
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Physiol. , 19 November 2020
Sec. Integrative Physiology
Volume 11 - 2020 | https://doi.org/10.3389/fphys.2020.595005
This article is part of the Research Topic The Tribute of Physiology for the Understanding of COVID-19 Disease View all 39 articles
 Hasnae Benkirane1
Hasnae Benkirane1 Jaafar Heikel2
Jaafar Heikel2 Fatima Zahra Laamiri3
Fatima Zahra Laamiri3 Amina Bouziani1*
Amina Bouziani1* Houria Lahmam1
Houria Lahmam1 Ayoub Al-Jawaldeh4
Ayoub Al-Jawaldeh4 Noureddine El Haloui1
Noureddine El Haloui1 Khalid Ennibi5
Khalid Ennibi5 Naim Akhtar-Khan6
Naim Akhtar-Khan6 El Mostafa El Fahime7
El Mostafa El Fahime7 Majdouline Obtel8
Majdouline Obtel8 Amina Barkat9
Amina Barkat9 Hassan Aguenaou1
Hassan Aguenaou1Background: The epidemic of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), causing coronavirus disease 2019 (COVID-19), presents a significant and urgent threat to global health. This alarming viral infection, declared as pandemic by the WHO in February 2020, has resulted millions of infected patients and thousands of deaths around the world. In Morocco, despite the efforts made by the authorities, the SARS-CoV-2 continues to spread and constitutes a burden of morbidity and mortality. The objective of this study is to describe clinical characteristics of COVID-19 Moroccan patients and to establish the relationship between specific clinical symptoms, namely ageusia and/or anosmia, with these characteristics.
Methods: We performed a descriptive, non-interventional cross-sectional study analyzing data from 108 patients admitted to the VINCI clinic, Casablanca (Morocco). The database includes 39 parameters including epidemiological characteristics, anthropometric measurements and biological analyzes.
Results: The average of age of the patients was 43.80 ± 15.75 years with a sex ratio of 1:1. The mean body mass index of the patients was 25.54 ± 4.63 Kg/m2. The majority of patients had, at least, one comorbidity and among 75% symptomatic patients, about 50% had, at least, three symptoms namely, fever (40.7%), cough (39.8%), myalgia (28.7%), and anosmia and/or ageusia (20.4%). From biological analyzes, we noticed lymphopenia and an elevated protein C reactive and lactate dehydrogenases levels in 24.1, 36.1, and 35.2% of patients, respectively. A disturbance in liver function markers was observed in 15.7% of cases. For the other hemostasis parameters, high levels of prothrombin and platelets were reported in 14.6 and 14.8% of patients, respectively. Comparisons related to the presence of anosmia and/or ageusia did not show any difference for demographic and anthropometric characteristics, while a possibility of a significant difference was revealed for certain biological parameters, particularly the levels of lymphocytes, D-dimer and troponin.
Conclusion: This study provides significant findings that will be used not only to supplement previous studies carried out in Morocco in order to resume the epidemiological situation in comparison with other countries, but also to improve the quality of the diagnosis of COVID-19 patients by identifying all the symptoms of the disease and better understanding its clinical outcomes.
The world is currently experiencing an alarming epidemic called coronavirus disease 2019 (COVID-19), caused by an infectious new viral strain belonging to the coronavirus family, i.e., severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), first detected in the Wuhan district of eastern China (Lu and Stratton, 2020). Infection of this virus quickly reached all corners of the world and saturated even the most resilient health systems (Organisation mondiale de la santé (OMS), 2020). Globally, 20% of infected subjects developed a severe or critical form of the disease, with a fatality rate currently above 3%, with higher rates in the older people and in those with chronic diseases (World Health Organization, 2020a).
Common signs of SARS-CoV-2 infection are respiratory symptoms, fever, cough, myalgia, shortness of breath, sore throat, and dyspnea. In more severe cases, the infection can cause pneumonia, severe acute respiratory syndrome and kidney failure (Hussain et al., 2020). However, some people, although infected, have only very mild symptoms or remain asymptomatic (Hussain et al., 2020).
Recent reports have also demonstrated the appearance of a new symptom in COVID-19 patients, i.e., sudden loss of the sense of smell and/or taste with the absence of the common clinical viral symptoms (Lechien et al., 2020a). It is a specific sign of COVID-19 infection that was recently added, by the WHO, to the list of other symptoms (World Health Organization, 2020a). The presence of anosmia and ageusia may appear in the early stages of COVID-19 (Zhou et al., 2020a) and represent an important diagnostic tool (Lee et al., 2020). Furthermore, the loss of taste and smell varies well according to sex and age. Interestingly, these sensorial alterations were generally more prevalent in women than men and young patients compared to adults (Giacomelli et al., 2020; Lechien et al., 2020b).
In parallel to these apparent symptoms, other immunological, biochemical and biological markers have been highlighted in COVID-19 patients (Yang et al., 2020c), they generally cover inflammatory and obesity indicators (Yang et al., 2020c; Arthur et al., 2020). Therefore, old age, chronic metabolic diseases and male sex make a favorable environment for SARS-CoV-2 infection that, in turn, can trigger acute and fatal hyperinflammation, called “cytokine storm” (Xu et al., 2020b). Several hypotheses have been proposed, suggesting that the smell and/or taste dysfunction could be due to inflammation of the nasal or oral neurological tissues. However, the physiopathological mechanism of this phenomenon remains unknown (Baig et al., 2020).
Additionally, obesity which is a major risk factor of several chronic diseases, including cardiovascular complications, diabetes, cancer, kidney dysfunction, etc., is also associated with a higher risk of respiratory tract infections, and hence the virus installation. Actually, an increase in adiposity has been shown to modify the integrity of the respiratory epithelium, which could lead to dysfunction of the respiratory tract (Honce and Schultz-Cherry, 2019) with an inflammatory response resulting in immunosuppression that could promote viral infections (Khan, 2006). In term of oro-sensory perception, olfaction or taste disorders can lead to weight gain or to an aggravation of the infection by distorting the feeling of food satiation (Tomassini et al., 2017). Furthermore, body mass index (BMI) affects olfactory function (Skrandies and Zschieschang, 2015). It has been suggested that obese subjects are at high risk of SARS-CoV-2 infection because they already have a low olfactory and gustatory capacity due to obesity which will mask the decrease in taste and odor induced by SARS-CoV-2 infection (Khan et al., 2020).
Most importantly, it has been increasingly evidenced that COVID-19 patients, before showing any clinical sign related to the viral infection, exhibit a loss of chemosensory perception of smell and taste. As mentioned above, some obese subjects suffer from the loss of gustatory perception, which may be explained by the association of obesity with “low grade” inflammation, marked with high concentrations of pro-inflammatory cytokines. COVID-19 is also marked with a “inflammatory cytokine storm.” So, we decided to categorize our COVID-19 patient population as with or without this oro-naso-sensory perception to better shed light at this aspect in relation with inflammation (Khan et al., 2020).
