
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Physiol., 21 January 2022
Sec. Exercise Physiology
Volume 12 - 2021 | https://doi.org/10.3389/fphys.2021.803102
This article is part of the Research TopicExercise Physiology and its Role in Chronic Disease Prevention and Treatment - Mechanisms and InsightsView all 17 articles
Background: Previous studies have found that aerobic exercise was more effective in improving vascular endothelial function than resistance training, high-intensity interval training (HIIT), and other types of exercise, while the effects between different intensities and durations of aerobic exercise were unclear. Therefore, we performed this meta-analysis to investigate the effects of different intensities and durations of aerobic exercise on the vascular endothelial function of middle-aged and elderly people.
Methods: Databases were searched up to April 2021 for studies evaluating the influences of different intensities and durations of aerobic exercise on endothelial function assessed by flow-mediated dilation (FMD) among healthy middle-aged and elderly people. Data were pooled using random-effects models to obtain the weighted mean difference (WMD) and 95% confidence intervals (CIs).
Results: A total of 9 studies involving 221 participants fulfilled the inclusion criteria. Aerobic exercise improved the overall FMD of healthy middle-aged and elderly people [WMD, 1.33 (95% CI, 0.37–2.28), P < 0.05]. Specifically, vigorous-intensity exercise increased FMD significantly in healthy middle-aged and elderly people [WMD, 1.10 (95% CI, 0.27–1.93), P < 0.05], while moderate-intensity exercise had no significant association with FMD [WMD, 1.49 (95% CI, −0.62 to 3.60), P = 0.17]. In addition, long-term (8 weeks or above) aerobic exercise increased the FMD in healthy middle-aged and elderly people [WMD, 1.63 (95% CI, 0.61–2.66), P < 0.05], while one-time acute aerobic exercise had no significant association with FMD of healthy middle-aged and elderly people [WMD, 0.89 (95% CI, −1.47 to 3.24), P = 0.46]. Specifically, 8 weeks or above of vigorous-intensity exercise increased FMD significantly in healthy middle-aged and elderly people [WMD, 1.48 (95% CI, 1.06–1.90), P < 0.01], while 8 weeks or above of moderate aerobic exercise had no significant association with FMD [WMD, 1.49 (95% CI, −0.62 to 3.60), P = 0.17].
Conclusion: Aerobic exercise, especially 8 weeks or above of vigorous-intensity aerobic exercise, improved the endothelial function in healthy middle-aged and elderly people.
Aging is an inevitable cardiovascular risk factor, and the increase in age will make the body more susceptible to pathological stress (Tian and Li, 2014) and increase the prevalence of various cardiovascular diseases (CVD) include arteriosclerosis, hypertension, stroke, and so on (North and Sinclair, 2012). Vascular endothelial cells are a single layer of cells adjacent to the lumen of blood vessels and play an important role in the regulation of vascular tone and the maintenance of hemodynamics (Jia et al., 2019), which can directly act on various cardiovascular and peripheral vascular diseases (Rajendran et al., 2013). Endothelium dysfunction, especially impaired endothelium-dependent vasodilation, has been linked to arterial stiffness, atherosclerosis, coronary artery disease, and so on (Ungvari et al., 2018). Flow-mediated dilation (FMD) of the brachial artery is currently used as a parameter in evaluating vasodilation (Thijssen et al., 2019) and is used to predict the risk of cardiovascular diseases in clinic studies, independently, which provides us with a non-invasive method to assess vascular endothelial function. In addition, the risk of CVD will increase 13% following every 1% reduction in brachial artery FMD (Inaba et al., 2010; Ras et al., 2013; Xu et al., 2014; Matsuzawa et al., 2015; Thijssen et al., 2019).
It is well-known that endothelial function is age-dependent (Ungvari et al., 2018). The epidemiologic study has shown that regular exercise can prevent CVD and reduce cardiovascular morbidity and mortality in the general population, especially healthy subjects (Eckel et al., 2014; Arnett et al., 2019; Seals et al., 2019). Therefore, this study pays more attention to the impact of aerobic exercise on improving vascular endothelial function in middle-aged and elderly people. Preliminary research suggested that aerobic exercise had a better effect than other types of exercise in improving vascular endothelial function and reducing the risk of CVD (Zhao et al., 2014; Boeno et al., 2020). The main mechanism was that aerobic exercise can improve the bioavailability of nitric oxide and reduce oxidative stress (Seals et al., 2019). However, some studies found that FMD does not always increase with the continuous training of 8–12 weeks (Tinken et al., 2010; Birk et al., 2012; Green et al., 2014; Green and Smith, 2018), which prompted that time characteristic was a key role. In addition, different aerobic exercise intensities have different effects on vascular endothelial function (Yoo et al., 2017; Green and Smith, 2018). In conclusion, there was not a unanimous result on the influence of different intensities and different durations of aerobic exercise on vascular endothelial function (Goto et al., 2003; Man et al., 2020). Therefore, we performed this meta-analysis to explore the effects of different intensities and durations of aerobic exercise on vascular endothelial function in healthy middle-aged and elderly people.
This meta-analysis was reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher et al., 2015).
All the studies before April 2021 on aerobic exercise to improve the vascular endothelial function in middle-aged and elderly people were searched in PubMed and Web of Science, using the following MESH terms and text words: aerobic exercise, middle-aged, elderly people, and vascular endothelial function. We also hand-searched reference lists of all identified studies. All studies used for meta-analysis need to meet the following criteria: (1) the participants were healthy middle-aged and elderly people; (2) the intervention used in the study was aerobic exercise; (3)FMD was used for evaluating vascular endothelial function. Articles were excluded if the language was non-English or using an animal model. Reviews and conference articles were also excluded from the analysis. As Li et al. (2021) reported, middle-aged and elderly people was defined as people ≥45 years old.
