- 1Faculty of Kinesiology and Physical Education, University of Toronto, Toronto, ON, Canada
- 2School of Kinesiology, University of British Columbia, Vancouver, BC, Canada
- 3Schizophrenia Program, Centre for Addiction and Mental Health, Toronto, ON, Canada
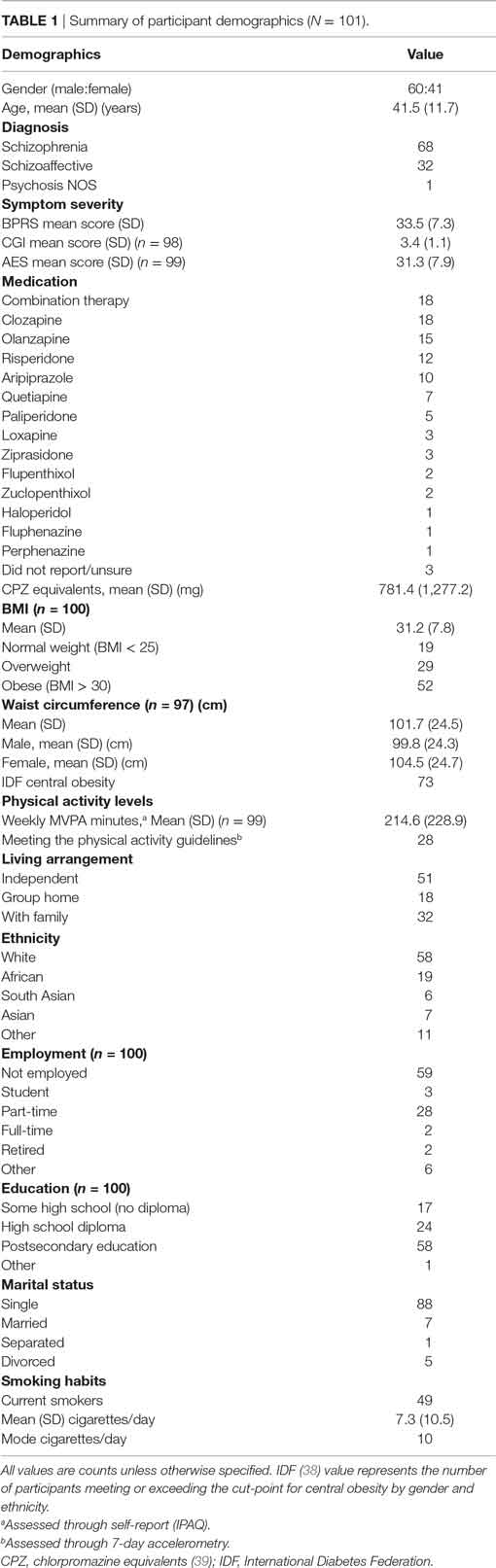
Research is needed to develop evidence-based behavioral interventions for preventing and treating obesity that are specific to the schizophrenia population. This study is the precursor to such intervention research where we examined the utility of the social cognitions outlined within the Health Action Process Approach (HAPA) model for predicting moderate to vigorous physical activity (MVPA) intentions and behavior among individuals with schizophrenia or schizoaffective disorder. A prospective cohort design [baseline (T1), week 2 (T2), and week 4 (T3)] was used to examine the HAPA constructs and MVPA across a sample of 101 adults (Mage = 41.5 ± 11.7 years; MBMI = 31.2 ± 7.8 kg/m2; 59% male). Two hierarchical regression analyses were conducted controlling for age, gender, BMI, and previous self-reported MVPA. In the first regression, intentions at T1 were regressed onto the T1 motivational HAPA constructs (risk perception, affective attitudes, task self-efficacy) and social support; MVPA status (meeting vs. not meeting the MVPA guidelines) assessed via accelerometry at T3 was regressed onto T1 social support and intentions followed by T2 action and coping planning, and maintenance self-efficacy in the second analysis. Overall, the motivational and social support variables accounted for 28% of the variance in intentions, with affective attitudes (β = 0.33, p < 0.01) and task self-efficacy (β = 0.25, p < 0.05) exhibiting significant, positive relationships. For MVPA status, the model as a whole explained 39% of the variance, with the volitional HAPA constructs explaining a non-significant 3% of this total variance. These findings suggest a need for interventions targeting self-efficacy and affective attitudes within this clinical population.
Introduction
Recent data indicate 13–15 years of life lost to schizophrenia compared to the general population (1). Cardiovascular death is a major contributor to this increased mortality (2). Potential causes of this excess mortality are varied, although they can be broadly categorized in terms of the iatrogenic effects of treatment (e.g., metabolic side effects of medication), greater prevalence of engagement in unhealthy behaviors (e.g., smoking, physical inactivity), and limited access to health care (3). Given the compelling evidence that physical activity prevents premature mortality, cardiovascular disease, and type 2 diabetes in the general population (4), one increasing focus of attention has been attempts to reduce physical inactivity in this population. Despite the many potential physical, psychosocial, and cognitive benefits of physical activity for individuals with schizophrenia (5), individuals with schizophrenia engage in significantly less moderate and vigorous physical activity compared to controls (6). Research is now required to inform the development of evidence-based behavioral interventions for increasing physical activity that are tailored to this population (7).
