- 1Faculty of Educational Studies, University Putra Malaysia, Selangor, Malaysia
- 2Department of Sports Teaching and Research, Lanzhou University, Lanzhou, China
- 3School of Physical Education, Xi’an Peihua University, Xi’an, China
- 4School of Physical Education, Xizang Minzu University, Xianyang, China
- 5School of Physical Education, Shenyang Medical College, Shenyang, China
Aerobic training with blood flow restriction (AT-BFR) has shown promise in enhancing both aerobic capacity and exercise performance. The aim of this review was to systematically analyze the evidence regarding the effectiveness of this novel training method on aerobic capacity, muscle strength, and hypertrophy in young adults. Studies were identified through a search of databases including PubMed, Scopus, Web of Science, SPORTDiscus, CINAHL, Cochrane Library, and EMBASE. A total of 16 studies, involving 270 subjects, were included in the meta-analysis. The results revealed that AT-BFR induced greater improvements in VO2max (SMD = 0.27, 95%CI: [0.02, 0.52], p < 0.05), and muscle strength (SMD = 0.39, 95%CI: [0.09, 0.69], p < 0.05), compared to aerobic training with no blood flow restriction (AT-noBFR). However, no significant effect was observed on muscle mass (SMD = 0.23, 95%CI: [-0.09, 0.56], p = 0.162). Furthermore, no moderating effects on the outcomes were found for individual characteristics or training factors. In conclusion, AT-BFR is more effective than AT-noBFR in improving aerobic capacity and muscle strength, making it a promising alternative to high-intensity training.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/, identifier CRD42024559872.
Introduction
Aerobic exercise offers significant benefits for athletic performance and overall health, including improved cardiorespiratory fitness (Andreu-Caravaca et al., 2021; Huang et al., 2005), improved muscle quality (Lee and Stone, 2020; Markov et al., 2022), enhanced recovery (Paneroni et al., 2017), and reduced cardiovascular disease risk (Brouwer et al., 2021; Kodama et al., 2009). However, low-intensity aerobic exercise may not be sufficient to achieve substantial improvements in these aspects. The American College of Sports Medicine recommends 5–7 days of moderate-intensity aerobic exercise or 3 days of vigorous exercise per week for adults to improve health and prevent disease (Garber et al., 2011). As aerobic capacity and performance improve, higher-intensity aerobic fitness methods are required to elicit training adaptations (Medicine, 2013). Nonetheless, high-intensity training is not suitable for some specific populations, such as the elderly, patients undergoing rehabilitation, or in-season athletes. Therefore, developing a low-intensity training method that can achieve similar benefits to high-intensity training is of great significance.
Blood flow restriction (BFR) training has gained increasing popularity in the fields of sports and rehabilitation (Hughes et al., 2017; Loenneke et al., 2010). This method involves applying an external constricting device to the proximal limbs to partially restrict venous return, thereby creating a hypoxic and stressful environment that promotes physical adaptations (Jessee et al., 2018). Previous meta-analyses have found that BFR resistance training can achieve effects similar to high-intensity resistance exercise, specifically regarding muscle strength and hypertrophy, while minimizing mechanical load (20–30% one repetition maximum) (Centner et al., 2019; Grønfeldt et al., 2020; Lixandrão et al., 2018). This suggests that BFR training may provide a viable alternative to high-intensity resistance training for the development of muscular strength and hypertrophy.
In effect, AT-BFR may offer an effective and practical method to improve aerobic capacity, muscle strength, and hypertrophy, particularly in older adults, clinical rehabilitation populations, and athletes during periods of reduced training intensity. Despite its potential benefits for these groups, most studies on AT-BFR have focused on young adults, primarily due to their better health and greater training adaptability, which help control experimental conditions and minimize confounding factors (Formiga et al., 2020; Silva et al., 2019). Recent research has aimed to determine the effects of AT-BFR on aerobic capacity and muscle performance in young adults, yielding conflicting results (Chen et al., 2021; Herda et al., 2024; Keramidas et al., 2012). While a previous meta-analysis has been conducted, it exhibits notable limitations. The meta-analysis by Formiga et al. (2020) focused exclusively on aerobic capacity, while the meta-analysis by de Lemos Muller et al. (2024) examined only muscle strength and hypertrophy, with both including a limited number of studies. Additionally, the review by Bennett and Slattery (2019) explored the effects of aerobic BFR on aerobic capacity and performance but relied on a narrative review without meta-analytical rigor, limiting the quantitative synthesis of evidence. These studies, while valuable, fail to comprehensively assess AT-BFR’s combined effects on aerobic capacity, muscle strength, and hypertrophy. Furthermore, individual characteristics (e.g., sex, training status) and training variables (e.g., intensity, frequency) are likely to moderate these outcomes (Wang et al., 2023a; Wilk et al., 2018), which highlights the need to evaluate their potential influences to better understand AT-BFR’s overall effectiveness. Investigating these outcomes together is crucial, as they represent the multidimensional adaptations influenced by AT-BFR. By creating localized hypoxia, increasing metabolic stress, and altering muscle fiber recruitment, AT-BFR triggers adaptations in both aerobic and muscular systems, making it effective for enhancing overall physical performance (Pope et al., 2013; Smith et al., 2022). These adaptations are essential for designing training protocols that balance cardiovascular and muscular performance.
This study aims to systematically evaluate the effects of AT-BFR on aerobic capacity, muscle strength, and hypertrophy in young adults, as well as well as the moderating effects of individual characteristics (e.g., gender, training level) and training variables (e.g., training duration, frequency, intensity, cuff pressure) on training outcomes. The findings could help inform the design of more personalized and optimized training protocols and improve the applicability of AT-BFR in both athletic and clinical settings.