The documental information of all qualified studies includes author information, participant characteristics (including sex distribution), age, training type, training intervention duration, training intensity, training frequency, time of one training, and research result indicators (FMD). Two reviewers (QY and LY) independently reviewed the titles, abstracts, and full texts of all citations to identify studies reporting the effects of aerobic exercise on vascular endothelial function in healthy middle-aged and elderly people. When the data could not be extracted or there was a dispute, two authors negotiated or contacted the author of the article to resolve it. Otherwise, the platform was used to extract the information (WebPlotDigitizer., 2021).
The Cochrane collaboration bias tool, which includes items on selection bias, performance bias, detection bias, attrition bias, and reporting bias, was used to evaluate the quality of eligible studies.
Data were pooled using random-effects models to obtain the weighted mean difference (WMD) and 95% confidence intervals (CIs). When analyzing whether aerobic exercise could improve the vascular endothelial function of healthy elderly people, the Chi-square (χ2) test was used. If there was a high level of heterogeneity in the test (I2 > 60%), we used subgroup analysis or sensitivity analysis to explain the results (Moher et al., 2015; Shamseer et al., 2015). In the subgroup analysis, we tried to use different intensities and durations of aerobic exercise to explore the impact on vascular endothelial function. The analysis result, funnel plot, and forest chart were generated using the software RevMan.5. In terms of overall impact, P < 0.05 was considered statistically significant.
The literature search results and research selection process were shown in Figure 1. Among the 1,426 articles identified, after reading the titles and abstracts, and then reading the full texts, 9 studies were considered eligible for meta-analysis (Nishiwaki et al., 2011; Pierce et al., 2011; Schaun et al., 2011; Akazawa et al., 2012; Swift et al., 2014; Serviente et al., 2016; Hunter et al., 2018; Bouaziz et al., 2019; Klonizakis et al., 2020).
The main characteristics of participants and exercise interventions were shown in Table 1. Nine studies involved 221 participants, of which 5 studies directly explored the effects of aerobic exercise on vascular endothelial function (Schaun et al., 2011; Akazawa et al., 2012; Swift et al., 2014; Serviente et al., 2016; Bouaziz et al., 2019), 4 studies explored factors related to aerobic exercise and endothelial function (Nishiwaki et al., 2011; Pierce et al., 2011; Schaun et al., 2011; Serviente et al., 2016), these articles contained perimenopausal women and postmenopausal women (Nishiwaki et al., 2011; Pierce et al., 2011; Akazawa et al., 2012; Swift et al., 2014; Serviente et al., 2016; Hunter et al., 2018; Bouaziz et al., 2019; Klonizakis et al., 2020), only one article discussed all men (Schaun et al., 2011). According to the position statement of physical activity and training intensity (Norton et al., 2010), we adjusted the intensity classification of aerobic exercise according to the included research situation: 1.6 < METs <3, 20% < maximal oxygen uptake (VO2max) <40%, 40% < maximal heart rate (HRmax) <55%, or 8 < RPE <10 were determined as light-intensity; 3 < METs <6, 40% < VO2max <60%, 55% < HRmax <70%, or 11 < RPE <13 were determined as moderate-intensity; 6 < METs <9, 60% < VO2max <85%, 70% < HRmax <90%, or 14 < RPE <16 were determined as vigorous intensity.
Cochrane risk assessment tool was used to evaluate the methodological quality of the included literature, mainly from six aspects: selection bias, performance bias, detection bias, attrition bias, reporting bias, and other bias (Figure 2). The quality score was made according to three levels (low risk, high risk, and unclear). The quality of the included literature was divided into three levels from high to low: high quality, medium quality, and low quality (Figure 2). Publication bias was assessed visually by inspecting the funnel plot (Figure 3).
After analyzing the data of all included studies, we found that aerobic exercise could increase the FMD of healthy middle-aged and elderly people. However, this increase did not distinguish between exercise intensities and durations. As shown in Figure 4, aerobic exercise increased the FMD significantly [WMD, 1.33 (95% CI, 0.37–2.28), P < 0.05], while there was a significant heterogeneity (I2 = 85%, Figure 4).
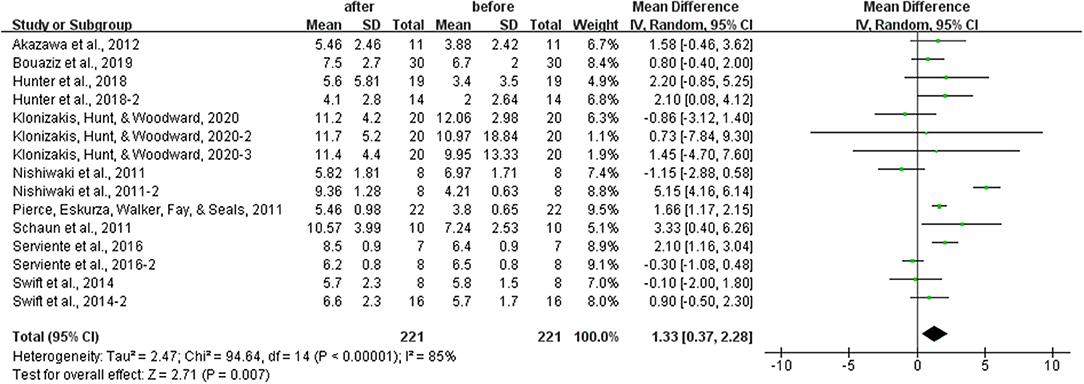
Figure 4. Meta-analysis results of the effects of aerobic exercise on the FMD in healthy middle-aged and elderly people. The pooled estimates were obtained from random effects analysis. Diamonds indicated the effect size of each study summarized as WMD. The size of the shaded squares was proportional to the percentage weight of each study. Horizontal lines represented the 95% CI and the vertical line represented the overall effect. Aerobic exercise improved FMD significantly [WMD, 1.33 (95% CI, 0.37–2.28), P < 0.05].
