
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Physiol., 03 February 2022
Sec. Clinical and Translational Physiology
Volume 13 - 2022 | https://doi.org/10.3389/fphys.2022.822953
Background: Currently, many systematic reviews (SRs) of moxibustion as a treatment of KOA have been published. However, the evidence of different SRs of moxibustion to treat KOA has not been comprehensively evaluated.
Aim: This overview aimed to evaluate the existing results and provide scientific evidence of the effectiveness and safety of moxibustion in the treatment of KOA.
Methods: We conducted a comprehensive search of Embase, PubMed, Web of Science, Cochrane Library, SinoMed, CNKI, Wanfang, VIP, and other databases until October 31, 2021. A Measurement Tool to Assess Systematic Reviews 2 (AMSTAR-2) was used to assess the methodological quality of SRs. Preferred Reporting Item for Systematic Reviews and Meta-Analyses was used to evaluate the reporting quality, and the risk of bias in SRs was evaluated by ROBIS Tool. We used the Grading of Recommendations Assessment, Development and Evaluation (GRADE) tool to determine the strength of evidence and conducted a meta-analysis of the total effectiveness rate.
Results: Finally, 10 qualified SRs were included, including 57 randomized controlled trials and 5,149 participants. All SRs evaluated by AMASTAR-2 had more than one critical deficiency, so all SRs were rated as critically low. In the PRISMA checklist, the manuscript structures of the included SRs were relatively complete. Including four SRs with a low risk of bias and six with a high risk of bias using the ROBIS tool. In GRADE, two items (6.25%) were rated as high quality, three (9.37%) as medium quality, 17 (53.12%) as low quality and 10 (31.25%) as very low quality. A re-meta-analysis showed that moxibustion and moxibustion combined treatment improved the total effectiveness rate in knee osteoarthritis (risk ratio = 1.17, 95% confidence interval 1.13–1.21, P < 0.001 and risk ratio = 1.13, 95% CI: 1.04–1.23, P < 0.001), with low heterogeneity (I2 = 36.3%, P = 0.020, and I2 = 0.0%, P = 0.956). A total of eight SRs reported adverse events, and no serious adverse events occurred in the moxibustion group and control group.
Conclusion: Moxibustion seems to be effective in treating KOA. Four SRs reported 10 common discomfort symptoms caused by moxibustion, and these adverse events can spontaneously subside, even can be avoided, therefore, moxibustion for KOA appears to be safe. However, the reliability of the results is reduced by the high risk of bias of the original studies and the low methodological quality of SRs. Therefore, future studies should pay more attention to the quality of the original study and the evidence quality of the SRs to provide more powerful and scientific evidence of the effectiveness and safety of moxibustion treatment of KOA.
Osteoarthritis is the most common joint disease in the world, and knee osteoarthritis (KOA) is the most common type with a high disability rate (Vos et al., 2012), and its pathological features are mainly persistent knee pain and dysfunction and degenerative changes of the articular cartilage (Hunter and Bierma-Zeinstra, 2019). Globally, KOA is ranked as the 11th leading cause of disability, with a prevalence rate of 3.8%, and is higher in women than in men (Cross et al., 2014). The prevalence of symptomatic KOA in older Chinese people (≥60 years old) was 19.4% (Xiang and Dai, 2009). Known risk factors for KOA are aging, overweight or obesity, occupational exposure, joint damage, and genetic factors (Wallace et al., 2017; Snoeker et al., 2020). New evidence proves that low-density inflammation is a key mediator in the pathogenesis of OA (Robinson et al., 2016). However, the deeper causes of the high prevalence of KOA remain unclear.
At present, KOA is still incurable, and its primary treatment goals are to relieve pain, improve mobility and walking, improve the quality of life, and slow down its progress when possible (Michael et al., 2010). According to the recommendations of the European League against Rheumatism (EULAR), KOA should be treated conservatively, that is, with a combination of drugs and non-drugs and surgical treatment if necessary, and treatment should be individualized (Pendleton et al., 2000). Non-drug therapy is the basis of drug therapy and surgical treatment. Moxibustion, as a physical therapy, is widely used to treat KOA in Asian countries (Huang et al., 2012b), which is also recommended by the Chinese Medical Association Bone Science Branch (2007).
Evidence from two systematic reviews (SRs) (Li et al., 2016; Song et al., 2016) showed that patients with KOA who received moxibustion obtained greater benefit in pain relief and improved function than those who received conventional care or sham moxibustion. However, there is a gap in the evidence and methodological quality among SRs. Although SRs are important for guiding evidence-based clinical practice, low reporting quality and high-risk SR may mislead clinical decision making. An overview of SRs is a new research method used to assess the quality of multiple SRs and try to resolve inconsistencies in evidence (Smith et al., 2011; Pollock et al., 2016). At present, the scientific quality of different SRs on the moxibustion treatment of KOA has not been comprehensively evaluated. Therefore, we evaluated the existing results through an overview of these SRs and provided scientific evidence of the effectiveness and safety of moxibustion in the treatment of KOA.
We conducted a comprehensive search of the following eight databases: Embase, PubMed, Web of Science, Cochrane Library, SinoMed databases, China National Knowledge Infrastructure, Wanfang and VIP, and selected eligible SRs that had been published as of October 31, 2021. The search terms mainly include “osteoarthritis, knee,” “osteoarthritis,” “knee osteoarthritis,” “KOA,” “OA,” “moxibustion,” “systematic review,” “systematic evaluation,” and “meta-analysis.” The search format was adjusted to suit different databases (Supplementary Material 1). In addition, we manually searched for relevant references for review articles.
