
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Polit. Sci., 22 January 2021
Sec. Political Participation
Volume 2 - 2020 | https://doi.org/10.3389/fpos.2020.601323
This article is part of the Research TopicHealth and Political BehaviorView all 6 articles
 Cydney M. McGuire1*
Cydney M. McGuire1* Sarah E. Gollust1
Sarah E. Gollust1 Molly De Marco2,3
Molly De Marco2,3 Thomas Durfee4
Thomas Durfee4 Julian Wolfson5
Julian Wolfson5 Caitlin E. Caspi6,7
Caitlin E. Caspi6,7Objective: The purpose of this study is to identify health resources associated with propensity to vote at the local-level among low-wage workers in two United States. cities. Literature confirms individuals of lower income have a lower propensity of turning out to vote, yet few studies have focused on low-income populations to identify the variation in factors associated with voting within this group. Furthermore, few studies have investigated health and voter turnout at the local-level. In this study, we examine factors related to political participation at the local-level within a low-wage sample, examine mental, physical, behavioral, and social health and their association with voter turnout, and assess if these relationships differ by city.
Methods: We use cross-sectional survey data from a sample of 974 low-wage workers in Minneapolis, MN and Raleigh, NC. We computed descriptive statistics and employed a logistic regression to predict their likelihood of local voter turnout, with the key independent variables being health resources, such as self-rated health, body mass index (BMI), mental disability, smoking status, and health insurance status. We employed a logistic regression fully interacted with a city indicator variable to assess if these associations differed by city.
Results: In both cities, less than 50 percent of respondents reported voting in the last election for mayor or city council. About three-quarters of the sample reported food or housing insecurity and the majority of respondents reported utilizing some government assistance, such as supplemental nutrition programs. BMI greater than 30 was significantly associated with lower likelihood of voter turnout compared to those of lower BMI status (marginal effect = −0.10, p = 0.026). Never smoking or quitting was significantly associated with higher likelihood of voter turnout compared to those who reported being a current smoker (marginal effect = 0.10, p = 0.002). Those with health insurance were significantly more likely to report voting compared to those without any insurance (marginal effect = 0.10, p = 0.022). These results did not significantly differ by city.
Conclusions: Our research suggests low-wage workers face significant health burdens which may impact their propensity to vote at the local-level, and these associations do not significantly vary by city despite demographic and political differences between two jurisdictions.
Political participation by citizens is a requirement for a functioning democracy, yet in the United States citizens do not always participate, such as through voting, signing petitions, and donating to political campaigns or candidates. There are many theories as to why or why not people may participate politically, involving both the resources they have available to them and the context in which they live.
One prominent theory is the resource model of participation, which argues that an individual’s likelihood of participating politically is a function of their available resources–money, time, and civic skills (Brady et al., 1995). This model draws upon stratification theory in the field of sociology which suggests class and status hierarchies are critical features in modern society and are also determinants of political behavior (Dahrendorf, 1966; Brady et al., 1995). The model also draws upon rational choice economic theory which takes into account constraints on time, money, and investment in human capital (Becker, 1965, 2013; Michael, 1973; Brady et al., 1995). The resource model of participation considers the costs of using resources and that multiple constraints on resources–including the variation in flow of resources due to social stratification–limit individuals’ participation behaviors (Brady et al., 1995). Consistent with this model, abundant empirical research demonstrates that lower-income people are less likely to participate in politics. In the United States, it is now well-documented that those of higher income participate in politics—such as through voting and donating to political causes–at higher levels than those of lower income (Schlozman et al., 2012; Erikson, 2015).
Other theories of political participation include political institutional models, which suggest that an individual’s decision to vote is influenced not only by the resources they have at their disposal but also by the political and institutional context in which citizens live, such as the voting laws in their jurisdiction or the closeness of elections (Blais and Dobrzynska, 1998; Geys, 2006; Smets and van Ham, 2013). The political and institutional context in which citizens live may be particularly relevant for citizens who are low-income, and thus engage with many government programs which have means-based qualifications. Previous work suggests that the design and implementation of public policy may impact political efficacy and behavior (Soss, 1999; Mettler and Soss, 2004; Campbell, 2011; Sharp, 2013). Michener, (2018) Contextualized Feedback Model of Participation integrates theory on policy feedback with individual and contextual factors which shape political participation. Michener argues that the design, implementation, and constraints of public policy are subject to geographical context, (e.g. states, counties, and neighborhoods) and that macro-institutions, (e.g. federalism or civil law) structure these contexts. Michener contends that these institutionally embedded contexts impact individuals’ experiences with policies which, along with other individual characteristics, shape individuals’ political capacity and behavior (Michener, 2018).
Although much previous theoretical work has been conducted on the factors that relate to individual-level political participation, as described above, individuals’ health is not explicitly included in these models. However, health may impact political participation through established politically relevant resources or other possible mechanisms (Pacheco and Fletcher, 2015; Lahtinen et al., 2017). A substantial body of emerging research has identified health as a potentially important variable shaping political participation (Brown et al., 2020); however there are still gaps in this research.
Previous work has demonstrated that health is associated with the likelihood of participating in the political system in various ways, such as voting, signing petitions, and engaging with elected officials (Denny and Doyle, 2007; Mattila et al., 2013; Matsubayashi and Ueda, 2014; Gollust and Rahn, 2015; Ojeda, 2015; Pacheco and Fletcher, 2015; Burden et al., 2017; Couture and Breux, 2017; Hassell and Settle, 2017; Lahtinen et al., 2017; Wass et al., 2017; Brown et al., 2020). Poor health and chronic conditions have been associated with differential likelihood of turning out to vote in the United States and globally (Denny and Doyle, 2007; Mattila et al., 2013; Gollust and Rahn, 2015; Pacheco and Fletcher, 2015; Sund et al., 2016; Burden et al., 2017; Wass et al., 2017; Gagné et al., 2019). For example, lower self-rated health has been associated with lower propensity to turnout to vote (Denny and Doyle, 2007; Mattila et al., 2013; Pacheco and Fletcher, 2015; Gagné et al., 2019), while cancer diagnosis has been associated with a higher likelihood of voting (Gollust and Rahn, 2015; Sund et al., 2016). The relationship between self-rated health and turnout may be mediated by social connectedness, where, for example, an individual’s social network is weakened due to poor health and this depresses participation (Mattila et al., 2013). Cancer diagnoses may be positively associated with propensity for voter turnout due to mobilization among cancer “survivors” who engage in advocacy, may be connected socially with other survivors, and volunteer with cancer-related organizations (Gollust and Rahn, 2015). These relationships between health and voting also vary by other individual characteristics, including race, education status, and income (Gollust and Rahn, 2015).
Poor health is also related to other disadvantages and barriers to political participation. Economic adversity, including unemployment, poverty, and decline in financial well-being reduce likelihood of turnout (Rosenstone, 1982). Further, it is well known that income is a fundamental social determinant of health, with low-income people generally less healthy than those with more income (Marmot, 2002). As outlined by Lahtinen et al. (2017), health can intersect with the social class-income-turnout relationship through a variety of mechanisms, whether as a mediator of the relationship or as a moderator. As a mediator, the fact that health is worse among lower social class groups suggests that poor health may be one mechanism through which lower social class relates to poorer turnout. As a moderator, the relationship between social class and turnout may differ depending on whether health is good or poor. Lahtinen and colleagues find that health has a modifying effect, in which the relationship between social class and voter turnout is stronger among those in good health compared to those in weaker health (Lahtinen et al., 2017).
While research particularly in the last 5 years has amassed important evidence on the relationship between health and voter turnout, as described above (Ojeda, 2015; Pacheco and Fletcher, 2015; Sund et al., 2016; Couture and Breux, 2017; Mattila et al., 2017; Ojeda and Pacheco, 2019; Brown et al., 2020), there are some notable gaps in this literature, including the measurement of health, the level of voting, and the populations studied.
First, as our conceptual model below illuminates, health is a much broader construct than typically explored in existing studies. Most existing studies use either single items of self-rated health or measures of diagnosis with chronic diseases. However, the literature in public health points to the importance of the broad “social determinants of health” which are likely important determinants of political participation as well, encompassing such factors as food insecurity, housing insecurity, and stress (Braveman et al., 2011). Very limited research has examined how a range of health-related factors–not limited to self-rated health but broadened to include health behaviors and experiences with other determinants of health–might be related to political outcomes. For instance, previous research has linked housing to political behavior, suggesting that homeowners are more likely to turnout to vote in local elections, while residing in a neighborhood with poor street conditions is associated with lower likelihood of turnout (Martikainen et al., 2005; Clarke et al., 2011; Mccabe, 2013; Zavisca and Gerber, 2016). In addition, smoking, which is considered a health behavior, has been examined as a determinant of political behavior in two previous studies and associated with lower likelihood of voter turnout (Denny and Doyle, 2007; Albright et al., 2016). Given the limited research on these topics, it is still not clear what relationship risky health behaviors or housing insecurity may have on political behavior and if other social determinants of health may influence political outcomes.
