
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 14 March 2018
Sec. Psychopathology
Volume 9 - 2018 | https://doi.org/10.3389/fpsyt.2018.00084
Background: A diagnosis of psychotic disorder is traditionally considered incompatible with borderline personality disorder (BPD), even though patients sometimes fulfill the diagnostic criteria for both disorders. How often this happens is barely known, as is the influence of comorbid psychotic disorders on the outcome of BPD. Since studies on isolated auditory verbal hallucinations in patients with BPD indicate that these perceptual symptoms have severe consequences and are associated with suicidal behavior and hospitalization, patients with comorbid psychotic disorders are unlikely to fare better.
Objective: To examine the point prevalence of psychotic disorders in patients with BPD, their association with the outcome of BPD, and their predictive value for outcome.
Methods: In a cross-sectional design, 84 female outpatients diagnosed with BPD were interviewed with the aid of the MINI-International Neuropsychiatric Interview to establish the point prevalence of comorbid psychotic and other comorbid disorders. After termination of their treatment at a specialized outpatient clinic, the type of referral was considered to be a “good” outcome when they were referred to their general practitioner or to basic psychiatric care for noncomplex patients, and a “poor” outcome when referred to a specialized psychiatric department or to a psychiatric district team for patients with severe psychiatric disorders.
Results: Psychotic disorders were present in 38% of the patients with BPD. With a prevalence of 20%, psychotic disorder not otherwise specified (NOS) was the most common subtype; the least common types were schizophrenia (2%), substance-induced psychotic disorder (2%), and brief psychotic disorder (1%). Among six types of comorbid disorders, only psychotic disorders were associated with a poor outcome; they were also predictors for a poor outcome, along with comorbid mood disorders, eating disorders, and somatoform disorders, as well as the severity of BPD, and, counterintuitively, more years of education.
Conclusion: Psychotic disorders, notably of the psychotic disorder NOS subtype, are common among patients with BPD, and their presence is associated with a poor outcome. This implies that adequate diagnosis and treatment of both disorders is warranted in this subgroup with a dual diagnosis.
Borderline personality disorder (BPD) is conceptualized as a combination of affective dysregulation, impulsive/behavioral dyscontrol, disturbed interpersonal relatedness, and cognitive-perceptual symptoms (1–3). Symptoms of the latter include suspiciousness, ideas of reference, paranoid ideation, illusions, derealization, depersonalization, and hallucination-like symptoms. One of the criteria for BPD is that “transient, stress-related paranoid ideation may be present” (4). Moreover, psychotic features among patients with BPD are “by definition considered as mild and transient and hallucination-like in nature.” BPD is often accompanied by dissociation, intense episodes of anger, and suicidal ideation and behavior, resulting in functional impairment and increased health care utilization (2, 3, 5). Clinical studies indicate that BPD can also be accompanied by comorbid disorders such as mood and anxiety disorders, substance abuse disorders, and eating disorders (6–8). However, few data are available on the prevalence of psychotic disorders in patients with BPD. This is at least partly due to the fact that classifications such as the Diagnostic and Statistical Manual of Mental Disorders [DSM-5 (4)] and the International Classification of Diseases and Related Health Problems [ICD-10 (9)] stipulate that the presence of a major psychotic disorder precludes BPD as a diagnosis (10). This is unfortunate, as these disorders are characterized by different sets of symptoms and, moreover, hallucinations are experienced by 26–54% of patients diagnosed with BPD (11–14) and delusions by 17–29% (12, 13, 15). The additional burden caused by such psychotic symptoms is often substantial, as is demonstrated, for example, by increased levels of distress, more frequent suicide plans and attempts, and substantially higher needs for hospitalization in patients with BPD who also suffer from auditory verbal hallucinations (16).
Because so little is known about the co-occurrence of psychotic disorders and BPD, it is also unknown to what extent they determine the long-term outcome of BPD, which in itself can vary substantially, allowing patients to either live meaningful and fairly stable lives (whether or not with a partner, children, and a paid job) or end up in a secluded nursing ward with highly specialized care for the remainder of their lives. The long-term outcome of BPD has been investigated in two large-scale prospective cohort studies, i.e., the Collaborative Longitudinal Personality Disorders Study (17) and the McLean Study of Adult Development (18). In these studies, remission rates ranged from 30 to 50% by the second year of follow-up, to up to 80% by the tenth year, with the mean number of symptoms decreasing steadily over time. Despite these encouraging results, some 20% of the patients under study failed to recover substantially within 10 years. What distinguishes the latter patients from those who did recover is not fully known, even though many variables were found to affect the symptomatic outcome of BPD, including sociodemographic factors, severity of symptoms, personality traits, comorbid posttraumatic stress disorder (PTSD), and comorbid substance abuse disorders, whereas the co-occurrence of mood disorders, anxiety disorders, and eating disorders did not negatively affect outcome (19–21). However, since comorbid psychotic disorders, such as schizophrenia, were an exclusion criterium in the above-mentioned studies, their influence on the long-term outcome of BPD was not assessed.