SRs based on random control trails (RCTs), moreover, meta-analysis has been used as a statistical method in the SRs to analyze and summarize the results of the included studies. All patients were diagnosed with KOA, regardless of age, sex, course, or severity.
Moxibustion is the main intervention, including all non-intrusive moxibustion (such as traditional moxibustion, indirect moxibustion, heat-sensitive moxibustion, and thunder-fire moxibustion), or moxibustion combined with other treatments.
The studies have compared routine treatment, placebo (sham moxibustion or blank control) or therapies other than moxibustion.
The study included at least one of the following: total effectiveness rate, pain score, Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scale, WOMAC pain score, Lysholm score, 36-Item Short Form Survey (SF-36) scale, and Lequesne index. Because these are the most widely used outcomes to observe the efficacy of KOA. The total effectiveness rate was a compound outcome and total effectiveness rate = (basically cured patients + markedly improved patients + improved patients)/total number of patients (Zhang, 1999).
1. The main intervention was not moxibustion, or the intervention was invasive moxibustion, such as warm-needle moxibustion.
2. SRs of the comparison of different types of moxibustion.
3. Other types of research, such as animal experiments, protocols, conference papers, case reports, and guidelines.
4. Literatures with duplication of data and inaccessibility of the full text.
Two reviewers (SY and ZYH) conducted literature screening independently. All search results were imported into Endnote (X9.3) to remove duplicates, and inconsistent articles were then removed based on their titles and abstracts. Finally, the full text was read, and eligible SRs were included. Unresolved differences were resolved by a third reviewer (FYZ).
Two reviewers (JF and LZ) independently extracted the basic characteristics of the literature, including authors, year of publication, diagnostic criteria, sample size, intervention, comparison, outcomes, adverse effects, and methodological evaluation tool. Two reviewers cross-checked the extracted content and consulted a third reviewer (FYZ) for any differences.
Two reviewers (SY and ZL) used the following four evaluation tools: A Measurement Tool to Assess Systematic Reviews 2 (AMSTAR-2) (Shea et al., 2017; Tao et al., 2018), Preferred Reporting Item for Systematic Reviews and Meta-Analyses (PRISMA) (Liberati et al., 2009), ROBIS tool (Whiting et al., 2016), and Grading of Recommendations Assessment, Development, and Evaluation (GRADE) (Atkins et al., 2004). They independently evaluated the included SRs and then cross-checked. Any differences were resolved through negotiation and unresolvable consultation with a third reviewer (FYZ).
AMSTAR-2 is used to evaluate the methodological quality of the included SR. It contains 16 items, of which 2, 4, 7, 9, 11, 13, and 15 are key items. Then, an overall assessment of SR (high, medium, low, and critically low) is performed based on the evaluation of key items and non-critical items.
PRISMA is used to assess the quality of report, covering 27 items. Each item can be assessed as “yes,” “partial yes,” and “no,” and the rate is listed according to the evaluation of each item.
ROBIS is a tool used to evaluate the risk of bias (RoB) in SR. It is divided into three phases. The first phase is optional, and the second phase consists of four key areas: “study eligibility criteria,” “identification and selection of studies,” “data collection and study appraisal,” and “synthesis and findings.” The third phase is based on the evaluation of the four areas in the second stage for comprehensive evaluation, and the SRs are evaluated as “low risk,” “high risk,” and “unclear risk.”
GRADE is used to evaluate the quality of evidence for results based on five key factors: RoB, inconsistency, indirectness, imprecision, and publication Bias. The quality of evidence is rated as “high,” “moderate,” “low,” and “very low.”
In addition to the descriptive analysis of existing data, we re-analyzed the main outcome to observe the efficacy of moxibustion and combination therapy in the treatment of KOA. Stata15.1 was used in the data analysis, and dichotomous variables are represented by the risk ratio (RR) and 95 confidence interval (CI), if P < 0.05, it means there is a statistical significance. When there is obvious heterogeneity (I2 > 50%), the random-effects model should be used and to explore the source of heterogeneity. Funnel plot and Egger's test were used to detect publication bias, and sensitivity analysis was used to test the stability of the results.
A total of 868 records were retrieved from the database. After removing 482 duplicative items, 351 articles were screened according to the title and abstract, and the full texts of the 35 articles were then evaluated. Finally, 10 SRs of moxibustion treatment of KOA were included (Figure 1). The excluded articles and reasons for exclusions in “full-text assessed for eligibility” are shown in the (Supplementary Material 1).