Materials and methods
Search strategy and study selection
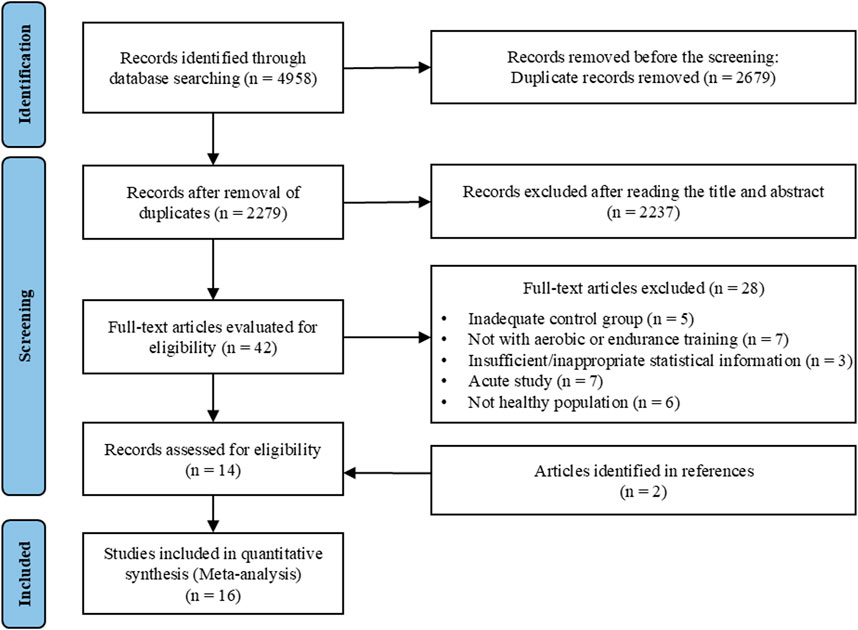
This systematic review and meta-analysis were conducted in accordance with the PRISMA guidelines (Page et al., 2021) (Prospero registration number: CRD42024559872). Comprehensive searches were conducted across multiple electronic databases, including PubMed, Scopus, Web of Science, SPORTDiscus, CINAHL, Cochrane Library, and EMBASE, up to 15 June 2024. Boolean operators AND and OR were applied to predefined combinations of keywords and MeSH terms in each database: (“blood flow restriction therapy” OR “ischemia” OR “vascular occlusion” OR “tourniquets” OR “occlusion training”) AND (“endurance exercise” OR “aerobic exercise” OR “cycling” OR “running” OR “walking”). Detailed search strings are provided in Supplementary Material 1. After deduplication, the titles and abstracts of the retrieved articles were screened, followed by a full-text review (Figure 1). Additionally, reference lists of included studies were scrutinized for further relevant articles. Two researchers (T. W. and X.W.) independently retrieved articles, with any discrepancies resolved by a third researcher (Z.G.).
Eligibility criteria
Eligibility criteria for article inclusion were as follows: (a) healthy young adults; (b) the study design allowed comparisons between AT-BFR and AT-noBFR; (c) aerobic capacity, muscle strength and/or muscle hypertrophy were assessed pre- and post-training; (e) publications in English.
Methodological quality assessment and risk of bias
The quality of the included studies was assessed using the PEDro scale (Verhagen et al., 1998), which evaluates methodologies based on 11 criteria, such as randomization, blinding, and outcome measures. The scale has a maximum score of 10 points, with the first item not being scored. Following established research standards (Stojanović et al., 2017; Wang et al., 2024), studies scoring below 4 on the PEDro scale were considered low quality. In addition, the revised Cochrane risk-of bias tool for randomized trials (RoB-2 tool version 2) was employed to assess potential bias across five domains: randomization, deviations from the intended intervention, missing data, outcome measurement, and selective reporting (Sterne et al., 2019). The assessment of methodological quality was independently conducted by two reviewers (Y.L. and J.Z.), with any discrepancies resolved by consensus with a third reviewer (L. L.). Additionally, potential bias was evaluated through visual inspection of funnel plots and Egger’s test.
Data extraction
The following data were extracted: participant demographics (i.e., age, gender, training status), and study characteristics (i.e., training duration, frequency, intensity, volume, occlusion pressure). For outcome measures, data were collected on aerobic capacity testing (e.g., VO2max or lactate threshold), muscle strength testing (e.g., dynamic, isometric, and isokinetic testing), and muscle mass testing (e.g., assessed by magnetic resonance imaging, and ultrasound). When multiple time points for training outcomes were available, the latest time point was used as the post-training value for analysis. In cases where the required data were unavailable, they were requested directly from the authors. In the absence of a response, the study outcome was excluded. The specific characteristics of the participants and plyometric training protocol were presented in Table 1.
Statistical analyses
All meta-analyses were conducted using R version 4.3.0 (R Foundation for Statistical Computing, Vienna, Austria). Meta-analysis was conducted using the metacont() function from the meta package, with subgroup analyses performed via the update() function. Sensitivity analyses were carried out using the InfluenceAnalysis() function from the dmetar package. The effect size difference for between-group comparisons (AT-BFR vs. AT-noBFR) was calculated using pre- and post-intervention data (mean, standard deviation, and sample size). The change in standard deviation (
The magnitude of effect size was categorized as follows: <0.40 = small, 0.40–0.70 = moderate, and >0.70 = large (Higgins, 2008). A random effects model was employed to account for heterogeneity and measurement variability among the included studies. Heterogeneity was verified with the I2 statistic, with I2 ≤ 25% indicating low heterogeneity, 25%–75% indicating moderate heterogeneity, and >75% indicating high heterogeneity (Higgins et al., 2003).