As insight into the predictive factors for the outcome of BPD is urgently needed to allow for optimization of treatment and prevention of chronic hospitalization, the present study was designed to answer the following questions:
1. What is the point prevalence of comorbid psychotic disorders in patients diagnosed with BPD?
2. Is the long-term outcome of BPD associated with the presence of comorbid psychotic disorders?
3. Can individual disorders or conditions be identified that predict outcome in patients with BPD?
Patients with BPD, diagnosed in accordance with the criteria issued by the DSM-IV-TR (1) between May 2012 and March 2015, were recruited at the Department of Personality Disorders (an outpatient clinic specialized in the treatment of personality disorders) at Parnassia Psychiatric Institute, The Hague. Data collection for this study was part of a treatment protocol described in Niemantsverdriet et al. (14). All patients referred to the clinic were help seeking. The majority of patients were referred by their primary clinician and the remainder by other departments of Parnassia Psychiatric Institute. Criteria for inclusion were (i) a diagnosis of BPD as established with the aid of the Structural Clinical Interview for Axis II Personality Disorders (22), (ii) age ≥18 years, and (iii) written, informed consent. The study was approved by Parnassia’s Institutional Review Board (registration number 6237) in accordance with the Declaration of Helsinki.
For this cross-sectional study, the presence of psychotic disorders and other comorbid disorders was assessed with the aid of the MINI-International Neuropsychiatric Interview [MINI PLUS (23)]. Thus, the presence of seven groups of disorders at that moment was explored, comprising mood disorders (i.e., depressive disorder, bipolar disorder), anxiety disorders (i.e., panic disorder, agoraphobia, social phobia, obsessive-compulsive disorder, and general anxiety disorder), substance abuse disorders (i.e., alcohol dependence, alcohol abuse, substance (non-alcohol) abuse, and substance dependence), PTSD, eating disorders (i.e., anorexia nervosa and bulimia nervosa), somatoform disorders (i.e., hypochondriasis, body dysmorphic disorder, and pain disorder), and psychotic disorders (i.e., schizophrenia, schizoaffective disorder, schizophreniform disorder, brief psychotic disorder, delusional disorder, psychotic disorder due to a general medical condition, substance-induced psychotic disorder, psychotic disorder not otherwise specified (NOS), major depressive disorder with psychotic features, and bipolar I disorder with psychotic features). Thus, we defined psychotic disorders as disorders listed in the DSM-5 under the heading of Schizophrenia Spectrum and Other Psychotic Disorders, plus three diagnostic categories that were included in the MINI PLUS, i.e., psychotic disorders due to a medical condition, mood disorders with psychotic features, and substance abuse disorders with psychotic features. Kappa coefficient, sensitivity, and specificity were good or very good for all diagnoses (i.e., kappa coefficients varied from 0.76 to 0.93), with the exception of those for generalized anxiety disorder (kappa = 0.36), agoraphobia (sensitivity = 0.59), and bulimia nervosa (kappa = 0.53 (23)). Inter-rater and test-retest reliability were good.
Interviewers were two psychologists, two residents of psychology, and one resident of psychiatry who had been trained in conducting the MINI PLUS. They participated in monthly meetings to safeguard the inter-rater reliability during the inclusion phase.
At the outpatient clinic, patients generally remained under treatment as long as specialized psychiatric care was expected to enable further improvement of their BPD symptoms. When this could no longer be reasonably expected, each patient was offered four options for further care, comprising (i) referral to their general practitioner when psychiatric care was no longer necessary, (ii) referral to basic psychiatric care for noncomplex patients when they were expected to need ≤800 min of care per year, and crisis management was no longer necessary, (iii) referral to another specialized psychiatric department when treatment of a comorbid disorder was necessary, and (iv) referral to a psychiatric district team for patients with severe psychiatric disorders when the estimated duration of further treatment was ≥2 years, problems in psychosocial functioning were present, and adjuvant social care was needed. For the present study, outcomes (i) and (ii) were defined as “good” and outcomes (iii) and (iv) as “poor.” After termination of care at the outpatient clinic, the type of follow-up treatment for each individual patient could be retrieved from their electronic medical records.
Data analysis was performed with SPSS version 23 and R version 3.3.2. Demographic differences between the two groups were analyzed with Chi2 tests, t-tests for independent samples, and the Mann–Whitney U-test, as the duration of treatment was not normally distributed. Differences in outcome between the groups (i.e., good versus poor outcome) in relation to comorbid disorders were analyzed with Chi2 tests and odds ratios (OR). The Benjamini–Hochberg correction was used to correct for multiple testing (24). To search for predictive factors for good and poor outcome, a logistic regression analysis was performed. As the number of patients was relatively small, we applied elastic net regularization (25) using the glmnet package (26) within R (27). After exclusion of all cases with missing data, the dataset was changed into a dataset with all predictors, and a vector Y with the outcome variables. A regression analysis was conducted by penalizing regression coefficients to 0, i.e., by decreasing the variance of the predictors toward 0. Whenever a variable had regression coefficient 0, it was erased from the regression model. Two-dimensional cross-validation was used to explore which combination of penalization degree and mixture led to the smallest prediction error (28) applying the one-standard-error rule (29). The dependent value was outcome (i.e., good versus poor), whereas independent values were age, total years of education, total number of BPD criteria, and comorbid disorders.
