- Department of Hematology, Ningbo First Hospital, Ningbo, China
Multiple myeloma (MM) is the second most common hematological disorder. Although several drugs have been developed to treat MM, their efficacy is uncertain. In addition, how normal physical activities can decrease inflammatory responses and clinical biomarkers in MM patients needs to be better defined. Therefore, this study evaluated possible clinical and inflammatory markers to determine the early diagnosis of MM during physical activity. This study selected 30 MM patients with normal or no physical activity with ages of >50 years. This study did not require any specific exercise protocols other than noting patients’ daily life activities and considering them as physical activity for 17 days. Then, blood samples were collected to assess clinical and inflammatory markers. Regarding clinical markers, daily life activities in MM patients decreased their LDH, calcium, and β2-microglobulin levels significantly compared to other clinical biomarkers such as creatine and total protein. Further, this study observed no significant differences between daily life activities of MM patients and normal MM patients regarding levels of immunoglobulins except IgM. Furthermore, IL-6 level was significantly increased with the daily life activities of MM patients, suggesting the role of physical activities in increasing anti-inflammatory response along with altering the biochemical profiles including LDH, calcium and β2-microglobulin in MM patients.
Introduction
Physical activity and exercise have been linked to improving cancer patients’ quality of life in terms of patient outcomes (Spreafico et al., 2021). This may be due to decreases in body composition, systemic inflammation, and oxidative stress and to increased immune function. Studies have shown that exercise increases the immune response in tumors, and the mechanism behind this may be the increased mobilization of immune cells (Sitlinger et al., 2020; Sitlinger et al., 2022). In addition, lower-to-moderate-intensity exercise decreases the risk of cancers and other chronic diseases, especially because it improves physiological and psychological functions among cancer patients (McTiernan et al., 2018; Morishita et al., 2020). This effect has been documented in several meta-analyses. Further, physical activities and exercise impact cellular and bodily functions, which can reduce the recurrence of cancer and increase the survival capacity of patients (Meyerhardt et al., 2006). However, there are no established mechanisms concerning exercise types and cancer types. Further, how exercise influences biochemical inflammatory parameters in cancer patients has been little studied. Therefore, this study aimed to understand how physical activity influences biochemical and inflammatory parameters in multiple myeloma (MM) patients.
Worldwide, cancer has been diagnosed more than ever before in recent years; this may be due to advancements in early detection and effective treatments, which can also increase survival numbers after diagnosis (Loud and Murphy, 2017). Although the treatment strategy has been supportive in increasing survival, the side effects in patients impact their physiological and psychological functions, such as fatigue, pain, and decreased cardiac efficiency. As mentioned above, physical activity and exercise could effectively overcome these side effects. However, designing protocols for MM patients requires great attention as they have weaker immune systems, suggesting that exercise should be prescribed only to those who are in good condition (Nowrousian et al., 2005; Wefelnberg et al., 2022). Furthermore, MM patients with sedentary lifestyles could develop other conditions, such as obesity, cardiac problems, and osteoarthritis, which can accumulate to put the patients in life-threatening conditions. Therefore, performing physical activities can be worthwhile for patients. The present study considers daily life activities as a way to improve MM patients’ quality of life.
Methods and materials
Study design
This study divided 30 MM patients into two groups—normal physical activities involved group (n = 17) and normal MM patients (n = 13)—and followed 17 days of follow-up programs. On the 17th day, they were all asked to donate their blood samples. Prior consent had been obtained from patients, and the analysis had been accepted by the relevant ethics committee.
Subjects
Every patient seen at the inpatient clinic of the Hematology Department at Ningbo First Hospital from January 2019 to November 2020 was analyzed before treatment. Authorization was acquired from the research ethics board at Ningbo First Hospital (Approval No: 2022RS002). Out of the total 30 patients with MM, 21 females and nine males were selected for blood testing for immunoglobulin profiles, biochemical parameters, and anti-inflammatory markers.
Inclusion criteria
Newly diagnosed cases of MM of age >55 years, who gave informed consent and fulfilled the diagnostic criteria for MM, were included.