Different results were shown when considering exercises intensities. Specifically, vigorous-intensity exercise increased the FMD significantly [WMD, 1.10 (95% CI, 0.27–1.93), P < 0.05], while moderate-intensity exercise had no significant association with FMD in healthy middle-aged and elderly people [WMD, 1.49 (95% CI, −0.62 to 3.60), P = 0.17]. However, both subgroups had significant heterogeneity (I2 = 77% and I2 = 87%, respectively; Figure 5).
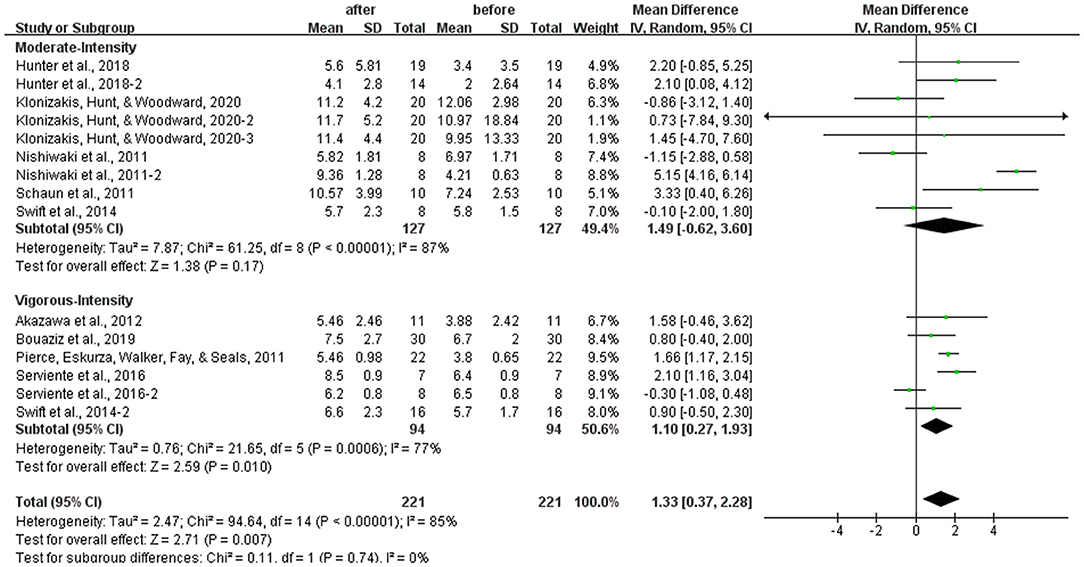
Figure 5. Meta-analysis of the effects of different intensities of aerobic exercise on the FMD in healthy middle-aged and elderly people. The pooled estimates were obtained from random effects analysis. Diamonds indicated the effect size of each study summarized as WMD. The size of the shaded squares was proportional to the percentage weight of each study. Horizontal lines represented the 95% CI and the vertical line represented the overall effect. Moderate-intensity aerobic exercise had no significant relationship with FMD in the middle-aged and elderly people [WMD, 1.49 (95% CI, −0.62 to 3.60), P = 0.17], while vigorous-intensity aerobic exercise improved FMD significantly [WMD, 1.10 (95% CI, 0.27–1.93), P < 0.05].
The subgroup analysis of different durations of aerobic exercise showed that long-term (8 weeks or above) aerobic exercise increased the FMD significantly [WMD, 1.63 (95% CI, 0.61–2.66], P < 0.01], which had a significant heterogeneity (I2 = 80%, Figure 6). However, one-time acute exercise had no significant associations with FMD in healthy middle-aged and elderly people [WMD, 0.89 (95% CI, −1.47 to 3.24), P = 0.46], which had a significant heterogeneity (I2 = 93%, Figure 6).
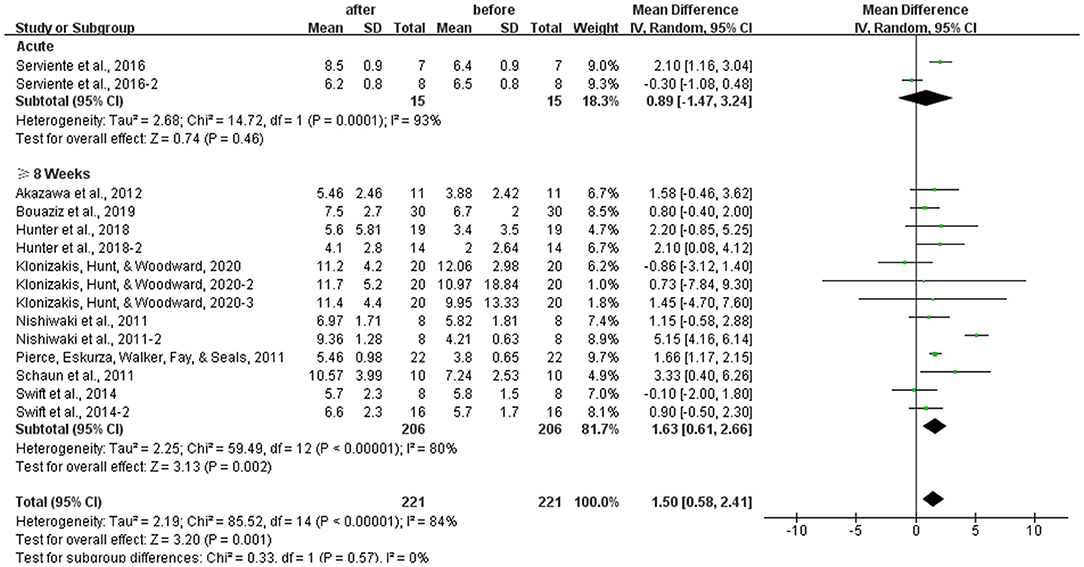
Figure 6. Meta-analysis of the effects of different durations of aerobic exercise on the FMD in healthy middle-aged and elderly people. The pooled estimates were obtained from random effects analysis. Diamonds indicated the effect size of each study summarized as WMD. The size of the shaded squares was proportional to the percentage weight of each study. Horizontal lines represented the 95% CI and the vertical broken line represented the overall effect. One-time acute aerobic exercise had no significant associations with FMD in healthy middle-aged and elderly people [WMD, 0.89 (95% CI, −1.47 to 3.24), P = 0.46], while 8 weeks or above of aerobic exercise improved FMD significantly in the middle-aged and elderly people [WMD, 1.63 (95% CI, 0.61–2.66), P < 0.05].
