) published a Cochrane Review on short-term psychodynamic psychotherapies for common mental disorders. They identified different outcome measures for therapy success like general, somatic, anxiety and depression reduction.
The present study aims to determine predictors and determinants for therapy success in inpatient psychotherapy measured by reduction of depressiveness. Empathy of the therapist perceived by patients has not—or without using a validated questionnaire—been considered in previous studies of inpatient psychosomatic treatment. Therefore, in addition to sociodemographic factors such as gender, age, education, partnership, depression at beginning of therapy, therapy motivation, therapist's empathy perceived by patients is to be investigated as a possible influencing factor using the internationally validated CARE-questionnaire.
Consecutive patients of the psychotherapy inpatient ward of the Department for Psychosomatics and Psychotherapy, University Hospital of Cologne, were included in a retrospective cohort study including a follow-up assessment. Standardized patient questionnaires at T1 (inpatient admission), T2 (a few days before discharge) and T3 (follow-up, i.e., 10–38 months after discharge) were used. The psychotherapeutic intervention—according to the operations and procedures key for medical interventions (OPS key number 9-63 for so-called psychosomatic-psychotherapeutic complex treatment in German departments of psychosomatics and psychotherapy)1—consists in our clinic of the following elements:
• frequent psychodynamic psychotherapy in an individual-setting (2 sessions à 50 min weekly)
• psychodynamic psychotherapy in a group-setting (2 sessions of 60 min per week)
• psychodynamic movement psychotherapy in a small group-setting (2 sessions à 60 min a week)
• art therapy in a small group-setting (1 session à 125 min per week)
• music therapy in a small group-setting (2 sessions à 50 min per week)
• daily team rounds
• weekly visit of the head of the department with an indication conference
• participation in a somatic consultation session, which takes place at least once a week
• integration into a daily ward routine as well as regular therapeutic nursing care
• sports therapy, physiotherapy
• if necessary, disorder-specific treatments (e.g., pain, PTSD), diaries, imaginative exercises, mindfulness exercises or disturbance-specific elements in other disorders such as eating disorders or anxiety disorders.
From 2007 until 2010 the psychotherapists of our department are four long-term experienced physicians for psychiatry/psychosomatics with additional supervision. The study was approved by the Ethics Commission of Cologne University's Faculty of Medicine (code 09-263, 28th April, 2010). All subjects gave written informed consent in accordance with the Declaration of Helsinki.
Inclusion criteria were a hospital-stay of minimum 1 week (in the period from February 1, 2007 to December 31, 2010) as well as completed questionnaires for admission, discharge and follow-up for all questions relevant for the study. Subsequent stays of patients who were readmitted or who have had multiple inpatient stays during this period were excluded.
All questionnaires at T3 were sent to the patients by mail. In case of non-reply, a second postal sending of the questionnaires and repeated telephone call attempts were carried out according to the Dillman method (44).
At the time of hospital admission the patients completed the Psy-BaDo basic documentation on sociodemographic data according to Heuft and Senf (45). The Psy-BaDo therapist's questionnaire was also completed at admission. With this questionnaire, the therapist rated the patients' therapeutic motivation on a scale from 0 to 4 (0 = not motivated to 4 = very motivated). In addition, the questionnaire contains questions regarding the duration of complaints, referring clinician or institution, pre-treatment aspects, severity of impairment, symptoms according to ICD-10 and functional level.
To assess the severity of depression, the German version by Hautzinger et al. (46) of the Beck Depression Inventory (BDI) (47) was used at all three measurement times. The BDI is a valid, reliable and objective 21-question self-report inventory. It measures cognitive as well as affective, somatic, motivational and behavioral aspects. The symptoms of the last 8 days are rated by the patient on a four-level scale from 0 (nonexistent) to 3 (strong). For evaluation, the sum of the 21 items (0–63 points) is calculated and the degree of severity of the depression assessed. There are no depressive symptoms for sum scores below 10 points, 10–18 points indicate mild, 19–29 points moderate, and 30 or more points a severe depressive symptomatology.
The Consultation and Relational Empathy Measure (CARE) was used to measure patients' perceived empathy of the therapist at the time of T3. The one-dimensional CARE is a 10 item measure tool with good psychometric properties (48, 49). Four empathic components are described and assessed: emotive, moral, cognitive and behavioral aspects. Thus, the concept of empathy has to be distinguished from the purely emotional definition as well as from the concept of sympathy. Empathy is seen as a professional and learnable therapeutic ability (48, 50). Neumann et al. (50) developed a German version of CARE.
Nearly all of our patients in our heterogeneous sample suffered from depressiveness. Therefore, we decided to use depressiveness as marker of therapy success. The change in BDI (BDIΔT1/T3) was chosen as the main therapy outcome. Mean values of the BDI sum scores at admission (T1), discharge (T2), and follow-up (T3) were compared with the t-tests for paired samples.
The following variables were examined as possible predictors of therapy success: gender, age, level of education, partnership status, severity of depression (BDI at T1), therapy motivation (at T1) and patients' perceived empathy of the therapist at T3 (CARE Measure). To test if the BDI pre-treatment score contributes to a high percentage of explained variance a second regression analysis was performed without BDI at baseline. For identification of differences between patient groups with successful and less successful/unsuccessful therapy and to identify any predictors for this, the dependent variable (BDIΔT1/T3) was dichotomized by means of a typical (51) 1:2-split into two groups: 33.3% (no or only slight improvement in depressive symptoms) vs. 66.7% (clinically relevant improvement in depressive symptoms).