Theory-based physical activity interventions in the general adult population have been shown to be more effective at increasing physical activity than atheoretical interventions (8). A theoretical framework provides guidance in how to develop and implement interventions, identifies key modifiable constructs to target in intervention work, and informs measurement development to confidently assess how well interventions are influencing potential constructs mediating behavior change. Researchers have begun to examine theoretical factors that are most strongly related to physical activity among individuals with schizophrenia. For example, the Transtheoretical Model (9, 10), Self-Determination Theory (11), and Protection Motivation Theory (12) appear to be applicable frameworks to understand and predict physical activity within this population. More recently, Twyford and Lusher (13) tested the applicability of the Theory of Planned Behavior in predicting exercise intention and behavior among 105 individuals with schizophrenia and 109 community controls. Self-efficacy, perceived behavioral control, and health professional support predicted 33.4% of variance in intention to exercise. Fruit and vegetable intake and self-efficacy accounted for 12.7% of the variance in exercise behavior.
One gap in these theoretically informed studies is that they have all been cross-sectional in design. It is not known, for example, if increasing self-efficacy causes an increase in physical activity in this population. Identifying causal relationships is necessary for identifying the most salient determinants to target in future physical activity interventions (14). Given the lack of prospective theory-based research in this population, the relative importance of potential modifiable physical activity determinants specific to persons with schizophrenia still needs to be identified (15).
To address this concern, we prospectively examined the theoretical determinants of moderate to vigorous physical activity (MVPA) in the schizophrenia population. We used the Health Action Process Approach (HAPA) (16, 17) model to undertake this research as it allowed for the examination of different social–cognitive predictors across two phases of behavior change—motivation and volition (18). During the preintentional motivation phase, beliefs related to risk perceptions, outcome expectancies, and confidence to perform the target behavior (task self-efficacy) are predictive of one’s intention to enact the behavior. Meanwhile, in the second, postintentional volition phase, self-regulatory beliefs pertaining to planning, initiating, and maintaining the behavior (e.g., action and coping planning and maintenance self-efficacy) are most salient to behavior change. This two-phased approach of the HAPA is very fitting to the schizophrenia population where motivation impairments are a common negative symptom of the illness (19).
The utility of HAPA for developing tailored health behavior interventions in various populations suggests that it would be an appropriate theoretical framework for promoting physical activity in the schizophrenia population. Within the first stage of our research, we adapted and piloted a HAPA-based inventory to capture the salient, modifiable determinants of MVPA. After initial development with participant input, the inventory was assessed for internal consistency and test–retest reliability with 25 outpatients. Preliminary support was found for the criterion validity of the inventory, adequate to excellent indices for consistency, and reliability for all but two scales (20). In this second stage, we prospectively examine the utility of the constructs within the HAPA model for predicting objectively measured MVPA in a larger sample of adults with schizophrenia. Consistent with the underlying assumptions of the HAPA model (16, 17), we hypothesized that, once controlling for key demographic characteristics, (a) risk perceptions, outcome expectancies, and task self-efficacy at time 1 would be significant predictors of intentions at time 1, (b) intentions, action and coping planning, and maintenance self-efficacy at time 2 would be significant predictors of MVPA behavior at time 3, and (c) social support would be a significant predictor of both MVPA intentions and behavior.
Materials and Methods
Study Design
A prospective, 4-week cohort design with three measurement points [baseline (T1), week 2 (T2), and week 4 (T3)] was used to examine the HAPA constructs and MVPA intentions and behavior across a sample of community-dwelling adults with schizophrenia. This measurement period was consistent with guidelines for testing the assumptions of the HAPA model (16, 17, 21).
Participants
Research ethics approval was obtained from the Centre for Addiction and Mental Health (CAMH), Toronto, ON, Canada, and through the University of Toronto in September 2013. Study referral occurred through nurses, psychiatrists, and other studies at CAMH. All sessions were completed in a designated meeting room at either CAMH or the Mental Health and Physical Activity Research Centre at the University of Toronto. Similar to the first phase (20), all participants were required to have a diagnosis of schizophrenia or schizoaffective disorder, be between the ages of 18 and 64 years (22), and outpatients or inpatients with full privileges. Participants were screened on the phone by a nurse and excluded if they had been hospitalized within the past 12 months for angina pectoris, myocardial infarction, congestive heart failure, or cardiac surgery of any kind, or currently had uncontrolled hypertension (i.e., blood pressure >140 systolic/90 diastolic). Diagnosis and substance dependence/abuse were confirmed after consent was obtained using the Mini-International Neuropsychiatric Interview [MINI; (23)]. Based on Green’s (24) sample size guidelines for a regression analysis with nine predictor variables, a sample of 113 participants was necessary to detect medium-sized effects at α = 0.05 and power of 0.80. This sample size would allow for a 30% attrition rate based on earlier clinical and research experiences with this population (25, 26) and is consistent with attrition rates published in earlier prospective research using the HAPA model to predict physical activity in other rehabilitation outpatients (27).
