
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Physiol., 09 December 2020
Sec. Redox Physiology
Volume 11 - 2020 | https://doi.org/10.3389/fphys.2020.588553
This article is part of the Research TopicCigarette Smoke, E-Cigarette/E-Vaping and COVID-19: Risks and Implications in This New EraView all 13 articles
 Mengyuan Dai1,2,3†
Mengyuan Dai1,2,3† Liyuan Tao4†
Liyuan Tao4† Zhen Chen5†
Zhen Chen5† Zhi Tian6†
Zhi Tian6† Xiaofang Guo7
Xiaofang Guo7 Diane S. Allen-Gipson6,8
Diane S. Allen-Gipson6,8 Ruirong Tan9
Ruirong Tan9 Rui Li9,10
Rui Li9,10 Li Chai11
Li Chai11 Fen Ai5*
Fen Ai5* Miao Liu11*
Miao Liu11*Background: The recent emergence and rapid global spread of coronavirus disease 2019 (COVID-19) is leading to public health crises worldwide. Alcohol consumption and cigarette smoking (CS) are two known risk factors in many diseases including respiratory infections.
Methods: We performed a multi-center study in the four largest hospitals designated for COVID-19 patients in Wuhan. There are totally 1547 patients diagnosed with COVID-19 enrolled in the study, alcohol consumption and CS history were evaluated among these patients. The epidemiology, laboratory findings and outcomes of patients contracted COVID-19 were further studied.
Results: Our findings indicated that COVID-19 patients with a history of CS tend to have more severe outcomes than non-smoking patients. However, alcohol consumption did not reveal significant effects on neither development of severe illness nor death rates in COVID-19 patients.
Conclusion: CS is a risk factor for developing severe illness and increasing mortality during the SARS-CoV-2 infection. We believe that our findings will provide a better understanding on the effects of alcohol intake and CS exposure in COVID-19 patients.
The recent emergence and rapid global spread of Severe Acute Respiratory Syndrome (SARS) Coronavirus 2 (SARS-CoV-2) and the resulting coronavirus disease 2019 (COVID-19) is associated with more than 12,077,210 cases and more than 550,327 deaths worldwide as of July 9, 2020 (COVID-19 Map from Johns Hopkins Coronavirus Resource Center). Considering the high rate of SARS-CoV-2 transmission and that there is no known cure for this disease at present, identifying vulnerable populations will be crucial for taking measures to protect those who are at increased risk of infection or of severe disease from COVID-19 (Clark et al., 2020).
Alcohol consumption and cigarette smoking (CS) are two known risk factors in many diseases including respiratory infections (Traphagen et al., 2015; Han et al., 2019). Chronic alcohol consumption has been identified as an important risk factor for the development of acute respiratory distress syndrome (ARDS) (Moss et al., 2003), which is one of the most severe complications of COVID-19. CS has been well-recognized as a high-risk factor for respiratory diseases; however, there is still no evidence indicating that it increases the risk of SARS-CoV-2 infection. Even though there are numerous studies focused on the link between smoking and COVID-19, it is still unclear whether CS increases the severity of COVID-19. A meta-analysis conducted by Vardavas and Nikitara (2020) suggested that smoking increases the risk of developing severe COVID-19; however, another meta-analysis demonstrated that active smoking is not associated with enhanced risk in the progressing to severe COVID-19 (Lippi and Henry, 2020). There even are data indicate that smoking might have protective properties against SARS-CoV-2 (Farsalinos et al., 2020b; van Zyl-Smit et al., 2020). The challenge of studies focused on smoking and COVID-19 is that most hospitalized patients have underlying medical conditions such as hypertension, diabetes, cardiovascular disease and chronic obstructive pulmonary disease (COPD).
Our multi-center study was performed in the four largest hospitals designated for COVID-19 patients in Wuhan. All hospitalized patients were confirmed COVID-19 positive according to the interim guidance from the World Health Organization and National Health Commission of China (World Health Organization, 2020), from February 01 to April 10, 2020. The severe illness was defined according to the New Coronavirus Pneumonia Prevention and Control Program (5th edition) issued by the National Health Commission of China (Supplementary Methods). The study was approved by the institutional ethics review board and the need for informed consent was waived.
