- 1Physical Education Institute, Jiangsu Normal University, Xuzhou, China
- 2Library, Jiangsu Normal University, Xuzhou, China
Context: Anterior cruciate ligament (ACL) injuries are prevalent in sports and often require surgical intervention followed by rehabilitation. Several rehabilitation methods have been used for patients after ACL surgery.
Objective: This study aimed to assess the overall efficacy of exercise therapy in improving outcomes for patients following ACL surgery using a systematic review and meta-analysis of randomized controlled trials (RCTs).
Data sources: PubMed, Web of Science, Embase, and the Cochrane Library were searched for randomized controlled trials published from 1 January 2000 to 30 August 2024. Study quality was assessed using the Cochrane Risk-of-Bias tool.
Study selection: A total of 11 randomized controlled trials (whole-body vibration training = 4, core-stability training = 2, strength training = 3, blood flow restriction training = 1, and aquatic training = 1) involving 552 anterior cruciate ligament surgery patients were included.
Data extraction: Two researchers individually screened the key information for each eligible study and evaluated the quality of the studies. Any dispute was discussed by a third researcher.
Results: Compared with conventional therapy, exercise therapy significantly reduced pain scores (mean difference: −0.53, 95% CI: −0.82 to −0.24, and p < 0.001) and improved muscle strength (flexion: 13.76 and extension: 12.46) and knee function (effect size: 2.06 and p = 0.001). Secondary outcomes, although less pronounced, also demonstrated improvement.
Limitation: The sources of heterogeneity among the included studies were not fully identified, particularly concerning variations in exercise protocols or patient characteristics. Additionally, the therapeutic effects of specific exercise modalities (e.g., strength training versus aquatic training) were not directly compared.
Conclusion: Exercise therapy is effective in reducing pain, enhancing muscle strength, and improving knee function in ACL surgery patients. These findings underscore the importance of integrating tailored exercise therapies into rehabilitation programs.
Systematic review registration number: https://www.crd.york.ac.uk/PROSPERO/, identifier registration number. CRD42023476653.
Introduction
The anterior cruciate ligament (ACL), an intra-articular ligament located outside the synovial membrane (Diermeier et al., 2020), plays as a pivotal role in the knee joint. It originates from the medial wall of the lateral condyle of the femur and consists of the anteromedial bundle and posterolateral bundle (Samuelsson et al., 2009; Acevedo et al., 2014). The ACL primarily acts as a stabilizer for the knee joint by resisting hyperextension of the knee, anterior tibia, and rotation (Acevedo et al., 2014). Additionally, it is also an important proprioceptive receptor that can signal changes in the knee joint (van Melick et al., 2016). However, many risk factors may cause damage to the ACL. The internal factors include high body mass index, lower limb muscle strength deficiency, sex (women are at greater risk of injury), and the state of the body during exercise (Diermeier et al., 2020; Acevedo et al., 2014). The external factors encompass the sports venue, weather, and competition level (Acevedo et al., 2014). At the same time, ACL is relatively fragile in response to acute torsional or shear forces (Jenkins et al., 2022). Hence, ACL injuries often occur during sudden sports activities.
ACL injury represents approximately 50% of knee injuries, of which 70%–80% were non-contact injuries (Kaeding et al., 2017; Boden et al., 2000). Non-contact injuries usually occur during a jump landing, swerving, or stopping (Boden et al., 2000). Once the ACL is injured, the tibia’s forward motion relative to the femur cannot be confined, thereby impairing the support, flexion, and extension functions of the lower limbs. In a short period of time, a large amount of fluid accumulates in the knee joint, and the degree of motion decreases significantly (Jenkins et al., 2022). A literature review in 2022 found that there were approximately 80,000 to 120,000 patients with ACL injuries in the United States each year (Gornitzky et al., 2016). After the injury occurred, some patients who were reluctant to undergo surgery also achieved better results. However, for young people and those who wish to return to pre-injury activity levels, surgery is the only option (Gerber et al., 2009). Bone–patella tendon–bone (BPTB) graft is considered the gold standard for surgical reconstruction (Diermeier et al., 2020), but it increases the risk of patellofemoral osteoarthritis (OA) and secondary diseases (Papageorgiou et al., 2001; Canzone et al., 2024). Compared to the BPTB graft, the autologous hamstring tendon (HT) graft reduces the risk of secondary diseases, but the rotational relaxation of the grafted ligaments increases over time (Samuelsson et al., 2009). Therefore, rehabilitation after surgery is equally important.
For patients undergoing ACL surgery (ACLS), rehabilitation is to restore joint movement, lower-limb muscle mass, and knee function (Jenkins et al., 2022) so as to achieve pre-injury activity levels and functional status. Clinical guidelines from the American Physical Therapy Association state that rehabilitation can enhance lower-limb muscle strength (Logerstedt et al., 2010). At the same time, it is recommended to conduct an early joint range of motion association 1 week after surgery to prevent the occurrence of soft tissue diseases such as joint contracture (Logerstedt et al., 2010). In addition, a study on postoperative rehabilitation has found that these training strategies can significantly reduce the risk of secondary injuries such as meniscus and arthritis (Suter and Herzog, 2000).
However, a standard postoperative rehabilitation strategy is lacking, and the design (Jenkins et al., 2022), type, and timing of rehabilitation programs vary widely (Kotsifaki et al., 2023; Buckthorpe, 2021). Therefore, it is particularly important to elucidate the advantages and disadvantages of various rehabilitation programs. Traditional therapy is currently the mainstay rehabilitation approach in clinical practice, which can facilitate the recovery of postoperative muscle strength and motion (Capin et al., 2018; Clark et al., 2015). Usually, it uses physical instrument therapy (e.g., cryotherapy and neuromuscular electrical stimulation), physical therapist-assisted therapy (e.g., continuous passive motion and Kinesio-taping), and some common forms of exercise (most are simple strength training) to achieve the effect of rehabilitation (Kotsifaki et al., 2023). However, due to the lack of targeted exercise training or treatment, patient recovery and outcomes are often compromised. Therefore, it is necessary to include specific exercises in the patient’s rehabilitation program.
Exercise therapy (ET) techniques mainly include strength training, progressive training, and functional training (Kotsifaki et al., 2023; Korakakis et al., 2021; Beard and Dodd, 1998; Culvenor et al., 2022), which are essential for patients to regain their original mobility. One of the most common training methods in exercise therapy, strength training, commonly used in the postoperative rehabilitation of sport-related injuries, is considered the best strategy to prevent muscle atrophy (Logerstedt et al., 2010; Kotsifaki et al., 2023; Buckthorpe, 2021). In addition to the conventional exercise training methods, some new training methods have emerged in other fields. As for postoperative rehabilitation training for ACL patients, these new methods are also worth studying. For example, whole-body vibration training (WBVT) can improve neuromuscular activation to some extent (Moezy et al., 2008). It works by providing rapid, brief, and repetitive intermittent vibrations to the body, causing the body to produce vertical, horizontal, or interactive displacement (Shantakumari and Ahmed, 2023). The trainer himself needs to use body force to maintain balance in order to achieve the purpose of training (Shantakumari and Ahmed, 2023). This approach is more effective in enhancing postural control, muscle, and stability in patients after ACLS than traditional rehabilitation methods (Fu et al., 2013). Moreover, some new training methods have emerged in recent years, such as blood flow restriction training (BFRT) and water-based exercise, which have been used for the rehabilitation of patients after ACLS. The mechanism of BFRT involves the trainer creating an ischemic and hypoxic environment in the affected area during BFR, which increases metabolism (Hughes et al., 2017). At the same time, the combination of BFR and exercise can induce mechanical tension (Hughes et al., 2017). These are key factors in the development of muscle hypertrophy (Hughes et al., 2017; Pearson and Hussain, 2015). Current research on BFRT has focused on the mechanism of delaying muscle atrophy (Charles et al., 2020). Water-based exercise involves performing exercises, which are generally performed on land, in water. This method is characterized by exercising in water. On one hand, due to the presence of buoyancy, the risk of injury is reduced for individuals with excessive weight or reduced lower-limb strength (Zhu et al., 2023). On the other hand, due to the presence of resistance in water, exercisers will be subjected to additional stimulation (Zhu et al., 2023).
In recent years, published reviews of the efficacy of ET in patients after ACLS have mostly focused on a single exercise or just an evidence-based guideline (Kotsifaki et al., 2023; Buckthorpe, 2021; Culvenor et al., 2022; Poretti et al., 2023; Wengle et al., 2022). Meanwhile, clinical trials have high specificity, but few articles have systematically reviewed the role of exercise therapy in rehabilitation programs. To address these shortcomings, we conducted a systematic review and meta-analysis of randomized controlled trials (RCTs) published since 2000 to explore the role of exercise therapy in the rehabilitation of patients after ACLS.