The 10 included SRs were published between 2016 and 2021, of which two were published in English and the remaining eight were published in Chinese. A total of 57 RCTs and 5,149 participants were included in this overview after duplicates removed (Supplementary Material 2). Each SR included 4–16 RCTs, with sample sizes of 634–1,593 participants. The diagnostic criteria vary: six SRs (Li et al., 2016, 2019; Song et al., 2016; Ma et al., 2017; Wang et al., 2017; Fan et al., 2018) used the diagnostic criteria of the American College of Rheumatology, one SR (Zhang et al., 2017) adopted the guiding principle of clinical research on new drugs in the treatment of KOA and the remaining three SRs (Lu et al., 2019; Deng et al., 2020; Zhang et al.) did not report the basis of diagnostic criteria. Four SRs (Li et al., 2016; Song et al., 2016; Zhang et al., 2017; Lu et al., 2019) reported adverse events in the treatment and control groups, three SRs (Li et al., 2019; Deng et al., 2020; Zhang et al.) only reported adverse events in the control group, one SR (Wang et al., 2017) showed no adverse events and two SRs (Ma et al., 2017; Fan et al., 2018) did not mention adverse events. Regarding the quality assessment of the original studies, the Cochrane risk of bias tool was used for seven SRs (Li et al., 2016, 2019; Song et al., 2016; Ma et al., 2017; Fan et al., 2018; Lu et al., 2019; Zhang et al.), the Jadad scale was used for two SRs (Wang et al., 2017; Zhang et al., 2017) and the Cochrane risk of bias tool plus Jadad scale was used for one SR (Deng et al., 2020). Detailed basic characteristics of the included SRs are shown in Table 1.
AMASTAR-2 was used to assess the methodological quality of the SRs included in this study, and all SRs were rated as having critically low quality due to more than one serious deficiency in critical items 2, 4, 7, 9, 11, 13, and 15 and multiple deficiencies in non-critical items. In critical items, nine SRs (Li et al., 2016, 2019; Song et al., 2016; Wang et al., 2017; Zhang et al., 2017; Fan et al., 2018; Lu et al., 2019; Deng et al., 2020; Zhang et al.) did not specify the registration in advance research project (item 2), all SRs did not provide a comprehensive literature search strategy (item 4) and exclusion and exclusion criteria (item 7). Five SRs (50%) (Song et al., 2016; Ma et al., 2017; Fan et al., 2018; Li et al., 2019; Deng et al., 2020) selected appropriate effect sizes and statistical methods during the meta-analysis and investigated the sources of heterogeneity and reasonable explanations (item 11). Six SRs (60%) (Ma et al., 2017; Zhang et al., 2017; Fan et al., 2018; Li et al., 2019; Deng et al., 2020; Zhang et al.) reported publication bias (item 15). Of the non-critical items, only one SR (10%) (Zhang et al.) explained the reasons for the type of design included in the study (item 3), eight SRs (80%) (Li et al., 2016; Song et al., 2016; Ma et al., 2017; Zhang et al., 2017; Fan et al., 2018; Lu et al., 2019; Deng et al., 2020; Zhang et al.) mentioned that two people independently performed literature screening (item 5) and data extraction (item 6) and one SR (10%) (Lu et al., 2019) reported the source of funding for the included RCTs (item 10). None of the SRs assessed the potential effect of RoB in a single RCT (item 12), five SRs (50%) (Song et al., 2016; Ma et al., 2017; Fan et al., 2018; Li et al., 2019; Deng et al., 2020) had no heterogeneity or did not explain the heterogeneity reasonably (item 14) and two SRs (20%) (Li et al., 2016; Song et al., 2016) claimed no conflict of interest and identified funding sources (item 16). Detailed results are shown in Table 2.
The quality assessment results of the PRISMA checklist are shown in Table 3. The manuscript structures of the SRs included in this overview were relatively complete. The title, introduction and discussion sections have good integrity (100%); however, other sections have some deficiencies. For example, item 5 (protocol and registration), item 8 (search), item 15 (risk of bias across studies), and item 16 (additional analyses) in the abstract (structured summary) and methods and item 23 (additional analysis) in results, all reported incomplete or unreported issues (<50%).
The RoB assessments of SRs included in this overview are shown in Table 4 and Figure 2. Four SRs (40%) were rated as low risk, and six SRs (60%) were rated as high risk through the comprehensive assessment in phase 3. Failure to properly explain and deal with the RoB may lead to high RoB in SR.
Ten SRs included a total of 32 outcomes. The results showed that two (6.25%) were rated as high quality, three (9.37%) as moderate quality, 17 (53.12%) as low quality and 10 (31.25%) as very low quality. RoB (29/32, 90.62%), inconsistency (10/32, 31.25%), and publication bias (26/32, 81.25%) were the main factors for demoting results. Related results are shown in Table 5.
We performed a comprehensive analysis of the seven primary outcomes, as at least two SRs assessed these measures. The seven SRs (Song et al., 2016; Wang et al., 2017; Zhang et al., 2017; Li et al., 2019; Lu et al., 2019; Deng et al., 2020; Zhang et al.) reported that the total effectiveness rate is better in the treatment group than in the control group (P < 0.05). Compared with the control group, the treatment group of five SRs (Ma et al., 2017; Wang et al., 2017; Li et al., 2019; Deng et al., 2020; Zhang et al.) had a better reduction in pain score (P < 0.05), the treatment group of three SRs (Li et al., 2019; Lu et al., 2019; Zhang et al.) had a lower WOMAC pain score (P < 0.05) and the treatment group of two SRs (Ma et al., 2017; Zhang et al.) had a lower WOMAC scale score (P < 0.05). The Lysholm score of three SRs (Wang et al., 2017; Li et al., 2019; Lu et al., 2019) and the Lequesne index of two SRs (Li et al., 2019; Deng et al., 2020) in the treatment group were significantly different from that in the control group (P < 0.05). However, the SF-36 scale showed no significant difference between the treatment group and the control group (Li et al., 2016; Ma et al., 2017). More results are shown in Table 5.