Clinical course, laboratory findings and outcomes were obtained and reviewed. The medical records were analyzed by three investigators independently. Information included demographic characteristics, symptoms, signs, underlying comorbid conditions and treatments were collected from the medical records. Laboratory data on the day of admission were collected. Smoking history was defined according to the WHO guidelines, including smoking for more than 6 months, or smoking more than 5 or more cigarettes per day (US Department of Health and Human Services, 2014); alcohol consumption was defined as an average of more than 7 standard drinks per week or more than 3 standard drinks per day (1 standard drink = 14 g of ethanol) (Burton and Sherons, 2018).
Categorical variables were described as frequency rates and percentages. Continuous variables were presented as mean ± standard deviation (SD) or mean, and interquartile range (IQR) as appropriately. We used the Mann–Whitney U test, x2 test, or Student’s t-test to compare differences between two different groups where appropriate. Univariable and multivariable logistic regression analyses were used to identify any association between serious illness and smoking history. Univariable and multivariable cox regression analyses were used to identify any association between death and smoking history. Variables with a P-value less than 0.05 at univariable analysis were subjected to multivariable analysis, and odds ratios with 95% confidence intervals (CIs) were reported. The areas under the receiver operating characteristic curve were used to evaluate the discriminative abilities of the disease severity status. P-values less than 0.05 were considered to indicate statistical significance. Statistical analyses were performed by using statistical software (SPSS version 26.0).