A total of three meta-analyses were conducted. The analyses examined the impact of AT-BFR versus AT-noBFR on aerobic capacity (VO2max), maximal muscle strength, and muscle mass, which were the primary outcomes of this systematic review and meta-analysis. Additionally, Secondary outcomes were evaluated through subgroup analyses, which examined the potential moderating effects of variables such as gender, training status (trained or untrained), training duration (<8 weeks and ≥8 weeks), training frequency (≤3 days/week and >3 days/week), training intensity (low intensity, walking; moderate intensity, running, swimming, or rowing), occlusion pressure (<180 mmHg or ≥180 mmHg) on these primary outcomes. The threshold for statistical significance was set at p < 0.05.
The meta-analysis involved some deviations from the registered protocol. To enhance homogeneity, the analysis focused on a more consistent participant group, specifically younger adults. Furthermore, subgroup analyses were conducted only when each subgroup included at least three homogeneous datasets, resulting in the exclusion of certain subgroups due to a limited number of studies.
Results
Study selection
A total of 4,958 studies were identified in the initial search. After title and abstract screening, 42 studies were subjected to full-text review based on the eligibility criteria. Of these, 14 studies met the inclusion criteria. Additionally, two studies were identified through reference lists of the selected articles. Ultimately, 16 studies were included in the final systematic review and meta-analysis. An overview of these studies is provided in Figure 1.
Methodological quality assessment and risk of bias
The quality assessment of the included studies identified 9 studies as moderate quality (scores of 4–5) and 10 studies as high quality (scores of 6–10). With a median score of 6 out of 10, the overall quality of the studies was determined to be moderate to high, supporting the reliability of the findings. Detailed PEDro scale scores are provided in the Supplementary Material 2.
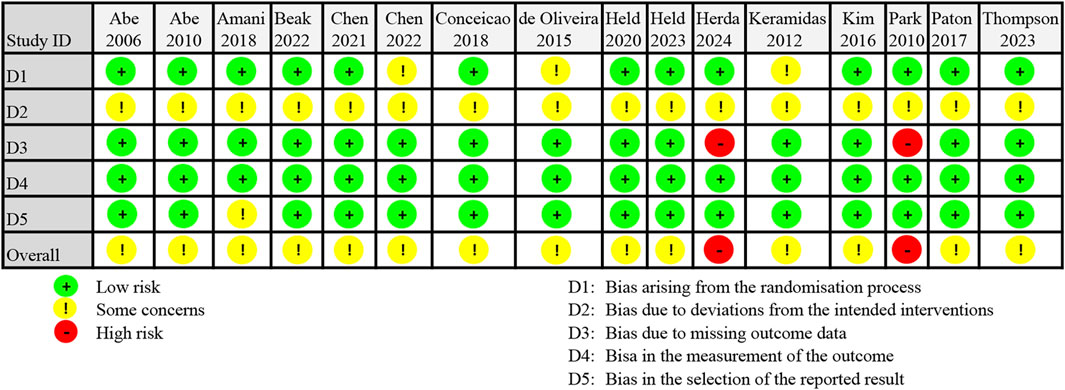
The ROB2 assessment revealed that 14 studies were rated as having some concern regarding risk of bias, while other 2 studies were classified as high risk (see Figure 2). All studies exhibited deviations from the intended interventions (Domain 2), attributed to the lack of access to trial protocols and absence of trial registration information. In Domain 1, baseline differences between intervention groups in three studies raised concerns regarding group comparability. Two studies were classified as high risk in Domain 3 due to outcome data being available for fewer than 85% of participants. In Domain 4, all studies were considered low risk for measurement methods, as reliable instruments were employed. One study showed some results that appeared unreasonable, raising concerns in Domain 5. Detailed risk of bias percentages are provided in Supplementary Material 3.
Egger’s test revealed no significant publication bias for VO2max (b = 2.38, t = 1.85, p = 0.09), while it was not applicable for muscle strength and muscle mass due to the limited number of studies (n < 10). The funnel plots from the four meta-analyses demonstrated a relatively symmetrical distribution, suggesting no significant publication bias or selective reporting (see Supplementary Material 4).
Meta-analysis results
Thirteen studies comparing the effects of AT-BFR and AT-noBFR were included in this meta-analysis (see Figure 3). The mean VO2max gain was 5.7% ± 3.2% for the AT-BFR group and 2.4% ± 7.0% for the AT-noBFR group. The meta-analysis results showed AT-BFR had a small effect on VO2max compared to AT-noBFR (SMD = 0.27, 95%CI: [0.02, 0.52], p = 0.031 < 0.05). The I2 statistic indicated minimal heterogeneity (0%).
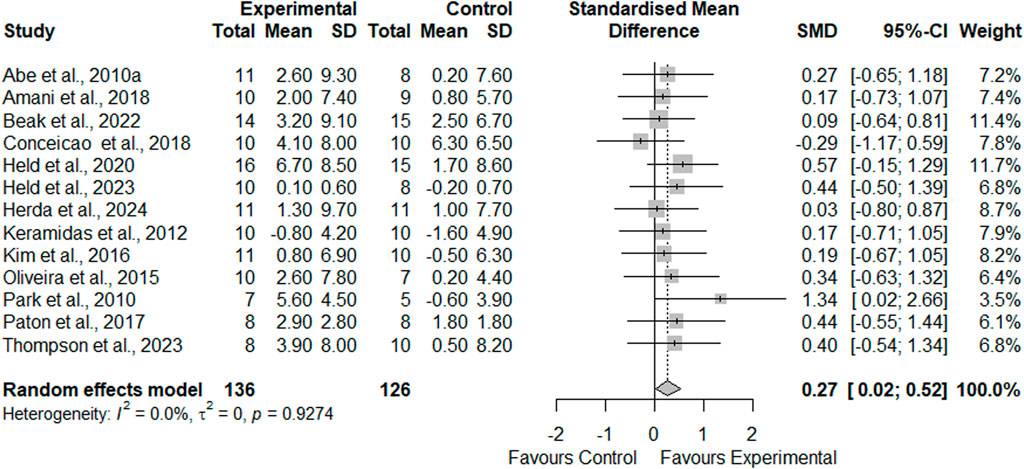
Figure 3. Forest plot demonstrating the effects of aerobic training with blood flow restriction vs. without blood flow restriction on VO2max.