We conducted a meta-analysis on the total effectiveness rate (Song et al., 2016; Wang et al., 2017; Zhang et al., 2017; Fan et al., 2018; Li et al., 2019; Lu et al., 2019; Deng et al., 2020; Zhang et al.). A total of 34 RCTs (2,828 participants) were included after duplicates were removed, meta-analysis results of moxibustion for KOA showed significant homogeneity among all studies (I2 = 36.3%, P = 0.020), the effect of moxibustion on the total effectiveness rate of KOA was better than that of the control group (RR = 1.17, 95% CI: 1.13–1.21, and P < 0.001; Figure 3). The funnel plot and Egger's test showed obvious publication bias (Figure 4), and the sensitivity analysis showed that the results are stable (Supplementary Material 1). The results of the moxibustion combined treatment for KOA showed no heterogeneity (I2 = 0.0%, P = 0.956), moxibustion combined treatment group could better improve the total effectiveness rate of KOA patients compared with the control group (RR = 1.13, 95% CI: 1.04–1.23, P < 0.001, 4 RCTs, and 360 participants; Figure 5).
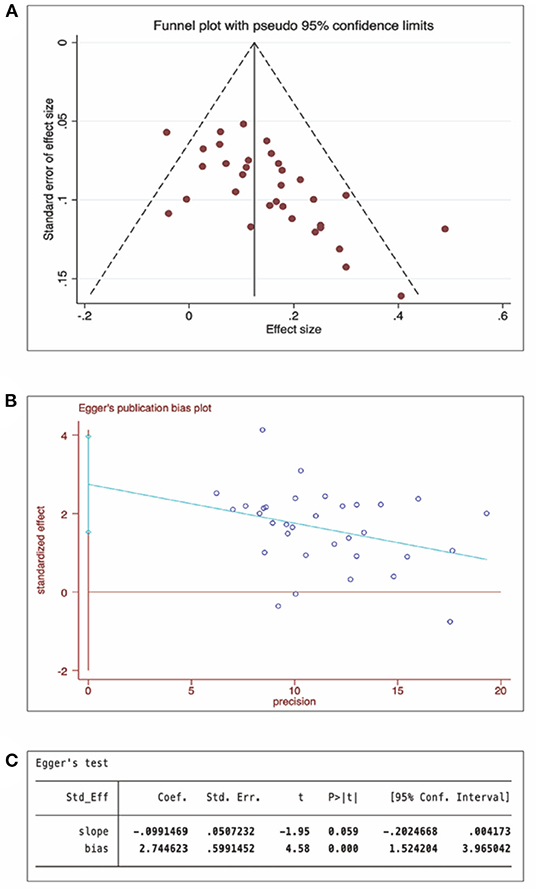
Figure 4. Publication bias of total effectiveness rate (moxibustion for KOA). (A) Funnel plot, (B) Egger's test, and (C) Egger's test P-value.
A total of eight SRs mentioned adverse events, among which four SRs (Li et al., 2016; Song et al., 2016; Zhang et al., 2017; Lu et al., 2019) reported common discomfort symptoms such as blisters, skin flushing, burn wounds, rash and itching, caused by moxibustion. One SR (Zhang et al., 2017) indicated that the symptoms of moxibustion were milder relative to the control group (P < 0.01). Another SR (Deng et al., 2020) conducted a meta-analysis of adverse events, and the results showed that the moxibustion group did not show significant differences when compared with the control group (P > 0.05).
This overview comprehensively evaluated the available evidence from 10 different SRs on the efficacy and safety of moxibustion for KOA and evaluated the quality of methodology and evidence. In the PRISMA checklist, the quality of SRs was relatively good, and the manuscript structures were relatively complete. However, in the GRADE results, the evidence quality was poor, and all SRs evaluated by AMASTAR-2 had more than one critical deficiency, so all SRs were rated as critically low. AMSTAR-2 was updated in 2017, and the two SRs (Li et al., 2016; Song et al., 2016) before that may have biased the evaluation results because they did not conceal some items of AMSTAR-2. Six SRs were rated as having high RoB using the ROBIS tool. Finally, we performed an updated meta-analysis on the total effectiveness rate of the original study. Evidence shows that the moxibustion and moxibustion combined treatment of KOA has a higher total effectiveness rate than the control treatment, and the heterogeneity is low. Although moxibustion and moxibustion combined treatment showed consistent results, the small effect size indicated that the effect was not very significant, and more original studies of higher quality are needed to support this result in the future.
While all SRs appeared to show the benefits of moxibustion, the results of the comprehensive overview were not ideal. We considered two main reasons: (a) The author's report on SR was incomplete, and the neglect of some items directly led to the degradation of the methodological quality. Key items such as early registration protocol, detailed exclusion list and reasonable explanation of bias risk are not stated in the SR. (b) To trace the root of the issue, the quality of the original research was the basis for determining the quality of the SR evidence. We found that each RCT used different criteria. For example, the inclusion criteria of the patients, evaluation of patients' condition, setting of the control group, selection of observation indicators, and other reasons may lead to bias. When RCTs of different criteria are included, the RoB in SR may increase, with high heterogeneity, and precise research results cannot be obtained, which also reduces the credibility of evidence for the moxibustion treatment of KOA to some extent. Therefore, we make the following important suggestions: (a) Regardless of whether it is SR or RCT, it is necessary to follow the relevant literature reporting guidelines [such as the PRISMA checklist (Zhang et al., 2020) and CONSORT statement (Cheng et al., 2013)]. (b) The adoption of internationally agreed diagnostic criteria and the evaluation criteria for effectiveness may reduce heterogeneity. (c) Moxibustion is a non-invasive treatment method, and sham moxibustion devices are often used to verify the specificity of moxibustion in clinical practice. Although sham moxibustion can reduce the skin irritation caused by its warm effect as much as possible (Zhao et al., 2006; Kim et al., 2011), it may still bring false-positive results. Therefore, researchers should pay more attention to the long-term efficacy of moxibustion in the treatment of KOA, increase the follow-up time and verify the specific therapeutic effect of moxibustion. Of the 10 SRS included in this study, a few reported available data during follow-up, and we encourage better study design to maximize scientific evidence of the effectiveness of moxibustion for the treatment of KOA.
