- 1Central American Institute for Studies on Toxic Substances (IRET), Universidad Nacional de Costa Rica, Heredia, Costa Rica
- 2Institute for Family Medicine, Faculty of Medicine, University of Zurich, Zurich, Switzerland
- 3Centro de Investigación y Diagnóstico en Salud y Deporte (CIDISAD-NARS), Escuela Ciencias del Movimiento Humano y Calidad de Vida, Universidad Nacional de Costa Rica, Heredia, Costa Rica
- 4Sport Injury Clinic, Escuela Ciencias del Movimiento Humano y Calidad de Vida, Universidad Nacional de Costa Rica, Heredia, Costa Rica
Editorial on the Research Topic
Acute and Long-term health issues of occupational exposure to heat and high physical loads
In recent years, light has been shed on the dangers of excessive heat and the strenuous demands of physical labor in occupational settings. In the case of heat, some of this attention is driven by increased awareness of climate change, making us more conscious of heat events, which are projected to continue to be more frequent and severe (Intergovernmental Panel on Climate Change, 2023). Unfortunately, some of our awareness also comes from the fact that undesired health outcomes have been documented in working populations (Arbury et al., 2014; Heinzerling et al., 2020; Spector et al., 2023). The same is true for heavy or repetitive movements in the workplace where, despite clear evidence that these exposures can cause severe acute (Lucas et al., 2020) or chronic health outcomes (López-Ruiz et al., 2015), workers continue to be exposed in alarming numbers (Lucas et al., 2020).
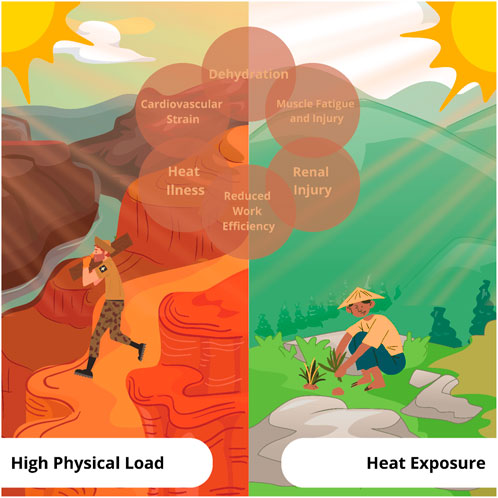
For many populations across the globe, the simultaneous combination of high physical demands, inadequate worker protection measures, and high heat exposure continues to be a major challenge for employers, policymakers and, most of all, workers (Morris et al., 2020). Working in heat, particularly with high physical demands can cause a variety of acute health problems ranging from relatively mild heat illness to a dangerous rise in core body temperature that when left untreated, can have catastrophic outcomes (Sorensen and Hess, 2022). These issues are magnified in populations in the informal sector where individuals often juggle more than one job (Venugopal et al., 2021). Even for those in the formal sector, professions including fire fighters, miners, athletes, agricultural laborers, and soldiers, can be in situations where they are quite literally pushing their bodies’ endurance and resistance to the maximum (Lazaro and Momayez, 2021; Carballo-Leyenda et al., 2022; Kim and Lee, 2023). Occupational heat exposure is associated with a number of undesirable health outcomes ranging from headache and nausea to more severe outcomes such as cardiovascular failure (Ebi et al., 2021) or acute kidney injury (Kupferman et al., 2018; Wesseling et al., 2020). Likewise, heavy or repetitive workloads are associated with outcomes ranging from fatigue to acute or chronic musculoskeletal problems (Briggs et al., 2018). Both heavy workload and heat exposure increase the probability that workers will be injured on the job (Fatima et al., 2021; Morrissey et al., 2023).