Nine studies comparing the effects of AT-BFR and AT-noBFR were included for meta-analysis (Figure 4). Across comparisons, AT-BFR resulted in an average percentage increase of 7.3% ± 2.5% in muscle strength, compared to AT-noBFR with 2.3% ± 2.5%. Quantitative analyses demonstrated that AT-BFR had a moderate effect on muscle strength compared to AT-noBFR (SMD = 0.39, 95%CI: [0.09, 0.69], p = 0.011 < 0.05). The I2 statistic indicated minimal heterogeneity (0%).
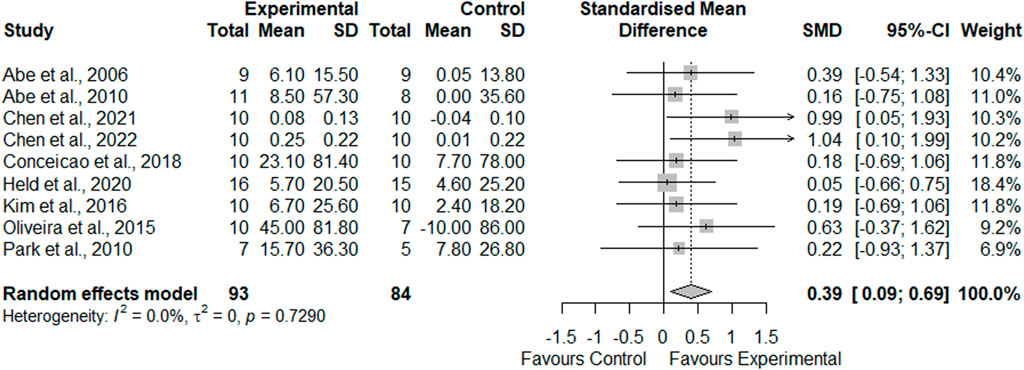
Figure 4. Forest plot demonstrating the effects of aerobic training with blood flow restriction vs. without blood flow restriction on muscle strength.
Seven studies comparing the effects of AT-BFR and AT-noBFR on muscle mass were included in this meta-analysis (Figure 5). Between-group comparisons showed higher increases in muscle mass following AT-BFR (5.8% ± 2.7%) compared to AT-noBFR (2.1% ± 2.2%). Statistical examination revealed that AT-BFR had a small effect on muscle mass compared to AT-noBFR (SMD = 0.23, 95%CI: [-0.09, 0.56], p = 0.162). The I2 statistic indicated minimal heterogeneity (0%).
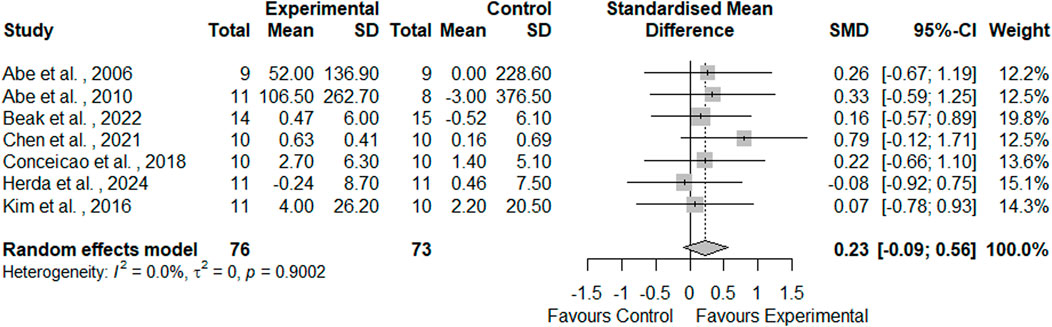
Figure 5. Forest plot demonstrating the effects of aerobic training with blood flow restriction vs. without blood flow restriction on muscle mass.
The sensitivity analysis revealed no significant changes, with effect sizes and heterogeneity remaining stable after excluding individual studies, further confirming the robustness and reliability of the results (see Supplementary Material 5). Subgroup analyses were conducted if at least three relatively homogeneous datasets were available for each subgroup. A total of 13 subgroup analyses were performed for aerobic capacity, muscle strength, and hypertrophy based on gender, training level, training intensity, training frequency, training duration, and occlusion pressure (see Supplementary Material 6). The results showed that all subgroup analyses were non-significant.
Discussion
This meta-analysis compared the effects of AT-BFR and AT-noBFR on aerobic capacity (i.e., VO2max), muscle strength, and muscle mass. The main findings indicated that AT-BFR induced greater improvements in VO2max and maximal strength compared to AT-noBFR. However, no significant differences were observed in muscle mass. Additionally, personal characteristics and training-related factors did not appear to significantly moderate the training outcomes.