As regards outcomes, pain, knee function, and total effectiveness rate are commonly used outcomes in the study of KOA. In evaluating the improvement of KOA pain, visual analog scale (VAS), and numerical rating scale are the two most used scales with excellent retest reliability. Among them, VAS has the highest reliability in measuring KOA pain. Evidence showed that the two scales demonstrated a good correlation (Alghadir et al., 2018). For better statistical analysis, we combined the two indexes into the pain score. WOMAC, Lysholm score, Lequesne index, and SF-36 scale are comprehensive assessment scales with different emphasis. The WOMAC scale is divided into pain, stiffness, and body function, which can effectively evaluate the course and treatment effect in patients with KOA and is widely used (Xie et al., 2008; Collins et al., 2011). The Lysholm score and Lequesne index are commonly used to evaluate the knee function of patients with KOA with high reliability (Nilsdotter and Bremander, 2011; Lecorney et al., 2018; Ahmed et al., 2019). As a general quality of life self-assessment scale, the SF-36 scale is widely used. In this study, two SRs (Li et al., 2016; Ma et al., 2017) reported this outcome, and the results showed that moxibustion had no significant difference in improving the quality of life of patients with KOA compared with the control group. However, whether the SF-36 scale can be used as an evaluation standard for moxibustion to improve the quality of life of patients with KOA remains to be further explored (Li et al., 2003; Lins and Carvalho, 2016). Inconsistent diagnostic criteria for SRs may lead to inconsistent assessment criteria for effectiveness, ultimately affecting the reliability of results.
The traditional Chinese medicine theory believes that the efficacy of moxibustion is based on two aspects: the role of meridians and moxa fire. KOA is one of the common indications for moxibustion (Huang et al., 2012a), and its analgesic mechanism may involve the thermal, radiation and pharmacological effects of moxibustion and its combustion products (Zhu et al., 2017). In addition, moxibustion treatment of KOA involves multiple inflammatory signaling pathways (Zhang et al., 2021). It is also associated with cytokines, matrix metalloproteinases, chondrocytes and other factors (He et al., 2017). Pain is the primary reason for patients with KOA to seek medical attention. Arthritis pain and functional limitation seriously affect the quality of life of patients. Therefore, most studies have regarded the improvement of moxibustion on inflammatory knee pain as the main outcome. Based on existing evidence, moxibustion has great prospects in relieving KOA pain and improving joint function, but its effectiveness still needs to be confirmed by more high-quality RCTs.
Moxibustion is a double-edged sword. Manifestations such as burns, itching, fatigue, blisters, and skin flushing resulting from the moxibustion process are not only the factors of therapeutic effect of moxibustion, but also the main contributing factors of adverse events. However, these adverse events can spontaneously subside, even adverse events such as burns and blisters can be avoided and most patients can accept moxibustion treatment (Ren et al., 2015). The main product of moxibustion is moxa smoke, functioning as antibacterial disinfection, increasing immunity, anti-aging, and regulating blood lipids. However, the concentrations of mono-aromatic hydrocarbons, formaldehyde, and polycyclic aromatic hydrocarbons produced by moxa smoke seriously exceed the standard, which also causes harm to the human body and environment (Mo et al., 2014; Deng et al., 2021). In the main biological pathway of toxic chemical components, high concentrations of moxa smoke are toxic to a certain extent to the heart, liver, and kidney. However, there are no clinical reports of related toxic and side effects; thus, the characteristics of the clinical application of traditional Chinese medicine should be considered comprehensively instead of discussing its toxicity in isolation (Xu, 2021). An RCT compared smokeless moxibustion with conventional moxibustion in the treatment of KOA and showed that moxa smoke did not affect the efficacy of moxibustion in the treatment of KOA but may be limited to patients with moderate KOA pain or functional limitations (Luo et al., 2019). Essentially, the effectiveness and safety of moxibustion for KOA should be fully considered. For patients with KOA of different severities, its effectiveness should be verified. Among the 10 SRs evaluated in this study, we did not obtain data on the patient's condition. From the existing evidence, we still support moxibustion as an effective and safe method to treat KOA.
This overview comprehensively searched relevant literature and comprehensively evaluated the effectiveness and safety of moxibustion in the treatment of KOA by including different moxibustion treatments of KOA based on existing evidence. We reported the quality of reporting, methodological quality, and RoB for SRs using the AMSTAR-2, PRISMA, and ROBIS assessment tools and assessed the quality of evidence of clinical outcomes using GRADE. All assessments involved at least two independent reviewers, thus ensuring the reliability of the overview results as far as possible. Finally, we reconstructed the total effectiveness rate of individual RCTs included in all SRs and showed that acupuncture was effective in treating KOA with stable results.