In the study, we compared the effects of 8 weeks or above of moderate-intensity aerobic exercise and vigorous-intensity aerobic exercise on the FMD, and our results showed that 8 weeks or above of moderate-intensity aerobic exercise had no effect on the FMD in healthy middle-aged and elderly people [WMD, 1.49 (95% CI, −0.62 to 3.60), P = 0.17], which had a significant heterogeneity (I2 = 87%, Figure 7). However, 8 weeks or above of vigorous-intensity aerobic exercise increased the FMD significantly in healthy middle-aged and elderly people [WMD, 1.48 (95% CI, 1.06–1.90), P < 0.01}, with no evidence of heterogeneity (I2 = 0%, Figure 7).
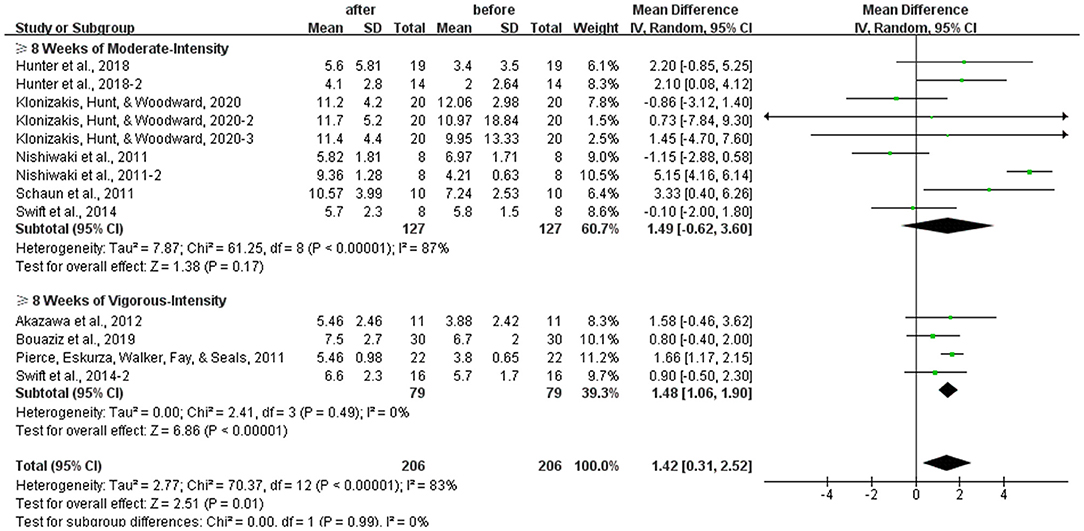
Figure 7. Meta-analysis of the effects of different intensities of 8 weeks or above of aerobic exercise on the FMD in healthy middle-aged and elderly people. The pooled estimates were obtained from random effects analysis. Diamonds indicated the effect size of each study summarized as WMD. The size of the shaded squares was proportional to the percentage weight of each study. Horizontal lines represented the 95% CI and the vertical broken line represented the overall effect. Eight weeks or above of moderate-intensity aerobic exercise had no association with the FMD in healthy middle-aged and elderly people [WMD, 1.49 (95% CI, −0.62 to 3.60), P = 0.17], while 8 weeks or above of vigorous-intensity aerobic exercise significantly improved FMD in middle-aged and elderly people [WMD, 1.48 (95% CI, 1.06–1.90), P < 0.01].
Our meta-analysis showed that aerobic exercise, especially different intensities and durations, significantly improved vascular endothelial function in healthy middle-aged and elderly people, as expressed by increased FMD. Noteworthy, 8 weeks or above of vigorous-intensity aerobic exercise significantly increased FMD in healthy middle-aged and elderly people. However, our meta-analysis did not provide adequate evidence on which exercise intensity was superior in improving vascular endothelial function, since subgroup analysis failed to show significant difference between vigorous-intensity and moderate-intensity. At the same time, it was obvious that aerobic exercise improved vascular endothelial function by increasing the FMD, requiring more proper exercise intensity and longer exercise duration.
Our study showed that aerobic exercise contributed to an overall improvement in the FMD by 1.33%, which was of clinical importance for healthy middle-aged and elderly people. According to previous studies, the increase of the FMD was positively correlated with the reduction of the risk of CVD, which will decrease 13% following every 1% increase in brachial artery FMD (Inaba et al., 2010; Ras et al., 2013; Xu et al., 2014; Matsuzawa et al., 2015; Thijssen et al., 2019). Therefore, we could conclude that people who participated in aerobic exercise for a longer time (8 weeks or above) had better effects on vascular function than those who did not participate in aerobic exercise regularly. The lifestyle of long-term aerobic exercise might provide a protective mechanism for middle-aged and elderly people to slow down the rate of vascular degeneration. Although the mechanism of aerobic exercise improving vascular endothelial function had not been fully revealed, it was speculated that the beneficial effect of exercise on endothelial function might be strengthened through the following mechanisms.
