- 1Athletic Training Institute, Tianjin University of Sport, Tianjin, China
- 2School of Athletic Performance, Shanghai University of Sport, Shanghai, China
- 3School of Human Sciences (Exercise and Sport Science), The University of Western Australia, Perth, Australia
Objective: This meta-analysis aims to evaluate the effects of blood flow restriction (BFR) training on cardiometabolic health and body composition in adults with overweight and obesity.
Method: Following PRISMA guidelines, a systematic search of PubMed (MEDLINE), EMBASE, Web of Science, Cochrane, and Scopus databases was conducted on 15 March 2024. Pooled effects for each outcome were summarized using Hedge’s g (g) through meta-analysis-based random effects models, and subgroup analyses were used to explore moderators.
Results: A total of 11 studies with 242 participants (Age:32.6 ± 3.6, BMI:27.2 ± 3.5) were included. Regarding cardiometabolic health, BFR training significantly reduced systolic blood pressure (g = 0.62 [0.08, 1.16], p = 0.02), while no significant differences were observed in maximal oxygen uptake (g = 0.48 [-0.21, 1.17], p = 0.17) or diastolic blood pressure (g = 0.31 [-0.22, 0.84], p = 0.25). Regarding body composition, BFR training significantly reduced body fat percentage (g = 0.30 [0.01, 0.58]; p = 0.04), while no significant differences (p > 0.05) were observed in body weight (g = 0.14 [-0.14, 0.42]), body mass index (g = 0.08 [-0.21, 0.38]), waist circumference (g = 0.13 [-0.28, 0.53]), or waist-to-hip ratio (g = 0.48 [-0.19, 1.15]). Subgroup analysis revealed no significant difference in improving systolic blood pressure (g = 0.57 [-0.10, 1.24] vs. g = 0.70 [-0.18, 1.59]) and body fat percentage (g = 0.20 [-0.20, 0.61] vs. g = 0.45 [-0.05, 0.95]) between BFR resistance training and BFR aerobic training. In all selected studies, the overall risk of bias was categorized as “some concern”. The certainty of evidence for the BFR outcomes was low.
Conclusion: BFR training shows promise in improving cardiometabolic health and body composition, indicating that it may serve as a beneficial, individualized exercise prescription for improving cardiovascular disease risk and fat loss in adults with excess body weight and obesity.
Systematic Review Registration:: https://archive.org/details/osf-registrations-uv6jx-v1.
Introduction
Global obesity rates have surged in recent years, doubling in over 70 countries since 1980, and are projected to reach 57.8% by 2030 (GBD, 2015 Obesity Collaborators et al., 2017). Overweight and obesity are defined by an increased body mass index (BMI), calculated as weight (kg) divided by height (m)^ 2 (Nuttall, 2015; Keys et al., 2014). High BMI is strongly associated with various chronic diseases, including cardiovascular disease, diabetes, chronic kidney disease, and musculoskeletal disorders (GBD, 2015 Obesity Collaborators et al., 2017). This contributes to a decreased quality of life and elevated health risks, posing a major global public health challenge that demands urgent attention (Haslam and James, 2005). According to a recently published expert consensus on global fitness trends for 2025, exercise-induced weight loss remains a top priority, ranking as the fourth largest trend. While regular physical activity provides health benefits regardless of weight status, it is essential to incorporate exercise into a long-term, multifaceted approach for effective weight management and maintenance (Newsome et al., 2024).
Numerous studies have shown that exercise can significantly reduce BMI and lower cardiovascular disease risk in adults with overweight and obesity (Wu et al., 2009; Johns et al., 2014; Oppert et al., 2021). For example, high-intensity interval training is a time-efficient strategy that can induce physiological and psychological adaptations related to improved cardiometabolic health in adults with overweight and obesity (Batrakoulis et al., 2021; Poon et al., 2024; Yin et al., 2024a; Yin et al., 2023). Combining resistance training with aerobic or endurance training not only significantly improves cardiometabolic health in this population but also enhances fat loss (Garber et al., 2011; Oppert et al., 2023). Among them, combined aerobic exercise and diet play a key role in various aspects of cardiometabolic health, including blood pressure, lipid homeostasis, glucose homeostasis, adipose tissue dysfunction, and chronic inflammation in adults with obesity (Al-Mhanna et al., 2023). In addition, aerobic training and high-intensity interval training can reduce body weight (BW), body fat percentage (BF%), and abdominal visceral fat, while resistance training helps preserve fat-free mass (FFM) (Alberga et al., 2011). The latest meta-analysis shows that combined training is the most effective approach for improving cardiometabolic health outcomes in these populations (Batrakoulis et al., 2022).
From a practical perspective, adults with overweight and obesity may be at increased risk of sports injuries due to prolonged physical inactivity, participation in intense activities (e.g., high-intensity interval training), or unfamiliar forms of exercise (e.g., resistance training) (Kim and Yoon, 2021). Therefore, this population must adopt appropriate and progressive training methods to ensure both safety and effectiveness. Blood flow restriction (BFR) training, which involves applying external pressure to the proximal part of the upper or lower limb using a cuff or inflatable device during exercise (Lorenz et al., 2021), offers a potential solution. The term BFR training used in the following text refers to blood flow restriction combined with both aerobic and resistance training. Research suggests that BFR combined with low-intensity resistance or aerobic exercise can mimic the effects of high-intensity exercise, providing comparable benefits in cardiometabolic health and body composition (Bradley et al., 2023; Patterson et al., 2019). For example, BFR combined with resistance training or aerobic training can significantly improve muscle mass and maximal oxygen uptake (V̇O2max) (Kim et al., 2021; Yin et al., 2025). In addition, BFR combined with low-load resistance training is more effective at increasing muscle mass than low-load resistance training alone (Hughes et al., 2017).
While BFR combined with low-intensity resistance or aerobic exercise has proven benefits for improving cardiometabolic health and body composition in rehabilitation and healthy populations, its effects on adults with overweight and obesity remain less clear. A meta-analysis showed that BFR training effectively reduced BMI (mean difference [MD] = -0.77, p = 0.02) in these individuals, without distinguishing between exercise modes (Sun, 2022). But no significant changes were observed in body weight (MD = −1.32, p = 0.15), waist circumference (MD = −0.73, p = 0.19), and body fat percentage (MD = −0.66, p = 0.10), as these results did not reach statistical significance. However, with only four studies included, the meta-analysis may have lacked sufficient statistical power, potentially affecting the accuracy of the findings. In addition, the analysis was influenced by a few heavily weighted studies (e.g., body fat percentage at 84.9%, BMI at 62.4%), which may have introduced bias into the pooled results.
Currently, no systematic review or meta-analysis has specifically examined the effects of BFR training on cardiometabolic health in adults with overweight and obesity. Furthermore, studies comparing the differential effect of resistance or aerobic exercise with BFR on cardiometabolic health remain lacking. This research gap limits a comprehensive understanding of the health-promoting effects of BFR training in these populations. Evidence shows that, compared to aerobic exercise without BFR, aerobic exercise with BFR significantly increases V̇O2max by 12.6% (Adalberto, 2019) and reduces systolic blood pressure (SBP) by 2.8% (Ferreira Junior et al., 2019). In contrast, while resistance exercise with BFR demonstrates an effect in lowering SBP (Su et al., 2024), some studies report no significant improvement in cardiometabolic health (Bradley et al., 2023; Libardi et al., 2015a). These findings suggest that aerobic exercise with BFR may provide greater benefits for cardiometabolic health than resistance exercise with BFR. However, due to the limited number of studies and inconsistent results, a meta-analysis is urgently needed to systematically review and synthesize the current evidence, clarifying the specific effects and relative advantages of resistance exercise with BFR and aerobic exercise with BFR on cardiometabolic health in adults with overweight and obesity.
Therefore, the present meta-analysis focuses on the effects of BFR training on cardiometabolic health and body composition in adults with overweight and obesity, and examines how training protocol parameters may influence these outcomes.
Methods
This review follows the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines (Page et al., 2021), and is registered in the Open Science Framework (https://doi.org/10.17605/OSF.IO/UV6JX).
Literature search
Literature searches were performed in PubMed, Scopus, Embase, Web of Science and Cochrane. Keywords were drawn from controlled vocabularies (e.g., Medical Subject heading: MeSH). Search terms included: (“Blood flow restriction” or “Blood flow occlusion” or “Kaatsu” or “Vascular occlusion” or “Restricted blood flow” or “Occlusion training” or “Occluded training”)and (“BMI” or “waist circumference” or “hip circumference or” waist to “hip ratio” or “resting heart rate” or “%body fat” or “lean body mass” or “fat mass” or “Muscle mass” or “body weight” or “free fat mass”) and (“blood pressure” or “V̇O2max” or “fitness” or “cardiorespiratory fitness” or “V̇O2peak”) and (“Human” (MeSH)). Publications were searched from the inception of each database until 15 March 2024. A reference list of articles that met the inclusion and exclusion criteria is also provided. Two authors (KH and ZYL) conducted the initial search to remove duplicates and screened the papers according to the inclusion criteria. Any disagreements were resolved through discussion with a third author (SQG).