The study designs of the original literature varied, and the evaluation results of SRs were highly heterogeneous, which may be the primary reason for the degradation of the outcomes. Secondly, the RoB assessment in this study was conducted for a single SR, and we were unable to retrieve all available data from the original study, and the results may not be comprehensive enough. Therefore, this may have hindered the overall evaluation of this study.
This overview suggests that moxibustion seems to be effective in treating KOA. However, the reliability of the results is reduced by the high RoB of the original studies and the low methodological quality of SRs. Thus, we continue to support the value of moxibustion as a non-invasive treatment for KOA. Future studies should pay more attention to the quality of original studies and evidence quality of SR to provide more powerful and scientific evidence for the effectiveness and safety of moxibustion in the treatment of KOA.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
SY and FZ: study conception and design. LL and DC: administrative support. ZL, JF, LZ, and ZH: collection and assembly of data. SY and ZL: data analysis and interpretation. SY and FZ: manuscript writing. All authors: final approval of manuscript. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphys.2022.822953/full#supplementary-material
Ahmed, K. M., Said, H. G., Ramadan, E. K. A., Abd El-Radi, M., and El-Assal, M. A. (2019). Arabic translation and validation of three knee scores, Lysholm Knee Score (LKS), Oxford Knee Score (OKS), and International Knee Documentation Committee Subjective Knee Form (IKDC). Sicot J. 5:6. doi: 10.1051/sicotj/2018054
Alghadir, A. H., Anwer, S., Iqbal, A., and Iqbal, Z. A. (2018). Test-retest reliability, validity, and minimum detectable change of visual analog, numerical rating, and verbal rating scales for measurement of osteoarthritic knee pain. J. Pain Res. 11, 851–856. doi: 10.2147/JPR.S158847
Atkins, D., Eccles, M., Flottorp, S., Guyatt, G. H., Henry, D., Hill, S., et al. (2004). Systems for grading the quality of evidence and the strength of recommendations I: critical appraisal of existing approaches the GRADE Working Group. BMC Health Serv. Res. 4:38. doi: 10.1186/1472-6963-4-38
Cheng, C. W., Fu, S. F., Zhou, Q. H., Wu, T. X., Shang, H. C., Tang, X. D., et al. (2013). Extending the CONSORT Statement to moxibustion. J. Integr. Med. 11, 54–63. doi: 10.3736/jintegrmed2013009
Chinese Medical Association Bone Science Branch (2017). Guidelines for diagnosis and treatment of osteoarthritis (2007 edition). Chin J Orthopaedic Surg. 27, 793–79. doi: 10.3760/j.issn:0253-2352.2007.10.016
Collins, N. J., Misra, D., Felson, D. T., Crossley, K. M., and Roos, E. M. (2011). Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care Res (Hoboken) 63(Suppl. 11), S208–S228. doi: 10.1002/acr.20632
Cross, M., Smith, E., Hoy, D., Nolte, S., Ackerman, I., Fransen, M., et al. (2014). The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann. Rheum. Dis. 73, 1323–1330. doi: 10.1136/annrheumdis-2013-204763
Deng, K.-f., Zhu, Y., Wei, X.-c., Yan, J.-x., Gao, Q., Ma, Y.-l., et al. (2020). Meta analysis of clinical efficacy and safety of thunder fire moxibustion in treatment of knee osteoarthritis. Clin. J. Acupunct. Moxibustion 36, 44–50. doi: 10.3969/j.issn.1005-0779.2020.03.012
Deng, W., Shan, S., Xu, X., Wang, W., Wang, S., and Liu, H. (2021). Effect and safety evaluation of Moxa smoke. World Sci. Technol. 23, 1042–1047. doi: 10.11842/wst.20200511001
Fan, J.-c., Zhang, H.-m., Zhang, M., Men, H.-l., Guo, Q.-q, Li, P.-y., et al. (2018). Cumulative meta-analysis and sequential trial analysis of moxibustion for knee osteoarthritis. J. Nurs. 25, 35–43. doi: 10.16460/j.issn1008-9969.2018.11.035
He, L., Cai, R., Hu, L., Song, X., Wu, Z., Wang, J., et al. (2017). Summary of experimental research on moxibustion for knee osteoarthritis in recent 10 years. J. Yunnan Univ. Tradit. Chin. Med. 40, 94–97. doi: 10.19288/j.cnki.issn.1000-2723.2017.02.022
Huang, Q.-f., Wu, H.-g., Liu, J., and Hong, J. (2012a). Metrological analysis and evaluation of moxibustion disease spectrum in modern literature. Shanghai J. Acupunct. Moxibustion 31, 1–5. doi: 10.3969/j.issn.1005-0957.2012.01.001
Huang, Q.-F., Xie, C., Wu, H.-G., Yang, G., Liu, J., Guo, X.-C., et al. (2012b). Bibliometric analysis of diseases spectrum of moxibustion therapy. Acupunct. Massage Med. 10, 342–348. doi: 10.1007/s11726-012-0633-6