Methods
Procedures
This study protocol was registered in the PROSPERO database (registration no. CRD42023476653; 2023.11.23), and this study was reported according to the PRISMA guidelines (Moher et al., 2009).
Search strategy
PubMed, Web of Science, Embase, and the Cochrane Library were searched for RCTs on ET for the rehabilitation of patients after ACLS. Mesh terms and free-text words were combined to create the search terms, including “anterior cruciate ligament reconstruction,” “anterior cruciate ligament injuries,” “exercise therapy,” “kinesiotherapy,” and “random allocation.” The complete search strategy is detailed in Supplementary Material S1. Two researchers independently searched for potential studies published between 1 January 2000 and 30 August 2024 (we only included studies published within this period). Disagreements, if any, were addressed by a third reviewer.
Eligibility criteria
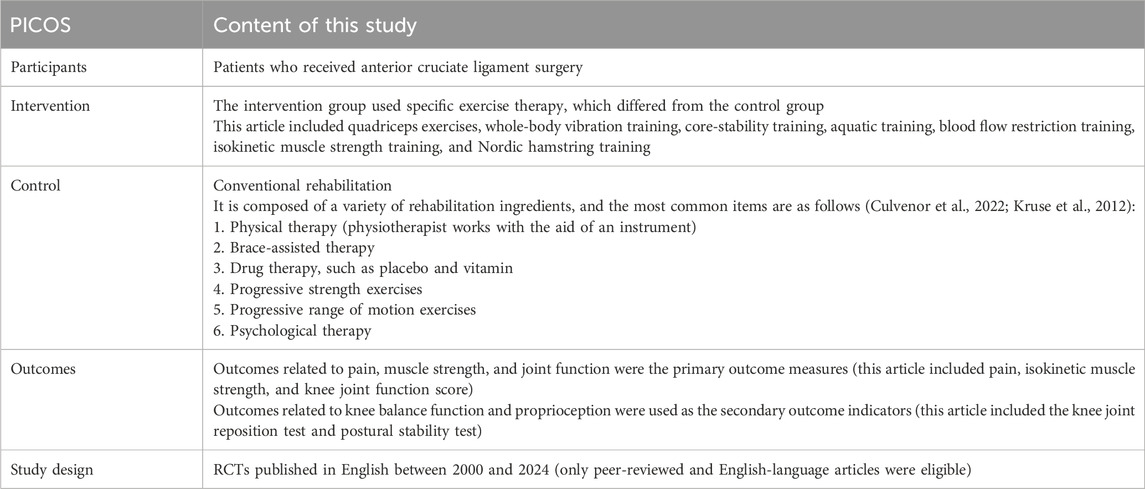
The criteria for inclusion were designed following the PICOS principle, which was as follows (Diermeier et al., 2020): participants: patients had to undergo ACLS (Samuelsson et al., 2009). Intervention: the intervention group used ET, which differed from the one used by the control group (strength training, aquatic training, and vibration training) (Acevedo et al., 2014). Control: the control group used conventional rehabilitation (van Melick et al., 2016). Study design: RCTs published in English between 2000 and 2024 were eligible (Jenkins et al., 2022). Only peer-reviewed and English-language articles were eligible. The exclusion criteria were as follows (Diermeier et al., 2020): patients with ACL injury who did not undergo surgery (Samuelsson et al., 2009); ET types that were not significantly different from that of the control group (such as aerobic exercise, cycling, or walking; these exercises were used in the usual treatment group and could not be compared to the control group in some studies) or reported outcome measures (psychological indexes or electroencephalogram indexes; these results were relevant to ACL rehabilitation, but our study focused on outcomes of joint function rather than psychological outcomes) that were unrelated (Acevedo et al., 2014); a sample size of fewer than 10 cases in each group (if the sample size was too small, we believe that the quality of the results was low, and there may be particularities and chance involved) (van Melick et al., 2016); case reports, animal experiments, review articles, and unpublished articles (Jenkins et al., 2022); the control group used the same or other exercise rehabilitation interventions as the experimental group (Kaeding et al., 2017); and research methods were of low quality, or peer review was unclear. Details are shown in Table 1.
Data extraction
After removing duplicates, unrelated studies were filtered out through the examination of titles and abstracts. The full texts of the remaining studies were carefully read to screen eligible trials. Two reviewers independently undertook data extraction. The extracted data encompassed the author, information on the participants (such as origin, number, type of operation, and age), and intervention design (such as inserted exercise type, details of exercise, and duration). We used Microsoft Excel to manage and convert data. All results were extracted in the form of mean and standard deviation, and only two decimal places were retained. In the event of data loss, we contacted the authors to obtain the original data. If the authors could not be contacted, this part of the data was excluded as missing data. Any disagreements were addressed by a third reviewer. The three researchers discussed the dissents and finally reached a consensus.
Outcome measures
The outcome measures were recorded at each assessment point (baseline and post-intervention). The primary outcomes were pain, the isokinetic muscle strength test, and the knee function score. Among them, pain was measured by the visual analog scale (VAS), one of the prevalent methods to assess the health-associated quality of life (Åström et al., 2023). The isokinetic muscle strength test is a safe method to measure muscle strength using a specific instrument and a fixed angular speed (Cheng et al., 2019). The scales for measuring knee joint function were different across studies, and we finally analyzed the Lysholm and International Knee Documentation Committee (IKDC) scores. Secondary outcomes encompassed the knee joint reduction test and postural stability test. In addition, these outcomes were depicted as the mean and standard deviation. In case of disagreements, a third reviewer was consulted to help reach a resolution.
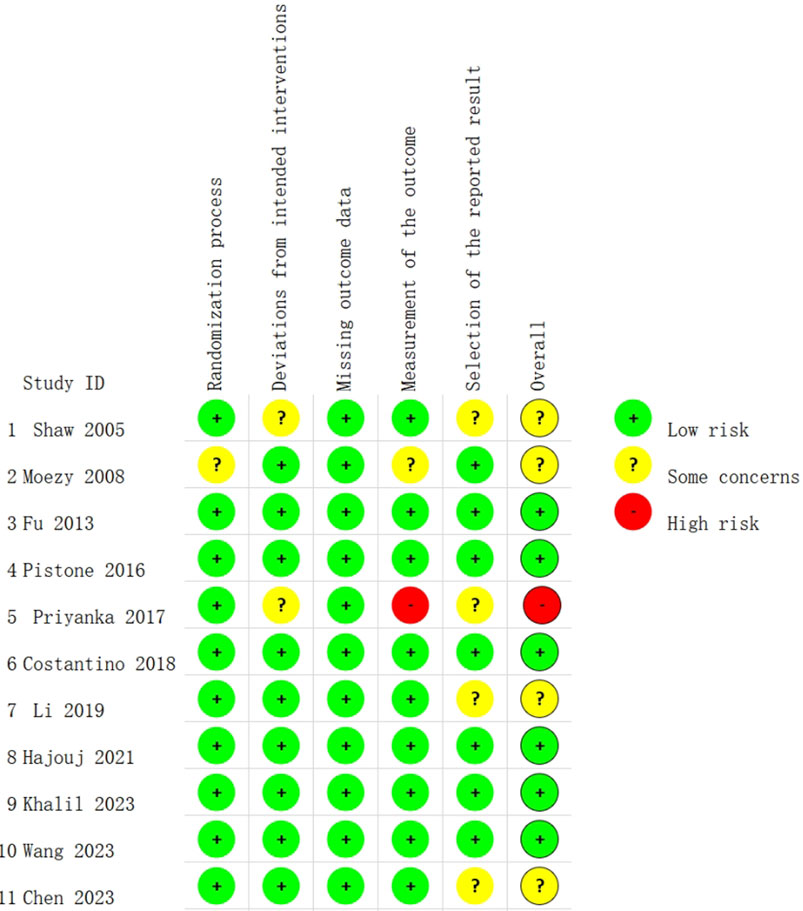
Risk of bias
Two reviewers, working independently, evaluated the risk of bias (RoB) in the recruited RCTs utilizing the Cochrane Risk-of-Bias Tool (RoB 2.0). Each study was assessed and graded as “low RoB,” “some concerns,” or “high RoB” in five domains, namely, randomization process, deviations from intended intervention, missing outcome data, outcome measurement, and selection of the reported results, including deviations from the registered protocol. In cases where a trial exhibited a high risk in at least one domain, it was graded as having an overall high RoB, while it was graded as having an overall low risk if the RoB across all domains was low.