With regard to aerobic capacity, this meta-analysis found that AT-BFR was more effective in improving VO2max than AT-noBFR, consistent with the meta-analysis by Formiga et al. (2020). Furthermore, several studies included in this meta-analysis reported superior improvements in running economy and time to exhaustion with AT-BFR compared to AT-noBFR (Herda et al., 2024; Paton et al., 2017). The enhanced aerobic capacity observed with AT-BFR can be attributed to several potential mechanisms. Firstly, BFR exercise induces higher heart rate and blood pressure during activity, creating increased cardiovascular stress and stimulating adaptive cardiovascular responses (Takano et al., 2005). Secondly, Second, BFR-induced hypoxia, resulting from reduced oxygen delivery and impaired metabolite clearance, triggers increased oxidative stress, activating AMPK signaling pathways that are crucial for mitochondrial biogenesis and cellular energy regulation (Christiansen et al., 2018). These molecular adaptations improve mitochondrial function, angiogenesis, and capillary density within muscle tissue, facilitating better oxygen delivery and utilization (Barjaste et al., 2021; Christiansen et al., 2020). Moreover, the fluid shear stress caused by ischemia and reperfusion during BFR exercise may strongly promote the expression of angiogenesis-related factors, contributing to vascular adaptation (Hudlicka and Brown, 2009). These combined mechanisms likely contribute to the observed improvements in both aerobic capacity.
Although this study did not find a significant effect of AT-BFR on muscle mass, the analysis showed that AT-BFR significantly enhanced maximal strength. This phenomenon can be attributed to the mechanisms of blood flow restriction training, which involves recruitment of fast-twitch fibers, stimulation of protein synthesis, and activation of anabolic growth factors, all of which play a key role in strength improvement (Crane et al., 2013; Loenneke et al., 2010; Markov et al., 2022). However, the lack of significant muscle mass improvement may be due to the limitations of low-intensity aerobic training in promoting muscle hypertrophy. Aerobic training primarily enhances exercise performance through improvements in cardiovascular endurance, with relatively minor effects on muscle mass, especially at lower training intensities (Hendrickse et al., 2021; Jones and Carter, 2000). In contrast, de Lemos Muller (2024) reported increases in muscle hypertrophy, likely due to their use of localized measures such as cross-sectional area, which are more sensitive to site-specific adaptations. Additionally, their inclusion of a broader age range (18–60 years) may have introduced greater variability in baseline muscle characteristics and adaptive potential, compared to our focus on young adults with more uniform responses. These differences highlight the specificity of AT-BFR’s effects and suggest it is more effective for increasing strength than muscle mass, particularly in training programs balancing strength and endurance or in low-intensity regimens for injured athletes.
Although individual and training factors did not significantly moderate training outcomes, this systematic review and meta-analysis provides valuable insights. No significant differences were found between training intensities (40%–90% VO2max), indicating that low-intensity (40%–60% VO2max) AT-BFR can produce similar effects to high-intensity training. This makes it particularly beneficial for individuals undergoing rehabilitation or athletes who need to maintain performance during the competitive season without overtraining. Regarding training duration, while the studies included in this meta-analysis ranged from 2 to 8 weeks, even short-term (2–4 weeks) training was effective in significantly improving aerobic capacity and strength, making it suitable for athletes requiring rapid recovery or performance maintenance. A training frequency of 2–6 days per week was also effective, demonstrating the flexibility of AT-BFR in various training programs. Regarding cuff pressure, no significant impact on training outcomes was observed within the 90–240 mmHg range. However, for individuals with lower physical capacity or cardiovascular conditions, it is recommended to use lower occlusion pressure to enhance safety. Overall, AT-BFR demonstrates broad adaptability across different training conditions. However, these findings are based on a limited number of studies, and further research is needed to strengthen the evidence base and optimize its application.
Limitations
This meta-analysis has several limitations that should be carefully considered in the interpretation of the findings. Although BFR training is widely discussed in scientific research (Hughes et al., 2017; Scott et al., 2015; Wang et al., 2023b), the number of studies examining the effects of AT-BFR is still sparse. More high-quality studies are needed in the future to enhance the robustness and applicability of the results. Secondly, while the included studies have not documented adverse reactions or injuries associated with AT-BFR, this does not imply that the training is devoid of potential safety concerns. Thirdly, while most studies were of high quality, some were of fair quality, and nearly all failed to blind participants, coaches, or assessors. Future research should improve blinding and randomization procedures, and provide detailed reports on study design and analysis methods to enhance the reliability and reproducibility of results.
Conclusion
The present meta-analysis demonstrated that AT-BFR significantly improves VO2max and maximal strength compared to AT-noBFR, with no significant effect on muscle mass. Individual characteristics and training factors did not notably influence these outcomes. AT-BFR appears to provide a viable and effective alternative to high-intensity training.
From a practical standpoint, aerobic exercise plays a crucial role in maintaining cardiovascular health and function, as well as enhancing athletic performance. This review demonstrates that AT-BFR can improve aerobic capacity and muscle performance at low exercise intensities. This approach is particularly beneficial for groups that cannot tolerate high-intensity exercise, such as older adults, individuals undergoing rehabilitation, and endurance athletes during the competitive season. AT-BFR offers a flexible and safe alternative to high-intensity training, allowing for significant improvements in aerobic capacity and strength with minimal risk of overtraining. Its effectiveness is maintained across different training durations and frequencies, with even short-term (2–4 weeks) training showing positive outcomes. However, further research is needed to refine optimal protocols and expand its applicability across different populations and training goals.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Author contributions
ZG: Conceptualization, Formal Analysis, Investigation, Methodology, Software, Writing–original draft. YL: Conceptualization, Investigation, Methodology, Writing–review and editing. JZ: Data curation, Formal Analysis, Methodology, Software, Writing–original draft. LL: Data curation, Formal Analysis, Software, Writing–original draft. TW: Data curation, Formal Analysis, Writing–original draft. XW: Data curation, Formal Analysis, Software, Writing–original draft. HW: Conceptualization, Investigation, Writing–original draft, Writing–review and editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work is supported by the Fundamental Research Funds for the Central Universities in China (Project number: 22lzujbkydx045).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphys.2024.1506386/full#supplementary-material
References
Abe T., Fujita S., Nakajima T., Sakamaki M., Ozaki H., Ogasawara R., et al. (2010). Effects of low-intensity cycle training with restricted leg blood flow on thigh muscle volume and VO2max in young men. J. sports Sci. and Med. 9, 452–458.