Second, the majority of studies examining associations of individual characteristics and political participation have been conducted using national populations and lack analysis of political behavior and voter turnout at the local-level; the same is true of the literature on health and voting (Gollust and Rahn, 2015; Ojeda, 2015; Pacheco and Fletcher, 2015). Yet, local-level political participation, (e.g., for mayor or city council) has the potential to meaningfully change the circumstances of citizens in their local communities, and thus potentially to improve their health or reduce health inequities (Sharp, 2013). A 2016 study using data on mayoral votes from 356 midsized cities in the United States reported the average rate of turnout to be about 19 percent (Aldag, 2016). Other studies estimate that rates of turnout in local elections are less than one-quarter of the voting-age population in some municipalities or about half that of national elections (Alford and Lee, 1968; Morlan, 1984; Bridges, 1997; Hajnal and Lewis, 2003). More research is needed to understand the factors that contribute to local turnout. Research suggests that social contexts, such as neighborhoods and social networks, may also drive political behavior at the local-level (Huckfeldt, 1979; Baybeck, 2014). For instance, evidence suggests residing in a poverty-concentrated neighborhood and social isolation are barriers to local-level political participation (Cohen and Dawson, 1993; Alex-Assensoh, 1997). Other work indicates that the racial composition of communities is a relevant determinant of local political participation (Matsubayashi, 2010). However, it is not yet clear to what extent health-related factors are associated with local political participation.
Third, there is a gap in research examining the associations of health and political participation within lower income groups, which are already known to experience barriers and lower rates of political participation. The United States has large disparities in health and distribution of resources, where disadvantaged social groups, (e.g. the poor, racial/ethnic minorities, or women) systematically experience worse health or higher health risks than advantaged groups, which deepens avoidable health inequities (Braveman, 2006). Income is also a key factor in shaping political participation, and the association between income and political participation persists in models which include health factors (Gollust and Rahn, 2015). Income has been demonstrated to explain social class differences in voter turnout (Lahtinen et al., 2017) and recent work examining income and political participation indicates that both childhood poverty and current income levels play a role in individual’s likelihood of political participation (Ojeda, 2018). This work suggest that short-vs. long-term economic stability has differential effects on political behavior (Ojeda, 2018). Further work indicates that intergenerational transmission of disadvantages may reduce the likelihood of turnout, finding that parental socioeconomic position and voting history are key determinants in propensity to vote (Lahtinen et al., 2019). Yet what is not yet clear is the extent to which the health detriment associated with having lower socioeconomic status might be related to lower participation among low-income populations. Further research is necessary investigating the relationship between health factors and political behavior among under-resourced groups.
The current study responds to the three gaps in research outlined above. The study examines the relationship between local voter turnout and health in two urban United States. contexts among low-wage workers, a population with known low rates of turnout. We aim to examine the contribution of diminished health resources among this group as an explanation for lower levels of participation. The objective of this paper is thus to describe voter turnout among low-wage workers in the United States in two large cities, to assess which health resources are associated with propensity to vote in local elections, and determine if the impact of health on voter turnout varies by geographical location. This work is of great significance because health inequality and participation inequality have a cyclical relationship; if health inequity perpetuates inequity in representation, then inequitable political representation will deepen health inequity in the United States.
Figure 1 shows the conceptual model for this study. The conceptual model is based on the Resource Model of Participation, uses a socioecological approach, and is also informed by the Contextualized Model of Policy Feedback (McLeroy, 1988; Brady et al., 1995; Michener, 2018). Resource theories of political participation generally contend that having more resources reduces barriers to participation and thereby leads to more political activity (Mattila et al., 2017). Previous scholars have considered how health may be a resource for participation, suggesting that poor health raises barriers and obstacles to participation which reduces the time and energy available for political activity (Mattila et al., 2017). Furthermore, social context and social identity may play a role in these relationships (Mattila et al., 2017).
In order to identify how health might contribute to political participation in this study, we first define what health is. The World Health Organization defines health as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity”. The physical dimensions of health include measures such as body mass index (BMI) and blood pressure (Breslow, 2006). The mental dimensions of health may be evaluated through cognition and mood assessment (Breslow, 2006). The social dimensions of health refer to the social conditions which contribute to well-being such as networks of friends and relatives (Breslow, 2006), but also more broadly may refer to social determinants of health, defined as the conditions in which individuals grow, live, and work that are fundamental drivers of health, such as food and housing security (Commission on Social Determinants of Health, 2008; Braveman and Gottlieb, 2014). The WHO conceptualization of health as a “resource” was introduced in 1986 at the First International Conference on Health Promotion in Ottawa. The Ottawa Charter for Health Promotion states that:
“To reach a state of complete physical, mental and social well-being, an individual or group must be able to identify and to realize aspirations, to satisfy needs, and to change or cope with the environment. Health is, therefore, seen as a resource for everyday life, not the objective of living. Health is a positive concept emphasizing social and personal resources, as well as physical capacities,” (World Health Organization, 1986, p.1).
This definition extends our understanding of health as a resource for other activities in life, including political participation. Since this first identification of health as a resource, others have used similar conceptual definitions, including government organizations such as the United States. Centers for disease Control and Prevention and professional societies, for instance the Canadian Public Health Association (Gewurtz et al., 2016; Centers for Disease Control and Prevention, 2018). Building on this definition, Williamson and Carr described health as a type of capital resource which provides individuals with reserves of biopsychosocial resources that they draw upon to participate in society (Williamson and Carr, 2009). Thus, individuals can invest in their stock of biopsychosocial reserves by engaging in healthful behaviors and maintaining levels of physical, mental, and social well-being. Operationalizing health as a resource can be done through a variety of quantitative measures, such as measuring different dimensions of health (i.e., physical, mental, and social) or measuring health-related practices and healthy behaviors, (e.g., exercise and avoiding smoking), which heavily influence future health (Breslow, 2006; Williamson and Carr, 2009). Considering this definition of health as a resource for living, then, health is relevant to several of the models of political participation introduced above. For example, health is relevant to political institutional models and feedback models, since the social determinants of health shape the extent to which people are exposed to or use government safety-net services, such as Medicaid (a state health insurance program for low-income people), or the Supplemental Nutrition Assistance Program (SNAP, a government program providing food support for people with low incomes who face food insecurity) (Soss, 1999; Michener, 2018).
In our model, an individual’s likelihood of turning out to vote is a function of their available resources, which may be grouped into several broad categories. These categories are similar to the Brady resource model, but modified for this study to incorporate health. As previously stated, the resource model of political participation includes three key resources–time, money, and civic skills (Brady et al., 1995). In our adapted model for this study, the key resources included are time, money, and health. Similar to Brady, time in our model represents the free time an individual has available after normal work and other activities. Money refers to the financial or monetary resources available to an individual. In Brady’s model, civic skills is the third resource and refers to the communication and organizational skills necessary to be politically active (Brady et al., 1995). In this study, we do not have similar measures of civic skills but some assessment of civic skills may be captured through educational attainment, which is included in this study (Brady et al., 1995). In addition to the resources outlined by Brady, our model explicitly incorporates health as an additional resource, given the emerging relationship between health and participation outlined in previous research (Brown et al., 2020).
We take a socioecological approach to the conceptualization of health in which factors at multiple levels, including personal and social, all contribute to the promotion of health (McLeroy, 1988). This is consistent with the Contextualized Model of Policy Feedback which suggests that political behavior occurs within the context of and is influenced by economic, social, and political conditions in individuals’ cities, states and neighborhoods (Michener, 2018). Thus, in our model health as a resource for political participation refers to a stock of biopsychosocial capital, made up of physical, mental, behavioral, and social components, which help individuals fulfill their needs in everyday life to promote well-being (Williamson and Carr, 2009). In this definition, health is a resource to maximize the potential for living and is influenced by the context in which the individual lives and can be measured quantitatively by breaking out the different dimensions in which individuals can invest in their health (Breslow, 2006). The key dimensions of health in this model are physical, mental, behavioral, and social. The entire model is situated within the context described by the Contextualized Model of Policy Feedback such that the context of one’s political environment (i.e., the city in which one lives) also matters (Michener, 2018). Cities have different political cultures, resources available for low-income groups, and different laws surrounding the ease of voting and/or voter suppression. This signifies that health resources and other characteristics may have different associations with political participation depending on the city in which one resides.
The next section describes the study context in which we apply the above conceptual model to assess the associations between these health resources and voter turnout in two large United states cities.
We analyzed a cross-section of survey data from a longitudinal multi-year study including 974 low-wage workers in Minneapolis, MN and Raleigh, NC designed to assess the health effects of the minimum wage ordinance passed by the Minneapolis City Council in June 2017 (Williams, 2017). Although the data set was originally designed to evaluate a minimum wage ordinance and not propensity to vote, it is unique and has great value for the investigation of health and political participation, as the survey asks about many measures of health as well as voter turnout in local elections in two distinct urban contexts. Raleigh serves as the control site because it is located in a state with a minimum wage preemption law1 but has similar relevant demographics to Minneapolis based on United states Census data (Shanafelt et al., 2020). This broad study, of which the cross-sectional survey examined here is just one component, is called the Wages Study. Data collection is conducted annually through scheduled appointments with participants which include annual weight and height measurements, an online survey, and wage verification. We enrolled participants via face-to-face appointments from February 2018 to October 2018.