Exclusion criteria
Patients who did not give consent were excluded.
Methods
Free light chain assay and biochemical parameter assays
All the biochemicals and immunoglobulins were measured using commercially available kits (total proteins, calcium, creatine, β2-microglobulin, IgG, IgD, IgM, and free light chains) (Anhui Yi Pu Nuo Kang Biotechnology Co. Ltd.).
LDH and IL-6 assessments
Serum LDH and IL-6 levels were measured using commercially available kits (Anhui Yi Pu Nuo Kang Biotechnology Co. Ltd.).
Statistical analysis
Data are expressed as means ± standard deviations (SD). Statistical significance was determined using the non-parametric t-test, and significance was set at p ≤ 0.05. Graph Pad Prism software version 9 was used for all analyses.
Results
Biochemical profiles assist in the early diagnosis of any cancer, and fluctuations in biochemical parameters can impact cancer patients’ health outcomes. Therefore, this study aimed to investigate whether physical activity can influence biochemical parameters such as creatinine, calcium, and total protein levels. This study observed that calcium and β-2 microglobulin levels decreased significantly in MM + PA patients compared to MM patients. This was further reflected in the creatinine levels of the MM + PA patients. However, there were no significant differences observed in total protein levels between MM + PA patients and MM patients (Figure 1).
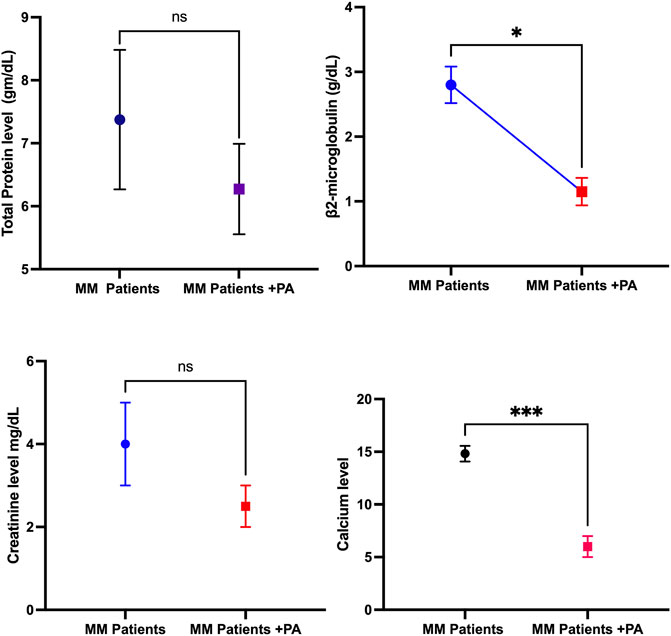
FIGURE 1. Effects of physical activity with MM on biochemical parameters such as total protein, β2-microglobulin, creatinine level, and calcium level.
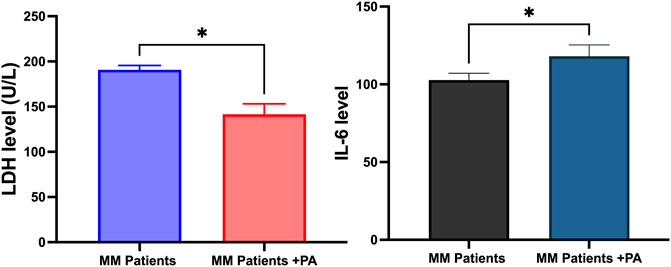
LDH accumulation indicates the onset of MM on rare occasions. The overall survival rate of MM patients is lower in the LDH accumulation state. This study found that LDH levels decreased significantly in the MM + PA patients compared to the MM patients (Figure 2). Interleukin-6 level is linked with MM severity and tumor cell mass. This study observed that MM + PA patients had increased IL-6 levels compared to MM patients (Figure 2).