Data analysis
The first step was to calculate the changes in outcomes of the experimental and control groups from baseline to post-intervention. The mean difference (MD) or weighted mean difference (WMD) with a 95% confidence interval (CI) was reported for continuous data. STATA 15.0 was used for meta-analysis. Cochran’s Q test and Higgins I2 test were executed to gauge heterogeneity. p < 0.10 or I2 > 50% implied substantial heterogeneity, and then a random-effects model was adopted. Otherwise, a fixed-effects model was utilized. Sensitivity and subgroup analyses were conducted to determine the origin of heterogeneity in cases of high heterogeneity. p < 0.05 indicated a statistical difference. To assess publication bias statistically, Egger’s and Begg’s tests were employed, and funnel plots were used for visual inspection. The trim and filling method was utilized to clarify the influence of publication bias on the meta-analysis result.
Result
Search result
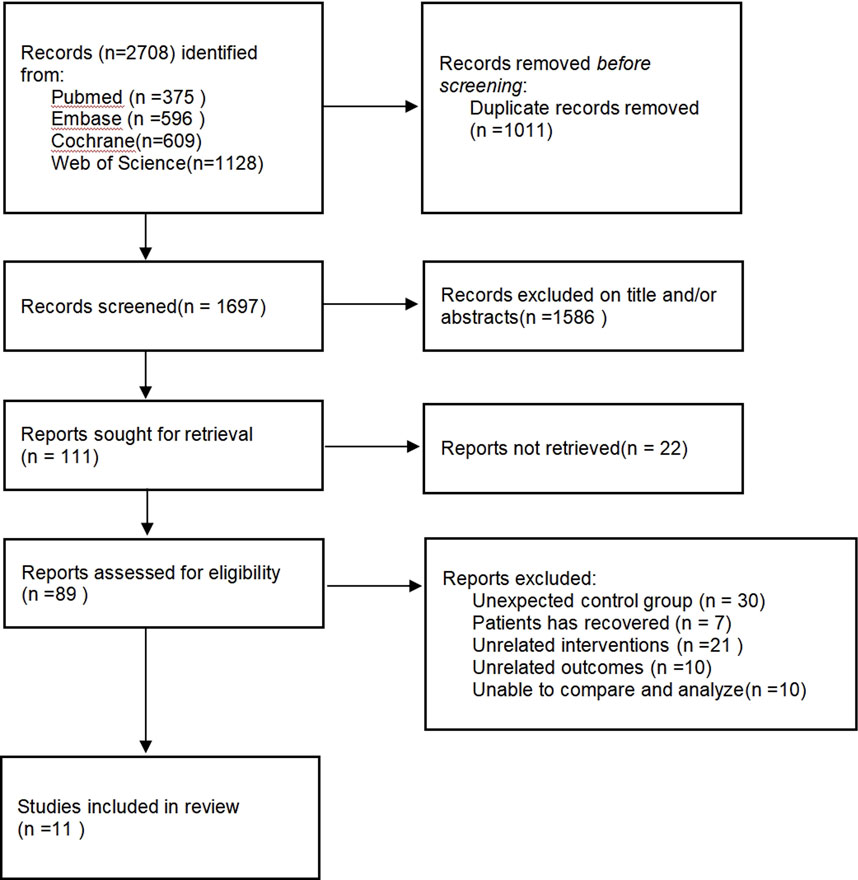
Figure 1 displays the literature retrieval and screening process. A total of 2,708 potential studies were obtained from electronic databases. Based on the title, abstract, and duplicate records, 2,597 studies were eliminated. After reading the full texts of the remaining 111 reports, 100 were ruled out due to unexpected control groups (n = 30), unrelated interventions (n = 21), and unrelated outcomes (n = 10). Finally, 11 RCTs were included.
Study characteristics
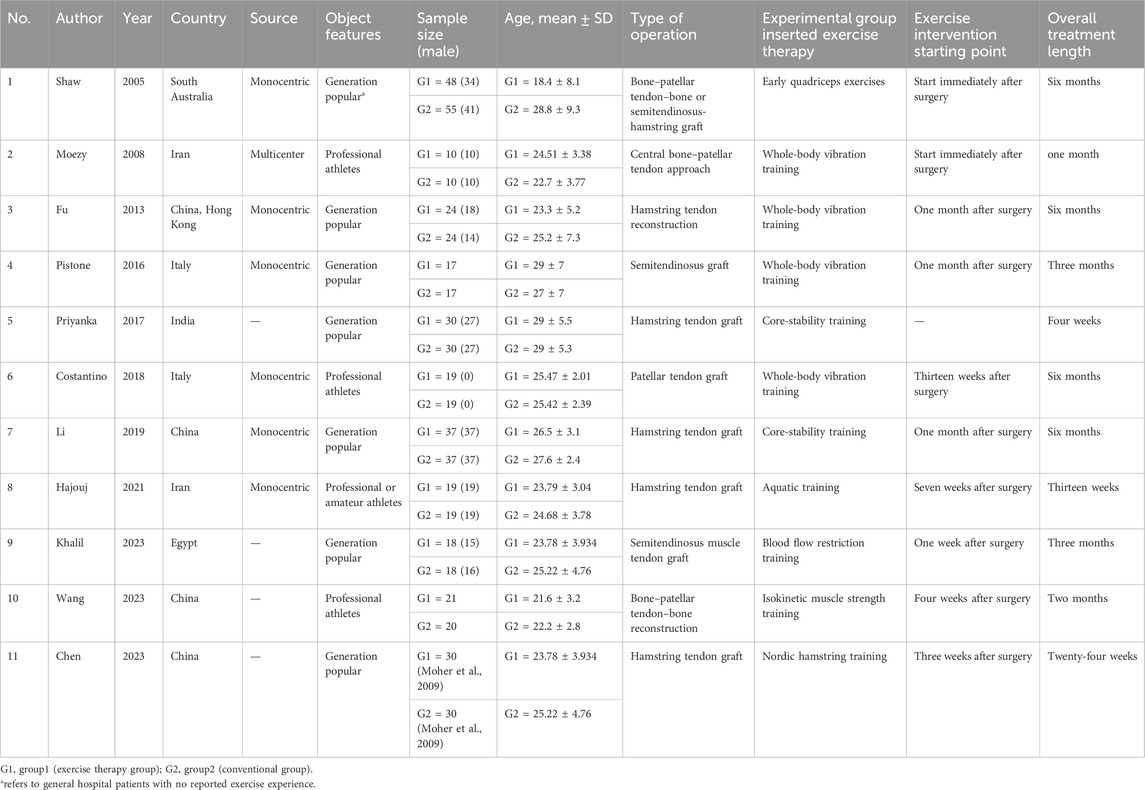
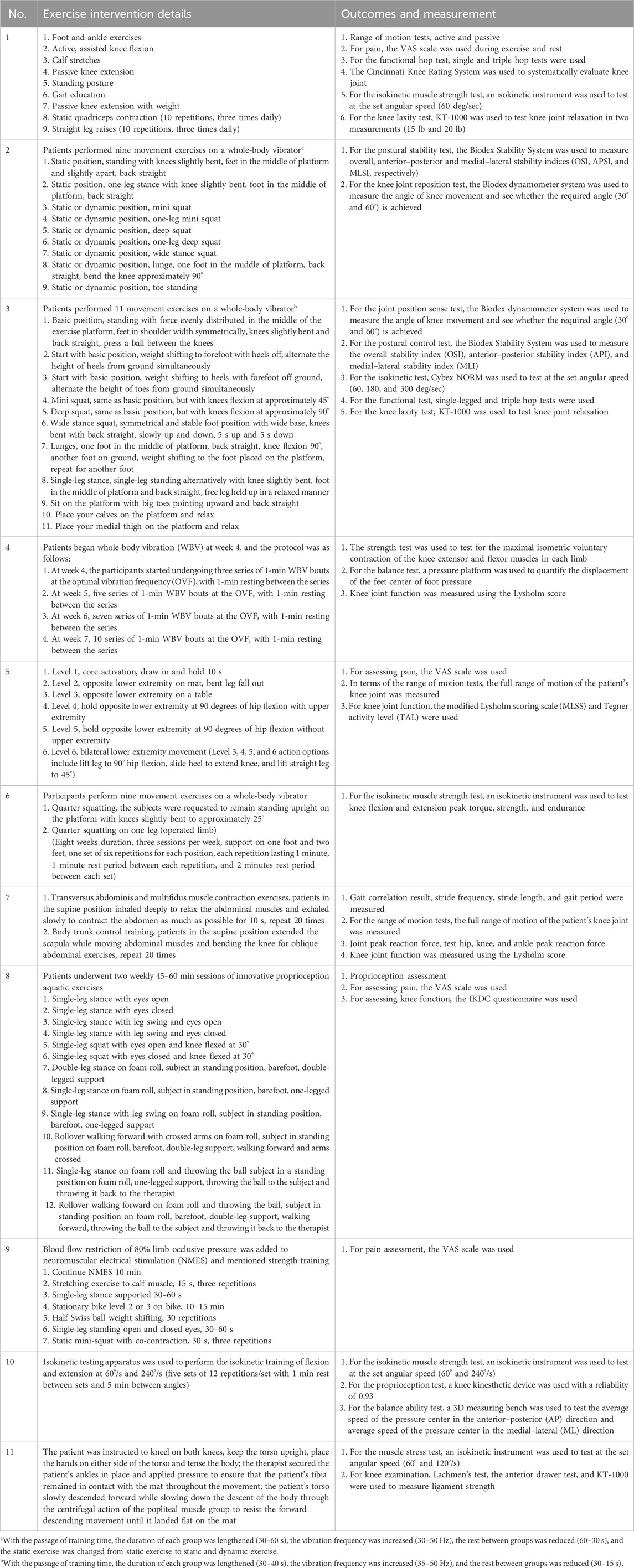
The included RCTs were published between 2000 and 2023, and the exercise intervention, duration, and outcome measures varied across these studies. There were 552 participants from seven regions, and all participants underwent ACL surgery recently. The sample size of each group ranged from 10 to 55 cases, with participants aged 10–36 years, and most participants were male. The treatment duration varied from 1 to 6 months. WBVT was used in four studies, core-stability training in two studies, strength training in three studies, BFRT in one study, and aquatic training in one study. The detailed characteristics are provided in Tables 2, 3.