Besides, in Morocco, the data available on coronavirus mainly focused on generalities (description of the virus, its mode of spread and diagnosis, the adopted treatments, the number of cases, etc.) (Bourhanbour and Bakkouri, 2020; Traore et al., 2020; Zoukal et al., 2020). However, further studies testing more characteristics of COVID 19 patients remain limited. Therefore, the present study aims to describe anthropometric and clinical characteristics of Moroccan patients with COVID-19 and to define differences for each parameter according to the olfactory or gustatory dysfunction. This study will also allow us to specify the part of the population most at risk (males or females, young or old population, etc.) to assess the condition of the patients studied and to study the disease’s severity in order to guide treatment and therapeutic management of patients.
This is a descriptive, non-interventional cross-sectional study. It was carried out among COVID-19 patients admitted to the VINCI clinic in Casablanca (Morocco) from 20 March to 04 June 2020.
The study, including patient monitoring and all performed analyzes, was carried out in partnership with the VINCI clinic in Casablanca, Mother and Child Health & Nutrition Research team, Faculty of Medicine and Pharmacy, Mohammed V University, Rabat, Ministry of Health as well as National Center for Scientific and Technical Research, Rabat (Morocco).
A trained medical staff of the VINCI clinic realized data collection, using a validated questionnaire by all parties involved in this study and presented as separated sections. Thus, the identity of each patient and its contact details were recorded. Likewise, measurements of anthropometric and biological parameters were carried out.
In addition, data on olfactory or gustatory dysfunction (taste and/or smell) were also collected from questions reported in a separate section and which are scored based on questionnaires already used by researchers (Mattos et al., 2019; Lechien et al., 2020a).
The data-set covers patients admitted for COVID-19 at the VINCI Clinic in Casablanca. Indeed, only information on adult patients (men and women) confirmed by a positive COVID-19 (using PCR test and CT chest) and aged 18 years or older was noted. Thus, a total of 108 patients were enrolled in this study. This represents the total number of patients who, were hospitalized at the Vinci clinic at the time of writing this article. With the lifting of confinement, the cases’ number is currently increasing. The Vinci clinic is again involved in hospitalizations.
Among patients meeting the inclusion criteria, the following steps, measures and interventions have been performed by the clinical staff in-charge:
Infection confirmation was enrolled based on PCR test and radiological examination.
PCR was carried out at Pasteur’s institute in Casablanca. Indeed, extraction of viral RNA from nasopharyngeal and oropharyngeal swabs was adopted according to the “Berlin protocol” which was developed and made available worldwide in mid-January 2020 by Professor Christian Drosten, Director of the Institute of Virology at the Charité Hospital in Berlin. This test targets the SARS-CoV-2 E and RdRp gene (Corman et al., 2020).
This examination was realized using a United UCT 528 multi-barrette scanner with use of the CORADS score and determination, by specific software, of the percentage of the reached territory.
For each participant, data was collected on age, sex and alcohol or tobacco use. Studied patients were classified into different age groups, i.e., 18–34, 35–44, 45–54, 55–64, and ≥65 years.
The anthropometric parameters were measured following the WHO measurement standards (World Health Organization, 1995). These parameters included body weight and height. The BMI was calculated as the body weight in kilogram divided by the height squared in meter. According to obtained BMI values, the participants were classified into different groups, based on the WHO reference values (World Health Organization, 1995), as follows: underweight, BMI < 18.5 Kg/m2; normal, 18.5 ≤ BMI < 25 Kg/m2; overweight, 25 ≤ BMI < 30 Kg/m2; obesity class 1, 30 ≤ BMI < 35 Kg/m2; obesity class 2, 35 ≤ BMI < 40 Kg/m2, and obesity class 3: BMI ≥ 40 Kg/m2.
During the consultation, a clinical survey was prospectively realized for each patient. Data on common symptoms associated with COVID-19 infection principally fever, cough, myalgia, headache, asthenia, pharyngitis, digestive disorders, breathing difficulties and anosmia and/or ageusia were noted. Also, the presence of any other conditions and specifically severe non-communicable diseases, such as diabetes, cardiovascular disease, dyslipidemia, high blood pressure, etc., was recorded.
Using a validated questionnaire, the anosmia and/or ageusia was/were evaluated in a specific section. This part was attributed to define the olfactory and/or gustatory dysfunction.
In the Institute Pasteur Laboratory in Casablanca, a number of biological parameters were analyzed in blood samples. On the first day of consultation and after 5 days of hospitalization, a set of biological parameter such as glycemia, hemoglobin (Hb), white blood cells (WBC), lymphocyte, prothrombin time (PT), reactive protein C (CRP), ferritin, D-dimers, aspartate aminotransferase (AST), alanine aminotransferase (ALT), gamma-glutamyl transpeptidase (GGT), troponin, creatine phosphokinase (CPK), lactate dehydrogenase (LDH) were measured for each recruited patient.
The biological analysis of these parameters was made on the basis of paraclinical examinations recommended by the national scientific commission of COVID-19. In addition to the etiological diagnosis and epidemiological surveillance, these laboratory examinations are used to monitor patients according to their cases and their comorbidities, to guide treatment and therapeutic management, and also to avoid a double bacterial infection.
Therewith, for each studied parameter, a defined diagnostic technique was used:
• Hemogram (Hb, WBC, lymphocyte): Sample: whole blood EDTA- SYSMEX flow cytometry- Reference values: adult annals clinical biology 2014-Pediatrics RFL 2009;
• Prothrombin: Sample: citrated plasma-SIEMENS Reagent (Human Thromboplastin) Sysmex CA 620 Automate
• CRP: ROCHE immunoturbidimetric technique;
• Ferritin: ROCHE Electrochemiluminescence technique;
• D-Dimers: ELFA bioMérieux automated technique;
• ASAT, ALAT, and GGT transaminases: IFCC technique 37°C ROCHE;
• Troponin: Electrochemiluminescence technique on COBAS ROCHE;
• C.P.K and LDH: Technique UV 37 ROCHE.
Statistical analysis was performed using SPSS software-version 23.0 (IBM SPSS Statistics 23.0.0.0, New York, NY, United States). Baseline characteristics and clinical features of all patients with SARS-CoV-2 infection were described, as numbers and percentages by adding confidence interval estimates for better precision. Biological parameters were also analyzed and presented as mean ± standard deviation or as medians (quartiles), and each variable was categorized into different groups (Low, normal, and high), according to the biological variations, as follows:
– Hb (Man) categorized into 2 groups: <13.4 and >13.4 g/dl;
– Hb (Woman) categorized into 2 groups: <11.5 and >13.4 g/dl;
– WBC categorized into 3 groups: <4550/mm3, 4550–11000 mm3, and 30–155 mg/l;
– CRP categorized into 3 groups: <5, 5–30, and 30–155 mg/l;
– CPK categorized into 2 groups: <190 and >190 UI/l;
– LDH categorized into 2 groups: <225 and >225 UI/l;
– Procalcitonin categorized into 2 groups: >0,5 and >0,5 ng/ml;
– AST categorized into 2 groups: <40 and >40 UI/l;
– ALT categorized into 2 groups: <41 and >41 UI/l;
– Prothrombin time categorized into 3 groups: <70, 70–130 and >130%.