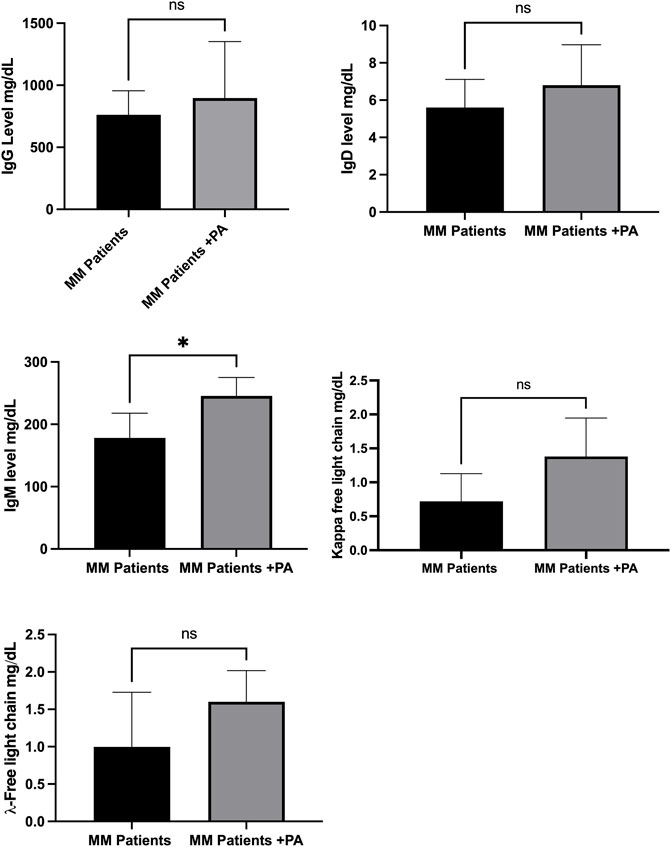
Figure 3 shows that MM patients involved in normal physical activities had no changes in levels of antibodies, such as IgD, IgG, kappa, and lambda free light chains compared to MM patients with no activities. However, the IgM level was significantly increased in the MM + PA group compared to the MM group.
Discussion
Physical activities and moderate exercise have improved cancer patients’ quality of life, including in MM. However, different treatments and their side effects and co-morbidities hinder the prescribing or performing of exercise for gaining the full benefits of exercise in improving cancer patients’ quality of life (Teke et al., 2014). Proper exercise may improve survivorship among patients. LDH level is correlated with MM disease progression. Studies have showed increased LDH in MM onset and disease progression (Barlogie et al., 1989; Terpos et al., 2010). This may be due to increased tumor mass. This study observed that normal physical activities decreased the LDH level relative to the MM patients, suggesting the role of physical activities in decreasing LDH levels. At the same time, daily activities increased IL-6 levels in the MM patients, suggesting the possible effect of physical activities in improving anti-inflammatory response in the MM patients. Studies have linked IL-6 with increasing the pathogenesis of the MM condition by preventing the MM cells from undergoing apoptosis, suggesting that targeting IL-6 could be an effective strategy for reducing tumorigenesis (Gadó et al., 2000). In contrast, other studies have shown that IL-6 activates, proliferates, and increases the survival rates of lymphocytes during the immune response, suggesting a dual face of IL-6 in regulating various signaling pathways in the tumor microenvironment (Fisher et al., 2014). In this way, physical activities reshape the IL-6 pathways from negative to positive effects for improving MM conditions, possibly interfering with oxidative stress pathways.
High calcium levels are linked with MM, possibly due to an increase in bone destruction that can release calcium into the blood. Also, abnormal functions of the parathyroid gland can cause an imbalance of calcium levels in MM patients. This study observed a decrease in calcium levels in the MM + PA group compared to the MM patients. This is also partially reflected by the small decrease in creatine levels in the MM + PA patients compared to the MM patients. Several studies have reported that increased calcium levels increase blood creatinine (Faiman et al., 2011; Martínez Mateu et al., 2011; Cheng et al., 2021). However, this is not reflected in total protein levels. Studies have reported that increased calcium levels do not implicate an increase in total protein levels. This may be due to hypercalcemia with metastatic osteolytic carcinoma; in this scenario, protein levels are normal (Gutman and Gutman, 1936).