Correlations between any two variables were summarized by Spearman's rho correlation coefficient. We chose spearman's rho due to the apparent non-normality of data distributions. While equidistant scaling may aid in interpretation, it is not required for the coefficient to be a valid measure of the strength of a monotone relationship (between any two variables). Differences in distribution between any two variables were evaluated by Mann-Whitney U-test or Pearson's chi-square test, contingent on distributional characteristics. Subsequently, a stepwise logistic regression model was fitted with variables entered in two separate blocks. In the first block, the variables gender, age, level of education, partnership status, severity of depression (BDI at T1) and the duration of follow-up were entered. Therapy motivation (at T1) and patients' perceived empathy of the therapist (CARE Measure at T3) were entered in the second block (final logistic regression model). Additionally, bivariate analyses were performed to examine whether the patients who participated in the follow-up survey (T3) were different from those who had not participated. All analyses were performed with SPSS Statistics for Windows, version 22 (IBM Corp., Armonk, NY, United States). We visually checked the normality of data distributions as a requirement for using parametric tests.
Between 2007 and 2010 199 psychotherapy inpatients were treated.
In this cohort study 182 Patients are eligible (Figure 1). Seventeen patients have refused to participate in this study, 3 patients have died because of somatic diseases (no suicide), from 15 patients the new address was unknown and 55 patients did not respond. In the end, we could include 92 patients.
The sociodemographic and clinical characteristics of the sample are depicted in Figure 1.
In this study the patients have suffered from different mental disorders (Figure 1). The duration of inpatient psychotherapy lasted 8.7 weeks ± 3.6 [min. 1, max. 33 weeks]. The follow-up assessment has taken place 19.2 ±7.8 months [min. 10, max. 38 months].
After data cleaning 86 of 92 patients could be included in the analysis, i.e., 47.3% of the eligible patients. There are no significant differences regarding gender, age, education level, partnership status, therapy motivation, severity of depressive symptoms and duration of the follow-up between the patients who have participated in the follow-up and the patients who have not participated.
Nearly all patients showed depressive symptoms at the beginning of the treatment. Only 13 patients (7.6%) have BDI scores in the normal range. These patients were not excluded from analysis because an impairment of depression during the treatment was possible.
There was an unequivocal improvement of BDI sum scores between admission and discharge (BDIΔT1/T3; p < 0.001). At admission (T1) 92.4% of the patients (n = 159) revealed depressive symptoms in the BDI (42 patients [24.4%] mild, 75 patients [43.6%] moderate and 42 patients [24.4%] severe depressive symptoms) with a mean score of 23.1 ± 9.83 [0–50] and a median of 23.0. At discharge 46.7% of the patients (n = 72) were no longer depressed, 31.2% (n = 48) showed mild, 16.9% (n = 26) moderate and 5.2% (n = 8) severe depressive symptoms.
At T3 some patients demonstrated a small increase of depression. 39.2% of the patients (n = 36) were below the threshold regarding depressive symptoms, 29.3% (n = 27) revealed mild depressive symptoms, 17.4% (n = 16) moderate and 14.1% (n = 13) severe depressive symptoms (Figure 2).
Between admission and discharge a strong improvement of BDI sum scores could be demonstrated (p < 0.001; mean 10.52 ± 8.76, 95% CI 9.1; 11.9). Between admission and T3 (p < 0.001, mean 7.79 ± 11.32, 95% CI 5.4; 10.2) and between discharge and T3 (p = 0.005, mean −2.93 ± 9.10, 95% CI −4.9; −0.9) a significant improvement of BDI sum scores could be demonstrated.
Besides age, gender, education, existence of partnership and severity of depressive symptoms at the beginning of the therapy the variables therapy motivation and perceived empathy of the therapist at T3 and the BDI sum score between admission (T1) and follow-up (T3) were included in the correlational analyses. There were significant correlations between the outcome variable BDIΔT1/T3and the BDI sum scores at admission (Spearman-Rho: P = 0.024, r = −0.240), education (Spearman-Rho: P = 0.023, r = 0.242), therapy motivation (Spearman-Rho: P < 0.001, r = −0.368) and patient-reported empathy of therapist (or empathy of therapist assessed by patients (Spearman-Rho: P = 0.028, r = −0.237).
Results of bivariate analyses revealed significant differences concerning education level, level of BDI sum score at admission, perceived empathy of therapist and therapy motivation (Table 1).