This Research Topic casts a wide net, covering a variety of issues that collectively highlight the nuances of workload and heat exposure while also demonstrating the different areas of science that might lead to better understanding of the physiology of heat exposure or ways to combat health effects resulting from that exposure. Each line of research provides a new bit of knowledge, whether it is the identification of novel biomarkers for the early detection of health issues (Schlader et al., 2019; Burtscher et al., 2022) or the creation of workplace regulations and methods that reduce heat stress (Borg et al., 2021; Morris et al., 2021). The investigation of fatigue recovery approaches and cutting-edge body cooling techniques is the rallying cry for innovation that might reduce occupational risk (Douma et al., 2020; Foster et al., 2020). Additionally, the ability to forecast heat exposure in the face of a changing climate and the continual creation of workforce adaptation techniques are essential for a resilient future (Morris et al., 2020; Habibi et al., 2021; Ioannou et al., 2022). Evidence and solutions are still needed to confront the problems that are triggered when there is an interaction between heat exposure and high physical load in occupational populations (e.g., dehydration, heat stress, renal injury) (see Figure 1).
We invited experts from multiple fields to share results related to health issues resulting from acute and prolonged exposure to heat or heavy physical demands resulting in the four original manuscripts published in this Research Topic. The first manuscript contributed by Arbeille et al., delves into the interplay between isolation and physical activity, demonstrating a lack of physiological effects from a 40-day isolation in a cavern, possibly attributed to sustained physical activity and reduced environmental stress. The second manuscript, contributed by Faricier et al., investigates the acute impact of lower-body cold-water immersion on neuromuscular fatigue after high-intensity exercise, revealing that short-term immersion did not significantly alter neuromuscular function during a maximal intensity fatigue task. The third study from Nguyen et al., illuminates the prevalence of neuropathic pain (e.g., spinal and osteoarthritis pain) among Vietnamese industrial workers, identifying several risk factors related to physical load, emphasizing the importance of ergonomic considerations, and noting other risk factors that were more common in those that reported neuropathic pain including noise, dust and heat. Finally, the fourth manuscript submitted by Wang et al., introduces an innovative approach, employing over-the-counter analgesic creams (e.g., 20% methyl salicylate and 6% L-menthol) as potential tools to enhance skin cooling and core body heat loss during exercise-induced hyperthermia.
Collectively, these manuscripts highlight the multidimensionality of the challenges faced by workers subjected to heat exposure and/or demanding physical loads. The diverse spectrum of outcomes discussed - from arterial wall adaptations to neuromuscular function, from neuropathic pain prevalence to skin cooling interventions - underscores the intricate interplay between the physiological and environmental factors influencing occupational health and therefore the diverse fields of science needed to reduce exposure and treat undesired outcomes when they happen.
As we reflect on the four manuscripts included here together with work published elsewhere in recent months, we encourage researchers from diverse backgrounds to continue to study occupational exposure to heat and high physical loads and to consider populations that may face less obvious risk. For example, heat exposure should be researched in populations including professional athletes and indoor workers in places with internal heat sources such as laundry. Similarly, research on high physical demands is needed for workers in confined spaces or unusual settings such as spacecraft. Finally, research is needed on both topics for workers in the informal sector (López-Ruiz et al., 2015; Julià et al., 2019). We hope this Research Topic encourages academics, professionals, and policymakers to pay special attention to occupational exposures to heat and physical load and to act from their areas of expertise in order to pave the way for safer working conditions.
Author contributions
JC: Conceptualization, Methodology, Writing–original draft, Writing–review and editing. BK: Conceptualization, Methodology, Writing–review and editing. DR-V: Conceptualization, Methodology, Writing–original draft, Writing–review and editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Arbury S., Jacklitsch B., Farquah O., Hodgson M., Lamson G., Martin H., et al. (2014). Heat illness and death among workers—United States, 2012–2013. MMWR Morb. Mortal. Wkly. Rep. 63 (31), 661–665.