We aimed to recruit a sample of those likely to be affected by the minimum wage ordinance across all workforce sectors in Minneapolis, and a comparable sample in Raleigh. This community-based sample was recruited though active recruitment at community organizations and events, as well as passive strategies, (e.g., flyers, advertisements). Wages study recruitment strategies are discussed in more detail in a previous publication (Shanafelt et al., 2020). Participants were eligible if they: 1) were 20 years old or older, 2) worked at least 20 h a week at a wage of less than $11.50/hour in Minneapolis/Raleigh OR were employed at that wage within the last 6 months and were currently seeking work in Minneapolis/Raleigh, 3) planned to serve in the workforce for at least 5 years, 4) had a means of being contacted for follow-up, and 5) spoke English or Spanish. Participants were excluded if they were federal/state workers, full-time students, or planned to retire or move more than 100 miles away. Participants received a $70 incentive for completing all baseline study measures. Wage eligibility was set at $11.50 an hour or less to capture workers earning up to 15 percent above the minimum wage at baseline, given that a rise in minimum wage can introduce a re-scaling of wages just above it.
The survey was administered on a laptop through the REDCap program, a secure web-based application used to collect data and create databases. Participants completed the survey at the time of enrollment. Participants had the option of taking the survey independently or having a research team member assist them. This gave the possibility of participants not answering all of the questions when taking the survey on their own. Participants also had the option of skipping any questions that they were uncomfortable with answering.
The main dependent variable is a single survey item asking respondents: “Did you vote in the last local election, like for mayor or city council member?” Options included “Yes” or “No”. After removing observations that were missing on the dependent variable, the total number of observations remaining was 962.
The key independent variables are measures of health resources. We include self-rated health as a measure of overall health and well-being, which has been shown to be associated with voter turnout in the United states in previous work (1 = Excellent, 2 = Very good, 3 = Good, 4 = Fair, 5 = Poor) (Gollust and Rahn, 2015). Within the four domains of health resources outlined in the conceptual model, measures of physical health include body mass index (BMI) and physical disability. BMI is assessed through calculations based on anthropometric measures of participants’ height and weight by the research team. Survey items to measure physical and mental disability were designed specifically for the larger study to assess the minimum wage ordinance, therefore both of the physical and mental disability items assume the respondent can perform some amount of work but may be limited due to their condition. Physical disability is measured using a survey item asking respondents: “Do you have a physical health condition or disability that affects the number of hours of work you perform in a week?” (0 = No, 1 = Yes). We measure mental health with a single survey item asking respondents “Do you have mental health condition or disability that affects the number of hours of work you perform in a week?” (0 = No, 1 = Yes). We include one measure of behavioral health which asks respondents their smoking status; response options included “Current smoker”; “Quit less than 12 months ago”; “Quit more than 12 months ago”; and, “Never smoked”; this item was collapsed to be dichotomous (0 = Current Smoker, 1 = Never smoked/Quit).
We include several measures of social conditions that are related to health, including the social determinants of health and stress. Health insurance is measured using one survey item asking respondents “What type(s) of health insurance/health coverage do you currently have?” Respondents were instructed to check all those that applied from eight different options, for example Medicare, Medicaid, health insurance plan offered through your employer, or private insurance plan. This variable was collapsed to be dichotomous indicating those who were uninsured and those with any form of insurance reported (0 = Uninsured, 1 = Any insurance). Food security was measured using the 6-item United States Department of Agriculture (USDA) survey instrument and categorized as “high food security”; “low food security”; or, “very low food security” (USDA ERS, USDA, 2012). Housing security was measured using three survey items based on previous work which assesses basic needs (Goldrick-Rab et al., 2018): 1) “In the last year (12 months), was there a time when you were not able to pay the mortgage or rent on time?” (0 = Yes, 1 = No); 2) “In the last year (12 months), was there a time when you did not have a steady place to sleep or slept in a shelter (including now)?” (0 = Yes, 1 = No); and, 3) “In the last year (12 months), how many places have you lived?” Response options for the number of places lived included zero, one, two, three, or more than three. Responses which indicated zero, three, or more than three places lived in the last year were coded as housing insecure and categorized as “Yes”; responses which indicated one or two places lived were coded as housing secure and categorized as “No” (0 = Yes, 1 = No). Responses which were categorized as “Yes” for any of the previous three measures were coded to indicate housing insecurity (0 = Housing secure, 1 = Housing insecure). Any government assistance is measured using five separate survey items with the prompt “In the last month (30 days) did you or anyone in your household receive any of the following?” Response options included “Yes”, “No”, and “Not Sure” for the following items under the prompt: 1) Women, Infants, and Children program (WIC); 2) Food stamps (SNAP); 3) Free or reduced price school lunch; 4) Minnesota Family Investment Program (MFIP, Cash Assistance, Childcare Assistance); and, 5) State housing subsidy, (e.g., Bridges Housing Subsidy, HUD Rental Assistance, Section 8 Housing, Public Housing, Section 42 Housing). Responses of “Yes” for any of the previous five items were categorized as using government assistance (0 = No, 1 = Yes). Finally, stress is measured using the validated Perceived Stress Scale 4 (PSS4) with four survey items (Cohen et al., 1983), categorized into three groups: low (0–6), medium (7–8), and high (9–15).
Other variables in the conceptual model are measures of time and money. We assess time using two measures: commute time and working time. Commute time is measured using a survey item asking respondents to report the amount of time they spend commuting to their workplace in minutes. This item was collapsed into three categories (0 = ≤15 min, 1 = 16–30 min, 2 = >30 min). The amount of time respondents spend working per week is measured using a survey item asking respondents the usual number of hours worked during the week; if respondents reported two jobs the hours reported for each job were summed for a total number of hours worked per week. Working time per week is included as a continuous variable. Household income is measured using a survey item which asks respondents to report their annual household income last year, before taxes. Response options included “Less than $5,000”; “$5,001 to $10,000”; “$10,001 to $20,000”; “$20,001 to $30,000”; “$30,001 to $40,000”; “$40,001 to $50,000”; “More than $50,000.” Household income was collapsed to four categories (0 = ≤$5,000, 1 = $5,001 to $10,000, 2 = $10,001 to $20,000, 3 = >$20,000).
We include several demographic variables. Respondents were asked to report the city in which they work (0 = Minneapolis, 1 = Raleigh). Educational attainment was measured using a survey item asking respondents the highest grade or level of school they have completed. Response options include “less than high school”; “some high school; “high school diploma”; “associate/technical degree”; “some college”; “bachelor’s degree”; “graduate degree.” Educational attainment was collapsed to four categories (0 = Less than high school, 1 = High school degree, 2 = Some college, 3 = College degree or more). Racial identity is measured using a survey item which asked respondents to self-report their race; response options include “American Indian/Alaska”; “Native”; “Asian”; “Black or African American”; “Native Hawaiian or Other”; “Pacific Islander”; “White”; “Other.” Due to few responses in some categories, this item was collapsed to three categories (0 = White, 1 = Black, 2 = Native/Asian/Mixed/Other). Age is measured by a single survey item asking respondents to report their age in years; this item was grouped into four categories (0 = 18–29, 1 = 30–39, 2 = 40–49, 3 = 50+). Sex is measured using a survey item asking respondents to indicate if they identify as one of three response options which include “Male”, “Female”, and “Non-binary”. Due to few response in the non-binary category, this item was collapsed to be dichotomous (0 = Female, 1 = Male) and responses in the non-binary category were coded as missing. Marital status is measured using a survey item asking respondents to report their status (0 = Married/partnered, 1 = Single). After accounting for all missing observations on the dependent variable and covariates the analytic sample size for all subsequent analysis was 799.
Using the final analytic sample of 799 observations, we computed descriptive statistics for all covariates by city and estimated bivariate logistic regression models with voter turnout for each covariate. We then estimated a multivariate logistic regression model of voter turnout in the last local election with the key independent variables being measures of health resources, controlling for commute time, working time, household income, educational attainment, race, age, sex, and marital status. We also adjusted for whether the respondent worked in Minneapolis or Raleigh. We examined the potential for multicollinearity across all variables included in the final model by estimating variation inflation factors (VIFs) and all VIFs estimated were less than 2.5 for the model presented. We estimated marginal effects to produce predicted probabilities of turnout. We also estimated a fully interactive model with a dummy variable for city to statistically test whether the relationships between covariates and turnout varied by city. We performed likelihood ratio and Wald tests to estimate the additive value of the interactions by city to the model. Statistical analyses were conducted using Stata version 16.1 (StataCorp, College Station, Texas, United states).
