
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
EDITORIAL article
Front. Physiol., 16 September 2022
Sec. Exercise Physiology
Volume 13 - 2022 | https://doi.org/10.3389/fphys.2022.1030871
This article is part of the Research TopicExercise and Heart FailureView all 5 articles
 Elisabetta Salvioni1*
Elisabetta Salvioni1* Stefania Paolillo2
Stefania Paolillo2 Carlo Vignati1
Carlo Vignati1 Damiano Magrì3
Damiano Magrì3 Massimo Mapelli1,4
Massimo Mapelli1,4 Piergiuseppe Agostoni1,4
Piergiuseppe Agostoni1,4Editorial on the Research Topic
Exercise and Heart Failure
Heart failure (HF) is a complex disease that plagues public health with a still very high degree of mortality regardless of ejection fraction: reduced (HFrEF) or preserved (HFpEF) (Owan et al., 2006). The study of exercise physiology is of crucial importance to define the functional status of HF patients, to estimate prognosis, to guide therapy as well as to plan a possible rehabilitation program. In fact, exercise limitation is one of the cardinal symptoms of the patient with HF, not only in the case of maximal exertion, but also with regard to activities of daily living whose limitation negatively affects quality of life (Wilson and Mancini, 1993; Mapelli et al., 2020).
The driver of exercise is the metabolic cost coupled by the hemodynamic and respiratory response, so that the jamming of one of the “gears” participating in this complex mechanism is actually the main cause of the disease.
The most important parameter for measuring exercise capacity is oxygen uptake (VO2), which, according to Fick’s law, depends on cardiac output and arteriovenous oxygen content difference.
Therefore, at a first glance exercise limitation is basically due to insufficient or delayed supply of O2 to the muscle, and in particular to the mitochondria. The proper delivery of oxygen to exercising muscles mitochondria basically depends on three variables: O2 delivery, pO2 reduction from arteries to capillaries, and O2 diffusion from capillaries to the mitochondrion (Wagner, 1992; Wagner, 1996; Rovai et al., 2021).
The complex adjustment of these three factors is exemplified by Wagner’s diagram (Wagner, 1996; Rovai et al., 2021) (Figure 1), which shows:
-O2 delivery changes as a result of altered cardiac output, due to exercise induced cardiac output increase, redistribution of blood flow and hemoconcentration;
-pO2 reduction depending on O2 flow from the capillary to mitochondria which on its turn depends on the pO2 differences between capillaries and mitochondria and resistance to O2 flow;
-O2 diffusion from capillaries to the mitochondrion, which depends on length (distance from capillary to the mitochondria) and resistance to O2 flow due to fibrosis, cells, and whatever is located between capillaries and mitochondria.
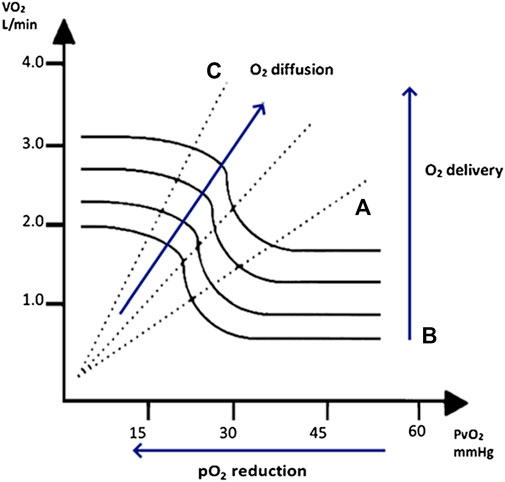
FIGURE 1. On the left, the relation between the O2 venous pressure (PvO2) and oxygen uptake (VO2) represented by Wagner diagram with the trend of O2 diffusion, O2 delivery, and O2 pression (pO2) reduction. During exercise VO2 increases by three independent mechanisms: (A) increase in O2 delivery (exercise-induced cardiac output increase and hemoconcentration (bold lines); (B) pO2 reduction in the capillary bed (X axis); and (C) differences in O2 diffusion from the capillary to the mitochondria (dashed lines). Reproduced with permission from Rovai et al., 2021 (Rovai et al., 2021).
The complexity of this system and the interdependence among the factors involved make the study of exercise physiology in the decompensated patient a difficult and heterogeneous task.
The articles collected in this Research Topic address this issue from different points of view.
Aerobic training is commonly used to improve patients exercise capacity. The randomized trial proposed by Gasser et al., will explore the field of exercise pathophysiology in HFpEF patients, whose diagnosis is still difficult and the underlying mechanisms not fully elucidated. As a consequence, also the rehabilitation programs need to be compared in an objective manner in this context, considering the pathophysiological mechanisms involved and their effectiveness. Specifically, the study aims to compare high-intensity interval training vs. moderate continuous training and it will focus not only on exercise capacity, but also on disease-specific blood biomarkers, cardiac and arterial vessel structure and function, total hemoglobin mass, metabolic requirements, habitual physical activity, and quality of life.