Borg M. A., Xiang J., Anikeeva O., Pisaniello D., Hansen A., Zander K., et al. (2021). Occupational heat stress and economic burden: a review of global evidence. Environ. Res. 195, 110781. doi:10.1016/j.envres.2021.110781
Briggs A. M., Woolf A. D., Dreinhöfer K., Homb N., Hoy D. G., Kopansky-Giles D., et al. (2018). Reducing the global burden of musculoskeletal conditions. Bull. World Health Organ. 96 (5), 366–368. doi:10.2471/BLT.17.204891
Burtscher J., Vanderriele P.-E., Legrand M., Predel H.-G., Niebauer J., O’Keefe J. H., et al. (2022). Could repeated cardio-renal injury trigger late cardiovascular sequelae in extreme endurance athletes? Sports Med. 52 (12), 2821–2836. doi:10.1007/s40279-022-01734-8
Carballo-Leyenda B., Villa-Vicente J. G., Delogu G. M., Rodríguez-Marroyo J. A., Molina-Terrén D. M. (2022). Perceptions of heat stress, heat strain and mitigation practices in wildfire suppression across southern europe and Latin America. Int. J. Environ. Res. Public Health 19 (19), 19. doi:10.3390/ijerph191912288
Douma M. J., Aves T., Allan K. S., Bendall J. C., Berry D. C., Chang W.-T., et al. (2020). First aid cooling techniques for heat stroke and exertional hyperthermia: a systematic review and meta-analysis. Resuscitation 148, 173–190. doi:10.1016/j.resuscitation.2020.01.007
Ebi K. L., Capon A., Berry P., Broderick C., Dear R. D., Havenith G., et al. (2021). Hot weather and heat extremes: health risks. Lancet 398 (10301), 698–708. doi:10.1016/S0140-6736(21)01208-3
Fatima S. H., Rothmore P., Giles L. C., Varghese B. M., Bi P. (2021). Extreme heat and occupational injuries in different climate zones: a systematic review and meta-analysis of epidemiological evidence. Environ. Int. 148, 106384. doi:10.1016/j.envint.2021.106384
Foster J., Hodder S. G., Goodwin J., Havenith G. (2020). Occupational heat stress and practical cooling solutions for healthcare and industry workers during the COVID-19 pandemic. Ann. Work Expo. Health 64 (9), 915–922. doi:10.1093/annweh/wxaa082
Habibi P., Moradi G., Dehghan H., Moradi A., Heydari A. (2021). The impacts of climate change on occupational heat strain in outdoor workers: a systematic review. Urban Clim. 36, 100770. doi:10.1016/j.uclim.2021.100770
Heinzerling A., Laws R. L., Frederick M., Jackson R., Windham G., Materna B., et al. (2020). Risk factors for occupational heat-related illness among California workers, 2000–2017. Am. J. Ind. Med. doi:10.1002/ajim.23191
Intergovernmental Panel on Climate Change. (2023). IPCC Workshop on the Use of Scenarios in the Sixth Assessment Report and Subsequent Assessments.