Table 1 presents descriptive statistics of the demographic characteristics, money, and time resources variables. About 45 percent of respondents reported voting in the last local election2. Almost half of the respondents completed some college education or more (47 percent), were aged 40 years or older (50 percent) and the majority of respondents identified as Black (72 percent). The majority of respondents commuted 30 min or less to their place of work (72 percent) and on average respondents worked about 31 h per week, yet almost half of respondents (48 percent) reported an annual household income of less than $10,000.
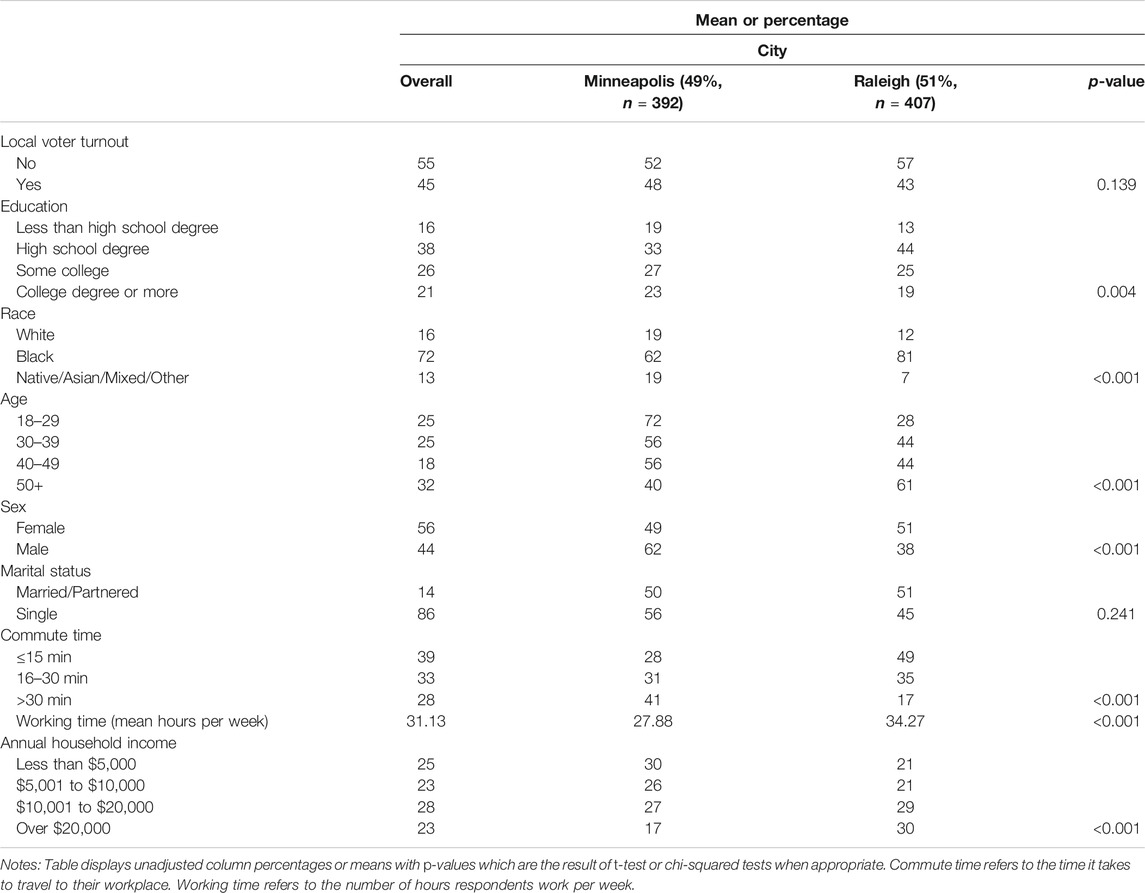
TABLE 1. Descriptive Statistics of Analytic Sample–Demographics and Other Resources, stratified by city (n = 799).
Table 2 shows descriptive statistics of the health resource variables. The majority of respondents in the sample were overweight or obese (72 percent) and current smokers (52 percent). In addition, 33 percent of respondents reported being in only fair or poor health. Most respondents reported having some form of health insurance (74 percent) but about three-quarters of the sample reported food or housing insecurity (75 percent and 72 percent, respectively) and the majority of respondents reported utilizing some government assistance (64 percent), such as supplemental nutrition programs.
Table 3 displays the results from bivariate logistic regression analyses examining the relationship between turnout and the demographic variables and the non-health resources. Respondents who reported attaining a college degree or more were significantly more likely to report turning out to vote at the local-level compared to those who reported not completing high school (p = 0.049). Those who identified as Black were significantly more likely to report turning out to vote compared to those who identified as White (p < 0.001), while identifying as male was associated with significantly lower likelihood of turnout compared to those who identified as female (p < 0.001). All of the age categories were significant, indicating that those aged 30 years or older were significantly more likely to report turning out to vote compared to those aged 18–29 years.
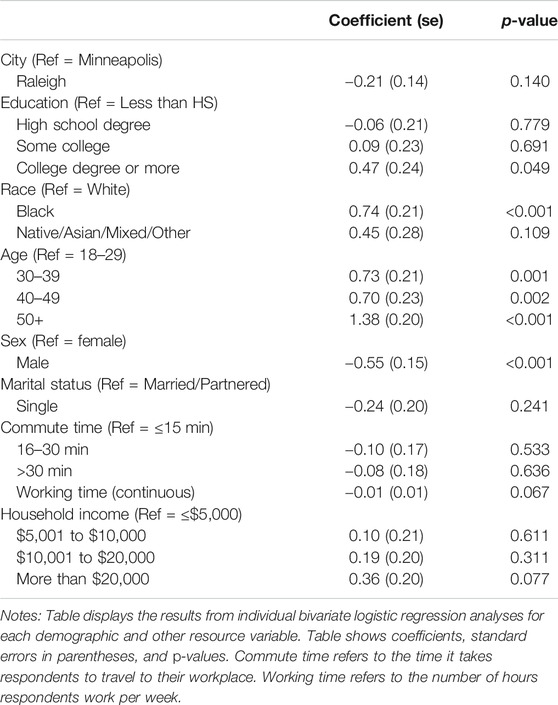
TABLE 3. Associations with turnout at the local-level from bivariate logistic regression models–Demographics and Other Resources (n = 799).
Table 4 displays the results from bivariate logistic regression analyses examining health resources and voter turnout. The results indicate that those individuals who have a BMI greater than 30 were significantly less likely to report voting at the local-level compared to those with a BMI less than 25 (p = 0.002). Those who reported never smoking or having quit smoking were significantly more likely to report turning out to vote compared to current smokers (p < 0.001). Those with insurance were significantly more likely to report voting at the local-level compared to those without any insurance (p < 0.001). Self-rated health, however was not significantly associated with voter turnout, nor was physical disability or mental disability. Food security, housing security, government assistance, and stress were also not significantly associated with voter turnout in the bivariate models.
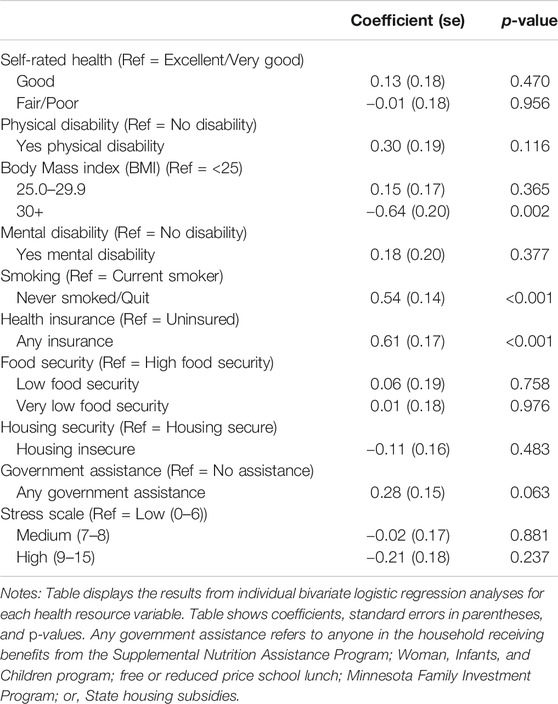
TABLE 4. Associations with turnout at the local-level from bivariate logistic regression models–Health Resources (n = 799).
Results from a multivariate logistic regression model examining local-level voter turnout are shown in Table 5 and indicate that those individuals who have a BMI greater than 30 were significantly less likely to report voting at the local-level compared to those with a BMI less than 25 (marginal effect = −0.10, p = 0.026). Those who reported never smoking or quitting were significantly more likely to report turning out to vote compared to current smokers (marginal effect = 0.10, p = 0.002). Those with insurance were significantly more likely to report voting at the local-level compared to those without any insurance (marginal effect = 0.10, p = 0.022). Marginal effects for all of the health resources are illustrated in Figure 2. Other health resources included in the multivariate model that were not significantly associated with turnout include self-rated health, physical disability, mental disability, food security, housing security, government assistance, and stress.