Hunter, D. J., and Bierma-Zeinstra, S. (2019). Osteoarthritis. Lancet 393, 1745–1759. doi: 10.1016/S0140-6736(19)30417-9
Kim, S. Y., Yi, S. H., Cho, J. H., Yin, C. S., Lee, H., and Park, H. J. (2011). Heat stimulation on the skin for medical treatment: can it be controlled? J. Altern. Complement. Med. 17, 497–504. doi: 10.1089/acm.2010.0072
Lecorney, J., Verhoeven, F., Chouk, M., Guillot, X., Prati, C., and Wendling, D. (2018). Correlation between catastrophizing and Lequesne index in case of osteoarthritis of the knee: a prospective study. Joint Bone Spine 85, 605–607. doi: 10.1016/j.jbspin.2017.10.002
Li, A., Wei, Z. J., Liu, Y., Li, B., Guo, X., and Feng, S. Q. (2016). Moxibustion treatment for knee osteoarthritis: a systematic review and meta-analysis. Medicine (Baltimore) 95:e3244. doi: 10.1097/MD.0000000000003244
Li, L., Wang, H. M., and Shen, Y. (2003). Chinese SF-36 Health Survey: translation, cultural adaptation, validation, and normalisation. J. Epidemiol. Community Health 57, 259–263. doi: 10.1136/jech.57.4.259
Li, X.-j., Liu, P., Zhao, L.-n., Jiang, Z.-m., Cai, R.-l., Yu, Q., et al. (2019). Meta-analysis of moxibustion therapy for knee osteoarthritis. J. Hainan Med. Coll. 25, 1723–1730. doi: 10.13210/j.cnki.jhmu.20191025.001
Liberati, A., Altman, D. G., Tetzlaff, J., Mulrow, C., Gøtzsche, P. C., Ioannidis, J. P., et al. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700. doi: 10.1136/bmj.b2700
Lins, L., and Carvalho, F. M. (2016). SF-36 total score as a single measure of health-related quality of life: Scoping review. SAGE Open Med 4:2050312116671725. doi: 10.1177/2050312116671725
Lu, X., Wang, F., Yan, Z., Xuan, Y., and Liu, D. (2019). Systematic evaluation of clinical effect of moxibustion therapy on patients with knee osteoarthritis. Light Tradit. Chin. Med. 34, 1615–1620. doi: 10.3969/j.issn.1003-8914.2019.10.062
Luo, L., Liao, M., Peng, J. X., Ma, Q., Zhou, J. Y., Zhu, L. L., et al. (2019). Comparison of the efficacy between conventional moxibustion and smoke-free moxibustion on knee osteoarthritis: a randomized controlled trial. Evid. Based Complement. Alternat. Med. 2019:1291947. doi: 10.1155/2019/1291947
Ma, X.-r., Chai, Z., Liu, F.-y., and Liu, Y. (2017). Systematic evaluation and meta analysis of moxibustion therapy for knee osteoarthritis. Shanghai J. Tradit. Chin. Med. 51, 19–23+36. doi: 10.16305/j.1007-1334.2017.09.005
Michael, J. W., Schlüter-Brust, K. U., and Eysel, P. (2010). The epidemiology, etiology, diagnosis, and treatment of osteoarthritis of the knee. Dtsch. Arztebl. Int. 107, 152–162. doi: 10.3238/arztebl.2010.0152
Mo, F., Chi, C., Guo, M., Chu, X., Li, Y., and Shen, X. (2014). Characteristics of selected indoor air pollutants from moxibustion. J. Hazard. Mater. 270, 53–60. doi: 10.1016/j.jhazmat.2014.01.042
Nilsdotter, A., and Bremander, A. (2011). Measures of hip function and symptoms: Harris Hip Score (HHS), Hip Disability and Osteoarthritis Outcome Score (HOOS), Oxford Hip Score (OHS), Lequesne Index of Severity for Osteoarthritis of the Hip (LISOH), and American Academy of Orthopedic Surgeons (AAOS) Hip and Knee Questionnaire. Arthritis Care Res (Hoboken) 63(Suppl. 11), S200–S207. doi: 10.1002/acr.20549
Pendleton, A., Arden, N., Dougados, M., Doherty, M., Bannwarth, B., Bijlsma, J. W., et al. (2000). EULAR recommendations for the management of knee osteoarthritis: report of a task force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT). Ann. Rheum. Dis. 59, 936–944. doi: 10.1136/ard.59.12.936
Pollock, M., Fernandes, R. M., Becker, L. A., Featherstone, R., and Hartling, L. (2016). What guidance is available for researchers conducting overviews of reviews of healthcare interventions? A scoping review and qualitative metasummary. Syst. Rev. 5:190. doi: 10.1186/s13643-016-0367-5
Ren, X., Yao, C., Wu, F., Li, Z., Xing, J., and Zhang, H. (2015). Effectiveness of moxibustion treatment in quality of life in patients with knee osteoarthritis: a randomized, double-blinded, placebo-controlled trial. Evid. Based Complement. Alternat. Med. 2015:569523. doi: 10.1155/2015/569523
Robinson, W. H., Lepus, C. M., Wang, Q., Raghu, H., Mao, R., Lindstrom, T. M., et al. (2016). Low-grade inflammation as a key mediator of the pathogenesis of osteoarthritis. Nat. Rev. Rheumatol. 12, 580–592. doi: 10.1038/nrrheum.2016.136
Shea, B. J., Reeves, B. C., Wells, G., Thuku, M., Hamel, C., Moran, J., et al. (2017). AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 358:j4008. doi: 10.1136/bmj.j4008
Smith, V., Devane, D., Begley, C. M., and Clarke, M. (2011). Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med. Res. Methodol. 11:15. doi: 10.1186/1471-2288-11-15