RoB
The Cochrane Risk-of-Bias Tool (RoB 2.0) was used to evaluate the RoB. Figure 2 shows the RoB assessment results. Each RCT described the random sequence generation process. In terms of outcome reporting, four studies (Shaw et al., 2005; Priyanka et al., 2017; Li and Xie, 2019; Chen et al., 2023) were deemed to have some concerns. The deviation from the intended intervention was not clear in two studies (Shaw et al., 2005; Priyanka et al., 2017), and no studies had a RoB of missing outcome data. Overall, six studies (Fu et al., 2013; Pistone et al., 2016; Costantino et al., 2018; Hajouj et al., 2021; Wang et al., 2023; Khalil et al., 2023) were graded as having low RoB, four studies (Moezy et al., 2008; Shaw et al., 2005; Li and Xie, 2019; Chen et al., 2023) were graded as having some concern, and only one study (Priyanka et al., 2017) was graded as having high RoB. The high RoB may be ascribed to the insufficient description of relevant information on participants.
Effect of ET on primary outcomes
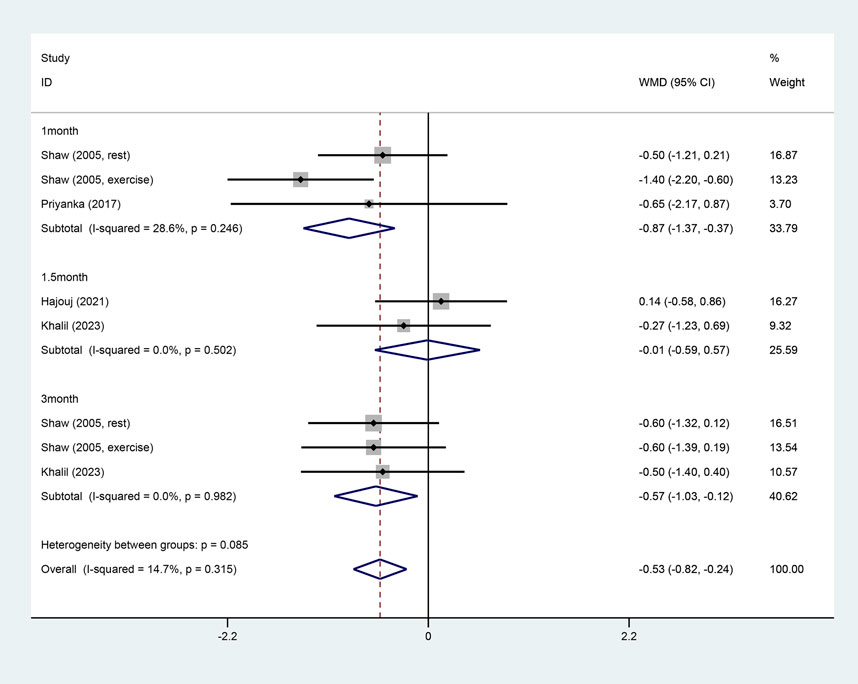
Pain rated by VAS
Four studies reported pain (Shaw et al., 2005; Priyanka et al., 2017; Hajouj et al., 2021; Khalil et al., 2023). Due to small heterogeneity (I2 = 14.7%), a fixed-effect model was adopted. ET significantly lowered VAS scores compared to conventional rehabilitation (WMD = −0.53, 95% CI: −0.82 - −0.24, and p < 0.001). Additionally, a subgroup analysis by intervention duration found that ET significantly relieved pain in both short term (WMD = −0.87, 95% CI: −1.37 - −0.37, and p = 0.001) and long term (WMD = −0.57, 95% CI: −1.03 - −0.12, and p = 0.014) but not in the medium term (WMD = −0.01, 95% CI: −0.59 - 0.57, and p = 0.975) (Figure 3).
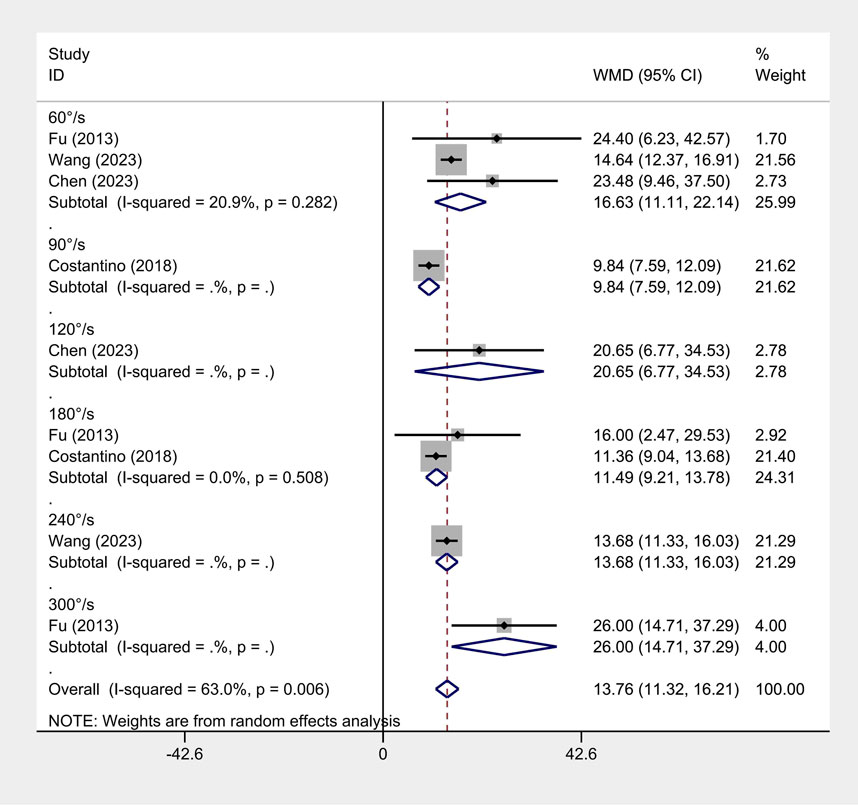
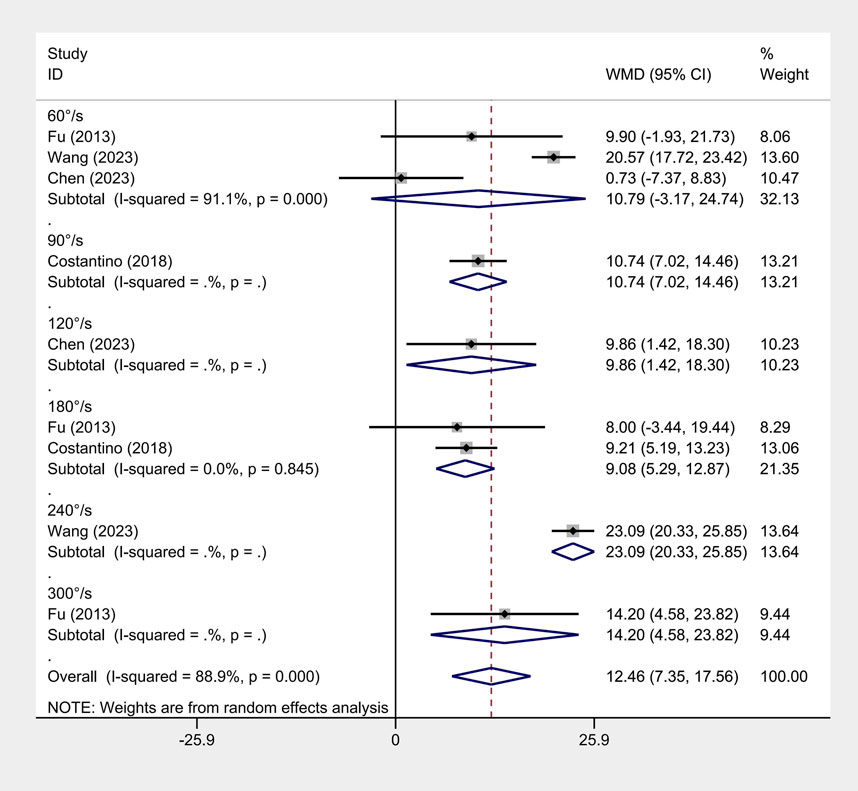
Isokinetic muscle strength
Four articles reported isokinetic muscle strength (Fu et al., 2013; Chen et al., 2023; Costantino et al., 2018; Wang et al., 2023). Due to large heterogeneity (flexion I2 = 63% and extension I2 = 88.9%), a random-effects model was employed. ET significantly improved isokinetic muscle strength at both flexion (WMD = 13.76, 95% CI: 11.32 - 16.21, and p < 0.001) and extension (WMD = 12.46, 95% CI: 7.35 - 17.56, and p < 0.001). A subgroup analysis by angular velocity found significant differences between ET and conventional rehabilitation (Figures 4, 5).