Eligibility criteria
The PICOS (Participants, Interventions, Comparators, Outcomes, and Study Design) framework was applied to assess the eligibility of the studies. Peer-reviewed articles were excluded if they involved non-human experiments or recruited unhealthy participants. The specific inclusion and exclusion criteria are listed below:
Population
The study recruited healthy adults with overweight (BMI: 25.0–29.9) or obesity (BMI: ≥30), people aged 18 or older, regardless of sex or country. Athletes or trained adults were excluded.
Intervention
BFR is a technique that restricts blood flow to the muscles, typically by applying light pressure using specialized bands or cuffs on the upper or lower limbs. We included both resistance training and aerobic exercise because our primary focus is on the broad application of blood flow restriction training for cardiometabolic health in adults with overweight and obesity. Therefore, we did not limit ourselves to a specific type of exercise but aimed to explore the broader effects of blood flow restriction. We will address this potential confusion through subgroup analyses. Resistance training is defined as exercises involving external resistance (e.g., squats (Kim et al., 2021; Su et al., 2024), elbow flexion (Su et al., 2024; Libardi et al., 2015b; Farzaneh Hesari et al., 2018; da Silva et al., 2020), knee extension (Kim et al., 2021; Farzaneh Hesari et al., 2018; da Silva et al., 2020), bench press (Kim et al., 2021),deadlift (Bradley et al., 2023)). Aerobic exercise is defined as low-intensity, sustained activities (e.g., walking (Adalberto, 2019), cycling (Chen et al., 2022), rowing (Bradley et al., 2023)). During aerobic or resistance training, participants used commercially available BFR devices. Studies needed to provide sufficient data to calculate effect sizes and assess the chronic effects.
Comparison
The intervention group added BFR to aerobic training, resistance training, or a combination of both, while the control group did not. The primary difference between the intervention and control groups throughout the study was the use of BFR. Baseline demographic characteristics between the groups were not different to ensure an accurate assessment of the intervention’s effects.
Outcomes
The study evaluated the effect of BFR training on at least one of the following outcome measures, comparing post-intervention results to baseline/pre-training values: 1) V̇O2max: assessed using gas-exchange data and heart rate during progressive exercise tests including treadmill (Adalberto, 2019; Libardi et al., 2015b), stationary rowing machine (Bradley et al., 2023), or gradient cycling (Li et al., 2022). 2) Heart rate: measured using a Polar chest strap. 3) Blood pressure: SBP and Diastolic Blood Pressure (DBP) were measured at rest and before and after exercise with automated electronic sphygmomanometer or mercury sphygmomanometers. 4) Body composition: BW, BMI, FFM, Fat Mass (FM), BF%, and MM were measured using body composition analyzers (DX-200, Inbody 720, and Maltron BF-906), dual-energy X-ray absorptiometry (DEXA), and Waist Circumference (WC) was measured with inelastic measuring tape for Waist-to-Hip Ratio (WHR) calculation.
Study design
The analysis included randomized controlled trials with clear descriptions of the intervention and outcome measures.
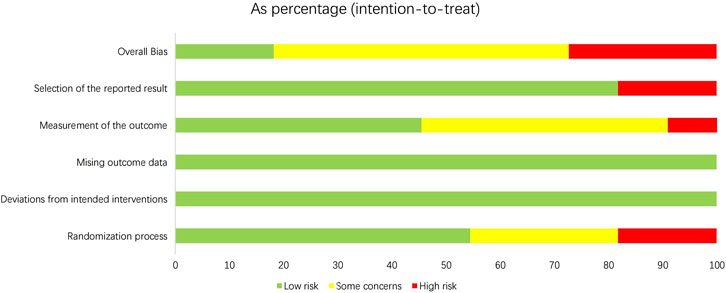
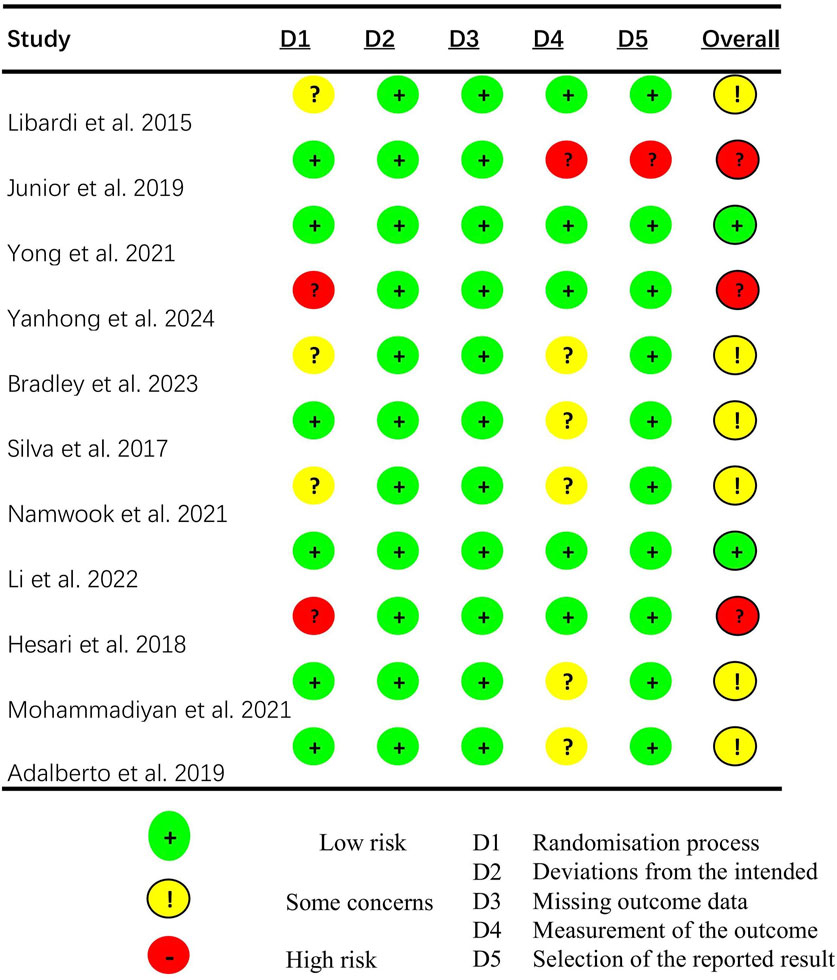
Risk of bias assessment
The Cochrane Risk of Bias 2 (RoB) tool was used to assess studies that met the inclusion criteria. It assesses five potential sources of bias: 1. randomization process; 2. deviations from the intended intervention (including distributional effects and adherence); 3. missing outcome indicators; 4. outcome measures; and 5. selection of reported outcomes. Each domain was rated as “yes”, “probably yes”, “probably no”, or “no”. According to the Cochrane guidelines (the “Cochrane Handbook for Systematic Reviews of Interventions”), the overall risk of bias is categorized as “high” (if at least one domain indicates high risk), “some concern” (if at least one domain indicates concern but no high risk), and “low” (if all domains show low risk).
Data extraction and conversion
We extracted mean, standard deviation, and sample size data for each group before and after the intervention. The effects were summarized as differences between pre- and post-intervention outcomes. Mean differences were calculated by subtracting pre-intervention means from post-intervention means for each group. For studies reporting standard errors (SEM), these were converted to standard deviation (SD) using the formula SD = SEM
The SD of the difference in means was then calculated as follows:
where SDdiff is the standard deviation of the pre- and post-intervention differences, SDpre and SDpost are the standard deviations for pre- and post-intervention measures, respectively, and r is the correlation coefficient between pre- and post-intervention measurements.
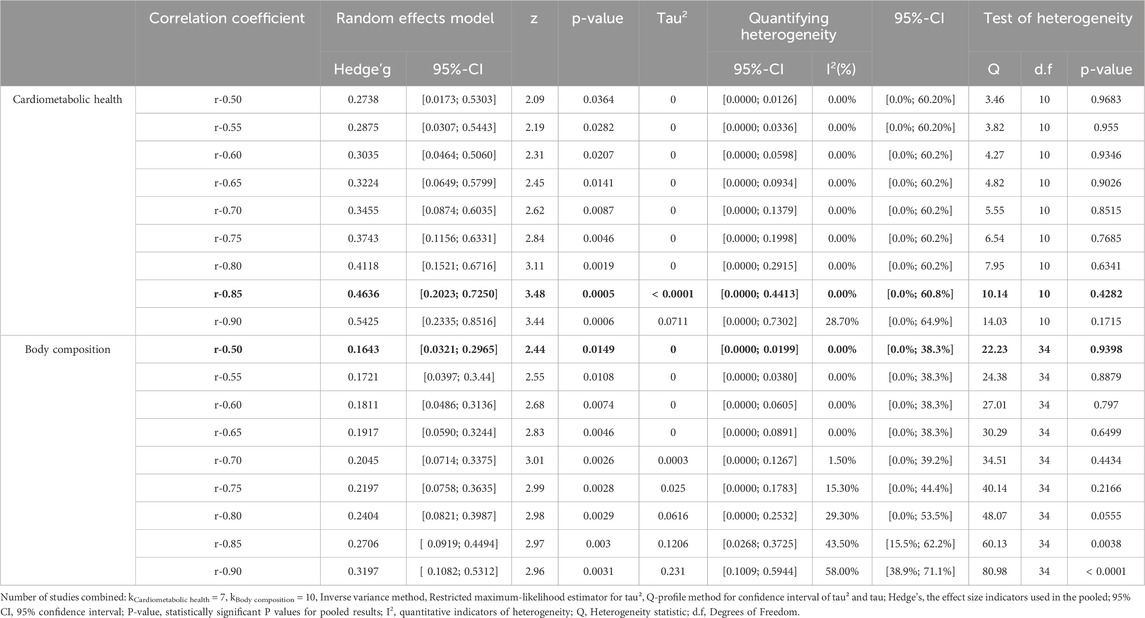
As the original studies did not report Pearson’s correlation coefficients (r) for pre- and post-intervention outcomes, we referred to meta-analyses with similar results and chose r = 0.5 for body composition indicators and r = 0.6 for cardiometabolic indicators for sensitivity analyses (Table 1).