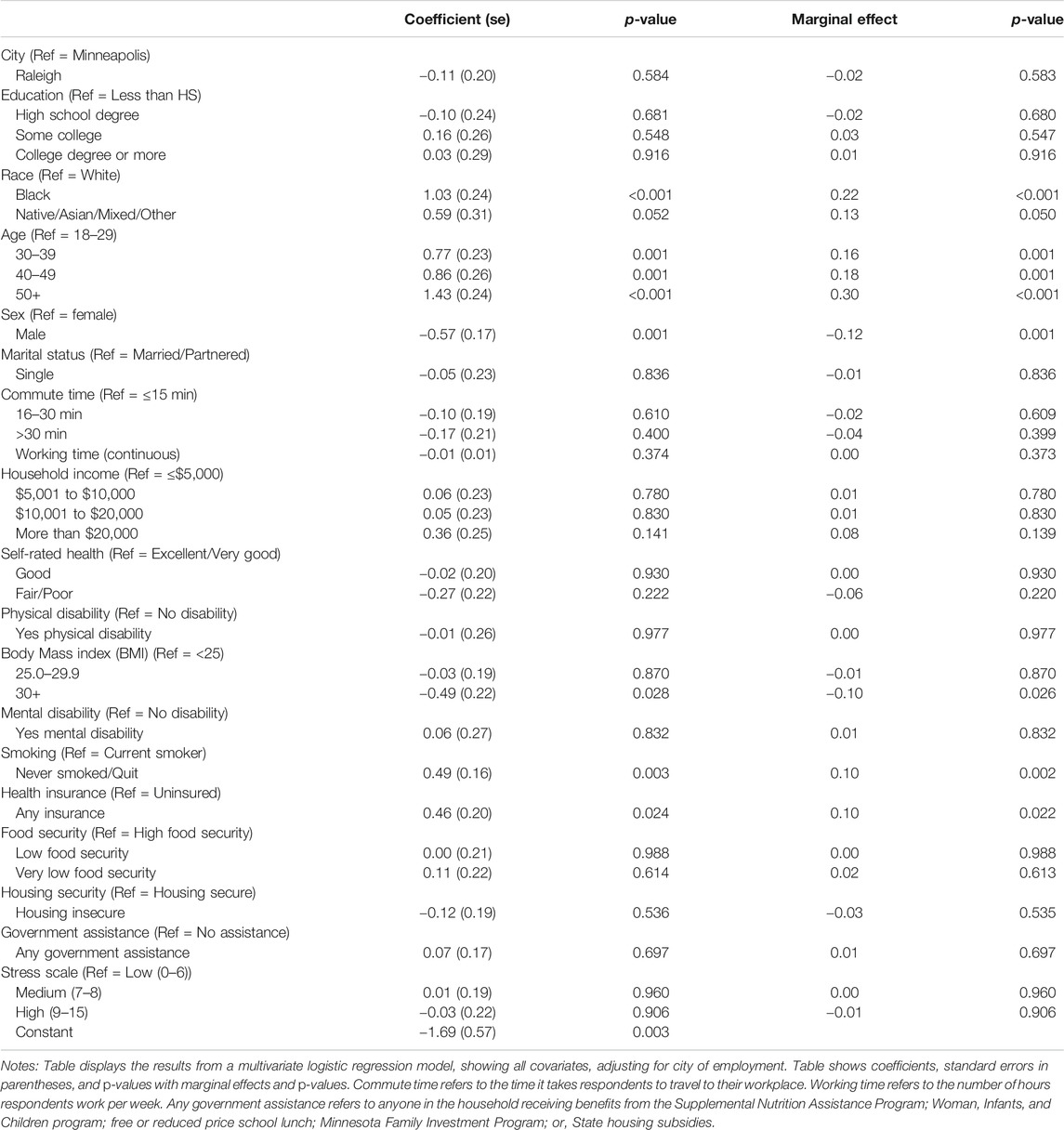
TABLE 5. Associations with turnout at the local-level from multivariate logistic regression model and marginal effects (n = 799).
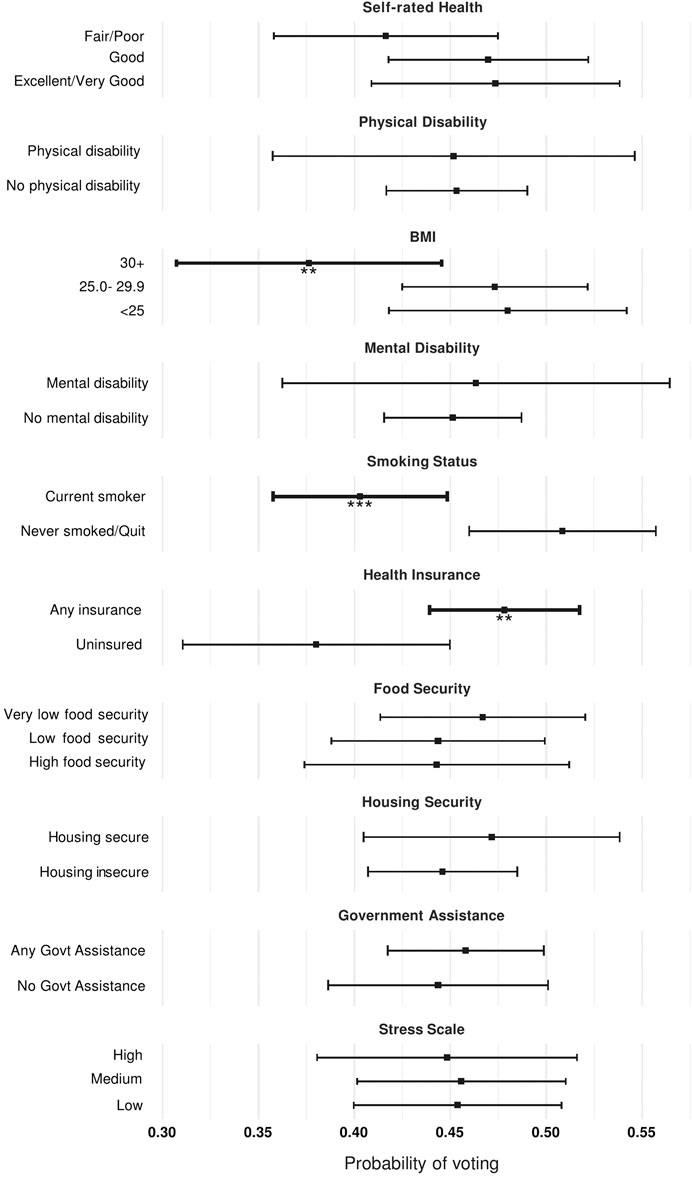
FIGURE 2. Predicted probability of voting in the last local election by health resources. Notes: Figure shows predicted likelihoods with 95 percent confidence intervals from logistic regression model estimating probability of local voter turnout, adjusting for city, education, race, age, sex, marital status, commute time, working time, and household income.***p < 0.01, **p < 0.005.
The multivariate model further show that those who identified as Black were significantly more likely to turnout to vote compared to those who identified as White (marginal effect = 0.22, p = <0.001). Those who reported being aged 30 or more years were significantly more likely to report turning out to vote compared to those aged 18–29 years and those who reported being male were significantly less likely to report turning out to vote compared to females. Education, however, which was significant in the bivariate logistic regression model, was not statistically significant in the multivariate model, controlling for other covariates.
Examining the data by city, in Minneapolis 48 percent of respondents reported turning out to vote, while in Raleigh 43 percent of respondents reported voting in the last local election. These differences in turnout by city were not statistically significant in either the bivariate (Table 3) or multivariate models (Table 5). Results from logistic regression model fully interacted with a city indicator variable suggests that overall there are not significant differences by city in the relationship of the health and demographic covariates with turnout (see Supplementary Table S2 for full regression model). Results from both Wald and likelihood ratio tests suggest that the addition of the interaction terms did not significantly contribute to improving the fit of the model (results not shown).
The purpose of this study was to describe the voter turnout of low-income workers in Raleigh and Minneapolis and examine the associations between health resources and propensity to turnout to vote at the local-level. It is not surprising that less than 50 percent of participants in both cities voted in the last local election for mayor or city council, as a previously mentioned study estimated the average rate of voter turnout for mayoral elections in several United states cities to be only about 19 percent (Aldag, 2016). By city, in Minneapolis 48 percent of participants reported turning out to vote, compared to 43 percent in Raleigh, but these turnout estimates may be overstated due to social desirability bias or recall error (Holbrook and Krosnick, 2010). In 2017, voter turnout in Minneapolis was the highest recorded in the last 20 years for a local-only and odd-year election with an estimated 42 percent turnout (Minneapolis City Council, 2018). However, the estimated turnout in the 2017 runoff election in Raleigh was only about 17 percent of eligible voters (Wake County Government, 2017).
The study population was extremely low-income, with only 23 percent earning more than $20,000 per year as a household. Several characteristics, even within this high-poverty sample, predicted turnout in ways that were consistent with previous literature drawing on nationally representative populations. For instance, older adults were significantly more likely to turnout and those of higher household income had a higher propensity of turnout. Education was significantly associated with turnout in bivariate analyses but was not significant in the multivariate model we estimated, which controlled for many other covariates which may impact this association. Education has long been regarded as one of the best predictors of turnout, however recent work suggests educational attainment may only be an indicator for other pre-adult experiences linked to turnout (Gidengil et al., 2019).