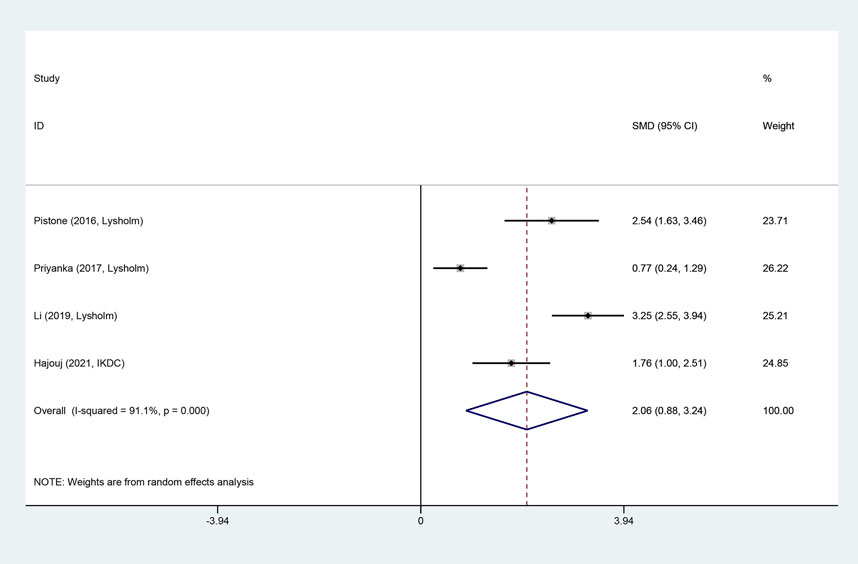
Knee joint function score
Four articles reported knee joint function scores after the intervention. Due to large heterogeneity (I2 = 91.1%), a random-effects model was utilized. ET significantly improved knee joint function (SMD = 2.06, 95% CI: 0.88 - 3.24, and p = 0.001). In the original studies, although both the ET and conventional rehabilitation groups had an average knee function score of more than 70 points (a score of over 65 indicated a favorable knee function), the ET group exhibited higher scores than the conventional rehabilitation group (Figure 6).
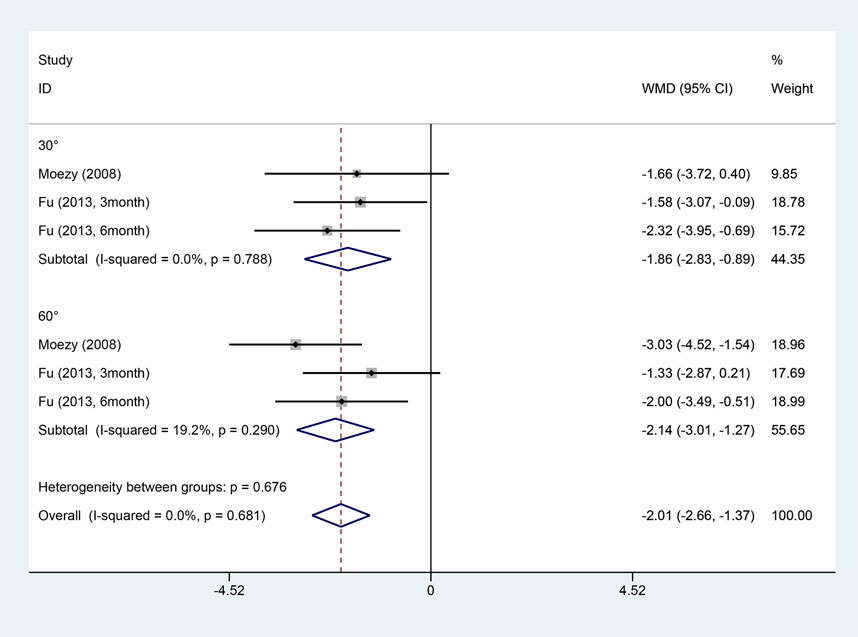
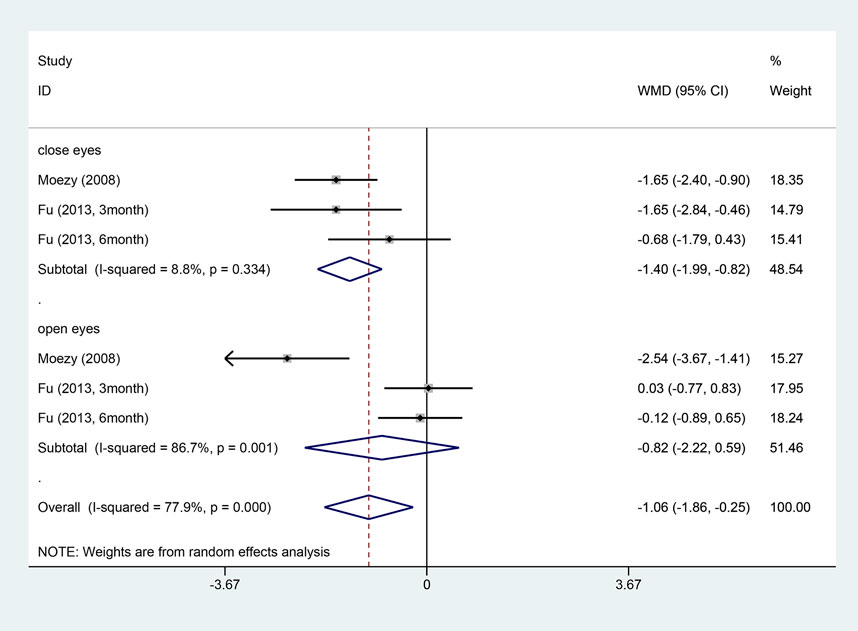
Effect of ET on secondary outcomes
Two articles reported on the knee joint reposition test (Moezy et al., 2008; Fu et al., 2013). Due to small heterogeneity (I2 = 0%), a fixed-effects model was employed. Two studies applied the postural stability test (Moezy et al., 2008; Fu et al., 2013). Due to large heterogeneity (I2 = 77.9%), a random-effects model was utilized. ET outperformed conventional rehabilitation in both the joint reposition test (WMD = −2.01, 95% CI: −2.66 - −1.37, and p < 0.001) and the postural stability test (WMD = −1.06, 95% CI: −1.86 - −0.25, and p = 0.01) (Figures 7, 8). A subgroup analysis by postural stability test noted significant differences between the two groups when their eyes were closed (WMD = −1.40, 95% CI: −1.99 - −0.82, and p < 0.001), but no difference was observed when their eyes were open (WMD = −0.82, 95% CI: −2.22 - 0.59, and p = 0.254).
Sensitivity analysis
Sensitivity analysis was performed for four outcomes, namely, pain score, isokinetic muscle strength, joint reposition test, and postural stability test. By individually removing one study at a time, sensitivity analysis unraveled no statistically notable changes in the meta-analysis results.
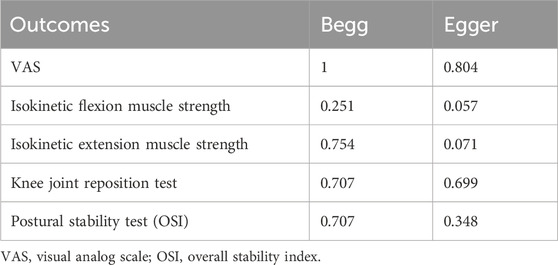
Publication bias
Begg’s and Egger’s tests demonstrated little evidence of publication bias in the primary outcomes (VAS: Begg’s test = 1 and Egger’s test = 0.804; IFMS: Begg’s test = 0.251 and Egger’s test = 0.057; and IEMS: Begg’s test = 0.754, and Egger’s test = 0.071) or secondary outcomes (KJRT: Begg’s test = 0.707 and Egger’s test = 0.699 and OSI: Begg’s test = 0.707 and Egger’s test = 0.348) (Table 4).