Measures
Participant Psychopathology and Demographic Characteristics
A series of instruments were self-administered to obtain demographic, health, and psychopathology characteristics of the sample. Participants were required to self-report age, gender, height, weight, living arrangements, employment and marital status, educational attainment, smoking habits, and current prescribed medications. Waist circumference was measured at the umbilicus, while past MVPA behavior was assessed using the short-form version of the International Physical Activity Questionnaire [IPAQ; (28)]. The IPAQ has previously been validated in adults with schizophrenia (26).
Symptom severity was assessed using the Brief Psychiatric Rating Scale [BPRS; (29)], and the severity scale of the Clinical Global Impression [CGI-S; (30)], with higher scores representing greater mental illness severity. The anchored Apathy Evaluation Scale [AES; 18-items; (31)] was used to assess amotivation, with higher scores representing greater apathy. Internal consistency for the AES was 0.85.
HAPA Inventory
Seven of the 11 subscales within the original HAPA inventory for adults with schizophrenia (20) were included in the current study. These subscales included: risk perceptions, affective attitudes, task self-efficacy, MVPA intentions, action planning, coping planning, and maintenance self-efficacy. Each item was rated on a seven-point adjectival scale with anchors varying according to the content of the scales. Higher scores on each subscale represent more positive responses. All scales targeted performing at least 150 min of physical activity of at least moderate-intensity over the next week as the outcome, which is consistent with the Canadian physical activity guidelines for adults (22). Internal consistency for the subscales in the current study ranged from 0.72 to 0.95. A more detailed description of the items within each of the seven subscales is reported by Arbour-Nicitopoulos et al. (20).
Social Support
Social support was assessed using the 12-item Multidimensional Scale of Perceived Social Support (MSPSS) (32), which captures the perceived emotional and informational aspects of social support from family, friends, and significant others. An example of one item included within this scale is, “I get the emotional help and support I need from my family.” The MSPSS has demonstrated exemplary internal consistency (α > 0.89 for all three subscales), acceptable convergent validity, and strong factor loadings (>0.70) in psychiatric outpatients (33).
Physical Activity Behavior
MVPA behavior was assessed using 7-day accelerometry (Actigraph® GT3X). This measurement period is based on best practices for accelerometer use (34), which suggest that a 7-day protocol provides a reliable and valid estimate of physical activity behavior (ICC > 75%). A 1-min epoch was used to record activity counts (35), with each participant instructed to wear their accelerometer at all times and remove the device only for water-based activities. Activity counts were converted to weekly minutes of MVPA, using Troiano et al.’s (35) established adult cut-points for physical activity, with only bouts ≥10 min being included as per the physical activity guidelines (22). A dichotomized MVPA behavior (meeting/not meeting the guidelines for adults of 150 min of MVPA per week) was then created and used as the outcome variable in the analyses.
Procedures
Participants took part in three, in-person assessments over a 4-week time period. During the first session (T1), participants provided written consent and were administered the MacArthur Competence Assessment Tool for Clinical Research [MacCAT-CR; (36)] by a trained research assistant to assess their competence to consent. Once capacity to consent was verified, participants completed the psychopathology (i.e., MINI, AES, and CGI), health and demographic (e.g., age, weight, and waist circumference) instruments, followed by the motivational subscales of the HAPA inventory (i.e., risk perceptions, affective attitudes, task self-efficacy, and intentions), and social support measure. At the second assessment (T2), the volitional subscales of the HAPA inventory (i.e., action and coping planning, maintenance self-efficacy) were self-administered. Participants then met with the research assistant between T2 and T3 to obtain their accelerometer and detailed instructions on how to wear the device over the 7-day period. During the T3 assessment (held on week 4), participants returned their accelerometers.
Data Analysis
All statistical analyses were conducted using IBM’s SPSS 23.0 and, for the accelerometer data, Actigraph’s ActiLife® software version 5.0. Data were first examined for missing values, outliers, and errors. Values ≥3 SDs from the mean were removed as outliers (37). For the accelerometer data, participants had to have ≥10 h of wear time for at least four of the seven days to be included in the analyses (34, 35). Mean wear time on each of the valid days was 14.1 (1.9) h.
Descriptive analyses were conducted to examine demographic, health, and psychopathology characteristics and scale means and SDs. Hierarchical regression analyses were then used to test the ability of the HAPA model to predict MVPA intentions and behavior, controlling for age, gender, BMI, and previous self-reported MVPA behavior. In accordance with the HAPA model (16, 17, 21), in the first linear regression, intentions at T1 were regressed onto the motivational HAPA constructs at T1 (risk perception, affective attitudes, and task self-efficacy) and social support. In the second logistic regression analysis, MVPA behavior (meeting vs. not meeting the physical activity guidelines) assessed via accelerometry at T3 was regressed onto T1 social support and intentions followed by T2 action and coping planning, and maintenance self-efficacy.
Results
Participant Characteristics
A total of 141 participants were screened for study eligibility, 9 of whom were deemed ineligible as a result of not having the capacity to provide consent (n = 2) or not having a diagnosis of schizophrenia (n = 7). Of the remaining 132 eligible participants, 101 (76.5%) completed all three assessments as well as having valid accelerometer data. Table 1 summarizes the sample characteristics of these 101 participants. Overall, the sample was judged by the research team to be generally representative of the larger outpatient schizophrenia population at CAMH, exhibiting similar symptom severity and apathy scores, and high rates (52%) of obesity.