Statistical analysis
Statistical analyses were performed using the ‘meta’ and ‘metafor’ packages of the R statistical software (Version.4.3.3). Meta-analyses utilized the general inverse variance merging method, with effect sizes combined using the random effects model of the DerSimonia-Laird method to summarise the effects of BFR combined with resistance or aerobic training on body composition and cardiometabolic fitness compared to controls (DerSimonian and Laird, 1986). Effects were expressed as Standardized Mean Difference (SMD) and estimated Hedge’g, categorised as negligible (0.2), small (0.2–0.5), medium (0.5–0.8), and large (>0.8). Statistical significance was set at p < 0.05. Heterogeneity was assessed using I2, with thresholds of 25%, 50%, 75%, and >75% indicating low, medium, high and very high thresholds, respectively. We calculated 95% confidence intervals (CI) and determined prediction intervals (PIs) using t-distribution to account for heterogeneity (Nagashima et al., 2018). Studies with CI that did not overlap with the combined effect CI were considered statistical outliers. The impact of individual studies was assessed through impact analyses using the leave-one-out method.
We conducted a separate meta-analysis to evaluate the effects of BFR training on cardiometabolic health and body composition in adults with overweight and obesity. Due to the limited number of studies, we subsequently performed subgroup analyses based on exercise modality to compare the effects of aerobic or resistance exercise combined with BFR on cardiometabolic health and body composition. Additionally, for body composition, considering that only one study involved sprint training, the subgroup analysis was restricted to aerobic exercise with BFR and resistance exercise with BFR.
Quality of evidence
The quality of scientific evidence was assessed using the GRADE manual recommendations (Schünemann et al., 2019). The GRADEpro GDT software was employed to rate the quality of evidence across four domains: high, moderate, low, and very low. The evaluation of BFR training interventions for improving body composition and cardiometabolic health considered the risk of bias, inconsistency of results, indirectness of evidence, imprecision of results, and publication bias. Initially, evidence was rated as having a high degree of certainty but was downgraded according to the following criteria: (GBD, 2015 Obesity Collaborators et al., 2017): Risk of bias: downgraded one level for some concerns and two levels for high risk; (Nuttall, 2015); Indirectness: downgraded one level for indirectness (e.g., inconsistent populations, interventions, comparators, and outcomes) and two levels if the indirectness was widespread; (Keys et al., 2014); Publication bias: downgraded one level if publication bias was suspected, as indicated by Egger’s test; (Haslam and James, 2005); Inconsistency: downgraded one level for high inter-study heterogeneity (I2 > 50%) or poor overlap of confidence intervals; (Newsome et al., 2024); Imprecision: downgraded one level for sample sizes of <800 or non-significant results, and two levels if both criteria for imprecision applied.
Results
Study selection
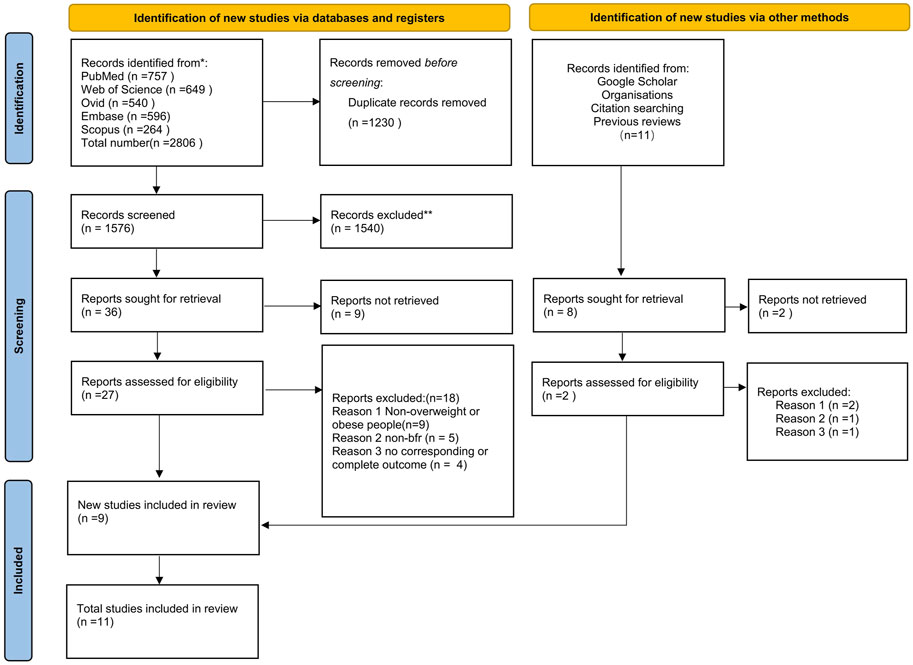
An initial database search identified 2806 publications. After screening, 11 papers were deemed eligible for inclusion in the meta-analysis (Figure 1).
Study characteristics
The studies included in this systematic review spanned the period 2015–2024. A total of 242 adults with overweight and obesity were assessed, including 97 males and 74 females, with 71 subjects having unspecified gender (Age: 32.6 ± 3.6; BMI: 27.2 ± 3.5). Detailed descriptions of participant characteristics, BFR cuff position and pressure, and interventions are provided in Tables 2, 3.
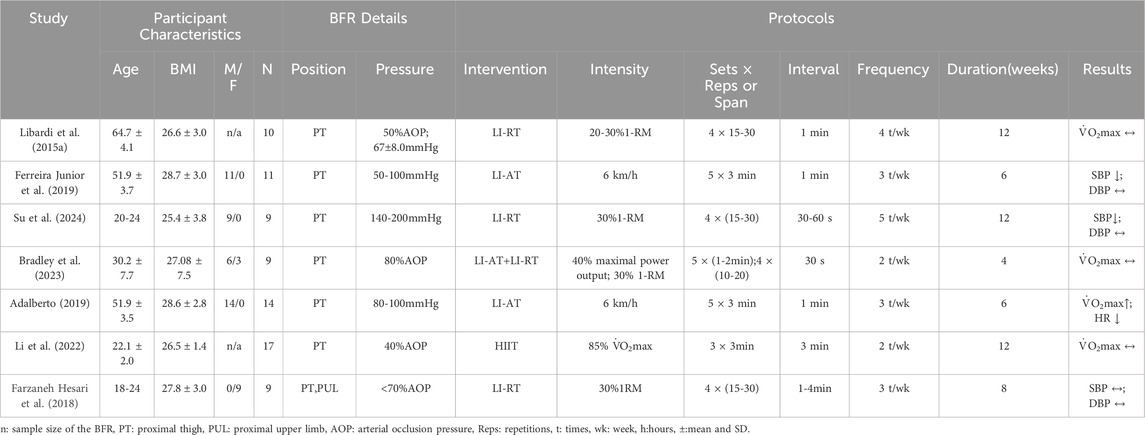
Table 2. Characteristics of studies on blood flow restriction training for cardiometabolic health in adults with overweight and obesity.
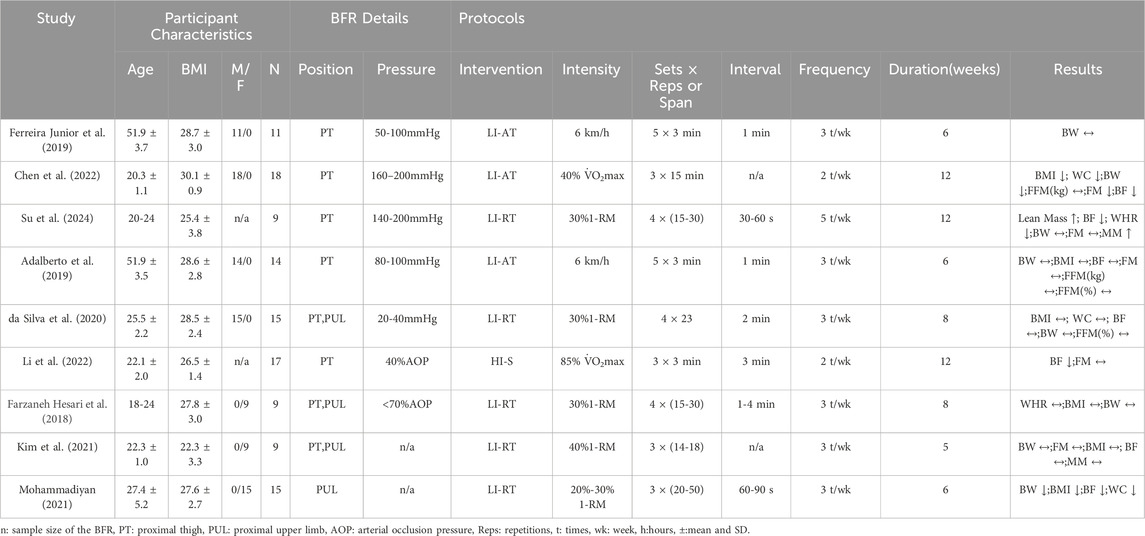
Table 3. Characteristics of studied on blood flow restriction training for body composition in adults with overweight and obesity.