Discussion
This paper comprehensively compares the efficacy of the rehabilitation program with specific ET and conventional rehabilitation in patients after ACLS from 2000 to 30 August 2024. A total of 11 studies were screened, involving 552 individuals undergoing ACLS. The results evinced that the specific ET-based rehabilitation program was more effective in alleviating pain and improving joint muscle strength and knee joint functions than the conventional rehabilitation program. Subgroup analyses demonstrated marked differences in pain relief between the two rehabilitation programs in both the short and long terms, but no difference was observed in the medium term. Second, ET also enhanced the stability of the knee joint and facilitated joint reduction. Heterogeneity analyses pointed out high heterogeneity in all outcomes except for the pain and knee joint reduction test, which may be related to differences in participants and intervention durations.
Pain was assessed through the VAS scale, which determines pain levels by measuring the distance between pain-free points and marked points (Hawker et al., 2011). Our findings aligned with those reported in recent reviews on exercise interventions, which suggest that exercise can significantly reduce pain in patients (Culvenor et al., 2022; Owen et al., 2020; Fernández-Rodríguez et al., 2022). The reason for pain relief may be that exercise can improve muscle tension and modify abnormal activity patterns (Kim and Yim, 2020; Barbieri et al., 2019). This explanation is based on the perspective of muscle function. Furthermore, a recent study has suggested a link between pain relief and the regulation of the central nervous system (Belavy et al., 2021). For example, mind–body exercises such as yoga can reduce the intensity of self-perceived pain and, thus, increase pain tolerance (Cherkin and Herman, 2018). Chronic exercise training can not only induce adaptive muscle hypertrophy but also enhance the plasticity of the central nervous system, thus managing pain; vigorous exercises also reduce pain sensitivity, thereby raising the pain threshold (Belavy et al., 2021). According to the subgroup analysis, the statistical analysis revealed a significant difference in pain relief between the rehabilitation program with specific ET and conventional rehabilitation for both the short-term (1 month) and long-term (3 months) results, while the medium-term (1.5 months) results did not show any marked differences. This finding has profound implications for the timing of ET. While ensuring patients’ safety (no secondary injury or disease), early exercise rehabilitation training can relieve pain and accelerate recovery. In addition, there are differences in pain relief between different types of ET. An RCT has found that in the early postoperative period, resistance training combined with BFRT is more effective in pain relief than resistance training alone (Vieira de Melo et al., 2022). Nonetheless, our study only explored the effect of adding ET to treatment programs and failed to compare different ET types. More trials are needed to examine the differences in their efficacy.
Several articles measured muscle strength using an isokinetic muscle strength test. Despite a strict requirement for test equipment, it can well-avoid secondary injury in patients during the test. Our subgroup analysis by angular velocity proved that ET significantly improved isokinetic muscle strength more at angular velocities ranging from 60°/s to 300°/s. This result may benefit from resistance exercises (Owen et al., 2020; Fyfe et al., 2022; Hurst et al., 2022). Appropriate resistance exercise can produce certain mechanical tension, which is essential for strength recovery (Fyfe et al., 2022). Additionally, the maintenance of muscle hypertrophy requires intense stimulation. Conversely, with proper resistance, muscle strength can be increased and maintained with little need for stimulation (Fyfe et al., 2022; Chodzko-Zajko et al., 2009). Importantly, resistance exercise is deemed the only non-pharmacological treatment that can improve muscle mass and strength (Fyfe et al., 2022; Dent et al., 2018). Although the intervention duration was not analyzed, our findings showed that ET outperformed conventional rehabilitation in maintaining and increasing muscle strength in both short- and long-term studies.
In addition to pain and strength, this study also focused on knee joint function scores. The Lysholm and IKDC scsales have been used to measure knee joint function in many studies. The former is often used to evaluate knee joint function after knee ligament surgery, especially symptoms of instability (Collins et al., 2011). The latter is often used to assess knee ligament damage (Collins et al., 2011). The Lysholm scores are graded as excellent (95–100), good (84–94), and fair (65–83) (Collins et al., 2011). This study only analyzed the post-intervention Lysholm scores. After the exercise treatment, the average Lysholm score was higher than 70, and the ET group exhibited a higher overall score than the conventional rehabilitation group. Furthermore, both scales include walking, running, knee stability, and thigh atrophy (Collins et al., 2011). Frequent use of the knee joint and stress stimulation with appropriate intensity during exercise accelerated recovery and greatly improved the knee joint function. Traditionally, individuals undergoing ACLS receive passive physical therapy, which emphasizes the effectiveness of instruments with less active exercise or specific sports training. This may explain why the ET group exhibited better functional recovery.
The meta-analysis results of the knee joint reduction and postural stability tests showed that ET outperformed conventional rehabilitation. This may be ascribed to the frequent engagement of the knee joint during exercise, which can facilitate recovery, improve joint functions, and enhance the proprioception of the knee joint (Şahin et al., 2015). However, since these two outcomes are less frequently reported, supporting these findings requires the accumulation of more evidence and studies.
Strengths and limitations
Summarizing the role of exercise interventions in ACLS patients’ rehabilitation programs, this paper represents the most recent compilation of evidence and focuses on three primary outcome measures and two secondary outcomes during knee recovery. Furthermore, compared with the current mainstream analysis of drugs and physical therapies, this study concentrates on the advantages of exercise.
There are also some limitations. Among the screened RCTs, the frequency, type, and intensity of exercise vary significantly, which may lead to some heterogeneity. Although relevant subgroup analyses were conducted for the results with high heterogeneity, the source of heterogeneity remained unclear. Furthermore, due to the insufficient data, heterogeneity was not explained comprehensively, which may introduce bias in the result reporting. Furthermore, differences in participants’ information, such as age, gender, height, weight, and type of surgery, may have affected the results. Across the studies included, the average age spanned from 18 to 29 years, and the gender ratio also varied. It is unknown whether ET is equally effective for individuals of different ages and gender. In addition, the original studies did not provide relevant information on possible adverse events, hindering further analysis in our study. Finally, because our analysis only included studies written in English, there may be some selection biases. To reduce heterogeneity, future research can include studies on the same type of exercise to investigate the effect of different frequencies, intensities, and durations of exercise.
Practical implications
ET can help improve physical conditions in exercisers without external drug intake or physical stimulation. Therefore, such rehabilitation approaches are beneficial for patients with muscle and ligament injuries. This finding suggests that more treatment methods are available in clinical practice. For example, exercise interventions may be used instead of medications to relieve pain. Although many trials have demonstrated the benefits of ET, the appropriate type, intensity, and frequency of exercise remain to be elucidated. Meanwhile, for patients undergoing knee surgery, the timing of adding ET to rehabilitation programs remains inconclusive. Thus, a pooled analysis in this regard can provide an evidence-based basis for the formulation and updating of clinical guidelines.
Conclusion
ET outperformed conventional rehabilitation in alleviating pain and enhancing muscle strength and knee functions in individuals undergoing ACLS. Further research is needed to investigate the appropriate frequency, intensity, and type of exercise to optimize personalized treatment for this population.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material; further inquiries can be directed to the corresponding author.
Author contributions
HZ: data curation, formal analysis, methodology, validation, visualization, writing–original draft, and writing–review and editing. JQ: data curation, formal analysis, methodology, and writing–review and editing. Y-MX: software, supervision, visualization, and writing–review and editing. LC: formal analysis, investigation, and writing–review and editing. Y-FB: conceptualization, funding acquisition, investigation, resources, supervision, and writing–review and editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This research was supported by the Jiangsu University blue project funding project.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphys.2025.1501458/full#supplementary-material
Abbreviations
ET, exercise therapy; ACLS, anterior cruciate ligament surgery; RCTs, randomized controlled trials; VAS, visual analog scale; ACL, anterior cruciate ligament; BPTB, bone–patella tendon–bone; OA, osteoarthritis; HT, hamstring tendon; WBVT, whole-body vibration training; BFRT, blood flow restriction training; RoB, risk of bias; MD, mean difference; WMD, weighted mean difference; CI, confidence interval; IKDC, International Knee Documentation Committee.
References
Acevedo R. J., Rivera-Vega A., Miranda G., Micheo W. (2014). Anterior cruciate ligament injury: identification of risk factors and prevention strategies. Curr. sports Med. Rep. 13 (3), 186–191. doi:10.1249/JSR.0000000000000053
Åström M., Thet Lwin Z. M., Teni F. S., Burström K., Berg J. (2023). Use of the visual analogue scale for health state valuation: a scoping review. Qual. life Res. Int. J. Qual. life aspects Treat. care rehabilitation 32 (10), 2719–2729. doi:10.1007/s11136-023-03411-3
Barbieri E., Capparucci I., Mannello F., Annibalini G., Contarelli S., Vallorani L., et al. (2019). Efficacy of a treatment for gonarthrosis based on the sequential intra-articular injection of linear and cross-linked hyaluronic acids. Orig. Art. 9(4).