Although previous work has focused on other resources which are key in determining political behavior, we sought to investigate specifically how diminished health resources among this group of low-wage workers may shape participation levels. Within our sample, 33 percent of respondents reported being in fair or poor health. This is starkly bleak compared to a representative sample of residents in the United states, in which only 18.4 percent of respondents reported being in fair or poor health in 2018; within Minnesota only 13.5 percent of respondents reported being in fair or poor health and 19.1 percent in North Carolina (Kaiser Family Foundation, 2019). Yet, although self-rated health has been associated with voter turnout in previous studies, we do not find within our sample that self-rated health is associated with local voter turnout among low-wage workers. This finding is consistent both in our bivariate and multivariate analyses.
We did find that the workers in our sample face significant resource burdens, as the majority reported food or housing insecurity, despite the majority of respondents also reporting some usage of safety-net services, including SNAP, WIC, and State housing subsidies. Yet, in the multivariate analyses neither food security nor housing security were significantly associated with voter turnout at the local level. However, being uninsured was associated with a decreased likelihood of turning out to vote, which is consistent with previous research using national-level data (Gollust and Rahn, 2015). The majority of respondents in our sample reported they have Medicaid as their health insurance provider. While experiences with Medicaid can drastically vary from state to state and can shape political participation (Michener, 2018), we found that the association with having any health insurance and voter turnout did not differ by city. North Carolina is one of only 12 states that has yet to expand Medicaid (Corbo et al., 2020), which we see played out in our study, as 92 percent of Minneapolis participants had insurance vs. only 56 percent in Raleigh. Other work has indicated that health inequities and the associated changes in voting patterns can impact electoral outcomes, therefore if being uninsured depresses turnout at the local-level as indicated here and at the national-level as indicated by other studies, (e.g. Gollust and Rahn, 2015), this has implications for how representative the participating population is regarding issues that affect health insurance in the United states (Rodriguez et al., 2015; Brown et al., 2020).
Body mass index greater than 30 was associated with lower propensity to vote compared to those with BMI less than 25. BMI is included in this study as a measure of physical health, and in the United states a BMI measurement of 30 or greater is a clinical indicator for obesity. Obesity is considered a chronic condition which can lead to various other health problems which may be demobilizing as well, such as increased risk for diabetes, high blood pressure, and other chronic conditions (Centers for Disease Control and Prevention, 2020b). For instance, diabetes and heart disease have been found to be related to lower turnout, albeit with different relationships based on the individual’s race (Gollust and Rahn, 2015). BMI greater than 30 was significant in both the bivariate and the multivariate models, indicating the robustness of the relationship and suggesting that BMI is not simply a proxy for poor self-rated health or physical disability, for which we controlled in the multivariate model. Research in this area should explore whether higher BMI is linked to political participation due to its impact on diminishing physical health or via other mechanisms.
Being a current smoker was associated with lower propensity to turnout to vote, compared to those who reported never smoking or quitting; like obesity, this finding was robust, consistent in both the bivariate and multivariate models. Smoking is included in this study as a health behavior measure through which individuals can invest or divest into their store of health resources. Similar to obesity as a risk factor, engaging in smoking is associated with chronic conditions such as coronary heart disease and lung cancer (Centers for Disease Control and Prevention, 2020a). Our finding that smoking is associated with lower likelihood of turning out to vote is comparable to previous research. For instance, using data on voters in the state of Colorado, one study found that daily smokers were significantly less likely to report turning out to vote in the 2004 United states presidential election compared to non-smokers (Albright et al., 2016). Smoking has been linked to political mistrust in previous studies, which may be attributable to widespread enactment of policies taxing tobacco or prohibiting smoking; however the relationships between smoking and voter turnout is still unclear (Lindström, 2009; Albright et al., 2016). Furthermore, both individuals who smoke and those of higher BMI face social stigmatization, which has been well-documented in other works (Puhl and Heuer, 2010; Riley et al., 2017). These factors may also be a marker for experiencing social marginalization, which could contribute to lower turnout (Gollust and Rahn, 2015). Future research examining smoking and political participation may investigate whether local-level policy regarding tobacco (i.e., cigarette taxes or smoking cessation programs) may impact this relationship and how diminished health attributable to smoking over time may affect likelihood of political participation.
Raleigh and Minneapolis differ in many ways, in terms of their social and political characteristics, as we discuss below. However, overall we did not find significant differences by city within our sample when examining associations between health resources and local-level voter turnout. This is surprising given that the two cities are different in ways that might matter for political participation and the social determinants of health. At the state-level, North Carolina has a preemption law disallowing municipalities from enacting minimum wage ordinances and a recent history of extreme voter suppression efforts, including blatant gerrymandering based on race and voter identification laws, both being challenged in court (Huizar and Lathrop, 2019; Tausanovitch and Root, 2020). At the local-level, until the November 2019 election, Raleigh had a fairly conservative city council, which had fought zoning ordinances that would result in more affordable housing and moved slowly in fully investing in public transit infrastructure (Napier, 2019). In Minnesota, voter suppression lawsuits are also being challenged in court regarding barriers to voting in person and by mail (Condon, 2020). At the local-level, Minneapolis is generally considered liberal, passing progressive policies such as the city minimum wage ordinance in 2017. However the experiences of residents of different races across the city varies drastically and large inequities in health and resources persist (Holder, 2020).
Several limitations of this study must be considered. First, the data for this study were collected in 2018 and both cities had their last mayoral election in 2017, which may have resulted in some recall error when respondents were asked to report their political participation in the last local election. Second, there may be some social desirability bias which may have caused over-reporting of voting (Holbrook and Krosnick, 2010). Third, these data are specific to Minneapolis and Raleigh and therefore are not generalizable to other cities or the United states as a whole. While the lack of generalizability of the data is a limitation, the novelty of the dataset is also a major strength of the study, as we were able to examine a very low-income sample and incorporate multiple measures of health, as opposed to only self-rated health or chronic conditions, in comparison to other United states-based investigations of health and turnout. Fourth, we included only one measure of political participation, local voter turnout, but citizens can participate in politics in a variety of ways, which may be related to their health-related resources. Though compared to studies of national voter turnout, there are few studies examining local voter turnout and health. Lastly, we controlled for city to adjust for any differences in the political or social contexts of Raleigh and Minneapolis, but we did not include any measures of community-level factors, such as political institutions or political leaning of the community, which future studies examining the relationship of community environments and local participation might do.
Looking forward, health will only become a more important determinant of turnout. In the 2020 United states election, state governments implemented new policies and methods of voting, such as voting by curbside in a vehicle and increasing access to voting by mail, amid the global coronavirus pandemic and the risk of COVID-19 associated with in-person voting (Vasilogambros and Van Ness, 2020). If continued, these new alternatives to typical in-person voting may benefit those of low-income or diminished health resources. The Wages Study will be adapting to capture the effects of the global COVID-19 pandemic and examine national-level voter turnout among this population. Overall, future research on local-level political participation should not only focus on voting but also examine behaviors such as volunteering for a campaign or candidate, donating, and protesting. Future scholarship is needed to examine the effects of health resources on local- and national-level voter turnout to understand how these factors may connect to inequitable distribution of political power, as well as electoral and policy outcomes. The ongoing pandemic and recession have already led to more Americans reporting food and housing insecurity, and the Affordable Care Act (ACA) which extended health insurance coverage to many low-income adults is currently being challenged in court (Center on Budget and Policy Priorities, 2020). Diminishing health resources among low-wage workers in the United states may therefore impact political participation in future local and national elections for years to come.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by University of Minnesota Institutional Review Board. The participants provided their written informed consent to participate in this study.
CM conceived the manuscript idea with the support of SG, MD, TD, JW, and CC. CM wrote the manuscript and conducted the data analysis with the support of SG and CC. MD contributed to manuscript writing. JW designed figure two. MD, TD, JW, and CC contributed to the the study design, implementation, and data collection.
This research was supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health (1R01DK118664-01); The National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health supported data management (UL1TR000114 ). A training grant from the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health (T32DK08325010, Principal Investigator: R. Jeffery) supported author CM. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Funding agencies had no role in the design, analysis or writing of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpos.2020.601323/full#supplementary-material.
1In 2016, North Carolina passed state law HB2 which supersedes and preempts any local or city-level policies regarding the compensation of employees, including wage levels (General Assembly of North Carolina, 2016).
2Estimated turnout in the 2017 minneapolis Municipal Election was 42.45 percent (Minneapolis City Council, 2018); estimated turnout in the 2017 Wake County Municipal Election and Runoff was 17.17 percent (Wake County Government, 2017).