Firstly, there might be a dose-response relationship between vascular endothelial function and aerobic exercise intensity and duration in healthy middle-aged and elderly people. Our results showed that vigorous-intensity exercise increased the FMD significantly, while moderate-intensity exercise had no significant association with FMD in healthy middle-aged and elderly people, which suggested that higher exercise intensity was more effective in improving FMD. Aerobic exercise could produce an increase in blood flow, thus increasing the shear stress on the endothelium to increase the synthesis and bioavailability of nitric oxide (NO) (Simmons et al., 2011; Reynolds et al., 2021), as different intensities of aerobic exercise could produce different arterial pressure, blood flow, and shear stress patterns (Green and Smith, 2018), the improvements of vascular function and vascular remodeling were more obvious in higher intensity aerobic exercise (Tinken et al., 2010; Birk et al., 2012). Ramos et al. (2015) showed that higher intensity aerobic exercise had a greater effect on the endothelial function in adults than moderate-intensity continuous aerobic exercise, which was consistent with our study. In addition, Rakobowchuk et al. (2008) observed the FMD was significantly improved after 6 weeks of 65% VO2peak (vigorous) intensity aerobic exercise, which was also consistent with our study. However, another study reported that both moderate-intensity and vigorous-intensity had a beneficial effect on improving vascular endothelial function (Islam et al., 2021). Therefore, further prospective and intervention studies were needed.
Furthermore, exercise intensity could not explain the improved vascular endothelial function alone, as the acute aerobic exercise of both moderate-intensity and vigorous-intensity did not affect improving the FMD. Harris et al. (2008) found that acute low-intensity (25% VO2max), moderate-intensity (50% VO2max), and vigorous-intensity (75% VO2max) did not influence the FMD response, which suggested that the dose-response relationship of aerobic exercise and vascular endothelial function was dependent not only on the intensity of exercise but also on the duration of exercise.
Secondly, aerobic exercise could reduce the expression of oxidative stress and pro-inflammatory molecules (Teixeira-Lemos et al., 2011). It was reported that regular aerobic exercise could enhance men's vascular endothelial function by reducing oxidative stress and maintaining the bioavailability of NO, which were the factors of endothelial dysfunction (Yoo et al., 2017; Seals et al., 2019). Aerobic exercise could help to restore the function of endothelial progenitor cells, promote endothelial repair, and then promote angiogenesis (Koutroumpi et al., 2012). However, these reactions required a certain exercise intensity and duration, which provided a new idea for increasing the FMD through aerobic exercise to improve vascular endothelial function and prevent CVD. Our results showed that 8 weeks or above of vigorous-intensity aerobic exercise improved the FMD significantly, which suggested that exercise duration was an important factor in improving vascular endothelial function in middle-aged and elderly people. However, this improvement was not observed in acute vigorous-intensity aerobic, and it might be caused by the following aspects. On the one hand, age-related endothelial damage could be prevented by long-time aerobic exercise through improving vascular endothelial function. And the mechanisms included changes in blood flow conditions, increases in blood flow, blood flow speed, and shear stress, and reduces in reactive oxygen species (ROS) production (DeSouza et al., 2000; Taddei et al., 2000), thereby increasing the bioavailability of NO in the vascular endothelium, maintaining vascular homeostasis (Simmons et al., 2011; Reynolds et al., 2021), delaying the rate of vascular degeneration (DeSouza et al., 2000), and finally having an effect on the prevention of age-induced endothelial dysfunction. On the other hand, the role of NO in the endothelium was unlikely to produce a response in a single skeletal muscle exercise (Gilligan et al., 1994), which was consistent with our results.
Third, according to previous studies, the FMD returned to normal after 60 min of acute exercise in elderly men, while postmenopausal women were not affected by vigorous-intensity exercise (Yoo et al., 2017; Seals et al., 2019), which suggested that sex affected the response of the FMD to aerobic exercise in middle-aged and elderly people. Reviewing our study, the heterogeneities in the subgroup might be related to the impaired vascular endothelial function in women perimenopausal or postmenopausal, since the impaired vascular endothelial function was more pronounced in perimenopausal women, which was more common in postmenopausal women with estrogen deficiency (Moreau et al., 2012). Previous study showed that compared with postmenopausal women, only perimenopausal women had improved vascular endothelial function under acute aerobic exercise (Serviente et al., 2016), which might be due to severe vascular endothelial damage caused by estrogen deficiency in postmenopausal women. Moreau et al. (2013) found that 12 weeks of moderate-intensity aerobic exercise could improve the FMD of postmenopausal women who received estradiol hormone therapy during exercise intervention, while FMD improvement was not seen in the postmenopausal women who did not receive estradiol hormone therapy during exercise intervention. The result of moderate-intensity aerobic exercise could not improve vascular endothelial function in postmenopausal women with estrogen deficiency was contrary to a previous study. Santos-Parker et al. (2017) reported that moderate-intensity aerobic exercise improved vascular endothelial function significantly in healthy middle-aged and elderly men, which suggested that estrogen had a protective effect on vascular endothelial function (Taddei et al., 1996). Estrogen could improve the damaged vascular endothelial function by increasing the bioavailability of NO, reducing endothelin-1 (ET-1), and generating vasodilatation to promote endothelial healing and increase angiogenesis (Mendelsohn and Karas, 2005; Chakrabarti et al., 2008). Furthermore, previous studies showed that despite the impaired vascular endothelial function, aerobic exercise could still improve the FMD significantly (Black et al., 2009; Green and Smith, 2018). However, at least 65%-80% HRmax and longer exercise duration were required (Moreau et al., 2012), which was also consistent with our results. Therefore, we believed that it was necessary to strengthen exercise stimulation (intensity, duration, or the volume of aerobic exercise) to continuously improve the vascular endothelial function of middle-aged and elderly women, which was consistent with the opinion of Seals et al. (2019).