Abe T., Kearns C. F., Sato Y. (2006). Muscle size and strength are increased following walk training with restricted venous blood flow from the leg muscle, Kaatsu-walk training. J. Appl. physiology 100, 1460–1466. doi:10.1152/japplphysiol.01267.2005
Amani A. R., Sadeghi H., Afsharnezhad T. (2018). Interval training with blood flow restriction on aerobic performance among young soccer players at transition phase. Montenegrin J. Sports Sci. and Med. 7. doi:10.26773/mjssm.180901
Andreu-Caravaca L., Ramos-Campo D. J., Chung L. H., Rubio-Arias J. Á. (2021). Dosage and effectiveness of aerobic training on cardiorespiratory fitness, functional capacity, balance, and fatigue in people with multiple sclerosis: a systematic review and meta-analysis. Archives Phys. Med. rehabilitation 102, 1826–1839. doi:10.1016/j.apmr.2021.01.078
Barjaste A., Mirzaei B., Rahmani-Nia F., Haghniyaz R., Brocherie F. (2021). Concomitant aerobic-and hypertrophy-related skeletal muscle cell signaling following blood flow-restricted walking. Sci. and Sports 36, e51–e58. doi:10.1016/j.scispo.2020.03.006
Beak H. J., Park W., Yang J. H., Kim J. (2022). Effect of low-intensity aerobic training combined with blood flow restriction on body composition, physical fitness, and vascular responses in recreational runners. Healthc. MDPI 1789. doi:10.3390/healthcare1009178
Bennett H., Slattery F. (2019). Effects of blood flow restriction training on aerobic capacity and performance: a systematic review. J. Strength and Cond. Res. 33 (2), 572–583. doi:10.1519/JSC.0000000000002963
Brouwer R., Wondergem R., Otten C., Pisters M. F. (2021). Effect of aerobic training on vascular and metabolic risk factors for recurrent stroke: a meta-analysis. Disabil. Rehabilitation 43, 2084–2091. doi:10.1080/09638288.2019.1692251
Centner C., Wiegel P., Gollhofer A., KöNIG D. (2019). Effects of blood flow restriction training on muscular strength and hypertrophy in older individuals: a systematic review and meta-analysis. Sports Med. 49, 95–108. doi:10.1007/s40279-018-0994-1
Chen Y.-T., Hsieh Y.-Y., Ho J.-Y., Ho C.-C., Lin T.-Y., Lin J.-C. (2022). Running interval training combined with blood flow restriction increases maximal running performance and muscular fitness in male runners. Sci. Rep. 12, 9922. doi:10.1038/s41598-022-14253-3
Chen Y.-T., Hsieh Y.-Y., Ho J.-Y., Lin T.-Y., Lin J.-C. (2021). Running training combined with blood flow restriction increases cardiopulmonary function and muscle strength in endurance athletes. J. Strength and Cond. Res. 36, 1228–1237. doi:10.1519/JSC.0000000000003938
Christiansen D., Eibye K., Hostrup M., Bangsbo J. (2020). Training with blood flow restriction increases femoral artery diameter and thigh oxygen delivery during knee-extensor exercise in recreationally trained men. J. physiology 598, 2337–2353. doi:10.1113/JP279554
Christiansen D., Murphy R. M., Bangsbo J., Stathis C. G., Bishop D. J. (2018). Increased FXYD1 and PGC-1α mRNA after blood flow-restricted running is related to fibre type-specific AMPK signalling and oxidative stress in human muscle. Acta physiol. 223, e13045. doi:10.1111/apha.13045
Conceicao M. S., Junior E. M., Telles G. D., Libardi C. A., Castro A., Andrade A. L., et al. (2019). Augmented anabolic responses after 8-wk cycling with blood flow restriction. Med. and Sci. Sports and Exerc. 51, 84–93. doi:10.1249/MSS.0000000000001755
Crane J. D., Macneil L. G., Tarnopolsky M. A. (2013). Long-term aerobic exercise is associated with greater muscle strength throughout the life span. Journals Gerontology Ser. A Biomed. Sci. Med. Sci. 68, 631–638. doi:10.1093/gerona/gls237
De Lemos Muller C. H., Farinha J. B., Leal-Menezes R., Ramis T. R. (2024). Aerobic training with blood flow restriction on muscle hypertrophy and strength: systematic review and meta-analysis. J. Strength and Cond. Res. 38 (7), 1341–1349. doi:10.1519/JSC.0000000000004800
De Oliveira M. F. M. D., Caputo F., Corvino R. B., Denadai B. S. (2016). Short-term low-intensity blood flow restricted interval training improves both aerobic fitness and muscle strength. Scand. J. Med. and Sci. sports 26, 1017–1025. doi:10.1111/sms.12540
Formiga M. F., Fay R., Hutchinson S., Locandro N., Ceballos A., Lesh A., et al. (2020). Effect of aerobic exercise training with and without blood flow restriction on aerobic capacity in healthy young adults: a systematic review with meta-analysis. Int. J. sports Phys. Ther. 15, 175–187. doi:10.26603/ijspt20200175
Garber C. E., Blissmer B., Deschenes M. R., Franklin B. A., Lamonte M. J., Lee I.-M., et al. (2011). American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med. Sci. sports Exerc. 43, 1334–1359. doi:10.1249/MSS.0b013e318213fefb