Risk of bias
In all selected studies, the overall risk of bias was categorized as “some concern”. According to the Rob two tool, a reduced risk of bias was noted concerning missing outcome data, while the selection and randomization processes for reporting outcomes were areas of increased risk in most studies (Figures 2, 3).
Effects of BFR training vs. control
Nine studies assessed the effects of BFR training (Three studies on aerobic exercise, five studies on resistance exercise, and one study on sprinting). on body composition compared to controls, and seven studies assessed its effects on cardiometabolic health (Two studies on aerobic exercise, three studies on resistance exercise, one study on combined aerobic and resistance exercise, and one study on sprinting). All participants were overweight and obesity.
Cardiometabolic health
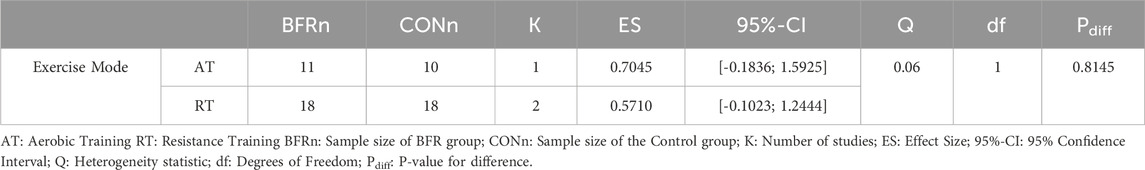
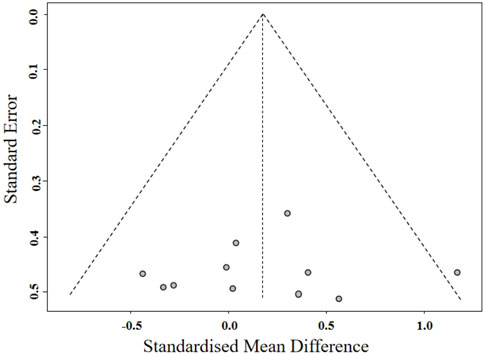
A meta-analysis of studies on cardiometabolic health indicators is shown in Figure 4. The results indicated that BFR training significantly improved SBP (g = 0.62 [0.08, 1.16], p = 0.02). Subgroup analysis revealed no significant difference in improving systolic blood pressure (g = 0.57 [-0.10, 1.24] vs. g = 0.70 [-0.18, 1.59]) between BFR resistance training and BFR aerobic training (Table 4). The meta-analysis found no statistically significant effect of BFR training on DBP (g = 0.31 [-0.22, 0.84], p = 0.25), V̇O2max (g = 0.48 [-0.21, 1.17], p = 0.17). In addition, Egger’s test showed no significant risk of publication bias (p = 0.865; Figure 5).
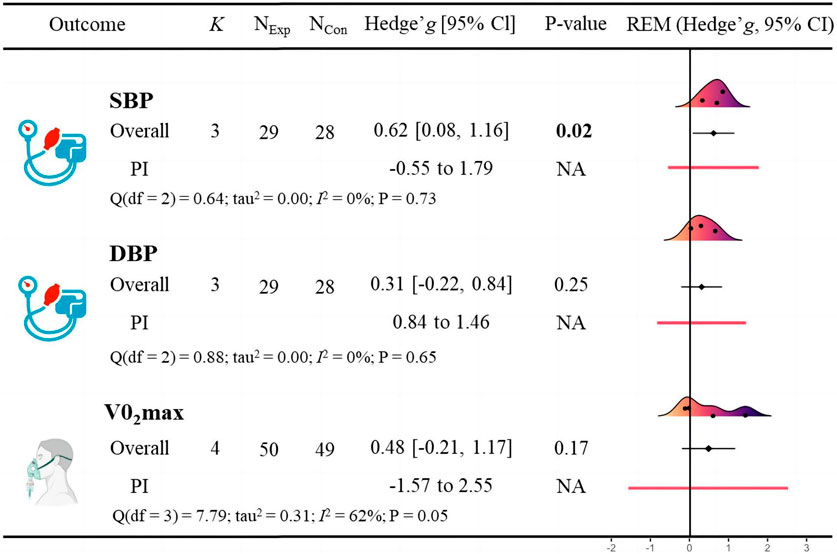
Figure 4. Effects of blood flow restriction training on cardiometabolic health in adults with overweight and obesity.
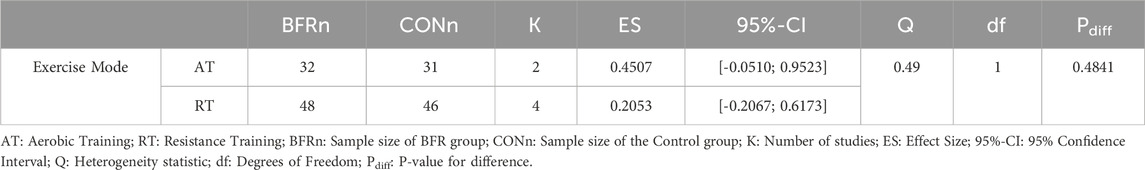
Body composition
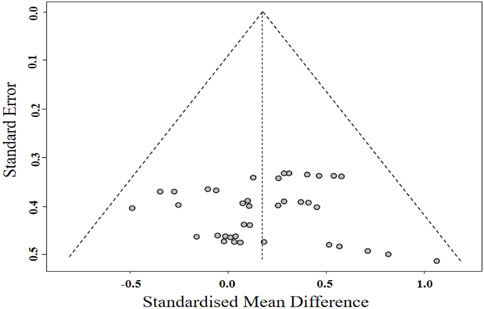
A meta-analysis of studies on body composition indicators is displayed in Figure 6. The meta-analysis revealed that BFR training had a significant positive effect on BF (g = 0.30 [0.01, 0.58], p = 0.04). Subgroup analysis revealed no significant difference in improving body fat percentage (g = 0.20 [-0.20, 0.61] vs. g = 0.45 [-0.05, 0.95]) between BFR resistance training and BFR aerobic training (Table 5). The meta-analysis found no statistically significant effect of BFR training on BMI (g = 0.08 [-0.21, 0.38], p = 0.58), BW (g = 0.14 [-0.14, 0.42], p = 0.34), FFM (g = -0.26 [-0.79, 0.27]. p = 0.17), WC (g = 0.13 [-0.28, 0.53], p = 0.54), and WHR (g = 0.48 [-0.19, 1.15], p = 0.16). Additionally, Egger’s test showed no significant risk of publication bias (p = 0.857; Figure 7).
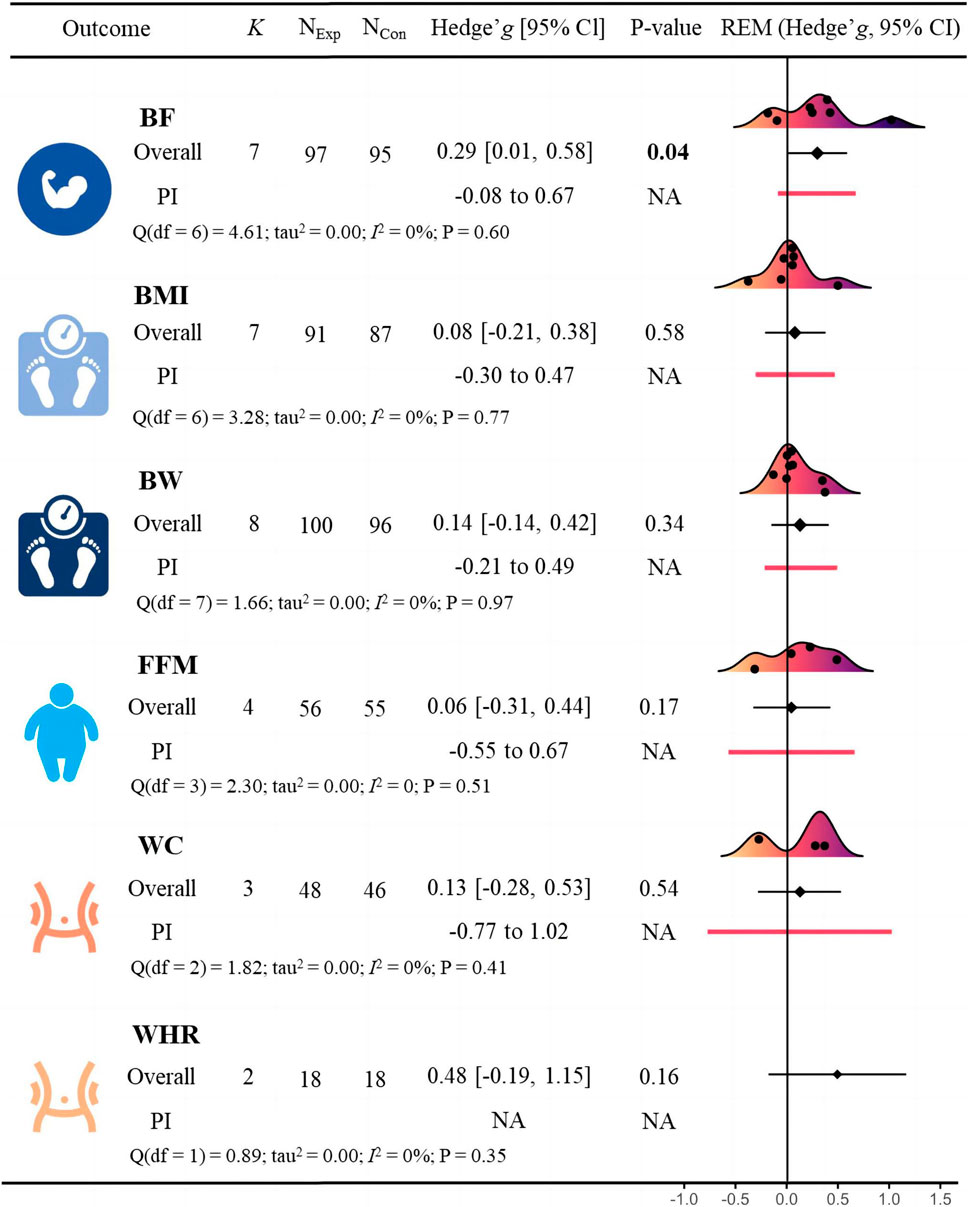
Figure 6. Effects of blood flow restriction training on body composition in adults with overweight and obesity.