Included were 84 female patients (and no male patients) with BPD; their demographic data are presented in Table 1. The treatment of all patients consisted of psychodynamic psychotherapy, cognitive-behavioral therapy, schema-focused therapy or dialectical behavior therapy, and supporting sessions, either individually or in a group. The choice of treatment depended on the patient’s capacity to participate within a group setting, their introspective ability, and the education of the therapist.
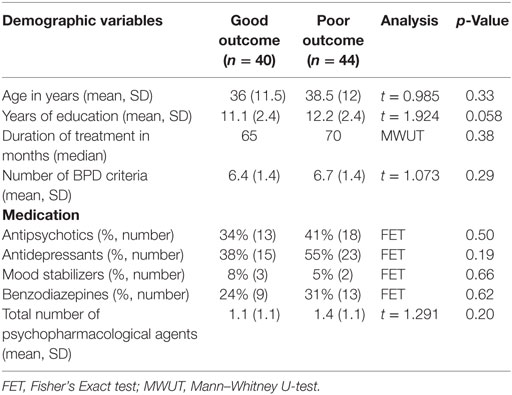
Table 1. Demographic data of patients with borderline personality disorder (BPD) with a good and bad long-term outcome.
In addition, many of the patients received medication, with half of those with a comorbid psychotic disorders using antipsychotics. Treatment duration ranged from 10 to 192 months, with 89% of the patients being under treatment for ≥24 months.
The point prevalence of comorbid disorders was 17–70%, with anxiety disorders being the most prevalent ones and eating disorders the least prevalent ones (Table 2). Psychotic disorders were present in 38% of the patients. With a point prevalence of 20%, psychotic disorder NOS was the most common of these, whereas schizophreniform disorder and mood disorders with psychotic features were present in 6 and 7% of the patients, respectively. Two patients (2%) fulfilled the criteria of schizophrenia and three (4%) the criteria of schizoaffective disorder.
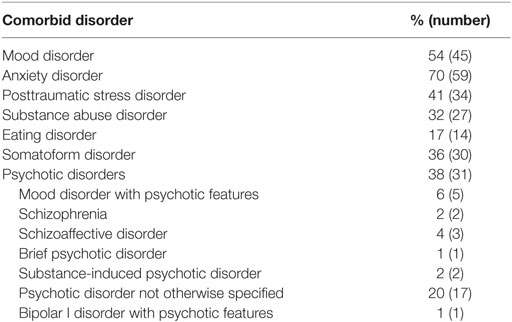
Table 2. Frequency of comorbid disorders present in at least one patient with borderline personality disorder (total group = 84 patients).
Of all 84 patients, 40 (48%) were identified as having a good outcome and 44 (52%) as having a poor outcome. No statistical difference was found between these two groups regarding demographic factors at baseline, use of medication, or duration of treatment. Table 3 shows the associations between all comorbid disorders and outcome. The association between psychotic disorders and outcome was significant (OR 3.0; 95% CI 1.175–7.657; p = 0.024) but was not significant for all other comorbid disorders.
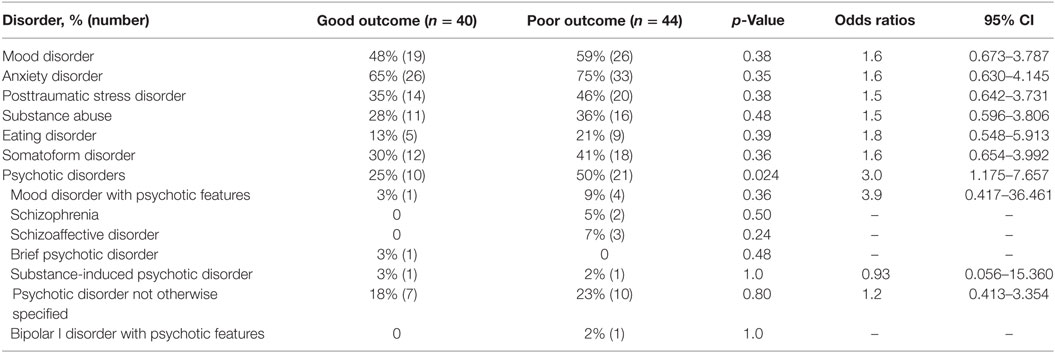
Table 3. Associations between outcome and comorbid disorders in at least one patient with borderline personality disorder (total group = 84 patients).
Regarding the logistic regression analysis, the variables that were preserved in the model with optimal penalization were mood disorders, psychotic disorders, eating disorders, somatoform disorders, more years of education, and total number of BPD criteria with the highest OR for eating disorders (Table 4).