GrøNFELDT B. M., Lindberg Nielsen J., Mieritz R. M., Lund H., Aagaard P. (2020). Effect of blood-flow restricted vs heavy-load strength training on muscle strength: systematic review and meta-analysis. Scand. J. Med. and Sci. sports 30, 837–848. doi:10.1111/sms.13632
Held S., Behringer M., Donath L. (2020). Low intensity rowing with blood flow restriction over 5 weeks increases V̇O2max in elite rowers: a randomized controlled trial. J. Sci. Med. sport 23, 304–308. doi:10.1016/j.jsams.2019.10.002
Held S., Rappelt L., Deutsch J.-P., Rein R., Wiedenmann T., Schiffer A., et al. (2023). Low-intensity swimming with blood flow restriction over 5 weeks increases VO2peak: a randomized controlled trial using Bayesian informative prior distribution. Eur. J. Sport Sci. 23, 1622–1628. doi:10.1080/17461391.2023.2180671
Hendrickse P. W., Venckunas T., Platkevicius J., Kairaitis R., Kamandulis S., Snieckus A., et al. (2021). Endurance training-induced increase in muscle oxidative capacity without loss of muscle mass in younger and older resistance-trained men. Eur. J. Appl. physiology 121 (11), 3161–3172. doi:10.1007/s00421-021-04768-4
Herda A. A., Cleary C. J., Young D., Rogers K. B., Umana Segura S. E., Bernard C., et al. (2024). Blood flow restriction during walking does not impact body composition or performance measures in highly trained runners. J. Funct. Morphol. Kinesiol. 9, 74. doi:10.3390/jfmk9020074
Higgins J. P. (2008). Cochrane handbook for systematic reviews of interventions version 5.0. 1. Chichester, UK: The Cochrane Collaboration. Available at: http://www.cochrane-handbook.org.
Higgins J. P., Thompson S. G., Deeks J. J., Altman D. G. (2003). Measuring inconsistency in meta-analyses. Bmj 327, 557–560. doi:10.1136/bmj.327.7414.557
Huang G., Gibson C. A., Tran Z. V., Osness W. H. (2005). Controlled endurance exercise training and VO2max changes in older adults: a meta-analysis. Prev. Cardiol. 8, 217–225. doi:10.1111/j.0197-3118.2005.04324.x
Hudlicka O., Brown M. D. (2009). Adaptation of skeletal muscle microvasculature to increased or decreased blood flow: role of shear stress, nitric oxide and vascular endothelial growth factor. J. Vasc. Res. 46, 504–512. doi:10.1159/000226127
Hughes L., Paton B., Rosenblatt B., Gissane C., Patterson S. D. (2017). Blood flow restriction training in clinical musculoskeletal rehabilitation: a systematic review and meta-analysis. Br. J. sports Med. 51, 1003–1011. doi:10.1136/bjsports-2016-097071
Jessee M. B., Mattocks K. T., Buckner S. L., Dankel S. J., Mouser J. G., Abe T., et al. (2018). Mechanisms of blood flow restriction: the new testament. Tech. Orthop. 33, 72–79. doi:10.1097/bto.0000000000000252
Jones A. M., Carter H. (2000). The effect of endurance training on parameters of aerobic fitness. Sports Med. 29, 373–386. doi:10.2165/00007256-200029060-00001
Keramidas M. E., Kounalakis S. N., Geladas N. D. (2012). The effect of interval training combined with thigh cuffs pressure on maximal and submaximal exercise performance. Clin. physiology Funct. imaging 32, 205–213. doi:10.1111/j.1475-097X.2011.01078.x
Kim D., Singh H., Loenneke J. P., Thiebaud R. S., Fahs C. A., Rossow L. M., et al. (2016). Comparative effects of vigorous-intensity and low-intensity blood flow restricted cycle training and detraining on muscle mass, strength, and aerobic capacity. J. Strength and Cond. Res. 30, 1453–1461. doi:10.1519/JSC.0000000000001218
Kodama S., Saito K., Tanaka S., Maki M., Yachi Y., Asumi M., et al. (2009). Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. Jama 301, 2024–2035. doi:10.1001/jama.2009.681
Lee J., Stone A. J. (2020). Combined aerobic and resistance training for cardiorespiratory fitness, muscle strength, and walking capacity after stroke: a systematic review and meta-analysis. J. Stroke Cerebrovasc. Dis. 29, 104498. doi:10.1016/j.jstrokecerebrovasdis.2019.104498
LixandrãO M. E., Ugrinowitsch C., Berton R., Vechin F. C., ConceiçãO M. S., Damas F., et al. (2018). Magnitude of muscle strength and mass adaptations between high-load resistance training versus low-load resistance training associated with blood-flow restriction: a systematic review and meta-analysis. Sports Med. 48, 361–378. doi:10.1007/s40279-017-0795-y
Loenneke J., Wilson G., Wilson J. (2010). A mechanistic approach to blood flow occlusion. Int. J. sports Med. 31, 1–4. doi:10.1055/s-0029-1239499
Markov A., Chaabene H., Hauser L., Behm S., Bloch W., Puta C., et al. (2022). Acute effects of aerobic exercise on muscle strength and power in trained male individuals: a systematic review with meta-analysis. Sports Med. 52, 1385–1398. doi:10.1007/s40279-021-01615-6
Medicine A. C. O. S. (2013). ACSM's guidelines for exercise testing and prescription. Lippincott williams and wilkins.