Motivational HAPA Constructs Predicting MVPA Intentions
Table 2 summarizes the mean motivational HAPA subscale scores, along with the regression coefficients, significance tests, effect sizes, and variance explained in intentions for engaging in MVPA behavior. Overall, the model explained 46% (R2adjusted = 0.42, SE = 1.38) of the variance in MVPA intentions, with the motivational HAPA constructs accounting for 28% of the total explained variance. Affective attitudes (β = 0.33, p < 0.01) and task self-efficacy (β = 0.25, p < 0.05) were the only significant predictors of intentions.
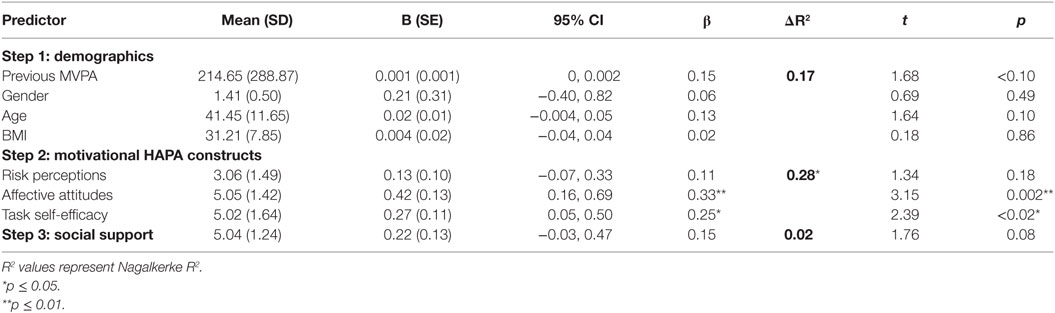
Table 2. Summary of hierarchical linear regression (N = 99) of motivational HAPA stage constructs predicting MVPA intentions.
Volitional HAPA Stage Constructs Predicting MVPA Behavior
Table 3 summarizes the mean volitional HAPA subscale scores, along with the odds ratios and 95% confidence intervals, regression coefficients, significance tests, and variance explained in MVPA behavior. Overall, the model accounted for 39% of the variance in meeting the physical activity guidelines, with intentions and social support explaining 8% of the total variance, and the volitional HAPA constructs explaining an additional 3% of the total variance. No significant relationships were exhibited between the HAPA constructs or social support and MVPA behavior.
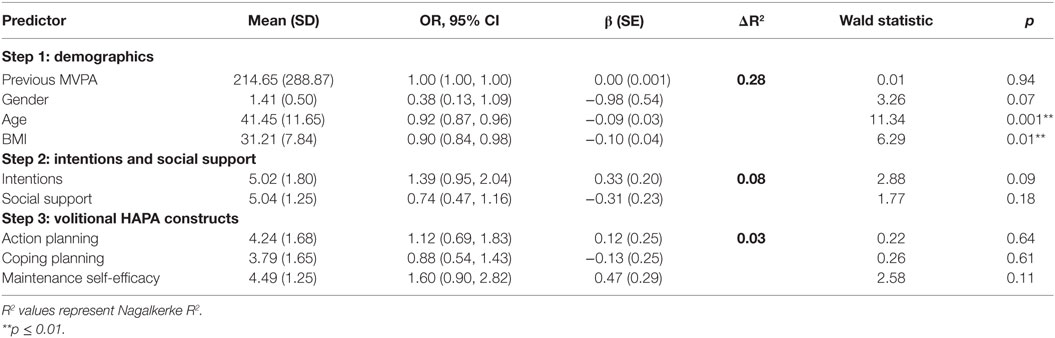
Table 3. Summary of hierarchical logistic regression (N = 99) of volitional HAPA constructs predicting MVPA behavior assessed via accelerometry at T3.
Significant negative relationships were found between age and BMI and MVPA behavior, suggesting that lower BMI and greater age, respectively, were predictive of meeting the guidelines.
Discussion
Our findings provide partial support for the utility of the HAPA model in predicting MVPA intentions, yet not MVPA behavior, among individuals with schizophrenia. The model was able to explain nearly a third of the variance in MVPA intentions, while only 3% of the variance was explained in MVPA behavior. Affective attitudes and task self-efficacy predicted intentions. No significant relationships were found for the volitional HAPA variables and MVPA behavior.
Our findings highlight distinct roles for both affective attitudes and task self-efficacy on MVPA intentions. Given the limited role of other HAPA variables in predicting intentions and behavior, the findings suggest that more parsimonious theoretical frameworks might be of value in informing intervention work in this population. Grounding physical activity interventions in the tenets of social cognitive theory (40) is one possible starting point. Self-efficacy, a situation-specific form of self-confidence, is integral to social cognitive theory and is a consistent predictor of behavior change in various situations (41). Self-efficacy has also been a consistent correlate of physical activity in this population (12, 13, 42), and our findings add further support to the importance of this construct using a prospective design. Further research is required to develop and evaluate the effectiveness of self-efficacy-based interventions that target MVPA intentions and behavior in persons with schizophrenia. In particular, studies are required that target changes in self-efficacy and include mediational analyses to determine whether changes in self-efficacy explain changes in physical activity. It should be noted, however, that such hypothetical links have not always been demonstrated among obese adults (43).