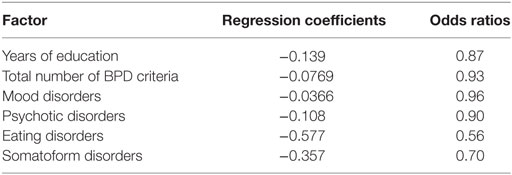
Table 4. Logistic regression analysis for age, total years of education, total number of borderline personality disorder (BPD) criteria, comorbid disorders, and outcome in patients with BPD.
This study investigated the point prevalence of psychotic disorders in 84 female patients diagnosed with BPD and the association of these disorders with outcome. In addition, other comorbid disorders, demographic variables, and the severity of BPD were explored as predictive factors for outcome. All seven groups of comorbid disorders that we assessed were represented in our sample, with prevalence rates ranging from 17% for eating disorders to 70% for anxiety disorders. Psychotic disorders were present in 38% of the patients, with psychotic disorder NOS as the most common variant (20%). Schizophrenia was present in 2% of the patients and schizoaffective disorder in 4%. Despite the high prevalence rate of mood disorders among patients with BPD (93%), mood symptoms did rarely contribute to a diagnosis of psychotic disorders. A significant correlation was found between psychotic disorders and (poor) outcome. Psychotic disorders also constituted a risk factor for poor outcome, along with mood disorders, eating disorders, and somatoform disorders, as well as the severity of BPD, and more years of education.
The relatively small numbers of patients diagnosed with schizophrenia and schizoaffective disorder are in accordance with the studies of Thompson et al. (30), Kingdon et al. (12), and Turner et al. (31). The remaining diagnostic categories of the group of psychotic disorders have hardly been studied in patients with BPD. In a prior study of 379 inpatients with BPD, 1.3% had a lifetime diagnosis of psychotic disorders, as established with the aid of the Structured Clinical Interview for DSM-III-R (7), with no further distinction being made for the specific type of psychotic disorder. Thompson et al. (30) explored the transition to psychosis within 24 months in 14 outpatients with an ultra-high risk for psychosis and BPD; of whom, 13% developed a schizophrenia spectrum disorder (i.e., schizophrenia, schizoaffective disorder, or schizophreniform disorder) and 10% “other psychotic disorders” (i.e., brief psychotic disorder, delusional disorder, psychotic disorder due to a medical condition, substance-induced psychotic disorder, or substance-induced mood disorder with manic features and psychotic disorder NOS); no differences in prevalence rates between these groups were reported. In a community population of 46 patients with non-suicidal self-injury and BPD, the lifetime prevalence of psychotic disorders was 4.5% (31). More specifically, schizoaffective disorder, substance-induced psychotic disorder, and psychotic disorder NOS were present in 2.3, 2.3, and 9.5% of the patients, respectively. Finally, in a study by Kingdon et al. (12) among 52 inpatients and outpatients with BPD, 37% had BPD as well as schizophrenia; the presence of other types of schizophrenia spectrum disorder was not investigated. “Exploring the presence of BPD in patients with schizophrenia reveals more or less similar prevalence rates, i.e., 2 to 7% (32–35).”
The present study is the first to report on the point prevalence of all types of psychotic disorders in conjunction with BPD. Although comorbidity of BPD with other disorders (such as mood, anxiety, and substance abuse disorders) has been assessed before (6), our findings indicate that the clinical impact of comorbid psychotic disorders is much more relevant for the outcome of BPD. According to our analysis, this group of disorders is associated with a poor outcome of BPD and is a predictor for poor outcome; however, for this finding, no comparison can be made due to lack of prior studies in this specific area. What is known, however, is that the presence of auditory verbal hallucinations in BPD is associated with a marked increase of suicidal plans and attempts and with more frequent hospitalization (16). Moreover, it is known that auditory verbal hallucinations in patients with BPD often have a relatively long duration (36, 37) and that their phenomenological characteristics (as well as the distress they evoke) are similar to those in patients diagnosed with schizophrenia (12, 36, 38).
In addition, we found that mood disorders, eating disorders, and somatoform disorders are predictors for a poor outcome of BPD. This is at odds with prior studies, the majority of which reported that comorbid disorders do not predict the outcome of BPD at all (19, 39–42). Incidentally, comorbidity with somatoform disorders was not assessed in these studies.
Thus, our findings for comorbidity with mood and eating disorders as predictors for a poor outcome of BPD are at odds with the majority of studies, whereas no comparison could be made with previous studies on the role of comorbid psychotic disorders and somatoform disorders. This is probably because previous studies did not include patients with more severe and/or complex personality disorders. Another reason might be that most earlier studies focused on lifetime prevalence rates for comorbid disorders, thereby yielding different results.
We do not think that the levels of comorbidity are the result of the specialized nature of the clinic, as our clinic is specialized in the treatment of personality disorders in general and offers no treatment specifically aimed at patients with BPD and psychotic features.