Ioannou L. G., Foster J., Morris N. B., Piil J. F., Havenith G., Mekjavic I. B., et al. (2022). Occupational heat strain in outdoor workers: a comprehensive review and meta-analysis. Temperature 9 (1), 67–102. doi:10.1080/23328940.2022.2030634
Julià M., Belvis F., Vives A., Tarafa G., Benach J. (2019). Informal employees in the European Union: working conditions, employment precariousness and health. J. Public Health (Oxford, Engl. 41 (2), e141–e151. doi:10.1093/pubmed/fdy111
Kim D.-H., Lee J.-Y. (2023). Heat strain while wearing pesticide protective clothing in hot environments: effects of textile physical properties and ambient humidity. Int. J. Industrial Ergonomics 93, 103388. doi:10.1016/j.ergon.2022.103388
Kupferman J., Ramírez-Rubio O., Amador J. J., López-Pilarte D., Wilker E. H., Laws R. L., et al. (2018). Acute kidney injury in sugarcane workers at risk for mesoamerican nephropathy. Am. J. Kidney Dis. 72 (4), 475–482. doi:10.1053/j.ajkd.2018.04.014
Lazaro P., Momayez M. (2021). Heat stress in hot underground mines: a brief literature review. Min. Metallurgy Explor. 38 (1), 497–508. doi:10.1007/s42461-020-00324-4
López-Ruiz M., Artazcoz L., Martínez J. M., Rojas M., Benavides F. G. (2015). Informal employment and health status in Central America. BMC Public Health 15 (1), 698. doi:10.1186/s12889-015-2030-9
Lucas D. L., Lee J. R., Moller K. M., O’Connor M. B., Syron L. N., Watson J. R. (2020). Using workers’ compensation claims data to describe nonfatal injuries among workers in Alaska. Saf. Health A. T. Work 11 (2), 165–172. doi:10.1016/j.shaw.2020.01.004
Morris N. B., Jay O., Flouris A. D., Casanueva A., Gao C., Foster J., et al. (2020). Sustainable solutions to mitigate occupational heat strain – an umbrella review of physiological effects and global health perspectives. Environ. Health 19 (1), 95. doi:10.1186/s12940-020-00641-7
Morris N. B., Piil J. F., Morabito M., Messeri A., Levi M., Ioannou L. G., et al. (2021). The HEAT-SHIELD project—perspectives from an inter-sectoral approach to occupational heat stress. J. Sci. Med. Sport 24 (8), 747–755. doi:10.1016/j.jsams.2021.03.001
Morrissey M. C., Kerr Z. Y., Brewer G. J., Tishukaj F., Casa D. J., Stearns R. L. (2023). Analysis of exertion-related injuries and fatalities in laborers in the United States. Int. J. Environ. Res. Public Health 20 (3), 2683. doi:10.3390/ijerph20032683
Schlader Z. J., Hostler D., Parker M. D., Pryor R. R., Lohr J. W., Johnson B. D., et al. (2019). The potential for renal injury elicited by physical work in the heat. Nutrients 11 (9), 9. doi:10.3390/nu11092087
Sorensen C., Hess J. (2022). Treatment and prevention of heat-related illness. N. Engl. J. Med. 387 (15), 1404–1413. doi:10.1056/NEJMcp2210623
Spector J. T., Sampson L., Flunker J. C., Adams D., Bonauto D. K. (2023). Occupational heat-related illness in Washington State: A descriptive study of day of illness and prior day ambient temperatures among cases and clusters, 2006–2021. Am. J. Ind. Med. 66(8), 623–636. doi:10.1002/ajim.23506
Venugopal V., Lennqvist R., Latha P. K., S R., Suraya A., Jakobsson K., Kjellstrom T. (2021). Challenges in conducting epidemiological field studies evaluating associations between heat stress and renal health among workers in informal sectors: Experiences from India. Environ. Res. 200, 111343. doi:10.1016/j.envres.2021.111343
Keywords: work-related injuries, heat, occupational health, physiological stress, heat stress, ergonomics
Citation: Crowe J, Knechtle B and Rojas-Valverde D (2023) Editorial: Acute and long-term health issues of occupational exposure to heat and high physical loads. Front. Physiol. 14:1304229. doi: 10.3389/fphys.2023.1304229
Received: 29 September 2023; Accepted: 04 October 2023;
Published: 11 October 2023.
Edited and reviewed by:
Richard D. Boyle, National Aeronautics and Space Administration (NASA), United StatesCopyright © 2023 Crowe, Knechtle and Rojas-Valverde. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jennifer Crowe, amVubmlmZXIuY3Jvd2VAdW5hLmNy; Daniel Rojas-Valverde, ZHJvamFzdkBob3RtYWlsLmNvbQ==
 Jennifer Crowe
Jennifer Crowe Beat Knechtle
Beat Knechtle Daniel Rojas-Valverde
Daniel Rojas-Valverde