The normality of the distribution was evaluated using the Kolmogorov-Smirnov (KS) test.
Between the group of patients with olfactory (or gustatory) dysfunction and those without such dysfunction, comparisons have been made according to demographic, anthropometric and biological data employing different statistical tests depending on the studied variable. The comparison of quantitative variables with normal distribution was carried out by the student t-test and when the parametric hypotheses were not satisfactory, the Mann-Whitney test was performed. Association between qualitative variables was made using the Chi-square test or Fisher’s exact test. A value of p < 0.05 was considered for all statistical analyzes.
NB: Variables with missing data < 1% (GGT gamma-glutamyltranspeptidase, procalcitonin, and troponinemia) or <5% (BMI: Body mass index) were processed after exclusion of missing data. While for CPK and D-dimer, the missing data is greater than 10%, therefore statistical comparison tests were applied on valid data.
This study is a part of an overall project on the COVID-19 pandemic which has obtained the approval from the Ethical Committee and Biomedical Research (CEBR) of the College of Medicine and Pharmacy of Mohammed V University (Rabat, Morocco). The Committee approved the inclusion of the patients’ data, provided by the VINCI clinic, in order to analyze all the data and to make the different possible correlations (Approval number: 17/20, delivered on 12/06/2020). Written informed consent was obtained from each participating patient or from their family member in the case of severe conditions.
A total of 108 patients with laboratory-confirmed COVID-19 were included in this study. The general characteristics of the population are shown in Table 1. The age of our patients ranged from 18 to 82 years with an average of 43.80 ± 15.75 years. Almost one third of the patients (27.77%) were over 55 years old and 32.4% were young patients under 35 years old. The distribution by sex was statistically similar. The mean BMI of the patients was 25.54 ± 4.63 years with extremes of 18.90 and 42.90 Kg/m2. Almost half of the patients (42.59%) were either overweight (28.8%; 95% CI: 20.2–37.5) or obese (15.4%; 95% CI: 8.7–22.1). The majority of patients neither consumed tobacco, nor alcohol. Analysis of the comorbidity profile revealed that 28.7% had, at least, one comorbidity (95% CI: 20.4–37). Diabetes and arterial hypertension were the most common comorbidities.
Analysis of Table 2, representing the distribution of patients on admission according to clinical signs, showed that 25% (95% CI: 15.7–33.3) had no clinical signs. Infection was symptomatic in three quarters of the study population (75%; 95% CI: 66.7–84.3).
Among the 81 symptomatic patients, we found that more than half (59.25%) had more than three clinical signs with a preponderance of the following signs: fever, cough, myalgia, asthenia, ageusia and anosmia. The distribution of patients according clinical signs and comorbidity was statistically similar (p = 0.177). In fact, the number of symptomatic patients was statistically higher as compared to asymptomatic patients both in the group with comorbidity (83.9 vs. 16.9%) and in the group without comorbidity (71.4 vs. 28.6%).
A minority of the patients suffered from cardiovascular disorders other than high blood pressure or chronic respiratory conditions, while nephropathy was almost absent in all of the patients.
The distribution of Covid-19 patients according to their general parameters, comorbidities and clinical signs in relation to age groups, is described in Table 3.
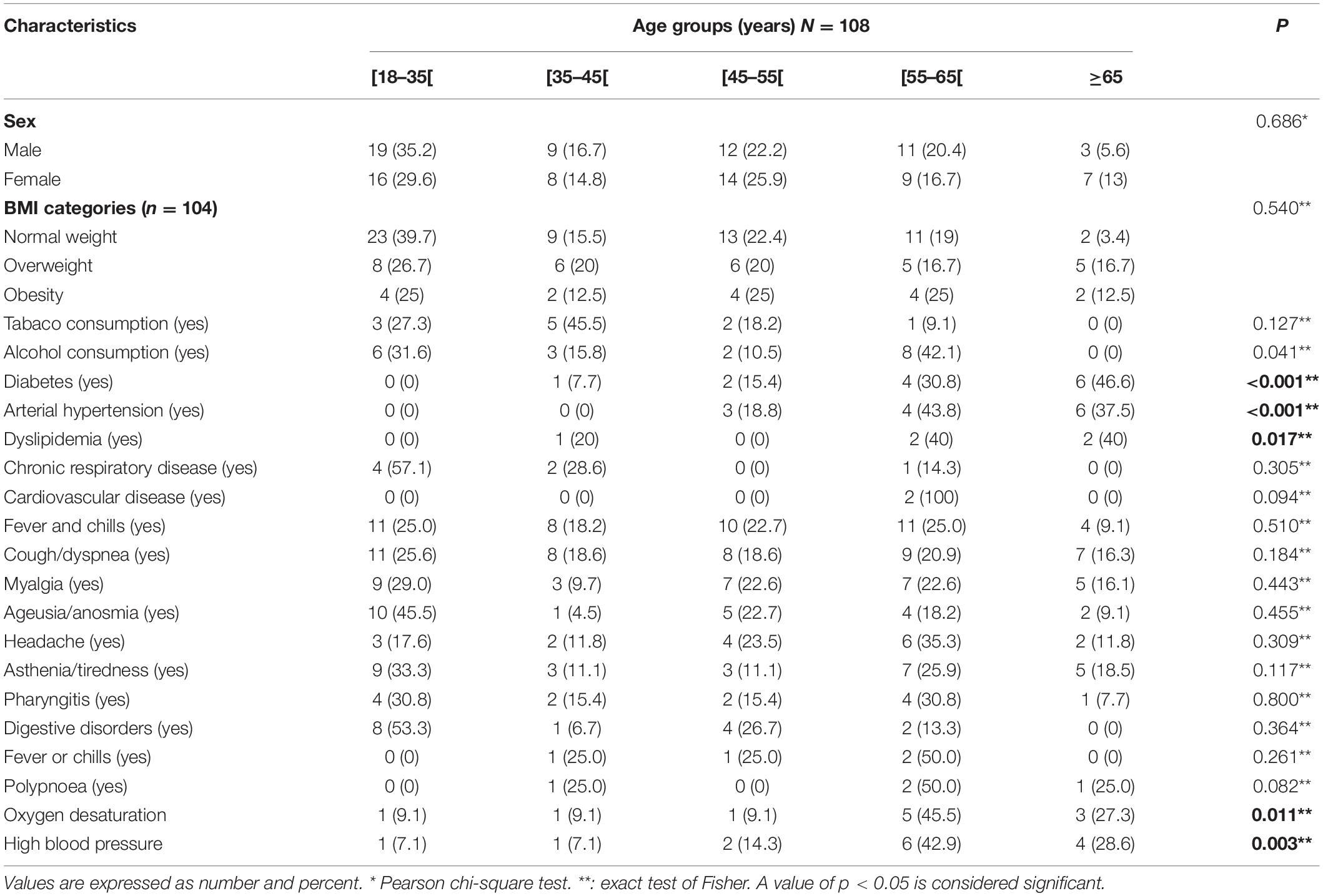
Table 3. Distribution of Covid-19 patients by age groups according to general characteristics and clinical symptoms.