Such interventions could be informed by Bandura’s (40) sources of self-efficacy—past performance, vicarious experiences, social persuasion, and physiological/affective factors. Past performance (i.e., mastery) is commonly considered the most powerful source of an individual’s self-efficacy. Adopting a gradual approach to increasing (and ultimately maintaining) physical activity through the use of self-monitoring and goal setting is recommended. Vicarious experiences, seeing others succeed, particularly those similar to oneself, is another source of self-efficacy. Creating opportunities to observe influential others (e.g., friends, relatives, and/or individuals with schizophrenia) performing physical activity could be considered. Notably, social support was not a significant predictor of intentions or behavior in our analyses. This may be a measurement issue as the instrument used was not specific to a physical activity context. Rather, the MSPSS assesses a more general perception of support and it may be that more tangible forms of support (e.g., informational and emotional) are required to assist individuals with schizophrenia adopt as well as maintain physical activity participation (44).
Social persuasion concerns verbal and non-verbal strategies used by others to promote self-efficacy. As others have noted, long-term support to participate in physical activity by health professionals may be necessary for some individuals (45, 46). Health professional support predicted intention to exercise in the study reported by Twyford and Lusher (13). Practical facilitation in which a health professional organizes physical activity participation and possibly attends each physical activity session in person to provide verbal encouragement, reassurance, and support may be vital (45) and reflects the nature of the intervention in one of the first exercise and schizophrenia studies reported (47).
Finally, one’s physiological and affective states can also be a source of, or threat to, self-efficacy. As one example, an individual’s perception of physiological responses to exercise might alter that individual’s self-efficacy. The extent to which a bout of physical activity makes someone feel bad rather than good may be associated with non-adherence to physical activity. Affective attitudes were related to intentions for MVPA in our study. Systematic reviews have also shown a moderate relationship between affective judgment (enjoyment) and physical activity (48). Irrespective of risk perceptions and the instrumental benefits of physical activity, greater priority might be placed on ensuring individuals enjoy the experience of physical activity. A recent acute study confirms that individuals with schizophrenia can derive acute feelings of pleasure from exercise (49). Practically, this suggests recommending participants be physically active in a way that maintains a constant or improving (but not diminishing) level of pleasure (50). Individuals could be encouraged to monitor how they feel before, during, and after bouts of physical activity in order to regulate how they feel more reliably. This may alleviate feelings of low energy commonly reported by individuals with schizophrenia (51).
Notably, MVPA was not determined by intention as Twyford and Lusher (13) also reported in their study of the Theory of Planned Behavior using a self-report measure of physical activity. This is not an uncommon finding and may reflect an “intention-behavior gap.” While intention is a critical psychological determinant of physical activity within HAPA and the Theory of Planned Behavior, it is clear that the best intentions do not always lead to behavior. Planning is one post-intentional self-regulatory strategy that is theorized to assist with when, where, and how an intention will be translated into action. However, planning did not predict MVPA in our sample. Measurement may also have been an issue in this instance. Behavior was measured objectively through accelerometry while intentions and other psychosocial constructs were assessed through self-report. Given modest correlations between self-reported and objectively measured physical activity (52), there may be a subsequent lack of correspondence between the psychosocial constructs and MVPA.
This is not to suggest planning may not have a role to play in future interventions. A review of mediators of behavior change in physical activity interventions indicates that self-regulatory constructs (e.g., planning, contingency strategies, and self-monitoring) are the most consistent agents of change in otherwise healthy adults (53). A more recent review similarly found action planning to be significantly associated with positive changes in self-efficacy (43). Planning may support behavior change indirectly via improvements in self-efficacy. Further investigation of how planning can be linked to self-monitoring and goal setting in this population is warranted.
While not the primary focus of this study, age and BMI were significant predictors of MVPA behavior, albeit not intentions. Participants with lower BMI values were more likely to be meeting the physical activity guidelines as determined via accelerometry. Given the higher rates of obesity and type 2 diabetes among individuals with schizophrenia (54, 55), this finding further illustrates the importance of integrating physical activity into clinical care. Of interest, older participants in our study were more likely to meet the guidelines than younger respondents. Although reasons for this finding can only be speculated upon it may be that having lived longer with the disorder these individuals are coping more effectively in general and this is reflected in higher levels of habitual physical activity.
There are a number of strengths as well as limitations to note for this study. This is the first prospective study assessing the theoretical determinants of objectively measured physical activity among individuals diagnosed with schizophrenia or schizoaffective disorder. However, due to inadequate power, path analysis or structural equation modeling was not possible and these would have produced a more comprehensive analysis incorporating measured variables and latent constructs, and specifying measurement error. Regression analyses are recommended to test the HAPA model in such cases (56). Even with our regression models we were slightly underpowered to fully test the effects of the relationships between the HAPA constructs and MVPA. While our physical activity behavior outcome was aligned with national physical activity guidelines, i.e., achieving at least 150 min of MVPA per week (22), dichotomizing a continuous variable comes with important limitations to recognize such as loss of information and power (57, 58). However, dichotomizing continuous data is justified when the distribution of an outcome variable is highly skewed (57), which was the case for the physical activity behavior data in this study.