Snoeker, B., Turkiewicz, A., Magnusson, K., Frobell, R., Yu, D., Peat, G., et al. (2020). Risk of knee osteoarthritis after different types of knee injuries in young adults: a population-based cohort study. Br. J. Sports Med. 54, 725–730. doi: 10.1136/bjsports-2019-100959
Song, G. M., Tian, X., Jin, Y. H., Deng, Y. H., Zhang, H., Pang, X. L., et al. (2016). Moxibustion is an alternative in treating knee osteoarthritis: the evidence from systematic review and meta-analysis. Medicine (Baltimore) 95:e2790. doi: 10.1097/MD.0000000000002790
Tao, H., Yang, L., Ping, A., Quan, L.-L., Yang, X., Zhang, Y.-,g, et al. (2018). Interpretation of quality evaluation tool AMSTAR 2 for systematic evaluation of randomized and nonrandomized preventive studies. Chin. J. Evid. Based Med. 18, 101–108. doi: 10.7507/1672-2531.201711005
Vos, T., Flaxman, A. D., Naghavi, M., Lozano, R., Michaud, C., Ezzati, M., et al. (2012). Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380, 2163–2196. doi: 10.1016/S0140-6736(12)61729-2
Wallace, I. J., Worthington, S., Felson, D. T., Jurmain, R. D., Wren, K. T., Maijanen, H., et al. (2017). Knee osteoarthritis has doubled in prevalence since the mid-20th century. Proc. Natl. Acad. Sci. U. S. A. 114, 9332–9336. doi: 10.1073/pnas.1703856114
Wang, Y., Wu, Y.-J., Jing, S.-k., and Chen, L.-j. (2017). Meta analysis of the clinical effect of moxibustion on knee osteoarthritis. Hunan J. Tradit. Chin. Med. 33, 148–151. doi: 10.16808/j.cnki.issn1003-7705.2017.09.070
Whiting, P., Savović, J, Higgins, J. P., Caldwell, D. M., Reeves, B. C., Shea, B., et al. (2016). ROBIS: A new tool to assess risk of bias in systematic reviews was developed. J. Clin. Epidemiol. 69, 225–234. doi: 10.1016/j.jclinepi.2015.06.005
Xiang, Y. J., and Dai, S. M. (2009). Prevalence of rheumatic diseases and disability in China. Rheumatol. Int. 29, 481–490. doi: 10.1007/s00296-008-0809-z
Xie, F., Li, S. C., Goeree, R., Tarride, J. E., O'Reilly, D., Lo, N. N., et al. (2008). Validation of Chinese Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) in patients scheduled for total knee replacement. Qual. Life Res. 17, 595–601. doi: 10.1007/s11136-008-9340-7
Xu, X (2021). Composition Analysis of Moxa Smoke and Its Acute Toxicity to SD Rats [Master's]. Jiangxi University of Traditional Chinese Medicine.
Zhang, F (1999). Summary of the first meeting of the Chinese seminar on evaluation criteria of drug efficacy in the treatment of arthritis. J. Rheumatol. 4, 260–261.
Zhang, H., Yu, L., Wang, L., Wang, X., and Xie, Z. (2021). Research progress of key signaling pathways in knee osteoarthritis. Chin. J. Orthopedics Traumatol. 29, 84–88.
Zhang, R., Zhou, X., and Zhang, Y. (2017). Meta analysis of clinical efficacy and safety of septum moxibustion in treatment of knee osteoarthritis. Chin. Tradit. Med. Emerg. 26, 799–803. doi: 10.3969/j.issn.1004-745X.2017.05.014
Zhang, X., Tan, R., Lam, W. C., Cheng, C. W., Yao, L., Wang, X. Q., et al. (2020). PRISMA extension for moxibustion 2020: recommendations, explanation, and elaboration. Syst. Rev. 9:247. doi: 10.1186/s13643-020-01502-7
Zhang, Y, Dong, X, Yang, Y, and Guan, X Systematic evaluation meta analysis of the clinical effect of thunder fire moxibustion on knee osteoarthritis. J. Liaoning Univ. Tradit. Chin. Med. 1–12. Available online at: http://lib.cdutcm.edu.cn:7001/rwt/CNKI/http/NNYHGLUDN3WXTLUPMW4A/kcms/detail/21.1543.R.20210629.1012.004.htm
Zhao, B., Wang, X., Lin, Z., Liu, R., and Lao, L. (2006). A novel sham moxibustion device: a randomized, placebo-controlled trial. Complement. Ther. Med. 14, 53–60; discussion 1. doi: 10.1016/j.ctim.2005.06.003
Keywords: moxibustion, knee osteoarthritis, overview, systematic reviews, methodological quality
Citation: Yin S, Zhu F, Li Z, Che D, Li L, Feng J, Zhang L and Huo Z (2022) An Overview of Systematic Reviews of Moxibustion for Knee Osteoarthritis. Front. Physiol. 13:822953. doi: 10.3389/fphys.2022.822953
Received: 02 December 2021; Accepted: 12 January 2022;
Published: 03 February 2022.
Edited by:
Johannes Fleckenstein, Goethe University Frankfurt, GermanyReviewed by:
Cuncun Lu, China Academy of Chinese Medical Sciences, ChinaCopyright © 2022 Yin, Zhu, Li, Che, Li, Feng, Zhang and Huo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fengya Zhu, bm90Zm91bmRzQGZveG1haWwuY29t
†ORCID: Fengya Zhu orcid.org/0000-0002-2574-0748
Shao Yin orcid.org/0000-0003-3865-3122
‡These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.