Certainty of evidence
The certainty of evidence for the BFR outcomes was low, based primarily on limited sample size for comparison and Risk of study bias is “some concerns”.
Discussion
To our knowledge, this is the first systematic review and meta-analysis to assess the effects of BFR training on cardiometabolic health and body composition in adults with overweight and obesity. Our main findings indicate BFR training improved SBP and body fat percentage, while showing limited potential on V̇O2max, diastolic blood pressure, body weight, BMI, waist circumference, fat-free mass, waist-to-hip ratio, or muscle mass. Additionally, the effects of aerobic exercise with BFR on cardiometabolic health and body composition were not different compared to those with resistance exercises with BFR.
Effect of BFR training on cardiometabolic health
Our meta-analysis found that low-intensity BFR training significantly reduced SBP in adults with overweight and obesity (g = 0.62 [0.08, 1.16]). Further subgroup analysis revealed no significant difference in improving systolic blood pressure (g = 0.57 [-0.10, 1.24] vs. g = 0.70 [-0.18, 1.59]) between BFR resistance training and BFR aerobic training; however, this difference was not statistically significant. Interestingly, recent research has shown that resistance training results in a greater improvement in SBP (10.2%) compared to aerobic training (1.9%) in adults with overweight and obesity (Batrakoulis et al., 2022). Additionally, other studies have found that resistance training significantly improved diastolic blood pressure (SMD = −0.33) in individuals with obesity, but no significant difference was observed in systolic blood pressure (SMD = −0.04) (AL-Mhanna et al., 2024). This difference may reflect the distinct physiological mechanisms underlying the different training modalities. It is also important to note that the effect of BFR combined with aerobic exercise on SBP was evaluated in only one study, which may limit the statistical power and robustness of this finding.
High SBP is a major modifiable risk factor for cardiovascular disease (Lewington and Qizilbash, 2002) and is associated with increased incidence and mortality from cardiovascular conditions (Rutan et al., 1988; Stamler et al., 1993; Sesso et al., 2000). In addition, BMI is nearly linearly related to both SBP and DBP across different populations (Hall, 2003), suggesting a high prevalence of hypertension among adults with overweight and obesity. While not all adults with overweight and obesity suffer from hypertension, weight gain shifts blood pressure distribution to higher levels, increasing the risk of developing hypertension (Hall et al., 2015).
Exercise is known to effectively lowers blood pressure (AL-Mhanna et al., 2024; Arroll and Beaglehole, 1992; Fagard, 1993). Our meta-analysis suggests that BFR combined with low-intensity resistance or aerobic exercise may enhance this antihypertensive effect by providing additional stimuli to the body. Specifically, BFR training increases venous pressure, which can alter venous compliance, vessel wall tone, and endothelial function (Stamler et al., 1993). These changes lead to increased blood flow and shear stress, triggering positive vascular adaptations such as increased levels of vascular endothelial growth factor and endothelial-type nitric oxide synthase, thereby increasing nitric oxide production. The increase in nitric oxide helps dilate blood vessels, thereby lowering blood pressure (Rutan et al., 1988). Although BFR training can cause temporary increases in heart rate and blood pressure during training, long-term BFR training has been shown to more effectively lowers SBP compared to equivalent intensity exercise without external limb compression (Hackney et al., 2012). The significant reduction in SBP observed in our study suggests that BFR training provides an effective, lower-intensity exercise option for adults with overweight and obesity, potentially reducing the exercise burden while improving cardiovascular health. Therefore, BFR training may represent a valuable strategy for preventing hypertension in these populations.
Moreover, existing research has shown that even a modest decrease in systolic blood pressure of 2–3 mmHg is sufficient to significantly reduce the occurrence of cardiovascular events (Elliott, 1991), and a reduction of 4 mmHg or more is expected to lead to a 5%–20% decrease in cardiovascular disease mortality (Adler et al., 2014). Therefore, the findings of our study (a reduction in systolic blood pressure of 3.38–9.28 mmHg) have important clinical significance, demonstrating the potential of BFR training as an effective low-intensity exercise option for adults with overweight and obesity, which not only reduces the exercise burden but also significantly improves cardiovascular health.
However, despite the significant effects of BFR training on blood pressure regulation, its safety remains a topic of debate. A narrative review by Spranger et al. suggests that excessive vascular occlusion induced by the cuff during BFR training may lead to overactivation of muscle reflexes (e.g., activation of type IV and III afferent fibers), which in turn may trigger excessive sympathetic nervous system activity, resulting in increased cardiac function, blood pressure, and vascular resistance (Spranger et al., 2015). Therefore, based on the existing literature, it is recommended that healthcare providers set the restriction pressure during BFR training at 40%–60% of each participant’s arterial occlusion pressure to ensure that no participant experiences unnecessary health risks due to excessively high pressure (Mouser et al., 2017).
The meta-analysis showed no statistically significant effect of BFR training on V̇O2max (g = 0.48 [-0.21, 1.17]). V̇O2max, a skey indicator of cardiorespiratory fitness, typically requires longer periods of moderate-to high-intensity aerobic exercise to show improvement (Swain and Franklin, 2006; Blair et al., 2001; Wenger and Bell, 1986). Engaging in sufficient and regular aerobic or resistance exercise can also reduce the risk of cardiovascular disease and high BMI, as well as improve insulin resistance (Badri Al-mhanna et al., 2024). The low intensity and short duration of BFR training may be insufficient to induce significant cardiorespiratory adaptations. However, the lack of significant effect on V̇O2max does not diminish the clinical value of BFR training. It remains a safe and potentially beneficial option for adults with overweight and obesity who may not be suited for high-intensity training.
While BFR training significantly improved SBP, its effect on V̇O2max remains unclear. Future research should focus on optimizing Aerobic or resistance exercises with BFR protocols and explore the potential of combining different exercise modalities with blood flow restriction for improving cardiometabolic health and body composition in adults with overweight and obesity. Increasing the intensity and duration of BFR training interventions may help determine their impact on V̇O2max and further enhance the application of BFR training for adults with overweight and obesity.
Effects of BFR training on body composition
We found that BFR training significantly reduced BF% (g = 0.30 [0.01, 0.58]) in adults with overweight and obesity compared to controls. Further Subgroup analysis revealed no significant difference in improving body fat percentage (g = 0.20 [-0.20, 0.61] vs. g = 0.45 [-0.05, 0.95]) between BFR resistance training and BFR aerobic training. In addition, it did not significantly affect body weight (g = 0.14 [-0.14, 0.42]), BMI (g = 0.08 [-0.21, 0.38]), waist circumference (g = 0.13 [-0.28, 0.53]), waist-to-hip ratio (g = 0.48 [-0.19, 1.15]), fat free mass (g = 0.06 [-0.31, 0.44]). This contrasts with a previous meta-analysis that reported no improvement in BF% with BFR training in adults with overweight and obesity (Sun, 2022). Although weight loss and the associated reduction in BMI are often primary goals in treating overweight or obesity, our findings indicate that BFR training or control (unrestricted) groups had limited effects on body weight. The mean weight loss ranged from −1.30–3.14 kg in both groups (Figure 8). A meta-analysis of adults with overweight and obesity suggests that achieving clinically meaningful weight loss requires at least 60 min of moderate-to vigorous-intensity aerobic exercise per day (Fogelholm and Kukkonen-Harjula, 2000). Therefore, low-intensity aerobic or resistance exercise alone is insufficient for significant weight loss. Effective weight management relies on maintaining a calorie balance, and combining exercise with dietary control is essential to maximize weight loss and manage obesity effectively (Romieu et al., 2017).