The first step in developing effective interventions is to identify theoretically informed and modifiable determinants of physical activity behavior change. Our findings provide one framework on which to build physical activity interventions, and measures have been developed for evaluating social-cognitive constructs potentially mediating behavior change within this clinical population. Although limited evidence was found for the utility of the HAPA model in predicting MVPA behavior, the results suggest a need for interventions targeting self-efficacy and affective attitudes with ongoing support from health professionals.
Ethics Statement
This study was carried out in accordance with the recommendations of the Research Ethics Boards of the Centre for Addiction and Mental Health (CAMH) and the University of Toronto with written informed consent from all subjects. All subjects gave written informed consent in accordance with the Declaration of Helsinki. The protocol was approved by the Research Ethics Boards of the Centre for Addiction and Mental Health (CAMH) and the University of Toronto.
Author Contributions
KA-N and GF designed the study. All authors contributed to data analysis and interpretation. KA-N and GF developed the first draft of the article. All authors contributed to critical revisions of the article, and gave final approval of the version to be submitted.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to acknowledge Ms. Carol Borlido and Ms. Mehala Subramanieapillai for all of their support with participant recruitment and data collection. We would also like to acknowledge the study participants and the staff at the Centre for Addiction and Mental Health.
Funding
Funding for this project was provided by the Canadian Institute of Health Research (CIHR) operating grant #MOP-115709. GF is supported by a CIHR-PHAC Chair in Applied Public Health award.
References
1. Hjorthøj C, Stürup AE, McGrath JJ, Nordentoft M. Years of potential life lost and life expectancy in schizophrenia: a systematic review and meta-analysis. Lancet Psychiatry (2017) 4(4):295–301. doi:10.1016/S2215-0366(17)30078-0
2. Ringen PA, Engh JA, Birkenaes AB, Dieset I, Andreassen OA. Increased mortality in schizophrenia due to cardiovascular disease – a non-systematic review of epidemiology, possible causes, and interventions. Front Psychiatry (2014) 5:137. doi:10.3389/fpsyt.2014.00137
3. Casey D, Hansen TE. Excessive mortality and morbidity associated with schizophrenia. 2nd ed. In: Meyer JM, Nasrallah HA, editors. Medical Illness and Schizophrenia. Washington, DC: American Psychiatric Publishing (2009). p. 17–35.
4. Warburton DE, Charlesworth S, Ivey A, Nettlefold L, Bredin SS. A systematic review of the evidence for Canada’s physical activity guidelines for adults. Int J Behav Nutr Phys Act (2010) 7:39. doi:10.1186/1479-5868-7-39
5. Firth J, Cotter J, Elliott R, French P, Yung AR. A systematic review and meta-analysis of exercise interventions in schizophrenia patients. Psychol Med (2015) 45:1343–61. doi:10.1017/S0033291714003110
6. Stubbs B, Firth J, Berry A, Schuch FB, Rosenbaum S, Gaughran F, et al. How much physical activity do people with schizophrenia engage in? A systematic review, comparative meta-analysis and meta-regression. Schizophr Res (2016) 176:431–40. doi:10.1016/j.schres.2016.05.017
7. Vancampfort D, Rosenbaum S, Probst M, Connaughton J, du Plessis C, Yamamoto T, et al. What are the top 10 physical activity research questions in schizophrenia? Disabil Rehabil (2016) 38:2235–43. doi:10.3109/09638288.2015.1116622
8. Kahn EB, Ramsey LT, Brownson RC, Health GW, Howze EH, Powell KE, et al. The effectiveness of interventions to increase physical activity: a systematic review. Am J Prev Med (2002) 22:73–107. doi:10.1016/S0749-3797(02)00434-8
9. Gorczynski P, Faulkner G, Greening S, Cohn T. Exploring the construct validity of the transtheoretical model to structure physical activity interventions for individuals with serious mental illness. Psychiatr Rehabil J (2010) 34:61–4. doi:10.2975/34.1.2010.61.64
10. Bassilios B, Judd F, Pattison P, Nicholas A, Moeller-Saxone K. Predictors of exercise in individuals with schizophrenia: a test of the transtheoretical model of behavior change. Clin Schizophr Relat Psychoses (2015) 8:173–82. doi:10.3371/CSRP.BAJU.030113
11. Vancampfort D, De Hert M, Vansteenkiste M, De Herdt A, Scheewe TW, Soundy A, et al. The importance of self-determined motivation towards physical activity in patients with schizophrenia. Psychiatry Res (2013) 210:812–8. doi:10.1016/j.psychres.2013.10.004
12. Leas L, Mccabe M. Health behaviors among individuals with schizophrenia and depression. J Health Psychol (2007) 12:563–79. doi:10.1177/1359105307078162
13. Twyford J, Lusher J. Determinants of exercise intention and behaviour among individuals diagnosed with schizophrenia. J Ment Health (2016) 25:303–9. doi:10.3109/09638237.2015.1124399
14. Bauman AE, Sallis JF, Dzewaltowski DA, Owen N. Toward a better understanding of the influences on physical activity: the role of determinants, correlates, causal variables, mediators, moderators, and confounders. Am J Prev Med (2002) 23:5–14. doi:10.1016/S0749-3797(02)00469-5
15. Vancampfort D, Knapen J, Probst M, Scheewe T, Remans S, De Hert M. A systematic review of correlates of physical activity in patients with schizophrenia. Acta Psychiatr Scand (2012) 125:352–62. doi:10.1111/j.1600-0447.2011.01814.x
16. Schwarzer R. Self-efficacy in the adoption and maintenance of health behaviors: theoretical approaches and a new model. In: Schwarzer R, editor. Self-Efficacy: Thought Control of Action. Washington, DC: Hemisphere (1992). p. 217–43.