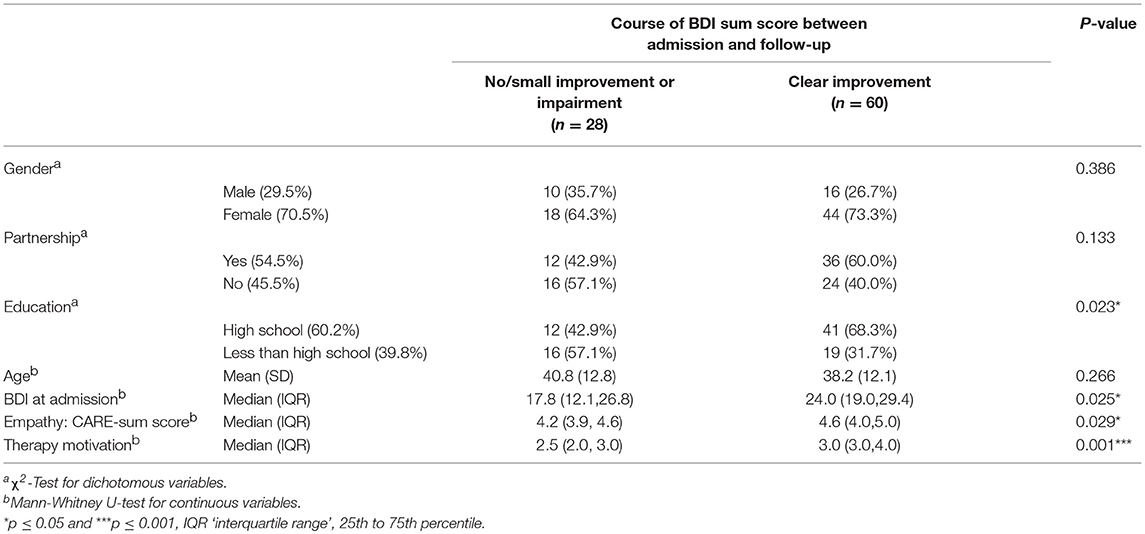
Table 1. Comparison of outcome variables “no/small improvement“ vs.” improvement of BDI sum score (BDIΔT1/T3).”
A moderator analysis was conducted to exclude a potential bias driven by depression severity at T1 on therapy motivation and perceived empathy of therapists. A possible relationship could be that patients with severe depressive symptoms when compared with patients who have a lower level of depression might perceive a lower level of therapist's empathy and/or a lower therapy motivation.
Therefore, a further dichotomous outcome variable was calculated to conduct an extreme group comparison: 25% of the worst results of change of BDI scores (missing improvement or impairment of BDI sum scores) were compared with the remaining 75% in regard to therapy motivation and CARE sum scores in Mann-Whitney-U-Tests. There were not any significant differences between both groups. Therefore, it seems that the severity of depression did not relevantly impact on the assessment of therapeutic empathy and therapy motivation.
In the first step of logistic regression analysis the sociodemographic parameters which are depicted (Table 2) could explain nearly 25% of the variance of therapy success “improvement of BDI sum score” (χ2 = 17.468, df = 6, p = 0.008, Nagelkerke R2 = 0.256), respectively, nearly 14% without BDI at baseline in the regression analysis (χ2 = 8.944, df = 5, p = 0.11, Nagelkerke R2 = 0.138). In the second step of logistic regression analysis the variables therapy motivation and perceived empathy (CARE sum score) were incorporated in the model. This model could explain nearly 42% of the variance of therapy success (χ2 = 13.855, df = 2, p = 0.001, Nagelkerke R2 = 0.426), respectively nearly 37 % without BDI at baseline in the regression analysis (χ2 = 17,898, df = 2, p < 0.001, Nagelkerke R2 = 0.374).
If the therapy motivation of the patient increased by one unit, the relative odds decreased by 61% that a person is part of the high risk group (worst third/ group “1”) (0.385–1 = −0.615).
If the perceived psychotherapist's empathy rated by the patient increased by one unit, the relative odds decreased by 65% that a person is part of the high risk group (worst third /group “1”) (0.346–1 = −0.654).
The entire model could predict 87.9% of the patients correctly who achieved an important improvement of depressive symptoms, and 57.1% of the patients who experienced no or only a small improvement. The quality of the model amounted to 77.9% of correctly classified cases. A predicted probability from the (multiple) logistic regression of 0.5 or greater was considered to indicate therapy success, thus 0.5 was chosen as the threshold for classifying cases.
This study aimed to detect predictors of therapy success. The effective treatment of depressive symptoms represents an important goal of the whole treatment and impact on the results of the therapy (2, 6, 15, 52, 53). Therefore, the change of depression over time has been chosen as dependent variable because nearly all included patients revealed depressive symptoms at admission.
Beside sociodemographic factors the perceived empathy of the therapist and the therapy motivation of the patient were assessed as possible predictors. Both attributes revealed a significant impact on therapy success. The first time we talk about empathy in psychotherapy corresponds to citations (29–42) in introduction, and some are recited here. The results corresponded to two meta-analyses in which empathy was assigned to have an impact of 10%, respectively 9% on therapy success (36, 39). Comparably to other studies concerning inpatient psychotherapy with mixed patient population the sociodemographic variables gender, age, education and partnership were not significant (2, 5–7, 12, 16). The above described final logistic regression model explained 42% of the variation. To control the impact of depression at baseline we excluded this variable and calculated a further regression analyses. The perceived empathy of the therapist and the therapy motivation still remained significant. The explained variation was likewise quite high (37%). Goodness-of-fit of the second step amounted to 80%, respectively nearly 75% correctly classified cases (model with respectively without BDI at baseline) which seems a very satisfiable value.
The innovative contribution of our study consists in the first-time use of “Consultation and Relational Empathy Measure” (CARE) for inpatient psychotherapy. Until now CARE was used exclusively in the somatic context.