Overall, the statistical analysis revealed a statistically significant difference between the age groups concerning the following variables: Alcohol (p = 0.041), diabetes (p < 0.001), dyslipidemia (p = 0.017), oxygen desaturation (p = 0.011) and high blood pressure (p = 0.003).
The distribution of patients for these main parameters was marked by high numbers, particularly for the group of participants aged between 55 and 65 years and for those aged ≥65 years.
Table 4 summarizes the main laboratory parameters of patients on admission. Analysis of the results showed hyperglycemia in 25.2% (95% CI: 17.8–34.6). WBC count were low (<4050/mm3) in 12% of cases (95% CI: 6.5–18.5), normal (4050–11000/mm3) in 81.5% of cases (95% CI: 74.1–88) and high (>11000/mm3) in only 6.5% (95% CI: 1.9–12) of cases. The lymphocyte count was below 1241/mm3 in 24.1% (95% CI: 16.7–32.4), normal in 75% (95% CI: 66.7–82.4) and above 3919/mm3 in only 0.9% (95% CI: 0–2.87) of cases. The prevalence of anemia was 11.1% (95% CI: 2.8–13.1) in men and 14.8% in women (95% CI: 5.6–25.9). Exploration of hemostasis parameters showed a disturbance of PT whose levels exceeded 100% in 14.6% (95% CI: 7.8–22.3), as well as platelets whose number was less than 161 × 103/mm3 in 14.8% (95% CI: 8.3–21.3) of cases. Our results also revealed an increase in inflammation markers, in particular CRP, which exceeded 5 mg/l, in 36.1% of cases (95% CI: 26.9–45.4), ferritin which was above 400 ng/ml in 13.9% of cases (95% CI: 7.4–20.4) and D-dimers whose increase (>500 ng/ml) was noticed in 13.2% (95% CI: 5.9–22.1) of patients. A disturbance of biological markers of hepatic function was also marked by an increase in aspartate aminotransferase (AST > 40 UI/l), alanine aminotransferase (ALT > 41 UI/l) and gamma-glutamyl transpeptidase (GGT > 60 UI/l) in 15.7% (95% CI: 9.3–23.1), 19.4% (95% CI: 12–26.9) and in 18.9% (95% CI: 11.3–26.4) of patients, respectively. In addition, our results reported a slight alteration in blood troponin and creatinine phosphokinase (CPK) which were, respectively, higher than 14 ng/l in 7.5% (95% CI: 2.8–13.1) and 190 IU/l in 7.8% (95% CI: 2.2–13.3). Furthermore, our results revealed an increase in lactate dehydrogenase (LDH) and procalcitonin (PCT) which exceeded, respectively, 225 UI/l in 35.2% (95% CI: 26.9–44.4) and 0.5 mg/ml in 2.8% (95% CI: 0–6.5) of patients.
In order to explore the demographic and anthropometric profile in the group with olfactory and/or taste dysfunction, we compared these parameters (Table 5). The comparison of the biological parameters made it possible to highlight a statistically significant difference which concerned only the number of lymphocytes, the levels of troponin and D-dimer in the blood. Indeed, we observed in the group with taste and or olfactory dysfunction compared to the group without any alteration in this function, a significantly high increase in the percentage of patients with lymphopenia (29.1% vs. 4.5%; p = 0.019), D-dimer >500 ng/ml (77.8 vs. 22.2% p = 0.002) and troponinemia >14 ng/l (18.2% vs. 4.1%; p = 0.032).
Our study aims to describe the demographic, anthropometric, clinical and biological characteristics of Moroccan COVID-19 patients. It presents a detailed analysis which complements previous Moroccan researches by analyzing different characteristics cited and possible correlations. In particular the differences of each parameter according to the olfactory or taste dysfunction were examined. In general, the results of our study show some points of similarity and others of differences with the previous studies for the different parameters. However, the present research work reports original results in relation to the symptoms like anosmia or ageusia wherein we did not observe any difference according to demographic and anthropometric characteristics. A possibility of a significant difference was noticed, however, for certain biological parameters, particularly the levels of lymphocytes, of the D-dimer and of the troponin.
We recruited 108 adult patients with a mean age of 43.80 ± 15.75 years and a sex ratio of 1:1. There was no difference in the proportion of men and women, which was inconsistent with the results of a study that have been conducted by Guan et al. (2020) who observed that men were more likely to be infected than women. The same result has been demonstrated by a Danish team (Kragholm et al., 2020).
In terms of the analysis of BMI values, we observed that almost half of the patients (44.3%) were overweight or obese (28.8 and 15.4% respectively). A similar obesity prevalence (48.3%) among COVID patients has been published by Finer et al. (2020), while, other researchers noted a high prevalence of obesity among patients with SARS-CoV-2 infection (Arthur et al., 2020; Peng et al., 2020). Furthermore, our results suggest that overweight and obesity could be risk factors for severe infection with COVID-19 in line with emerging data published in other clinical studies (Hamer et al., 2020; Sattar et al., 2020). Indeed, potential mechanisms have been linked to immune hyperresponsiveness, altered metabolic responses and pulmonary dysfunction, including a reduction in forced expiratory volume and a forced biological capacity, to the problem of overweight or obesity (Khan et al., 2020; Sattar et al., 2020). Also, lipid peroxidation is a key factor giving rise to reactive lipid aldehydes which will affect the prognosis of patients infected with SARS-CoV-2 (Demetrios et al., 2020). Physiologically, it has been shown that angiotensin converting enzyme 2 (ACE2) is the assumed receptor for the entry of SARS-CoV-2 in host cells. Given the expression level of this receptor is very high in the tissues, the possibility of risk in obese patients infected by this virus increases greatly (Zhou et al., 2020c).
In relation to comorbidities, this survey pointed out that almost a third of the population had, at least, one comorbidity with a slight dominance for diabetes and hypertension compared to the other studied comorbidities (dyslipidemia, chronic respiratory disease and cardiovascular disease). Similar results were found in a cohort of 85 patients in Wuhan, China, with first-degree diabetes followed by high blood pressure in patients presenting 68% for comorbidities (Du et al., 2020).