A total of 1547 subjects, including 802 male patients (51.8%) and 745 female patients (48.2%), were enrolled in the study. According to past medical history, the most common concurrent diseases were hypertension (27.34%), diabetes (12.93%) and cardiovascular disease (10.92%) (Supplementary Table 1). Among 1547 patients, there are 390 severe patients (25.21%), and 257 death patients (16.61%).
Firstly, the population was divided into sub-groups according to whether they had a history of smoking. In the smoking group, the proportion of males was higher than that in the non-smoking group (87.59% vs. 48.15%, p < 0.001). There was no statistically significant difference in age, BMI, comorbidities and symptoms between the smoking group and the non-smoking group. However, in terms of biochemical indicators, the counts of lymphocyte and thrombocyte of the smoking group were lower than that of the non-smoking group, while C-reactive protein and AST were higher than that of the non-smoking group. The difference was statistically significant (all p-values < 0.05, Table 1). To further describe the effects of smoking, we conducted a Kaplan-Meier survival curves for COVID-19 patients. The results revealed that the smoking groups had greater deteriorated outcomes than the non-smoking groups (Figure 1).
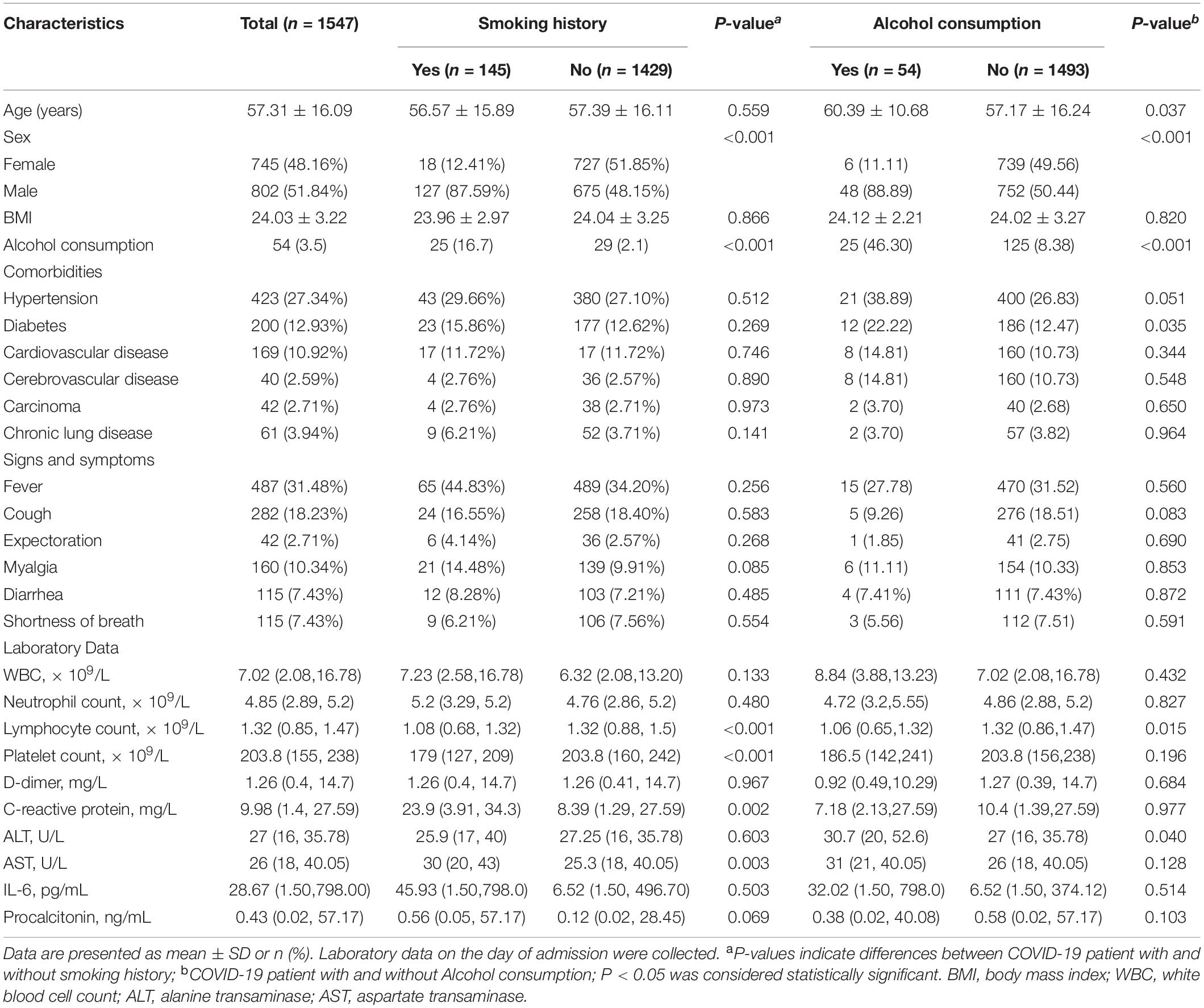
Table 1. Characteristics of patients with COVID-19 with and without smoking history and alcohol consumption.
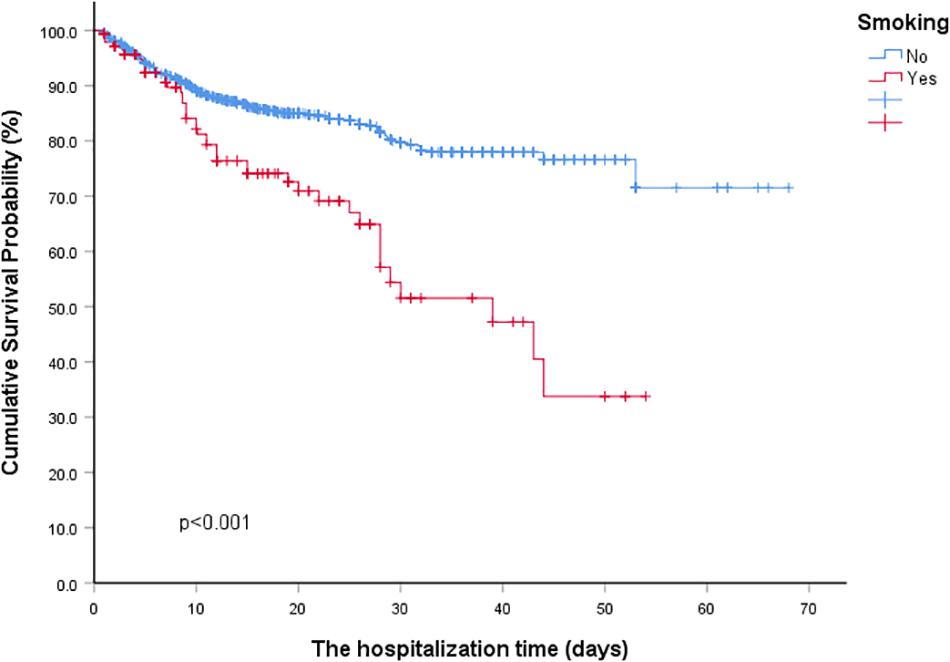
Figure 1. Kaplan-Meier survival curves for COVID-19 patients with and without Smoking history. *P < 0.01 for smoking group vs. non-smoking group.