Our study demonstrates that perceived empathy reveals a high significant predictor for the therapy success of multimodal inpatient psychotherapy: The higher the perceived empathy the better the therapy success. Earlier studies aiming at the impact of therapist's empathy on therapy success used other instruments like the Barrett-Lennard Relationship Inventory (BLRI) (31, 32, 39). Watson et al. (32) assessed the impact of perceived empathy assessed with the BLRI by depressed outpatients who were treated with cognitive behavior therapy.
Contrary to the studies of Konzag et al. (25, 54) who showed that empathy has no impact on the therapy success our study clearly demonstrates significant effects. However, Konzag et al. ascertained empathy by the therapists themselves and not from the point of view of the patients.
This discrepancy corresponds to the results of a meta-analysis of Elliot et al. (39) regarding the relationship between empathy and outcome in the psychotherapeutic context. They found that empathy which is perceived by patients could significantly better predict therapy success than empathy assessed by therapist or observer. Malin and Pos (31) also showed that therapists‘ expressed empathy significantly affected the outcome of therapy of depression (reduction of depressive symptoms). Watson et al. (32) showed a significant direct relationship between therapists' empathy and improvement of depression.
We could demonstrate that the application the “Consultation and Relational Empathy Measure” (CARE) is a useful tool in the measurement of psychosomatic and psychotherapeutic therapy success. Comparable to the usage of CARE in a somatic setting (50, 55–58) we could show that the empathy of the physician respectively of the therapist represents a strong influencing factor of the therapy success. On the other site it is quite important to perform research on empathy in somatic diseases and in the health system, too. For example, Decety and Fotopoulou (59) examined why empathy has a positive impact on others and briefly reviewed the various effects of empathy on health outcomes in the domain of medicine. Di Blasi et al. (60) showed that physicians with an empathic manner are more effective. According to a meta-analysis of Kelley et al. (61) the patient-clinician relationship has a significant effect on healthcare outcomes.
The therapy motivation of the patients—assessed by therapists at the beginning of the treatment—was a further important predictor of therapy success in our analysis. This result is in accordance with previous studies (6, 14, 17, 19, 20). Bleichhardt et al. (18) detected therapy motivation as positive predictor of therapy success. Klauer et al. (62) and Zwerenz et al. (63) investigated patients who terminated the inpatient psychotherapy ahead of time. At the beginning of the therapy these patients are strongly less motivated than other patients. It should be assessed in further studies whether initially weak motivation could be positively influenced in the first therapy sessions and could be interrelated to the therapy success (14, 19). Therefore, therapists should aim at a “positive sensitizing” of the patient for his/her psychotherapy already at the beginning of the therapy (17) to reduce potential prejudices against therapeutic measures. This should be done with an open, empathetic attitude in order to modify cognitive attitudes and to reduce existing anxieties of psychotherapy.
Beside the perceived empathy of the therapist and the therapy motivation of the patient the education level and the depression level ad admission also showed to have a significant impact on the therapy outcome.
In other studies the influence of the education level on therapy outcome was contrarily discussed. On the one hand, in the study of Riedel (14) patients with a low education level showed a significantly lower reduction of symptoms in psychotherapy. However, on the other hand, Hiller et al. (15) showed that a lower education level correlated with better symptom improvement. Other studies could not detect any relationship between education and therapy success (6, 16). In our study the influence of the education level was significant, but not prominent compared to therapy motivation and therapist's empathy. Our study showed a significant relationship between the level of depressive symptoms ad admission and therapy outcome. This is in accordance with other studies also showing a higher benefit for depressed patients (2, 10, 21, 22).
In this study, a heterogeneous sample regarding main diagnoses was enquired, not especially depressive disorders. Nevertheless, we chose the improvement of depressive symptomatology as indicator of therapy success because almost all patients showed depressive symptoms ad admission.
One limitation constitutes that the perceived empathy was first assessed at the follow-up of the survey. Nevertheless, there was the risk of patients giving socially desirable answers to questions during the inpatient psychotherapy. Additionally there were multiple therapeutic relationships that exist during the inpatient psychotherapy which could be characterized by empathy. Patients often report in the Psy-BaDo that the relationship to a single psychotherapist is of utmost importance. This is congruent to the results of two other studies (23, 24), in which just the single session psychotherapy was a relevant factor for the success of inpatient psychotherapy.
Furthermore, there is a limitation because of the relative broad range of the length of the follow-up. However, in our regression analysis we could demonstrate that there is no significant impact of the length of the follow-up on the improvement of depressiveness. Additionally, Fliege et al. (12) showed that the time interval between discharge and follow-up does not predict the results of therapy at follow-up.
A further limitation reveals the heterogeneity of the patient sample which constitutes a strength of the study in terms of the naturalistic study design. Because of missing data it could not be investigated how the perceived empathy was assessed by patients who did not participate in the study or who did interrupt their therapy in an early stage. It remains to be seen whether perceived empathy has an impact on the termination of the treatment and on the refusal of study participation. Furthermore, it has to be critically remarked that patients with good therapy success estimate the therapeutic relationship better when compared with patients who have less therapy success. From our point of view this could be transferred on perceived empathy. On the one hand the initially perceived empathy could foster the development of a good therapeutic relationship and contribute to the therapy success. On the other hand after a successful therapy the assessment of perceived empathy could be influenced positively in retrospect. It has to be emphasized that perceived empathy was not assessed during the inpatient psychotherapy but rather at follow-up. Our results could speak for an internalization of object relationship to the therapist as a sustained therapy effect. Furthermore, we have to consider that therapy motivation in our study was only assessed by the therapist and was not supplemented by a self-rating questionnaire of the patient. The question has to be posed which aspects of the patients influenced the perception of the therapist concerning the assessment of motivation. Nevertheless, the results showed unequivocally that the therapy motivation of the patient reveals a clear success criterion.