For non-communicable diseases, lifestyle risk factors have been consistently associated with morbidity, mortality, and loss of disease-free life years (Colpani et al., 2018; Nyberg et al., 2020; Schlesinger et al., 2020). For example, physical inactivity and smoking appear to be independently associated with a higher risk of community-acquired pneumonia and pneumonia mortality (Baik et al., 2000; Wang et al., 2014; Paulsen et al., 2017). However, the evidence from alcohol consumption and diet on the risk of respiratory infection is less clear (Paulsen et al., 2017; Hamer et al., 2019). Fortunately, most of the participants in this study were non-smokers (about 89.8%) and were not alcohol dependent (82.4%).
On the other hand, data on the characteristics of clinical complications revealed that a quarter of patients did not present any symptoms. In the symptomatic population, the predominant clinical signs were fever (40.7%), cough (39.8%), myalgia (28.7%), fatigue (25%), and anosmia and/or ageusia (20.4%). Nevertheless, high blood pressure, cardiovascular disorders and respiratory conditions were present in a limited number of our patients and nephropathy was almost absent. Such results have been reported by numerous researches studying COVID-19 patients (Wang et al., 2020; Yu et al., 2020; Zhang et al., 2020b). However, other studies observed an association between the SARS-CoV-2 infection and the elevated risk of developing diseases such as chronic kidney disease, heart disorders, diabetes, etc. (Arentz et al., 2020; Gorbalenya et al., 2020).
Regarding biological parameters, our results showed that hyperleukocytosis and lymphopenia, which represent a key indicator of infection, were noticed in some patients. In this context, numerous studies have reported that more than 80% of infected patients with SARS-CoV-2 presented these symptoms particularly lymphopenia (Mostafa et al., 2020; Yang et al., 2020c). Indeed, many researchers have revealed that in patients who died from lymphopenia, a trace of severe SARS-CoV-2 infection was confirmed. This can be explained by the death of endothelial cells due to endothelial dysfunction in certain chronic diseases which then causes excessive leakage of WBC and a disruption of the blood tissue barrier that may reflect the lymphocytes decrease found in patients with severe COVID infection (Bermejo-Martin et al., 2020). More studies have also reported that a significant increase in WBC presents a clinical worsening sign that has been shown to be significantly elevated in dead subjects (Henry et al., 2020). However, another study has found normal WBC values with lymphocyte decrease in diagnosed COVID-19 patients (Golnaz et al., 2020).
Concerning inflammatory markers, our results also detected a particular increase in CRP in 36.1% of patients with a general median value of 2.25 mg/l. Such an increase might be due to viral inflammation (Sproston and Ashworth, 2018). In our study, CRP reflected the COVID-19 pathogenesis presenting an immune response to this viral infection (Mostafa et al., 2020). In clinical laboratories, the test of this marker is currently widely used for the assessment of SARS-CoV-2 infection (Zhang et al., 2020b). For D-dimer, ferritin and LDH, as other parameters of inflammation, we also noted an increase in 13.2, 13.9, and 35.2% of cases, respectively. This finding is in line with results of previous researches which showed that blood levels of D-dimers, presenting also a sign of coagulation, were higher in severe SARS-CoV-2 infected cases (Wang et al., 2020; Yang et al., 2020b), while a study by Sun Ziyong of Huazhong University of Science and Technology in Wuhan, China, has shown that D-dimer is linked to a poor prognosis for COVID-19 patients (Tang et al., 2020b). Similarly, elevated ferritin levels could be interpreted as a sign of infection with SARS-CoV-2. In agreement with this observation, Zhou and his collaborators have also noted high ferritin levels in 200 adult patients (Zhou et al., 2020b). Indeed (Wenzhong and Hualan, 2020), based on an in silico analysis (not yet validated by peers) of the SARS-CoV-2 genome, reported the sequences encoding non-structural proteins that attack hemoglobin, in particular one of the beta chains, from which they would extract the iron atom, leading to ferritin increase in blood of COVID-19 patients.
Besides D-dimer, prothrombin and platelets are other important coagulation and thrombotic indicators commonly used in clinical laboratories for the early diagnosis of infection. Several reports have pointed out that high level of prothrombin is generally linked with the severity of the infection, of which hypercoagulation is the main result of this increase (Ling et al., 2020; Zhou et al., 2020a). Interestingly, the number of platelets has been shown to be negatively correlated with the risk of mortality in SARS-CoV-2 infected patients (Tang et al., 2020a). However, the precise mechanism by which the SARS-CoV-2 virus acts on platelet function remains unclear (Manne et al., 2020).
Additionally, the present study demonstrated a disruption of biological markers of liver function with an increase in AST, ALT and GGT transaminases, in accordance with previous studies that have shown an increase in transaminases in 25 to 35% of COVID-19 patients (Fan et al., 2020; Xu et al., 2020a; Zhang et al., 2020a; Zhou et al., 2020a).
As for the comparison of patients with and without anosmia and/or ageusia according to their demographic and anthropometric, we found no statistically significant difference between the two groups. Nevertheless, the comparison of the biological parameters revealed a significant difference between two groups with remarkable lymphopenia, a high level of D-dimer and troponemia in patients with anosmia and/or ageusia. This is in the opposite direction with the study of Hornuss et al. (2020) who reported similar clinical and laboratory test outcomes in patients with and without anosmia or hyposmia. Likewise, another study COVID-19 patients showed no difference in lymphocyte and D-dimer levels between those with peripheral nervous system disorders with loss of taste and smell as the main symptom and those without these disorders and, therefore, without anosmia or ageusia (Ling et al., 2020). These noticeable alterations in biological parameters including inflammatory (D-dimer) and immune (lymphocytes) indicators in subjects suffering from anosmia and/or ageusia can be attributed to the severity of the clinical symptoms which strongly activate the immune system, leading to a severe inflammatory (Trotier et al., 2007; Khan et al., 2020; Ling et al., 2020).
There are several limitations, linked to the current study. First, the processed data relate to a single hospital center, which does not allow conclusions to be drawn on all Moroccan patients. Secondly, with regard to the symptom of dysfunction of the senses, details on the type (olfactory or gustatory or both) and on the specificity of the total or partial loss have not been made. Thirdly, no specific test on the loss of taste and smell was performed, and these observations are derived from self-reported questionnaire. Fourth, although PCR tests can usually determine whether a person is currently infected with the Sars-Cov-2 virus, they are still not 100% accurate. Indeed, false negatives can occur with a frequency of around 30% because, within 2 weeks of exposure. Thus, this test does not determine whether people who have been exposed to SARS-CoV-2 will develop Covid-19 or not (Longokolo et al., 2020) and it is not recommended by the WHO for clinical use (Haute Autorité de Santé (HAS), 2020).