Beard D. J., Dodd C. A. (1998). Home or supervised rehabilitation following anterior cruciate ligament reconstruction: a randomized controlled trial. J. Orthop. sports Phys. Ther. 27 (2), 134–143. doi:10.2519/jospt.1998.27.2.134
Belavy D. L., Van Oosterwijck J., Clarkson M., Dhondt E., Mundell N. L., Miller C. T., et al. (2021). Pain sensitivity is reduced by exercise training: evidence from a systematic review and meta-analysis. Neurosci. Biobehav. Rev. 120, 100–108. doi:10.1016/j.neubiorev.2020.11.012
Boden B. P., Dean G. S., Feagin J. A., Garrett W. E. (2000). Mechanisms of anterior cruciate ligament injury. Orthopedics 23 (6), 573–578. doi:10.3928/0147-7447-20000601-15
Buckthorpe M. (2021). Recommendations for movement re-training after ACL reconstruction. Sports Med. Auckl. NZ 51 (8), 1601–1618. doi:10.1007/s40279-021-01454-5
Canzone A., Roggio F., Patti A., Giustino V., Mannucci C., Di Mauro D., et al. (2024). Classification of physical activity programs based on the kellgren and lawrence scale for knee osteoarthritis: a systematic review. A Syst. Rev. 22 (4), e70019. doi:10.1002/msc.70019
Capin J. J., Khandha A., Zarzycki R., Arundale A. J. H., Ziegler M. L., Manal K., et al. (2018). Gait mechanics and tibiofemoral loading in men of the ACL-sports randomized control trial. J. Orthop. Res. official Publ. Orthop. Res. Soc. 36 (9), 2364–2372. doi:10.1002/jor.23895
Charles D., White R., Reyes C., Palmer D. (2020). A systematic review of the effects of blood flow restriction training on quadriceps muscle atrophy and circumference post acl reconstruction. Int. J. sports Phys. Ther. 15 (6), 882–891. doi:10.26603/ijspt20200882
Chen J., Wu T., Guo Y. (2023). Nordic hamstring exercises in functional knee rehabilitation after anterior cruciate ligament reconstruction: a prospective, randomised, controlled study. Sci. Rep. 13 (1), 19039. doi:10.1038/s41598-023-45817-6
Cheng L., Chang S., Qian L., Wang Y., Yang M. (2019). Extracorporeal shock wave therapy for isokinetic muscle strength around the knee joint in athletes with patellar tendinopathy. J. sports Med. Phys. Fit. 59 (5), 822–827. doi:10.23736/S0022-4707.18.09023-0
Cherkin D. C., Herman P. M. (2018). Cognitive and mind-body therapies for chronic low back pain and neck pain: effectiveness and value. JAMA Intern. Med. 178 (4), 556–557. doi:10.1001/jamainternmed.2018.0113
Chodzko-Zajko W. J., Proctor D. N., Fiatarone Singh M. A., Minson C. T., Nigg C. R., Salem G. J., et al. (2009). American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med. Sci. sports Exerc. 41 (7), 1510–1530. doi:10.1249/MSS.0b013e3181a0c95c
Clark N. C., Röijezon U., Treleaven J. (2015). Proprioception in musculoskeletal rehabilitation. Part 2: clinical assessment and intervention. Man. Ther. 20 (3), 378–387. doi:10.1016/j.math.2015.01.009
Collins N. J., Misra D., Felson D. T., Crossley K. M., Roos E. M. (2011). Measures of knee function: international knee documentation committee (IKDC) subjective knee evaluation form, knee injury and osteoarthritis outcome score (KOOS), knee injury and osteoarthritis outcome score physical function short form (KOOS-PS), knee outcome survey activities of daily living scale (KOS-ADL), lysholm knee scoring scale, oxford knee score (OKS), western ontario and mcmaster universities osteoarthritis index (WOMAC), activity rating scale (ARS), and tegner activity score (TAS). Arthritis care and Res. 63 (11), S208–S228. doi:10.1002/acr.20632
Costantino C., Bertuletti S., Romiti D. (2018). Efficacy of whole-body vibration board training on strength in athletes after anterior cruciate ligament reconstruction: a randomized controlled study. Clin. J. sport Med. official J. Can. Acad. Sport Med. 28 (4), 339–349. doi:10.1097/JSM.0000000000000466
Culvenor A. G., Girdwood M. A., Juhl C. B., Patterson B. E., Haberfield M. J., Holm P. M., et al. (2022). Rehabilitation after anterior cruciate ligament and meniscal injuries: a best-evidence synthesis of systematic reviews for the OPTIKNEE consensus. Br. J. sports Med. 56 (24), 1445–1453. doi:10.1136/bjsports-2022-105495
Dent E., Morley J. E., Cruz-Jentoft A. J., Arai H., Kritchevsky S. B., Guralnik J., et al. (2018). International clinical practice guidelines for sarcopenia (ICFSR): screening, diagnosis and management. J. Nutr. health and aging 22 (10), 1148–1161. doi:10.1007/s12603-018-1139-9
Diermeier T., Tisherman R., Hughes J., Tulman M., Baum Coffey E., Fink C., et al. (2020). Quadriceps tendon anterior cruciate ligament reconstruction. Knee Surg. sports traumatology, Arthrosc. official J. ESSKA 28 (8), 2644–2656. doi:10.1007/s00167-020-05902-z
Fernández-Rodríguez R., Álvarez-Bueno C., Cavero-Redondo I., Torres-Costoso A., Pozuelo-Carrascosa D. P., Reina-Gutiérrez S., et al. (2022). Best exercise options for reducing pain and disability in adults with chronic low back pain: pilates, strength, core-based, and mind-body. A network meta-analysis. J. Orthop. sports Phys. Ther. 52 (8), 505–521. doi:10.2519/jospt.2022.10671
Fu C. L., Yung S. H., Law K. Y., Leung K. H., Lui P. Y., Siu H. K., et al. (2013). The effect of early whole-body vibration therapy on neuromuscular control after anterior cruciate ligament reconstruction: a randomized controlled trial. Am. J. sports Med. 41 (4), 804–814. doi:10.1177/0363546513476473
Fyfe J. J., Hamilton D. L., Daly R. M. (2022). Minimal-dose resistance training for improving muscle mass, strength, and function: a narrative review of current evidence and practical considerations. Sports Med. Auckl. NZ 52 (3), 463–479. doi:10.1007/s40279-021-01605-8
Gerber J. P., Marcus R. L., Dibble L. E., Greis P. E., Burks R. T., LaStayo P. C. (2009). Effects of early progressive eccentric exercise on muscle size and function after anterior cruciate ligament reconstruction: a 1-year follow-up study of a randomized clinical trial. Phys. Ther. 89 (1), 51–59. doi:10.2522/ptj.20070189
Gornitzky A. L., Lott A., Yellin J. L., Fabricant P. D., Lawrence J. T., Ganley T. J. (2016). Sport-specific yearly risk and incidence of anterior cruciate ligament tears in high school athletes: a systematic review and meta-analysis. Am. J. sports Med. 44 (10), 2716–2723. doi:10.1177/0363546515617742
Hajouj E., Hadian M. R., Mir S. M., Talebian S., Ghazi S. (2021). Effects of innovative aquatic proprioceptive training on knee proprioception in athletes with anterior cruciate ligament reconstruction: a randomized controlled trial. archives bone Jt. Surg. 9 (5), 519–526. doi:10.22038/abjs.2020.50106.2485
Hawker G. A., Mian S., Kendzerska T., French M. (2011). Measures of adult pain: visual analog scale for pain (VAS pain), numeric rating scale for pain (NRS pain), McGill pain questionnaire (MPQ), short-form McGill pain questionnaire (SF-mpq), chronic pain grade scale (CPGS), short form-36 bodily pain scale (SF-36 BPS), and measure of intermittent and constant osteoarthritis pain (ICOAP). Arthritis care and Res. 63 (Suppl. 11), S240–S252. doi:10.1002/acr.20543
Hughes L., Paton B., Rosenblatt B., Gissane C., Patterson S. D. (2017). Blood flow restriction training in clinical musculoskeletal rehabilitation: a systematic review and meta-analysis. Br. J. sports Med. 51 (13), 1003–1011. doi:10.1136/bjsports-2016-097071
Hurst C., Robinson S. M., Witham M. D., Dodds R. M., Granic A., Buckland C., et al. (2022). Resistance exercise as a treatment for sarcopenia: prescription and delivery. Age ageing 51 (2), afac003. doi:10.1093/ageing/afac003
Jenkins S. M., Guzman A., Gardner B. B., Bryant S. A., Del Sol S. R., McGahan P., et al. (2022). Rehabilitation after anterior cruciate ligament injury: review of current literature and recommendations. Curr. Rev. Musculoskelet. Med. 15 (3), 170–179. doi:10.1007/s12178-022-09752-9
Kaeding C. C., Léger-St-Jean B., Magnussen R. A. (2017). Epidemiology and diagnosis of anterior cruciate ligament injuries. Clin. sports Med. 36 (1), 1–8. doi:10.1016/j.csm.2016.08.001
Khalil A. A., Fayaz N. A., Fawzy E., Mohamed N. A., Waly A. H., MmjjoPT M., et al. (2023). Influence of blood flow restriction training on knee pain after anterior cruciate ligament reconstruction: a double blinded randamized controlled trial. J. of Pop. Thera. and Cli. Pharma. 30(7):30–38.