Our study found that both low-intensity resistance training combined with blood flow restriction and low-intensity aerobic training combined with blood flow restriction can effectively improve body fat percentage in adults with overweight and obesity, but did not significantly affect body weight. This could be due to exercise-induced muscle growth offsetting weight loss from fat loss, thereby improving overall body composition. Literature supports this, showing that both aerobic and resistance training effectively reduce body fat while maintaining fat-free body weight without significant weight loss (Willis et al., 2012; Ross et al., 2000; Stiegler and Cunliffe, 2006). In addition, body fat is often more responsive to exercise than body weight, making it a more relevant health indicator for evaluating exercise interventions (Millstein, 2014). For example, a recent meta-analysis reported a greater mean reduction in body fat (MD = −0.39) compared to body weight (MD = −0.30) from aerobic exercise (Kim et al., 2019). Therefore, Aerobic with BFR may be more effective for fat loss than traditional aerobic training, suggesting that low-intensity BFR training can achieve similar fat loss benefits as moderate-to high-intensity aerobic exercise. This highlights its value for managing obesity and improving health in adults with overweight and obesity.
This study demonstrates the potential of BFR training in improving abdominal fat, which is closely associated with cardiovascular health. Abdominal fat is an important indicator of mortality risk and a more effective predictor of obesity-related diseases than body weight or BMI (Moore et al., 2014). Measures of abdominal fat, such as waist circumference and waist-to-hip ratio, are strongly associated with cardiovascular disease risk (de Koning et al., 2007). Research has shown that each 1 cm increase in WC corresponds to a 2% rise in cardiovascular disease risk, while each 0.01 increase in WHR corresponds to a 5% increase in risk (de Koning et al., 2007). Our meta-analysis supports these findings, showing that BFR training significantly reduced waist circumference (g = 0.13 [-0.28, 0.53]) and waist-to-hip ratio (g = 0.48 [-0.19, 1.15]) in adults with overweight and obesity. The effects of BFR training on these measures were comparable to, and in some cases larger than, the effect observed without BFR training.
Practice application
BFR training improves systolic blood pressure and body fat percentage in adults with overweight or obesity. The low-intensity nature of BFR training allows individuals to enhance cardiovascular health and body composition without imposing excessive strain on the body. By activating muscles under lower loads, BFR training is particularly suitable for those with higher body weight, improving training outcomes while minimizing stress on joints and bones. This characteristic also reduces the risk of exercise-related injuries, which is especially important for individuals with limited physical activity who may struggle to adapt to high-intensity training. Several studies in our review suggest that BFR training can be easily incorporated into daily life through low-intensity activities such as walking, cycling, or bodyweight exercises, whether at home or in the workplace. This approach creates more opportunities for physical activity, helping to reduce sedentary behavior and enhancing the practicality and feasibility of BFR training. Combining BFR with “exercise snacks” (Islam et al., 2022; Yin et al., 2024b) at lower intensity performed multiple times daily may further promote cardiometabolic health (Yin et al., 2024c; Yin et al., 2024d) while mitigating the negative effects of sedentary behavior (Yin et al., 2024e; Pinto et al., 2023; Dunstan et al., 2021). However, achieving significant reductions in body weight and BMI likely requires longer durations of BFR training combined with dietary interventions, as exercise alone often has limited effects on weight loss (Swift et al., 2014). Nonetheless, the lack of significant reductions in body weight and BMI does not diminish the potential benefits of incorporating low-intensity BFR training into daily routines.
Limitations
This study is not without limitations. Firstly, the limited amount of literature available restricted our ability to conduct subgroup analyses. For example, among the studies assessing BF%, six recruited participants younger than 45 years (young adults aged 20–44 and middle-aged individuals aged 45–59) (Kim et al., 2021; Su et al., 2024; da Silva et al., 2020; Chen et al., 2022; Li et al., 2022; Mohammadiyan, 2021), while only one study had participants older than 45 (25). There was also a significant imbalance in the intensity of interventions, with 10 studies using low-intensity BFR training and only one using high-intensity interventions (Li et al., 2022). This uneven distribution hindered more detailed subgroup analyses. Secondly, the lack of standardization in cuff pressure (20–200 mmHg; 50%–80% AOP) and width (5–26 cm) across studies presents another limitation. Future studies should consider that optimal cuff pressure may vary depending on the specific health outcomes being targeted, such as different aspects of cardiometabolic health and body composition. For instance, improving certain indices may require higher pressures. Additionally, cuff pressure should be evaluated alongside exercise intensity, as both factors likely influence the overall efficacy of the intervention (Rossow et al., 2012; Spitz et al., 2019).
Conclusion
BFR training effectively improves systolic blood pressure and body fat percentage in adults with overweight and obesity, with no significant difference in the effects between aerobic and resistance exercises. Additionally, BFR training did not show significant effects on body weight, BMI, diastolic blood pressure, and V̇O2max. This suggests that BFR training can be an effective exercise option for improving cardiovascular health and preventing hypertension in adults with overweight and obesity. Its ability to reduce body fat while maintaining fat-free mass highlights its potential importance in the management of overweight and obesity.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
HK: Conceptualization, Software, Data curation, Validation, Visualization, Methodology, Supervision, Formal analysis, Visualization, Writing–original draft, Writing–review and editing. YZ: Conceptualization, Software, Validation, Visualization, Methodology, Supervision, Writing–original draft, Writing–review and editing. MY: Conceptualization, Data curation, Validation, Visualization, Writing–review and editing. KX: Methodology, Software, Data curation, Validation, Visualization, Writing–review and editing. QS: Supervision, Writing–review and editing. YX: Supervision, Writing–review and editing. OG: Conceptualization, Methodology, Validation, Supervision, Writing–review and editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Adalberto A. (2019). Effect of walk training with blood flow restriction on oxygen uptake kinetics, maximum oxygen uptake and muscle strength in middle-aged adults - medicina dello Sport 2019 December. Available at: https://www.minervamedica.it/en/journals/medicina-dello-sport/article.php?cod=R26Y2019N04A0616.
Adler A. J., Taylor F., Martin N., Gottlieb S., Taylor R. S., Ebrahim S. (2014). Reduced dietary salt for the prevention of cardiovascular disease. Cochrane Database Syst. Rev. 2014 (12), CD009217. doi:10.1002/14651858.CD009217.pub3
Alberga A. S., Sigal R. J., Kenny G. P. (2011). A review of resistance exercise training in obese adolescents. Physician Sportsmed. 39 (2), 50–63. doi:10.3810/psm.2011.05.1895
AL-Mhanna S. B., Batrakoulis A., Ghazali W. S. W., Mohamed M., Aldayel A., Alhussain M. H., et al. (2024). Effects of combined aerobic and resistance training on glycemic control, blood pressure, inflammation, cardiorespiratory fitness and quality of life in patients with type 2 diabetes and overweight/obesity: a systematic review and meta-analysis. PeerJ 12, e17525. doi:10.7717/peerj.17525
Al-Mhanna S. B., Rocha-Rodriguesc S., Mohamed M., Batrakoulis A., Aldhahi M. I., Afolabi H. A., et al. (2023). Effects of combined aerobic exercise and diet on cardiometabolic health in patients with obesity and type 2 diabetes: a systematic review and meta-analysis. BMC Sports Sci. Med. Rehabil. 15 (1), 165. doi:10.1186/s13102-023-00766-5
Arroll B., Beaglehole R. (1992). Does physical activity lower blood pressure: a critical review of the clinical trials. J. Clin. Epidemiol. 45 (5), 439–447. doi:10.1016/0895-4356(92)90093-3
Badri Al-mhanna S., Wan Ghazali W. S., Batrakoulis A., Alkhamees N. H., Drenowatz C., Mohamed M., et al. (2024). The impact of various types of exercise on lipid metabolism in patients with type 2 diabetes and concurrent overweight/obesity: a narrative review. Ann. Appl. Sport Sci. 12 (0), 0. doi:10.61186/aassjournal.1324
Batrakoulis A., Jamurtas A. Z., Fatouros I. G. (2021). High-intensity interval training in metabolic diseases: physiological adaptations. ACSM’s Health and Fit. J. 25 (5), 54–59. doi:10.1249/fit.0000000000000703
Batrakoulis A., Jamurtas M., Perivoliotis K., Liguori G., Feito Y., Riebe D., et al. (2022). Comparative efficacy of 5 exercise types on cardiometabolic health in overweight and obese adults: a systematic review and network meta-analysis of 81 randomized controlled trials. Circulation Cardiovasc. Qual. Outcomes 15 (6), e008243. doi:10.1161/CIRCOUTCOMES.121.008243
Blair S. N., Cheng Y., Holder J. S. (2001). Is physical activity or physical fitness more important in defining health benefits? Med. Sci. Sports Exerc 33 (6), S379–S399. doi:10.1097/00005768-200106001-00007
Bradley K. M., Bunn J. A., Feito Y., Myers B. J. (2023). Effects of blood flow restriction training on muscle size, power, and V̇O2max in active adults. Transl. J. Am. Coll. Sports Med. 8 (1), e000219. doi:10.1249/tjx.0000000000000219
Chen Y., Ma C., Wang J., Gu Y., Gao Y. (2022). Effects of 40% of maximum oxygen uptake intensity cycling combined with blood flow restriction training on body composition and serum biomarkers of Chinese college students with obesity. Int. J. Environ. Res. Public Health 19 (1), 168. doi:10.3390/ijerph19010168
da Silva I. M., Santos M. A., Galvão S. L., Dorneles G. P., Lira F. S., Romão P. R. T., et al. (2020). Blood flow restriction impairs the inflammatory adaptations of strength training in overweight men: a clinical randomized trial. Appl. Physiol. Nutr. Metab. 45 (6), 659–666. doi:10.1139/apnm-2019-0700
de Koning L., Merchant A. T., Pogue J., Anand S. S. (2007). Waist circumference and waist-to-hip ratio as predictors of cardiovascular events: meta-regression analysis of prospective studies. Eur. Heart J. 28 (7), 850–856. doi:10.1093/eurheartj/ehm026
DerSimonian R., Laird N. (1986). Meta-analysis in clinical trials. Control. Clin. Trials 7 (3), 177–188. doi:10.1016/0197-2456(86)90046-2
Dunstan D. W., Dogra S., Carter S. E., Owen N. (2021). Sit less and move more for cardiovascular health: emerging insights and opportunities. Nat. Rev. Cardiol. 18 (9), 637–648. doi:10.1038/s41569-021-00547-y
Elliott P. (1991). Sodium and blood pressure: a review of the evidence from controlled trials of sodium reduction and epidemiological studies. Klin. Wochenschr 69 (Suppl. 25), 3–10.