This study is the first of its kind to be conducted among Moroccan patients with SARS-CoV-2 infection. It provides important information on the demographic, anthropometric, clinical and biological characteristics of these patients. The majority of cases present the common coronavirus symptoms with remarkable disturbances in inflammatory and other biological markers as an immune response to defend against the viral infection. Thus, this is an essential work that presents the part of the Moroccan Health Department’s efforts to improve the quality of the diagnosis of COVID-19 based on the identification of all the disease symptoms. It also presents an important baseline study for future studies focusing on the possible correlations between the SARS-CoV-2 epidemic and its various symptoms, especially the olfactory and gustatory dysfunctions, considered to be as an important sign for the diagnosis of patients, especially for asymptomatic cases.
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation after terminating its exploitation for future publications.
The studies involving human participants were reviewed and approved by the Ethical Committee and Biomedical Research (CEBR) of the College of Medicine and Pharmacy of Mohammed V University (Rabat, Morocco) (Approval umber: 17/20, delivered on 12/06/2020). The patients/participants provided their written informed consent to participate in this study.
HB, HA, and NE designed, coordinated and drafted the manuscript for publication. HA had oversight responsibility over the project. JH, EE, and KE collected the data and provided laboratory analyzes. HB and HL wrote the manuscript. ABO translated the manuscript. ABA, FL, and MO analyzed the results and performed statistical analysis. HA and ABA reviewed the manuscript. AE performed the scientific review of the manuscript. NA-K contributed to the critical advice for editing the manuscript. All authors read and approved the final version of the manuscript.
The study was entirely carried out using the database provided by the VINCI clinic, which fully covered hospitalization costs of the 108 COVID patients included in this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We would to kindly thank all participants in the present study for their patience, time and consent. We also thank to health workers, medical staff of the VINCI clinic, partners, local authorities and all persons who successfully aided in the realization of this work research.
Arentz, M., Yim, E., Klaff, L., et al. (2020). Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington Statejama. JAMA 323, 1612–1614. doi: 10.1001/jama.4326
Arthur, S., Chetboun, M., Poissy, J., Raverdy, V., Noulette, J., Duhame, A., et al. (2020). High Prevalence of Obesity in Severe Acute RespiratorySyndrome Coronavirus-2 (SARS-CoV-2) Requiring Invasive Mechanical Ventilation. Obesity 28, 1195–1199. doi: 10.1002/oby.22831
Baig, A. M., Khaleeq, A., Ali, U., and Syeda, H. (2020). Evidence of the COVID-19 Virus Targeting the CNS: Tissue Distribution, Host-Virus Interaction, and Proposed Neurotropic Mechanisms. ACS Chem. Neurosci. 11, 995–998. doi: 10.1021/acschemneuro.0c00122
Baik, I., Curhan, G. C., Rimm, E. B., Bendich, A., Willett, W. C., and Fawzi, W. W. (2000). A prospective study of age and lifestyle factors in relation to community-acquired pneumonia in US men and women Arch. Intern. Med. 160, 3082–3308. doi: 10.1001/archinte.160.20.3082
Bermejo-Martin, J. F., Almansa, R., Menéndez, R., Mendez, R., Kelvin, D. J., and Torres, A. (2020). Lymphopenic community acquired pneumonia as signature of severe COVID-19 infection: Lymphopenia in severe COVID-19 infection. J. Infect. 80:e23–e24. doi: 10.1016/j.jinf.2020.02.029
Bourhanbour, A. D., and Bakkouri, J. E. (2020). Connaissances actuelles de l’immunopathologie du COVID-19. Revue marocaine de santepublique 7:10.
Colpani, V., Baena, C. P., Jaspers, L., vanDijk, G. M., and Farajzadegan, Z. (2018). Lifestyle factors, cardiovascular disease and all-cause mortality in middle-aged and elderly women: a systematic review and meta-analysis Eur. J. Epidemiol. 33, 831–845. doi: 10.1007/s10654-018-0374-z
Corman, V. M., Landt, O., Kaiser, M., Molenkamp, R., Meijer, A., Chu, D. K. W., et al. (2020). Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Eurosurveillance 25:23. doi: 10.2807/1560-7917.ES.2020.25.3.2000045
Demetrios, P., Margină, D., Tsarouhas, K., Tekos, F., Stan, M., Nikitovic, D., et al. (2020). Obesity - a risk factor for increased COVID-19 prevalence, severity and lethality. Mol. Med. Rep. 22, 9–19. doi: 10.3892/mmr.2020.11127
Du, Y., Tu, L., Zhu, P., Mu, M., Wang, R., Yang, P., et al. (2020). Clinical Features of 85 Fatal Cases of COVID-19 from Wuhan: A Retrospective Observational Study. Am. J. Respir. Crit. Care Med. 201, 1372–1379. doi: 10.1164/rccm.202003-0543oc
Fan, Z., Chen, L., Li, J., Cheng, X., Jingmao Yang, Tian, C., et al. (2020). Clinical Features of COVID-19-Related Liver Damage. Clin. Gastroenterol. Hepatol. 18, 1561–1566. doi: 10.1016/j.cgh.2020.04.002
Finer, N., Garnett, S., and Bruun, J. (2020). COVID−19 and obesity. Clin. Obesity 10:e12365. doi: 10.1111/cob.12365
Giacomelli, A., Pezzati, L., Conti, F., et al. (2020). Self-reported olfactory and taste disorders in sars-cov-2 patients: A cross-sectional study. Clin. Infect. Dis. doi: 10.1093/cid/ciaa330
Golnaz, V., Mansourian, M., Karimi, R., Ghahdarijani, K. H., Rouhi, P., Shariati, M., et al. (2020). Inflammatory markers in Covid-19 Patients: a systematic review and meta-analysis. Preprint. doi: 10.1101/2020.04.29.20084863
Gorbalenya, A. E., Baker, S. C., Baric, R. S., et al. (2020). Severe acute respiratory syndrome-related coronavirus: the species and its viruses—a statement of the Coronavirus Study Group. bioRxiv 11, Preprint. doi: 10.1101/2020.02.07.937862 (preprint).
Guan, W., Ni, Z., Hu, Y., Liang, W., Ou, C., He, J., et al. (2020). Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 382, 1708–1720. doi: 10.1056/NEJMoa2002032
Hamer, M., Kivimäki, M., Gale, C., and Batty, G. (2020). Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: A community-based cohort study of 387,109 adults in UK. Brain Behav. Immun. 87, 184–187. doi: 10.1016/j.bbi.2020.05.059
Hamer, M., O’Donovan, G., and Stamatakis, E. (2019). Lifestyle risk factors, obesity and infectious disease mortality in the general population: linkage study of 97,844 adults from England and Scotland. Prev. Med. 123, 65–70. doi: 10.1016/j.ypmed.2019.03.002
Haute Autorité de Santé (HAS) (2020). Cahier des charges définissant les modalités d’évaluation des performances des tests sérologiques détectant les anticorps dirigés contre le SARS-CoV-2. France: Haute Autorité de Santé.