Within the same population, two groups were divided according to whether they had a history of alcohol consumption. The proportion of males in the alcohol group was higher than that in the non-alcohol group (88.89% vs. 50.44%, p < 0.001). There was no statistically significant difference in age and BMI. Concerning comorbidities and symptoms upon admission, COVID-19 patients with and without alcohol consumption were similar except for a higher proportion of diabetes (22.22% vs. 12.47%, p = 0.035). In terms of laboratory indicators, the counts of lymphocyte from the alcohol group were lower than that of the non-alcohol group, while ALT was higher than that of the non-alcohol group. The difference was statistically significant (p < 0.05, Table 1). The Odds Ratio (OR) for the effect of CS on severe illness was 1.910 (95% CI = 1.203–3.033, p = 0.001), indicating that the risk of severe illness in patients with previous CS history was 1.91 times higher than that in non-smokers.
However, in both univariable and multivariable analyses, alcohol consumption did not reveal any significant effect on developing severe illness in COVID-19 patients (Table 2). Among them, CS had a Hazard Ratios (HR) = 1.825 (95% CI = 1.275-2.613, p = 0.001), indicating that the risk of death in smokers was 1.825 times higher than that in non-smokers. Also, lymphocyte count, C-reactive protein, and ALT were risk factors for death. However, alcohol consumption did not show a significant effect on death rates of COVID-19 patients in both univariable and multivariable analyses (Table 3). In this study, we analyzed the association between alcohol consumption, CS, and the risk of COVID-19. Our findings indicated that COVID-19 patients with a history of CS tend to have more severe outcomes than non-smoking patients. However, alcohol consumption did not reveal significant effects on neither development of severe illness nor death rates in COVID-19 patients.
Alcohol is the most commonly abused drug in the world. It affects almost every organ of our body. At this time, patients with a history of alcohol consumption did not develop more severe outcomes compared to patients without. That might be because the time we collect our data is still in the early stage of the pandemic. With the SARS-CoV-2 rapidly spreading, governments across the world have issued stay-at-home and face covering orders, which resulted in trillions of people being isolated from each other for long periods of time. Combining with the stress of rising unemployment, excessive use of alcohol consumption becomes a public health crisis (Clay and Parker, 2020). Several meta-analyses suggested that there is a significant association between COVID-19 and CS; however, they also admitted their analyses were limited by sample size and number of primary researches (Farsalinos et al., 2020a). In our study, the counts of lymphocyte of the smoking group were lower than that of the non-smoking group, which may contribute to the deteriorated outcomes. Immunosuppression caused by smoking inhibits the effective activation of T cells, which also inhibit B cells to proliferate and produce antibodies, thus making humoral immunity incapable (McBride et al., 2003). C-reactive protein is positively correlated with smoking. Increased inflammatory in COVID-19 patients with smoking history could contribute to the worse outcome in this subpopulation (Chen et al., 2020). Studies have shown that smoking may increase multiple enzymes in the human liver. Cirrhosis of the liver has a recognized immune dysfunction status that includes immunodeficiency and systemic inflammation, making it reasonable for those patients to be more susceptible to SARS-CoV-2 infection (Velarde-Ruiz Velasco et al., 2020). In this study, the data we collected containing a total of 1,547 patients with 150 smokers, which will provide a better understanding of the effects of CS in COVID-19. Based on our analysis, COVID-19 patients with a history of CS had more severe outcomes when compared to the population without a CS history.
In conclusion, CS is a risk factor for developing severe illness and increasing mortality during the SARS-CoV-2 infection. We believe that our findings will provide a better understanding on the effects of alcohol intake and CS exposure in COVID-19 patients.
ML designed the research. MD and ZC were in charge of data collection and manuscript writing. All authors contributed to the article and approved the submitted version.
The study was supported by the National Natural Science Foundation of China 82002770 (to MD) and Xiu Research Fund (to LC).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphys.2020.588553/full#supplementary-material
Burton, R., and Sherons, N. (2018). Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 392, 987–988.
Chen, N., Zhou, M., Dong, X., Qu, J., Gong, F., Han, Y., et al. (2020). Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 395, 507–513. doi: 10.1016/s0140-6736(20)30211-7
Clark, A., Jit, M., Warren-Gash, C., Guthrie, B., Wang, H. H. X., Mercer, S. W., et al. (2020). Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study. Lancet Glob Health 8, e1003–e1017.