This study comes with a few limitations that should be taken into consideration. In the process of literature quality evaluation, subjective factors might cause a certain deviation, and there might be some differences in the FMD measurement methods as it was reported that peak expansion measurement cuff release might lead to an underestimation of the real FMD by up to 40% after 60 s (Black et al., 2008), even though this factor seemed to have little impact on the results of the FMD, and these methods were generally well-defined. In addition, only one study on acute exercise was included in the meta-anlysis, it might cause bias to the comparison of exercise duration.
In summary, this meta-analysis indicated that aerobic exercise, especially 8 weeks or above of vigorous-intensity aerobic exercise, improved the endothelial function in healthy middle-aged and elderly people.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
QY and LY contributed to literature search, figures, study design, data analysis, data interpretation, and writing. GL and HH contributed to data interpretation and writing. YL contributed to study design, figures, data analysis, data interpretation, and writing. All authors contributed to the article and approved the submitted version.
LY was supported by Chinese Universities Scientific Fund (2021QN001). GL was supported by Graduate Students' Innovative Scientific Research Program of Beijing Sport University (20212011).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Akazawa, N., Choi, Y., Miyaki, A., Tanabe, Y., Sugawara, J., Ajisaka, R., et al. (2012). Curcumin ingestion and exercise training improve vascular endothelial function in postmenopausal women. Nutr. Res. 32, 795–799. doi: 10.1016/j.nutres.2012.09.002
Arnett, D. K., Blumenthal, R. S., Albert, M. A., Buroker, A. B., Goldberger, Z. D., et al. (2019). 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J. Am. Coll. Cardiol. 74, e177–e232. doi: 10.1016/j.jacc.2019.03.010
Birk, G. K., Dawson, E. A., Atkinson, C., Haynes, A., Cable, N. T., Thijssen, D. H., et al. (2012). Brachial artery adaptation to lower limb exercise training: role of shear stress. J. Appl. Physiol. 112, 1653–1658. doi: 10.1152/japplphysiol.01489.2011
Black, M. A., Cable, N. T., Thijssen, D. H., and Green, D. J. (2008). Importance of measuring the time course of flow-mediated dilatation in humans. Hypertension 51, 203–210. doi: 10.1161/HYPERTENSIONAHA.107.101014
Black, M. A., Cable, N. T., Thijssen, D. H., and Green, D. J. (2009). Impact of age, sex, and exercise on brachial artery flow-mediated dilatation. Am. J. Physiol. Heart Circ. Physiol. 297, H1109–1116. doi: 10.1152/ajpheart.00226.2009
Boeno, F. P., Ramis, T. R., Munhoz, S. V., Farinha, J. B., Moritz, C. E. J., Leal-Menezes, R., et al. (2020). Effect of aerobic and resistance exercise training on inflammation, endothelial function and ambulatory blood pressure in middle-aged hypertensive patients. J. Hypertens. 38, 2501–2509. doi: 10.1097/hjh.0000000000002581
Bouaziz, W., Lang, P. O., Schmitt, E., Leprêtre, P. M., Lefebvre, F., Momas, C., et al. (2019). Effects of a short-term interval aerobic training program with recovery bouts on vascular function in sedentary aged 70 or over: a randomized controlled trial. Arch. Gerontol. Geriatr. 82, 217–225. doi: 10.1016/j.archger.2019.02.017
Chakrabarti, S., Lekontseva, O., and Davidge, S. T. (2008). Estrogen is a modulator of vascular inflammation. IUBMB Life 60, 376–382. doi: 10.1002/iub.48
DeSouza, C. A., Shapiro, L. F., Clevenger, C. M., Dinenno, F. A., Monahan, K. D., Tanaka, H., et al. (2000). Regular aerobic exercise prevents and restores age-related declines in endothelium-dependent vasodilation in healthy men. Circulation 102, 1351–1357. doi: 10.1161/01.cir.102.12.1351
Eckel, R. H., Jakicic, J. M., Ard, J. D., de Jesus, J. M., Houston Miller, N., Hubbard, V. S., et al. (2014). 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 63(25 Pt B), 2960–2984. doi: 10.1016/j.jacc.2013.11.003
Gilligan, D. M., Panza, J. A., Kilcoyne, C. M., Waclawiw, M. A., Casino, P. R., and Quyyumi, A. A. (1994). Contribution of endothelium-derived nitric oxide to exercise-induced vasodilation. Circulation 90, 2853–2858. doi: 10.1161/01.cir.90.6.2853
Goto, C., Higashi, Y., Kimura, M., Noma, K., Hara, K., Nakagawa, K., et al. (2003). Effect of different intensities of exercise on endothelium-dependent vasodilation in humans: role of endothelium-dependent nitric oxide and oxidative stress. Circulation 108, 530–535. doi: 10.1161/01.CIR.0000080893.55729.28
Green, D. J., Eijsvogels, T., Bouts, Y. M., Maiorana, A. J., Naylor, L. H., Scholten, R. R., et al. (2014). Exercise training and artery function in humans: nonresponse and its relationship to cardiovascular risk factors. J. Appl. Physiol. 117, 345–352. doi: 10.1152/japplphysiol.00354.2014
Green, D. J., and Smith, K. J. (2018). Effects of exercise on vascular function, structure, and health in humans. Cold Spring Harb Perspect Med. 8:a029819. doi: 10.1101/cshperspect.a029819