Page M. J., Mckenzie J. E., Bossuyt P. M., Boutron I., Hoffmann T. C., Mulrow C. D., et al. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Bmj 372, n71. doi:10.1136/bmj.n71
Paneroni M., Simonelli C., Vitacca M., Ambrosino N. (2017). Aerobic exercise training in very severe chronic obstructive pulmonary disease: a systematic review and meta-analysis. Am. J. Phys. Med. and Rehabilitation 96, 541–548. doi:10.1097/PHM.0000000000000667
Park S., Kim J. K., Choi H. M., Kim H. G., Beekley M. D., Nho H. (2010). Increase in maximal oxygen uptake following 2-week walk training with blood flow occlusion in athletes. Eur. J. Appl. physiology 109, 591–600. doi:10.1007/s00421-010-1377-y
Paton C. D., Addis S. M., Taylor L.-A. (2017). The effects of muscle blood flow restriction during running training on measures of aerobic capacity and run time to exhaustion. Eur. J. Appl. physiology 117, 2579–2585. doi:10.1007/s00421-017-3745-3
Pope Z. K., Willardson J. M., Schoenfeld B. J. (2013). Exercise and blood flow restriction. J. Strength and Cond. Res. 27 (10), 2914–2926. doi:10.1519/JSC.0b013e3182874721
Scott B. R., Loenneke J. P., Slattery K. M., Dascombe B. J. (2015). Exercise with blood flow restriction: an updated evidence-based approach for enhanced muscular development. Sports Med. 45, 313–325. doi:10.1007/s40279-014-0288-1
Silva J. C. G., Pereira Neto E. A., Pfeiffer P. A. S., Neto G. R., Rodrigues A. S., Bemben M. G., et al. (2019). Acute and chronic responses of aerobic exercise with blood flow restriction: a systematic review. Front. physiology 10, 1239. doi:10.3389/fphys.2019.01239
Smith N. D., Scott B. R., Girard O., Peiffer J. J. (2022). Aerobic training with blood flow restriction for endurance athletes: potential benefits and considerations of implementation. J. Strength and Cond. Res. 36 (12), 3541–3550. doi:10.1519/JSC.0000000000004079
Sterne J. A., Savović J., Page M. J., Elbers R. G., Blencowe N. S., Boutron I., et al. (2019). RoB 2: a revised tool for assessing risk of bias in randomised trials. Bmj 366, 14898. doi:10.1136/bmj.l4898
Stojanović E., Ristić V., Mcmaster D. T., Milanović Z. (2017). Effect of plyometric training on vertical jump performance in female athletes: a systematic review and meta-analysis. Sports Med. 47, 975–986. doi:10.1007/s40279-016-0634-6
Takano H., Morita T., Iida H., Asada K.-I., Kato M., Uno K., et al. (2005). Hemodynamic and hormonal responses to a short-term low-intensity resistance exercise with the reduction of muscle blood flow. Eur. J. Appl. physiology 95, 65–73. doi:10.1007/s00421-005-1389-1
Thompson K. M. A., Gamble A. S. D., Kontro H., Lee J. B., Burr J. F. (2024). Low- and high-volume blood-flow restriction treadmill walking both improve maximal aerobic capacity independently of blood volume. Scandinavian. J. Medicine. Science. Sports. 34 (1), e14534. doi:10.1111/sms.14534
Verhagen A. P., De Vet H. C., De Bie R. A., Kessels A. G., Boers M., Bouter L. M., et al. (1998). The Delphi list: a criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. J. Clin. Epidemiol. 51, 1235–1241. doi:10.1016/s0895-4356(98)00131-0
Wang X., Qin X.-M., Ji S., Dong D. (2023a). Effects of resistance training with blood flow restriction on explosive power of lower limbs: a systematic review and meta-analysis. J. Hum. Kinet. 89, 259–268. doi:10.5114/jhk/168308
Wang X., Wang Y., Yang X., Mohd Nasiruddin N. J. B., Dong D., Samsudin S. B., et al. (2023b). Effects of blood flow restriction training on bone metabolism: a systematic review and meta-analysis. Front. Physiology 14, 1212927. doi:10.3389/fphys.2023.1212927
Wang X., Zhang K., Bin Samsudin S., Bin Hassan M. Z., Bin Yaakob S. S. N., Dong D. (2024). Effects of plyometric training on physical fitness attributes in handball players: a systematic review and meta-analysis. J. Sports Sci. Med. 23, 177–195. doi:10.52082/jssm.2024.177
Keywords: blood flow restriction, aerobic training, aerobic capacity, muscle strength, muscle hypertrophy
Citation: Gao Z, Li Y, Zhang J, Li L, Wang T, Wang X and Wang H (2025) Effects of aerobic training with blood flow restriction on aerobic capacity, muscle strength, and hypertrophy in young adults: a systematic review and meta-analysis. Front. Physiol. 15:1506386. doi: 10.3389/fphys.2024.1506386
Received: 05 October 2024; Accepted: 23 December 2024;
Published: 07 January 2025.
Edited by:
Muaz Belviranli, Selçuk University, TürkiyeReviewed by:
Luis Leitão, Instituto Politecnico de Setubal (IPS), PortugalHao-Nan Wang, Sichuan University, China
Copyright © 2025 Gao, Li, Zhang, Li, Wang, Wang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hao Wang, wh8362377@gmail.com; Yan Li, li_yan@lzu.edu.cn
†These authors have contributed equally to this work
 Zhendong Gao
Zhendong Gao