Kim B., Yim J. (2020). Core stability and hip exercises improve physical function and activity in patients with non-specific low back pain: a randomized controlled trial. Tohoku J. Exp. Med. 251 (3), 193–206. doi:10.1620/tjem.251.193
Korakakis V., Kotsifaki A., Korakaki A., Karanasios S., Whiteley R. (2021). Current perspectives and clinical practice of physiotherapists on assessment, rehabilitation, and return to sport criteria after anterior cruciate ligament injury and reconstruction. An online survey of 538 physiotherapists. Phys. Ther. sport official J. Assoc. Chart. Physiother. Sports Med. 52, 103–114. doi:10.1016/j.ptsp.2021.08.012
Kotsifaki R., Korakakis V., King E., Barbosa O., Maree D., Pantouveris M., et al. (2023). Aspetar clinical practice guideline on rehabilitation after anterior cruciate ligament reconstruction. Br. J. sports Med. 57 (9), 500–514. doi:10.1136/bjsports-2022-106158
Kruse L. M., Gray B., Wright R. W. (2012). Rehabilitation after anterior cruciate ligament reconstruction: a systematic review. J. bone Jt. Surg. Am. volume 94 (19), 1737–1748. doi:10.2106/JBJS.K.01246
Li J., Xie X. (2019). Effects of core-stability training on gait improvement in patients after anterior cruciate ligament reconstruction. Int J Clin Exp Med 12(5):5731–5737.
Logerstedt D. S., Snyder-Mackler L., Ritter R. C., Axe M. J.Orthopaedic Section of the American Physical Therapist Association (2010). Knee stability and movement coordination impairments: knee ligament sprain. J. Orthop. sports Phys. Ther. 40 (4), A1–a37. doi:10.2519/jospt.2010.0303
Moezy A., Olyaei G., Hadian M., Razi M., Faghihzadeh S. (2008). A comparative study of whole body vibration training and conventional training on knee proprioception and postural stability after anterior cruciate ligament reconstruction. Br. J. sports Med. 42 (5), 373–378. doi:10.1136/bjsm.2007.038554
Moher D., Liberati A., Tetzlaff J., Altman D. G.PRISMA Group (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. open-access J. 3 (3), e123–e130. doi:10.7326/0003-4819-151-4-200908180-00135
Owen P. J., Miller C. T., Mundell N. L., Verswijveren S., Tagliaferri S. D., Brisby H., et al. (2020). Which specific modes of exercise training are most effective for treating low back pain? Network meta-analysis. Br. J. sports Med. 54 (21), 1279–1287. doi:10.1136/bjsports-2019-100886
Papageorgiou C. D., Kostopoulos V. K., Moebius U. G., Petropoulou K. A., Georgoulis A. D., Soucacos P. N. (2001). Patellar fractures associated with medial-third bone-patellar tendon-bone autograft ACL reconstruction. Knee Surg. sports traumatology, Arthrosc. official J. ESSKA 9 (3), 151–154. doi:10.1007/s001670100207
Pearson S. J., Hussain S. R. (2015). A review on the mechanisms of blood-flow restriction resistance training-induced muscle hypertrophy. Sports Med. Auckl. NZ 45 (2), 187–200. doi:10.1007/s40279-014-0264-9
Pistone E. M., Laudani L., Camillieri G., Di Cagno A., Tomassi G., Macaluso A., et al. (2016). Effects of early whole-body vibration treatment on knee neuromuscular function and postural control after anterior cruciate ligament reconstruction: a randomized controlled trial. J. rehabilitation Med. 48 (10), 880–886. doi:10.2340/16501977-2150
Poretti K., Ghoddosi N., Martin J., Eddo O., Cortes N., Clark N. C. (2023). The nature of rehabilitation programs to improve musculoskeletal, biomechanical, functional, and patient-reported outcomes in athletes with ACL reconstruction: a scoping review. Sports health, 19417381231158327.
Priyanka P., Nilima B., Parag S., Ashok S. (2017). Effects of lumbar core stability exercise programme on knee pain, range of motion, and function post anterior cruciate ligament reconstruction. Jou. of Ortho. Trau. and Reha. 23(1):39–44. doi:10.1016/j.jotr.2016.10.003
Şahin N., Bianco A., Patti A., Paoli A., Palma A., Gjjopts E. (2015). Evaluation of knee joint proprioception and balance of young female volleyball players: a pilot study. J. Phys. Ther. Sci. 27 (2), 437–440. doi:10.1589/jpts.27.437
Samuelsson K., Andersson D., Karlsson J. (2009). Treatment of anterior cruciate ligament injuries with special reference to graft type and surgical technique: an assessment of randomized controlled trials. Arthrosc. J. Arthrosc. and Relat. Surg. official Publ. Arthrosc. Assoc. N. Am. Int. Arthrosc. Assoc. 25 (10), 1139–1174. doi:10.1016/j.arthro.2009.07.021
Shantakumari N., Ahmed M. (2023). Whole body vibration therapy and cognitive functions: a systematic review. AIMS Neurosci. 10 (2), 130–143. doi:10.3934/Neuroscience.2023010
Shaw T., Williams M. T., Chipchase L. S. (2005). Do early quadriceps exercises affect the outcome of ACL reconstruction? A randomised controlled trial. Aust. J. Physiother. 51 (1), 9–17. doi:10.1016/s0004-9514(05)70048-9
Suter E., Herzog W. (2000). Does muscle inhibition after knee injury increase the risk of osteoarthritis? Exercise and sport sciences reviews. Exerc. Sport Sci. Rev. 28 (1), 15–18.
van Melick N., van Cingel R. E., Brooijmans F., Neeter C., van Tienen T., Hullegie W., et al. (2016). Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br. J. sports Med. 50 (24), 1506–1515. doi:10.1136/bjsports-2015-095898
Vieira de Melo R. F., Komatsu W. R., Freitas M. S., Vieira de Melo M. E., Cohen M. (2022). Comparison of quadriceps and hamstring muscle strength after exercises with and without blood flow restriction following anterior cruciate ligament surgery: a randomized controlled trial. J. rehabilitation Med. 54, jrm00337. doi:10.2340/jrm.v54.2550
Wang K., Cheng L., Wang B., He B. (2023). Effect of isokinetic muscle strength training on knee muscle strength, proprioception, and balance ability in athletes with anterior cruciate ligament reconstruction: a randomised control trial. Front. physiology 14, 1237497. doi:10.3389/fphys.2023.1237497
Wengle L., Migliorini F., Leroux T., Chahal J., Theodoropoulos J., Betsch M. (2022). The effects of blood flow restriction in patients undergoing knee surgery: a systematic review and meta-analysis. Am. J. sports Med. 50 (10), 2824–2833. doi:10.1177/03635465211027296
Keywords: exercise therapy, anterior cruciate ligament reconstruction, anterior cruciate ligament injuries, kinesiotherapy, anterior cruciate ligament
Citation: Zhou H, Qian J, Xing Y-M, Cui L and Bu Y-F (2025) How effective is the addition of specific exercise therapy for patients after anterior cruciate ligament surgery? A systematic review and meta-analysis. Front. Physiol. 16:1501458. doi: 10.3389/fphys.2025.1501458
Received: 25 September 2024; Accepted: 06 January 2025;
Published: 24 January 2025.
Edited by:
Antonino Patti, University of Palermo, ItalyReviewed by:
Javier Sanchez-Sanchez, Pontifical University of Salamanca, SpainMarco Gervasi, University of Urbino Carlo Bo, Italy
Copyright © 2025 Zhou, Qian, Xing, Cui and Bu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yi-Feng Bu, YnV5aWZlbmdAanNudS5lZHUuY24=
†ORCID: Yi-Feng Bu, orcid.org/0009-0007-1786-2183
 Hao Zhou1
Hao Zhou1 Long Cui
Long Cui Yi-Feng Bu
Yi-Feng Bu