Fagard R. H. (1993). Physical fitness and blood pressure. J. Hypertens. 11, S47–S52. doi:10.1097/00004872-199312050-00008
Farzaneh Hesari A., Ebrahimi A., Azizi Zanjani M., Mahdavi S. (2018). Effects of resistance training with and without blood flow restriction on cardiovascular risk factors in overweight females. Med. Laboratory J. 12 (1), 31–36. doi:10.29252/mlj.12.1.31
Ferreira Junior A., Schamne J. C., Altimari L. R., Okano A. H., Okuno N. M. (2019). Effect of walk training combined with blood flow restriction on resting heart rate variability and resting blood pressure in middle-aged men. Mot. Rev. Educ. Fis. 25, e101945. doi:10.1590/s1980-6574201900020005
Fogelholm M., Kukkonen-Harjula K. (2000). Does physical activity prevent weight gain – a systematic review. Obes. Rev. 1 (2), 95–111. doi:10.1046/j.1467-789x.2000.00016.x
Garber C. E., Blissmer B., Deschenes M. R., Franklin B. A., Lamonte M. J., Lee I. M., et al. (2011). American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med. and Sci. Sports and Exerc. 43 (7), 1334–1359. doi:10.1249/MSS.0b013e318213fefb
GBD 2015 Obesity Collaborators, Afshin A., Forouzanfar M. H., Reitsma M. B., Sur P., Estep K., Lee A., et al. (2017). Health effects of overweight and obesity in 195 countries over 25 years. N. Engl. J. Med. 377, 13–27. doi:10.1056/NEJMoa1614362
Hackney K. J., Everett M., Scott J. M., Ploutz-Snyder L. (2012). Blood flow-restricted exercise in space. Extrem Physiol. Med. 1 (1), 12. doi:10.1186/2046-7648-1-12
Hall J. E. (2003). The kidney, hypertension, and obesity. Hypertension 41 (3), 625–633. doi:10.1161/01.HYP.0000052314.95497.78
Hall J. E., do Carmo J. M., da Silva A. A., Wang Z., Hall M. E. (2015). Obesity-induced hypertension: interaction of neurohumoral and renal mechanisms. Circ. Res. 116 (6), 991–1006. doi:10.1161/CIRCRESAHA.116.305697
Haslam D. W., James W. P. T. (2005). Obesity. Lancet. 366 (9492), 1197–1209. doi:10.1016/S0140-6736(05)67483-1
Hughes L., Paton B., Rosenblatt B., Gissane C., Patterson S. D. (2017). Blood flow restriction training in clinical musculoskeletal rehabilitation: a systematic review and meta-analysis. Br. J. Sports Med. 51 (13), 1003–1011. doi:10.1136/bjsports-2016-097071
Islam H., Gibala M. J., Little J. P. (2022). Exercise snacks: a novel strategy to improve cardiometabolic health. Exerc Sport Sci. Rev. 50 (1), 31–37. doi:10.1249/JES.0000000000000275
Johns H. B., Hartmann-Boyce J., Jebb S. A., Aveyard P. (2014). Diet or exercise interventions vs combined behavioral weight management programs: a systematic review and meta-analysis of direct comparisons. J. Acad. Nutr. Dietetics 114 (10), 1557–1568. doi:10.1016/j.jand.2014.07.005
Keys A., Fidanza F., Karvonen M. J., Kimura N., Taylor H. L. (2014). Indices of relative weight and obesity. Int. J. Epidemiol. 43 (3), 655–665. doi:10.1093/ije/dyu058
Kim J., Yoon J. H. (2021). Does obesity affect the severity of exercise-induced muscle injury? J. Obes. Metab. Syndr. 30 (2), 132–140. doi:10.7570/jomes20100
Kim K. B., Kim K., Kim C., Kang S. J., Kim H. J., Yoon S., et al. (2019). Effects of exercise on the body composition and lipid profile of individuals with obesity: a systematic review and meta-analysis. J. Obes. Metab. Syndr. 28 (4), 278–294. doi:10.7570/jomes.2019.28.4.278
Kim N., Lee D., Lee S., Kim N., Lee D., Lee S. (2021). Effects of 5 Week low-intensity blood flow restriction resistance exercise and moderate-intensity resistance exercise on body composition and blood lipids in normal weight obese women. Exerc Sci. 30 (1), 70–79. doi:10.15857/ksep.2021.30.1.70
Lewington C., Qizilbash P. (2002). Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 360 (9349), 1903–1913. doi:10.1016/s0140-6736(02)11911-8
Li S., Guo R., Yu T., Li S., Han T., Yu W. (2022). Effect of high-intensity interval training combined with blood flow restriction at different phases on abdominal visceral fat among obese adults: a randomized controlled trial. Int. J. Environ. Res. Public Health 19 (19), 11936. doi:10.3390/ijerph191911936
Libardi C. A., Chacon-Mikahil M. P. T., Cavaglieri C. R., Tricoli V., Roschel H., Vechin F. C., et al. (2015a). Effect of concurrent training with blood flow restriction in the elderly. Int. J. Sports Med. 36 (5), 395–399. doi:10.1055/s-0034-1390496
Libardi C. A., Chacon-Mikahil M. P. T., Cavaglieri C. R., Tricoli V., Roschel H., Vechin F. C., et al. (2015b). Effect of concurrent training with blood flow restriction in the elderly. Int. J. Sports Med. 36, 395–399. doi:10.1055/s-0034-1390496
Lorenz D. S., Bailey L., Wilk K. E., Mangine R. E., Head P., Grindstaff T. L., et al. (2021). Blood flow restriction training. J. Athl. Train. 56 (9), 937–944. doi:10.4085/418-20
Millstein R. A. (2014). Measuring outcomes in adult weight loss studies that include diet and physical activity: a systematic review. J. Nutr. Metabolism 2014 (1), 421423. doi:10.1155/2014/421423
Mohammadiyan M. (2021). The effect of two different intensities of resistance training with blood flow restriction on muscle strength, body fat percentage and serum level of Irisin in overweight women. Iran J Obstetrics. Gynecol. Infertil. 24 (3), 42–50. doi:10.22038/ijogi.2021.18302
Moore K., Cerhan J., Jacobs E. J., Rosenberg P. S., Adami H. O., Kitahara C. M., et al. (2014). A pooled analysis of waist circumference and mortality in 650,000 adults. Mayo Clin. Proc. 89 (3), 335–345. doi:10.1016/j.mayocp.2013.11.011
Mouser J. G., Dankel S. J., Jessee M. B., Mattocks K. T., Buckner S. L., Counts B. R., et al. (2017). A tale of three cuffs: the hemodynamics of blood flow restriction. Eur. J. Appl. Physiol. 117 (7), 1493–1499. doi:10.1007/s00421-017-3644-7
Nagashima K., Noma H., Furukawa T. A. (2018). Prediction intervals for random-effects meta-analysis: a confidence distribution approach. Stat. Methods Med. Res. 28, 1689–1702. doi:10.1177/0962280218773520
Newsome A. M., Batrakoulis A., Camhi S. M., McAvoy C., Sansone J., Reed R., et al. (2024). 2025 ACSM worldwide fitness trends: future directions of the health and fitness industry. ACSM’s Health and Fit. J. 28 (6), 11–25. doi:10.1249/fit.0000000000001017
Nuttall F. Q. (2015). Body mass index: obesity, BMI, and health: a critical review. Nutr. Today 50 (3), 117–128. doi:10.1097/NT.0000000000000092
Oppert J. M., Bellicha A., van Baak M. A., Battista F., Beaulieu K., Blundell J. E., et al. (2021). Exercise training in the management of overweight and obesity in adults: synthesis of the evidence and recommendations from the European association for the study of obesity physical activity working group. Obes. Rev. 22 (Suppl. 4), e13273. doi:10.1111/obr.13273
Oppert J. M., Ciangura C., Bellicha A. (2023). Physical activity and exercise for weight loss and maintenance in people living with obesity. Rev. Endocr. Metab. Disord. 24 (5), 937–949. doi:10.1007/s11154-023-09805-5
Page M. J., McKenzie J. E., Bossuyt P. M., Boutron I., Hoffmann T. C., Mulrow C. D., et al. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372, n71. doi:10.1136/bmj.n71
Patterson S. D., Hughes L., Warmington S., Burr J., Scott B. R., Owens J., et al. (2019). Blood flow restriction exercise: considerations of methodology, application, and safety. Front. Physiol. 10, 533. doi:10.3389/fphys.2019.00533
Pinto A. J., Bergouignan A., Dempsey P. C., Roschel H., Owen N., Gualano B., et al. (2023). Physiology of sedentary behavior. Physiol. Rev. 103 (4), 2561–2622. doi:10.1152/physrev.00022.2022