The types of MM are categorized according to the production of immunoglobulins, and MM plasma cells can produce monoclonal immunoglobulins, which are inefficient in fighting infection. This study observed that daily life activities had an impact on increasing levels of immunoglobulins such as IgM. Studies have shown that exercise increases immunoglobulin, which may be due to exercise-induced immune activation or immunoglobulin redistribution (Campbell et al., 2016). Similarly, this study shows that daily activities can induce immune activation by increasing IgM levels. However, other immunoglobulins were also increased, suggesting that better differentiation of all these immunoglobulins under physical exercise conditions is required, as they can be produced by both normal and MM cells.
Conclusion
In conclusion, MM patients involved in normal physical activities had increased immune stimulation, as confirmed by increases in IgM and other immunoglobulins. MM patients also had decreased levels of calcium and creatine, suggesting that daily physical activities may increase quality of life and increase immune stimulation in MM patients. However, this study had some limitations, such as determining the type or duration of physical activity among the patients and minimal sampling, which can obscure the complete effects of exercise and physical activity. Therefore, further studies are warranted to prescribe exercise and physical activities as the main tools to improve the patient’s quality of life.
Data availability statement
The original contributions presented in the study are included in the article and supplementary material, and further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Ningbo First Hospital, Ningbo, China. The patients/participants provided their written informed consent to participate in this study.
Author contributions
Conceptualization and manuscript writing: JW; data curation: LS and GO; manuscript editing: ZX. All the authors fully read the manuscript and agreed to its final format.
Funding
This study was supported by the Science and Technology Foundation of Zhejiang (China), under award No. LGF2H080002.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Barlogie B., Smallwood L., Smith T., Alexanian R. (1989). High serum levels of lactic dehydrogenase identify a high-grade lymphoma-like myeloma. Ann. Intern. Med. 110 (7), 521–525. doi:10.7326/0003-4819-110-7-521
Campbell J. P., Eijsvogels T. M., Wang Y., Hopman M. T., Jacobs J. F. (2016). Assessment of serum free light chain levels in healthy adults immediately after marathon running. Clin. Chem. Lab. Med. 54 (3), 459–465. doi:10.1515/cclm-2015-0431
Cheng J., Zhang W., Zhao Y., Li X., Lv R., Li H., et al. (2021). Association of serum calcium levels with renal impairment and all-cause death in Chinese patients with newly diagnosed multiple myeloma: A cross-sectional, longitudinal study. Nutr. Metab. 18 (1), 19. doi:10.1186/s12986-020-00525-0
Faiman B. M., Mangan P., Spong J., Tariman J. D. (2011). Renal complications in multiple myeloma and related disorders: Survivorship care plan of the international myeloma foundation nurse leadership board. Clin. J. Oncol. Nurs. 15, 66–76. doi:10.1188/11.CJON.S1.66-76
Fisher D. T., Appenheimer M. M., Evans S. S. (2014). The two faces of IL-6 in the tumor microenvironment. Semin. Immunol. 26 (1), 38–47. doi:10.1016/j.smim.2014.01.008
Gadó K., Domján G., Hegyesi H., Falus A. (2000). Role of INTERLEUKIN-6 in the pathogenesis of multiple myeloma. Cell. Biol. Int. 24 (4), 195–209. doi:10.1006/cbir.2000.0497