Therapy motivation of the patients at the beginning of the treatment as well as perceived empathy of the therapist by the patient seems to have a relevant impact on success of inpatient psychotherapy regarding the improvement of depressive symptomatology. Therapy motivation should therefore be assessed at the beginning of the therapy and be fostered by therapeutic procedures if necessary (17, 19).
Because of the strong influence of therapist's empathy the claim of other authors (27, 30) is justified to focus more on this ability in the postgraduate training of psychotherapists and in the context of supervision and special trainings. Summers presented a guide for a psychiatry residency psychodynamic therapy course (64). He described a model for teaching psychotherapy with empathy as important attitude for the building of a therapeutic alliance. It should be an essential aim for all psychotherapists to develop an empathetic attitude to the patient which could influence the therapy success in a positive manner.
Datasets are available on request. The raw data supporting the conclusions of this manuscript will be made available by the authors, without undue reservation, to any qualified researcher.
FV, ST, and OO contributed to the conception and design of the study. FV and ST organized the database. MH, FV, ST, and OO performed the statistical analysis. FV and ST wrote the first draft of the manuscript. OO, HP, CA, and MH wrote sections of the manuscript. All authors contributed to the manuscript revision, read and approved the submitted version.
FV was supported by the German Federal Ministry of Research and Education (BMBF grant 01KN1106). The sponsor had no involvement in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. ^DIMDI - OPS Operationen- und Prozedurenschlüssel http://www.dimdi.de/static/de/klassi/ops/index.htm (accessed Jul 29, 2018)
1. Grawe K, Donati R, Bernauer F. Psychotherapie im Wandel: Von der Konfession zur Profession Psychotherapy changinging: from denomination to profession. Goettingen: Hogrefe (1994).
2. Franz M, Janssen P, Lensche H, Schmidtke V, Tetzlaff M, Martin K, et al. Effekte stationärer psychoanalytisch orientierter Psychotherapie–eine Multizenterstudie On the effects of psychoanalytic oriented psychotherapy-an inpatient multicenter study. Z Psychosom Med Psychother. (2000) 46:242–58.
3. Mestel R, Erdmann A, Schmid N, Klingelhöfer J, Stauss K, Hautzinger M. “1-3 Jahres Katamnese bei 800 stationär behandelten depressiven Patienten. Catamnesis of 800 depressed patients 1-3 years after inpatient treatment,” In: Bassler M, editor. Leitlinien Zur Stationären Psychotherapie: Pro und Kontra. Gießen: Psychosozial Verlag (2000). p. 243–73.
4. Lempa W, Sack M, Lamprecht F, Schmid-Ott G. Individualized therapy goals and treatment efficacy – a follow-up study one year after inpatient psychotherapy. Z Für Psychosom Med Psychother. (2003) 49:63–73. doi: 10.13109/zptm.2003.49.1.63
5. Beutel ME, Hoeflich A, Kurth R, Brosig B, Gieler U, Leweke F, et al. Stationäre Kurz- und Langzeitpsychotherapie–Indikationen, Ergebnisse, Prädiktoren Short-term and long-term inpatient psychotherapy–indications, results, predictors. Z Für Psychosom Med Psychother. (2005) 51:145–62. doi: 10.13109/zptm.2005.51.2.145
6. Herrmann AS, Huber D. Was macht stationäre Psychotherapie erfolgreich? Der Einfluss von Patienten- und Behandlungsmerkmalen auf den Therapieerfolg in der stationären Psychotherapie The influence of patient- and treatment-related factors on the success of inpatient psychotherapy. Z Für Psychosom Med Psychother. (2013) 59:273–89. doi: 10.13109/zptm.2013.59.3.273
7. Bassler M. Evaluation der Differentiellen Wirkung von Psychoanalytisch Fundierter Stationärer Psychotherapie: Eine Studie zum Therapieerfolg mit 1-Jahres-Katamnese bei 295 Stationär Behandelten Patienten Evaluation of Differential Effects of Psychotherapy in Psychodynamic Inpatient Psychotherapy: A Study of Therapy Success With 1-Year-Catamnesis of 295 Patients in Inpatient Treatment. Postdoctoral Lecture Qualification. Mainz: Johannes Gutenberg-Universität. (1994) 1–148.
8. Junge A, Ahrens S. Inpatient psychosomatic treatment–patient markers and treatment success. Psychother Psychosom Med Psychol. (1996) 46:430–7.
9. Höflich A. Ergebnisse und Vorhersagemerkmale Einer Stationären Psychodynamischen Kurzzeit-Therapie. Results and Predictors of Inpatient Psychodynamic Short-term Therapy. dissertation. Gieße: University of Gießen. (2006) Available online at: http://geb.uni-giessen.de/geb/volltexte/2006/2795/pdf/HoeflichAnke-2006-02-20.pdf (Accessed October 29, 2016).