The paper by Paneroni et al. also fits into the landscape of studies of rehabilitation programs in patients with chronic HF. Here the authors proposed a novel approach to evaluate program effectiveness, using a battery of standardized activities of daily living, evaluated before and after the rehabilitation program. This strategy is particularly interesting because it evaluates performance based on activities that the patients perform in their normal life. Therefore, improvement is measured on activities well-known by the patient and most effectively reflects changes in their quality of life, mirroring exercises from everyday. From a physiological point of view cardiac rehabilitation involves all the three components of the Wagner diagram.
Differently, Wagner et al. work is based on the complex study of exercise physiology in a ramp protocol cardiopulmonary test, thus using a kind of exercise that is far away from every day activities, but, on the other hand, is highly controlled. Specifically, it focuses on the analysis of physiology, delving into the more complex mechanisms involved in the kinetics of exercise used as a mirror reflecting the efficiency of the system (i.e., the organism) in performing the effort. The authors found particularly meaningful the VO2 kinetic from the end of exercise to recovery transition, following ramp test termination (off-kinetics), a parameter that can be used as an alternative to peak VO2 when it is not reliable. We have no definite data to report on the original Wagner diagram (Figure 1) the time related changes of these variables involved in the VO2 kinetic of exercise recovery, but it is intriguing to speculate that O2 delivery reduction, i.e., mainly cardiac output and its distribution, is slowed down in HF patients compared to normal subjects, keeping VO2 reduction deferred.
The fourth paper by Aleksova et al. included in this Research Topic is a Review outlining the changes at the molecular level induced by exercise and the drugs available to modify these processes. Thus, in this case the study of HF exercise is done from a biomolecular perspective, analyzing the potentials expressed by different types of exercises, available programs, exercise-induced biological modifications, and additional complications due to concomitant conditions (e.g., vitamin D deficiency).
Taken together, the articles collected in this Research Topic show how broad the spectrum of analysis of HF and its relationship to exercise capacity is. Thus, there is no doubt that a great deal of work is still needed to investigate the different aspects, from the more molecular ones, to the physiology, to what can be considered a more “practical” approach. It is in fact of crucial importance to translate the application of the results obtained in the laboratory in the patient’s daily life, thus not stopping at the fundamental result of improving prognosis, but also focusing on everyday patients’ quality of life, considering the data obtained on the ability to perform efforts on a daily basis.
The evidence gathered draws attention to the importance of studying exercise as an expression of the patient’s ability to perform activity and thus a great indicator of their health and well-being, which is what really matters from a patient’s point of view. Moreover, the presented evidences further support the need to consider exercise as an indicator of the results achieved through drug therapy, as well as to consider physical activity a therapy itself.
ES, PA Drafted the manuscript. SP, CV, DM, and MM critically revised the text. All authors agree to be accountable for the content of the work.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Mapelli M., Salvioni E., Bonomi A., Gugliandolo P., De Martino F., Vignati C., et al. (2020). How patients with heart failure perform daily life activities: An innate energy-saving strategy. Circ. Heart Fail. 13, e007503. doi:10.1161/CIRCHEARTFAILURE.120.007503
Owan T. E., Hodge D. O., Herges R. M., Jacobsen S. J., Roger V. L., Redfield M. M. (2006). Trends in prevalence and outcome of heart failure with preserved ejection fraction. N. Engl. J. Med. 355, 251–259. doi:10.1056/NEJMoa052256
Rovai S., Mattavelli I., Salvioni E., Corra U., Cattadori G., Campodonico J., et al. (2021). Exercise dynamic of patients with chronic heart failure and reduced ejection fraction. Curr. Cardiol. Rep. 23, 92. doi:10.1007/s11886-021-01491-6
Wagner P. D. (1996). Determinants of maximal oxygen transport and utilization. Annu. Rev. Physiol. 58, 21–50. doi:10.1146/annurev.ph.58.030196.000321
Wagner P. D. (1992). Gas exchange and peripheral diffusion limitation. Med. Sci. Sports Exerc. 24, 54–58. doi:10.1249/00005768-199201000-00010
Keywords: heart failure, exercise, exercise physiology, oxygen uptake, quality of life
Citation: Salvioni E, Paolillo S, Vignati C, Magrì D, Mapelli M and Agostoni P (2022) Editorial: Exercise and heart failure. Front. Physiol. 13:1030871. doi: 10.3389/fphys.2022.1030871
Received: 29 August 2022; Accepted: 31 August 2022;
Published: 16 September 2022.
Edited and reviewed by:
Giuseppe D'Antona, University of Pavia, ItalyCopyright © 2022 Salvioni, Paolillo, Vignati, Magrì, Mapelli and Agostoni. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elisabetta Salvioni, ZWxpc2FiZXR0YS5zYWx2aW9uaUBjY2ZtLml0
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.