Our finding that also the severity of BPD is a predictive factor for outcome is in line with others (39, 43). Our final finding, that a greater number of years of education is a predictive factor for poor outcome, was based on a rather small difference in years of education between the two groups, i.e., a mean of 11.1 years for the group with a good outcome and 12.2 years for the group with a poor outcome. This finding is difficult to explain, as higher levels of education are generally viewed as predictors for success in life; therefore, replication of this finding is needed.
The present study has several limitations. First, only female patients with BPD were included in the analysis (since only four men had enrolled in the study); therefore, our findings cannot be generalized to men with BPD. Second, because this study had a cross-sectional design, no causal conclusions can be drawn. Third, the sample size of 84 patients was relatively small and may, therefore, have influenced the power of our study. Fourth, because we were unable to collect individual data on the type/types of psychotherapy that the patients had received, no distinction could be made regarding the influence of different forms of psychotherapy on outcome. Fifth, the MINI Neuropsychiatric Interview only assesses the presence of auditory and visual hallucinations and not other hallucinations such as tactile, olfactory, or gustatory hallucinations; the prevalence of psychotic disorder NOS might be higher if these hallucinations were included. Sixth, we did not explore the presence of schizotypal personality disorder. Seven percent of the patients with BPD also fulfill the criteria for a comorbid schizotypal personality disorder (8), which can also be accompanied by psychotic features. The aim of our study, however, was to explore the presence of psychotic disorders in a sample of patients with BPD as a primary diagnosis. We therefore recommend to direct future research at the additional value of schizotypal personality disorder within a population of patients with BPD and comorbid psychotic features. Finally, we did not assess the severity of psychiatric comorbidity, which has been associated with greater or lesser symptom improvement (39).
In addition, something that might be construed as a limitation (although in our opinion it is not) is the basic premise of our study, i.e., that BPD and psychotic disorders can be diagnosed simultaneously in individual patients, whereas diagnostic guidelines indicate that, in such cases, a diagnosis of psychotic disorders should prevail over BPD. The reason why we do not concur with this approach is that clinical practice indicates that patients can fulfill the diagnostic criteria of both disorders, that both disorders tend to show only few overlapping symptoms, and that both disorders require their own type of psychiatric treatment. That said, we agree that careful diagnosis is of ultimate importance in such cases and that, sometimes, patients may need to be rediagnosed when either of the two disorders is substantially more prominent than the other, or when patients initially diagnosed with BPD go on to develop a major psychotic disorder. Thus, in the present sample, the two patients diagnosed with “comorbid” schizophrenia and the three with schizoaffective disorder, might have to be relabeled at some point in time as suffering from schizophrenia or a related disorder, rather than from BPD. Nevertheless, this does not contradict the finding that, during our study, they did fulfill the diagnostic criteria of both disorders, and that the overwhelming majority of patients in our study did not fulfill the criteria for a major psychotic disorder.
Our findings imply that more attention should be paid to the presence of psychotic disorders in patients diagnosed with BPD and, if present, efforts should be directed at offering these patients specialized treatment for both disorders since both require different treatments, and outcome depends substantially on the presence or absence of a comorbid psychotic disorders. That said, the inevitable question of what type of treatment should be offered is not an easy one to answer, since little is known about the treatment of psychosis in patients with BPD. In clinical practice, only a minority of BPD patients receive treatment specifically aimed at their psychotic symptoms. This is reflected in our own patient sample, in which only half of those with a comorbid psychotic disorders were treated with antipsychotics. As an alternative, inspiration might be derived from the field of psychotic disorders, where many evidence-based interventions have been developed, including antipsychotics, cognitive-behavioral therapy, and transcranial magnetic stimulation (44, 45); of these three, only the effects of antipsychotics have been studied in patients with BPD and cognitive-perceptual symptoms, such as suspiciousness, referential thinking, paranoid ideation, derealization, depersonalization, illusions, and related perceptual symptoms (46). Three meta-analyses have shown small to moderate effect sizes of this approach (46–48). The reason why effect sizes were not larger might be due to the tendency of clinicians to prescribe relatively low doses of antipsychotics for patients with BPD. In the studies mentioned, the effects of antipsychotics on the severity of specific psychotic symptoms were not assessed. Taken cumulatively, these results indicate that there is a need for further studies on the efficacy of antipsychotics and other interventions for psychotic symptoms and disorders in patients with BPD, preferentially of a design that makes it possible to take the severity of symptoms into account. Regarding psychotherapeutic treatment for BPD with comorbid depression, a number of studies has shown mixed results (49–51), whereas a combined treatment for BPD and eating disorders yielded positive results (52, 53). So far, it is unknown whether other comorbid disorders improve during treatment of BPD, with or without adjuvant strategies specifically directed at them. Therefore, future studies should focus on these types of treatment in BPD with comorbid disorders.
In our sample, psychotic disorders, especially of the subtype of psychotic disorder NOS, affected 38% of the patients diagnosed with BPD. The presence of such comorbid disorders is associated with a poor outcome and even serves as a predictive factor for poor outcome, along with current mood, eating disorders, and somatoform disorders, the severity of BPD, and more years of education. These findings imply that more attention should be paid to the treatment of psychotic disorders and other comorbid disorders in patients with BPD.