Gutman A. B., Gutman E. B. (1936). Calcium-protein relation in hyperproteinemia: Total and diffusible serum calcium in lymphogranuloma inguinale and myeloma. Exp. Biol. Med. (Maywood). 35 (3), 511–515. doi:10.3181/00379727-35-9033c
Loud J. T., Murphy J. (2017). Cancer screening and early detection in the 21st century. Semin. Oncol. Nurs. 33 (2), 121–128. doi:10.1016/j.soncn.2017.02.002
Martínez Mateu J. G., Losada González G. P., Munar Vila M. A., Uriol Rivera M., Gómez Marqués G., Tugores A. C. (2011). [Multiple myeloma, severe hypercalcaemia, acute renal failure and multiple organ failure due to calcinosis]. Nefrologia 31 (2), 233–234. doi:10.3265/Nefrologia.pre2010.Nov.10668
McTiernan A., Friedenreich C. M., Katzmarzyk P. T., Powell K. E., Macko R., Buchner D., et al. (2018). Physical activity in cancer prevention and survival: A systematic review. Med. Sci. Sports Exerc. 51 (6), 1252–1261. doi:10.1249/MSS.0000000000001937
Meyerhardt J. A., Giovannucci E. L., Holmes M. D., Chan A. T., Chan J. A., Colditz G. A., et al. (2006). Physical activity and survival after colorectal cancer diagnosis. J. Clin. Oncol. 24 (22), 3527–3534. doi:10.1200/JCO.2006.06.0855
Morishita S., Hamaue Y., Fukushima T., Tanaka T., Fu J. B., Nakano J. (2020). Effect of exercise on mortality and recurrence in patients with cancer: A systematic review and meta-analysis. Integr. Cancer Ther. 19, 1534735420917462. doi:10.1177/1534735420917462
Nowrousian M. R., Brandhorst D., Sammet C., Kellert M., Daniels R., Schuett P., et al. (2005). Serum free light chain analysis and urine immunofixation electrophoresis in patients with multiple myeloma. Clin. Cancer Res. 11 (24 Pt 1), 8706–8714. doi:10.1158/1078-0432.CCR-05-0486
Sitlinger A., Brander D. M., Bartlett D. B. (2020). Impact of exercise on the immune system and outcomes in hematologic malignancies. Blood Adv. 4 (8), 1801–1811. doi:10.1182/bloodadvances.2019001317
Sitlinger A., Deal M. A., Garcia E., Connelly M., Thompson D., Stewart T., et al. (2022). Associations of clinical and circulating metabolic biomarkers with low physical fitness and function in adults with chronic lymphocytic leukemia. Front. Oncol. 12, 933619. doi:10.3389/fonc.2022.933619
Spreafico F., Barretta F., Murelli M., Chisari M., Gattuso G., Terenziani M., et al. (2021). Positive impact of organized physical exercise on quality of life and fatigue in children and adolescents with cancer. Front. Pediatr. 9, 627876. doi:10.3389/fped.2021.627876
Terpos E., Katodritou E., Roussou M., Pouil A., Michalis E., Delimpasi S., et al. (2010). High serum lactate dehydrogenase adds prognostic value to the international myeloma staging system even in the era of novel agents. Eur. J. Haematol. 85 (2), 114–119. doi:10.1111/j.1600-0609.2010.01466.x
Teke Ü., Başak M., Teke D., Kanbay M. (2014). Serum level of lactate dehydrogenase is a useful clinical marker to monitor progressive multiple myeloma diseases: A case report. Turk. J. Haematol. 31 (1), 84–87. doi:10.4274/Tjh.2013.0044
Keywords: physical activity, inflammation, multiple myeloma, antibodies, free light chains
Citation: Wang J, Sheng L, Lai Y, Ouyang G and Xu Z (2023) Effects of physical activity on clinical and inflammatory markers in diagnosing multiple myeloma patients. Front. Physiol. 13:1094470. doi: 10.3389/fphys.2022.1094470
Received: 10 November 2022; Accepted: 02 December 2022;
Published: 04 January 2023.
Edited by:
Anand Thirupathi, Ningbo University, ChinaReviewed by:
Kalaiselvan Ashokan, MV Hospital for Diabetes, IndiaVijayakumar Mayakrishnan, Sejong University, South Korea
Copyright © 2023 Wang, Sheng, Lai, Ouyang and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiaping Wang, Y2hlcnJ5amlhcGluZzg4QDE2My5jb20=
 Jiaping Wang
Jiaping Wang Lixia Sheng
Lixia Sheng Yanli Lai
Yanli Lai