Harris, R. A., Padilla, J., Hanlon, K. P., Rink, L. D., and Wallace, J. P. (2008). The flow-mediated dilation response to acute exercise in overweight active and inactive men. Obesity 16, 578–584. doi: 10.1038/oby.2007.87
Hunter, S. D., Laosiripisan, J., Elmenshawy, A., and Tanaka, H. (2018). Effects of yoga interventions practised in heated and thermoneutral conditions on endothelium-dependent vasodilatation: the Bikram yoga heart study. Exp. Physiol. 103, 391–396. doi: 10.1113/ep086725
Inaba, Y., Chen, J. A., and Bergmann, S. R. (2010). Prediction of future cardiovascular outcomes by flow-mediated vasodilatation of brachial artery: a meta-analysis. Int. J. Cardiovasc. Imaging 26, 631–640. doi: 10.1007/s10554-010-9616-1
Islam, R. A., Khalsa, S. S. S., Vyas, A. K., and Rahimian, R. (2021). Sex-specific impacts of exercise on cardiovascular remodeling. J. Clin. Med. 10:3833. doi: 10.3390/jcm10173833
Jia, G., Aroor, A. R., Jia, C., and Sowers, J. R. (2019). Endothelial cell senescence in aging-related vascular dysfunction. Biochim. Biophys. Acta Mol. Basis Dis. 1865, 1802–1809. doi: 10.1016/j.bbadis.2018.08.008
Klonizakis, M., Hunt, B. E., and Woodward, A. (2020). The association between cardiovascular function, measured as FMD and CVC, and long-term aquatic exercise in older adults (ACELA Study): a cross-sectional study. Front. Physiol. 11:603435. doi: 10.3389/fphys.2020.603435
Koutroumpi, M., Dimopoulos, S., Psarra, K., Kyprianou, T., and Nanas, S. (2012). Circulating endothelial and progenitor cells: evidence from acute and long-term exercise effects. World J. Cardiol. 4, 312–326. doi: 10.4330/wjc.v4.i12.312
Li, M., Yun, H., Huang, J., Wang, J., Wu, W., Guo, R., et al. (2021). Hair selenium content in middle-aged and elderly Chinese population. Biol. Trace Elem. Res. 199, 3571–3578. doi: 10.1007/s12011-020-02482-4
Man, A. W. C., Li, H., and Xia, N. (2020). Impact of lifestyles (diet and exercise) on vascular health: oxidative stress and endothelial function. Oxid. Med. Cell Longev. 2020:1496462. doi: 10.1155/2020/1496462
Matsuzawa, Y., Kwon, T. G., Lennon, R. J., Lerman, L. O., and Lerman, A. (2015). Prognostic value of flow-mediated vasodilation in brachial artery and fingertip artery for cardiovascular events: a systematic review and meta-analysis. J. Am. Heart Assoc. 4:2270. doi: 10.1161/JAHA.115.002270
Mendelsohn, M. E., and Karas, R. H. (2005). Molecular and cellular basis of cardiovascular gender differences. Science 308, 1583–1587. doi: 10.1126/science.1112062
Moher, D., Shamseer, L., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., et al. (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 4:1. doi: 10.1186/2046-4053-4-1
Moreau, K. L., Hildreth, K. L., Meditz, A. L., Deane, K. D., and Kohrt, W. M. (2012). Endothelial function is impaired across the stages of the menopause transition in healthy women. J. Clin. Endocrinol. Metab. 97, 4692–4700. doi: 10.1210/jc.2012-2244
Moreau, K. L., Stauffer, B. L., Kohrt, W. M., and Seals, D. R. (2013). Essential role of estrogen for improvements in vascular endothelial function with endurance exercise in postmenopausal women. J. Clin. Endocrinol. Metab. 98, 4507–4515. doi: 10.1210/jc.2013-2183
Nishiwaki, M., Kawakami, R., Saito, K., Tamaki, H., Takekura, H., and Ogita, F. (2011). Vascular adaptations to hypobaric hypoxic training in postmenopausal women. J. Physiol. Sci. 61, 83–91. doi: 10.1007/s12576-010-0126-7
North, B. J., and Sinclair, D. A. (2012). The intersection between aging and cardiovascular disease. Circ. Res. 110, 1097–1108. doi: 10.1161/CIRCRESAHA.111.246876
Norton, K., Norton, L., and Sadgrove, D. (2010). Position statement on physical activity and exercise intensity terminology. J. Sci. Med. Sport 13, 496–502. doi: 10.1016/j.jsams.2009.09.008
Pierce, G. L., Eskurza, I., Walker, A. E., Fay, T. N., and Seals, D. R. (2011). Sex-specific effects of habitual aerobic exercise on brachial artery flow-mediated dilation in middle-aged and older adults. Clin. Sci. 120, 13–23. doi: 10.1042/cs20100174
Rajendran, P., Rengarajan, T., Thangavel, J., Nishigaki, Y., Sakthisekaran, D., Sethi, G., et al. (2013). The vascular endothelium and human diseases. Int. J. Biol. Sci. 9, 1057–1069. doi: 10.7150/ijbs.7502
Rakobowchuk, M., Tanguay, S., Burgomaster, K. A., Howarth, K. R., Gibala, M. J., and MacDonald, M. J. (2008). Sprint interval and traditional endurance training induce similar improvements in peripheral arterial stiffness and flow-mediated dilation in healthy humans. Am. J. Physiol. Regul. Integr. Comp. Physiol. 295, R236–242. doi: 10.1152/ajpregu.00069.2008
Ramos, J. S., Dalleck, L. C., Tjonna, A. E., Beetham, K. S., and Coombes, J. S. (2015). The impact of high-intensity interval training versus moderate-intensity continuous training on vascular function: a systematic review and meta-analysis. Sports Med. 45, 679–692. doi: 10.1007/s40279-015-0321-z
Ras, R. T., Streppel, M. T., Draijer, R., and Zock, P. L. (2013). Flow-mediated dilation and cardiovascular risk prediction: a systematic review with meta-analysis. Int. J. Cardiol. 168, 344–351. doi: 10.1016/j.ijcard.2012.09.047