The Stichting Medisch-Ethische Toetsingscommissie Instellingen Geestelijke Gezondheidszorg approved the protocol of this study, study number 6237, CCMO registration number NL1371209706, conform the Guidelines of Helsinki. The procedure was as follows, all documents were presented to this board, during a meeting all documents were discussed, and questions were formulated for the researchers. After the researchers had answered the questions, approval was given to conduct this study.
CS and MN contributed to the conception and design of the work and to the acquisition, analysis, and interpretation of data for the work, drafted and revised the work, gave final approval for the final version to be published, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. JB and IS contributed to the conception and design of the work and to the analysis and interpretation of data for the work, revised the work, gave final approval for the final version to be published, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. MD contributed to the analysis and interpretation of data for the work, revised the work, gave final approval for the final version to be published, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
This study was supported by NWO ZonMW (Dutch Organisation for Scientific Research—Dutch Organisation for Health Research and Development, grant number 100002033) and Stichting tot Steun (Foundation for Support, grant number 3125).
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington, DC: American Psychiatric Association (2000).
2. Skodol AE, Gunderson JG, McGlashan TH, Dyck IR, Stout RL, Bender DS, et al. Functional impairment in patients with schizotypal, borderline, avoidant, or obsessive-compulsive personality disorder. Am J Psychiatry (2002) 159:276–83. doi:10.1176/appi.ajp.159.2.276
3. Skodol AE, Gunderson JG, Pfohl B, Widiger TA, Livesley WJ, Siever LJ. The borderline diagnosis: psychopathology, comorbidity, and personality structure. Biol Psychiatry (2002) 51:936–50. doi:10.1016/S0006-3223(02)01324-0
4. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Washington, DC: American Psychiatric Association (2013).
5. Soeteman DI, Hakkaart-van Roijen L, Verheul R, Busschbach JJ. The economic burden of personality disorders in mental health care. J Clin Psychiatry (2008) 69:259–65. doi:10.4088/JCP.v69n0212
6. Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry (2008) 69:533–45. doi:10.4088/JCP.v69n0404
7. Zanarini MC, Frankenburg FR, Dubo ED, Sickel AE, Trikha A, Levin A, et al. Axis I comorbidity of borderline personality disorder. Am J Psychiatry (1998) 155:1733–9. doi:10.1176/ajp.155.12.1733
8. Zanarini MC, Frankenburg FR, Dubo ED, Sickel AE, Trikha A, Levin A, et al. Axis II comorbidity of borderline personality disorder. Compr Psychiatry (1998) 39:296–302. doi:10.1016/S0010-440X(98)90038-4
9. World Health Organization. International Classification of Diseases and Related Health Problems, Tenth Revised Edition. Geneva: World Health Organization (2008).
10. Schroeder K, Fisher HL, Schäfer I. Psychotic symptoms in patients with borderline personality disorder: prevalence and clinical management. Curr Opin Psychiatry (2013) 26:113–9. doi:10.1097/YCO.0b013e32835a2ae7
11. Chopra HD, Beatson JA. Psychotic symptoms in borderline personality disorder. Am J Psychiatry (1986) 143:1605–7. doi:10.1176/ajp.143.12.1605
12. Kingdon DG, Ashcroft K, Bhandari B, Gleeson S, Warikoo N, Symons M, et al. Schizophrenia and borderline personality disorder: similarities and differences in the experience of auditory hallucinations, paranoia, and childhood trauma. J Nerv Ment Dis (2010) 198:399–403. doi:10.1097/NMD.0b013e3181e08c27
13. Links PS, Steiner M, Mitton J. Characteristics of psychosis in borderline personality disorder. Psychopathology (1989) 22:188–93. doi:10.1159/000284595
14. Niemantsverdriet MBA, Slotema CW, Blom JD, Franken IH, Hoek HW, Sommer IEC, et al. Hallucinations in borderline personality disorder: prevalence, characteristics and associations with comorbid symptoms and disorders. Sci Rep (2017) 7:13920. doi:10.1038/s41598-017-13108-6
15. Pearse LJ, Dibben C, Ziauddeen H, Denman C, McKenna PJ. A study of psychotic symptoms in borderline personality disorder. J Nerv Ment Dis (2014) 202:368–71. doi:10.1097/NMD.0000000000000132
16. Slotema CW, Niemantsverdriet MB, Blom JD, van der Gaag M, Hoek HW, Sommer IE. Suicidality and hospitalisation in patients with borderline personality disorder who experience auditory verbal hallucinations. Eur Psychiatry (2017) 41:47–52. doi:10.1016/j.eurpsy.2016.10.003
17. Skodol AE, Gunderson JG, Shea MT, McGlashan TH, Morey LC, Sanislow CA, et al. The Collaborative Longitudinal Personality Disorders Study (CLPS): overview and implications. J Pers Disord (2005) 19:487–504. doi:10.1521/pedi.2005.19.5.487
18. Zanarini MC, Frankenburg FR, Hennen J, Reich DB, Silk KR. Prediction of 10-year course of borderline personality disorder. Am J Psychiatry (2006) 163:827–32. doi:10.1176/ajp.2006.163.5.827
19. Gunderson JG, Daversa MT, Grilo CM, McGlashan TH, Zanarini MC, Shea MT, et al. Predictors of 2-year outcome for patients with borderline personality disorder. Am J Psychiatry (2006) 163:822–6. doi:10.1176/ajp.2006.163.5.822
20. Zanarini MC, Frankenburg FR, Hennen J, Reich DB, Silk KR. Axis I comorbidity in patients with borderline personality disorder: six-year follow-up and prediction of time to remission. Am J Psychiatry (2004) 161:2108–14. doi:10.1176/appi.ajp.161.11.2108
21. Zanarini MC, Frankenburg FR, Vujanovic AA, Hennen J, Reich SB, Silk KR. Axis II comorbidity in patients with borderline personality disorder: description of six-year course and prediction of time to remission. Acta Psychiatr Scand (2004) 110:416–20. doi:10.1111/j.1600-0447.2004.00362.x
22. First MV, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. User’s Guide for the Structured Clinical Interview for DSM-IV Axis II Personality Disorders. Washington, DC: American Psychiatric Press (1997).