10. Huber D, Albrecht C, Hautum A, Henrich G, Klug G. Langzeit-Katamnese zur Effektivität einer stationären psychodynamischen Psychotherapie Effectiveness of inpatient psychodynamic psychotherapy: a follow-up study. Z Für Psychosom Med Psychother. (2009) 55:189–199. doi: 10.13109/zptm.2009.55.2.189
11. Lambert MJ, Barley DE. Research summary on the therapeutic relationship and psychotherapy outcome. Psychother Theory Res Pract Train (2001) 38:357–61. doi: 10.1037/0033-3204.38.4.357
12. Fliege H, Rose M, Bronner E, Klapp BF. Prädiktoren des Behandlungsergebnisses stationärer psychosomatischer Therapie Predicting long-term outcome of in-patient psychosomatic treatment. Psychother Psychosom Med Psychol. (2002) 52:47–55. doi: 10.1055/s-2002-20184
13. Cuijpers P, Weitz E, Twisk J, Kuehner C, Cristea I, David D, et al. Gender as predictor and moderator of outcome in cognitive behavior therapy and pharmacotherapy for adult depression: an “individual patient data” meta-analysis. Depress Anxiety (2014) 31:941–51. doi: 10.1002/da.22328
14. Riedel W-P. Einige Patientenmerkmale als Determinanten des Therapieerfolgs in der stationären Psychotherapie Some patient characteristics as determinants of the success of in-patient psychotherapy. Z Für Psychosom Med Psychoanal (1991) 37:14–30.
15. Hiller W, Fichter MM, Rief W. A controlled treatment study of somatoform disorders including analysis of healthcare utilization and cost-effectiveness. J Psychosom Res. (2003) 54:369–80. doi: 10.1016/S0022-3999(02)00397-5
16. Oster J, Müller G, von Wietersheim J. Wer profitiert?”– patientenmerkmale als erfolgsprädiktoren in der psychosomatischen rehabilitation “who profits?”–patient characteristics as outcome predictors in psychosomatic rehabilitation. Die Rehabil (2009) 48:95–102. doi: 10.1055/s-0029-1214411
17. Schneider W, Klauer T, Janssen PL, Tetzlaff M. Zum Einfluss der Psychotherapiemotivation auf den Psychotherapieverlauf Influence of psychotherapy motivation on the course of psychotherapy. Nervenarzt (1999) 70:240–9. doi: 10.1007/s001150050428
18. Bleichhardt G, Timmer B, Rief W. Prädiktoren für den direkten und längerfristigen Therapieerfolg bei Patienten mit somatoformen Störungen nach verhaltenstherapeutischer Behandlung Predictors of direct and long-term therapy success of patients with somatoform disorders after behaviour therapy. Z Für Klin Psychol Psychiatr Psychother. (2005) 1:40–58.
19. Nickel C, Muehlbacher M, Kettler C, Tritt K, Egger C, Lahmann C, et al. Behandlungsmotivation und Ergebnisse der stationären Psychotherapie bei Frauen mit depressiven Erkrankungen: eine prospektive Studie treatment motivation and results of inpatient psychotherapy for women with depressive disorders: a prospective study. Gesundheitswesen (2006) 68:11–17. doi: 10.1055/s-2005-859011
20. Zeeck A, von Wietersheim J, Weiss H, Scheidt CE, Völker A, Helesic A, et al. Prognostic and prescriptive predictors of improvement in a naturalistic study on inpatient and day hospital treatment of depression. J Affect Disord. (2016) 197:205–14. doi: 10.1016/j.jad.2016.03.039
21. Rudolf G, Jakobsen T, Micka R, Schumann E. Störungsbezogene Ergebnisse psychodynamisch-stationärer Psychotherapie Results of psychodynamic inpatient psychotherapy in relation to diagnosis. Z Für Psychosom Med Psychother. (2004) 50:37–52. doi: 10.13109/zptm.2004.50.1.37
22. Schützwohl M, Koch R, Kallert TW. Prädiktoren für den psychopathologischen entlassungsbefund bei akutpsychiatrischer, tagesklinischer und vollstationärer behandlung predictors of the discharge status in acute day–hospital and inpatient care. a comparison between the two settings within a randomised controlled trial. Psychiatr Prax (2006) 33:226–32. doi: 10.1055/s-2004-834757
23. Sammet I, Staats H, Schauenburg H. Beziehungserleben und Therapieergebnis in stationärer Psychotherapie Relationship experiences and therapeutic outcome in inpatient psychotherapy. Z Für Psychosom Med Psychother. (2004) 50:376–93. doi: 10.13109/zptm.2004.50.4.376
24. Bassler M. prognosefaktoren für den erfolg von psychoanalytisch fundierter stationärer psychotherapie prognostic factors for the success of psychoanalytically founded inpatient psychotherapy. Z Für Psychosom Med Psychoanal. (1995) 41:77–97.