Poon E. T. C., Li H. Y., Little J. P., Wong S. H. S., Ho R. S. T. (2024). Efficacy of interval training in improving body composition and adiposity in apparently healthy adults: an umbrella review with meta-analysis. Sports Med. 54 (11), 2817–2840. doi:10.1007/s40279-024-02070-9
Romieu I., Dossus L., Barquera S., Blottière H. M., Franks P. W., Gunter M., et al. (2017). Energy balance and obesity: what are the main drivers? Cancer Causes Control 28 (3), 247–258. doi:10.1007/s10552-017-0869-z
Ross R., Dagnone D., Jones P. J. H., Smith H., Paddags A., Hudson R., et al. (2000). Reduction in obesity and related comorbid conditions after diet-induced weight loss or exercise-induced weight loss in men. A randomized, controlled trial. Ann. Intern Med. 133 (2), 92–103. doi:10.7326/0003-4819-133-2-200007180-00008
Rossow L. M., Fahs C. A., Loenneke J. P., Thiebaud R. S., Sherk V. D., Abe T., et al. (2012). Cardiovascular and perceptual responses to blood-flow-restricted resistance exercise with differing restrictive cuffs. Clin. Physiol. Funct. Imaging 32 (5), 331–337. doi:10.1111/j.1475-097X.2012.01131.x
Rutan G. H., Kuller L. H., Neaton J. D., Wentworth D. N., McDonald R. H., Smith W. M. (1988). Mortality associated with diastolic hypertension and isolated systolic hypertension among men screened for the Multiple Risk Factor Intervention Trial. Circulation 77 (3), 504–514. doi:10.1161/01.cir.77.3.504
Schünemann H. J., Higgins J. P., Vist G. E., Glasziou P., Akl E. A., Skoetz N., et al. (2019). “Completing ‘Summary of findings’ tables and grading the certainty of the evidence,” in Cochrane Handbook for systematic reviews of interventions (John Wiley and Sons, Ltd), 375–402. doi:10.1002/9781119536604.ch14
Sesso H. D., Stampfer M. J., Rosner B., Hennekens C. H., Gaziano J. M., Manson J. E., et al. (2000). Systolic and diastolic blood pressure, pulse pressure, and mean arterial pressure as predictors of cardiovascular disease risk in men. Hypertension 36 (5), 801–807. doi:10.1161/01.hyp.36.5.801
Spitz R. W., Chatakondi R. N., Bell Z. W., Wong V., Dankel S. J., Abe T., et al. (2019). The impact of cuff width and biological sex on cuff preference and the perceived discomfort to blood-flow-restricted arm exercise. Physiol. Meas. 40 (5), 055001. doi:10.1088/1361-6579/ab1787
Spranger M. D., Krishnan A. C., Levy P. D., O’Leary D. S., Smith S. A. (2015). Blood flow restriction training and the exercise pressor reflex: a call for concern. Am. J. Physiol. Heart Circ. Physiol. 309 (9), H1440–H1452. doi:10.1152/ajpheart.00208.2015
Stamler J., Stamler R., Neaton J. D. (1993). Blood pressure, systolic and diastolic, and cardiovascular risks: US population data. Archives Intern. Med. 153 (5), 598–615. doi:10.1001/archinte.153.5.598
Stiegler P., Cunliffe A. (2006). The role of diet and exercise for the maintenance of fat-free mass and resting metabolic rate during weight loss. Sports Med. 36 (3), 239–262. doi:10.2165/00007256-200636030-00005
Su Y., Wang F., Wang M., He S., Yang X., Luan Z. (2024). Effects of blood flow restriction training on muscle fitness and cardiovascular risk of obese college students. Front. Physiol. 14, 1252052. doi:10.3389/fphys.2023.1252052
Sun L. (2022). Effects of blood flow restriction training on anthropometric and blood lipids in overweight/obese adults: meta-analysis. Front. Physiol. 13, 1039591. doi:10.3389/fphys.2022.1039591
Swain D. P., Franklin B. A. (2006). Comparison of cardioprotective benefits of vigorous versus moderate intensity aerobic exercise. Am. J. Cardiol. 97 (1), 141–147. doi:10.1016/j.amjcard.2005.07.130
Swift D. L., Johannsen N. M., Lavie C. J., Earnest C. P., Church T. S. (2014). The role of exercise and physical activity in weight loss and maintenance. Prog. Cardiovasc. Dis. 56 (4), 441–447. doi:10.1016/j.pcad.2013.09.012
Wenger H. A., Bell G. J. (1986). The interactions of intensity, frequency and duration of exercise training in altering cardiorespiratory fitness. Sports Med. 3 (5), 346–356. doi:10.2165/00007256-198603050-00004
Willis L. H., Slentz C. A., Bateman L. A., Shields A. T., Piner L. W., Bales C. W., et al. (2012). Effects of aerobic and/or resistance training on body mass and fat mass in overweight or obese adults. J. Appl. Physiology 113 (12), 1831–1837. doi:10.1152/japplphysiol.01370.2011
Wu T., Gao X., Chen M., Van Dam R. M. (2009). Long-term effectiveness of diet-plus-exercise interventions vs. diet-only interventions for weight loss: a meta-analysis. Obes. Rev. 10 (3), 313–323. doi:10.1111/j.1467-789X.2008.00547.x
Yin M., Chen Z., Nassis G. P., Liu H., Li H., Deng J., et al. (2023). Chronic high-intensity interval training and moderate-intensity continuous training are both effective in increasing maximum fat oxidation during exercise in overweight and obese adults: a meta-analysis. J. Exerc Sci. Fit. 21 (4), 354–365. doi:10.1016/j.jesf.2023.08.001
Yin M., Deng S., Chen Z., Zhang B., Zheng H., Bai M., et al. (2024c). Exercise snacks are a time-efficient alternative to moderate-intensity continuous training for improving cardiorespiratory fitness but not maximal fat oxidation in inactive adults: a randomized controlled trial. Appl. Physiol. Nutr. Metab. 49 (7), 920–932. doi:10.1139/apnm-2023-0593
Yin M., Li H., Bai M., Liu H., Chen Z., Deng J., et al. (2024a). Is low-volume high-intensity interval training a time-efficient strategy to improve cardiometabolic health and body composition? A meta-analysis. Appl. Physiol. Nutr. Metab. 49 (3), 273–292. doi:10.1139/apnm-2023-0329
Yin M., Li H., Zhang B., Li Y. (2024b). Comment on “exercise snacks and other forms of intermittent physical activity for improving health in adults and older adults: a scoping review of epidemiological, experimental and qualitative studies”. Sports Med. 54 (8), 2199–2203. doi:10.1007/s40279-024-02080-7
Yin M., Xu K., Deng J., Deng S., Chen Z., Zhang B., et al. (2024e). Optimal frequency of interrupting prolonged sitting for cardiometabolic health: a systematic review and meta-analysis of randomized crossover trials. Scand. J. Med. Sci. Sports 34 (12), e14769. doi:10.1111/sms.14769
Yin M., Zheng H., Bai M., Huang G., Chen Z., Deng S., et al. (2024d). Effects of integrating stair climbing-based exercise snacks into the campus on feasibility, perceived efficacy, and participation perspectives in inactive young adults: a randomized mixed-methods pilot study. Scand. J. Med. Sci. Sports 34 (12), e14771. doi:10.1111/sms.14771
Keywords: vascular occlusion, kaatsu, body fat percentage, systolic blood pressure, obesity
Citation: Kong H, Zhang Y, Yin M, Xu K, Sun Q, Xie Y and Girard O (2025) Effects of blood flow restriction training on cardiometabolic health and body composition in adults with overweight and obesity: a meta-analysis. Front. Physiol. 15:1521995. doi: 10.3389/fphys.2024.1521995
Received: 03 November 2024; Accepted: 23 December 2024;
Published: 17 January 2025.
Edited by:
Tim Werner, Salisbury University, United StatesReviewed by:
Alexios Batrakoulis, University of Thessaly, GreeceYu Lun Tai, Texas A&M University Central Texas, United States
Copyright © 2025 Kong, Zhang, Yin, Xu, Sun, Xie and Girard. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: QingGuo Sun, cWdzajE2M0AxNjMuY29t
†These authors share first authorship
 Hao Kong
Hao Kong Yilin Zhang
Yilin Zhang Mingyue Yin
Mingyue Yin Kai Xu
Kai Xu QingGuo Sun1*
QingGuo Sun1* Olivier Girard
Olivier Girard