17. Schwarzer R. Modeling health behaviour change: how to predict and modify the adoption and maintenance of health behaviors. Appl Psychol (2008) 57:1–29. doi:10.1111/j.1464-0597.2007.00325.x
18. Heckhausen H, Kuhl J. From wishes to actions: the dead ends and short cuts on the long way to action. In: Frese M, Sabini J, editors. Goal-Directed Behavior: The Concept of Action in Psychology. Hillsdale, NJ: Erlbaum (1985). p. 134–59.
19. Fervaha G, Foussias G, Agid O, Remington G. Motivational deficits in early schizophrenia: prevalent, persistent, and key determinants of functional outcome. Schizophr Res (2015) 166:9–16. doi:10.1016/j.schres.2015.04.040
20. Arbour-Nicitopoulos KP, Duncan M, Remington G, Cairney J, Faulkner GE. Development and reliability testing of a health action process approach inventory for physical activity participation among individuals with schizophrenia. Front Psychiatry (2014) 5:68. doi:10.3389/fpsyt.2014.00068
21. Scholz U, Sniehotta FF, Schwarzer R. Predicting physical exercise in cardiac rehabilitation: the role of phase-specific self-efficacy beliefs. J Sport Exerc Psychol (2005) 27:135–51. doi:10.1123/jsep.27.2.135
22. Canadian Society for Exercise Physiology. Canadian Physical Activity Guidelines. Ottawa, ON (2011). Available from: www.csep.ca/guidelines
23. Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The mini-international neuropsychiatric interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry (1998) 59:22–33.
24. Green SB. How many subjects does it take to do a regression analysis? Multivariate Behav Res (1991) 20:499–510. doi:10.1207/s15327906mbr2603_7
25. Arbour-Nicitopoulos KP, Faulkner GE, Shyu V, Cohn TA, Golding N, Hsueh R. A 6-week weight management program for women with schizophrenia: the need for women-centred interventions. J Sport Exerc Psychol (2010) 32:S140.
26. Faulkner G, Cohn T, Remington G. Validation of a physical assessment tool for individuals with schizophrenia. Schizophr Res (2006) 82:225–31. doi:10.1016/j.schres.2005.10.020
27. Sniehotta FF, Scholz U, Schwarzer R. Bridging the intention-behaviour gap: planning, self-efficacy, and action control in the adoption and maintenance of physical exercise. Psychol Health (2005) 20:143–60. doi:10.1080/08870440512331317670
28. Craig CL, Marshall AL, Sjöström M, Baumanm AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc (2003) 35:1381–95. doi:10.1249/01.MSS.0000078924.61453.FB
29. Woerner MG, Mannuzza S, Kane JM. Anchoring the BPRS: an aid to improved reliability. Psychopharmacol Bull (1988) 24:112–7.
30. Guy W. Clinical Global Impressions. ECDEU Assessment Manual for Psychopharmacology. Rockville: National Institute of Mental Health (1976).
31. Marin RS, Biedrzycki RC, Firinciogullari S. Reliability and validity of the apathy evaluation scale. Psychiatry Res (1991) 38:143–62. doi:10.1016/0165-1781(91)90040-V
32. Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. J Pers Assess (1988) 52:30–41. doi:10.1207/s15327752jpa5201_2
33. Cecil H, Stanley MA, Carrion PG, Swann A. Psychometric properties of the MSPSS and NOS in psychiatric outpatients. J Clin Psychol (1995) 51:593–602. doi:10.1002/1097-4679(199509)51:5<593::AID-JCLP2270510503>3.0.CO;2-W
34. Ward DS, Evenson KR, Vaughn A, Rodgers AB, Troiano RP. Accelerometer use in physical activity: best practices and research recommendations. Med Sci Sports Exerc (2005) 37:S582–8. doi:10.1249/00005768-200505001-00735
35. Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc (2008) 40:181–8. doi:10.1249/mss.0b013e31815a51b3
36. Appelbaum PS, Grisso T. MacArthur Competence Assessment Tool for Clinical Research (MacCAT-CR). Sarasota, FL: Professional Resource Press (2001).
37. Tabachnick BG, Fidell LS. Using Multivariate Statistics. 4th ed. Boston, MA: Pearson, Allyn & Bacon (2000).
38. Alberti KG, Zimmet P, Shaw J. Metabolic syndrome – a new world-wide definition. A consensus statement from the International Diabetes Federation. Diabet Med (2006) 23:469–80. doi:10.1111/j.1464-5491.2006.01858.x
39. Gardner DM, Murphy AL, Donnell HO, Centorrino F, Baldessarini RJ. International consensus study of antipsychotic dosing. Am J Psychiatry (2010) 167:686–93. doi:10.1176/appi.ajp.2009.09060802
41. Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall (1986).