25. Konzag T-A, Fikentscher E, Bandemer-Greulich U. Vernetzte evaluierung von prozess- und ergebnisqualität in der stationären psychotherapie-eine praktikabilitätsstudie-a cross-linked evaluation of the quality of processes and results in in-patient psychotherapy-a practicability study. Psychother Psychosom Med Psychol. (2000) 50:376–83. doi: 10.1055/s-2000-9097
26. Holm-Hadulla RM. Die therapeutische Beziehung the therapeutic relationship. Psychotherapeut (2000) 45:124–36. doi: 10.1007/s002780050211
27. Lammers PDC-H, Schneider W. Die therapeutische Beziehung the therapeutic relationship. Psychotherapeut (2009) 54:469–85. doi: 10.1007/s00278-009-0701-7
28. Norcross JC, Wampold BE. Evidence-based therapy relationships: research conclusions and clinical practices. Psychotherapy (2011) 48:98–102. doi: 10.1037/a0022161
29. Strupp HH. Ein zeitgemäßer Blick auf die psychodynamische Psychotherapie und deren Zukunft A contemporary view on psychodynamic psychotherapy and its future. Psychotherapeut (2000) 45:1–9. doi: 10.1007/PL00006717
30. Berger PDM. Die unterschiedlichen Facetten der Psychotherapie The various facets of psychotherapy. Neuropsychiatrie (2013) 27:63–5. doi: 10.1007/s40211-012-0044-4
31. Malin AJ, Pos AE. The impact of early empathy on alliance building, emotional processing, and outcome during experiential treatment of depression. Psychother Res. (2015) 25:445–59. doi: 10.1080/10503307.2014.901572
32. Watson JC, Steckley PL, McMullen EJ. The role of empathy in promoting change. Psychother Res. (2014) 24:286–98. doi: 10.1080/10503307.2013.802823
33. Messina I, Palmieri A, Sambin M, Kleinbub JR, Voci A, Calvo V. Somatic underpinnings of perceived empathy: the importance of psychotherapy training. Psychother Res. (2013) 23:169–177. doi: 10.1080/10503307.2012.748940
34. Palmieri A, Kleinbub JR, Calvo V, Benelli E, Messina I, Sambin M, et al. Attachment-security prime effect on skin-conductance synchronization in psychotherapists: an empirical study. J Couns Psychol. (2018) 65:490–9. doi: 10.1037/cou0000273
35. Barnicot K, Wampold B, Priebe S. The effect of core clinician interpersonal behaviours on depression. J Affect Disord. (2014) 167:112–7. doi: 10.1016/j.jad.2014.05.064
36. Bohart AC, Elliot RE, Greenberg LS, Watson JC. “Empathy,” In: Norcross J, editor. Psychotherapy Relationships that Work: Therapist Contributions and Responsiveness to Patients. Oxford: Oxford University Press (2002) 132–52.
37. Lange E, Hillebrand V, Pfäfflin PDF. Beschwerden über Therapeuten Complaints about therapists. Psychotherapeut (2009) 54:307–9. doi: 10.1007/s00278-009-0682-638
38. Kaczmarek D-PS, Passmann K, Cappel R, Hillebrand V, Schleu A, Strauß B. Wenn Psychotherapie schadet… Systematik von Beschwerden über psychotherapeutische Behandlungen When psychotherapy causes harm… Systematics of complaints on psychotherapeutic treatment. Psychotherapeut (2012) 57:402–9. doi: 10.1007/s00278-012-0916-x
39. Elliott R, Bohart AC, Watson JC, Greenberg LS. Empathy. Psychotherapy (2011) 48:43–9. doi: 10.1037/a0022187
40. Nienhuis JB, Owen J, Valentine JC, Winkeljohn Black S, Halford TC, Parazak SE, et al. Therapeutic alliance, empathy, and genuineness in individual adult psychotherapy: a meta-analytic review. Psychother Res. (2016) 28:593–605. doi: 10.1080/10503307.2016.1204023
41. MacFarlane P, Anderson T, McClintock AS. Empathy from the client's perspective: a grounded theory analysis. Psychother Res. (2017) 27:227–38. doi: 10.1080/10503307.2015.1090038
42. Neumann M, Bensing J, Mercer S, Ernstmann N, Ommen O, Pfaff H. Analyzing the “nature” and “specific effectiveness” of clinical empathy: a theoretical overview and contribution towards a theory-based research agenda. Patient Educ Couns. (2009) 74:339–46. doi: 10.1016/j.pec.2008.11.013
43. Abbass AA, Kisely SR, Town JM, Leichsenring F, Driessen E, Maat SD, et al. Short-term psychodynamic psychotherapies for common mental disorders. Cochrane Database Syst Rev. (2014) 18:CD004687. doi: 10.1002/14651858.CD004687.pub4
44. Hoddinott SN, Bass MJ. The dillman total design survey method. Can Fam Physician (1986) 32:2366–8.
45. Heuft G, Senf W. Praxis der Qualitätssicherung in der psychotherapie. das manual der psy-BaDo practice of quality assurance in psychotherapy. the manual of Psy-BaDo. Stuttgart (1998) 7–33.
46. Hautzinger M, Bailer M, Worall H, Keller F. Beck-Depressions-Inventar (BDI) Beck Depression Inventory (BDI). Manual. Testhandbuch. 2nd Edn. Bern: Huber (1995).
47. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry (1961) 4:561. doi: 10.1001/archpsyc.1961.01710120031004
49. Mercer SW, Maxwell M, Heaney D, Watt GC. The consultation and relational empathy (CARE) measure: development and preliminary validation and reliability of an empathy-based consultation process measure. Fam Pract. (2004) 21:699–705. doi: 10.1093/fampra/cmh621
50. Neumann M, Wirtz M, Bollschweiler E, Warm M, Wolf J, Pfaff H. Psychometrische Evaluation der deutschen Version des Messinstruments Consultation and Relational Empathy” (CARE) am Beispiel von Krebspatienten Psychometric Evaluation of the German Version of the “Consultation and Relational Empathy” (CARE) Measure at the Example of Cancer Patients. Psychother Psychosom Med Psychol. (2008) 58:5–15. doi: 10.1055/s-2007-970791
51. Dobbin KK, Simon RM. Optimally splitting cases for training and testing high dimensional classifiers. BMC Med Genomics (2011) 4:31. doi: 10.1186/1755-8794-4-31
52. Bossert S, Schmölz U, Wiegand M, Junker M, Krieg JC. Predictors of short-term treatment outcome in bulimia nervosa inpatients. Behav Res Ther. (1992) 30:193–199.
53. Salzer S, Stiller C, Tacke-Pook A, Jacobi C, Leibing E. Screening for Generalized Anxiety Disorder in inpatient psychosomatic rehabilitation: pathological worry and the impact of depressive symptoms. Psychosoc Med. (2009) 6:Doc02. doi: 10.3205/psm000058
54. Konzag TA, Bandemer-Greulich U, Bahrke U, Fikentscher E. Therapeutische Beziehung und Therapieerfolg bei der stationären Psychotherapie von Persönlichkeitsstörungen Psychotherapeutic relationship and outcome in psychotherapy of personality disorders. Z Für Psychosom Med Psychother. (2004) 50:394–405. doi: 10.13109/zptm.2004.50.4.394
55. Steinhausen S, Ommen O, Antoine S-L, Koehler T, Pfaff H, Neugebauer E. Short- and long-term subjective medical treatment outcome of trauma surgery patients: the importance of physician empathy. Patient Prefer Adherence (2014) 8:1239–53. doi: 10.2147/PPA.S62925
56. Steinhausen S, Ommen O, Thüm S, Lefering R, Koehler T, Neugebauer E, et al. Physician empathy and subjective evaluation of medical treatment outcome in trauma surgery patients. Patient Educ Couns. (2014) 95:53–60. doi: 10.1016/j.pec.2013.12.007
57. Neumann M, Wirtz M, Bollschweiler E, Mercer SW, Warm M, Wolf J, et al. Determinants and patient-reported long-term outcomes of physician empathy in oncology: a structural equation modelling approach. Patient Educ Couns. (2007) 69:63–75. doi: 10.1016/j.pec.2007.07.003
58. Mercer SW, McConnachie A, Maxwell M, Heaney D, Watt GCM. Relevance and practical use of the Consultation and Relational Empathy (CARE) Measure in general practice. Fam Pract. (2005) 22:328–34. doi: 10.1093/fampra/cmh730
59. Decety J, Fotopoulou A. Why empathy has a beneficial impact on others in medicine: unifying theories. Front Behav Neurosci. (2015) 8:457. doi: 10.3389/fnbeh.2014.00457
60. Di Blasi Z, Harkness E, Ernst E, Georgiou A, Kleijnen J. Influence of context effects on health outcomes: a systematic review. Lancet Lond Engl. (2001) 357:757–762. doi: 10.1016/S0140-6736(00)04169-6
61. Kelley JM, Kraft-Todd G, Schapira L, Kossowsky J, Riess H. The Influence of the patient-clinician relationship on healthcare outcomes: a systematic review and meta-analysis of randomized controlled trials. PLoS ONE (2014) 9:94207. doi: 10.1371/journal.pone.0094207
62. Klauer T, Maibaum F, Schneider W. Selbst- und fremdeinschätzungen der therapiemotivation als prädiktoren von behandlungsabbrüchen in der stationären psychotherapie patient and therapist reports of treatment motivation as predictors of dropout from inpatient psychotherapy. Z Für Psychiatr Psychol Psychother. (2007) 55:59–66. doi: 10.1024/1661-4747.55.1.59
63. Zwerenz R, Knickenberg RJ, Beutel ME. Behandlungsabbrüche in der stationären psychosomatischen Rehabilitation Dropout behavior in inpatient psychosomatic rehabilitation. Z Für Psychosom Med Psychother. (2008) 54:241–62. doi: 10.13109/zptm.2008.54.3.241
Keywords: depression, follow-up, inpatient psychotherapy, outcome predictors, treatment outcome
Citation: Vitinius F, Tieden S, Hellmich M, Pfaff H, Albus C and Ommen O (2018) Perceived Psychotherapist's Empathy and Therapy Motivation as Determinants of Long-Term Therapy Success—Results of a Cohort Study of Short Term Psychodynamic Inpatient Psychotherapy. Front. Psychiatry 9:660. doi: 10.3389/fpsyt.2018.00660
Received: 25 August 2018; Accepted: 19 November 2018;
Published: 04 December 2018.
Edited by:
Michael Noll-Hussong, Universitätsklinikum des Saarlandes, GermanyReviewed by:
Jean Marc Guile, University of Picardie Jules Verne, FranceCopyright © 2018 Vitinius, Tieden, Hellmich, Pfaff, Albus and Ommen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Frank Vitinius, ZnJhbmsudml0aW5pdXNAdWsta29lbG4uZGU=
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.