Henry, B. M., de Oliveira, M. H. S., Benoit, S., Plebania, M., and Lippi, G. (2020). Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): a meta-analysis. Clin. Chem. Lab. Med. 58, 1021–1028. doi: 10.1515/cclm-2020-0369
Honce, R., and Schultz-Cherry, S. (2019). Impact of obesity on influenza a virus pathogenesis, immune response, and evolution. Front. Immunol. 10:1071. doi: 10.3389/fimmu.2019.01071
Hornuss, D., Lange, B., Schroter, N., Rieg, S., Kern, W. V., and Wagner, D. (2020). Anosmia in COVID-19 patients. Clin. Microbiol. Infect. 26, 1426–1427. doi: 10.1016/j.cmi.2020.05.017
Hussain, A., Kaler, J., Tabrez, E., Tabrez, S., and Tabrez, S. (2020). Novel COVID-19: A ComprehensiveReview of Transmission, Manifestation, and Pathogenesis. Cureus 12:e8184. doi: 10.7759/cureus.8184
Khan, A. S., Hichami, A., and Khan, N. A. (2020). Obesity and COVID-19: Oro-Naso-Sensory Perception. J. Clin. Med. 9:2158. doi: 10.3390/jcm9072158
Khan, N. A. (2006). Inflammation & Immunity: Implications in obesity and type-2 diabetes. Oilseeds Fats Crop. Lipids 13, 343–351. doi: 10.1051/ocl.2006.0047
Kragholm, K., Andersen, M., Gerds, T., Butt, J., Østergaard, L., Polcwiartek, C., et al. (2020). Association between male sex and outcomes of Coronavirus Disease 2019 (Covid-19) – a Danish nationwide, register-based study. Clin. Infect. Dis. 2020:ciaa924. doi: 10.1093/cid/ciaa924
Lechien, J. R., Chiesa-Estomba, C. M., De Siati Daniele, R., Horoi Mihaela, Le Bon, Serge, D., et al. (2020a). Olfactory and gustatory dysfonctions as a clinical presentation of mild to moderate forms of the coronavirus disease (COVID- 19): a multicenter european study. Eur. Arch. OtoRhinoLaryngol. 277, 2251–2261. doi: 10.1007/s00405-020-05965-1
Lechien, J. R., Chiesa-Estomba, C. M., Place, S., Van Laethem, Y., Cabaraux, P., Mat, Q., et al. (2020b). Clinical and Epidemiological Characteristics of 1,420 European Patients with mild-to-moderate Coronavirus Disease 2019. J. Intern. Med. 288:335–344. doi: 10.1111/joim.13089
Lee, Y., Min, P., Lee, S., and Kim, S.-W. (2020). Prevalence and Duration of Acute Loss of Smell or Taste in COVID-19 Patients. J. Kor. Med. Sci. 35:e174. doi: 10.3346/jkms.2020.35.e174
Ling, M., Jin, H., Wang, M., Hu, Y., Chen, S., He, Q., et al. (2020). Neurologic Manifestations of Hospitalized Patients With Coronavirus Disease 2019 inWuhan. China. JAMA Neurol. 77, 683–690. doi: 10.1001/jamaneurol.2020.1127
Longokolo, M.-M., Murhula, K. I., Kamwiziku, G., Ndona, M. M., Situakibanza, N. T. H., Bompeka, L. F., et al. (2020). Tests diagnostiques de l’infection à Coronavirus (COVID-19) : des atouts et des limites. Ann. Afr. Méd. 13, 3720–3726.
Lu, H., and Stratton, C. W. (2020). Outbreak of pneumonia of unknownetiology in Wuhan, China: The mystery and the miracle. J. Med. Virol. 92, 401–402. doi: 10.1002/jmv.25678
Manne, B. K., Denorme, F., Middleton, E., Portier, I., Rowley, J., Stubben, C., et al. (2020). Platelet Gene Expression and Function in COVID-19 Patients. Blood 136, 1317–1329. doi: 10.1182/blood.2020007214/1745894/blood
Mattos, J. L., Edwards, C., Schlosser, R. J., Hyer, M., Mace, J. C., Smith, T. L., et al. (2019). A brief version of the questionnaire of olfactory disorders in patients with chronic rhinosinusitis. Int. Forum Allergy Rhinol. 9, 1144–1150. doi: 10.1002/alr.22392
Mostafa, J., Bayani, M., Shokri, M., Sadeghi-Haddad-Zavareh, M., Babazadeh, A., Yeganeh, B., et al. (2020). Clinical and laboratory findings from patients with COVID-19 pneumonia in Babol North of Iran: a retrospective cohort study. Intern. Med. 0, 1–15.
Nyberg, S. T., Singh-Manoux, A., Pentti, J., Madsen, I. E. H., Sabia, S., Alfredsson, L., et al. (2020). Association of healthy lifestyle with years lived without major chronic diseases. JAMA Int. Med. 180, 760–768. doi: 10.1001/jamainternmed.2020.0618
Organisation mondiale de la santé (OMS) (2020). Maladie à coronavirus 2019 (COVID-19) : questions-réponses. Geneva: Organisation mondiale de la santé.
Paulsen, J., Askim, A., Mohus, R. M., et al. (2017). Associations of obesity and lifestyle with the risk and mortality of bloodstream infection in a general population: a 15-year follow-up of 64 027 individuals in the HUNT Study. Int. J. Epidemiol. 46, 1573–1581. doi: 10.1093/ije/dyx091
Peng, Y. D., Meng, K., Guan, H. Q., et al. (2020). Clinical characteristics and outcomesof 112 cardiovascular disease patients infected by 2019-nCoV. Zhonghua Xin Xue Guan Bing Za Zhi 48:E004.