23. Sheehan DV, Lecrubier Y, Harnett Sheehan K, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry (1998) 59(Suppl 20):22–33.
24. Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B Stat Methodol (1995) 57:289–300.
25. Zou H, Hastie T. Regularization and variable selection via the elastic net. J R Stat Soc Series B Stat Methodol (2005) 67:301–20. doi:10.1111/j.1467-9868.2005.00527.x
26. Friedman J, Hastie T, Tibshirani R. Regularization paths for generalized linear models via coordinate descent. J Stat Softw (2010) 33:1–22. doi:10.18637/jss.v033.i01
27. R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing (2016).
28. Hastie T, Tibshirani R, Friedman J. The Elements of Statistical Learning: Data Mining, Inference and Prediction. 2nd ed. NY, USA: Springer Verlag (2009). p. 662–4.
29. Breiman L, Friedman J, Olshen R, Stone C. Classification and Regression Trees. NY, USA: Wadsworth (1984).
30. Thompson A, Nelson B, Bechdolf A, Chanen AM, Domingues I, McDougall E, et al. Borderline personality features and development of psychosis in an ‘ultra high risk’ (UHR) population: a case control study. Early Interv Psychiatry (2012) 6:247–55. doi:10.1111/j.1751-7893.2012.00365.x
31. Turner BJ, Dixon-Gordon KL, Austin SB, Rodriguez MA, Rosenthal MZ, Chapman AL. Non-suicidal self-injury with and without borderline personality disorder: differences in self-injury and diagnostic comorbidity. Psychiatry Res (2015) 230:28–35. doi:10.1016/j.psychres.2015.07.058
32. Wei YY, Zhang TH, Chow A, Tang YY, Xu L, Dai YF, et al. Co-morbidity of personality disorder in schizophrenia among psychiatric outpatients in China: data from epidemiologic survey in a clinical population. BMC Psychiatry (2016) 16:224. doi:10.1186/s12888-016-0920-8
33. Solano JJR, De Chavez MG. Premorbid personality disorders in schizophrenia. Schizophr Res (2000) 44:137–44. doi:10.1016/S0920-9964(99)00203-0
34. Keshavan MS, Duggal HS, Veeragandham G, McLaughlin NM, Montrose DM, Haas GL, et al. Personality dimensions in first-episode psychoses. Am J Psychiatry (2005) 162:102–9. doi:10.1176/appi.ajp.162.1.102
35. Hogg B, Jackson HJ, Rudd RP, Edwards J. Diagnosing personality disorders in recent-onset schizophrenia. J Nerv Ment Dis (1990) 178:194–9. doi:10.1097/00005053-199003000-00007
36. Slotema CW, Daalman K, Blom JD, Diederen KM, Hoek HW, Sommer IEC. Auditory verbal hallucinations in patients with borderline personality disorder are similar to those in schizophrenia. Psychol Med (2012) 42:1873–8. doi:10.1017/S0033291712000165
37. Yee L, Korner AJ, McSwiggan S, Meares RA, Stevenson J. Persistent hallucinosis in borderline personality disorders. Compr Psychiatry (2005) 46:147–54. doi:10.1016/j.comppsych.2004.07.032
38. Tschoeke S, Steinert T, Flammer E, Uhlmann C. Similarities and differences in borderline personality disorder and schizophrenia with voice hearing. J Nerv Ment Dis (2014) 202:544–9. doi:10.1097/NMD.0000000000000159
39. Barnicot K, Katsakou C, Bhatti N, Savill M, Fearns N, Priebe S. Factors predicting the outcome of psychotherapy for borderline personality disorder: a systematic review. Clin Psychol Rev (2012) 32:400–12. doi:10.1016/j.cpr.2012.04.004
40. Bateman A, Fonagy P. Effectiveness of partial hospitalization in the treatment of borderline personality disorder: a randomized controlled trial. Am J Psychiatry (1999) 156:1563–9. doi:10.1176/ajp.156.10.1563
41. Barnicot K, Priebe S. Post-traumatic stress disorder and the outcome of dialectical behaviour therapy for borderline personality disorder. Personal Ment Health (2013) 7:181–90. doi:10.1002/pmh.1227