Clay, J. M., and Parker, M. O. (2020). Alcohol use and misuse during the COVID-19 pandemic: a potential public health crisis? Lancet Public Health 5:e259. doi: 10.1016/s2468-2667(20)30088-8
Farsalinos, K., Barbouni, A., Poulas, K., Polosa, R., Caponnetto, P., and Niaura, R. (2020a). Current smoking, former smoking, and adverse outcome among hospitalized COVID-19 patients: a systematic review and meta-analysis. Ther Adv Chronic Dis 11:2040622320935765.
Farsalinos, K., Niaura, R., Le, Houezec J, Barbouni, A., Tsatsakis, A., Kouretas, D., et al. (2020b). Editorial: Nicotine and SARS-CoV-2: COVID-19 may be a disease of the nicotinic cholinergic system. Toxicol Rep 7, 658–663. doi: 10.1016/j.toxrep.2020.04.012
Han, L., Ran, J., Mak, Y. W., Suen, L. K., Lee, P. H., Peiris, J. S. M., et al. (2019). Smoking and Influenza-associated Morbidity and Mortality: A Systematic Review and Meta-analysis. Epidemiology 30, 405–417. doi: 10.1097/ede.0000000000000984
Lippi, G., and Henry, B. M. (2020). Active smoking is not associated with severity of coronavirus disease 2019 (COVID-19). Eur J Intern Med 75, 107–108. doi: 10.1016/j.ejim.2020.03.014
McBride, C. M., Emmons, K. M., and Lipkus, I. M. (2003). Understanding the potential of teachable moments : the case of smoking cessation. Health Educ Res 18, 156–170. doi: 10.1093/her/18.2.156
Moss, M., Parsons, P. E., Steinberg, K. P., Hudson, L. D., Guidot, D. M., Burnham, E. L., et al. (2003). Chronic alcohol abuse is associated with an increased incidence of acute respiratory distress syndrome and severity of multiple organ dysfunction in patients with septic shock. Crit. Care Med. 31, 869–877. doi: 10.1097/01.ccm.0000055389.64497.11
Traphagen, N., Tian, Z., and Allen-Gipson, D. (2015). Chronic Ethanol Exposure: Pathogenesis of Pulmonary Disease and Dysfunction. Biomolecules 5, 2840–2853. doi: 10.3390/biom5042840
US Department of Health and Human Services (2014). The health consequences of smoking—50 years of progress: a report of the Surgeon General. Atlanta, GA.: US Department of Health and Human Services.
van Zyl-Smit, R. N., Richards, G., and Leone, F. T. (2020). Tobacco smoking and COVID-19 infection. Lancet Respir Med 8, 664–665. doi: 10.1016/s2213-2600(20)30239-3
Vardavas, C. I., and Nikitara, K. (2020). COVID-19 and smoking: A systematic review of the evidence. Tob Induc Dis 18:20.
Velarde-Ruiz Velasco, J. A., García-Jiménez, E. S., and Remes-Troche, J. M. (2020). Hepatic manifestations and impact of COVID-19 on the cirrhotic patient. Rev Gastroenterol Mex 85, 303–311. doi: 10.1016/j.rgmxen.2020.05.002
World Health Organization (2020). Clinical management of severe acute respiratory infection when novel coronavirus (2019-nCoV) infection is suspected: interim guidance. Available Online at: https://apps.who.int/iris/handle/10665/330893. [January 28, 2020].
Keywords: cigarette, alcohol, COVID-19, SARS-CoV-2, severity, death
Citation: Dai M, Tao L, Chen Z, Tian Z, Guo X, Allen-Gipson DS, Tan R, Li R, Chai L, Ai F and Liu M (2020) Influence of Cigarettes and Alcohol on the Severity and Death of COVID-19: A Multicenter Retrospective Study in Wuhan, China. Front. Physiol. 11:588553. doi: 10.3389/fphys.2020.588553
Received: 29 July 2020; Accepted: 13 November 2020;
Published: 09 December 2020.
Edited by:
Xiaofeng Yang, Lewis Katz School of Medicine at Temple University, United StatesReviewed by:
Xiao Huang, Second Affiliated Hospital of Nanchang University, ChinaCopyright © 2020 Dai, Tao, Chen, Tian, Guo, Allen-Gipson, Tan, Li, Chai, Ai and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Miao Liu, bWxpdTBAYndoLmhhcnZhcmQuZWR1; Fen Ai, YWlmZW5fMTAyMkAxNjMuY29t
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.