Albright, K., Hood, N., Ma, M., and Levinson, A. H. (2016). Smoking and (not) voting: the negative relationship between a health-risk behavior and political participation in Colorado. Nicotine Tob. Res. 18, 371–376. doi:10.1093/ntr/ntv098
Aldag, A. (2016). The local American voter: mayoral election turnout in midsized American cities. IL, United States: Honor. Proj. Illinois Wesley Univ. 48. Available at: https://digitalcommons.iwu.edu/polisci_honproj/48.
Alex-Assensoh, Y. (1997). Race, concentrated poverty, social isolation, and political behavior. Urban Aff. Rev. 33, 209–227. doi:10.1177/107808749703300205
Alford, R. R., and Lee, E. C. (1968). Voting turnout in American cities. Am. Polit. Sci. Rev. 6, 796–813. doi:10.2307/1953431
Baybeck, B. (2014). Local political participation. Oxford Handb. state local Gov,. New York: Oxford University Press 95–109. doi:10.1093/oxfordhb/9780199579679.013.009
Becker, G. S. (2013). Human capital. 2nd Edn. Chicago, IL, United States: The Concise Encyclopedia of Economics. doi:10.7208/chicago/9780226041223.001.0001
Blais, A., and Dobrzynska, A. (1998). Turnout in electoral democracies. Eur. J. Polit. Res. 33, 239–261. doi:10.1111/1475-6765.00382
Brady, H. E., Verba, S., and Schlozman, K. L. (1995). Beyond ses: a resource model of political participation. Am. Polit. Sci. Rev. 89, 271–294. doi:10.2307/2082425
Braveman, P., Egerter, S., and Williams, D. R. (2011). The social determinants of health: coming of age. Annu. Rev. Publ. Health. 32, 381–398. doi:10.1146/annurev-publhealth-031210-101218
Braveman, P., and Gottlieb, L. (2014). The social determinants of health: it’s time to consider the causes of the causes. Publ. Health Rep. 129 (Suppl 2), 19–31. doi:10.1177/00333549141291S206
Braveman, P. (2006). Health disparities and health equity: concepts and measurement. Annu. Rev. Publ. Health., 27, 167–194. doi:10.1146/annurev.publhealth.27.021405.102103
Breslow, L. (2006). Health measurement in the third era of health. Am. J. Publ. Health. 96, 17–19. doi:10.2105/AJPH.2004.055970
Bridges, A. (1997). Morning glories : municipal reform in the Southwest. Princeton, NJ, United States.: Princeton University Press.
Brown, C. L., Raza, D., and Pinto, A. D. (2020). Voting, health and interventions in healthcare settings: a scoping review. Publ. Health Rev. 41, 16. doi:10.1186/s40985-020-00133-6
Burden, B. C., Fletcher, J. M., Herd, P., Jones, B. M., and Moynihan, D. P. (2017). How different forms of health matter to political participation. J. Polit. 79, 166–178. doi:10.1086/687536
Campbell, A. L. (2011). Policy feedbacks and the impact of policy designs on public opinion. J. Health Polit. Policy Law., 36, 961. doi:10.1215/03616878-1460542
Center on Budget and Policy Priorities (2020). Tracking the COVID-19 recession’s effects on food, housing, and employment hardships Available at:Accessed: https://www.cbpp.org/research/poverty-and-inequality/tracking-the-covid-19-recessions-effects-on-food-housing-and November 4, 2020).
Centers for Disease Control and Prevention (2020a). Health effects of cigarette smoking Available at:Accessed: https://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/effects_cig_smoking/index.htm August 23, 2020).
Centers for Disease Control and Prevention (2018). No Title. Heal. Qual. life Available at:Accessed: https://www.cdc.gov/hrqol/wellbeing.htm July 13, 2020).
Centers for Disease Control and Prevention (2020b). Overweight and obesity Available at:Accessed: https://www.cdc.gov/obesity/index.html August 23, 2020).
Clarke, P. J., Ailshire, J. A., Nieuwenhuijsen, E. R., and de Kleijn-de Vrankrijker, M. W. (2011). Participation among adults with disability: the role of the urban environment. Soc. Sci. Med. 72, 1674–1684. doi:10.1016/j.socscimed.2011.03.025
Cohen, C. J., and Dawson, M. C. (1993). Neighborhood poverty and African American politics. Am. Polit. Sci. Rev. 87, 286–302. doi:10.2307/2939041
Cohen, S., Kamarck, T., and Mermelstein, R. (1983). A global measure of perceived stress. J. Health Soc. Behav. 24, 385–396. doi:10.2307/2136404
Commission on Social Determinants of Health (2008). Closing the gap in a generation: health equity through action on the social determinants of health. Final Report of the Commission on Social Determinants of HealthGeneva Available at: https://apps.who.int/iris/bitstream/handle/10665/43943/9789241563703_eng.pdf;jsessionid=3F57BB999A30E0FE96D267184684E200?sequence=1.
Condon, P. (2020). Washington , D.C. Democrats sue to overturn Minnesota voter assistance ban. Star Trib Available at: https://www.startribune.com/d-c-democrats-sue-to-overturn-minn-voter-assistance-ban/567230162/?refresh=true.
Corbo, A., Correa, S. Y., Greenberg, R., Logan, P., and Hunt, H. (2020). Violence against the Poor : the consequences of North Carolina’s failure to expand Medicaid Available at: https://law.unc.edu/wp-content/uploads/2020/06/MedicaidExpansion_final.pdf.
Couture, J., and Breux, S. (2017). The differentiated effects of health on political participation. Eur. J. Publ. Health. 27, 599–604. doi:10.1093/eurpub/ckw245
Dahrendorf, R. (1966). CLASS, status, and power: social stratification IN comparative perspective, Reinhard bendix and seymour martin lipset. 2d edn. NY, United States: The Free Press. Soc. Forces. Tables. $9.95, 677. doi:10.2307/2574402
Denny, K. J., and Doyle, O. M. (2007). “Take up thy bed, and vote” Measuring the relationship between voting behaviour and indicators of health. 17, 400–401. doi:10.1093/eurpub/ckm002
Erikson, R. S. (2015). Income inequality and policy responsiveness. Annu. Rev. Polit. Sci. 18, 11–29. doi:10.1146/annurev-polisci-020614-094706
Gagné, T., Schoon, I., and Sacker, A. (2019). Health and voting over the course of adulthood: evidence from two British birth cohorts, SSM—Popul. Heal. 10, 100531. doi:10.1016/j.ssmph.2019.100531
General Assembly of North Carolina (2016). House Bill 2/SL 2016-3Available at: https://www.ncleg.gov/Sessions/2015E2/Bills/House/PDF/H2v4.pdf.
Gewurtz, R. E., Moll, S. E., Letts, L. J., Larivière, N., Levasseur, M., and Krupa, T. M. (2016). What you do every day matters: a new direction for health promotion. Can. J. Public Health. 107, e205–e208. Available at: http://www.jstor.org/stable/90006457.
Geys, B. (2006). Explaining voter turnout: a review of aggregate-level research, Elect. Stud. 25, 637–663. doi:10.1016/j.electstud.2005.09.002
Gidengil, E., Tarkiainen, L., Wass, H., and Martikainen, P. (2019). Turnout and education: is education proxying for pre-adult experiences within the family?. Polit. Sci. Res. Methods 7, 349–365. doi:10.1017/psrm.2017.32
Goldrick-Rab, S., Richardson, J., and Kinsley, P. (2018). Guide to assessing basic needs insecurity in higher education. 1–33. Available at: http://www.wihopelab.com/publications/Basic-Needs-Insecurity-College-Students.pdf.
Gollust, S. E., and Rahn, W. (2015). The bodies politic: chronic health conditions and voter turnout in the 2008 election. J. Health Polit. Policy Law. 40, 1115. doi:10.1215/03616878-3424450
Hajnal, Z. L., and Lewis, P. G. (2003). Municipal institutions and voter turnout in local elections. Urban Aff. Rev. 38, 645–668. doi:10.1177/1078087403038005002
Hassell, H. J. G., and Settle, J. E. (2017). The differential effects of stress on voter turnout. Polit. Psychol. 38, 533–550. doi:10.1111/pops.12344
Holbrook, A. L., and Krosnick, J. A. (2010). Social desirability bias in voter turnout reports: tests using the item count technique. Publ. Opin. Q. 74, 37–67. doi:10.1093/poq/nfp065
Holder, S. (2020). Why this started in Minneapolis. Bloom. Citylab Available at:Accessed: https://www.bloomberg.com/news/articles/2020-06-05/revealing-the-divisive-history-of-minneapolis August 23, 2020).
Huckfeldt, R. R. (1979). Political participation and the neighborhood social context. Am. J. Pol. Sci. 23, 579–592. doi:10.2307/2111030
Huizar, L., and Lathrop, Y. (2019). Fighting wage pre-emption: how workers have lost billions in wages and how we can restore local democracy.
Kaiser Family Foundation (2019). KFF analysis of the Centers for disease control and prevention (CDC)’s 2013-2019 behavioral risk factor surveillance system (BRFSS) Available at:Accessed: https://www.kff.org/other/state-indicator/adult-self-reported-health-status/?currentTimeframe=1&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D November 4, 2020).