42. Black DW, Allen J, St John D, Pfohl B, McCormick B, Blum N. Predictors of response to systems training for emotional predictability and problem solving (STEPPS) for borderline personality disorder: an exploratory study. Acta Psychiatr Scand (2009) 120:53–61. doi:10.1111/j.1600-0447.2008.01340.x
43. Arntz A, Stupar-Rutenfrans S, Bloo J, van Dyck R, Spinhoven P. Prediction of treatment discontinuation and recovery from borderline personality disorder: results from an RCT comparing schema therapy and transference focused psychotherapy. Behav Res Ther (2015) 74:60–71. doi:10.1016/j.brat.2015.09.002
44. Sommer IEC, Slotema CW, Daskalakis ZJ, Derks EM, Blom JD, van der Gaag M. The treatment of hallucinations in schizophrenia spectrum disorders. Schizophr Bull (2012) 38:704–14. doi:10.1093/schbul/sbs034
45. Slotema CW, Blom JD, Hoek HW, Sommer IEC. Should we expand the toolbox of psychiatric treatment methods to include repetitive transcranial magnetic stimulation (rTMS)? A meta-analysis of the efficacy of rTMS in psychiatric disorders. J Clin Psychiatry (2010) 71:873–84. doi:10.4088/JCP.08m04872gre
46. Ingenhoven T, Lafay P, Rinne T, Passchier J, Duivenvoorden H. Effectiveness of pharmacotherapy for severe personality disorders: meta-analyses of randomized controlled trials. J Clin Psychiatry (2010) 71:14–25. doi:10.4088/JCP.08r04526gre
47. Ingenhoven TJ, Duivenvoorden HJ. Differential effectiveness of antipsychotics in borderline personality disorder: meta-analyses of placebo-controlled, randomized clinical trials on symptomatic outcome domains. J Clin Psychopharmacol (2011) 31:489–96. doi:10.1097/JCP.0b013e3182217a69
48. Lieb K, Völlm B, Rücker G, Timmer A, Stoffers JM. Pharmacotherapy for borderline personality disorder: cochrane systematic review of randomised trials. Br J Psychiatry (2010) 196:4–12. doi:10.1192/bjp.bp.108.062984
49. Blum N, St John D, Pfohl B, Stuart S, McCormick B, Allen J, et al. Systems training for emotional predictability and problem solving (STEPPS) for outpatients with borderline personality disorder: a randomized controlled trial and 1-year follow-up. Am J Psychiatry (2008) 165:468–78. doi:10.1176/appi.ajp.2007.07071079
50. Rossouw TI, Fonagy P. Mentalization-based treatment for self-harm in adolescents: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry (2012) 51:1304–13. doi:10.1016/j.jaac.2012.09.018
51. Neacsiu AD, Eberle JW, Kramer R, Wiesmann T, Linehan MM. Dialectical behavior therapy skills for transdiagnostic emotion dysregulation: a pilot randomized controlled trial. Behav Res Ther (2014) 59:40–51. doi:10.1016/j.brat.2014.05.005
52. Kröger C, Schweiger U, Sipos V, Kliem S, Arnold R, Schunert T, et al. Dialectical behaviour therapy and an added cognitive behavioural treatment module for eating disorders in women with borderline personality disorder and anorexia nervosa or bulimia nervosa who failed to respond to previous treatments. An open trial with a 15-month follow-up. J Behav Ther Exp Psychiatry (2010) 41:381–8. doi:10.1016/j.jbtep.2010.04.001
Keywords: comorbidity, outcome, predictive value, prevalence, psychotic disorder
Citation: Slotema CW, Blom JD, Niemantsverdriet MBA, Deen M and Sommer IEC (2018) Comorbid Diagnosis of Psychotic Disorders in Borderline Personality Disorder: Prevalence and Influence on Outcome. Front. Psychiatry 9:84. doi: 10.3389/fpsyt.2018.00084
Received: 25 November 2017; Accepted: 01 March 2018;
Published: 14 March 2018
Edited by:
Drozdstoy Stoyanov Stoyanov, Plovdiv Medical University, BulgariaReviewed by:
Diane Carol Gooding, University of Wisconsin-Madison, United StatesCopyright: © 2018 Slotema, Blom, Niemantsverdriet, Deen and Sommer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: C. W. Slotema, Yy5zbG90ZW1hQHBzeXEubmw=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.