Sattar, N. I, McInnes, B., and McMurray, J. J. V. (2020). Obesity Is a Risk Factor for Severe COVID-19 Infection. Multiple Potential Mechanisms. Circulation 142, 4–6. doi: 10.1161/CIRCULATIONAHA.120.047659
Schlesinger, S., Neuenschwander, M., Ballon, A., Nöthlings, U., and Barbaresko, J. (2020). Adherence to healthy lifestyles and incidence of diabetes and mortality among individuals with diabetes: a systematic review and meta-analysis of prospective studies J. Epidemiol. Community Health 74, 481–487. doi: 10.1136/jech-2019-213415
Skrandies, W., and Zschieschang, R. (2015). Olfactory and gustatory functions and its relation to body weight. Physiol. Behav. 142, 1–4. doi: 10.1016/j.physbeh.2015.01.024
Sproston, N. R., and Ashworth, J. J. (2018). Role of C-Reactive Protein at Sites of Inflammation and Infection. Front. Immunol. 9:754. doi: 10.3389/fimmu.2018.00754
Tang, N., Bai, H., Chen, X., Gong, J., Li, D., and Sun, Z. (2020a). Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J. Thromb. Haemost. 18, 1094–1099. doi: 10.1111/jth.14817
Tang, N., Li, D., Wang, X., and Sun, Z. (2020b). Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J. Thromb. Haemost. 18, 844–847. doi: 10.1111/jth.14768
Tomassini, B. I., Ozdener, M. H., Melis, M., Love-Gregory, L., Mitreva, M., Abumrad, N. A., et al. (2017). Variant in a common odorant-binding protein geneis associatedwith bitter sensitivity in people. Behav. Brain Res. 329, 200–204. doi: 10.1016/j.bbr.2017.05.015
Traore, B., Gladys, T. B., Samira, N., and Samira, H. (2020). COVID-19: Priseen charge therapeutique. Revue marocaine de santepublique 7:10. doi: 10.1016/s0992-5945(08)70274-5
Trotier, D., Bensimon, J. L., Herman, P., Tran, Ba, Huy, P., et al. (2007). Inflammatory obstruction of the olfactory clefts and olfactory loss in humans: a new syndrome? Chem. Senses 32, 285–292. doi: 10.1093/chemse/bjl057
Wang, D., Hu, B., Hu, C., et al. (2020). Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 323, 1061–1069. doi: 10.1001/jama.1585 published online Feb 7.
Wang, H. E., Baddley, J., Griffin, R. L., et al. (2014). Physical inactivity and long-term rates of community-acquired sepsis. Prev. Med. 65, 58–64. doi: 10.1016/j.ypmed.2014.04.017
Wenzhong, L., and Hualan, L. (2020). COVID-19: Attacks the 1-Beta Chain of Hemoglobin and Captures the Porphyrin to Inhibit Heme Metabolism. Preprint. doi: 10.26434/chemrxiv.11938173.v5
World Health Organization (1995). Physical Status: The Use and Interpretation of Anthropometry. Geneva: WHO.
World Health Organization (2020a). Coronavirus disease (COVID-19) pandemic. Geneva:World Health Organization. Available Online at: https://www. who.int/emergencies/diseases/novel-coronavirus-2019
World Health Organization (2020b). March 2020. Geneva:World Health Organization. Available Online at: https://www.who.int/health-topics/corona virus.2020
World Health Organization (2020c):mise à jour de la Stratégie covid-19. Geneva:World Health Organization. Available Online at: https://www.who.int/docs/default-source/coronaviruse/strategy-update-french.pdf?sfvrsn=b1cfe48a_2
Xu, L., Liu, J., Lu, M., Yang, D., and Zheng, X. (2020a). Liver injury during highly pathogenic human coronavirus infections. Liver Int. 40, 998–1004. doi: 10.1111/liv.14435
Xu, Z., Shi, L., Wang, Y., Zhang, J., Huang, L., Zhang, C., et al. (2020b). Pathological findingsof COVID-19 associated with acute respiratorydistress syndrome. Lancet Respir. Med. 8, 420–422. doi: 10.1016/S2213-2600(20)30076-X
Yang, A.-P., Liu, J.-P., Tao, W.-Q., and Li, H.-M. (2020a). The diagnostic and predictiverole of NLR, d-NLR and PLR in COVID-19 patients. Int. Immunopharmacol. 84:106504. doi: 10.1016/j.intimp.106504
Yang, W., Cao, Q., Qin, L., Wang, X., Cheng, Z., Pan, A., et al. (2020b). Clinical characteristics and imaging manifestations of the 2019 novel coronavirus disease (COVID-19): A multicenter study in Wenzhou city, Zhejiang, China. J. Infect. 80, 388–393. doi: 10.1016/j.jinf.2020.02.016
Yang, X., Yu, Y., Xu, J., SHu, H., Liu, H., Wu, Y., et al. (2020c). Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir. Med. 8, 475–481. doi: 10.1016/s2213-2600(20)30079-5
Yu, P., Zhu, J., Zhang, Z., Han, Y., and Huang, L. (2020). A familial cluster of infection associated with the 2019 novel coronavirus indicating potential person-to-person transmission during the incubation period. J. Infect. Dis. 221, 1757–1761. doi: 10.1093/infdis/jiaa077
Zhang, J., Zhou, L., Yang, Y., Peng, W., Wang, W., and Chen, X. (2020b). Therapeutic and triagestrategies for 2019 novel coronavirus disease in fever clinics. Lancet Respir. Med. 8, 11–12e. doi: 10.1016/S2213-2600(20)30071-0
Zhang, J.-J., Dong, X., Cao, Y.-Y., Yuan, Y.-D., Yang, Y.-B., Yan, Y.-Q., et al. (2020a). Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Epidemiol. Genet. 75, 1730–1741. doi: 10.1111/all.14238
Zhou, F., Yu, T., Du, R., Fan, G., Liu, Y., Liu, Z., et al. (2020a). Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan. China: a retrospective cohort study. Lancet 395, 1054–1062. doi: 10.1016/s0140-6736(20)30566-3
Zhou, M., Zhang, X., and Qu, J. (2020b). Coronavirus disease 2019 (covid-19): A clinical update. Front. Med. 14, 126–135. doi: 10.1007/s11684-020-0767-8
Zhou, P., Yang, X., Wang, X., et al. (2020c). A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 579, 270–273. doi: 10.1038/s41586-020-2012-7
Keywords: ageusia, anosmia, biological, epidemiological, demographic characteristics, Moroccan patients, COVID-19
Citation: Benkirane H, Heikel J, Laamiri FZ, Bouziani A, Lahmam H, Al-Jawaldeh A, El Haloui N, Ennibi K, Akhtar-Khan N, El Fahime EM, Obtel M, Barkat A and Aguenaou H (2020) Study of Clinical and Biological Characteristics of Moroccan Covid-19 Patients With and Without Olfactory and/or Gustatory Dysfunction. Front. Physiol. 11:595005. doi: 10.3389/fphys.2020.595005
Received: 14 August 2020; Accepted: 20 October 2020;
Published: 19 November 2020.
Edited by:
Denis Noble, University of Oxford, United KingdomReviewed by:
Hamid Reza Marateb, Universitat Politecnica de Catalunya, SpainCopyright © 2020 Benkirane, Heikel, Laamiri, Bouziani, Lahmam, Al-Jawaldeh, El Haloui, Ennibi, Akhtar-Khan, El Fahime, Obtel, Barkat and Aguenaou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Amina Bouziani, YW1pbmEuYm91emlhbmlAdWl0LmFjLm1h
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.