Lahtinen, H., Erola, J., and Wass, H. (2019). Sibling similarities and the importance of parental socioeconomic position in electoral participation. Soc. Forces. 98, 702–724. doi:10.1093/sf/soz010
Lahtinen, H., Mattila, M., Wass, H., and Martikainen, P. (2017). Explaining social class inequality in voter turnout: the contribution of income and health. Scand. Polit. Stud. 40, 388–410. doi:10.1111/1467-9477.12095
Lindström, M. (2009). Social capital, political trust and daily smoking and smoking cessation: a population-based study in southern Sweden. Publ. Health. 123, 496–501. doi:10.1016/j.puhe.2009.06.010
Marmot, M. (2002). The influence of income on health: views of an epidemiologist. Health Aff. 21 (2), 31–46. doi:10.1377/hlthaff.21.2.31
Martikainen, P., Martikainen, T., and Wass, H. (2005). The effect of socioeconomic factors on voter turnout in Finland: a register-based study of 2.9 million voters. Eur. J. Polit. Res. 44, 645–669. doi:10.1111/j.1475-6765.2005.00242.x
Matsubayashi, T., and Ueda, M. (2014). Disability and voting. Disabil. Health J. 7, 285–291. doi:10.1016/j.dhjo.2014.03.001
Matsubayashi, T. (2010). Racial environment and political participation. Am. Polit. Res. 38, 471–501. doi:10.1177/1532673X09335486
Mattila, M., Rapeli, L., Wass, H., and Söderlund, P. (2017). in Health and political engagement. Editors L. Rapeli, H. M. Wass, and P. Söderlund. (Oxfordshire United Kingdom: Taylor and Francis). doi:10.4324/9781315561691
Mattila, M., Söderlund, P., Wass, H., and Rapeli, L. (2013). Healthy voting: the effect of self-reported health on turnout in 30 countries. Elect. Stud. 32, 886–891. doi:10.1016/j.electstud.2013.07.010
Mccabe, B. J. (2013). Are homeowners better citizens? Homeownership and community participation in the United States. Soc. Forces 91, 929–954. doi:10.1093/sf/sos185
McLeroy, K. R., Bibeau, D., Steckler, A., and Glanz, K. 1988). An ecological perspective on health promotion programs. Health Educ. Q. 15, 351. doi:10.1177/109019818801500401
Mettler, S., and Soss, J. (2004). The consequences of public policy for democratic citizenship: bridging policy studies and mass politics. Perspect. Polit. 2, 55–73. doi:10.1017/S1537592704000623
Michael, R. T. (1973). Education in nonmarket production. J. Polit. Econ. 81, 306–327. doi:10.1086/260029
Michener, J. (2018). in Fragmented democracy : medicaid, federalism, and unequal politics. Editor P. (Cambridge, NY, United States: Cambridge UniversityCambridge University Press).
Minneapolis City Council (2018). The 2017 municipal election: an analysis and recommendations Available at: https://lims.minneapolismn.gov/Download/RCA/4684/2017 Municipal Election Report.pdf.
Morlan, R. L. (1984). Municipal vs. National election voter turnout: europe and the United States. Polit. Sci. Q. 99, 457–470. doi:10.2307/2149943
Napier, C. (2019). History has its eyes on the new Raleigh city council. Indyweek. Available at:Accessed: https://indyweek.com/news/voices/history-has-its-eyes-on-the-new-raleigh-city-council/(August 23, 2020).
Ojeda, C. (2015). Depression and political participation. Soc. Sci. Q. 96, 1226–1243. doi:10.1111/ssqu.12173
Ojeda, C., and Pacheco, J. (2019). Health and voting in young adulthood, Cambridge Core. 49, 1163–1186. doi:10.1017/S0007123417000151
Ojeda, C. (2018). The two income-participation gaps. Am. J. Pol. Sci. 62, 813–829. doi:10.1111/ajps.12375
Pacheco, J., and Fletcher, J. (2015). Incorporating health into studies of political behavior: evidence for turnout and partisanship. Polit. Res. Q. 68, 104–116. doi:10.1177/1065912914563548
Puhl, R. M., and Heuer, C. A. (2010). Obesity stigma: important considerations for public health. Am. J. Publ. Health. 100, 1019–1028. doi:10.2105/AJPH.2009.159491
Riley, K. E., Ulrich, M. R., Hamann, H. A., and Ostroff, J. S. (2017). Decreasing smoking but increasing stigma? Anti-tobacco campaigns, public health, and cancer Care. AMA J. ethics. 19, 475–485. doi:10.1001/journalofethics.2017.19.5.msoc1-1705
Rodriguez, J. M., Geronimus, A. T., Bound, J., and Dorling, D. (2015). Black lives matter: differential mortality and the racial composition of the United states electorate, 1970-2004. Soc. Sci. Med. 136-137, 193–199. doi:10.1016/j.socscimed.2015.04.014
Rosenstone, S. J. (1982). Economic adversity and voter turnout. Am. J. Pol. Sci. 26, 25–46. doi:10.2307/2110837
Schlozman, K. L., Verba, S., and Brady, H. E. (2012). The unheavenly chorus: unequal political voice and the broken promise of American democracy. NJ, United States: Princeton University Press.
Shanafelt, A., Sadeghzadeh, C., Chapman, L., De Marco, M., Harnack, L., Gust, S., et al. (2020). Recruitment of low-wage workers for a time-sensitive natural experiment to evaluate a minimum wage policy: challenges and lessons learned. Field Methods. (Accepted June 2, 2020).
Sharp, E. B. (2013). Does local government matter? How urban policies shape civic engagement. Int. J. Urban Reg. Res. 37, 1856–1857. doi:10.1111/1468-2427.12107_2
Smets, K., and van Ham, C. (2013). The embarrassment of riches? A meta-analysis of individual-level research on voter turnout. Elect. Stud. 32, 344–359 doi:10.1016/j.electstud.2012.12.006
Soss, J. (1999). Lessons of welfare: policy design, political learning, and political action. Am. Polit. Sci. Rev. 93, 363–380. doi:10.2307/2585401
Sund, R., Lahtinen, H., Wass, H., Mattila, M., and Martikainen, P. (2016). How voter turnout varies between different chronic conditions? A population-based register study. J. Epidemiol. Community Health. 71, 475. doi:10.1136/jech-2016-208314
Tausanovitch, A., and Root, D. (2020). How partisan gerrymandering limits voting rights. Available at: https://cdn.americanprogress.org/content/uploads/2020/07/07113745/GerrymanderVotingRights-brief.pdf?_ga=2.27199999.398824090.1598226663-95214874.1598226663.
USDA, E. R. S. (2012). Food security in the United States—survey tools Available at:Accessed https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/survey-tools/#six October 4, 2017).
Vasilogambros, M., and Van Ness, L. (2020). States expanded voting access for the pandemic. The changes might stick. Pew charit. Trust Available at:Accessed https://www.pewtrusts.org/en/research-and-analysis/blogs/stateline/2020/11/06/states-expanded-voting-access-for-the-pandemic-the-changes-might-stick December 18, 2020).
Wake County Government (2017). Municipal elections official results Available at:Accessed http://www.wakegov.com/elections/data/Past Election Results/2017-11-07 - Municipal Election and Runoff/20171107.Summary.htm December 18, 2020).
Wass, H., Mattila, M., Rapeli, L., and Söderlund, P. (2017). Voting while ailing? The effect of voter facilitation instruments on health-related differences in turnout. J. Elections, Public Opin. Parties. 27, 503–522. doi:10.1080/17457289.2017.1280500
Williams, B. (2017). Minneapolis council approves $15 an hour minimum wage. MPR News, Available at:Accessed https://www.mprnews.org/story/2017/06/30/minneapolis-council-approves-15-dollar-minimum-wage August 20, 2020).
Williamson, D. L., and Carr, J. (2009). Health as a resource for everyday life: advancing the conceptualization. Crit. Publ. Health. 19, 107–122. doi:10.1080/09581590802376234
World Health Organization (1986). Ottawa charter for health promotion. The 1st International Conference on Health Promotion, Ottawa, 1986, Ottawa, Canada, 17–21 November 1986.
Keywords: resources, health, low-income, voter turnout, political participation, social determinants of health
Citation: McGuire CM, Gollust SE, De Marco M, Durfee T, Wolfson J and Caspi CE (2021) Equity at the Ballot Box: Health as a Resource for Political Participation Among Low-Income Workers in Two United States Cities. Front. Polit. Sci. 2:601323. doi: 10.3389/fpos.2020.601323
Received: 31 August 2020; Accepted: 21 December 2020;
Published: 22 January 2021.
Edited by:
Hanna Wass, University of Helsinki, FinlandReviewed by:
Christopher Ojeda, The University of Tennessee, Knoxville, United StatesCopyright © 2021 McGuire, Gollust, De Marco, Durfee, Wolfson and Caspi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cydney M. McGuire, bWNndWk0MTdAdW1uLmVkdQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.