Reynolds, J. C., Lai, R. W., Woodhead, J. S. T., Joly, J. H., Mitchell, C. J., Cameron-Smith, D., et al. (2021). MOTS-c is an exercise-induced mitochondrial-encoded regulator of age-dependent physical decline and muscle homeostasis. Nat. Commun. 12:470. doi: 10.1038/s41467-020-20790-0
Santos-Parker, J. R., Strahler, T. R., Vorwald, V. M., Pierce, G. L., and Seals, D. R. (2017). Habitual aerobic exercise does not protect against micro- or macrovascular endothelial dysfunction in healthy estrogen-deficient postmenopausal women. J. Appl. Physiol. 122, 11–19. doi: 10.1152/japplphysiol.00732.2016
Schaun, M. I., Dipp, T., Rossato Jda, S., Wilhelm, E. N., Pinto, R., Rech, A., et al. (2011). The effects of periodized concurrent and aerobic training on oxidative stress parameters, endothelial function and immune response in sedentary male individuals of middle age. Cell Biochem. Funct. 29, 534–542. doi: 10.1002/cbf.1781
Seals, D. R., Nagy, E. E., and Moreau, K. L. (2019). Aerobic exercise training and vascular function with ageing in healthy men and women. J. Physiol. 597, 4901–4914. doi: 10.1113/JP277764
Serviente, C., Troy, L. M., de Jonge, M., Shill, D. D., Jenkins, N. T., and Witkowski, S. (2016). Endothelial and inflammatory responses to acute exercise in perimenopausal and late postmenopausal women. Am. J. Physiol. Regul. Integr. Comp. Physiol. 311, R841–R850. doi: 10.1152/ajpregu.00189.2016
Shamseer, L., Moher, D., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., et al. (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 354:i4086. doi: 10.1136/bmj.g7647
Simmons, G. H., Padilla, J., Young, C. N., Wong, B. J., Lang, J. A., Davis, M. J., et al. (2011). Increased brachial artery retrograde shear rate at exercise onset is abolished during prolonged cycling: role of thermoregulatory vasodilation. J. Appl. Physiol. 110, 389–397. doi: 10.1152/japplphysiol.00936.2010
Swift, D. L., Weltman, J. Y., Patrie, J. T., Saliba, S. A., Gaesser, G. A., Barrett, E. J., et al. (2014). Predictors of improvement in endothelial function after exercise training in a diverse sample of postmenopausal women. J. Womens Health 23, 260–266. doi: 10.1089/jwh.2013.4420
Taddei, S., Galetta, F., Virdis, A., Ghiadoni, L., Salvetti, G., Franzoni, F., et al. (2000). Physical activity prevents age-related impairment in nitric oxide availability in elderly athletes. Circulation 101, 2896–2901. doi: 10.1161/01.cir.101.25.2896
Taddei, S., Virdis, A., Ghiadoni, L., Mattei, P., Sudano, I., Bernini, G., et al. (1996). Menopause is associated with endothelial dysfunction in women. Hypertension 28, 576–582. doi: 10.1161/01.hyp.28.4.576
Teixeira-Lemos, E., Nunes, S., Teixeira, F., and Reis, F. (2011). Regular physical exercise training assists in preventing type 2 diabetes development: focus on its antioxidant and anti-inflammatory properties. Cardiovasc. Diabetol. 10, 12. doi: 10.1186/1475-2840-10-12
Thijssen, D. H. J., Bruno, R. M., van Mil, A., Holder, S. M., Faita, F., Greyling, A., et al. (2019). Expert consensus and evidence-based recommendations for the assessment of flow-mediated dilation in humans. Eur Heart J 40, 2534–2547. doi: 10.1093/eurheartj/ehz350
Tian, X. L., and Li, Y. (2014). Endothelial cell senescence and age-related vascular diseases. J. Genet. Genomics 41, 485–495. doi: 10.1016/j.jgg.2014.08.001
Tinken, T. M., Thijssen, D. H., Hopkins, N., Dawson, E. A., Cable, N. T., and Green, D. J. (2010). Shear stress mediates endothelial adaptations to exercise training in humans. Hypertension 55, 312–318. doi: 10.1161/HYPERTENSIONAHA.109.146282
Ungvari, Z., Tarantini, S., Donato, A. J., Galvan, V., and Csiszar, A. (2018). Mechanisms of vascular aging. Circ. Res. 123, 849–867. doi: 10.1161/CIRCRESAHA.118.311378
WebPlotDigitizer. (2021). E. coli. Available online at: https://automeris.io/WebPlotDigitizer/ (accessed October 27, 2021).
Xu, Y., Arora, R. C., Hiebert, B. M., Lerner, B., Szwajcer, A., McDonald, K., et al. (2014). Non-invasive endothelial function testing and the risk of adverse outcomes: a systematic review and meta-analysis. Eur. Heart J. Cardiovasc. Imaging 15, 736–746. doi: 10.1093/ehjci/jet256
Yoo, J. K., Pinto, M. M., Kim, H. K., Hwang, C. L., Lim, J., Handberg, E. M., et al. (2017). Sex impacts the flow-mediated dilation response to acute aerobic exercise in older adults. Exp. Gerontol. 91, 57–63. doi: 10.1016/j.exger.2017.02.069
Keywords: aerobic exercise, endothelial function, flow-mediated dilation, middle-aged people, elderly people
Citation: You Q, Yu L, Li G, He H and Lv Y (2022) Effects of Different Intensities and Durations of Aerobic Exercise on Vascular Endothelial Function in Middle-Aged and Elderly People: A Meta-analysis. Front. Physiol. 12:803102. doi: 10.3389/fphys.2021.803102
Received: 27 October 2021; Accepted: 06 December 2021;
Published: 21 January 2022.
Edited by:
Shunchang Li, Chengdu Sport University, ChinaCopyright © 2022 You, Yu, Li, He and Lv. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuanyuan Lv, c3VuZmxvd2VybHl5QGJzdS5lZHUuY24=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.