42. Ussher M, Stanbury L, Cheeseman V, Faulkner G. Physical activity preferences and perceived barriers to activity among persons with severe mental illness in the United Kingdom. Psychiatr Serv (2007) 58:405–8. doi:10.1176/ps.2007.58.3.405
43. Olander EK, Fletcher H, Williams S, Atkinson L, Turner A, French DP. What are the most effective techniques in changing obese individuals’ physical activity self-efficacy and behaviour: a systematic review and meta-analysis. Int J Behav Nutr Phys Act (2013) 10:29. doi:10.1186/1479-5868-10-29
44. Gross J, Vancampfort D, Stubbs B, Gorczynski P, Soundy A. A narrative synthesis investigating the use and value of social support to promote physical activity among individuals with schizophrenia. Disabil Rehabil (2016) 38:123–50. doi:10.3109/09638288.2015.1024343
45. Carless D. Phases in physical activity initiation and maintenance among men with serious mental illness. Int J Ment Health Promot (2007) 9:17–27. doi:10.1080/14623730.2007.9721835
46. Hodgson MH, McCulloch HP, Fox KR. The experiences of people with severe and enduring mental illness engaged in a physical activity programme integrated into the mental health service. Ment Health Phys Act (2011) 4:23–9. doi:10.1016/j.mhpa.2011.01.002
47. Faulkner G, Sparkes A. Exercise as therapy for schizophrenia: an ethnographic study. J Sport Exerc Psychol (1999) 21:39–51. doi:10.1123/jsep.21.1.52
48. Rhodes RE, Fiala B, Conner M. A review and meta-analysis of affective judgments and physical activity in adult populations. Ann Behav Med (2009) 38:180–204. doi:10.1007/s12160-009-9147-y
49. Duncan MJ, Faulkner G, Remington G, Arbour-Nicitopoulos K. Characterizing the affective responses to an acute bout of moderate-intensity exercise among outpatients with schizophrenia. Psychiatry Res (2016) 237:264–70. doi:10.1016/j.psychres.2016.01.030
50. Ekkekakis P, Parfitt G, Petruzzello SJ. The pleasure and displeasure people feel when they exercise at different intensities: decennial update and progress towards a tripartite rationale for exercise intensity prescription. Sports Med (2011) 41:641–71. doi:10.2165/11590680-000000000-00000
51. Firth J, Rosenbaum S, Stubbs B, Gorczynski P, Yung AR, Vancampfort D. Motivating factors and barriers towards exercise in severe mental illness: a systematic review and meta-analysis. Psychol Med (2016) 46:2869–81. doi:10.1017/S0033291716001732
52. Duncan MJ, Arbour-Nicitopoulos K, Subramanieapillai M, Remington G, Faulkner G. Revisiting the international physical activity questionnaire (IPAQ): assessing physical activity among individuals with schizophrenia. Schizophr Res (2016) 179:2–7. doi:10.1016/j.schres.2016.09.010
53. Rhodes RE, Pfaeffli LA. Mediators of physical activity behaviour change among adult non-clinical populations: a review update. Int J Behav Nutr Phys Act (2009) 7:37. doi:10.1186/1479-5868-7-37
54. Manu P, Dima L, Shulman M, Vancampfort D, De Hert M, Correll CU. Weight gain and obesity in schizophrenia: epidemiology, pathobiology, and management. Acta Psychiatr Scand (2015) 132:97–108. doi:10.1111/acps.12445
55. Suvisaari J, Keinänen J, Eskelinen S, Mantere O. Diabetes and schizophrenia. Curr Diab Rep (2016) 16:16. doi:10.1007/s11892-015-0704-4
56. Schwarzer R. The Health Action Process Approach. (2009). Available from: http://www.hapa-model.de/
57. Streiner DL. Breaking up is hard to do: the heartbreak of dichotomizing continuous data. Can J Psychiatry (2002) 47:262–6. doi:10.1177/070674370204700307
Keywords: schizophrenia, physical activity, determinants, theory based, accelerometry
Citation: Arbour-Nicitopoulos KP, Duncan MJ, Remington G, Cairney J and Faulkner GE (2017) The Utility of the Health Action Process Approach Model for Predicting Physical Activity Intentions and Behavior in Schizophrenia. Front. Psychiatry 8:135. doi: 10.3389/fpsyt.2017.00135
Received: 20 December 2016; Accepted: 12 July 2017;
Published: 04 August 2017
Edited by:
Stefan Borgwardt, University of Basel, SwitzerlandReviewed by:
Brendon Stubbs, King’s College London, United KingdomDrozdstoy Stoyanov Stoyanov, Medical University of Plovdiv, Bulgaria
Copyright: © 2017 Arbour-Nicitopoulos, Duncan, Remington, Cairney and Faulkner. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Guy E. Faulkner, Z3V5LmZhdWxrbmVyQHViYy5jYQ==
 Kelly P. Arbour-Nicitopoulos1
Kelly P. Arbour-Nicitopoulos1 Markus J. Duncan
Markus J. Duncan Gary Remington
Gary Remington John Cairney
John Cairney Guy E. Faulkner
Guy E. Faulkner